Abstract
The dilemma of acute non-traumatic abdominal pathologies in the pediatric population depends on the age of the patients and symptoms. Surgical etiologies in patients younger than 2 years of age include intussusception, pyloric stenosis, malrotation and midgut volvulus. In older patients, considerations become closer to differential etiologies in adults including acute appendicitis. Ultrasound and fluoroscopic examinations remain the mainstay for diagnosis that may even be therapeutic such as contrast/air enemas in intussusception reduction. There is an increasing role for CT in appendicitis and renal colic especially in assessing complications; however, it is less favored because it incurs radiation to the patient. This article summarizes the imaging approach to pediatric patients with acute abdominal pathologies presenting to the emergency department, and how imaging is instrumental in guiding diagnosis and treatment, with emphasis on radiation safety, in the context of providing typical imaging findings of each pathology in this pictorial review.
Keywords: abdominal pain, abdomen, pediatrics, appendicitis, intussusception, malrotation, pyloric stenosis, ovarian torsion, testicular torsion, pediatric emergency, abdominal imaging, ultrasound, computed tomography, radiograph
PICTORIAL REVIEW
Introduction
Acute non-traumatic abdominal pain is a common complaint in pediatric emergency departments. The differential diagnosis of acute abdominal pain depends on the age of the patient [1, 2]. Patients less than 2 years old are particularly a challenge because their symptoms are non-specific and may present with inconsolable crying, fussiness and lethargy. Differential considerations are guided primarily by associated symptoms such as bilious emesis pointing to an upper gastrointestinal obstruction, or currant jelly stool pointing to a lower gastrointestinal pathology, namely intussusception [3]. Most common etiologies of abdominal pain in this age group include the non-surgical causes such as gastroenteritis, constipation, and urinary tract infection. Etiologies needing prompt treatment or surgical exploration include incarcerated hernia, intussusception, pyloric stenosis, malrotation, and midgut volvulus [3, 4]. Appendicitis is low on the differential in this age group.
In preschool children between 2 and 5 years old, patients may be able to describe the type and location of abdominal pain. Surgical causes of abdominal pain in this age group include acute appendicitis, intussusception, and intestinal malrotation/volvulus [1, 5]. Less common etiologies include hepatitis, hemolytic anemia, rash or arthritis (Henoch-Schonlein purpura). Chronic constipation starts to increase in frequency in this age group. Extra-abdominal symptoms such as productive cough and pyrexia may be attributed to lobar pneumonia, which is an important differential diagnosis in patients with abdominal pain.
In patients 5 to 12 years old, intussusception and volvulus are less likely. Differential considerations in patients older than 12 years old become closer to those of abdominal pain in young adults, which include appendicitis, gastroenteritis, testicular/ovarian torsion, and gynecological conditions in female patients [1, 6–8]. The gynecological differential includes dysmenorrhea, ectopic pregnancy, threatened abortion, and ectopic pregnancy [1,2].
Main Text
There are multiple imaging modalities available to evaluate acute abdominal pain in pediatric patients. Abdominal radiographs are most often the initial assessment modality, although they are seldom specific. In infancy and early childhood, supine and left decubitus projections of the abdomen should be obtained, while supine and upright projections are required in older age groups. Ultrasound (US) and upper gastrointestinal contrast examinations are guided by the diagnostic considerations based on symptoms and patient age. Computed tomography examinations are less desirable in the pediatric population and are usually used as a last resort given the radiation dose incurred on the patient.
Intussusception
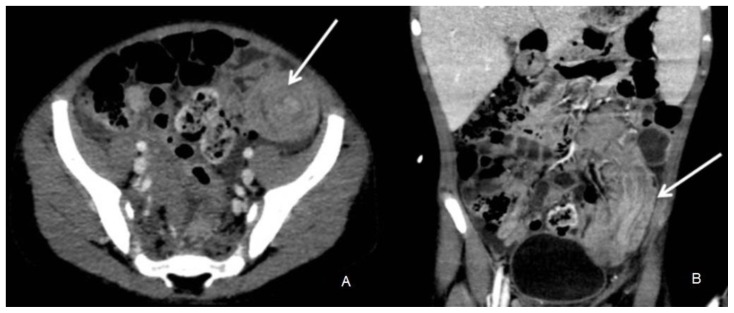
Intussusception is the most common abdominal emergency in early childhood, with a predilection for ages 9 to 24 months. Intussusception is an invagination of a proximal portion of the intestine into an adjacent distal segment. The most common type is ileo-colic invagination and it is more common in males. It is the second most common cause of intestinal obstruction in infants. Intussusception is seen most frequently between 3 months and 5 years of age with over 60% occurring in the first year of life. In infants, a pathologic lead point is found in less than 5–10% of cases. In older children 5 to 12 years of age, a pathologic lead point is more common and an attempt to find the underlying etiology should be made on ultrasound or CT, including Meckel’s diverticulum, submucosal hemorrhage from Henoch-Schonlein purpura (HSP), or lymphoma (Figure 1a &b) [3,9]. Other risk factors include viral gastroenteritis, rotavirus vaccination, polyps, duplication cysts, cystic fibrosis, celiac, and Crohn’s disease. The classic triad of intussusception is found in 20–40% of cases and includes intermittent colicky abdominal pain, vomiting, and currant jelly (bloody mucous) stool. However, at least two of these findings are seen in 60% of patients. Other clinical signs and symptoms include lethargy and abdominal mass [3].
Figure 1.
6 year old boy being evaluated for Burkitt lymphoma was found to have a distal ileal intussusception.
Findings: CT demonstrates an intussusception in axial and coronal reformatted images (arrow) with invagination of proximal bowel into distal bowel loops.
Technique: Axial contrast enhanced CT abdomen and pelvis in venous phase with coronal reformats. 120 KV, 180 mAs, 1.5 mm slice thickness, 10 ml optiray 300 IV contrast.
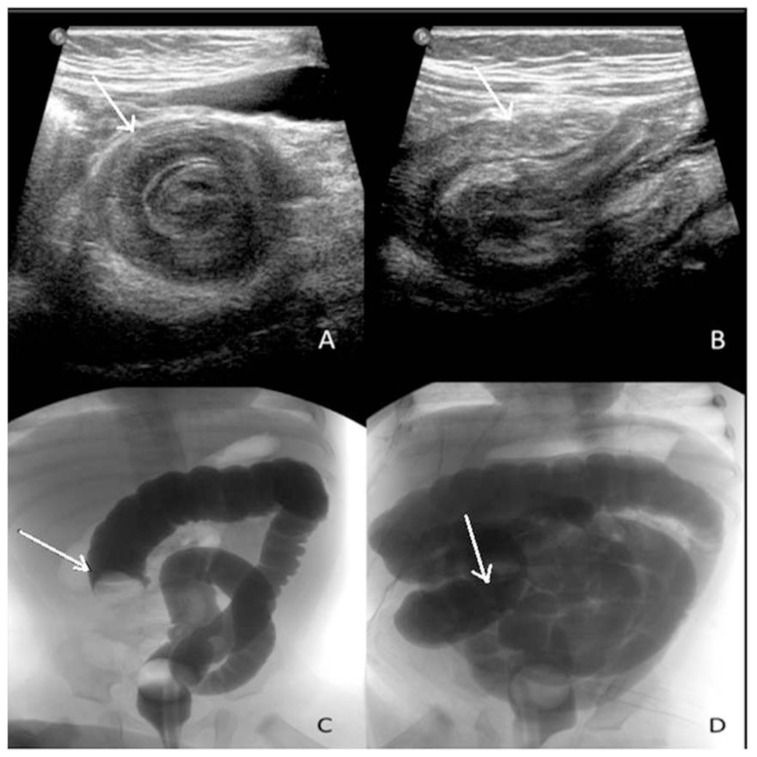
Abdominal radiographs are the initial study in children with possible intussusception. They are neither sensitive nor specific. Abnormal findings may include an abdominal mass, air-fluid levels, and dilated loops of small intestine. Abdominal radiographs are important to exclude free air suggesting perforation. The imaging modality of choice in suspected intussusception is ultrasound which is highly sensitive and specific in detecting intussusception [3]. Imaging findings on ultrasound include the “target sign”, a single hypoechoic ring with a hyperechoic center, and the ‘pseudokidney” sign which is superimposition of hypo- and hyperechoic areas representing the edematous walls of the intussusceptum (the part that prolapses into the other, while the receiving part is referred to as intussuscipiens) and layers of compressed mucosa, (Figure 2a & b) [3].
Figure 2.
5 month old boy presented to the emergency department with colicky abdominal pain, vomiting and diarrhea, found to have intussusception.
Findings: (A) Ultrasound demonstrates a target sign with a hypoechoic ring and a hyperechoic center on transverse view. (B) On the longitudinal US view, a pseudokidney sign with superimposed hypo- and hyperechoic areas representing the edematous walls of the intussusceptum and layers of compressed mucosa is observed. After confirming the lack of free air on the scout abdominal view (not shown), water soluble contrast enema (C) demonstrates a mass prolapsing in the lumen visualized as a convex shaped filling defect (arrow) that progressively reduced until contrast refluxed into the small bowels (D) with the arrow pointing to the cecum and ileocecal valve region.
Technique: (A+B) Real time ultrasound images of the right lower quadrant using 12 mHz linear probe. (C+D) Foley catheter placed in the rectum with inflation of the balloon, then, pulsed fluoroscopy following the instillation of water soluble gastrografin contrast solution.
Gastrografin water soluble enema is the gold standard for diagnosis of intussusception and is also the initial non-invasive therapeutic option (Figure 2c & d). Air contrast enema is an effective alternative avoiding the risk of chemical peritonitis caused by perforation with gastrografin enema. The final alternative is surgical reduction in cases whenever enema examinations are contraindicated such as in cases of prolonged symptoms (>24 hours), perforation, intestinal ischemia, and hypovolemic shock.
After a successful reduction by means of enema the child should be admitted for observation, because within 24 hours post reduction there is a 0.5–15% risk of recurrent intussusception. Nevertheless, recurrence may occur days or weeks later. Even after reduction by laparotomy, the recurrence rate is 2–5 % [4, 9–10].
Pyloric stenosis
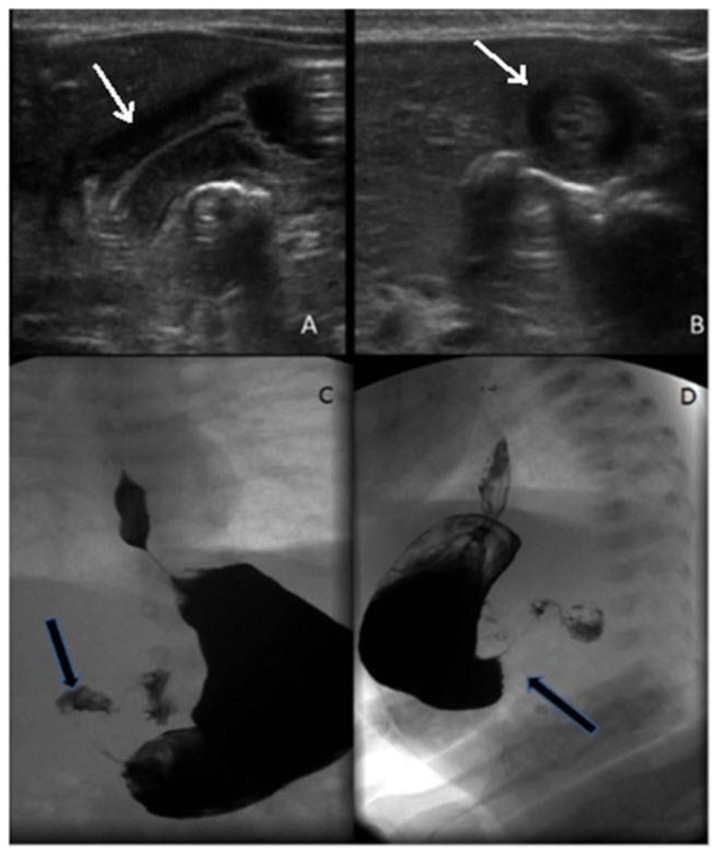
Pyloric stenosis is an idiopathic thickening of the pyloric muscle that causes gastric outlet obstruction with projectile non-bilious emesis. It usually occurs in early infancy between first weeks of life up to 6 months of age. There is a predilection in first-born males with a male to female ratio of 4:1. In addition, there is an increased risk with a similar history in a first degree relative [4, 11]. Other risk factors include preterm birth, maternal smoking, and maternal erythromycin and azithromycin use. The initial imaging modality of choice is an ultrasound examination which demonstrates thickening of more than 3 mm of a single muscle wall on a transverse image and a length of more than 15 mm on a longitudinal image (Figure 3a & b) [4,11]. However, the longitudinal measurement is less reliable than the pyloric thickness. It is important to look at the superior mesenteric artery (SMA) /superior mesenteric vein (SMV) orientation as an indirect sign of malrotation, which is in the differential diagnosis of an infant with vomiting. Dynamic visualization of gastric contents passing through the pylorus is important since opening of the pylorus nearly excludes pyloric stenosis. This is particularly important when measurements are borderline (2–3 mm) such as in pylorospasm [4]. Placing the patient in a right side down oblique position, possibly with the help of sugar water, is also helpful in providing an acoustic window and distending the antropyloric region.
Figure 3.
1 month old boy with recurrent vomiting found to have pyloric stenosis.
Findings: (A) In the longitudinal ultrasound view, there is an elongated pyloric canal (2 cm). (B) In the axial view, we observe a thickened pyloric muscle (0.5 cm single muscle wall). Upper gastrointestinal contrast examination, frontal (C) and right lateral oblique views (D) demonstrating a narrow elongated canal lumen (string-sign) (arrow) and an indentation on the duodenal bulb (arrow).
Technique: (A+B) Real time ultrasound images of the pylorus using 12 mHz linear probe. (C+D) Pulsed fluoroscopy following the ingestion of water soluble omnipaque oral contrast solution.
The diagnosis can also be confirmed with a fluoroscopic upper gastrointestinal study; however, this incurs a radiation dose to the patient. On an upper gastrointestinal study, the pylorus appears elongated with a narrow lumen and an indentation on the duodenal bulb (Figure 3c & d). Although the upper gastrointestinal series is associated with a radiation dose to the patient, it is helpful in assessing for other etiologies of vomiting in a young infant such as malrotation/volvulus and gastroesophageal reflux. After stabilizing the patient, the treatment is surgical pyloromyotomy, which has very low morbidity and a short hospital stay.
Pyloric thickening may be seen in pyloric spasm; however, the thickness does not usually exceed 3 mm. It is important to wait and observe for pyloric opening in these patients, and obtain a follow-up examination when thickened wall measurements are borderline [4].
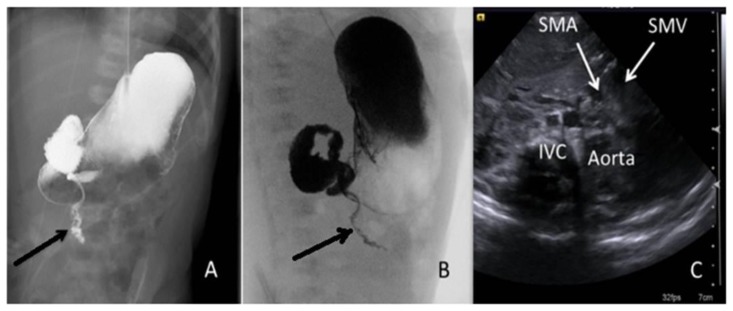
Intestinal malrotation / midgut volvulus
Intestinal malrotation can be either symptomatic or asymptomatic. It is a result of abnormal rotation of intestine in utero and has been linked to congenital diaphragmatic hernia, congenital heart disease, omphalocele, gastroschisis, esophageal atresia. This abnormality predisposes to midgut volvulus which is a surgical emergency. Midgut volvulus commonly presents in infancy with bilious vomiting. Although ultrasound may demonstrate an abnormal reversed rotation of the SMA/SMV orientation, the gold standard for suspected midgut volvulus is an upper gastrointestinal series [12, 13]. The duodenal sweep is normally a retroperitoneal structure where contrast should be seen progressing posteriorly on a lateral projection and the duodenojejunal junction in the left upper quadrant to the left of the spine on an anteroposterior projection. In malrotation, the duodenojejunal junction does not cross the midline. In the case of a midgut volvulus, the proximal jejunum remains inferior to the duodenum on the right side of the abdomen with a corkscrew appearance (Figure 4). There is no value to performing a contrast enema in patients with suspected malrotation because a normal position of the cecum does not exclude the diagnosis [12, 13]. The treatment is surgical correction (Ladd procedure) because of the risk of bowel ischemia. The presence of volvulus is associated with high mortality. Symptoms resolve with surgery but high mortality rate remains after due to associated complications such as sepsis and short bowel syndrome.
Figure 4.
2 week old baby girl presenting with vomiting due to intestinal malrotation.
Findings: Antero-posterior (A) and right anterior oblique (B) projections showing the proximal jejunum remaining inferior to the duodenum on the right side of the abdomen with a corkscrew appearance (arrow) and the duodenojejunal junction does not cross the midline to its normal location in the left upper quadrant. (C) Ultrasound image showing reversed SMV (superior mesenteric vein) (to the left) of the SMA (superior mesenteric artery) as annotated (arrows).
Technique: (A+B) Pulsed fluoroscopy following the ingestion of water soluble omnipaque oral contrast solution. (C) Real time ultrasound images of the pylorus using 8 mHz curvilinear probe.
Acute appendicitis
Acute appendicitis should always be considered in patients with right lower quadrant tenderness, particularly those with persistent pain associated with fever and leukocytosis. The findings on radiographs are non-specific and almost never diagnostic. The most specific finding of an abdominal plain film is the presence of a calcified appendicolith (Figure 5); however, this is only present in less than 10% of patients [14, 15]. Other findings on radiographs include localized bowel ileus and obliteration of the psoas shadow.
Figure 5.
12 year old boy with right lower quadrant pain due to appendicitis.
Findings: Scout view from the CT scan showing the presence of an appendicolith (arrow).
Technique: Axial contrast enhanced CT of the abdomen and pelvis. 120 KV, 160 mAs, 1.5 mm slice thickness.
Ultrasound plays an increasing important role in the prompt and accurate diagnosis of acute appendicitis in children. The principle diagnostic imaging test especially in pediatric patients includes graded-compression US. An inflamed appendix is usually aperistaltic, difficult to compress and measures ≥ 6 mm in diameter. It is important for ultrasound performers to visualize the entire appendix to avoid a false-negative reading because sometimes only the distal tip of the appendix is inflamed. A peri-appendiceal fluid accumulation may indicate an early perforation but may simply result from inflammation. Finally, ultrasound can assess for the presence of an associated abscess (Figure 6).
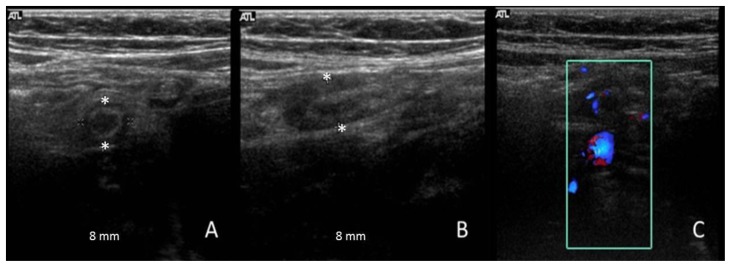
Figure 6.
16 year old girl with right lower quadrant pain due to appendicitis.
Findings: Ultrasound of the appendix demonstrates an enlarged appendix, thickened wall and peri-appendiceal echogenicity in keeping with inflammation in axial and longitudinal sections (A,B), and increased flow on color examination (C). There was no associated fluid or abscess.
Technique: real time ultrasound images of the right lower quadrant appendix using 12 mHz linear probe.
The principal advantages of graded-compression US are low cost, lack of ionizing radiation, and ability to delineate gynecological disease such as ruptured ovarian cysts and ovarian torsion. An important limitation is that of its diagnostic accuracy which is highly dependent on the skill of operators, as evidenced by the great variability in its reported diagnostic sensitivity and specificity for this condition. The reported sensitivity of US in children has ranged from 44% to 94% and the specificity has ranged from 47% to 95% [6].
CT has become the test of choice for surgeons when ultrasonography fails to give a definitive diagnosis. The CT examination is performed with IV contrast, which is sufficient for patients older than 6 years of age. Due to the paucity of fat in patients less than 6 years old, oral contrast is added in order to enhance the ability to visualize the appendix. Although some authors advocate the use of rectal contrast, it is significantly invasive for a pediatric patient. In addition, distending the colon can cause significant compression and suboptimal visualization of the appendix. CT is particularly useful in assessing complications when they are suspected such as defining the extent of abscess formation. The reported sensitivity of CT for the diagnosis of acute appendicitis in children has ranged from 87% to 100% and the specificity has ranged from 89% to 98% [5, 16]. Direct signs on CT include an enlarged appendix (> 7-mm transverse diameter), a non contrast opacified appendiceal lumen and significant wall enhancement with intravenous contrast material administration. Secondary signs of acute appendicitis include peri-appendiceal fat stranding, free fluid in the right lower quadrant of the abdomen or pelvis, and focal cecal wall thickening adjacent to an inflamed appendix. CT has dramatically improved our ability to detect appendicitis and its complications. It has led to improved patient outcomes and decreased the number of unnecessary surgeries (Figure 7).
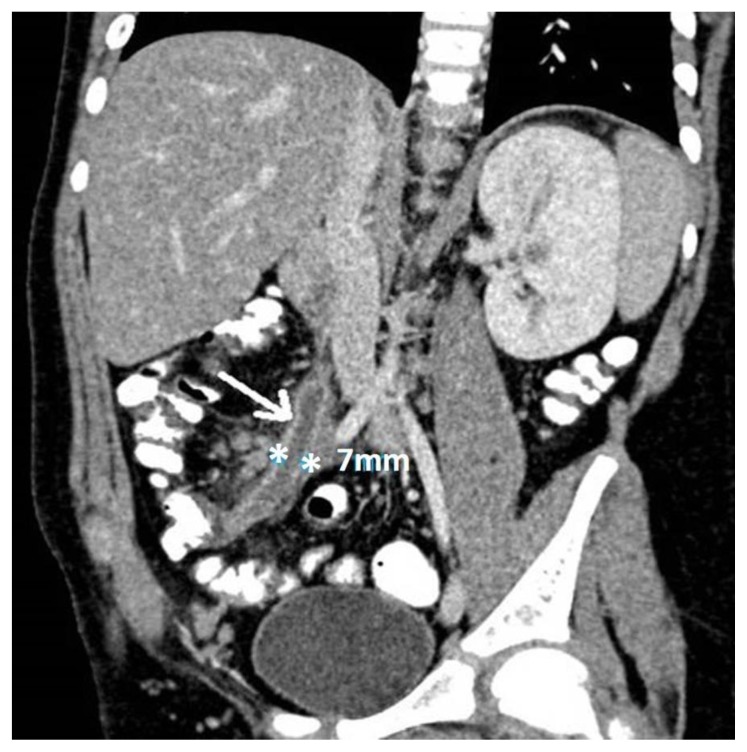
Figure 7.
8 year old male with 2 day history of fever and right lower quadrant pain, found to have appendicitis.
Findings: CT in appendicitis demonstrates an enlarged appendix measuring 7 mm with thickened enhancing wall and peri-appendiceal fat stranding (arrow).
Technique: Axial contrast enhanced CT abdomen and pelvis in venous phase with coronal reformats. 120 KV, 172 mAs, 4 mm slice thickness, 35 ml optiray 300 IV contrast.
Magnetic resonance imaging has a high diagnostic accuracy in diagnosing appendicitis in children; it has a sensitivity and specificity of 97.6% and 99%, respectively. However, it’s not always practical in such emergency situations due to the lengthy scan time needed. Moreover, MRI may not always be available [17, 18]. The scan time limitation of MRI inspired the innovation of the ultrafast 3-T MRI. Johnson et al. conducted a study which evaluated its accuracy in detecting appendicitis in the pediatric population (4–17 years). Scan time was in its favor for it took less than 8 mins 45 secs (median of 5 mins 40 seconds). Furthermore, ultrafast 3-T MRI had a sensitivity and specificity of 100% and 99%, respectively. This lays down a promising prospect for the usage of MRI in emergent situations [19].
When the diagnosis of appendicitis is made, preparing the child for the operating room is essential. If there are clinical or radiological signs of perforation, antibiotics with gram negative and anaerobic coverage should be started in the emergency department.
Torsion
Testicular pain is a common complaint of adolescent boys presenting to the emergency department. Ultrasound examination, using a high frequency ultrasound probe, is the only needed modality in these patients’ assessment. The most critical surgical emergency is identifying patients who have testicular torsion. However, ultrasound is also helpful in identifying other causes of testicular pain including epididymitis, epididymo-orchitis, and testicular appendage torsion, all of which will proceed to medical treatment. Testicular torsion in the adolescent is usually an intravaginal torsion where there is free rotation of the testicle and spermatic cord in the tunica vaginalis [20]. In testicular torsion, the affected testicle may be enlarged with diminished (incomplete torsion) or absent (complete torsion) flow on color Doppler examination. Heterogeneity in the echotexture indicates necrosis, which signifies a delayed presentation, and thus indicates the need for urgent surgical intervention [7]. The most specific sign is identifying a twisted spermatic cord (Whirlpool sign), which can also be accentuated by color imaging (Figures 8 and 9). Less frequently younger patients including neonates might present to the emergency department with pain, irritability, scrotal swelling, and/or discoloration [20]. Neonates usually present with extra-vaginal torsion where both the contents of the tunica and the tunica itself rotate [20].
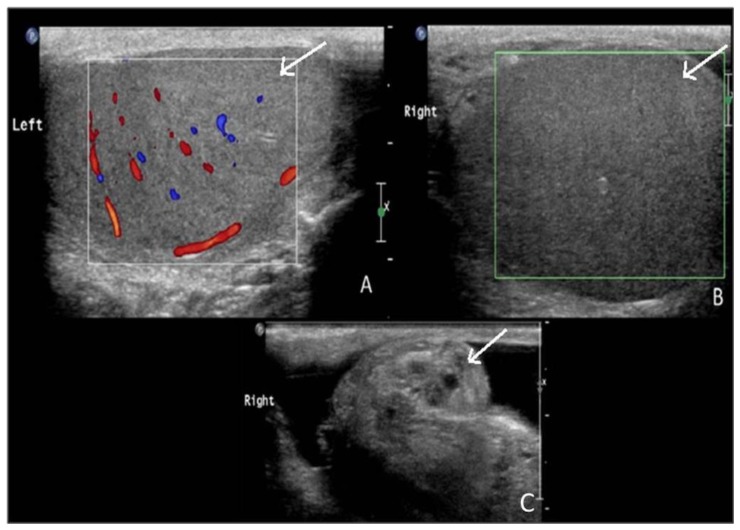
Figure 8.
14 year old male with right testicular pain due to testicular torsion.
Findings: The left testicle (A) shows a normal size with normal echogenicity and color flow. On the right, the testicle is enlarged with diminished echogenicity and no color flow (B). Evaluation of the spermatic cord demonstrates a twisted cord “whirlpool sign”, a highly specific sign (C).
Technique: real time ultrasound images of the testicles using 12 mHz linear probe.
Figure 9.
15 year old boy with left sided testicular pain due to partial testicular torsion.
Findings: Color flow was applied to the twisted pedicle to show the “whirlpool” sign (arrow) as demonstrated in this patient with a partial torsion of the left testicle.
Technique: real time ultrasound images of the testicles using 12 mHz linear probe.
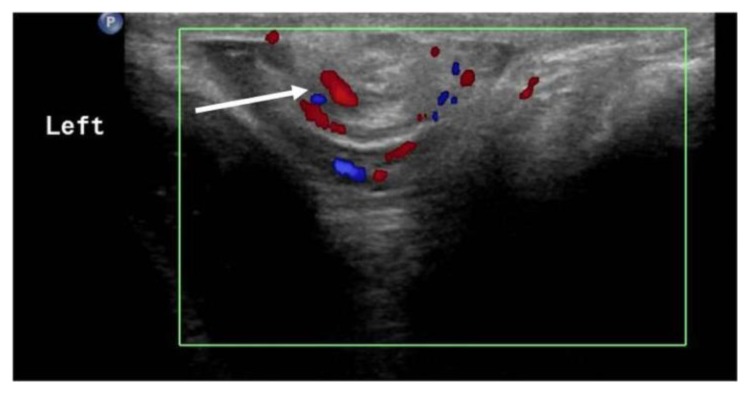
Ovarian torsion should be considered in a female patient with lower quadrant / pelvic pain. It is a major differential diagnosis in adolescent females with right lower quadrant pain. A similar predisposing cause of ovarian torsion in the pediatric population as in adults is an ovarian mass (benign or malignant). However, in the pediatric population, torsion of a normal ovary is more common due to hypermobility or associated developmental abnormalities of the fallopian tube. Ultrasound will demonstrate an enlarged edematous ovary with peripheral displacement of the follicles (Figure 10a). The presence of a twisted vascular pedicle is not often seen, however, it is a highly specific sign (figure 11) [8]. The absence of flow on Doppler suggests infarction, whereas its presence implies that the ovary is still viable. The presence of flow does not exclude torsion, since arterial flow might still be present, while venous flow is absent. In cases when ultrasound is not conclusive, MRI can be performed to assess for stromal edema and hemorrhagic infarcts (Figure 10c). CT scan is not routinely used for ovarian torsion; however, it might be seen in patients imaged for other causes of abdominal pain, mostly for suspected acute appendicitis (Figure 10b) [21, 22].
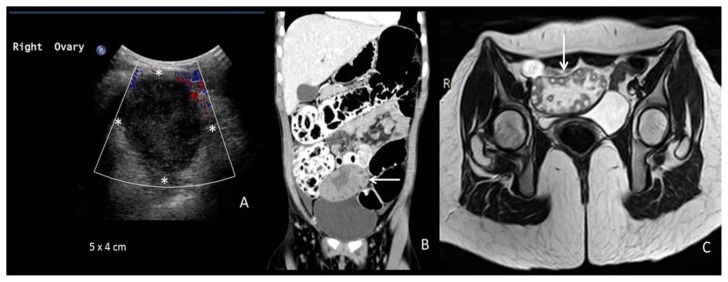
Figure 10.
8 year old female with right lower quadrant pain due to ovarian torsion.
Findings: Ultrasound (A) demonstrating an enlarged ovary with hypoechoic edematous stroma and peripheral displacement of the follicles. Although not typically performed in evaluation for ovarian torsion, the patient was imaged with an enhanced CT examination for suspected appendicitis. CT (B) demonstrates an enlarged enhancing ovary with peripheral displacement of the follicles and central necrosis (arrow) (B). MRI (C) reveals enlargement of the right ovary (arrow) with peripherally displaced follicles.
Technique: (A) Real time ultrasound images of the right ovary using 5 mHz curvilinear probe. (B) Axial contrast enhanced CT abdomen and pelvis in venous phase with coronal reformats. 120 KV, 201 mAs, 4 mm slice thickness, 35 ml optiray 300 IV contrast. (C) Axial T2-weighted MRI (1.5 Tesla) image (TR=3500, TE=90) of the pelvis.
Figure 11.
16 year old girl presenting with right lower quadrant pain found to have ovarian torsion.
Findings: MRI showing the right ovary located slightly superior to the left ovary. It is enlarged and edematous (lower arrow). There is a twisted pedicle located above the ovary (upper arrow).
Technique: Coronal T2-weighted MRI (1.5 Tesla) image (TR=860, TE=80) of the pelvis.
Renal colic
Although renal colic is uncommon in the pediatric population, there is an increase in pediatric emergency visits [23]. Metabolic derangements should be considered in pediatric patients with renal colic. As such, these patients need to be worked up for possible causes that will cause recurrent urolithiasis [24]. Risk factors include congenital/structural abnormalities, infection, metabolic disease, dehydration, immobilization, and medications. Abdominal plain radiographs might demonstrate radio-opaque renal stones but it has a sensitivity of less than 20% (Figure 12a) [25]. Intravenous urography is rarely used and has largely been replaced by non-contrast CT because of its inferior accuracy [24]. Due to its high sensitivity and specificity, the gold standard for identification of renal colic is non-enhanced CT scan. Nevertheless, in an attempt to lower both radiation risk and cost, ultrasound can be performed to provide information on the presence of the stone and associated obstruction (Figure 12b & c). Ultrasound findings include hydronephrosis, the “twinkle artifact”, identification of the stone due to its posterior shadowing, and absence of ureteral jets [24]. Ultrasound is particularly helpful in identifying ureteropelvic and ureterovesical junction stones; however, it remains limited in its ability to assess ureteral stones because of the technical challenge in assessing the retroperitoneal region. Treatment ranges from supportive care, treatment of underlying abnormalities, medical expulsive therapy, and urologic intervention, with generally good prognosis.
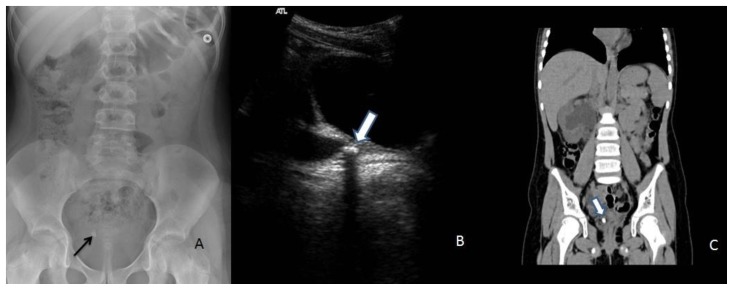
Figure 12.
9 year old girl with ureteral stone.
Findings: Abdominal radiograph (A) demonstrates a right pelvic stone (arrow).
The following two images are for the sister of the girl presented in (A). Ultrasound (B) demonstrating an echogenic focus with posterior shadowing (arrow) in the distal right ureter, with an associated dilated proximal ureter (arrowhead). On the non-enhanced CT (C) this corresponds to the calcific density in the distal ureter (arrow).
Technique: (A) Supine abdomen 80 KV, 120 mAs. (B) Real time ultrasound images of the pelvis using 5 mHz curvilinear probe. (C) Axial non-enhanced CT abdomen and pelvis with coronal reformats. 120 KV, 180 mAs, 1.5 mm slice thickness.
Ingestion injury and Foreign body ingestion
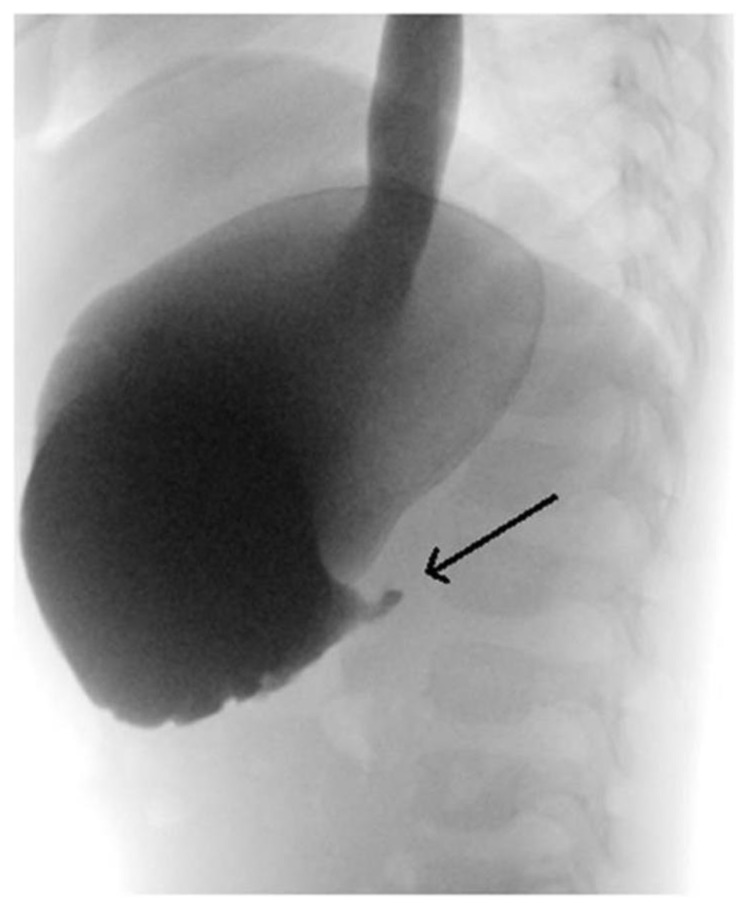
Ingestion of corrosive substances remains a cause of emergency referrals particularly in under-developed countries. The kind of injury to the upper gastrointestinal tract depends on the amount and type of substance ingested, (acid or alkali) [26]. In addition, the time of presentation since ingestion is imperative. Plain upright chest radiography is helpful in demonstrating free air in the mediastinum suggesting esophageal perforation, or under the diaphragm signifying a gastric perforation [26]. Upper gastrointestinal series can help assess the site and the extent of injury. In case of suspected perforation, a water-soluble contrast medium is better used than barium, with the understanding that both may be irritating [26]. The depth of injury caused at the level of the stomach is usually more severe with alkali substances when compared to acids (Figure 13). Moreover, alkali injuries tend to involve the esophagus, penetrate deeper and are more systemic [26]. CT scan has the advantage of being less invasive than endoscopy with better evaluation of transmural damage and necrosis. Endoscopy is safely performed up to 96 hours after the injury; however, it becomes more hazardous later during the healing period where tissues are more friable [26].
Figure 13.
3 year old male who presented with intractable vomiting after ingesting acidic solution from a car battery.
Findings: There is a stricture at the pylorus with complete gastric outlet obstruction with no passage of contrast beyond the pyloric stricture. The patient went on to surgery for pyloroplasty.
Technique: pulsed fluoroscopy following the ingestion of water soluble omnipaque oral contrast solution.
Foreign body ingestion is a common presenting problem of young children to the emergency room, mostly occurring in children between 6 months and 5 years. Foreign body ingestion is often suggested from the history. If unwitnessed, children may present with unknown cause of difficulty swallowing. The most commonly ingested foreign bodies are coins. Since most foreign bodies are radio-opaque, a plain radiograph of the neck, chest and abdomen is the modality of choice to determine the nature, location, and the presence of possible complications such as perforation [27]. Concerning the location in the chest, a coin in the trachea would appear in its sagittal plane (linear) on anteroposterior radiographs, while a coin in the esophagus would have a coronal orientation (round). Foreign bodies in the trachea should be promptly removed. In addition, esophageal foreign bodies should be removed if they do not pass within 24 hours.
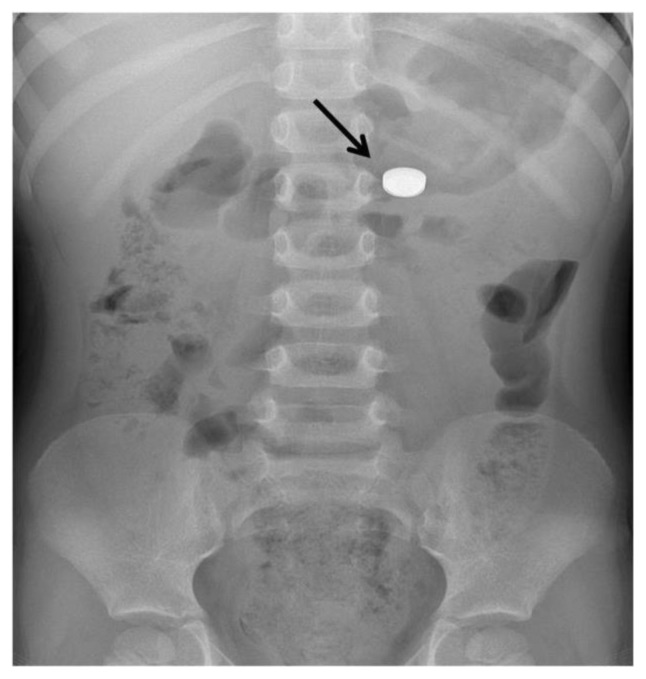
Batteries are a commonly ingested foreign body in children. The appearance on radiography is characteristic with a “double ring” appearance on frontal views and a beveled edge on lateral projections. These characteristics make it easy to differentiate it from coins (figure 14). Battery ingestion poses a risk of perforation and burns and need to be removed within two hours if they are noted in the esophagus.
Figure 14.
3 year old female presenting after ingesting a disc battery.
Findings: The disc battery (arrow) is seen in the stomach showing a “double ring” appearance.
Technique: supine abdomen 80 KV, 120 mAs.
Once in the stomach, most foreign bodies will usually pass spontaneously. Monitoring for passage of the foreign body can be performed clinically and / or with radiography. Patients and parents are instructed about signs of perforation and obstruction. Foreign bodies that do not pass the pylorus after 48 hours, or patients who show signs of peritonitis will require prompt endoscopic or surgical removal [28].
In conclusion, the differential considerations of acute non-traumatic abdominal pain in the pediatric patients presenting to the emergency department depends on the age of the patient and the associated symptoms. The choice of the imaging modality is highly dependent on the suspected etiology. Ultrasound plays a pivotal role in assessing these patients because it allows real-time imaging assessment and does not involve ionizing radiation. Fluoroscopic guided gastrointestinal examinations can be both diagnostic and therapeutic in cases such as intussusception reduction. CT should be the last resort in equivocal findings on ultrasound due to the associated radiation dose. MRI, although highly sensitive in detecting many pathologies, is of little use in emergency situations due to prolonged imaging time, which, if improved, has promising future implications.
TEACHING POINT
The most common non-traumatic causes of acute pediatric abdominal pain include intussusception, pyloric stenosis, midgut volvulus/intestinal malrotation, acute appendicitis, ovarian/testicular torsion, and renal colic. It is of crucial importance for physicians to be aware of the unique radiological findings of each entity.
Table 1.
Summary table of most common etiologies of acute non-traumatic abdominal pain in pediatric population.
| Etiology | Demographics | Risk Factors | Treatment | Prognosis | Imaging Findings |
|---|---|---|---|---|---|
| Intussusception | Estimated incidence 74 per 100,000 with M:F ratio3:2. Most common at 9–24 months | Viral gastroenteritis, rotavirus vaccine, Meckel diverticulum, duplication cysts, lymphomas, HSP, cystic fibrosis, celiac, Crohn disease. | Hydrostatic or pneumatic reduction, surgery for complicated cases. | Excellent with early diagnosis and treatment. May recur. | “target” and “pseudo-kidney” signs on US |
| Pyloric Stenosis | Around 2 to 3.5 per 1000 with male predominance (M:F 4:1 to 6:1). Rarely after 12 weeks of age | Preterm birth, maternal smoking, family history, maternal erythromycin and azithromycin use. | Pyloromyotomy | Excellent with early diagnosis and treatment. | Pyloric muscle thickness >3mm on US |
| Intestinal malrotation / midgut volvulus | 1 in 6000 live births. Estimated M:F 2:1 in neonates. Most before 1 year of age | Congenital diaphragmatic hernia, Congenital heart disease, Omphalocele, Gastroschisis, Esophageal atresia. | Surgical(Ladd procedure) | High mortality in volvulus. | Corkscrew appearance on upper GI series. |
| Acute Appendicitis | Incidence 19 to 28 per 10,000 children younger than 14. Slight male predominance and in second decade of life. | Nonspecific obstruction of the appendiceal lumen, lymphoid hyperplasia | Appendectomy | Excellent with surgery. | enlarged appendix, non-opacified lumen and significant contrast enhancement on CT |
| Testicular Torsion | 1 in 4000 males. Peaks in neonatal period and puberty. | Previous torsion, family history of torsion. | Orchiopexy if viable. Orchiectomy if nonviable testis. | Detorsion within 6 hrs –viable. Nonviable after 24 hrs. | Enlarged testicle with diminished flow on US. Whirlpool sign. |
| Ovarian Torsion | Estimated at 4.9 per 100,000 females. Most commonly at onset of reproductive age. |
Ovarian cysts, masses, prior torsion, strenuous exercise. | Surgical Detorsion | Prompt treatment may prevent irreversible ischemic damage | Enlarged edematous ovary with peripheral displacement of follicles. Twisted vascular pedicle. Diminished /absent blood flow on US |
| Renal Stones | Estimated range 36 to 57 per 100,000 children. Boys more commonly affected in 1stdecade, girls in second. Ages 12–17 years. | Congenital/structural abnormalities, infection, metabolic disease, dehydration, immobilization, medications. | Supportive care, treat underlying abnormalities, medical expulsive therapy, urologic intervention | Generally good prognosis. | Stone visualization on US or CT |
Table 2.
Imaging findings of most common etiologies of acute non-traumatic abdominal pain in pediatric population.
| Entity | Plain Radiograph/Fluoroscopy | Ultrasound | Computed Tomography/ Magnetic Resonance Imaging |
|---|---|---|---|
| Intussusception | Plain XR: Abdominal mass, air-fluid levels, and dilated loops of small intestine Gastrografin water enema is gold standard. Air contrast enema is an effective alternative. |
Findings include the “target sign” “pseudokidney” sign | Suboptimal imaging for this condition |
| Pyloric Stenosis | On fluoroscopy, pylorus appears elongated with a narrow lumen and an indentation on the duodenal bulb. | Pyloric thickness >3 mm of single muscle wall (transverse) and length of >15 mm (longitudinal) | Suboptimal imaging for this condition |
| Intestinal malrotation / midgut volvulus | Upper GI is gold standard. In malrotation, the duodenojejunal junction does not cross the midline. In the case of a midgut volvulus, the proximal jejunum remains inferior to the duodenum on the right side of the abdomen with a corkscrew appearance | Abnormal reversed rotation of the SMA/SMV orientation | Suboptimal imaging for this condition |
| Acute Appendicitis | XR: Calcified appendicolith (only in 10%); localized bowel ileus and obliteration of the psoas shadow. | Inflamed appendix is usually aperistaltic, measures ≥ 6 mm Peri-appendiceal fluid or associated abscess. | CT: Enlarged appendix (> 7-mm transverse diameter), non-opacified appendiceal lumen, peri-appendiceal fat stranding, free fluid in right lower quadrant, focal cecal wall thickening. MRI: high diagnostic accuracy but impractical in emergency |
| Testicular Torsion | Suboptimal imaging for this condition | Enlarged testicle with diminished /absent flow. Heterogeneity in echotexture (necrosis) signifies a delayed presentation. “Whirlpool sign” | Suboptimal imaging for this condition |
| Ovarian Torsion | Suboptimal imaging for this condition | Enlarged edematous ovary with peripheral displacement of the follicles, presence of a twisted vascular pedicle. Absence of flow suggests infarction. | In cases when ultrasound is not conclusive, MRI can be performed to assess for stromal edema and hemorrhagic infarcts |
| Nephrolithiasis | XR: Radio-opaque stones but sensitivity less than 20% | Stone visualization, hydronephrosis, the “twinkle artifact”, identification of stone due to its posterior shadowing, and absence of ureteral jet. | Gold standard for identification of renal calculi is non-enhanced CT scan. |
| Ingestion Injury | XR: May show free air in the mediastinum suggesting esophageal perforation, or under the diaphragm signifying a gastric perforation. Upper GI series can help assess the site and the extent of injury |
Suboptimal imaging for this condition | Less invasive than endoscopy with better evaluation of transmural damage and necrosis |
ABBREVIATIONS
- CT
Computed Tomography
- MRI
Magnetic Resonance Imaging
- SMA
Superior Mesenteric Artery
- SMV
Superior Mesenteric Vein
- US
Ultrasound
REFERENCES
- 1.Yang WC, Chen CY, Wu HP. Etiology of non-traumatic acute abdomen in pediatric emergency departments. World J Clin Cases. 2013 Dec;1(9):276–84. doi: 10.12998/wjcc.v1.i9.276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Tseng YC, Lee MS, Chang YJ, Wu HP. Acute Abdomen in Pediatric Patients Admitted to the Pediatric Emergency Department. Pediatr Neonatol. 2008 Aug;49(4):126–34. doi: 10.1016/S1875-9572(08)60027-3. [DOI] [PubMed] [Google Scholar]
- 3.Kuppermann N, O’Dea T, Pinckney L, Hoecker C. Predictors of intussusception in young children. Arch Pediatr Adolesc Med. 2000 Mar;154(3):250–55. doi: 10.1001/archpedi.154.3.250. [DOI] [PubMed] [Google Scholar]
- 4.Costa Dias S, Swinson S, Torrão H, et al. Hypertrophic pyloric stenosis: tips and tricks for ultrasound diagnosis. Insights Imaging. 2012 Jun;3(3):247–50. doi: 10.1007/s13244-012-0168-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rothrock SG, Pagane J. Acute appendicitis in children: emergency department diagnosis and management. Ann Emerg Med. 2000 Jul;36(1):39–51. doi: 10.1067/mem.2000.105658. [DOI] [PubMed] [Google Scholar]
- 6.Callahan MJ, Rodriguez DP, Taylor GA. CT of appendicitis in children. Radiology. 2002 Aug;224(2):325–32. doi: 10.1148/radiol.2242010998. [DOI] [PubMed] [Google Scholar]
- 7.Ritcey BW, Woo M, McInnes MD, Watterson J, Perry JJ. LO014: What ultrasonography characteristics predict surgical intervention for testicular torsion in adults? Can J Emerg Med. 2016 May;18(S1):35. [Google Scholar]
- 8.Lee EJ, Kwon HC, Joo HJ, Suh JH, Fleischer AC. Diagnosis of ovarian torsion with color Doppler sonography: depiction of twisted vascular pedicle. J Ultrasound Med. 1998 Feb;17(2):83–9. doi: 10.7863/jum.1998.17.2.83. [DOI] [PubMed] [Google Scholar]
- 9.Lui KW, Wong HF, Cheung YC, et al. Air enema for diagnosis and reduction of intussusception in children: clinical experience and fluoroscopy time correlation. J Pediatr Surg. 2001 Mar;36(3):479–81. doi: 10.1053/jpsu.2001.21604. [DOI] [PubMed] [Google Scholar]
- 10.Wang G, Liu XG, Zitsman JL. Nonfluoroscopic reduction of intussusception by air enema. World J Surg. 1995 May;19(3):435–38. doi: 10.1007/BF00299184. [DOI] [PubMed] [Google Scholar]
- 11.Blumhagen JD, Maclin L, Krauter D, Rosenbaum DM, Weinberger E. Sonographic diagnosis of hypertrophic pyloric stenosis. AJR Am J Roentgenol. 1988 Jun;150(6):1367–70. doi: 10.2214/ajr.150.6.1367. [DOI] [PubMed] [Google Scholar]
- 12.Long FR, Kramer SS, Markowitz RI, Taylor GE. Radiographic patterns of intestinal malrotation in children. Radiographics. 1996 May;16(3):547–56. doi: 10.1148/radiographics.16.3.8897623. [DOI] [PubMed] [Google Scholar]
- 13.Applegate KE, Anderson JM, Klatte EC. Intestinal malrotation in children: a problem-solving approach to the upper gastrointestinal series. Radiographics. 2006 Sep;26(5):1485–500. doi: 10.1148/rg.265055167. [DOI] [PubMed] [Google Scholar]
- 14.Andersson RE. Meta-analysis of the clinical and laboratory diagnosis of appendicitis. Br J Surg. 2004 Jan;91(1):28–37. doi: 10.1002/bjs.4464. [DOI] [PubMed] [Google Scholar]
- 15.Andersson RE, Hugander A, Ravn H, et al. Repeated clinical and laboratory examinations in patients with an equivocal diagnosis of appendicitis. World J Surg. 2000 Apr;24(4):479–85. doi: 10.1007/s002689910076. [DOI] [PubMed] [Google Scholar]
- 16.Lessin MS, Chan M, Catallozzi M, et al. Selective use of ultrasonography for acute appendicitis in children. Am J Surg. 1999 Mar;177(3):193–96. doi: 10.1016/s0002-9610(99)00002-1. [DOI] [PubMed] [Google Scholar]
- 17.Cogley JR, O’Connor SC, Houshyar R, Dulaimy KA. Emergent pediatric US: what every radiologist should know. Radiographics. 2012 May;32(3):651–65. doi: 10.1148/rg.323115111. [DOI] [PubMed] [Google Scholar]
- 18.Moore MM, Gustas CN, Choudhary AK, et al. MRI for clinically suspected pediatric appendicitis: an implemented program. Pediatr Radiol. 2012 Sep;42(9):1056–63. doi: 10.1007/s00247-012-2412-4. [DOI] [PubMed] [Google Scholar]
- 19.Johnson AK, Filippi CG, Andrews T, et al. Ultrafast 3-T MRI in the evaluation of children with acute lower abdominal pain for the detection of appendicitis. AJR Am J Roentgenol. 2012 Jun;198(6):1424–30. doi: 10.2214/AJR.11.7436. [DOI] [PubMed] [Google Scholar]
- 20.Traubici J, Daneman A, Navarro O, Mohanta A, Garcia C. Testicular torsion in neonates and infants: sonographic features in 30 patients. AJR Am J Roentgenol. 2003 Apr;180(4):1143–5. doi: 10.2214/ajr.180.4.1801143. [DOI] [PubMed] [Google Scholar]
- 21.Kimura I, Togashi K, Kawakami S, Takakura K, Mori T, Konishi NJ. Ovarian torsion: CT and MR imaging appearances. Radiology. 1994 Feb;190(2):337–41. doi: 10.1148/radiology.190.2.8284378. [DOI] [PubMed] [Google Scholar]
- 22.Hiller N, Appelbaum L, Simanovsky N, Lev-Sagi A, Aharoni D, Sella T. CT Features of Adnexal Torsion. AJR Am J Roentgenol. 2007 Jul;189(1):124–9. doi: 10.2214/AJR.06.0073. [DOI] [PubMed] [Google Scholar]
- 23.Kairam N, Allegra JR, Eskin B. Rise in emergency department visits of pediatric patients for renal colic from 1999 to 2008. Pediatr Emerg Care. 2013 Apr;29(4):462–4. doi: 10.1097/PEC.0b013e31828a302b. [DOI] [PubMed] [Google Scholar]
- 24.Kokorowski PJ, Hubert K, Nelson CP. Evaluation of pediatric nephrolithiasis. Indian J Urol. 2010 Oct;26(4):531. doi: 10.4103/0970-1591.74453. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Chan VO, Buckley O, Persaud T, Torreggiani WC. Urolithiasis: how accurate are plain radiographs? Can Assoc Radiol J. 2008 Jun;59(3):131–34. [PubMed] [Google Scholar]
- 26.Contini S, Scarpignato C. Caustic injury of the upper gastrointestinal tract: a comprehensive review. World J Gastroenterol. 2013 Jul;19(25):3918. doi: 10.3748/wjg.v19.i25.3918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Pugmire BS, Lim R, Avery LL. Review of ingested and aspirated foreign bodies in children and their clinical significance for radiologists. Radiographics. 2015 Aug;35(5):1528–38. doi: 10.1148/rg.2015140287. [DOI] [PubMed] [Google Scholar]
- 29.Lee JH. Foreign body ingestion in children. Clin endosc. 2018 Mar;51(2):129. doi: 10.5946/ce.2018.039. [DOI] [PMC free article] [PubMed] [Google Scholar]