This article evaluates barriers to cancer research among oncology trainees in one of the first clinical oncology training programs in East Africa.
Keywords: Research training, Oncology, Africa
Abstract
Background.
East Africa is one of the fastest growing regions in the world and faces a rising burden of cancer; however, few people are equipped to effectively conduct research in this area.
Materials and Methods.
A 31‐item questionnaire was distributed to current trainees and recent graduates of the Master in Medicine in Clinical Oncology Program at Muhimbili University of Health and Allied Sciences in Tanzania. Areas that were assessed included (a) demographic information, (b) prior research training, (c) prior and current research activities, (d) attitudes toward the importance of research, and (e) supports and barriers to inclusion of research in an oncology career path.
Results.
A total of 30 individuals responded to the survey, of whom 53% (n = 16) were male and 70% (n = 21) identified as current trainees. Among the majority of respondents, attitudes toward research were strongly favorable. Although only 37% (n = 11) reported receiving any formal training in research methodology, 87% (n = 26) reported intentions to incorporate research into their careers. The absence of protected time for research and lack of access to research funding opportunities were identified by a majority of respondents as critical barriers.
Conclusion.
A majority of current or recent oncology trainees in Tanzania desire to incorporate research into their careers, but most also lack adequate training in research methodology and longitudinal mentorship. Our future collaboration will focus on creation of appropriate research training curriculums and fostering an environment that catalyzes interprofessional development and transforms and extends context‐specific cancer research in East Africa.
Implications for Practice.
Current and recent oncology trainees in East Africa expressed a high enthusiasm for research, driven by a sense of urgency related to the burden from cancer that the region faces. This highlights the need for cancer research training and mentorship in this setting. This work hypothesizes that African principal investigators can operate effectively if proper attention is given to selection and provision of high‐quality foundational didactic training to learn the theory and implementation of research as well as to the development of an environment conducive to mentoring.
摘要
背景。东非是世界上发展最快的地区之一,同时面临着日益加重的癌症负担;但是,很少有人能够有效地开展这一领域的研究。
材料和方法。我们向坦桑尼亚穆希比利卫生和相关科学大学 (Muhimbili University of Health and Allied Sciences) 临床肿瘤学项目的当期学员和新近医学硕士毕业生分发了一份由 31 个问题组成的调查问卷。评估领域包括 (a) 人口统计信息,(b) 之前的研究培训,(c) 之前和当前的研究活动,(d) 对研究重要性的态度,以及 (e) 将研究纳入肿瘤学职业道路所获得的支持和面临的障碍。
结果。共有 30 人参与了该调查,其中,53% (n = 16) 为男性,70% (n = 21) 被确定为当期学员。大多数受访者对研究持强烈支持的态度。虽然只有 37% (n = 11) 的受访者报告曾接受过正式的研究方法培训,但有 87% (n = 26) 的受访者报告其有意在其职业生涯中从事研究工作。大多数受访者认为,缺乏受保护的研究时间和研究资助的机会是面临的主要 障碍。
结论。坦桑尼亚当期或新近的大多数肿瘤学学员都希望在其职业生涯中从事研究工作,但大多数人还缺乏足够的研究方法和纵向指导方面的培训。我们未来的合作将侧重于建立适当的研究培训课程,培养促进跨专业发展的环境,并改革和扩展东非特定背景下的癌症研究。
实践意义:受该地区面临的癌症负担所带来的紧迫感的影响,东非当期和新近肿瘤学学员表达了对研究的高度热情。这种热情更彰显了在这种环境下,人们对癌症研究培训和指导的迫切需求。这项工作假设,如果对高质量基础教学培训的选择和提供给予适当的重视,以学习研究理论和实施并发展有利于进行指导的环境,非洲的主要研究人员便可以有效工作。
Introduction
Africa is facing unprecedented growth in cancer burden and is inadequately prepared to meet this public health challenge. By 2030, 1.27 million new cancer cases per year are expected, with approximately 1 million expected deaths [1].
In 2011, ministers of health for countries in the World Health Organization African Region affirmed their awareness of this mounting disease burden by adopting the Brazzaville Declaration on Non‐communicable Diseases Prevention and Control [2]. The signatories to this declaration agreed to develop strategies for prevention and control to strengthen health systems and reduce noncommunicable disease (NCD) burden, to source finances necessary to fight NCDs, and to enable national health information systems to generate data on risk factors and on disease burden from NCDs. However, progress in the development of evidence‐based cancer control strategies has been slow since this declaration and has been outpaced by the increasing severity of the problem.
Over the past 2 decades, institutions in sub‐Saharan Africa have made remarkable progress in building human research capacity. However, most research has focused on infectious diseases, with little attention to noncommunicable diseases, including cancer [3]. In the context of limited prevention and health care resources in Africa, it is imperative to formulate cancer control policies that are evidence‐based and targeted to cancers with the highest incidence, morbidity, and mortality rates in the local region [4]. However, there are many factors, including the scarcity of trained health professionals, differences in the infrastructure for clinical care, and unique cancer epidemiology, that pose challenges for extrapolating clinical trial and other data from oncology research performed in resource‐rich settings [5]. Research conducted by those closest to care delivery will ultimately be necessary to address the etiology of cancers unique to East Africa and to develop locally appropriate strategies to prevent and treat cancers. Thus, it will be necessary to equip oncologists who practice in resource‐constrained settings with research skills and longitudinal mentorship to enable them to perform high‐quality cancer research that is relevant to the context in which they provide care.
With a population of more than 150 million in 2014, East Africa is one of the fastest growing regions in the world [6]. The rapid growth and projections for increased cancer burden related to industrialization and changes in dietary and lifestyle patterns pose challenges that demand the development of research skills and capacity to address the needs of the region [7]. To tackle the growing burden of cancer, the region requires competent, well‐trained African researchers with supportive infrastructure and environments to enable generation of local evidence by local investigators to inform cancer control planning.
Currently, oncology is a nascent medical specialty in East Africa, and very few individuals are equipped with both the clinical training and research skills to effectively conduct research in this area. The Master of Medicine (MMed) in Clinical Oncology program at Muhimbili University of Health and Allied Sciences (MUHAS) is one of the first programs in East Africa to train doctors to become specialists in clinical oncology, combining training in radiation and medical oncology at the Ocean Road Cancer Institute (ORCI) in Dar es Salaam, Tanzania. Since its inception in 2010, it has emerged as an oncology training hub for the East African region and beyond. Current international oncology trainees at MUHAS originate from Rwanda, Ethiopia, Kenya, Comoros Islands, the Democratic Republic of Congo, and Nigeria, all of whom will return to practice oncology in their home countries as part of a new cadre of oncology leaders in East Africa. In light of the critical need to improve research training and ultimately increase cancer‐related research output among oncologists in East Africa, we sought to evaluate the attitudes and barriers toward research among current and recent oncology trainees at a regional training hub in East Africa.
Materials and Methods
Study Design and Population
A descriptive cross‐sectional study was conducted in February 2018 targeting current trainees and recent graduates of the MMed in Clinical Oncology Program at MUHAS (n = 34).
Data Collection
We adapted a 31‐item questionnaire, which has been used to assess attitudes and barriers to conducting research in other medical subspecialty training programs [4], [5], to focus on oncology research. Areas that were assessed included (a) demographic information, (b) prior research training, (c) prior and current research activities, (d) attitudes toward the importance of research, and (e) supports and barriers to inclusion of research in an oncology career path. Attitudes toward the importance of research were scored on a five‐point Likert scale (1 = strongly agree; 5 = strongly disagree).
After informed consent was provided, an electronic questionnaire was sent out to all participants in English, which is the language of the medical school curriculum and the common language in this multinational group of current and recent trainees. Participants entered deidentified responses directly into Research Electronic Data Capture, a secure web‐based application for data storage.
Statistical Analysis
Descriptive statistics were used to summarize the level of knowledge, attitude, and research practice among the study participants. Categorical variables were presented as both totals and percentages. Continuous variables were presented with median values and ranges. Fisher's exact tests were performed to evaluate associations between demographic characteristics, including gender, nationality, and rank (trainee vs. faculty), with particular attitudes and barriers. All analysis was performed with Stata statistical software version 15 [8].
Ethical Considerations
The study was considered exempt from review by both the MUHAS Institutional Review Board and the University of California, San Francisco Committee for Human Research (IRB 17‐23670) because of minimal risk to participants. All participants provided written informed consent prior to completing the survey.
Results
Out of 34 current trainees and recent graduates that were invited to participate, the overall response rate was 88% (n = 30), of whom 53% (n = 16) were male, 70% (n = 21) were current trainees, and 53% (n = 16) originated from Tanzania. Demographic characteristics, research experiences, and career aspirations of the 30 respondents are summarized in Table 1. Respondents who identified as currently in a faculty role were more likely to be of Tanzanian nationality (50% vs. 7%, p = .01).
Table 1. Demographic characteristics, research experiences, and career aspirations of oncology trainees and recent graduates of a clinical oncology training program in Tanzania (n = 30).
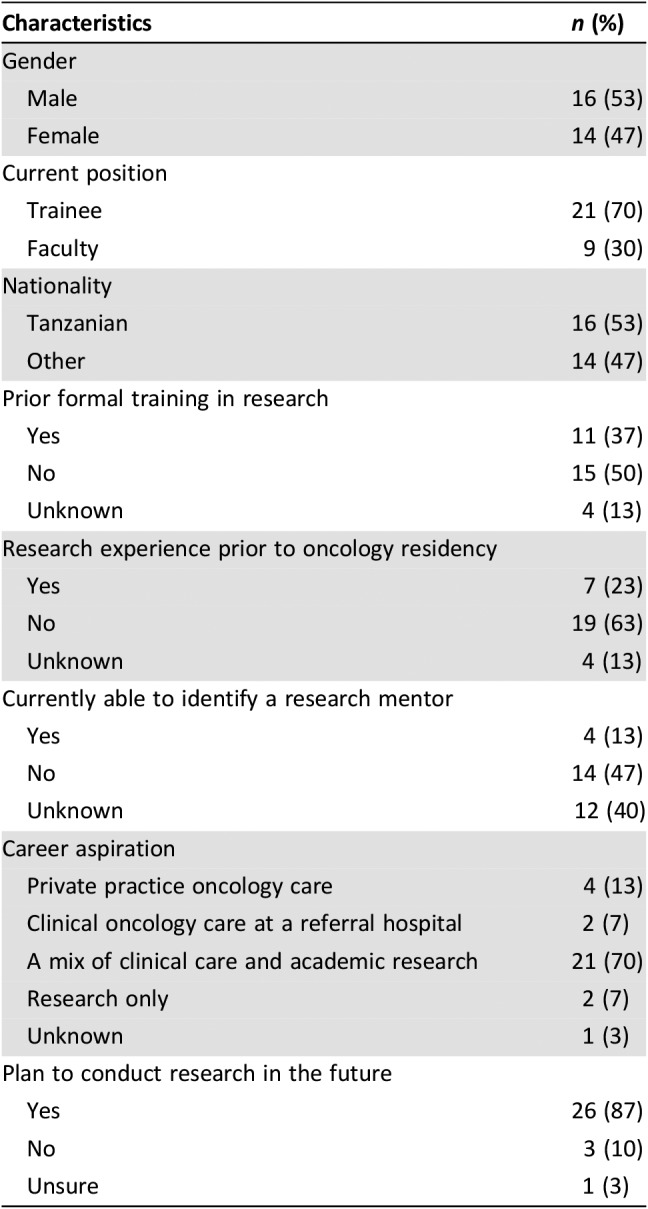
Of 30 respondents, 37% (n = 11) reported receiving some form of dedicated research training prior or in addition to the training provided during the MMed in Clinical Oncology curriculum; seven individuals reported prior completion of a master's degree (M.Sc. or M.P.H.), and four reported completion of research coursework in a nondegree program. Among seven respondents who reported that they began doing research prior to beginning their oncology training, six reported that the prior research resulted in a publication. Among practicing faculty, the median time in practice was 4 years (range: 1–5 years). Respondents who identified as current faculty oncologists at ORCI were less likely to report prior research experience, compared with respondents who identified as current trainees (0% vs. 39%; p = .04). Of the 18 respondents who responded to a question about existing mentorship, 22% (n = 4) identified as having a relationship with a research mentor.
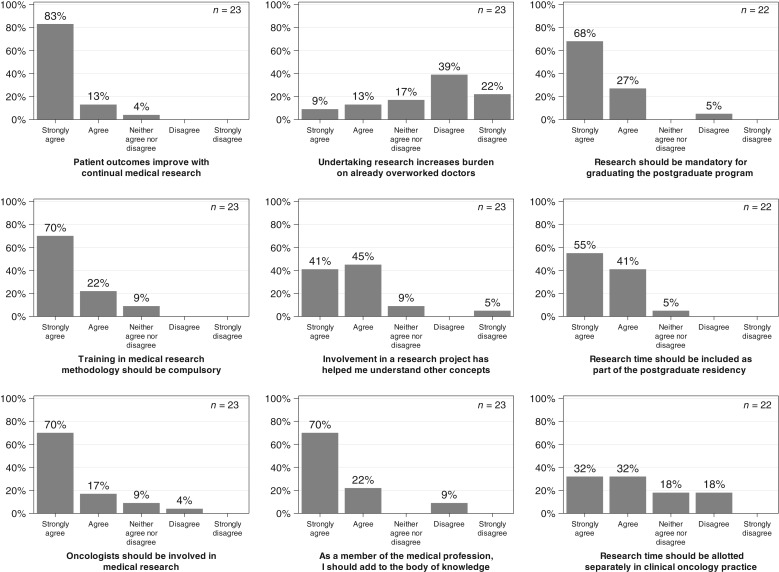
A total of 23 respondents completed all or most questions regarding their attitudes toward research, which are summarized in Figure 1. Respondents of Tanzanian nationality were more likely to disagree with the statement that research increases burden, compared with respondents of other nationalities (85% vs. 30%; p = .01). There were no other statistically significant differences in demographic characteristics, background, opinions on the impact of research, or opinions on mentorship between respondents of Tanzanian origin versus other nationalities or between researchers who are faculty versus current residents. There were no statistically significant differences in background, opinions related to the impact of research, or opinions on mentorship between female and male respondents.
Figure 1.
Self‐reported attitudes toward research among current and recent oncology trainees in Tanzania.
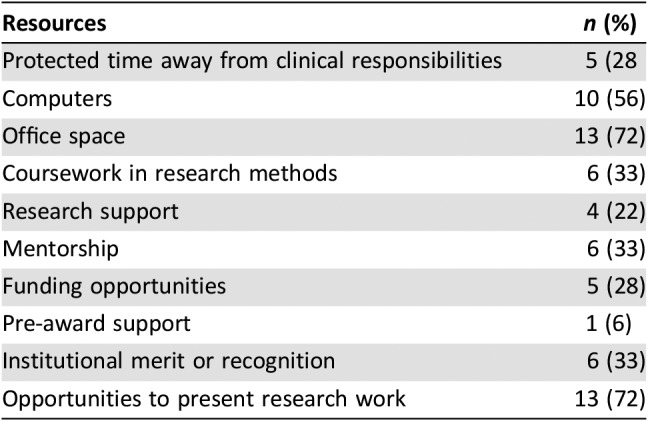
The reported availability of resources to support research development is summarized in Table 2. Of the 18 participants who provided responses regarding available resources to support research development, more than half reported adequate availability of computers (56%), office space (72%), and opportunities to present research (72%). In contrast, only 28% reported adequate protected time away from clinic work, and 28% reported adequate access to funding opportunities for research. Only one respondent (6%) identified availability of access to institutional support for preparation of a grant application (“pre‐award support”). In response to an open‐ended question asking respondents to identify the “greatest needs” for developing a research career, themes of “research training” and “mentorship” were consistently identified by 67% and 61% of respondents, respectively.
Table 2. Reported resources currently available to support research development among oncologists in Tanzania (n = 18).
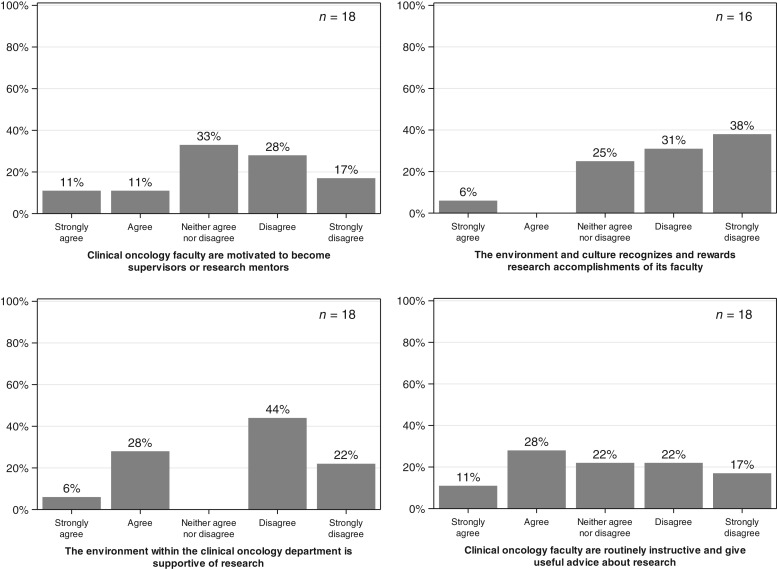
A total of 18 participants responded to questions regarding their impressions about the institutional research environment, which are summarized in Figure 2.
Figure 2.
Self‐reported impressions of institutional supports for research among current and recent oncology trainees in Tanzania.
Discussion
The findings of our survey of all current trainees and recent graduates of one of the first clinical oncology training programs in East Africa reflect a very strong motivation to actively engage in cancer research. Despite consistent identification of barriers and challenges to conducting research throughout the survey, 77% of respondents identified that they aspired to a career path that allowed for research or a mix of clinical care and academic research, confirming our impression of high levels of enthusiasm toward the development of cancer research training opportunities.
This finding is in stark contrast, however, with the current availability of infrastructure and institutional supports to effectively support fulfillment of these aspirations. Specifically, protected time for research away from clinical responsibilities, coursework in research methods, research support, and mentorship were identified by a majority of respondents as currently unavailable. These significant barriers echo those published by the American Society of Clinical Oncology International Affairs Committee, which previously reported that lack of financial support was the primary barrier to conducting clinical cancer research in both high‐income countries and low‐ and middle‐income countries (LMICs) [9].
The reported scarcity of available mentorship is particularly notable but not surprising in what is a relatively novel field of study in East Africa [10]. Structured and longitudinal mentorship from a competent and dedicated mentor is critical both during the primary educational experience and, especially, during the period that follows [11], [12], [13]. Thus, development of investigators with effective mentorship skills is a necessary first step toward the development of broader initiatives to create and enhance conditions that foster the upward mobility of East African scholars in cancer research. In addition to the requisite acquisition of research skills through dedicated training, formal training in mentorship techniques has been repeatedly shown to enhance mentor and mentee outcomes in academic settings [11], [12], [13], [14], [15], [16], [17], [18], [19], [20]. Attention will need to be paid in effort to identify context‐specific challenges in mentoring affecting trainees from LMICs, which could possibly include difficulties finding suitable mentoring; hierarchical structures that discourage mentee‐driven processes; feeling invisible; facing prejudice; feeling devalued; cultural inconsistencies; a lack of altruism in mentoring due to extreme academic pressure on local faculty; and/or a lack of knowledge associated with existing, but hidden, rules and customs common to academic settings.
The MMed in Clinical Oncology program at MUHAS currently requires trainees to complete and defend a dissertation as a compulsory component of the training program. Didactic coursework provides exposures to epidemiology, biostatistics, and medical ethics; however, the content of the existing curriculum rarely leads to independent research by the graduates of the training program. This is evidenced by limited publications of dissertation research or other research by recent graduates, and it is consistent with a previously published report that even those African scientists who achieve master's or doctorate‐level training remain noncompetitive for external funding sources, with fewer than 2% receiving two or more grants within 15 years after training. Low research productivity from the region is exemplified in the stagnant number of research publications and low citation counts from East Africa between 1999 and 2008 [21]. Notably, the absence of a prevailing academic culture that assigns merit to research accomplishment was identified by a majority of respondents in our study and merits further assessment. Moreover, we acknowledge that research may be deprioritized as trainees transition into the workforce in a specialty that is still heavily impacted by scarcity of trained health care professionals.
There are several limitations to this study that should be acknowledged. First, this analysis is based upon a small sample; however, this sample reflects the majority of current trainees and recent graduates of one of the first clinical oncology training programs in East Africa. Of note, the study population may not be representative of the preceding generation of oncologists in Tanzania or East Africa more broadly who were trained previously in clinical oncology training programs outside of Tanzania.
In addition, not all participants completed all components of the survey. For reasons that are unknown, only 18 of 30 respondents completed the entire survey, contributing to a high degree of missingness. Although the survey was administered in English rather than in Tanzania's official national language of Swahili, this is the language of the medical school curriculum; thus, language barriers were unlikely to account for the high incompletion rate. Significant attrition was noted in the questions related to the institutional environment; we speculate that concerns regarding confidentiality of the responses may have contributed to significantly lower response rates in this section of the questionnaire. Also, the survey tool was not previously validated; although it was primarily designed by local researchers, differences in how the participants interpreted and responded to survey questions may have impacted completeness of the responses. Finally, the study was primarily intended to be descriptive in nature, and findings of statistical significance may have been impacted by numerous potential confounding factors and therefore should be interpreted with caution.
Conclusion
We identified a striking contrast between the aspirations for incorporation of research into career development and the research training that is currently available to oncologists and oncology trainees at a regional training hub in East Africa. Despite consistent identification of barriers and challenges to conducting research, an impressive 77% of respondents identified that they aspire to a career path that allows for academic research, confirming our impression of high levels of enthusiasm toward the development of cancer research training opportunities in Tanzania. The results of this study underscore a resounding message regarding the readiness for cancer research training and mentorship in this setting, driven by a sense of urgency related to the burden from cancer that East Africa faces.
There is currently a critical need to establish a cadre of investigators in East Africa who are capable of conceptualizing, gaining funding for, implementing, analyzing, and publishing original research focused on cancer. We hypothesize that African principal investigators can operate effectively if proper attention is given to selection and provision of high‐quality foundational didactic training to learn the theory and implementation of research as well as to the development of an environment conducive to mentoring. While we continue our partnership to develop a research curriculum and mentoring programs, we also plan to perform a needs assessment to inform steps necessary to create an institutional environment that catalyzes interprofessional development and transforms and extends cancer research in East Africa.
Acknowledgments
Support was provided by the Fogarty International Center of the U.S. National Institutes of Health (1D71TW011202‐01). Content does not reflect the views of the Fogarty International Center or the U.S. National Institutes of Health.
Author Contributions
Conception/design: Fidel Rubagumya, Elia J. Mmbaga, Katherine Van Loon
Provision of study material or patients: Fidel Rubagumya, Emmanuel Balandya, Leyna H. Germana, Elia J. Mmbaga, Nazima Dharsee
Collection and/or assembly of data: Fidel Rubagumya, Hilary Chan, Alan Paciorek, Li Zhang, Katherine Van Loon
Data analysis and interpretation: Fidel Rubagumya, Alan Paciorek, Li Zhang, Katherine Van Loon
Manuscript writing: Fidel Rubagumya, Sarah K. Nyagabona, Khadija H. Msami, Achille Manirakiza, Ahuka N. Longombe, Theoneste Maniragaba, Alan Paciorek, Li Zhang, Emmanuel Balandya, Leyna H. Germana, Elia J. Mmbaga, Nazima Dharsee, Katherine Van Loon
Final approval of manuscript: Fidel Rubagumya, Sarah K. Nyagabona, Khadija H. Msami, Achille Manirakiza, Ahuka N. Longombe, Theoneste Maniragaba, Hilary Chan, Alan Paciorek, Li Zhang, Emmanuel Balandya, Leyna H. Germana, Elia J. Mmbaga, Nazima Dharsee, Katherine Van Loon
Disclosures
The authors indicated no financial relationships.
References
- 1.Sylla BS, Wild CP. A million Africans a year dying from cancer by 2030: What can cancer research and control offer to the continent? Int J Cancer 2012;130:245–250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.WHO Africa . Uniting against NCDs: The time to act is now. The Brazzaville Declaration on Noncommunicable Diseases Prevention and Control in the WHO African region. Updated 2011. Available at https://www.who.int/nmh/events/2011/ncds_brazzaville_declaration.pdf?ua=1. Accessed March 14, 2019.
- 3.Ramsay S. African health researchers unite. Lancet 2002;360:1665–1666. [DOI] [PubMed] [Google Scholar]
- 4.Clancy AA, Posner G. Attitudes toward research during residency: A survey of Canadian residents in obstetrics and gynecology. J Surg Educ 2015;72:836–843. [DOI] [PubMed] [Google Scholar]
- 5.Lingwood J, Boyle P, Milburn A et al. The challenge of cancer control in Africa. Nat Rev Cancer 2008;8:398–403. [DOI] [PubMed] [Google Scholar]
- 6.Tanzania National Bureau of Statistics. Available at http://www.nbs.go.tz/. Accessed October 1, 2018.
- 7.Khazaei S, Soheylizad M, Veisani Y et al. Global inequality in the incidence and mortality rates of esophageal cancer: A country‐level analysis. Cancer 2018;3:12. [Google Scholar]
- 8.StataCorp. 2017. Stata Statistical Software: Release 15. College Station, TX: StataCorp LLC.
- 9.Seruga B, Sadikov A, Cazap EL et al. Barriers and challenges to global clinical cancer research. The Oncologist 2014;19:61–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Anyangwe SC, Mtonga C. Inequities in the global health workforce: The greatest impediment to health in sub‐Saharan Africa. Int J Environ Res Public Health 2007;4:93–100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Straus SE, Johnson MO, Marquez C et al. Characteristics of successful and failed mentoring relationships: A qualitative study across two academic health centers. Acad Med 2013;88:82–89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cohen JG, Sherman AE, Kiet TK et al. Characteristics of success in mentoring and research productivity ‐ A case‐control study of academic centers. Gynecol Oncol 2012;125:8–13. [DOI] [PubMed] [Google Scholar]
- 13.Stamm M, Buddeberg‐Fischer B. The impact of mentoring during postgraduate training on doctors' career success. Med Educ 2011;45:488–496. [DOI] [PubMed] [Google Scholar]
- 14.Hoover EL. Mentoring women in academic surgery: Overcoming institutional barriers to success. J Natl Med Assoc 2006;98:1542–1545. [PMC free article] [PubMed] [Google Scholar]
- 15.Bussey‐Jones J, Bernstein L, Higgins S et al. Repaving the road to academic success: The IMeRGE approach to peer mentoring. Acad Med 2006;81:674–679. [DOI] [PubMed] [Google Scholar]
- 16.Feldman MD, Steinauer JE, Khalili M et al. A mentor development program for clinical translational science faculty leads to sustained, improved confidence in mentoring skills. Clin Transl Sci Aug 2012;5:362–367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Pfund C, Maidl Pribbenow C, Branchaw J et al. Professional skills. The merits of training mentors. Science 2006;311:473–474. [DOI] [PubMed] [Google Scholar]
- 18.Gandhi M, Fernandez A, Stoff DM et al. Development and implementation of a workshop to enhance the effectiveness of mentors working with diverse mentees in HIV research. AIDS Res Hum Retroviruses 2014;30:730–737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Gandhi M, Johnson M. Creating more effective mentors: Mentoring the mentor. AIDS Behav 2016;20(suppl 2):294–303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Johnson MO, Gandhi M. A mentor training program improves mentoring competency for researchers working with early‐career investigators from underrepresented backgrounds. Adv Health Sci Educ Theory Pract 2015;20:683–689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bloomfield GS, Baldridge A, Agarwal A et al. Disparities in cardiovascular research output and citations from 52 African countries: A time‐trend, bibliometric analysis (1999‐2008). J Am Heart Assoc 2015;4. [DOI] [PMC free article] [PubMed] [Google Scholar]