Abstract
Different neoadjuvant chemotherapies are available for triple-negative breast cancer (TNBC). Here, we performed a network meta-analysis to evaluate the pathological complete response (pCR) benefit and safety of treatment regimens. Pairwise and Bayesian network meta-analyses were performed to compare direct and indirect evidence, respectively. Twenty-three studies involving 12 regimens namely standard chemotherapeutic agents, bevacizumab (B)-, platinum salts (P)-, B plus P (BP)-, poly(ADP-ribose) polymerase inhibitors (Pi)-, P plus Pi (PPi)-, capecitabine (Ca)-, gemcitabine (Ge)-, zoledronic acid (Za)-, everolimus (E)-, P plus E (PE)-, and gefitinib (G)-containing regimens. The results showed that P-, B-, PPi-, and Za-containing regimens achieved higher pCR than standard chemotherapeutic agents. BP-containing regimens had a better pCR than B-containing regimens. In indirect comparisons, Za-, BP-, P-, and B-containing regimens were the top four strategies with the highest probability for pCR. Benefit-risk analysis showed that B-containing regimens had the highest acceptability of being the best treatment for better pCR achievement with fewer SAEs. The addition of P, B, BP, PPi, and Za to standard chemotherapeutic agents enhanced the pCR, but a balance between efficacy and safety should be carefully considered. B-containing regimens might be the best choice for neoadjuvant chemotherapy due to its better efficacy and tolerability.
Keywords: network meta-analysis, triple-negative breast cancer, neoadjuvant chemotherapy, pathological complete response
INTRODUCTION
Triple-negative breast cancer (TNBC) accounts for ~12%–17% of all breast cancers [1]. Because endocrine and anti-HER2 therapies are not suitable for TNBC patients, adjuvant chemotherapy is generally the only line of systemic treatment [1, 2]. Compared to other subtypes of breast cancer (e.g., hormone receptor or HER2 positive), TNBC patients suffer worse clinical outcomes [3]. In patients with early stage TNBC, neoadjuvant chemotherapy has become a standard approach and is more likely to achieve pathological complete response (pCR) than non-TNBC patients [4]. Event-free survival and overall survival is dramatically improved in TNBC patients who achieve a pCR after neoadjuvant chemotherapy, whereas patients with residual invasive disease after treatment have a high risk of recurrence [5].
Although there is a significant association between pCR and survival outcomes, the overall prognosis of TNBC remains unsatisfactory, and only ~30% of TNBC patients achieve pCR following treatment with standard anthracycline-, cyclophosphamide-, taxane-, and/or fluorouracil-based neoadjuvant chemotherapy [6]. Currently, different strategies are applied to increase TNBC pCR rates. For instance, adding platinum salts, which induce double-stranded DNA breaks and subsequent cell death, to standard neoadjuvant chemotherapy has been explored by several randomized control trials (RCTs), and has shown a promising pCR benefit in TNBC patients, especially in those with BRCA mutations [7–9]. However, severe toxicities resulting in hematological, gastrointestinal, and nervous system disorders have frequently been observed in patients treated with platinum-containing regimens [9]. Bevacizumab, a monoclonal antibody targeting vascular endothelial growth factor A, has been demonstrated to improve pCR rates when added to neoadjuvant chemotherapy in TNBC [10]. In I-SPY 2, a multicenter phase 2 trial, the addition of veliparib and carboplatin to standard neoadjuvant chemotherapy significantly increased the pCR proportion in TNBC patients compared with controls [11]. However, the NeoPARP study found no difference in pCR between an iniparib plus paclitaxel regimen vs. paclitaxel alone in TNBC [12].
Despite these results, the optimal regimen for TNBC treatment remains controversial due to the limitations of RCTs and conventional meta-analyses in comparing and integrating the efficacy of all available regimens. Network meta-analysis, also known as multiple-treatments or mixed-treatment analysis, not only allows the integration of the evidence without head-to-head comparison, but also can determine the superiority of different interventions by ranking probability and acceptability [13]. Therefore, we conducted a Bayesian network meta-analysis to estimate the efficacy and safety of the currently available neoadjuvant chemotherapies in TNBC. Here, we provide a systematic summary of different regimens that may aid in treatment decisions and future studies.
RESULTS
Overview of literature search and study characteristics
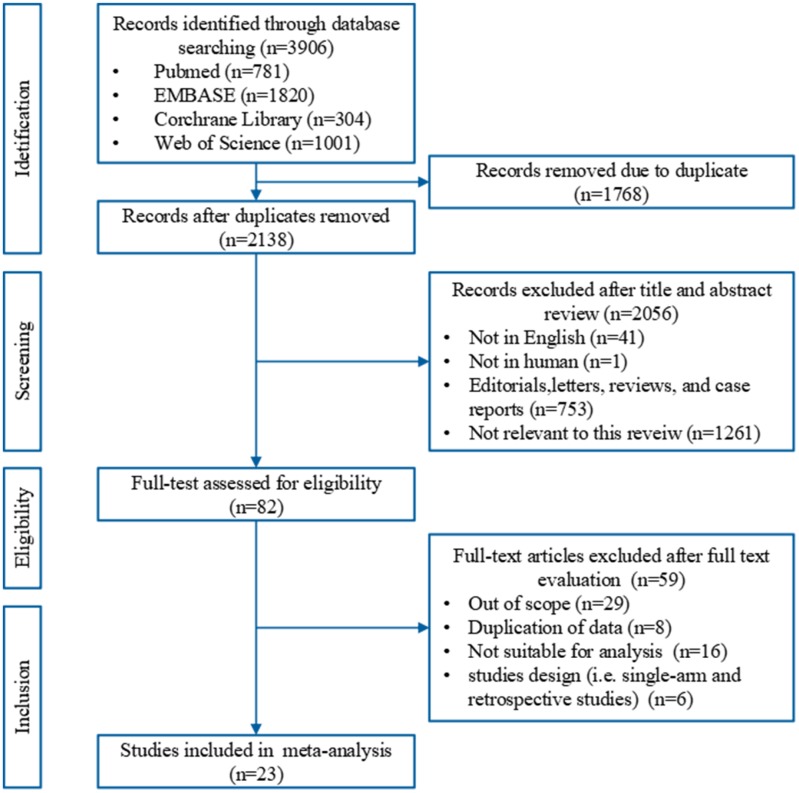
A total of 2,138 relevant records were identified in the electronic databases. Of these, 82 potentially eligible studies were reviewed with full text. Fifty-nine studies were excluded because 29 were out of scope, eight were duplicated data, 16 were not suitable for analysis, four were retrospective studies, and two were single-armed studies. However, although the study by Enriquez et al. [14] is a single-armed trial, it was controlled using historical patient data; this study was therefore included in our analysis. All together, 23 studies [7–12, 15–30] comprising 4,099 patients were included. Twenty-one studies were reported as full text publications and two [14, 25] as conference abstracts. The PRISMA flow chart of study selection is shown in Figure 1.
Figure 1.
A PRISMA flow chart of the literature search and study selection in this meta-analysis.
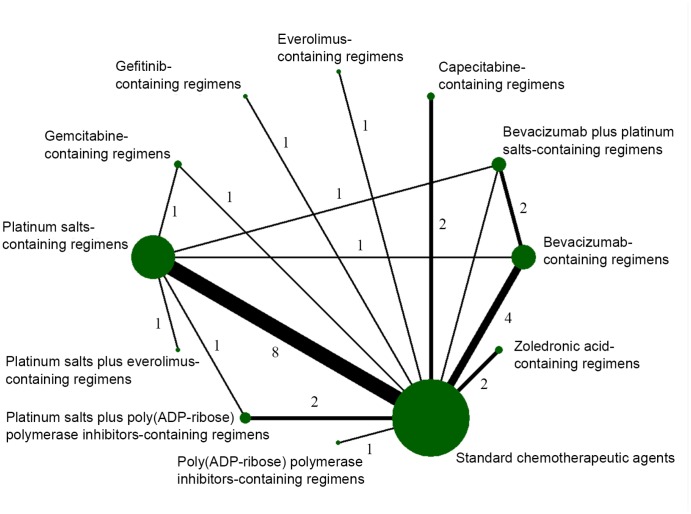
All eligible studies were published between 2010 and 2018, and patients were enrolled between 2003 and 2017. Except for the historical controlled trial (HCT) [14], all studies were randomized controlled trials (RCTs). There were six phase 3 and 17 phase 2 trials. The pCR was defined as ypT0/is ypN0 in 20 studies, whereas in three trials [15, 17, 24] pCR was defined as ypT0/is. The main characteristics of the included studies are summarized in Table 1. Twelve treatment regimens were assessed: standard chemotherapeutic agents, bevacizumab (B)-, platinum salts (P)-, B plus P (BP)-, poly(ADP-ribose) polymerase inhibitors (Pi)-, P plus Pi (PPi)-, capecitabine (Ca)-, gemcitabine (Ge)-, zoledronic acid (Za)-, everolimus (E)-, P plus E (PE)-, and gefitinib (G)-containing regimens (Figure 2). As for the four-armed GeparTrio trial [16], we only included the patients in the two arms without early response, as the other two arms compared the efficacy between four and six cycles of standard chemotherapeutic agents. Moreover, vinorelbine in the Ge-containing arm was ignored in the GeparTrio trial. In the SOLTI NeoPARP [12] trial, we combined the two arms that used different dosages of iniparib into the Pi-containing regimen for the final analysis. The treatment details of the included trials are shown in Supplementary Table 1.
Table 1. Characteristics of eligible studies.
| Study | First author country | Type of trail | Trial phase | Masking | Recruitment period | No. of center | Arms | TNBC definition | Clinical stage | No. of patients analyzed | Trial name/registry number |
| Aft 2010 | America | Prospective RCT | II | Open-label | 2003–2006 | Single | 2 | ER/PR=0%, HER2= –; 1+; 2+/Hish– | II-III | 40 | NCT00242203 |
| Houber 2010 | Switzerland | Prospective RCT | III | Open-label | 2002–2005 | Multiple | 4 | ER/PR<10%, HER2= –; 1+; 2+/Hish– | II-III | 89 | GeparTrio/NCT00544765 |
| Bernsdorf 2011 | Sweden | Prospective RCT | II | Double-blind | 2004–2007 | Multiple | 2 | NA | II-III | 82 | NCT 00239343 |
| Alba 2012 | Spain | Prospective RCT | II | Open-label | 2007–2010 | Multiple | 2 | ER/PR≤1%, HER2= –; 1+; 2+/Hish- | II-III | 93 | GEICAM/2006-03/NCT00432172 |
| Gerber 2013 | Germany | Prospective RCT | III | Open-label | 2007–2010 | Multiple | 2 | ER/PR<10%, HER2= –; 1+; 2+/Hish– | II-III | 663 | GeparQuinto/GBG 44/NCT00567554 |
| Ando 2014 | Japan | Prospective RCT | II | Open-label | 2010–2011 | Multiple | 2 | ER/PR<10%, HER2= –; 1+; 2+/Hish– | II-III | 75 | NA |
| Earl 2014 | UK | Prospective RCT | III | Open-label | 2005–2007 | Multiple | 4 | ER/PR-NA; HER2= –; 1+; 2+/Hish– | II-III | 157 | Neo-tAnGo/ NCT00070278 |
| Gonzalez-Angulo 2014 | America | Prospective RCT | II | Open-label | NA | Single | 2 | ER/PR≤5%; HER2= –; 1+; 2+/Hish- | II-III | 50 | NCT00499603 |
| Steger 2014 | Austria | Prospective RCT | III | Open-label | 2004–2008 | Multiple | 2 | ER/PR<10%, HER2= –; 1+; 2+/Hish– | Non-IV | 127 | ABCSG-24/NCT00309556 |
| von Minckwitz 2014 | Germany | Prospective RCT | II | Open-label | 2011–2012 | Multiple | 2 | ER/PR<1%, HER2= –; 1+; 2+/Hish– | II-III | 315 | GeparSixto-GBG 66/NCT01426880 |
| Earl 2015 | UK | Prospective RCT | III | Open-label | 2009–2013 | Multiple | 2 | ER/PR score=0–2/8; HER2= –; 1+; 2+/Hish– | II-III | 241 | ARTemis/NCT01093235 |
| Hasegawa 2015 | Japan | Prospective RCT | II | Open-label | 2010–2012 | Multiple | 2 | ER/PR-NA; HER2= –; 1+; 2+/Hish– | II-III | 34 | JONIE |
| Llombart-Cussac 2015 | Spain | Prospective RCT | II | Open-label | 2010–2011 | Multiple | 3 | ER/PR<10%, HER2= –; 1+; 2+/Hish– | II-III | 140 | SOLTI NeoPARP/ NCT01204125 |
| Martinez 2015 | Mexico | Prospective RCT | II | Open-label | NA | NA | 2 | NA | NA | 61 | NA |
| Sikov 2015 | America | Prospective RCT | II | Open-label | 2009–2012 | Multiple | 4 | ER/PR≤10%, HER2= –; 1+; 2+/Hish– | II-III | 433 | CALGB 40603 |
| Nahleh 2016 | America | Prospective RCT | II | Open-label | 2010–2012 | Multiple | 2 | ER/PR<1%, HER2= –; 1+; 2+/Hish– | II-III | 67 | SWOG S0800/ NCT00856492 |
| Zhang 2016 | China | Prospective RCT | II | Open-label | 2006–2012 | NA | 2 | ER/PR<10%, HER2= –; 1+; 2+/Hish– | II-III | 87 | NCT01276769 |
| Rugo 2016 | America | Prospective RCT | II | Open-label | 2010–2012 | Multiple | 2 | Special definition | II-III | 60 | I-SPY 2/NCT01042379 |
| Enriquez 2017 | Peru | Prospective HCT | II | Open-label | 2013–2014 | Single | 2 | NA | II-III | 61 | NA? |
| Gluz 2017 | Germany | Prospective RCT | II | Open-label | 2013–2015 | Multiple | 2 | ER/PR<1%, HER2= –; 1+; 2+/Hish– | Non-IV | 324 | WSG-ADAPT TN/NCT01815242 |
| Jovanović 2017 | America | Prospective RCT | II | Double-blind | 2009–2013 | Multiple | 2 | ER/PR<10%, HER2= –; 1+; 2+/Hish– | II-III | 145 | NCT00242203 |
| Loibl 2018 | Germany | Prospective RCT | III | Double-blind | 2014–2016 | Multiple | 3 | ER/PR<1%, HER2= –; 1+; 2+/Hish– | II-III | 634 | BrighTNess/NCT02032277 |
| Wu 2018 | China | Prospective RCT | II | Open-label | 2014–2017 | Single | 2 | ER/PR<10%, HER2= –; 1+; 2+/Hish– | I-III | 121 | ChiCTR-TRC-14005019 |
RCT, randomized controlled trail; HCT, historical controlled trial; NA, not available.
Figure 2.
Network diagram of eligible comparisons included in the network meta-analysis for pathological complete response (pCR). The node size is proportional to the total number of patients in the regimen. The width of each line is proportional to the number of studies comparing the two regimens linked by the line.
The quality of evidence was evaluated using the Cochrane risk of bias tool [46]. There was low risk of bias for the majority of categories. However, caution should be taken for the HCT [14] due to its high risk of selection bias. The results of quality assessment are shown in Supplementary Table 2.
Pairwise meta-analysis of primary outcome
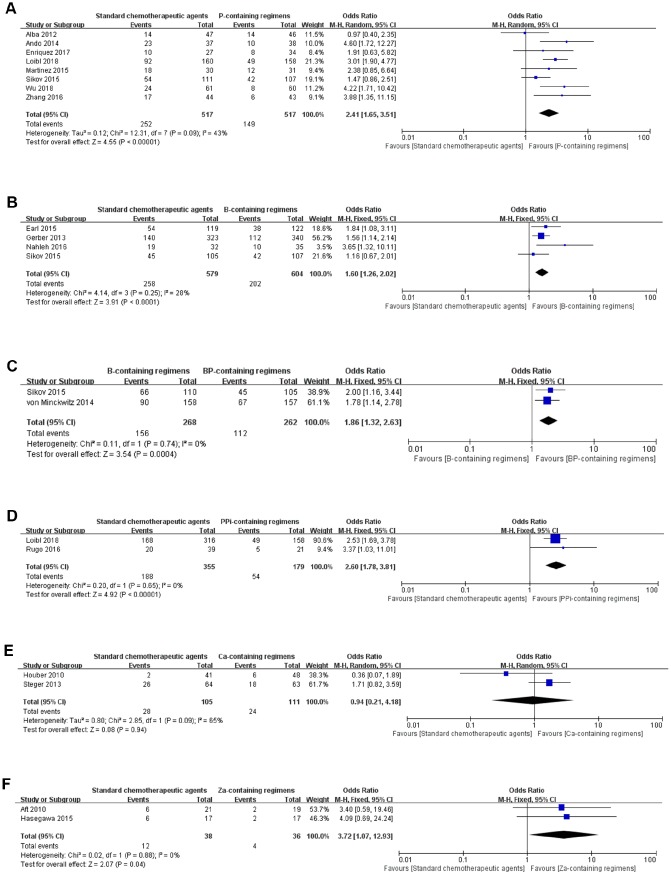
There were eight studies that directly compared standard chemotherapeutic agents with P-containing regimens. Because a modest heterogeneity (p=0.09, I2=43%) was detected, a pairwise comparison was performed with a random-effects model. We found that P-containing regimens were associated with a significant pCR benefit compared to standard chemotherapeutic agents (OR=2.41, 95% CI: 1.65–3.51, p<0.00001; Figure 3A). B-containing regimens had a better pCR than standard chemotherapeutic agents (OR=1.60, 95% CI: 1.26–2.02, p<0.0001) as analyzed by fixed-effect model (p=0.25, I2=28%; Figure 3B). BP-containing regimens were more effective than B-containing regimens (OR=1.86, 95% CI: 1.32–2.63, p=0.0004; Figure 3C). Two studies compared PPi-containing regimens with standard chemotherapeutic agents (OR=2.60, 95% CI: 1.78–3.81, p<0.00001), which indicated that PPi-containing regimens were superior in pCR achieving (Figure 3D); however, caution should be taken because the weights of the two studies were 90.6% and 9.4%, respectively. There was no significant difference between standard chemotherapeutic agents and Ca-containing regimens (OR=0.94, 95% CI: 0.21–4.18, p=0.94; Figure 3E). Za-containing regimens showed a significant pCR benefit (OR=3.72, 95% CI: 1.07–12.93, p=0.04) compared to standard chemotherapeutic agents (Figure 3F).
Figure 3.
Forest plots of pair-wise meta-analyses for pathological complete response (pCR). (A) Standard chemotherapeutic agents vs. P-containing regimens. (B) Standard chemotherapeutic agents vs. B-containing regimens. (C) B-containing regimens vs. BP-containing regimens. (D) Standard chemotherapeutic agents vs. PPi-containing regimens. (E) Standard chemotherapeutic agents vs. Ca-containing regimens. (F) Standard chemotherapeutic agents vs. Za-containing regimens.
Sensitivity analyses were conducted to detect the influence of individual studies on the comparisons of standard chemotherapeutic agents with P- and B-containing regimens by omitting one study at a time. Omission of any single study did not materially alter the pooled effects (data not shown). The shapes of funnel plots of the two comparisons were close to symmetric, and no significant publication bias was identified by Begg's and Egger's tests (Supplementary Figure 1).
Bayesian network meta-analysis of primary outcome
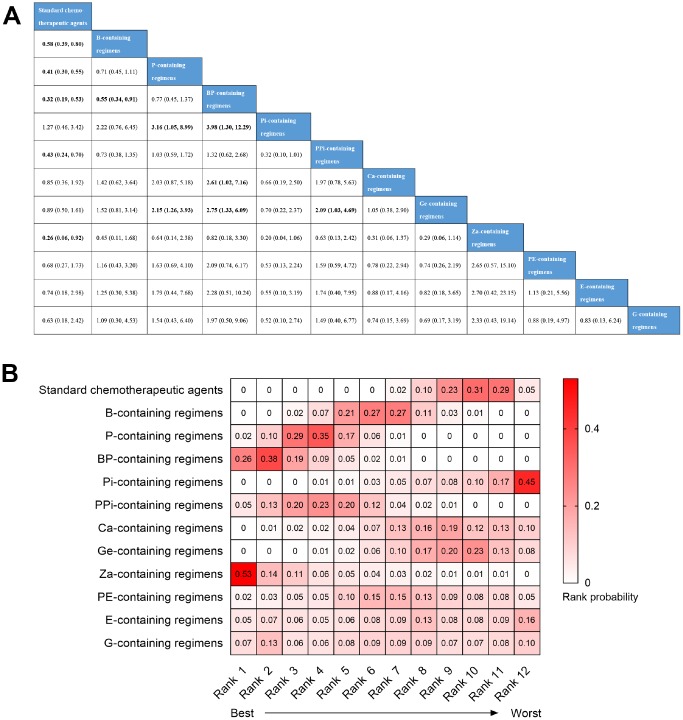
All of the 23 trials were included in the network meta-analysis for pCR. Node-splitting analysis was performed in order to evaluate the inconsistency, and no statistical difference was identified between direct and indirect evidence (data not shown). Therefore, the Bayesian network meta-analysis was conducted with a consistency model (Figure 4A). The results showed that the pCR incidence achieved by standard chemotherapeutic agents was significantly lower than B- (OR=0.58, 95% CI: 0.39–0.80), P- (OR=0.41, 95% CI: 0.30–0.55), BP- (OR=0.32, 95% CI: 0.19–0.53), PPi- (OR=0.43, 95% CI: 0.24–0.70), and Za-containing regimens (OR=0.26, 95% CI: 0.06–0.92). B-containing regimens had a poor pCR than BP-containing regimens (OR=0.55, 95% CI: 0.34–0.91). P-containing regimens were significantly related to pCR benefit compared with Pi- (OR=3.16, 95% CI: 1.05–8.99) and Ge-containing regimens (OR=2.15, 95% CI: 1.26–3.93). BP-containing regimens showed a significantly higher rate pCR than Pi- (OR=3.98, 95% CI: 1.30–12.29), Ca- (OR=2.61, 95% CI: 1.02–7.16), and Ge-containing regimens (OR=2.75, 95% CI: 1.33–6.09). Moreover, PPi-containing regimens showed a significant pCR advantage over Ge-containing regimens (OR=2.09, 95% CI: 1.03–4.69). Due to the pCR definition bias of three studies [15, 17, 24] and selection bias of the HCT [14], we further performed a subgroup analysis that excluded the regimens of the four studies. However, no significant change was observed for the positive results identified above (Supplementary Figure 2A), which demonstrated the robustness of these results.
Figure 4.
Bayesian network meta-analysis for pathological complete response (pCR). (A) The league table of comparisons. Data are presented as odds radio (OR) and 95% confidence intervals (CI). An OR>1 favors the column-defining treatment, and an OR<1 favors the row-defining treatment. (B) Heatmap of the rank probability of the twelve regimens for pCR. Rank 1 represents the best treatment and rank 12 represents the worst. Rank probabilities sum to one, both within a rank over treatments and within a treatment over ranks.
The rank probability of regimens was also analyzed. As shown in Figure 4B, the three best treatments were Za-containing regimens (53%), BP-containing regimens (38%), and P-containing regimens (29%) ranked first to third in pCR achieving, while Pi-containing regimens (45%), standard chemotherapeutic agents (29%), and Ge-containing regimens (23%) proved to be the three worst treatments, occupying rank 12 to rank 10. In the subgroup analysis of regimens without Za-containing regimens, BP-containing regimens (64%) were the best treatment for pCR followed by P-containing regimens (41%) and PPi-containing regimens (30%). Consistently, Pi-containing regimens (47%), standard chemotherapeutic agents (27%), and Ge-containing regimens (20%) remained the three worst treatments (Supplementary Figure 2B).
Meta-analysis for grade 3–4 hematological adverse events
There were 11 trails with eight regimens that reported anemia, 16 trials with 10 regimens that reported neutropenia, and 13 trials with seven regimens that reported thrombocytopenia (Supplementary Table 3 and Supplementary Figure 3). We found that P-containing regimens were associated with higher risk of anemia (OR=16.49, 95% CI: 7.52–36.14, p<0.00001), neutropenia (OR=3.30, 95% CI: 1.35–8.08, p=0.009), and thrombocytopenia (OR=12.93, 95% CI: 5.91–28.29, p<0.00001) compared with standard chemotherapeutic agents (Supplementary Figure 4A, 4B, and 4D). Consistently, subgroup analyses based on TNBC patients also revealed that P-containing regimens resulted in a higher incidence of anemia (OR=15.54, 95% CI: 6.64–36.34, p<0.00001), neutropenia (OR=3.36, 95% CI: 1.04–10.83, p=0.04) and thrombocytopenia (OR=13.84, 95% CI: 6.14–31.20, p<0.00001), compared to standard chemotherapeutic agents (Supplementary Figure 5A–5C). B-containing regimens were associated with a higher risk of neutropenia (OR=1.20, 95% CI: 1.01–1.43, p=0.04) than standard chemotherapeutic agents (Supplementary Figure 4C). No significant bias was identified by funnel plots or Begg's and Egger's tests (Supplementary Figure 6).
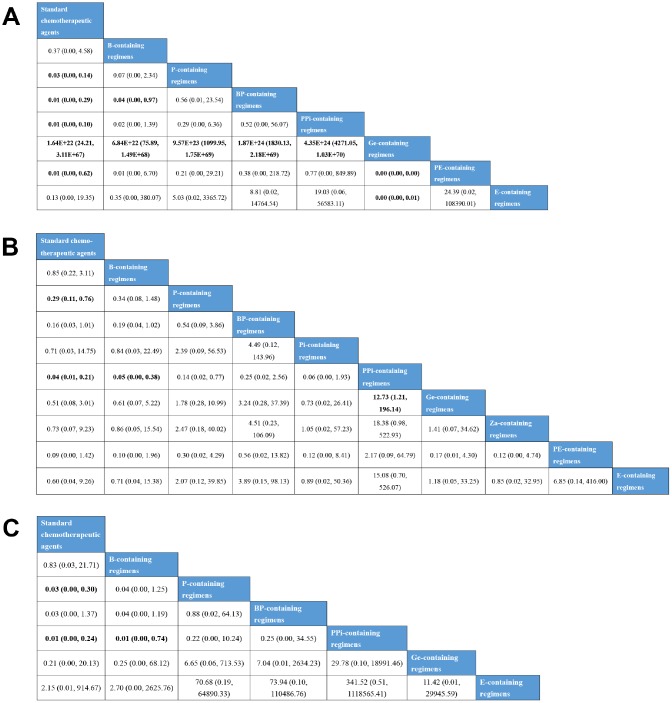
Indirect comparisons were then performed using a consistency model, as node-splitting analyses revealed no significant difference between the direct and indirect evidence for anemia, neutropenia, and thrombocytopenia (Figure 5). With respect to anemia, standard chemotherapeutic agents (OR=1.64E+22, 95% CI: 24.21–3.11E+67), B- (OR=6.84E+22, 95% CI: 75.89–1.49E+68), P- (OR=9.57E+23, 95% CI: 1099.95–1.75E+69), BP- (OR=1.87E+24, 95% CI: 1830.13–2.18E+69), PPi- (OR=4.35E+24, 95% CI: 4271.05–1.03E+70), PE- (OR=0.00, 95% CI: 0.00–0.00), and E-containing regimens (OR=0.00, 95% CI: 0.00–0.01) were associated with higher incidences than Ge-containing regimens. P- (OR=0.03, 95% CI: 0.00–0.14), BP- (OR=0.01, 95% CI: 0.00–0.29), PPi- (OR=0.01, 95% CI: 0.00–0.10), and PE-containing regimens (OR=0.01, 95% CI: 0.00–0.62) induced more anemia events than standard chemotherapeutic agents. BP-containing regimens (OR=0.04, 95% CI: 0.00–0.97) induced more anemia events than B-containing regimens. Neutropenia was significantly lower in standard chemotherapeutic agents than in P- (OR=0.29, 95% CI: 0.11–0.76) and PPi-containing regimens (OR=0.04, 95% CI: 0.01–0.21). B- (OR=0.05, 95% CI: 0.00–0.38) and Ge-containing regimens (OR=12.73, 95% CI: 1.21–196.14) were associated with lower incidences of neutropenia compared to PPi-containing regimens. With respect to thrombocytopenia, P- (OR=0.03, 95% CI: 0.00–0.30) and PPi-containing regimens (OR=0.01, 95% CI: 0.00–0.24) were associated with a higher risk of incidence than standard chemotherapeutic agents. PPi-containing regimens also had a higher risk of thrombocytopenia compared to B-containing regimens (OR=0.01, 95% CI: 0.00–0.74).
Figure 5.
Bayesian network meta-analysis for grade 3–4 hematological adverse events. (A) The league table for comparisons of anemia. (B) The league table for comparisons of neutropenia. (C) The league table for comparisons of thrombocytopenia. Data are presented as odds radio (OR) and 95% confidence intervals (CI). An OR>1 favors the row-defining treatment, and OR<1 favors the column-defining treatment.
The rank probability for each treatment inducing SAEs showed that Ge-containing regimens (99%) were the best treatment, resulting in the lowest incidence of anemia adverse events, whereas PE-containing regimens (45%) were found to be the worst treatment (Supplementary Figure 7A). PPi-containing regimens ranked first for the highest prevalence of neutropenia (60%) and thrombocytopenia (64%) events (Supplementary Figure 7B and 7C). Pi- (26%) and E-containing regimens (52%) had the lowest probability of leading to neutropenia and thrombocytopenia, respectively.
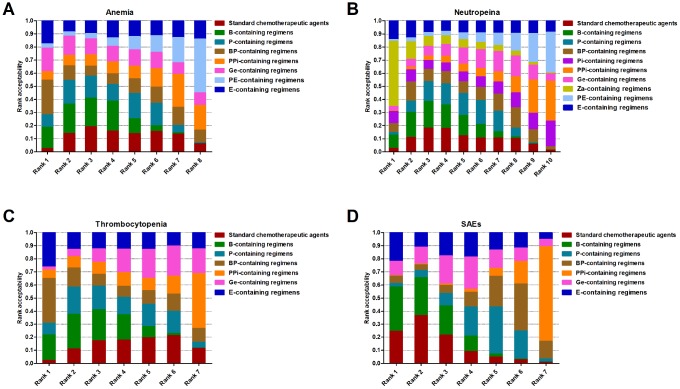
Stochastic multi-criteria acceptability analysis (SMAA)
Benefit-risk analyses were performed by SMAA with missing preferences. Standard chemotherapeutic agents were set as the baseline. The analyses between pCR and anemia showed that BP-containing regimens had the highest acceptability (26.46%), ranking first (Figure 6A) with a CF=0.34 (Supplementary Figure 8A). Za-containing regimens (49.72%, Figure 6B) were the best treatment when considering pCR and neutropenia with a CF=0.62 (Supplementary Figure 8B). BP-containing regimens ranked first in acceptability (34.18%, CF=0.42), resulting in a higher pCR and fewer thrombocytopenia events (Figure 6C and Supplementary Figure 8C). When considering pCR with the three SAEs, B-containing regimens were the best choice with highest rank acceptability (34.01%, Figure 6D) and a CF=0.43 (Supplementary Figure 8D).
Figure 6.
Stochastic multi-criteria acceptability analysis for benefit-risk. (A) Rank probability of regimens based on synthesizing pCR and anemia. (B) Rank probability of regimens based on synthesizing pCR and neutropenia. (C) Rank probability of regimens based on synthesizing pCR and thrombocytopenia. (D) Rank probability of regimens based on synthesizing pCR and the three serious adverse events. Rank 1 represents the best treatment and rank N represents the worst. The proportion corresponds to the probability of each regimen to be at a specific rank.
DISCUSSION
A growing number of clinical trials are being performed in order to improve the effectiveness of neoadjuvant chemotherapies in TNBC by adding different drugs to the standard chemotherapeutic agents. However, results are controversial and remain isolated in the absence of systematic integration. Therefore, a comprehensive study was warranted to give a summary of the results from these publications. To the best of our knowledge, this is the first network meta-analysis to investigate the pCR efficacy and safety of neoadjuvant chemotherapy regimens in TNBC.
In the present study, we enrolled 23 clinical trials with 4,099 TNBC individuals assigned to 12 neoadjuvant chemotherapy regimens, aiming to identify which treatment was optimal in achieving higher pCR rates and resulting in fewer SAEs. The results of pairwise meta-analyses showed that the most highly studied P-containing regimens were significantly associated with better pCR rates, but worse SAEs, compared with standard chemotherapeutic agents. Consistently, two previous meta-analyses also revealed that platinum-based neoadjuvant chemotherapies clearly increased pCR rates compared with platinum-free neoadjuvant chemotherapies [31, 32]. Although no survival benefit was observed for platinum-based neoadjuvant chemotherapy as pooled by two RCTs [31], many more studies with long-term follow-up are required to clarify the potential association between survival outcomes and platinum salts. TNBC was demonstrated to be more sensitive to platinum salts than non-TNBC [32], with the probable reason being that TNBC is more commonly related to BRCA mutations or homologous recombination DNA repair deficiencies [33, 34]. PARP inhibitors can block DNA repair pathways, which are crucial for tumor cell survival in patients with BRCA mutations or homologous recombination DNA repair deficiencies [34]. Therefore, it is reasonable to speculate that PARP inhibitors might enhance the anti-tumor activity of cytotoxic agents resulting in DNA damage, such as platinum salts. However, in this study, although PPi-containing regimens significantly increased pCR rates compared to standard chemotherapeutic agents, there was no difference in efficacy between P- and PPi-containing regimens, indicating that PARP inhibitors did not enhance the effects of platinum salts. This result is consistent with the findings of BrighTNess trial [9]. Moreover, a benefit-risk analysis showed that PPi-containing regimens might be the worst treatment choice when considering pCR and SAEs. In addition, we found that Pi-containing regimens without platinum salts were not superior to any other regimen. Thus, our results do not support further investigation into the use of PARP inhibitors added to standard chemotherapeutic agents or in combination with platinum salts at the present dosage in TNBC patients.
Bevacizumab is another frequently studied agent in neoadjuvant chemotherapy for TNBC. It has shown clinical efficacy in prolonging progression-free-survival, but not overall survival, in metastatic TNBC [35]. In our work, we found that B-containing regimens were significantly associated with a higher pCR rate than standard chemotherapeutic agents, while only a modest correlation between B-containing regimens and neutropenia prevalence was detected. However, bevacizumab may lead to other adverse events in the circulatory, nervous or urinary systems [26, 35]. Consistent with our study, a recent network meta-analysis reported that bevacizumab plus chemotherapy significantly improved pCR of TNBC patients when compared with chemotherapy plus placebo [36]. Moreover, bevacizumab plus chemotherapy was demonstrated to be significantly associated with longer progression-free survival than chemotherapy alone in advanced/metastatic TNBC [37]. Although no significant different was detected between B- and P-containing regimens in pCR rates, the combination of bevacizumab and platinum salts (BP-containing regimens) was able to increase the efficacy of both B- and P-containing regimens, when compared with standard chemotherapeutic agents. Importantly, our benefit-risk analysis revealed that B-containing regimens might be the best treatment to achieve a relatively high pCR rate with fewer hematological SAEs.
To our surprise, zoledronic acid, a nitrogen-containing bisphosphonate that induces osteoclast apoptosis and inhibits bone resorption [38], showed a significant pCR benefit when added to standard chemotherapeutic agents. No statistical difference in SAEs incidence was observed between Za-containing regimens and standard chemotherapeutic agents. Moreover, Za-containing regimens had the highest probability of being the best treatment for achieving pCR. However, caution should be taken due to the limited number of subjects in the two original RCTs investigating Za-containing regimens, with only 40 and 34 patients, respectively [15, 24]. Although the effects of zoledronic acid on pCR rate were not striking in the two RCTs, the pooled effect was statistically significant, mainly due to the larger sample size in our work. Accordingly, we hold the opinion that further RCTs with larger sample sizes are needed to confirm any potential pCR benefit of zoledronic acid, and to strengthen our results. In addition to its anti-metastatic properties within bone tissue, the anti-tumor activities of zoledronic acid may be explained by several mechanisms, including inducing tumor cell apoptosis, enhancing the cytotoxic effects of chemotherapeutic agents, suppressing neoangiogenesis, and involving immunomodulation [39–42]. Moreover, disease-free survival benefits of zoledronic acid have also been detected in premenopausal endocrine-positive patients [43, 44]. However, the survival benefit of zoledronic acid in TNBC remains unclear.
There are several limitations of the present study. First, the sample sizes of several trials were relatively small. Specifically, the three RCTs involving Za-containing regimens and the study of E-containing regimens only included approximately 50 TNBC patients, which might weaken the effects or lead to false positive results. In addition, there were only one study for E-, PE, and Ge-containing regimens and the number of SAEs very relatively small in these studies, which might result in the wide 95% CIs; therefore, the results of SEAs regarding these regimens should be interpreted with caution. Second, there are several potential heterogeneities in the included studies, such as pCR definition, study design, and the specific components of standard chemotherapeutic agents. However, subgroup and sensitivity analyses based on pCR definition and study design demonstrated that the heterogeneities were unlikely to refute the overall results. Moreover, we integrated taxanes, anthracyclines, cyclophosphamide, and fluorouracil as comparative standard chemotherapeutic agents, as most control arms of the included studies were based on these four kinds of drugs, but differences still existed between studies. Therefore, consideration of these heterogeneities should be taken into account in the interpretation of our findings. Third, the kinds of SAEs reported in each study were different, and SAE data were not available for several trials. Thus, it was difficult to conduct a comprehensive analysis for all SAEs and regimens. Although there was no evidence showing a significant correlation between SAEs and the molecular subtype of breast cancer, there may be bias in the pooled effects of SAEs compared to the real results. Fourth, the correlation between neoadjuvant chemotherapy and survival outcomes was not evaluated due to the lack of survival data in most studies. However, we noticed that some RCTs are still ongoing and a secondary analysis focusing on long-term survival benefits may be reported in the near future. Therefore, a subsequent updated network meta-analysis will help to integrate the effects of these regimens on clinical outcomes.
Despite the aforementioned limitations, our study has for the first time systematically compared the pCR efficacy and hematological SAEs of the currently available neoadjuvant chemotherapy regimens in TNBC. In conclusion, this study demonstrated that Za-, BP-, P-, and B-containing regimens are the top four treatment strategies, showing a high efficacy in achieving pCR. When considering both efficacy and SAEs, B-containing regimens had the highest acceptability to be the best treatment for achieving a relatively high pCR with fewer SAEs. However, additional well-designed RCTs with larger sample sizes are required to strengthen the findings of this meta-analysis and further determine the survival benefits of these neoadjuvant therapies in TNBC.
METHODS
Search strategy
This meta-analysis was performed in accordance with the guideline of Preferred Reporting Items for Systematic Reviews and Meta-analyses (PRISMA) [45]. Literatures, published before May 31, 2018, were identified in PubMed, Embase, Cochrane library, and Web of Science. The following key words were used: (breast OR mammary) AND (cancer OR cancers OR tumor OR neoplasm OR carcinoma) AND (neoadjuvant chemotherapy OR induction chemotherapy OR pre-operative chemotherapy) AND (TNBC OR triple-negative OR triple negative OR basal-like OR HER2 negative) AND (pathological complete response OR pCR), without any restrictions. The reference lists from relevant studies, reviews, and meta-analyses were manually screened for potentially eligible publications.
Selection criteria
The inclusion and exclusion criteria were prespecified. Eligible trials were studies prospectively comparing at least two arms of different neoadjuvant chemotherapy regimens in TNBC patients. Studies were excluded if they were: (1) non-human studies, letters, reviews, editorial comments or case reports; (2) single-arm or dosage-finding studies; (3) articles without raw data or with a sample size of less than 30; and (4) ongoing trials without reported results. If several publications from the same trial were identified, only the latest or complete publication was included. Two reviewers independently evaluated the risk of bias for eligible studies using the Cochrane Collaboration risk of bias tool [46]. Any discrepancies were resolved by discussing with all investigators.
Data extraction
Data were extracted by two independent authors. The following information was recorded for eligible studies: first author name, publication year, country, study design, trial phase, recruitment period, masking, number of centers, TNBC definition, clinical stage of patients, and trial name or registry number. Treatment regimens, sample size, primary outcome (pCR), and secondary outcome (grade 3–4 hematological adverse events), if available, were also recorded.
Treatment regimens and outcomes definition
Due to the widespread use of combinations of taxanes, anthracyclines, cyclophosphamide, and/or fluorouracil, we defined the regimen as standard chemotherapeutic agents, which consisted of treatment with certain or all four drugs. The addition of any other drugs based on the standard chemotherapeutic agents was regarded as a new regimen. In the case of multi-arm studies comparing different dosages of one agent with another, we combined the results of the same agent into one arm. Administration sequence and frequency were not considered in the present study. The primary outcome was pCR, which was defined as the absence of invasive breast cancer in the breast and axillary lymph nodes (ypT0/is ypN0). If ypT0/is ypN0 was not reported, ypT0/is, defined as the absence of invasive breast cancer in the breast, was substituted. Secondary outcomes were treatment-related serious (grade 3–4) adverse events (SAEs) in hematology, including anemia, neutropenia, and thrombocytopenia. As for SAEs, we hypothesized that there was no significant correlation between molecular subtypes and hematological adverse events. Therefore, if the SAEs of TNBC were not available, we included the number of SAEs from all molecular subtypes of breast cancer patients. If only the percentages of primary and secondary outcomes were reported, we calculated the number of events by multiplying percentages by the number of patients.
Statistical methods
The odds ratio (OR) was utilized for estimating pooling effect sizes. For the pairwise meta-analysis, heterogeneity was calculated using Cochrane Q statistics and an I2 test. Statistical heterogeneity was defined as p<0.1 and/or I2>50%. A pairwise meta-analysis was conducted with a random-effects model or a fixed-effect model depending on the existence of statistical heterogeneity or not, respectively. All pairwise meta-analyses were performed by Review Manager software version 5.2. Results were reported as OR and 95% confidence intervals (CIs). All p-values were two-sided and a value less than 0.05 was considered statistically significant. Publication bias was detected by funnel plots, Begg’s and Egger’s tests using Stata software version 12.0.
A Bayesian network-meta analysis was performed by Aggregate Data Drug Information System (ADDIS) software, version 1.16.8 (http://www.drugis.org) [47]. The consistency between direct and indirect evidence was verified by node splitting analyses. If no significant inconsistency was detected, a consistency model was used to analyze the relative effects of the interventions. Otherwise, an inconsistency model was applied. Convergence was assessed using the Brooks-Gelman-Rubin method, which compared within-chain and between-chain variance to calculate the potential scale reduction factor (PSRF). We defined a PSRF of less than 1.05 as an indication of achieving convergence, and finished the simulation. Otherwise, the model should be extended until the PSRF is less than 1.05. The results of the network meta-analyses were presented as OR and 95% CI. Rank probability for each treatment was calculated to achieve the treatment ranking. Benefit-risk analyses were performed with synthesis evidence by stochastic multi-criteria acceptability analysis (SMAA) to jointly analyze the efficacy and SAEs for interventions. Rank acceptability and confidence factor (CF) were calculated with missing preference.
Supplementary Material
Footnotes
AUTHOR CONTRIBUTIONS: Conceptualization, G.S.R. and H.Z.L.; Methodology, Y.H.L. and D.J.Y.; Formal Analysis, Y.H.L. and P.C.; Investigation, Y.H.L., D.J.Y. and P.C.; Data Curation, H.Z.L. and X.D.Y.; Writing—Original Draft Preparation, Y.H.L., D.J.Y. and P.C.; Writing—Review & Editing, Y.H.L., D.J.Y., J.Z.S. and X.D.Y.; Supervision, G.S.R. and H.Z.L.; Project Administration, H.Z.L.. All the authors read and approved the final manuscript.
CONFLICTS OF INTEREST: The authors declare no conflicts of interest.
FUNDING: This study was supported by National Natural Science Foundation of China (No. 81472475), Chongqing Science & Technology Commission (No. cstc2016jcyjA0313), and Scientific Research Foundation of Chongqing Medical University (No. 201408).
REFERENCES
- 1.Foulkes WD, Smith IE, Reis-Filho JS. Triple-negative breast cancer. N Engl J Med. 2010; 363:1938–48. 10.1056/NEJMra1001389 [DOI] [PubMed] [Google Scholar]
- 2.Joensuu H, Gligorov J. Adjuvant treatments for triple-negative breast cancers. Ann Oncol. 2012. (Suppl 6); 23:vi40–45. 10.1093/annonc/mds194 [DOI] [PubMed] [Google Scholar]
- 3.Berry DA, Cirrincione C, Henderson IC, Citron ML, Budman DR, Goldstein LJ, Martino S, Perez EA, Muss HB, Norton L, Hudis C, Winer EP. Estrogen-receptor status and outcomes of modern chemotherapy for patients with node-positive breast cancer. JAMA. 2006; 295:1658–67. 10.1001/jama.295.14.1658 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Carey LA, Dees EC, Sawyer L, Gatti L, Moore DT, Collichio F, Ollila DW, Sartor CI, Graham ML, Perou CM. The triple negative paradox: primary tumor chemosensitivity of breast cancer subtypes. Clin Cancer Res. 2007; 13:2329–34. 10.1158/1078-0432.CCR-06-1109 [DOI] [PubMed] [Google Scholar]
- 5.Cortazar P, Zhang L, Untch M, Mehta K, Costantino JP, Wolmark N, Bonnefoi H, Cameron D, Gianni L, Valagussa P, Swain SM, Prowell T, Loibl S, et al. Pathological complete response and long-term clinical benefit in breast cancer: the CTNeoBC pooled analysis. Lancet. 2014; 384:164–72. 10.1016/S0140-6736(13)62422-8 [DOI] [PubMed] [Google Scholar]
- 6.Liedtke C, Mazouni C, Hess KR, André F, Tordai A, Mejia JA, Symmans WF, Gonzalez-Angulo AM, Hennessy B, Green M, Cristofanilli M, Hortobagyi GN, Pusztai L. Response to neoadjuvant therapy and long-term survival in patients with triple-negative breast cancer. J Clin Oncol. 2008; 26:1275–81. 10.1200/JCO.2007.14.4147 [DOI] [PubMed] [Google Scholar]
- 7.Ando M, Yamauchi H, Aogi K, Shimizu S, Iwata H, Masuda N, Yamamoto N, Inoue K, Ohono S, Kuroi K, Hamano T, Sukigara T, Fujiwara Y. Randomized phase II study of weekly paclitaxel with and without carboplatin followed by cyclophosphamide/epirubicin/5-fluorouracil as neoadjuvant chemotherapy for stage II/IIIA breast cancer without HER2 overexpression. Breast Cancer Res Treat. 2014; 145:401–09. 10.1007/s10549-014-2947-1 [DOI] [PubMed] [Google Scholar]
- 8.Zhang P, Yin Y, Mo H, Zhang B, Wang X, Li Q, Yuan P, Wang J, Zheng S, Cai R, Ma F, Fan Y, Xu B. Better pathologic complete response and relapse-free survival after carboplatin plus paclitaxel compared with epirubicin plus paclitaxel as neoadjuvant chemotherapy for locally advanced triple-negative breast cancer: a randomized phase 2 trial. Oncotarget. 2016; 7:60647–56. 10.18632/oncotarget.10607 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Loibl S, O’Shaughnessy J, Untch M, Sikov WM, Rugo HS, McKee MD, Huober J, Golshan M, von Minckwitz G, Maag D, Sullivan D, Wolmark N, McIntyre K, et al. Addition of the PARP inhibitor veliparib plus carboplatin or carboplatin alone to standard neoadjuvant chemotherapy in triple-negative breast cancer (BrighTNess): a randomised, phase 3 trial. Lancet Oncol. 2018; 19:497–509. 10.1016/S1470-2045(18)30111-6 [DOI] [PubMed] [Google Scholar]
- 10.Earl HM, Hiller L, Dunn JA, Blenkinsop C, Grybowicz L, Vallier AL, Abraham J, Thomas J, Provenzano E, Hughes-Davies L, Gounaris I, McAdam K, Chan S, et al. , and ARTemis Investigators. Efficacy of neoadjuvant bevacizumab added to docetaxel followed by fluorouracil, epirubicin, and cyclophosphamide, for women with HER2-negative early breast cancer (ARTemis): an open-label, randomised, phase 3 trial. Lancet Oncol. 2015; 16:656–66. 10.1016/S1470-2045(15)70137-3 [DOI] [PubMed] [Google Scholar]
- 11.Rugo HS, Olopade OI, DeMichele A, Yau C, van ’t Veer LJ, Buxton MB, Hogarth M, Hylton NM, Paoloni M, Perlmutter J, Symmans WF, Yee D, Chien AJ, et al. , and I-SPY 2 Investigators. Adaptive Randomization of Veliparib-Carboplatin Treatment in Breast Cancer. N Engl J Med. 2016; 375:23–34. 10.1056/NEJMoa1513749 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Llombart-Cussac A, Bermejo B, Villanueva C, Delaloge S, Morales S, Balmaña J, Amillano K, Bonnefoi H, Casas A, Manso L, Roché H, Gonzalez-Santiago S, Gavilá J, et al. SOLTI NeoPARP: a phase II randomized study of two schedules of iniparib plus paclitaxel versus paclitaxel alone as neoadjuvant therapy in patients with triple-negative breast cancer. Breast Cancer Res Treat. 2015; 154:351–57. 10.1007/s10549-015-3616-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bafeta A, Trinquart L, Seror R, Ravaud P. Reporting of results from network meta-analyses: methodological systematic review. BMJ. 2014; 348:g1741. 10.1136/bmj.g1741 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Enriquez D, Nieto NP, Fuentes HA, Guerra H, Mendoza RE, Gomez HL. Improving pathological response in locally advanced triple negative breast cancer: comparison between CbD and AC-T regimens. J Clin Oncol. 2017; 35:35 10.1200/JCO.2017.35.15_suppl.585 [DOI] [Google Scholar]
- 15.Aft R, Naughton M, Trinkaus K, Watson M, Ylagan L, Chavez-MacGregor M, Zhai J, Kuo S, Shannon W, Diemer K, Herrmann V, Dietz J, Ali A, et al. Effect of zoledronic acid on disseminated tumour cells in women with locally advanced breast cancer: an open label, randomised, phase 2 trial. Lancet Oncol. 2010; 11:421–28. 10.1016/S1470-2045(10)70054-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Huober J, von Minckwitz G, Denkert C, Tesch H, Weiss E, Zahm DM, Belau A, Khandan F, Hauschild M, Thomssen C, Högel B, Darb-Esfahani S, Mehta K, Loibl S. Effect of neoadjuvant anthracycline-taxane-based chemotherapy in different biological breast cancer phenotypes: overall results from the GeparTrio study. Breast Cancer Res Treat. 2010; 124:133–40. 10.1007/s10549-010-1103-9 [DOI] [PubMed] [Google Scholar]
- 17.Bernsdorf M, Ingvar C, Jörgensen L, Tuxen MK, Jakobsen EH, Saetersdal A, Kimper-Karl ML, Kroman N, Balslev E, Ejlertsen B. Effect of adding gefitinib to neoadjuvant chemotherapy in estrogen receptor negative early breast cancer in a randomized phase II trial. Breast Cancer Res Treat. 2011; 126:463–70. 10.1007/s10549-011-1352-2 [DOI] [PubMed] [Google Scholar]
- 18.Alba E, Chacon JI, Lluch A, Anton A, Estevez L, Cirauqui B, Carrasco E, Calvo L, Segui MA, Ribelles N, Alvarez R, Sanchez-Muñoz A, Sanchez R, et al. A randomized phase II trial of platinum salts in basal-like breast cancer patients in the neoadjuvant setting. Results from the GEICAM/2006-03, multicenter study. Breast Cancer Res Treat. 2012; 136:487–93. 10.1007/s10549-012-2100-y [DOI] [PubMed] [Google Scholar]
- 19.Gerber B, Loibl S, Eidtmann H, Rezai M, Fasching PA, Tesch H, Eggemann H, Schrader I, Kittel K, Hanusch C, Kreienberg R, Solbach C, Jackisch C, et al. , and German Breast Group Investigators. Neoadjuvant vacizumab and anthracycline-taxane-based chemotherapy in 678 triple-negative primary breast cancers; results from the geparquinto study (GBG 44). Ann Oncol. 2013; 24:2978–84. 10.1093/annonc/mdt361 [DOI] [PubMed] [Google Scholar]
- 20.Earl HM, Vallier AL, Hiller L, Fenwick N, Young J, Iddawela M, Abraham J, Hughes-Davies L, Gounaris I, McAdam K, Houston S, Hickish T, Skene A, et al. , and Neo-tAnGo Investigators. Effects of the addition of gemcitabine, and paclitaxel-first sequencing, in neoadjuvant sequential epirubicin, cyclophosphamide, and paclitaxel for women with high-risk early breast cancer (Neo-tAnGo): an open-label, 2×2 factorial randomised phase 3 trial. Lancet Oncol. 2014; 15:201–12. 10.1016/S1470-2045(13)70554-0 [DOI] [PubMed] [Google Scholar]
- 21.Gonzalez-Angulo AM, Akcakanat A, Liu S, Green MC, Murray JL, Chen H, Palla SL, Koenig KB, Brewster AM, Valero V, Ibrahim NK, Moulder-Thompson S, Litton JK, et al. Open-label randomized clinical trial of standard neoadjuvant chemotherapy with paclitaxel followed by FEC versus the combination of paclitaxel and everolimus followed by FEC in women with triple receptor-negative breast cancer. Ann Oncol. 2014; 25:1122–27. 10.1093/annonc/mdu124 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Steger GG, Greil R, Lang A, Rudas M, Fitzal F, Mlineritsch B, Hartmann BL, Bartsch R, Melbinger E, Hubalek M, Stoeger H, Dubsky P, Ressler S, et al. , and Austrian Breast and Colorectal Study Group (ABCSG). Epirubicin and docetaxel with or without capecitabine as neoadjuvant treatment for early breast cancer: final results of a randomized phase III study (ABCSG-24). Ann Oncol. 2014; 25:366–71. 10.1093/annonc/mdt508 [DOI] [PubMed] [Google Scholar]
- 23.von Minckwitz G, Schneeweiss A, Loibl S, Salat C, Denkert C, Rezai M, Blohmer JU, Jackisch C, Paepke S, Gerber B, Zahm DM, Kümmel S, Eidtmann H, et al. Neoadjuvant carboplatin in patients with triple-negative and HER2-positive early breast cancer (GeparSixto; GBG 66): a randomised phase 2 trial. Lancet Oncol. 2014; 15:747–56. 10.1016/S1470-2045(14)70160-3 [DOI] [PubMed] [Google Scholar]
- 24.Hasegawa Y, Tanino H, Horiguchi J, Miura D, Ishikawa T, Hayashi M, Takao S, Kim SJ, Yamagami K, Miyashita M, Konishi M, Shigeoka Y, Suzuki M, et al. , and JONIE Study Group. Randomized Controlled Trial of Zoledronic Acid plus Chemotherapy versus Chemotherapy Alone as Neoadjuvant Treatment of HER2-Negative Primary Breast Cancer (JONIE Study). PLoS One. 2015; 10:e0143643. 10.1371/journal.pone.0143643 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Martinez MC, Arce-Salinas C, Alvarado-Miranda A, Lara-Medina F, Flores-Diaz D, Matus JA, Bargallo-Rocha E, Shaw-Dulin R, Maldonado H, Mendoza-Galindo L, Perez-Sanchez V. Randomized phase II trial to evaluate the safety and efficacy of neoadjuvant cisplatin in combination with taxanesanthracyclines vs taxanesanthracyclines alone in locally advanced triple negative breast cancer. J Clin Oncol. 2015; 33e12024–e12024. 10.1200/jco.2015.33.15_suppl.e12024 [DOI] [Google Scholar]
- 26.Sikov WM, Berry DA, Perou CM, Singh B, Cirrincione CT, Tolaney SM, Kuzma CS, Pluard TJ, Somlo G, Port ER, Golshan M, Bellon JR, Collyar D, et al. Impact of the addition of carboplatin and/or bevacizumab to neoadjuvant once-per-week paclitaxel followed by dose-dense doxorubicin and cyclophosphamide on pathologic complete response rates in stage II to III triple-negative breast cancer: CALGB 40603 (Alliance). J Clin Oncol. 2015; 33:13–21. 10.1200/JCO.2014.57.0572 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Nahleh ZA, Barlow WE, Hayes DF, Schott AF, Gralow JR, Sikov WM, Perez EA, Chennuru S, Mirshahidi HR, Corso SW, Lew DL, Pusztai L, Livingston RB, Hortobagyi GN. SWOG S0800 (NCI CDR0000636131): addition of bevacizumab to neoadjuvant nab-paclitaxel with dose-dense doxorubicin and cyclophosphamide improves pathologic complete response (pCR) rates in inflammatory or locally advanced breast cancer. Breast Cancer Res Treat. 2016; 158:485–95. 10.1007/s10549-016-3889-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Gluz O, Nitz U, Liedtke C, Christgen M, Grischke EM, Forstbauer H, Braun M, Warm M, Hackmann J, Uleer C, Aktas B, Schumacher C, Bangemann N, et al. Comparison of Neoadjuvant Nab-Paclitaxel+Carboplatin vs Nab-Paclitaxel+Gemcitabine in Triple-Negative Breast Cancer: Randomized WSG-ADAPT-TN Trial Results. J Natl Cancer Inst. 2018; 110:628–637. 10.1093/jnci/djx258 [DOI] [PubMed] [Google Scholar]
- 29.Jovanović B, Mayer IA, Mayer EL, Abramson VG, Bardia A, Sanders ME, Kuba MG, Estrada MV, Beeler JS, Shaver TM, Johnson KC, Sanchez V, Rosenbluth JM, et al. A Randomized Phase II Neoadjuvant Study of Cisplatin, Paclitaxel With or Without Everolimus in Patients with Stage II/III Triple-Negative Breast Cancer (TNBC): Responses and Long-term Outcome Correlated with Increased Frequency of DNA Damage Response Gene Mutations, TNBC Subtype, AR Status, and Ki67. Clin Cancer Res. 2017; 23:4035–45. 10.1158/1078-0432.CCR-16-3055 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Wu X, Tang P, Li S, Wang S, Liang Y, Zhong L, Ren L, Zhang T, Zhang Y. A randomized and open-label phase II trial reports the efficacy of neoadjuvant lobaplatin in breast cancer. Nat Commun. 2018; 9:832. 10.1038/s41467-018-03210-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Poggio F, Bruzzone M, Ceppi M, Pondé NF, La Valle G, Del Mastro L, de Azambuja E, Lambertini M. Platinum-based neoadjuvant chemotherapy in triple-negative breast cancer: a systematic review and meta-analysis. Ann Oncol. 2018; 29:1497–508. 10.1093/annonc/mdy127 [DOI] [PubMed] [Google Scholar]
- 32.Petrelli F, Coinu A, Borgonovo K, Cabiddu M, Ghilardi M, Lonati V, Barni S. The value of platinum agents as neoadjuvant chemotherapy in triple-negative breast cancers: a systematic review and meta-analysis. Breast Cancer Res Treat. 2014; 144:223–32. 10.1007/s10549-014-2876-z [DOI] [PubMed] [Google Scholar]
- 33.Sharma P, López-Tarruella S, García-Saenz JA, Ward C, Connor CS, Gómez HL, Prat A, Moreno F, Jerez-Gilarranz Y, Barnadas A, Picornell AC, Del Monte-Millán M, Gonzalez-Rivera M, et al. Efficacy of Neoadjuvant Carboplatin plus Docetaxel in Triple-Negative Breast Cancer: Combined Analysis of Two Cohorts. Clin Cancer Res. 2017; 23:649–57. 10.1158/1078-0432.CCR-16-0162 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Sonnenblick A, de Azambuja E, Azim HA Jr, Piccart M. An update on PARP inhibitors—moving to the adjuvant setting. Nat Rev Clin Oncol. 2015; 12:27–41. 10.1038/nrclinonc.2014.163 [DOI] [PubMed] [Google Scholar]
- 35.Miller K, Wang M, Gralow J, Dickler M, Cobleigh M, Perez EA, Shenkier T, Cella D, Davidson NE. Paclitaxel plus bevacizumab versus paclitaxel alone for metastatic breast cancer. N Engl J Med. 2007; 357:2666–76. 10.1056/NEJMoa072113 [DOI] [PubMed] [Google Scholar]
- 36.Chen H, Lu W, Zhang Y, Zhu X, Zhou J, Chen Y. A Bayesian network meta-analysis of the efficacy of targeted therapies and chemotherapy for treatment of triple-negative breast cancer. Cancer Med. 2019; 8:383–99. 10.1002/cam4.1892 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Ge L, Tang Y, Zhang QN, Tian JH, Wang XH, Pieper D, Pan B, Li L, Ling J, Bing ZT, Yang KH. A network meta-analysis on the efficacy of targeted agents in combination with chemotherapy for treatment of advanced/metastatic triple-negative breast cancer. Oncotarget. 2017; 8:59539–51. 10.18632/oncotarget.19102 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Kimmel DB. Mechanism of action, pharmacokinetic and pharmacodynamic profile, and clinical applications of nitrogen-containing bisphosphonates. J Dent Res. 2007; 86:1022–33. 10.1177/154405910708601102 [DOI] [PubMed] [Google Scholar]
- 39.Jagdev SP, Coleman RE, Shipman CM, Rostami-H A, Croucher PI. The bisphosphonate, zoledronic acid, induces apoptosis of breast cancer cells: evidence for synergy with paclitaxel. Br J Cancer. 2001; 84:1126–34. 10.1054/bjoc.2001.1727 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Kunzmann V, Bauer E, Feurle J, Weissinger F, Tony HP, Wilhelm M. Stimulation of gammadelta T cells by aminobisphosphonates and induction of antiplasma cell activity in multiple myeloma. Blood. 2000; 96:384–92. [PubMed] [Google Scholar]
- 41.Santini D, Vincenzi B, Dicuonzo G, Avvisati G, Massacesi C, Battistoni F, Gavasci M, Rocci L, Tirindelli MC, Altomare V, Tocchini M, Bonsignori M, Tonini G. Zoledronic acid induces significant and long-lasting modifications of circulating angiogenic factors in cancer patients. Clin Cancer Res. 2003; 9:2893–97. [PubMed] [Google Scholar]
- 42.Ottewell PD, Mönkkönen H, Jones M, Lefley DV, Coleman RE, Holen I. Antitumor effects of doxorubicin followed by zoledronic acid in a mouse model of breast cancer. J Natl Cancer Inst. 2008; 100:1167–78. 10.1093/jnci/djn240 [DOI] [PubMed] [Google Scholar]
- 43.Gnant M, Mlineritsch B, Schippinger W, Luschin-Ebengreuth G, Pöstlberger S, Menzel C, Jakesz R, Seifert M, Hubalek M, Bjelic-Radisic V, Samonigg H, Tausch C, Eidtmann H, et al. , and ABCSG-12 Trial Investigators. Endocrine therapy plus zoledronic acid in premenopausal breast cancer. N Engl J Med. 2009; 360:679–91. 10.1056/NEJMoa0806285 [DOI] [PubMed] [Google Scholar]
- 44.Gnant M, Mlineritsch B, Stoeger H, Luschin-Ebengreuth G, Heck D, Menzel C, Jakesz R, Seifert M, Hubalek M, Pristauz G, Bauernhofer T, Eidtmann H, Eiermann W, et al. , and Austrian Breast and Colorectal Cancer Study Group, Vienna, Austria. Adjuvant endocrine therapy plus zoledronic acid in premenopausal women with early-stage breast cancer: 62-month follow-up from the ABCSG-12 randomised trial. Lancet Oncol. 2011; 12:631–41. 10.1016/S1470-2045(11)70122-X [DOI] [PubMed] [Google Scholar]
- 45.Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JP, Clarke M, Devereaux PJ, Kleijnen J, Moher D. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. PLoS Med. 2009; 6:e1000100. 10.1371/journal.pmed.1000100 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Higgins JP, Altman DG, Gøtzsche PC, Jüni P, Moher D, Oxman AD, Savovic J, Schulz KF, Weeks L, Sterne JA, and Cochrane Bias Methods Group, and Cochrane Statistical Methods Group. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ. 2011; 343:d5928. 10.1136/bmj.d5928 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Van Valkenhoef G, Tervonen T, Zwinkels T, De Brock B, Hillege H. ADDIS: A decision support system for evidence-based medicine. Decis Support Syst. 2013; 55:459–75. 10.1016/j.dss.2012.10.005 [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.