Supplemental Digital Content is Available in the Text.
Key Words: HIV, differentiated care, service delivery, quality of care, efficiency
Background:
With the scale-up of antiretroviral treatment, many health facilities in low- and middle-income countries have implemented innovative practices targeted at overcoming operational challenges and delivering efficient quality HIV services. However, many of these practices remain largely unexplored as a means to better reach the global 90-90-90 targets.
Setting:
A study was conducted on selected facilities in districts of country programs supported by The Global Fund to Fight AIDS, Tuberculosis, and Malaria. The aims of the study were to understand how facilities seek to improve the delivery and uptake of HIV services and to examine what innovative practices might be contributing to their success.
Methods:
The study used a qualitative approach through observations, document reviews, and semistructured interviews with site management and clinical staff to identify service delivery innovations in 30 health facilities in Kenya and Uganda.
Results:
Eleven innovative practices were observed along the HIV care cascade. These practices led to improvements in the quality of testing, treatment, and retention across the facilities. Effective human resource and data management processes also enabled the implementation of these innovative practices.
Conclusions:
Many facilities use innovative practices along the HIV care cascade to address bottlenecks and challenges. These have the potential to improve the quality and efficiency of service delivery and support the attainment of the 90-90-90 treatment targets. Replicating these practices would require further implementation research and a mind shift of donors, governments, and implementers from a metric of coverage to a stronger focus on efficiency and impact.
INTRODUCTION
Current Landscape of HIV Programs
Over the past 2 decades, the world has achieved unprecedented gains in controlling the HIV epidemic. Efforts in primary prevention have been augmented by the impact of widespread antiretroviral therapy (ART) on both mortality and transmission.1 Further progress is needed, however, to achieve overall epidemic control and reach the global 90-90-90 targets for all population groups.
In 2016, nearly 26 million (70%) of the 36.7 million people living with HIV knew their HIV status; 19.5 million (77%) of these had access to ART, and 16 million (82%) of those on ART achieved viral suppression. Although, AIDS-related deaths have declined by nearly 50% between 2005 and 2016, the need for HIV services remains high in many low- and middle-income countries, and the coverage and quality of critical services is highly variable.1 The funding needed to implement evidence-based interventions outweighs what is available. Domestic resources have increased, and donor spending for HIV programs in low- and middle-income countries has declined with a reduction of US $1 billion (13%) between 2014 and 2015,2 resulting in limited resources to meet the treatment and prevention goals.
Thus, there is an urgent need to continually look for innovative ways, new ideas, or processes to improve the effectiveness and efficiency of program implementation. Implementing innovative approaches that would improve efficiency of programs could be a key component of greater impact, long-term sustainability, and a critical means toward achieving the 90-90-90 targets.3
Innovations in Service Delivery
Improvements in science and programmatic evidence have enabled many programs and health facilities to develop innovative ways to deliver services more effectively.4 This may be seen in models used to improve access to screening, testing and treatment services, and the delivery and distribution of drugs. For example, some HIV and tuberculosis (TB) programs in sub-Saharan Africa used mobile sites to improve access to both HIV and TB testing.5,6 A variety of mobile sites such as church rooms and trucks have been used to provide screening and testing to populations with limited access to health facilities. In a rural district in Kenya, this model helped to increase testing, reaching more individuals with no previous HIV test (88%) compared with standalone HIV centers (58%).5
Health facilities have used innovative community models to deliver and improve adherence to treatment services. For example, community-based adherence groups created by HIV programs have the potential to reduce the proportion of clients receiving ART lost-to-follow-up (LTFU) in programs.7,8 In a study in South Africa, participation in community-based adherence groups showed approximately two-thirds reduction in the risk of LTFU compared with facility-based care.9
Improvements in service delivery efficiency may also occur through innovation in operational processes. For example, a large ART center in South Africa provided 6-month prescriptions to stable clients through a fast-track system, leading to a significant decline in uncollected drugs and client waiting time, while improving client satisfaction.10
These innovations have the potential to drive significant improvements in health outcomes and lead to increased efficiencies.11 Identifying and replicating practices becomes increasingly important as countries and development partners work together within a shrinking fiscal landscape, to scale-up the growing evidence base of interventions and new technologies.
Study Objective
The aim of this study was to explore the development of innovative service delivery for HIV programs in low- and middle-income countries. Our theory is that well-performing sites often develop innovative processes to address service delivery implementation challenges to improve the efficiency of service delivery. Country program data were used to examine changes in the uptake and delivery of HIV testing and treatment services in 2 countries supported by The Global Fund to Fight AIDS, Tuberculosis, and Malaria. We explored service delivery practices in Kenya and Uganda using semistructured interviews, document reviews, and nonparticipant observation. This article reports on the new ideas and processes introduced to improve health service quality, outcomes, and efficiency.12
METHODS
Study Setting
The study was conducted in a real-life context in which Kenya and Uganda were purposefully selected based on key informant interviews.13 Data collection and reviews occurred between April and July 2015 in 4 different counties in each country.
Sampling Frame
A broad literature review was conducted to identify existing approaches to help inform sampling and to understand the breadth of the area. Pragmatic sampling was applied using key informant interviews to inform the selection of sites. The sample of facilities and interviewees was selected based on verbal consent and accessibility; thus, interview saturation was not reached.14 A study team including M.E., S.A., M.I., J.B., and S.B. made site visits to conduct interviews. Facilities were selected based on key informant interviews with stakeholders, availability of HIV programmatic indicators, level of The Global Fund to Fight AIDS, TB, and Malaria financing of health programs, accessibility, and availability of facility-level data (see Annex 1, Supplemental Digital Content, http://links.lww.com/QAI/B317 for the complete list of facilities).
Document Reviews
Potential innovations in service delivery were identified by reviewing health facility, clinical, and guidance documents from the Ministry of Health (see Annex 2, Supplemental Digital Content, http://links.lww.com/QAI/B317 for HIV programmatic indicators at each site).
Topic Guide Development
Semistructured interviews with experts in HIV service delivery were conducted by the study team. Questions to experts included challenges to quality of HIV programs and observed practices or processes implemented to overcome these challenges. This helped to inform the development of topics for the site interview guide. The questions in the guide focused on service delivery, human resource management, unique practices of site, staff roles and responsibilities, and data collection and use. The interviews were transcribed, and notes were taken. Semistructured interviews were conducted with facility managers on their management and service delivery practices (see Annex 3, Supplemental Digital Content, http://links.lww.com/QAI/B317 for site interview guide).
Recruitment Procedures
Interviews were conducted by a study team and performed with facility managers, medical, and nonmedical staff to better understand and document the observed innovative practices in these facilities. The study group obtained verbal consent to interview experts and medical staff. As this was primarily evaluating in situ services, separate ethical approval aside from verbal consent was not sought. Nonparticipant observation took place in health facilities. Observations were noted from tours of facilities that included observing client flow through sites. Observations of specific stations were conducted to further understand how services were provided to clients.
Analysis
The analyses of this case study were based on observations, interviews, and document analysis. Framework analysis was used to guide the data analysis and categorize recurring themes from the key informant interviews.15 The data were analyzed using Excel, and interventions were categorized based on approaches identified across HIV care cascade from key informant interviews.
RESULTS
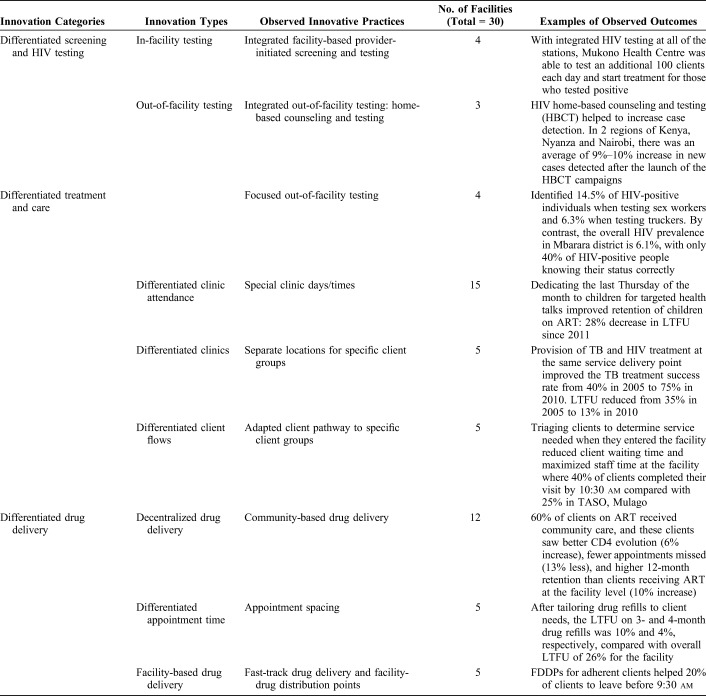
The innovative practices found in facilities can be grouped as either service delivery innovations or innovation enablers. The term “differentiated” is used to signify that the provision of service was not uniform but accounts for variability in client characteristics. Throughout the results, we use the term “clients” to refer to service users or patients. Table 1 shows the breakdown of facilities by type.
TABLE 1.
Types of Facilities in Uganda and Kenya
Service Delivery Innovations
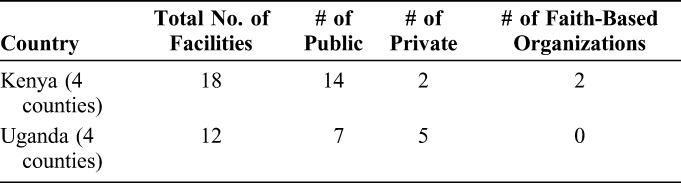
Using the HIV care continuum as a framework,16 the service delivery practices were categorized into 3 levels of differentiated approaches: Differentiated Screening and HIV Testing, Differentiated Treatment and Care, and Differentiated Drug Delivery (Table 2). The innovative models of care seek to increase access and options for HIV testing and treatment by considering variability in clients' characteristics. Table 3 highlights the observed practices and their outcomes. Some of these results contributed to the content outlined in The Global Fund's differentiated care toolkit for health facilities.17
TABLE 2.
Category and Types of Service Delivery Innovations
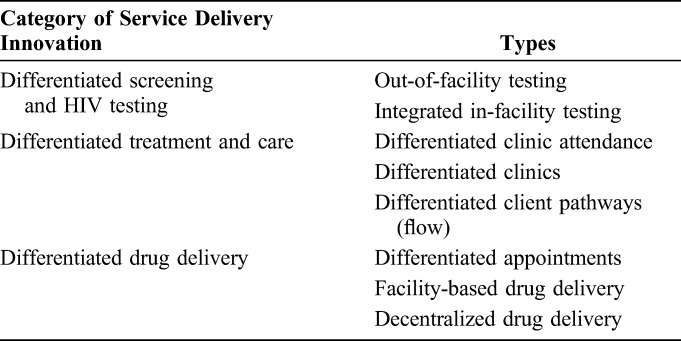
TABLE 3.
Innovative Practices in Service Delivery
Differentiated Screening and HIV Testing
Out-of-facility testing allows for specific high-risk or hard and far-to-reach population groups who would not have visited the facilities to receive HIV testing services. We observed that facilities performing out-of-facility testing used either a focused or an integrated approach. Focused out-of-facility testing brings coverage to underserved populations or specific geographical areas. In the AIDS Support Organization (TASO), Uganda, each TASO site targeted different key populations such as sex workers, fisher folk, and plantation workers at TASO, Entebbe, and truckers at TASO, Jinja. Focusing outreach on key populations allowed providers to identify more people who were HIV positive compared to nonfocused testing of general population. At the TASO, Mbarara, site, the positivity rate was 14.5% in sex workers and 6.3% when testing truckers. By comparison, the overall HIV prevalence in Mbarara district was 6.1%.
Integrated out-of-facility testing such as door-to-door testing is combined with other community health outreach and targets people who cannot easily access facilities for services. In Maseno, Kenya, HIV home-based counseling and testing (HBCT) helped increase HIV case detection. In 2 regions of Kenya, Nyanza and Nairobi, there was an average of 9%–10% increase in new HIV cases detected after the launch of HBCT campaigns.
Integrated in-facility testing joins testing between programs, such as HIV and TB, at multiple service points within the facility. This is referred to as integrated facility-based provider-initiated screening and testing, which was found in facilities with high volume of clients. Nonintegrated testing involves clients moving from one room to the other, such as from the antenatal care clinic to a laboratory, rather than offering services at a single point of care. In Mukono Health Centre (TC) in Uganda, integrated services for HIV, TB, antenatal care, and maternity care were provided. With integrated HIV testing at all of the stations, Mukono Health Centre was able to test an additional 100 clients each day and start treatment for those that tested positive as a “one stop shop” service.
Differentiated Treatment and Care
Differentiating clinic attendance allows for sites to designate special clinic days to specific groups of clients. In 2011, the health center in Riruta, Kenya, began to dedicate the last Thursday of the month for children allowing them to benefit from a child-friendly dedicated space and targeted health talks. Since then, the retention of children on ART has improved, with a 28% decrease in LTFU.
Although some sites allocated special times for different clients, some went further to enhance the clinical space. Differentiated clinics dedicate specific waiting areas or clinic space to specific client groups such as a children's clinic, antenatal clinic, or a TB/HIV clinic, and these may occur simultaneously on the same day. At Kericho district hospital in Kenya, TB and HIV treatment were provided at the same service delivery point. This reduced waiting times for clients and improved TB success rates as well as reduction in LTFU. In 2010, coinfected clients had a TB treatment success rate of 75%, compared with 40% in 2005, the year before services were integrated. LTFU reduced from 35% in 2005 to 13% in 2010.
Differentiated client flow allows for sites to designate specific service pathways for specific groups of clients. The sites set criteria and clinic flow for each client group identified as needing a specific pathway. This was observed in 5 sites in Uganda. At TASO Jinja health center in Uganda, clients were triaged when they entered to determine what services they need: pre-test or post-test counseling, HIV testing, visit to nurse or doctor, and laboratory testing such as CD4 count. By shortening pathways and cutting out unnecessary waits, this reduced client waiting time and maximized the utility of staff time (Fig. 1). In Jinja, 15% of clients had finished in the 1st hour compared with 0% with the median clinic time being 3 hours compared with 4 hours in Mulago.
FIGURE 1.
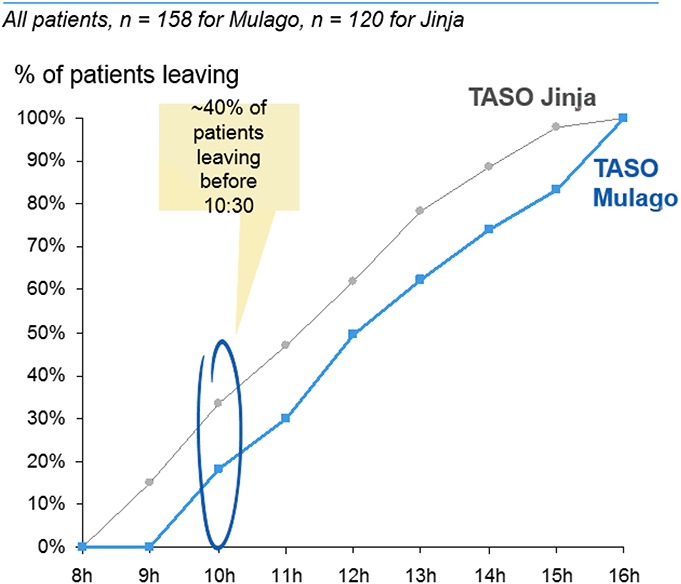
Example of difference in client waiting times in TASO, Jinja and Mulago.
Differentiated Drug Delivery
Provision of differentiated appointment times is an approach that tailors the space between appointment visits to clients' needs. For instance, established and stable HIV clients received the maximum follow-up of 3 months for drug refills or clinical consultations. In Riruta Health Center in Kenya, after tailoring to clients' needs in response to long wait times, the LTFU on 3- and 4-month drug refills was 10% and 4%, respectively, compared with overall LTFU of 26% for the facility.
Facility-based drug delivery was conducted through either fast-track drug refill or drug distribution points. Fast-track drug refill allows for the client to bypass steps in the care pathway. In this case, a stable client with good adherence can go directly to the pharmacy for refills rather than spending additional time in the clinic. At Homa Bay County in Kenya, they offer 6-month clinical appointments and fast-track drug refills every 3 months for stable clients. Of the 1839 clients enrolled, 86% of clients on 6-month refills and 83% on 3-month refills attended their appointments.
Facility-drug distribution points allow for the distribution of drugs to stable clients attending adherence clubs at the facility. These are facilitated by expert clients or peer educators with referrals to doctors, when required. At TASO sites in Uganda, there were facility-drug distribution points for stable clients. Peripheral health facilities such as health posts or dispensaries serve small groups of 10–15 clients, reducing burden on the health facility. At Kombewa hospital in Kenya, clients were referred to lower level facilities, equipped and trained by their staff.
In some communities, drug delivery occurred at community drug distribution points (CDDPs) or community client-led ART delivery (CCLAD) sites. Clients can visit every 2–3 months to pick up medication or have blood samples taken. In TASO Uganda, 60% of their clients on ART received community care, and these clients saw better CD4 evolution (6% increase), fewer appointments missed (13% less), and higher 12-month retention than clients receiving ART at the facility level (10% increase).
With community-based drug delivery by client groups, members of a stable ART group take turns collecting drugs from the clinic or CDDP and deliver them to individuals. In addition, they provide adherence support and monitoring for drug side effects. At TASO sites in Uganda, CCLADs have achieved similar treatment outcomes compared with facility-based models and community-based drug delivery by facility staff. CCLADs and CDDPs have an 88% adherence rate compared with facilities at 89%.
Innovation Enablers
In facilities with differentiated approaches, other distinct management practices were noted. These “enablers” complemented and enforced the differentiated approaches. Three groups of enablers were observed (see Annex 4, Supplemental Digital Content, http://links.lww.com/QAI/B317).
Knowledge Sharing Networks
From field observations and discussions, knowledge-sharing networks, or communities of practice, allowed for sharing of best practices and learnings across different facilities. For example, in Kisumu, Kenya, indicators for linkage to HIV care, prevention of mother-to-child transmission, treatment, pediatrics, and adults are tracked for its 22 facilities with quarterly meetings to discuss and share practices. Mapping performance across facilities identifies opportunities to adapt best practices from one high-performing facility to another with poorer performance.
Effective Data Management
In Kenya, 5 sites measured client-centric indicators, reviewing performance for quality improvement. In Kitebi Health Center in Uganda, clients were categorized into population groups and documented in custom registers, which are used to plan and monitor targeted interventions.
Human Resource Management
Nonmonetary compensation offered in-kind compensation and revenue-generating activities to employees. In Coptic, Kenya, regular staff meetings, feedback from managers, and incentives such as provision of study leave helped reduce staff turnover by 86%.
Career development offered trainings and career development on site. In Coptic HC, Kenya, there are opportunities for trainings and study leaves for additional learning to increase staff retention. In Uganda, TASO sites open management positions to staff with no medical background.
“At TASO, only 2 out of 11 centre managers are doctors so every counselor or lab technician knows they can grow here if they want”—TASO Management
Improving work environments by enhancing on-site infrastructures, medical facilities, and working interactions also seek to improve work conditions. Previously in Kitebi, Uganda, staff left work early because of lack of access to clean toilets. As a solution, separate toilets for staff were introduced. At Wakiso Health Centre in Uganda, tea and bites were offered to 36 health workers early in the morning, leading to a 25% increase in day-to-day effective working time. A cordial working environment improved staff retention at TASO, Masaka.
“People are staying at TASO because of the family spirit. I know I will not find a similar culture elsewhere”—Staff at TASO-Masaka
Recognition through performance-based incentives and rewards was also used. At Kiswa and Wakiso HCs in Uganda, and Coptic in Kenya, staff of the month and staff of the year awards were distributed, and pictures of winners were displayed on the wall. This helped to motivate and boost morale of the staff.
“Employees like their photos to be displayed as people recognise them as the award recipient… they ask for a copy of the announcement to show their families and proudly attach it to their CVs”—HR Manager (Coptic)
DISCUSSION
This study identified several different approaches used by facilities to overcome bottlenecks of implementation in service provision. These included tailoring approaches more closely to the needs of specific clients, for which the term differentiation is used, and a set of facility enablers or management approaches to improve the work experience. Differentiated approaches and enablers adapted across the HIV care continuum have the potential to improve service accessibility and efficiency.18 This can enhance the quality of the client experience and ensure the health system functions in an accountable and efficient way.19 Having reliable systems for collecting routine data and the effective use of these data allow for facilities to better understand their processes, gather insights on their client demographics, identify risk groups, and improve access to quality care.20
Many health facilities also face human resource challenges such as low staff motivation and retention, substantial absenteeism, and a large number of vacancies. As such, having strong human resource management systems becomes essential to increasing motivation and retention of staff and for developing an integrated people-centered approach to health services.21
Since this work began in 2015, several countries have advanced the differentiated care focus by revising national policies and guidance, applying these models to different population settings, and measuring the cost savings potential for some of these service delivery models.22 Guidance on differentiated care has evolved for advanced HIV clients, adolescents, children, pregnant and breastfeeding women, as well as key populations.19 Differentiated service delivery for key populations could increase the number of people who know their status if community-based and lay provider testing are implemented at scale,23,24 as seen with community outreach models in Uganda.
With almost all countries adopting WHO recommendations to provide immediate and lifelong ART to people living with HIV regardless of their CD4 count,25 replicating differentiated approaches may help reduce the demand pressure on health facilities and increase focus on individuals with the greatest need, as seen in Uganda TASO sites. Tailoring approaches to the facility's daily client intake and available resources can help deliver the appropriate care at the ideal service frequency to specific individuals.26
Implementing differentiated care models has certain caveats. First, health workers and facilities need to be motivated with incentives, financial or nonfinancial, as seen in health facilities in Uganda. Second, health facilities may face challenges in implementing differentiated care, which takes time and effort with the current focus on rapid scale-up of numbers on treatment, potentially sacrificing quality for rapid expansion. Host governments and donors should seek to create enabling environments for processes which may improve the quality of service delivery and reward facilities that achieve these improvements. Third, many health facilities in resource-limited settings lack the processes and systems needed for improving knowledge and documenting changes over time, but this can be addressed by implementing knowledge sharing networks and systems for sharing of best practices.27 Finally, programmatic changes, such as providing training or career development, and building systems to improve staff conditions may require frontloading financial investments to improve program quality and efficiency.
Study Limitations
Natural observation studies suffer from limitations related to sampling and reporting bias. Thus, the inferences from this study may be limited by the purposefully selected sample and selective reporting from interviews.13 A standard questionnaire and interview guide were used for observations for all facilities. Although, this does not eliminate all bias, the findings are still useful for governments and implementers in understanding innovations in HIV service delivery. Understanding the practices that occur in real-life settings allows for these to be adapted in other settings, under trial conditions, providing opportunities for future research.
CONCLUSIONS
At the facility level, many services address systems and financial constraints in innovative ways. Scaling up differentiated care models may offer a pathway to address programmatic constraints in low-resource settings. However, more studies are needed including costing studies to better understand potential efficiency gains.28 In addition, key metrics for measuring program improvement using financial data and the number of refill and clinical visits for clients retained in care will be practical for program managers to use.29
Differentiated models of care for HIV should be viewed as part of the wider focus on health systems strengthening. Tailoring services to population need can be applied to other types of service delivery across both communicable and noncommunicable diseases, critical to both global and national policy agendas. Replicating these models to scale will require on-going monitoring, so site managers can take strategic actions using client-centric indicators, integrating communities into workforce planning, and sharing of best practices across facilities to improve the quality of service delivery.
Supplementary Material
ACKNOWLEDGMENTS
The authors would like to acknowledge the support of the Kenya MOH and Uganda MOH. They would also like to thank Saman Zamani, the GF Uganda Country Team, John Ochero, Caroline Olwande, Dr. Martin Sirengo, Swetha Balachandran, Johanna Benesty for their support and contributions.
Footnotes
The authors have no conflicts of interest to disclose.
The study was conceptualized by M.D., A.F., M.J., and L.M. M.E., S.A., and M.I. supervised research activities and data collection. Data interpretation and analysis was conducted by S.K., H.S., and A.F. S.K., H.S. and A.F. developed the initial version of the manuscript. All authors contributed to manuscript review, editing, and approved the final version.
S.K. and H.S. contributed equally to the work.
Supplemental digital content is available for this article. Direct URL citations appear in the printed text and are provided in the HTML and PDF versions of this article on the journal's Web site (www.jaids.com).
REFERENCES
- 1.Joint United Nations Program on HIV/AIDS (UNAIDS) Global AIDS Update, 2018. Geneva, Switzerland: UNAIDS; 2018. [Google Scholar]
- 2.Kates J, Wexler A, Lief E. Financing the Response to HIV in Low and Middle-Income Countries: International Assistance from Donor Governments in 2015. Menlo Park, CA: Kaiser Family Foundation UNAIDS; 2016. [Google Scholar]
- 3.El-Sadr WM, Harripersaud K, Rabkin M. Reaching global HIV/AIDS goals: what got us here, won't get us there. PLoS Med. 2017;14:e1002421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.El Arifeen S, Christou A, Reichenbach L, et al. Community-based approaches and partnerships: innovations in health-service delivery in Bangladesh. Lancet . 2013;382:2012–2026. [DOI] [PubMed] [Google Scholar]
- 5.Grabbe KL, Menzies N, Taegtmeyer M, et al. Increasing access to HIV counseling and testing through mobile services in Kenya: strategies, utilization, and cost-effectiveness. J Acquir Immune Defic Syndr. 2010;54:317–323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.TB Reach. The National TB and Leprosy Control Programme. Cambodia: 2010. Available at: http://www.stoptb.org/assets/documents/global/awards/tbreach/Cambodia%20NTBLCP.pdf. Accessed November 15, 2017. [Google Scholar]
- 7.Franke MF, Kaigamba F, Socci AR, et al. Improved retention associated with community-based accompaniment for antiretroviral therapy delivery in rural Rwanda. Clin Infect Dis. 2012;56:1319–1326. [DOI] [PubMed] [Google Scholar]
- 8.Holmes CB, Sanne I. Changing models of care to improve progression through the HIV treatment cascade in different populations. Curr Opin HIV AIDS. 2015;10:447–450. [DOI] [PubMed] [Google Scholar]
- 9.Grimsrud A, Lesosky M, Kalombo C, et al. Community-based adherence clubs for the management of stable antiretroviral therapy clients in Cape Town, South Africa: a cohort study. J Acquir Immune Defic Syndr. 2016;71:e16–e23. [DOI] [PubMed] [Google Scholar]
- 10.Buzaalirwa L, Maharaj TER, Kgaka NOM, et al. Strategies to address clinic waiting time and retention in care; lessons from a large ART center in South Africa. Presented at: 17th International Conference on AIDS and STIs in Africa; December 9, 2013; Cape Town.
- 11.Saito S, Howard AA, Chege D, et al. Monitoring quality at scale: implementing quality assurance in a diverse, multi-country HIV program. AIDS. 2015;29:S129–S136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Omachonu VK, Einspruch NG. Innovation in healthcare delivery systems: a conceptual framework. Innovation J. 2010;15:1–20. [Google Scholar]
- 13.Patton MQ. Qualitative Research and Evaluation Methods. Thousand Oaks, CA: Sage Publications; 2002. [Google Scholar]
- 14.Glaser BG, Strauss AL. The Discovery of Grounded Theory: Strategies for Qualitative Research. Chicago, IL: Aldine Publishing Company; 1967. [Google Scholar]
- 15.Srivastava A, Thomson SB. Framework analysis: a qualitative methodology for applied policy research. J Adm Governance. 2009;4 [Internet] Available at: http://research.apc.org/images/a/ad/Framework_analysis.pdf. Accessed April 2, 2018. [Google Scholar]
- 16.Kay ES, Batey DS, Mugavero MJ. The HIV treatment cascade and care continuum: updates, goals, and recommendations for the future. AIDS Res Ther. 2016;13:35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.The Global Fund. A Toolkit for Health Facilities: Differentiated Care and for HIV and Tuberculosis. Geneva: The Global Fund; 2015. [Google Scholar]
- 18.Grimsrud A, Barnabas RV, Ehrenkranz P, et al. Evidence for scale up: the differentiated care research agenda. J Int AIDS Soc. 2017;20:22024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.It's Time to Deliver Differently [Internet]. International AIDS Society; 2018. Available at: http://www.differentiatedcare.org/. Accessed March 15, 2015. [Google Scholar]
- 20.Youngleson MS, Nkurunziza P, Jennings K, et al. Improving a mother to child HIV transmission programme through health system redesign: quality improvement, protocol adjustment and resource addition. PLoS One. 2010;5:e13891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Touré H, Audibert M, Dabis F. To what extent could performance-based schemes help increase the effectiveness of prevention of mother-to-child transmission of HIV (PMTCT) programs in resource-limited settings? A summary of the published evidence. BMC Public Health. 2010;10:702. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Prust ML, Banda CK, Nyirenda R, et al. Multi-month prescriptions, fast-track refills, and community ART groups: results from a process evaluation in Malawi on using differentiated models of care to achieve national HIV treatment goals. J Int AIDS Soc. 2017;20:41–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Macdonald V, Verster A, Baggaley R. A call for differentiated approaches to delivering HIV services to key populations. J Int AIDS Soc. 2017;20:28–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Mesic A, Fontaine J, Aye T, et al. Implications of differentiated care for successful ART scale‐up in a concentrated HIV epidemic in Yangon, Myanmar. J Int AIDS Soc. 2017;20(suppl 4):21644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.World Health Organization. Consolidated Guidelines on the Use of Antiretroviral Drugs for Treating and Preventing HIV Infection: Recommendations for a Public Health Approach. 2nd ed Geneva, Switzerland: WHO; 2016. [PubMed] [Google Scholar]
- 26.Duncombe C, Rosenblum S, Hellmann N, et al. Reframing HIV care: putting people at the centre of antiretroviral delivery. Trop Med Int Health. 2015;20:430–447. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Barker C, Dutta A, Klein K. Can differentiated care models solve the crisis in HIV treatment financing? Analysis of prospects for 38 countries in sub-Saharan Africa. J Int AIDS Soc. 2017;20:68–79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Virtual Community of Practice: M&E of DSD [Internet]. HIV Learning Network: The CQUIN Project for Differentiated Care. Columbia University; 2017. Available at: https://cquin.icap.columbia.edu/projects/virtual-community-of-practice-me-of-dsd/. Accessed March 15, 2018. [Google Scholar]
- 29.Ehrenkranz P, Calleja JMG, El-Sadr W, et al. A pragmatic approach to monitor and evaluate implementation and impact of differentiated ART delivery for global and national stakeholders. J Int AIDS Soc. 2018;21:1–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.