Abstract
Objective
To assess family medicine residents’ knowledge of, attitudes toward, and clinical practices related to environmental health (EH).
Design
Two-part study with questionnaire construction using a modified Delphi method, and a Web-based questionnaire administered to family medicine residents between November 2015 and January 2016.
Setting
All Canadian family medicine programs (for questionnaire construction) and 4 Ontario family medicine training programs (for questionnaire administration).
Participants
First- to third-year family medicine residents (for questionnaire administration).
Main outcome measures
Responses to 93 survey items that measured family medicine residents’ knowledge of, attitudes toward, and clinical practices related to EH.
Results
For the final administered questionnaire, 203 of 887 (22.9%) family medicine residents responded. Although 92.0% of respondents somewhat or strongly believed that taking an environmental exposure history was important, only 18.1% of them had specific training in taking environmental exposure history, and 48.4% believed that taking an exposure history takes up too much time in office practice. While 82.9% of residents correctly identified recreational water use as a cause of gastroenteritis, only 60.2% correctly identified radon as a cause of lung cancer and 37.6% knew that elevated ground-level ozone is associated with asthma. Only 10.8% believed their supervisors had a good understanding of environmental exposures. Residents who believed their supervisors understood environmental exposures were more likely to take exposure histories for patients with uncontrolled asthma (P < .05), and those who discussed EH exposure with supervisors frequently, or thought environmental exposure histories were very important, were more likely to provide patients with EH education materials (P < .01).
Conclusion
Although family medicine residents are aware of the importance of assessing patients’ environmental exposures, they lack training and mentorship in EH. As a health determinant of critical importance, EH should be a high priority for inclusion in postgraduate family medicine education.
Résumé
Objectif
Évaluer les connaissances, les attitudes et les pratiques cliniques des résidents en médecine familiale en matière de santé environnementale (SE).
Type d’étude
Étude en 2 étapes, notamment la formulation du questionnaire au moyen d’une méthode Delphi modifiée, et un questionnaire sur le Web, administré entre novembre 2015 et janvier 2016.
Contexte
Tous les programmes canadiens en médecine familiale (pour la conception du questionnaire) et 4 programmes de formation en médecine familiale en Ontario (pour l’administration du questionnaire).
Participants
Des résidents de première, deuxième et troisième années en médecine familiale (pour l’administration du questionnaire).
Principaux paramètres à l’étude
Les réponses aux 93 éléments du sondage qui mesuraient les connaissances, les attitudes et les pratiques cliniques des résidents en médecine familiale en matière de SE.
Résultats
Lors de l’administration du questionnaire final, 203 des 887 (22,9 %) résidents en médecine familiale ont répondu. Même si 92,0 % des répondants estimaient qu’un bilan des expositions environnementales était assez ou très important, seulement 18,1 % d’entre eux reçu une formation précise en anamnèse des expositions environnementales, et 48,4 % croyaient qu’un bilan des expositions prenait trop de temps en clinique. Si 82,9 % des résidents ont correctement identifié que l’eau à des fins récréatives était une cause de gastroentérite, seulement 60,2 % savaient à juste titre que le radon pouvait causer le cancer du poumon, et 37,6 % connaissaient l’association entre des concentrations élevées d’ozone au niveau du sol et l’asthme. Seulement 10,8 % étaient d’avis que leurs superviseurs connaissaient bien les expositions environnementales. Les résidents qui croyaient que leurs superviseurs comprenaient bien les expositions environnementales étaient plus enclins à procéder à une anamnèse des expositions si leurs patients souffraient d’asthme non contrôlé (p < ,05), et ceux qui discutaient souvent avec leurs superviseurs d’expositions en SE ou qui jugeaient les bilans des expositions environnementales très importants étaient plus enclins à fournir du matériel d’information sur la SE à leurs patients (p < ,01).
Conclusion
Même si les résidents en médecine familiale sont conscients de l’importance d’évaluer les expositions environnementales des patients, ils manquent de formation et de mentorat en SE. Étant donné son importance critique en tant que déterminant de la santé, il faudrait accorder une grande priorité à l’inclusion de la SE dans la formation médicale postdoctorale en médecine familiale.
In Canada, deaths from modifiable environmental risks account for 9% to 14% of all mortality.1 Articles highlighting the need for improvement of physician education in environmental health (EH) have been present in literature since 1972.2 Calls for this improvement have been made twice by the Institute of Medicine3,4 and have echoed through the training of pediatricians,5–7 obstetricians and gynecologists,8,9 and family physicians.10–12 However, articles as recent as 2013 in the United States13 and 2009 in Canada14 have shown that training in EH is still largely absent.
Family physicians are front-line providers in addressing sources of environmental exposure and environmental-related illnesses, and training is required to effectively assess and manage these concerns. Several studies have assessed the EH concerns and learning needs of practising physicians. A survey of rural, small-urban, and large-urban community family physicians in Ontario found that all groups had high concern about the respiratory, carcinogenic, and teratogenic effects of environmental exposures.11 In this study, more than half of the physicians recalled receiving questions from patients pertaining to sunlight, food additives, radiation, and lead.11 A survey conducted with health care providers and parents attending public health clinics in Edmonton, Alta,15 found high concern about children’s environmental exposures among both groups. In Italy, a cross-sectional mail survey of primary care physicians found that 84% thought that evaluating sources of exposure by taking an environmental history was very important.16
Studies directly investigating clinical competence in EH have mainly focused on occupational asthma. These studies consistently found problems of delayed diagnosis, underdiagnosis, and undermanagement,17–19 with 41% of patients believing that lack of inquiry by their primary care physician about the work-relatedness of symptoms was the main factor in diagnosis delay, which averaged 4.9 years.18 An audit of primary care practices found that only 14% of patients with adult-onset asthma had their occupation recorded.19 A mail survey of family physicians in Texas reported that 86% of family physicians had no specific training in EH, while almost 92% wanted to learn more about EH hazards. Patients initiated questions about drinking water, herbicides, and indoor and outdoor pollution more frequently than physicians did.12
Assessments of family medicine residents’ learning needs in and knowledge of EH are very limited. A pilot study of family medicine residents at an Ontario university in 2001 found that, compared with practising physicians, their self-reported knowledge was similarly low and EH concerns similarly high, when measured using the same survey tool (Sanborn MD, Scott EA, Cole D, unpublished data, 2001). A national survey of US family medicine training programs in 2008 found that only 68% of them had any occupational or environmental medicine content; however, almost 92% of responding residency directors thought training in occupational medicine was important.20
This study of family medicine residents was undertaken to investigate the combination of high interest in EH with low self-reported knowledge found in studies of practising physicians, and to generate information to identify family medicine EH curriculum gaps, improve EH training in family medicine, and graduate family physicians who are better prepared to diagnose and treat environmental exposure–related illnesses.
METHODS
The study was conducted in 2 parts: questionnaire construction using the modified Delphi method, and questionnaire administration to family practice residents.
Questionnaire construction
Developing a questionnaire for a previously unstudied target group requires a reliable method to ensure the content validity of the survey tool. The Delphi method has been extensively used in health care research, including in curriculum development,21–23 providing independent expert opinions on content areas and questions to be included in surveys, guidelines, and health priorities.24,25 The modified method is implemented by iteratively asking participants, by e-mail, to identify priority questions to include in the survey, questions not to include, and their own ideas regarding important questions.25
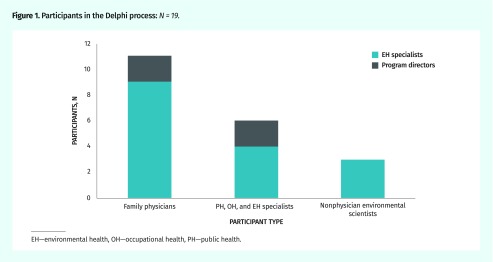
Forty invitees, including EH experts and all Canadian family medicine program directors, were asked to participate in the Delphi process; the composition of respondents is shown in Figure 1. Questions for the initial round were taken from previous surveys or developed through research group discussions. There were 19 participants in the first Delphi round, and 15 of them also participated in the second round. Questions were included in the final survey if they were approved (a rating of 4 or 5 on a 5-point Likert scale) by more than 74% of the Delphi respondents. The full survey is available at https://fammedmcmaster.ca/research/survey-of-environmental-health-concerns.
Figure 1.
Participants in the Delphi process: N = 19.
EH—environmental health, OH—occupational health, PH—public health.
Survey of family medicine residents
After ethics approval of the final questionnaire by all institutions included in the survey, all first- to third-year family medicine residents in 4 Ontario training programs were invited to participate in the online survey between November 2015 and January 2016. Each resident received 3 reminders over a 6-week period.
Response proportion varied according to the contact method (for invitation to participate and reminders) approved by each department of family medicine. In the 3 programs that contacted residents individually, response rates were 27.7% to 37.4%, and in 1 program that included the survey invitation as an item in the departmental e-newsletter, 11.5% of residents responded. The overall response proportion was 22.9% (203 of 887 residents).
Analyses
We expressed continuous data as means and standard deviations, or as medians and interquartile ranges when data were skewed. For categorical data, we presented the proportion endorsing each category as well as those not responding. Demographic characteristics were used to compare residents with a substantial amount of missing data (≥ 25%) to those with sufficiently complete responses. Associations were assessed among a subset of the questions determined a priori by the research team. Specifically, the association between ordinal variables assessing the frequency of discussing exposure history domains and asking about specific sources of environmental exposure with confidence or answering patient questions about those exposures was assessed using the Spearman ρ. Generalized logistic models with a probit link function were used to identify factors associated with a correct answer to each of the knowledge questions. Independent variables included previous EH education or experience, satisfaction with training, perceived level of supervisor understanding, and frequency of discussions with supervisor. Multicollinearity of independent variables was assessed using bivariate Spearman correlation coefficients, and model fit was assessed using the Akaike information criterion.
RESULTS
Initial analyses were conducted to test for clustering effects at the program and year levels to determine whether there were differences among the 4 programs surveyed, as well as between first-year residents and second- and third-year residents. There were no statistically significant differences in EH attitudes, knowledge, or clinical practices found among the 4 programs. There were also no differences in EH knowledge or the frequency of performing relevant clinical practices between first-year residents and second- and third-year residents. Therefore, all subsequent analyses were conducted using the pooled responses from all 4 programs and all years.
Population
Table 1 presents respondent characteristics. Of 203 participants, 45 (22.2%) either did not finish the survey or did not answer a substantial portion of the questions (ie, ≥ 25% of questions). Of 13 characteristics, only 1—intention to practice in an urban area—was associated with more missing data (P = .03).
Table 1.
Family medicine respondent characteristics: N = 181.*
| CHARACTERISTICS | RESPONDENTS, % |
|---|---|
| Female sex | 76.2 |
| Age ≥ 30 y | 29.3 |
| Year of training | |
| • First-year resident | 50.8 |
| • Second- or third-year resident | 49.2 |
| Had pre-residency environmental health training | 17.1 |
| Have children aged < 18 y | 13.8 |
| Location of MD training | |
| • Ontario | 70.7 |
| • Other province | 13.8 |
| • IMG | 15.5 |
IMG—international medical graduate, MD—medical doctor.
Not all 203 respondents finished the survey.
Exposure history taking
As environmental exposure history taking is considered a key EH skill,26 several questions examined this skill. Although 92.0% of respondents somewhat or strongly agreed that taking an exposure history is important, only 18.1% had specific training in taking one. Two clinical scenarios were presented, asking how often the resident would take an exposure history in the setting of A) a patient with poorly controlled asthma or frequent asthma exacerbations and B) a patient with recurrent miscarriage. While 75.3% would take an exposure history for the asthma patient half the time or more often, only 20.2% of residents would take an exposure history for the miscarriage patient half the time or more often. The statement “taking an exposure history takes up too much time in office practice” was endorsed by 48.4% of respondents.
A further line of questioning asked how often the CH2OPD2 (Community, Home and Hobbies, Occupation, Personal habits, Diet and Drugs)27 exposure domains were assessed during exposure history taking. As shown in Table 2, the exposure domains of community, home and hobbies, occupation (for adults), and school (for children) were asked about less than half the time.
Table 2.
Frequency of assessing environmental health exposure during history taking, by exposure domain
| EXPOSURE DOMAIN (CH2OPD2)* | TOTAL ANSWERS, N (%) | MISSING ANSWERS, N (%) | ANSWERS, N (%) | ||||
|---|---|---|---|---|---|---|---|
|
| |||||||
| NEVER | OCCASIONALLY | HALF THE TIME | USUALLY | ALWAYS | |||
| Community or neighbourhood (C) | 159 (78.3) | 44 (21.7) | 80 (50.3) | 58 (36.5) | 11 (6.9) | 10 (6.3) | 0 (0.0) |
| Housing or home (H) | 162 (79.8) | 41 (20.2) | 21 (13.0) | 69 (42.6) | 32 (19.8) | 38 (23.5) | 2 (1.2) |
| Hobbies (H) | 160 (78.8) | 43 (21.2) | 46 (28.8) | 72 (45.0) | 21 (13.1) | 19 (11.9) | 2 (1.3) |
| Occupation (for adults) (O) | 163 (80.3) | 40 (19.7) | 16 (9.8) | 72 (44.2) | 31 (19.0) | 38 (23.3) | 6 (3.7) |
| School (for children) (O) | 162 (79.8) | 41 (20.2) | 67 (41.4) | 58 (35.8) | 13 (8.0) | 18 (11.1) | 6 (3.7) |
| Diet or food (D) | 164 (80.8) | 39 (19.2) | 14 (8.5) | 48 (29.3) | 38 (23.2) | 42 (25.6) | 22 (13.4) |
| Drugs (including alternative medications and supplements) (D) | 163 (80.3) | 40 (19.7) | 18 (11.0) | 46 (28.2) | 26 (16.0) | 43 (26.4) | 30 (18.4) |
| Personal habits (P) | 164 (80.8) | 39 (19.2) | 1 (0.6) | 7 (4.3) | 7 (4.3) | 59 (36.0) | 90 (54.9) |
CH2OPD2 (Community, Home and Hobbies, Occupation, Personal habits, Diet and Drugs) is an exposure-history mnemonic tool.
Table 3 shows results for the 8 most clinically relevant exposures. For example, 89.6% of respondents had never discussed radon exposure with their patients. Table 4 presents respondents’ confidence levels in answering patient questions about sources of exposure. For example, 63.5% felt not at all confident answering patient questions about radon. Frequency of asking about specific environmental exposures was moderately correlated with confidence in answering patients’ questions about these exposures (Spearman ρ range of 0.34 to 0.54, all P < .001, data not shown).
Table 3.
Frequency of asking patients about several clinically relevant sources of exposure
| EXPOSURE SOURCE | TOTAL ANSWERS, N (%) | MISSING ANSWERS, N (%) | ANSWERS, N (%) | ||||
|---|---|---|---|---|---|---|---|
|
| |||||||
| NEVER | OCCASIONALLY | HALF THE TIME | USUALLY | ALWAYS | |||
| Sun | 162 (79.8) | 41 (20.2) | 0 (0.0) | 26 (16.0) | 35 (21.6) | 74 (45.7) | 27 (16.7) |
| Outdoor air pollution | 163 (80.3) | 40 (19.7) | 71 (43.6) | 72 (44.2) | 12 (7.4) | 6 (3.7) | 2 (1.2) |
| Radon | 163 (80.3) | 40 (19.7) | 146 (89.6) | 12 (7.4) | 2 (1.2) | 2 (1.2) | 1 (0.6) |
| Pesticides | 162 (79.8) | 41 (20.2) | 105 (64.8) | 47 (29.0) | 4 (2.5) | 5 (3.1) | 1 (0.6) |
| Heavy metals | 162 (79.8) | 41 (20.2) | 77 (47.5) | 69 (42.6) | 10 (6.2) | 5 (3.1) | 1 (0.6) |
| Carbon monoxide indoors | 163 (80.3) | 40 (19.7) | 29 (17.8) | 63 (38.7) | 35 (21.5) | 32 (19.6) | 4 (2.5) |
| Recreational water | 161 (79.3) | 42 (20.7) | 71 (44.1) | 65 (40.4) | 16 (9.9) | 8 (5.0) | 1 (0.6) |
| Mold | 159 (78.3) | 44 (21.7) | 61 (38.4) | 73 (45.9) | 13 (8.2) | 11 (6.9) | 1 (0.6) |
Table 4.
Respondents’ confidence levels in answering patients’ questions about sources of exposure
| EXPOSURE SOURCE | TOTAL ANSWERS, N (%) | MISSING ANSWERS, N (%) | ANSWERS, N (%) | ||||
|---|---|---|---|---|---|---|---|
|
| |||||||
| NOT AT ALL | SOMEWHAT | MODERATELY | QUITE | VERY | |||
| Sun | 155 (76.4) | 48 (23.6) | 0 (0.0) | 6 (3.9) | 26 (16.8) | 62 (40.0) | 61 (39.4) |
| Outdoor air pollution | 156 (76.8) | 47 (23.2) | 40 (25.6) | 50 (32.1) | 41 (26.3) | 20 (12.8) | 5 (3.2) |
| Radon | 156 (76.8) | 47 (23.2) | 99 (63.5) | 34 (21.8) | 14 (9.0) | 8 (5.1) | 1 (0.6) |
| Pesticides | 156 (76.8) | 47 (23.2) | 70 (44.9) | 55 (35.3) | 22 (14.1) | 8 (5.1) | 1 (0.6) |
| Heavy metals | 156 (76.8) | 47 (23.2) | 51 (32.7) | 64 (41.0) | 31 (19.9) | 10 (6.4) | 0 (0.0) |
| Carbon monoxide indoors | 155 (76.4) | 48 (23.6) | 23 (14.8) | 42 (27.1) | 37 (23.9) | 39 (25.2) | 14 (9.0) |
| Recreational water | 155 (76.4) | 48 (23.6) | 45 (29.0) | 49 (31.6) | 38 (24.5) | 20 (12.9) | 3 (1.9) |
| Mold | 153 (75.4) | 50 (24.6) | 35 (22.9) | 66 (43.1) | 36 (23.5) | 15 (9.8) | 1 (0.7) |
Knowledge of EH
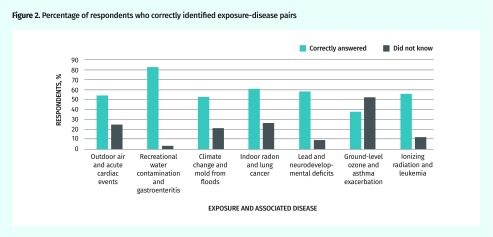
Knowledge was assessed by asking respondents to match sources of exposure with diseases. These were grouped in sets of 4, providing a 25% possibility of a correct answer by chance. Figure 2 shows the wide range of correct answers for 7 exposure-disease pairs. While 82.9% of residents correctly identified recreational water use as a cause of gastroenteritis, only 60.2% correctly identified radon as a cause of lung cancer and 37.6% knew that elevated ground-level ozone is associated with asthma. Correctly answering 2 air-quality questions (ie, matching air pollution with cardiac events and ground-level ozone with asthma) was highly correlated (P < .001).
Figure 2.
Percentage of respondents who correctly identified exposure-disease pairs
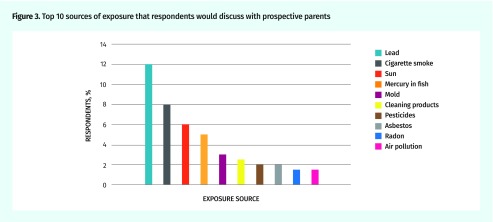
An open-ended knowledge question asked respondents to list a few exposures that are important to discuss with prospective parents. There was a 75.9% response rate, with residents who intended to provide future prenatal or well-baby care being more likely to respond (P < .025). The top 10 responses are presented in Figure 3.
Figure 3.
Top 10 sources of exposure that respondents would discuss with prospective parents
Regression analyses of various factors
Factors associated with knowledge of exposure-disease pairs.
For the knowledge questions about the radon exposure association with lung cancer and the ground-level ozone exposure associated with asthma, none of the following factors was statistically significantly associated with a correct answer: previous environmental exposure education, satisfaction with environmental exposure training, perceived supervisors’ knowledge of environmental exposure, or frequency of discussions with supervisors regarding environmental exposure.
Factors associated with clinical practices.
Residents who perceived their supervisors’ understanding of environmental exposures as moderate to very good were more likely to take exposure histories for patients with uncontrolled asthma (P < .05, odds ratio [95% CI] of 1.85 [1.02 to 3.34]). For spontaneous abortion, the perception that supervisors’ EH knowledge was poor was associated with not taking an exposure history (P < .01, odds ratio [95% CI] of 1.85 [1.16 to 2.97]). Only 10.8% of residents surveyed thought their supervisors understood environmental exposures quite well or very well.
Factors associated with educational material.
Most respondents (52.3%) never provided patient education materials about environmental exposures to patients. Providing patients with such materials was positively associated with the belief that taking an exposure history is very important (P < .01) and with discussing exposure-disease links with a supervisor at least once a month (P < .01).
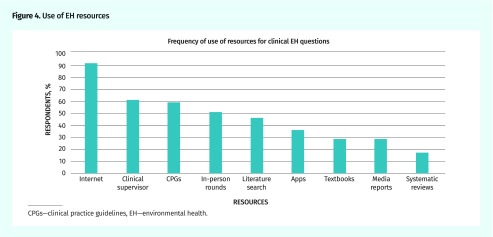
Sources of EH information
The most commonly reported resource used to answer a clinical EH question was the Internet, followed by the clinical supervisor and clinical practice guidelines (Figure 4). The most commonly used Web resource was the subscription site UpToDate, mentioned by 48 respondents. Fourteen government or academic websites and 8 commercial websites were each named between 1 and 5 times.
Figure 4.
Use of EH resources
CPGs—clinical practice guidelines, EH—environmental health.
DISCUSSION
This study confirms previous findings that, although EH is considered important by concerned family physicians in training, there is a gap between its perceived value and the knowledge, effective teaching, and clinical practices necessary for diagnosing exposure-related conditions.
Taking an exposure history is a key clinical skill that should be addressed in resident and faculty education, and respondents reported a lack of training and negative attitudes toward this skill, which is considered the fundamental clinical practice for diagnosing exposure-related illness.3 Half of residents thought taking an exposure history took too much time in office practice, similar to the 52% of Italian family physicians who thought taking an EH history “takes too much time.” Although Health Canada recommends asking all patients to test their homes for radon, 89.6% of residents had never discussed radon with a patient. So that taking an exposure history “requires only a few minutes of the clinician’s time,”3 the process has been refined using the clinical mnemonic CH2OPD2,27 which can be applied clinically in diagnosing many different exposures.4
The results indicate a need for educational measures to enhance EH knowledge and practice skills among family medicine residents and their preceptors. Given that no difference was observed between first-year residents and second- and third-year residents in these measures, it is important to determine where and when current knowledge, attitudes, and clinical skills are being learned. Notably, although residents rated their supervisors’ knowledge of EH as low, they continued to use supervisors as their second most frequent source of information when confronted with a clinical problem.
Strengths and limitations
The survey tool development was a strength of this study, with good agreement on the important questions achieved through a Delphi process. The study was also strengthened by sampling residents from 4 programs and finding no differences among the programs in the survey measures. However, the response rate, although typical of provider surveys, was low. This study did not survey clinical supervisors, and this group might provide additional information to improve EH in family medicine education.
Conclusion and future directions
Given public and patient concern, proposed strategies to incorporate EH education in physician training need to be implemented. Basic competencies recommended for both medical students3 and primary care physicians4 could be modified for family medicine residents. The importance of stressing the central role of the exposure history as a core skill is reiterated in many articles.14,26,27 Environmental health can be integrated into current training rather than being taught in a specially created curriculum.26 Cited barriers to incorporating EH into medical training include lack of time,6 expert faculty,6,28 and sufficient space in the curriculum.6,28 Faculty champions and institutional leadership are essential for overcoming these barriers, as exemplified in the literature.14,29,30 As a health determinant of critical importance,1 EH should be a high priority for inclusion in postgraduate family medicine education.
Acknowledgments
This research was funded by a Janus Research Grant to Dr Sanborn, with in-kind assistance early in the project from the Ontario College of Family Physicians through use of its teleconference line. Dr Griffith is supported by a Canadian Institutes of Health Research New Investigator Award and the McLaughlin Foundation Professorship in Population and Public Health. We thank the Delphi respondents for their large contribution to the survey design, Karla Lancaster for statistical analysis, and Dr Mehvish Mehrani for initial analysis work. We also thank the Department of Family Medicine at McMaster University for contributing administrative support to this research and the McMaster Faculty of Health Sciences Program for Education Research, Innovation, and Theory (MERIT) for supporting the administration of the survey tool.
Editor’s key points
▸ Family physicians are front-line providers in addressing sources of environmental exposure and environmental-related illnesses, and training is required to effectively assess and manage these concerns. The goal of this study was to determine family medicine residents’ learning needs in and knowledge of environmental health (EH).
▸ This study found that although EH is considered important by family physicians in training, there is a gap between its perceived value and the knowledge, effective teaching, and clinical practices necessary for diagnosing exposure-related conditions. Taking an exposure history is a key clinical skill that should be addressed in resident and faculty education, and respondents reported a lack of training and negative attitudes toward this skill.
▸ The results indicate a need for educational measures to enhance EH knowledge and practice skills among family medicine residents and their preceptors. Given that no difference was observed between first-year residents and second- and third-year residents in these measures, it is important to determine where and when current knowledge, attitudes, and clinical skills are being learned. Notably, although residents rated their supervisors’ knowledge of EH as low, they continued to use supervisors as their second most frequent source of information when confronted with a clinical problem.
Points de repère du rédacteur
▸ Les médecins de famille sont en première ligne quand il sagit de cerner les sources dexposition environnementale et les maladies qui leur sont liées, et ils doivent recevoir la formation nécessaire pour évaluer et prendre en charge efficacement ces préoccupations. Cette étude avait pour but de déterminer les besoins des résidents en médecine familiale en matière dapprentissage et de connaissances en santé environnementale (SE).
▸ On a constaté dans cette étude que, même si les médecins de famille en formation considèrent la SE importante, il existe des lacunes entre la valeur quils lui accordent, et les connaissances, l’enseignement efficace et les pratiques cliniques nécessaires pour diagnostiquer les problèmes associés aux expositions. Faire l’anamnèse des expositions est une compétence clinique essentielle qu’il faudrait perfectionner dans l’éducation des résidents et du corps professoral, et les répondants ont signalé un manque de formation et des attitudes négatives face à cette compétence.
▸ Les résultats pointent vers la nécessité de prendre les mesures pédagogiques voulues pour améliorer les connaissances et les compétences professionnelles en SE chez les résidents en médecine familiale et leurs précepteurs. Étant donné l’absence de différences observées dans ces résultats entre les résidents, qu’ils soient en première, deuxième ou troisième année, il importe de déterminer où et quand les connaissances récentes, les attitudes et les compétences cliniques sont apprises. Fait à remarquer, même si les résidents ont accordé une faible cote aux connaissances de leurs superviseurs en SE, ils continuaient à les consulter comme leur deuxième source la plus fréquente d’information lorsqu’ils étaient confrontés à un problème clinique.
Footnotes
Contributors
Drs Sanborn, Grierson, Upshur, Marshall, Vakil, Griffith, Scott, and Cole were involved in research design, contributed to development of the survey tool, and participated in discussion of results and analyses. Drs Vakil, Marshall, Upshur, Sanborn, and Scott were site coordinators responsible for obtaining ethics reviews, departmental permissions, and resident champions at their respective universities. Dr Grierson facilitated data collection and data security for the Delphi surveys and the resident survey through the Program for Education Research and Development at McMaster University. Dr Griffith provided expert consultation and mentoring for research assistants during the statistical analyses. Dr Benusic was a resident champion for one site and provided a literature review. All authors contributed to writing and editing the paper and have approved its final version.
Competing interests
None declared
This article has been peer reviewed.
Cet article a fait l’objet d’une révision par des pairs.
References
- 1.Prüss-Ustün A, Wolf J, Corvalán C, Bos R, Neira M. Preventing disease through healthy environments: a global assessment of the burden of disease from environmental risks. Geneva, Switz: World Health Organization; 2016. [Google Scholar]
- 2.Williams N. Medical student education in environmental health. J Occup Med. 1972;14(10):779–81. [PubMed] [Google Scholar]
- 3.Institute of Medicine Committee on Curriculum Development in Environmental Medicine; Pope A, Rall DP, editors. Environmental medicine: integrating a missing element into medical education. Washington, DC: National Academy Press; 1995. [PubMed] [Google Scholar]
- 4.Institute of Medicine. Division of Health Promotion and Disease Prevention. Role of the primary care physician in occupational and environmental medicine. Washington, DC: National Academy Press; 1988. [Google Scholar]
- 5.Kilpatrick N, Frumkin H, Trowbridge J, Escoffery C, Geller R, Rubin L, et al. The environmental history in pediatric practice: a study of pediatricians’ attitudes, beliefs, and practices. Environ Health Perspect. 2002;110(8):823–7. doi: 10.1289/ehp.02110823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Roberts JR, Gitterman BA. Pediatric environmental health education: a survey of US pediatric residency programs. Ambul Pediatr. 2003;3(1):57–9. doi: 10.1367/1539-4409(2003)003<0057:peheas>2.0.co;2. [DOI] [PubMed] [Google Scholar]
- 7.Roberts JR, Balk SJ, Forman J, Shannon M. Teaching about pediatric environmental health. Acad Pediatr. 2009;9(2):129–30. doi: 10.1016/j.acap.2008.12.009. [DOI] [PubMed] [Google Scholar]
- 8.Tinney VA, Paulson JA, Bathgate SL, Larsen JW. Medical education for obstetricians and gynecologists should incorporate environmental health. Am J Obstet Gynecol. 2015;212(2):163–6.e1. doi: 10.1016/j.ajog.2014.07.038. Epub 2014 Jul 25. [DOI] [PubMed] [Google Scholar]
- 9.Stotland NE, Sutton P, Trowbridge J, Atchley DS, Conry J, Trasande L, et al. Counseling patients on preventing prenatal environmental exposures—a mixed-methods study of obstetricians. PLoS One. 2014;9(6):e98771. doi: 10.1371/journal.pone.0098771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Schenk M, Popp SM, Neale AV, Demers RY. Environmental medicine content in medical school curricula. Acad Med. 1996;71(5):499–501. doi: 10.1097/00001888-199605000-00022. [DOI] [PubMed] [Google Scholar]
- 11.Sanborn MD, Scott EA. Environmental health concerns in urban and rural family practice. Can Fam Physician. 1998;44:1466–72. [PMC free article] [PubMed] [Google Scholar]
- 12.Hamilton WJ, Ryder DJ, Cooper HP, Jr, Williams DM, Weinberg AD. Environmental health: a survey of Texas primary care physicians. Tex Med. 2005;101(10):62–70. [PubMed] [Google Scholar]
- 13.Gómez A, Balsari S, Nusbaum J, Heerboth A, Lemery J. Perspective: environment, biodiversity, and the education of the physician of the future. Acad Med. 2013;88(2):168–72. doi: 10.1097/ACM.0b013e31827bfbeb. [DOI] [PubMed] [Google Scholar]
- 14.Wiseman CL, Stefanovic IL. Children’s health and environment education and training for health care professionals in Canada: assessing gaps, barriers, and needs. Int J Occup Environ Health. 2009;15(4):410–5. doi: 10.1179/oeh.2009.15.4.410. [DOI] [PubMed] [Google Scholar]
- 15.Buka I, Rogers WT, Osornio-Vargas AR, Hoffman H, Pearce M, Li YY. An urban survey of paediatric environmental health concerns: perceptions of parents, guardians and health care professionals. Paediatr Child Health. 2006;11(4):235–8. [PMC free article] [PubMed] [Google Scholar]
- 16.Nicotera G, Nobile CG, Bianco A, Pavia M. Environmental history-taking in clinical practice: knowledge, attitudes, and practice of primary care physicians in Italy. J Occup Environ Med. 2006;48(3):294–302. doi: 10.1097/01.jom.0000184868.77815.2a. [DOI] [PubMed] [Google Scholar]
- 17.Shofer S, Haus BM, Kuschner WG. Quality of occupational history assessments in working age adults with newly diagnosed asthma. Chest. 2006;130(2):455–62. doi: 10.1378/chest.130.2.455. [DOI] [PubMed] [Google Scholar]
- 18.Poonai N, van Diepen S, Bharatha A, Manduch M, Deklaj T, Tarlo SM. Barriers to diagnosis of occupational asthma in Ontario. Can J Public Health. 2005;96(3):230–3. doi: 10.1007/BF03403697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Walters GI, McGrath EE, Ayres JG. Audit of the recording of occupational asthma in primary care. Occup Med (Lond) 2012;62(7):570–3. doi: 10.1093/occmed/kqs114. Epub 2012 Jul 25. [DOI] [PubMed] [Google Scholar]
- 20.Michas MG, Iacono CU. Overview of occupational medicine training among US family medicine residency programs. Fam Med. 2008;40(2):102–6. [PubMed] [Google Scholar]
- 21.Flynn L, Verma S. Fundamental components of a curriculum for residents in health advocacy. Med Teach. 2008;30(7):e178–83. doi: 10.1080/01421590802139757. [DOI] [PubMed] [Google Scholar]
- 22.Feigenbaum DF, Boscardin CK, Frieden IJ, Mathes EF. What should primary care providers know about pediatric skin conditions? A modified Delphi technique for curriculum development. J Am Acad Dermatol. 2014;71(4):656–62. doi: 10.1016/j.jaad.2014.06.032. Epub 2014 Jul 30. [DOI] [PubMed] [Google Scholar]
- 23.Lloyd S, Tan ZE, Taube MA, Doshi J. Development of an ENT undergraduate curriculum using a Delphi survey. Clin Otolaryngol. 2014;39(5):281–8. doi: 10.1111/coa.12293. [DOI] [PubMed] [Google Scholar]
- 24.Wielenga JM, Tume LN, Latour JM, van den Hoogen A. European neonatal intensive care nursing research priorities: an e-Delphi study. Arch Dis Child Fetal Neonatal Ed. 2015;100(1):F66–71. doi: 10.1136/archdischild-2014-306858. Epub 2014 Sep 26. [DOI] [PubMed] [Google Scholar]
- 25.Wong ST, Browne AJ, Varcoe C, Lavoie J, Fridkin A, Smye V, et al. Development of health equity indicators in primary health care organizations using a modified Delphi. PLoS One. 2014;9(12):e114563. doi: 10.1371/journal.pone.0114563. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Gehle KS, Crawford JL, Hatcher MT. Integrating environmental health into medical education. Am J Prev Med. 2011;41(4 Suppl 3):S296–301. doi: 10.1016/j.amepre.2011.06.007. [DOI] [PubMed] [Google Scholar]
- 27.Marshall L, Weir E, Abelsohn A, Sanborn MD. Identifying and managing adverse environmental health effects: 1. Taking an exposure history. CMAJ. 2002;166(8):1049–55. [PMC free article] [PubMed] [Google Scholar]
- 28.Graber DR, Musham C, Bellack JP, Holmes D. Environmental health in medical school curricula: views of academic deans. J Occup Environ Med. 1995;37(7):807–11. doi: 10.1097/00043764-199507000-00009. [DOI] [PubMed] [Google Scholar]
- 29.McCurdy LE, Roberts J, Rogers B, Love R, Etzel R, Paulson J, et al. Incorporating environmental health into pediatric medical and nursing education. Environ Health Perspect. 2004;112(17):1755–60. doi: 10.1289/ehp.7166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Rogers B, McCurdy LE, Slavin K, Grubb K, Roberts JR. Children’s Environmental Health Faculty Champions Initiative: a successful model for integrating environmental health into pediatric health care. Environ Health Perspect. 2009;117(5):850–5. doi: 10.1289/ehp.0800203. Epub 2008 Dec 5. [DOI] [PMC free article] [PubMed] [Google Scholar]