Abstract
Background
Anxiety disorder, one of the highly disabling, prevalent and common mental disorders, is known to be more prevalent in persons with type 2 diabetes mellitus (T2DM) than the general population, and the comorbid presence of anxiety disorders is known to have an impact on the diabetes outcome and the quality of life. However, the information on the type of anxiety disorder and its prevalence in persons with T2DM is limited.
Aims
To assess the prevalence and correlates of anxiety disorder in people with type 2 diabetes in different countries.
Methods
People aged 18–65 years with diabetes and treated in outpatient settings were recruited in 15 countries and underwent a psychiatric interview with the Mini-International Neuropsychiatric Interview. Demographic and medical record data were collected.
Results
A total of 3170 people with type 2 diabetes (56.2% women; with mean (SD) duration of diabetes 10.01 (7.0) years) participated. The overall prevalence of anxiety disorders in type 2 diabetic persons was 18%; however, 2.8% of the study population had more than one type of anxiety disorder. The most prevalent anxiety disorders were generalised anxiety disorder (8.1%) and panic disorder (5.1%). Female gender, presence of diabetic complications, longer duration of diabetes and poorer glycaemic control (HbA1c levels) were significantly associated with comorbid anxiety disorder. A higher prevalence of anxiety disorders was observed in Ukraine, Saudi Arabia and Argentina with a lower prevalence in Bangladesh and India.
Conclusions
Our international study shows that people with type 2 diabetes have a high prevalence of anxiety disorders, especially women, those with diabetic complications, those with a longer duration of diabetes and poorer glycaemic control. Early identification and appropriate timely care of psychiatric problems of people with type 2 diabetes is warranted.
Keywords: diabetes mellitus, anxiety disorders, panic disorders, multicentre study, prevalence
Introduction
Anxiety disorders are characterised by excessive worries, hyperarousal states and fear, which are counterproductive and debilitating.1 The global prevalence of anxiety disorder in the general population is about 7.3% (4.8%–10.9%),2 and it is one of the leading causes of disability with 390 disability-adjusted life years per 100 000 persons.3 Anxiety disorders mainly comprise generalised anxiety disorder (GAD), panic disorder, agoraphobia, social phobia, obsessive-compulsive disorder (OCD) and post-traumatic stress disorder (PTSD). Recent high-quality studies,4–9 including a systematic review,10 have reported a higher prevalence and incidence of anxiety disorders in people with type 2 diabetes mellitus compared with the general population. It has also been suggested that there may be a bidirectional relationship between these two disorder conditions.11 12 Female sex, younger age, low socioeconomic status and concomitant chronic illnesses are particular vulnerability factors for developing anxiety disorders.5 13 14 The most prevalent anxiety disorders in people with diabetes mellitus are GAD (21%), social phobia (7%) and panic disorder (2.5%).15 A substantial proportion of people with diabetes also exhibit higher subsyndromal anxiety and elevated anxiety symptoms.10 14 16 In diabetes, anxiety is associated with poor glycaemic control,16–20 increased risk of diabetes-related complications, increased risk of stroke21 and poor quality of life,22 23 which may improve with anxiolytics and non-pharmacological treatments.24–26 Hence, it is essential to identify and address anxiety in persons with diabetes early on, in order to reduce the burden of comorbid disease, improve blood glucose control and therefore reduce the risk of diabetes complications.
There are wide variations in the prevalence of anxiety disorders across countries and within, which could be due to heterogeneous study samples, the use of different assessment tools and even using different cut-off levels within the same scales. In addition, many studies have reported the presence of both elevated anxiety symptoms and the syndromal anxiety disorders with less clear distinction between them.14 16
More specifically, the prevalence of anxiety symptoms in patients with type 2 diabetes using the Hospital Anxiety and Depression Scale in Pakistan was reported to be around 57.9%,27 with a much lower prevalence of 9% in Germany.28 In Saudi Arabia, the prevalence of psychiatric disorders in the general population is still unknown. However, the prevalences of primary anxiety disorders among inpatient and outpatient psychiatric patients in Saudi Arabia have been reported as 1.6% and 16.3%, respectively.29 With regard to diabetes populations in Saudi Arabia (which has one of the highest prevalence rates of type 2 diabetes), studies have reported the prevalence of significant anxiety symptoms to be 28.5%, which was higher in women, those smoking, with a longer duration of diabetes and being unmarried.30 Another study in Saudi Arabia, using the Hamilton Anxiety Scale, reported a prevalence of 3.3% of people with diabetes compared with 5% of controls with no significant difference.31 Among hospitalised patients with type 2 diabetes 50.6% were identified as suffering from anxiety which was independently associated with physical inactivity.9 Approximately similar prevalence rates were observed in two studies of patients with type 2 diabetes, with physical inactivity and poor social support being explanatory factors.9 10
In Poland, a nationwide study conducted between 2010 and 2011 on a large population of 10 081 persons aged 18–64 showed the prevalence of different anxiety disorders to be between 0.1% and 6.2%;32 however, there are no reports of anxiety in persons with diabetes. In contrast, one study in Russia observed a much higher rate of anxiety disorders of 60%.33 Diabetes-specific phobias (phobias of needles, blood, hypoglycaemia) were also observed in 1.7%.34 These studies have combined people with type 1 and type 2 diabetes so it is difficult to infer the exact prevalence and association of anxiety disorders in each of the subtypes of diabetes.
In a collaborative study across 15 countries differing in socioeconomic status, cultural background and levels of healthcare services, we aimed to study the prevalence and treatment of comorbid anxiety disorder in a large cohort of people with type 2 diabetes. The same study protocol was used across the countries which included both a clinical interview and a screening instrument to detect clinically significant anxiety.35
Methods
A full description of the protocol of the International Prevalence and Treatment of Diabetes and Depression (INTERPRET-DD) study used in the present study is provided in earlier papers.35 36 In brief, consecutive outpatient clinic attendees with type 2 diabetes, diagnostic criteria according to WHO criteria (random plasma glucose ≥11.1 mmol/L or fasting plasma glucose ≥7.0 mmol/L or 2-hour plasma glucose ≥11.1 mmol/L), at each of the study sites were invited to participate in the study between September 2013 and May 2015. Site investigator teams were recruited from leading centres of excellence in each country, which included at least one psychiatrist and endocrinologist for each country. The treating physician/diabetologist in the diabetes clinic invited individuals to participate in the study. Diabetes clinics were based in either secondary or tertiary care centres, depending on the facilities available in each country. However, from Pakistan, another centre from primary care was also included. The observations presented here pertain to the first cross-sectional assessment of the subjects during the first intake.
Inclusion/exclusion criteria
Full details of the eligibility criteria have been described elsewhere.35 36 In brief, the participants were adults (aged 18–65 years) with type 2 diabetes diagnosed at least 12 months before the point of contact at the diabetes outpatient facilities. Detailed medical records and sociodemographic details of the participants were obtained.
A psychiatric interview was conducted by a trained interviewer using the Mini-International Neuropsychiatric Interview (MINI, version 5 or version 6 depending on the current psychiatric practice at the study site).37 The MINI is a reliable diagnostic tool that has been widely used in a range of different populations, suitable for subjects with serious illness as well as in community surveys, and is in accordance with the Diagnostic and Statistical Manual of Mental Disorders Fifth Edition criteria.38 Individuals diagnosed with anxiety disorders were advised to consult their physician for further assessment and treatment. In the case of any psychiatric emergencies such as suicidal risk,the interviewing psychiatrist initiated immediate appropriate clinical care.
Statistical analysis
SPSS V.2339 was used to analyse the data. Comparative profiles of demographic and clinical variables between people with type 2 diabetes with and without anxiety disorder were examined using independent samples t-test or χ2 test as applicable.
Results
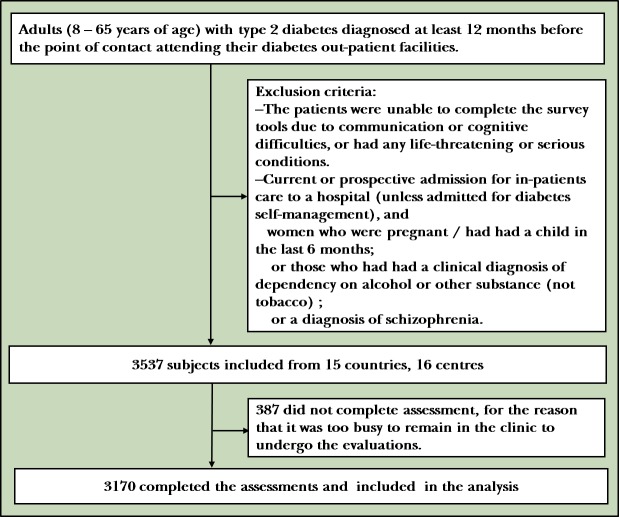
A total of 3170 people with type 2 diabetes (56.2% women; mean (SD) duration of diabetes 10.01 (7.0) years) participated (see figure 1). The mean (SD) age of the study population was 53.43 (9.52) years.
Figure 1.
Flowchart of the sample recruitment.
The prevalence of anxiety disorders in type 2 diabetes persons was 18% (table 1). The most common anxiety disorders were GAD (8.5%) and lifetime panic disorder (5.1%). More than one type of anxiety disorders were observed in 2.8% of the study population. Only 4% of the study subjects had more than one psychiatric disorder like dysthymia or major depressive episode.
Table 1.
Prevalence of anxiety disorders by country (n, %)
| Countries (n) | GAD | Panic disorder (lifetime) | Panic disorder (current) | Agoraphobia | Social phobia | OCD | %† | Prevalence* |
| Argentina (134) | 32 (23.9%) | 12 (9.0%) | 19 (14.2%) | 12 (9.0%) | 7 (5.2%) | 3 (2.2%) | 1.6 | 37.6 |
| China (388) | 19 (4.9%) | 11 (2.8%) | 4 (1.0%) | 17 (4.4%) | 9 (2.3%) | 9 (2.3%) | 1.4 | 11.3 |
| Germany (117) | 3 (2.5%) | 3 (2.5%) | 1 (0.9%) | 13 (11%) | 0 (0.0%) | 0 (0.0%) | 0.5 | 12.7 |
| India (197) | 1 (0.5%) | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | 0.0 | 0.5 |
| Italy (202) | 4 (2.0%) | 9 (4.4%) | 2 (1.0%) | 4 (2%) | 0 (0.0%) | 0 (0.0%) | 0.6 | 8.9 |
| Kenya (184) | 12 (6.5%) | 18 (9.8%) | 8 (4.3%) | 10 (5.4%) | 11 (6.0%) | 6 (3.3%) | 1.8 | 30.4 |
| Mexico (203) | 26 (12.8%) | 11 (5.4%) | 15 (7.4%) | 4 (2.0%) | 1 (0.5%) | 2 (1.0%) | 1.4 | 22.2 |
| Pakistan (207) | 1 (0.5%) | 1 (0.5%) | 1 (0.5%) | 2 (1.0%) | 2 (1.0%) | 1 (0.5%) | 0.1 | 1.9 |
| Poland (217) | 23 (10.6%) | 14 (6.5%) | 9 (4.1%) | 8 (3.7%) | 10 (4.6%) | 1 (0.5%) | 1.1 | 16.6 |
| Russia (200) | 37 (18.5%) | 25 (12.5%) | 20 (10%) | 28 (14%) | 21 (10.5%) | 5 (2.5%) | 2.2 | 35.5 |
| Serbia (200) | 1 (0.5%) | 2 (1.0%) | 0 (0.0%) | 3 (1.5%) | 0 (0.0%) | 0 (0.0%) | 0.2 | 2.5 |
| Ukraine (132) | 12 (9.1%) | 44 (33.3%) | 30 (22.7%) | 6 (4.5%) | 11 (8.3%) | 6 (4.5%) | 3.0 | 72.7 |
| Uganda (198) | 9 (4.5%) | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | 0.3 | 5.1 |
| Pakistan (PC 214) | 19 (8.9%) | 0 (0.0%) | 2 (0.9%) | 1 (0.5%) | 0 (0.0%) | 1 (0.5%) | 0.7 | 9.9 |
| Bangladesh (194) | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | 0 (0.0%) | 0.0 | 0.0 |
| Saudi Arabia (174) | 71 (41%) | 11 (6.3%) | 9 (5.2%) | 2 (1.1%) | 9 (5.2%) | 9 (5.2%) | 3.0 | 52.2 |
| Total | 270 (8.5%) | 161 (5.1%) | 120 (3.8%) | 110 (3.5%) | 81 (2.6%) | 43 (1.4%) |
*Prevalence of anxiety disorder in each country.
†Per cent of anxiety disorder cases contributed by each country.
GAD, generalised anxiety disorder; OCD, obsessive-compulsive disorder; PC, primary care (Pakistan).
Particularly Ukraine, Saudi Arabia and Argentina showed higher rates of anxiety disorders (72.7%, 52.2% and 37.6%, respectively) whereas prevalences were found to be lower/absent in India and Bangladesh (0.5% and 0.0%, respectively) as shown in table 1. These differences were statistically different between the countries. However, it is not possible to compute these differences for different types of anxiety disorders in different countries due to small (or absent) numbers in many categories in different countries.
Female gender was positively associated with all anxiety disorders (table 2).
Table 2.
Gender differences across anxiety disorders in people with diabetes
| Gender | χ2 | P value | ||
| Female n (% of total sample) |
Male n (% of total sample) |
|||
| GAD (current) | 193 (6.1) | 77 (2.4) | 27.78 | <0.001 |
| Panic disorder (current) | 80 (2.5) | 40 (1.3) | 5.43 | 0.020 |
| Agoraphobia | 84 (2.7) | 26 (0.8) | 18.71 | <0.001 |
| OCD | 36 (1.1) | 7 (0.2) | 13.32 | <0.001 |
| Social phobia | 60 (1.9) | 21 (0.7) | 10.71 | <0.001 |
| Panic disorder (lifetime) | 118 (3.7) | 43 (1.4) | 19.96 | <0.001 |
GAD, generalised anxiety disorder; OCD, obsessive-compulsive disorder.
Presence of GAD (t=3.08, p=0.002) and current panic disorder (t=1.98, p=0.04) as well as lifetime panic disorder (t=2.21, p=0.027) were all significantly associated with poorer glycaemic control as indicated by HbA1c levels compared with participants without anxiety disorders (table 3).
Table 3.
Diabetic control (HbA1c %) by anxiety disorders
| HbA1c % in those with anxiety disorders n (mean (SD)) |
HbA1c % in those without anxiety disorders n (mean (SD)) |
T-test statistics | P value | 95% CI | |
| GAD | 215 (8.79 (2.45)) |
2074 (8.27 (2.36)) |
−3.08 | 0.002 | 0.86 to 0.19 |
| Panic disorder (current) | 109 (8.76 (2.05)) |
2179 (8.30 (2.39)) |
−1.98 | 0.040 | 0.90 to 0.00 |
| Agoraphobia | 98 (8.45 (2.21)) |
2192 (8.31 (2.380)) |
−0.52 | 0.580 | 0.61 to 0.34 |
| OCD | 39 (8.69 (2.27)) |
2251 (8.31 (2.38)) |
−0.99 | 0.320 | 1.13 to 0.37 |
| Social phobia | 73 (8.78 (2.32)) |
2217 (8.30 (3.28)) |
−1.70 | 0.088 | 1.03 to 0.72 |
| Panic disorder (lifetime) | 149 (8.73 (2.36)) |
2141 (8.29 (2.38)) |
−2.21 | 0.027 | 0.84 to 0.05 |
GAD, generalised anxiety disorder; OCD, obsessive-compulsive disorder.
Duration of diabetes was positively correlated with the presence of GAD (t=4.645, p=0.001), OCD (t=2.064, p=0.039) and PTSD (t=3.201, p=0.001) (table 4).
Table 4.
Duration of diabetes by anxiety disorders
| Yes n (mean (SD)) |
No n (mean (SD)) |
T-test statistics | P value | 95% CI | |
| GAD | 268 (11.91 (7.87)) | 2884 (9.83 (6.90)) | −4.64 | <0.001 | 1.19 to 0.44 |
| Panic disorder (current) | 120 (10.83 (6.52)) | 3031 (9.98 (7.03)) | −1.29 | 0.194 | 0.43 to 0.65 |
| Agoraphobia | 109 (10.05 (6.86)) | 3043 (10.01 (7.01)) | 0.05 | 0.955 | 1.30 to 0.68 |
| Social phobia | 81 (10.32 (6.12)) | 3071 (10.01 (7.03)) | 0.39 | 0.694 | 1.23 to −0.31 |
| OCD | 43 (12.20 (7.45)) | 3109 (9.98 (7.00)) | −2.06 | 0.039 | −0.11 to 1.07 |
| Panic disorder (lifetime) | 161 (10.59 (7.18)) | 2992 (9.98 (7.00)) | −1.06 | 0.287 | 0.50 to 0.56 |
GAD, generalised anxiety disorder; OCD, obsessive-compulsive disorder.
Those with anxiety disorders except OCD showed statistically significantly higher rates of diabetic complications than those without anxiety disorders (table 5). The diabetic complications recorded were mainly in the form of diabetic nephropathy and neuropathy. Almost half the subjects had one or more diabetes-related medical complications as reported in our previous study on the same subject samples.35
Table 5.
Diabetes complications by anxiety disorder
| Diabetic complication | χ2 statistic | P value | ||
| Yes n (% of total sample) |
No n (% of total sample) |
|||
| GAD (current) | 154 (5.3) | 93 (3.2) | 9.21 | 0.002 |
| Panic disorder | 82 (2.8) | 32 (1.1) | 16.75 | <0.001 |
| Agoraphobia | 69 (2.4) | 39 (1.3) | 5.21 | 0.022 |
| Social phobia | 52 (1.8) | 25 (0.9) | 6.56 | 0.010 |
| OCD | 26 (0.9) | 15 (0.5) | 1.76 | 0.185 |
| Panic disorder (lifetime) | 100 (3.4) | 55 (1.9) | 8.50 | 0.004 |
GAD, generalised anxiety disorder; OCD, obsessive-compulsive disorder.
Discussion
Main findings
In our study we observed a substantially high prevalence of anxiety disorder (18%) in people with type 2 diabetes. The most prevalent anxiety disorders were found to be GAD and panic disorder. Some countries had statistically higher rates of anxiety disorders than others. However, whether these statistical differences reflect differences in the overall rates in these countries is difficult to comment as the general population prevalence of anxiety disorders in all the countries is not available. Female gender, the presence of diabetes complications, longer duration of diabetes and poorer glycaemic control were all observed to be correlates of anxiety disorders, however there was wide variation of occurrence of anxiety disorders across the 15 countries studied. The predominance of anxiety disorders in females with diabetes may be a reflection of the overall pattern for anxiety disorders. This study identified differences in the prevalence of anxiety symptoms, as well as the clinical diagnosis of anxiety disorders among the countries. Similar observations were described in the report on depressive disorders in diabetes mellitus, in this same sample group.35 This may reflect differences in the acceptance/stigma of acknowledging symptoms of psychological and emotional distress in different cultural groups. It is difficult to speculate whether the different rates can be attributed to between-country characteristics, as this aspect was not studied in detail.35 The exact ratio of anxiety disorders in the general population of each country was not available to derive any conclusive inference about the effect of gender on occurrence of anxiety disorders in people with diabetes. We observed a high percentage of anxiety disorders in the Russian sample which may be caused by the relatively higher proportion of women in the sample, which was 76.5%. The detection of anxiety disorders in women compared with men was higher, especially in agoraphobia (16.3% vs 6.4%). The increased frequency of anxiety disorders in participants from Russia may be related to the high frequency of PTSD, which reached 7.5%.
The findings of this study make an important contribution to the evidence of occurrence of anxiety disorders in people with type 2 diabetes. In particular, we have used the same methodology for identification across all the countries and so comparisons are more appropriate. Similar findings were reported in studies from the USA40 and others on higher risk of development and prevalence of anxiety disorders in persons with diabetes.10 12 15 41 However, there is wide variation in prevalence of anxiety disorders across studies which could be due to differences in methodology such as the tools used for assessment, ethnic background, cultural variation or diabetes-related factors.10
Like other studies,14 22 we have observed wide differences in rates of anxiety disorders across the 15 countries, with higher rates in countries such as Ukraine, Saudi Arabia and Argentina, and lower rates in countries such as India, Bangladesh and Pakistan. It is interesting to note that the rates of anxiety disorders in this study were lower than the World Mental Health Survey (WMHS) initiative42 in two countries, Germany and Italy, and markedly higher in another two countries, namely Ukraine and Mexico. In the clinical sample in this study, we would have expected higher rates compared with the general population sample in WMHS, but the findings do not indicate this consistently. The differences between countries that we have observed could be speculated to be due to cultural differences in the reporting and experience of anxiety symptoms, possibly due to the stigma associated with having a mental health problem or due to the extensive social support offered by families in some countries which may aid onset prevention. In addition, anxiety disorders in the general population have been reported to be less prevalent in the Indo/Asian countries than in the rest of the world,13 which supports our findings. A South American country (Brazil) has reported a much higher prevalence of GAD and panic disorder compared with the prevalence we observed in Argentina. This difference could be due to differences in diabetes duration (the Brazilian study only included people with more than 5 years of diabetes compared with the current study in which participants are included with at least 1 year of diabetes). In our study, duration of diabetes was a significant factor associated with anxiety disorders.
The results in the sample of patients from Poland show a strikingly higher prevalence of anxiety disorders in persons with type 2 diabetes in comparison to the general population. The prevalence of social phobia was over three times higher, GAD almost 10 times higher, panic disorder almost 14 times higher and agoraphobia almost 19 times higher in persons with type 2 diabetes when compared with the most recent data from a large sample of the general population.32 With the current methodology, it is difficult to speculate on the possible reasons for this observation.
Our findings of a relationship between symptoms of anxiety and other physical comorbidities, along with poorer glycaemic control, support the findings of other countries mentioned above. In our previous report on this study sample, insulin use was reported by 41.8%, and 50.8% of subjects reporting one or more complications.35
Limitations
As in other studies, the present study also has some limitations. First, the severity of the anxiety disorders was not measured. Second, details about the use of psychotropic medications for the persons with clinically significant anxiety which could have provided an indirect measure of severity of the symptoms were not available. Third, details about insulin requirements for the management of diabetes could have given information as to whether the psychological distress related to use of insulin has an impact on the anxiety symptoms.43 Although the assessments and interviews were conducted by trained and qualified interviewers, the inter-rater reliability between the interviewers was not attempted due to the location of centres across the 15 countries. In our follow-up study, we will be able to examine the longitudinal associations of the use of psychotropic medications or non-pharmacological management of anxiety disorders on glycaemic control. Fourth, because the present study took place in specialty clinics, which may not be representative of the wider population of people with diabetes, the prevalence rates in the present study cannot be generalised to the wider diabetes population.
Implications
The INTERPRET-DD study has a number of strengths. It was a collaborative study of the prevalence of anxiety disorders in people with type 2 diabetes, carried out at the same time using the same protocol in 15 different countries. This study included more than 3000 people with a clinical diagnosis of type 2 diabetes,35 36 and is methodologically strong with the use of a reliable diagnostic tool for identifying anxiety disorders implemented by trained interviewers. In addition, the investigators in each country ensured that the diagnostic tools were culturally applicable through a series of discussions and testing by a range of healthcare professionals and people with type 2 diabetes, which focused on the meaning of terms as well as language.
Conclusion
This report presents the cross-sectional findings on the occurrence of anxiety disorders, hence, it is difficult to comment on whether the anxiety disorder is a complication or sequelae of diabetes, or just a comorbid psychiatric condition. It is not possible to comment on which anxiety disorders were present prior to diagnosis of diabetes, and which were a consequence of having diabetes. The result of our prospective follow-up study is likely to shed light on this aspect. It is essential to pay additional attention to mental health issues such as anxiety in persons with diabetes to ensure better quality of life22 and better glycaemic control,44 and to lessen the burden of diabetes-related complications.21 45 It is likely that anxiety may be a protective factor for diabetes complications as anxious people may consult more for minor symptoms and ailments.46
Anxiety disorder was observed in 18% of people with type 2 diabetes. Factors associated with higher prevalence of anxiety disorders were female gender, longer duration of diabetes, more diabetes complications and poorer diabetic control. The International Diabetes Federation recommends regular screening for psychological problems such as depression,47 and the findings of this present study extend this to anxiety. Hence, it is important to identify and address the comorbid anxiety in persons with diabetes at the earliest in order to offer psychological interventions which could improve diabetic control, so reducing the risk of developing diabetes complications which have negative consequences for quality of life.
Biography
 Dr Santosh K Chaturvedi, MD, FRCPE [Edinburgh UK], FRCPsych [UK] is a Senior Professor of Psychiatry at the National Institute of Mental Health & Neurosciences, Bangalore, India. He was one of the principal investigators along with Professor Y Nakane in the International Collaborative Study on Quality of Life of Caregivers of Dementia patients, Japan, 1997 to 1999. He is the Editor-in-Chief of the Journal of Psychosocial Rehabilitation and Mental health, published by Springer Nature. His research interests include consultation liaison psychiatry, chronic pain & somatization, neuropsychiatry, quality of life research, psycho-oncology & palliative care, dementia, cultural psychiatry, instruments & scales development & translations, and postgraduate training & teaching methods. He has more than 550 publications in different international and national journals, with more than 280 citations / listings in PUBMED / MEDLINE; He has edited and / or published sixteen books, manuals or journals. H index 33; i10 index 111; Citations >4000
Dr Santosh K Chaturvedi, MD, FRCPE [Edinburgh UK], FRCPsych [UK] is a Senior Professor of Psychiatry at the National Institute of Mental Health & Neurosciences, Bangalore, India. He was one of the principal investigators along with Professor Y Nakane in the International Collaborative Study on Quality of Life of Caregivers of Dementia patients, Japan, 1997 to 1999. He is the Editor-in-Chief of the Journal of Psychosocial Rehabilitation and Mental health, published by Springer Nature. His research interests include consultation liaison psychiatry, chronic pain & somatization, neuropsychiatry, quality of life research, psycho-oncology & palliative care, dementia, cultural psychiatry, instruments & scales development & translations, and postgraduate training & teaching methods. He has more than 550 publications in different international and national journals, with more than 280 citations / listings in PUBMED / MEDLINE; He has edited and / or published sixteen books, manuals or journals. H index 33; i10 index 111; Citations >4000
Footnotes
Correction notice: This paper has been updated since it was first published. The affiliations of Umberto Valentini and Gianluca Castelnuovo have been amended.
Authors contributions: SKC and SMG analysed the data and prepared the first draft of the manuscript. All authors from the 15 countries contributed to the study in its planning, data collection and analysis. All authors contributed to the manuscript and approved the final versions.
Funding Statement: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: AB has received a research grant from Abbott, and fees for lectures from Lundbeck. CL has received travel expenses paid by unrestricted grants from Eli Lily and Sanofi to attend the World Diabetes Congress and the American Psychiatric Association conference. The Association for the Improvement of Mental Health Programs, which sponsored this programme and financially supported tasks related to its management and data analysis, received unrestricted grants from Eli Lilly and Sanofi. NS received travel support and fees from Janssen, Cilag, Lundbeck International Neuroscience Foundation, Servier: all outside the activities related to work on this study or on this paper. WW has received personal fees from Roche Pharma, outside the submitted work.
Patient consent for publication: Not required.
ETHICAL APPROVAL: Prior to commencing the study, ethical approval was obtained in all study settings. Ethical approval was also obtained from the Open University, UK, where the data were stored for analysis.
Provenance and peer review: Not commissioned; externally peer reviewed.
Data availability statement: Data available at coordinating centre
References
- 1. Simpson HB, Neria Y, Lewis-Fernández R, et al. Anxiety DisordersTheory, research and clinical perspectives. Cambridge University Press, 2010. [Google Scholar]
- 2. Baxter AJ, Scott KM, Vos T, et al. Global prevalence of anxiety disorders: a systematic review and meta-regression. Psychol Med 2013;43:897–910. 10.1017/S003329171200147X [DOI] [PubMed] [Google Scholar]
- 3. Baxter AJ, Vos T, Scott KM, et al. The global burden of anxiety disorders in 2010. Psychol Med 2014;44:2363–74. 10.1017/S0033291713003243 [DOI] [PubMed] [Google Scholar]
- 4. Huang C-J, Chiu H-C, Lee M-H, et al. Prevalence and incidence of anxiety disorders in diabetic patients: a national population-based cohort study. Gen Hosp Psychiatry 2011;33:8–15. 10.1016/j.genhosppsych.2010.10.008 [DOI] [PubMed] [Google Scholar]
- 5. Fisher L, Skaff MM, Mullan JT, et al. A longitudinal study of affective and anxiety disorders, depressive affect and diabetes distress in adults with type 2 diabetes. Diabet Med 2008;25:1096–101. 10.1111/j.1464-5491.2008.02533.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Lin EHB, Von Korff M, Alonso J, et al. Mental disorders among persons with diabetes--results from the World Mental Health Surveys. J Psychosom Res 2008;65:571–80. 10.1016/j.jpsychores.2008.06.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Peyrot M, Rubin RR. Levels and risks of depression and anxiety symptomatology among diabetic adults. Diabetes Care 1997;20:585–90. 10.2337/diacare.20.4.585 [DOI] [PubMed] [Google Scholar]
- 8. Carroll D, Phillips AC, Thomas GN, et al. Generalized anxiety disorder is associated with metabolic syndrome in the Vietnam experience study. Biol Psychiatry 2009;66:91–3. 10.1016/j.biopsych.2009.02.020 [DOI] [PubMed] [Google Scholar]
- 9. Chaudhary R, Kumar P, Chopra A, et al. Comparative study of psychiatric manifestations among type I and type II diabetic patients. Indian J Psychol Med 2017;39:342–6. 10.4103/IJPSYM.IJPSYM_35_17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Smith KJ, Béland M, Clyde M, et al. Association of diabetes with anxiety: a systematic review and meta-analysis. J Psychosom Res 2013;74:89–99. 10.1016/j.jpsychores.2012.11.013 [DOI] [PubMed] [Google Scholar]
- 11. Chien I-C, Lin C-H. Increased risk of diabetes in patients with anxiety disorders: a population-based study. J Psychosom Res 2016;86:47–52. 10.1016/j.jpsychores.2016.05.003 [DOI] [PubMed] [Google Scholar]
- 12. Deschênes SS, Burns RJ, Schmitz N, et al. Associations between diabetes, major depressive disorder and generalized anxiety disorder comorbidity, and disability: findings from the 2012 Canadian Community Health Survey--Mental Health (CCHS-MH). J Psychosom Res 2015;78:137–42. 10.1016/j.jpsychores.2014.11.023 [DOI] [PubMed] [Google Scholar]
- 13. Remes O, Brayne C, van der Linde R, et al. A systematic review of reviews on the prevalence of anxiety disorders in adult populations. Brain Behav 2016;6:e00497 10.1002/brb3.497 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Hermanns N, Kulzer B, Krichbaum M, et al. Affective and anxiety disorders in a German sample of diabetic patients: prevalence, comorbidity and risk factors. Diabet Med 2005;22:293–300. 10.1111/j.1464-5491.2005.01414.x [DOI] [PubMed] [Google Scholar]
- 15. Maia ACCdeO, Braga AdeA, Brouwers A, et al. Prevalence of psychiatric disorders in patients with diabetes types 1 and 2. Compr Psychiatry 2012;53:1169–73. 10.1016/j.comppsych.2012.03.011 [DOI] [PubMed] [Google Scholar]
- 16. Grigsby AB, Anderson RJ, Freedland KE, et al. Prevalence of anxiety in adults with diabetes: a systematic review. J Psychosom Res 2002;53:1053–60. [DOI] [PubMed] [Google Scholar]
- 17. Berlin I, Bisserbe JC, Eiber R, et al. Phobic symptoms, particularly the fear of blood and injury, are associated with poor glycemic control in type I diabetic adults. Diabetes Care 1997;20:176–8. 10.2337/diacare.20.2.176 [DOI] [PubMed] [Google Scholar]
- 18. Kojima K, Mohamed S, Fujimaru Y, et al. Effects of both the emotional behavior and feeding conditions on the circulating plasma volume and plasma glucose levels in cats. Auton Neurosci 2000;86:58–64. 10.1016/S1566-0702(00)00236-8 [DOI] [PubMed] [Google Scholar]
- 19. Niemcryk SJ, Speers MA, Travis LB, et al. Psychosocial correlates of hemoglobin alc in young adults with type I diabetes. J Psychosom Res 1990;34:617–27. 10.1016/0022-3999(90)90105-D [DOI] [PubMed] [Google Scholar]
- 20. Turkat ID. Glycosylated hemoglobin levels in anxious and nonanxious diabetic patients. Psychosomatics 1982;23:1056–8. 10.1016/S0033-3182(82)73301-8 [DOI] [PubMed] [Google Scholar]
- 21. Tsai M-T, Erickson SR, Cohen LJ, et al. The association between comorbid anxiety disorders and the risk of stroke among patients with diabetes: an 11-year population-based retrospective cohort study. J Affect Disord 2016;202:178–86. 10.1016/j.jad.2016.03.060 [DOI] [PubMed] [Google Scholar]
- 22. Santos MABdos, Ceretta LB, Réus GZ, et al. Anxiety disorders are associated with quality of life impairment in patients with insulin-dependent type 2 diabetes: a case-control study. Braz J Psychiatry 2014;36:298–304. 10.1590/1516-4446-2013-1230 [DOI] [PubMed] [Google Scholar]
- 23. de Ornelas Maia ACC, Braga AdeA, Paes F, et al. Comorbidity of depression and anxiety: association with poor quality of life in type 1 and 2 diabetic patients. Clin Pract Epidemiol Ment Health 2013;9:136–41. 10.2174/1745017901309010136 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Rubin RR, Peyrot M. Psychological issues and treatments for people with diabetes. J Clin Psychol 2001;57:457–78. 10.1002/jclp.1041 [DOI] [PubMed] [Google Scholar]
- 25. Baumeister H, Hutter N, Bengel J. Psychological and pharmacological interventions for depression in patients with diabetes mellitus: an abridged cochrane review. Diabet Med 2014;31:773–86. 10.1111/dme.12452 [DOI] [PubMed] [Google Scholar]
- 26. Lustman PJ, Griffith LS, Clouse RE, et al. Effects of alprazolam on glucose regulation in diabetes. Results of double-blind, placebo-controlled trial. Diabetes Care 1995;18:1133–9. 10.2337/diacare.18.8.1133 [DOI] [PubMed] [Google Scholar]
- 27. Khuwaja AK, Lalani S, Dhanani R, et al. Anxiety and depression among outpatients with type 2 diabetes: a multi-centre study of prevalence and associated factors. Diabetol Metab Syndr 2010;2 10.1186/1758-5996-2-72 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Wittchen HU, Müller N, Pfister H, et al. [Affective, somatoform and anxiety disorders in Germany--initial results of an additional federal survey of "psychiatric disorders"]. Gesundheitswesen 1999;61 Spec No:S216–22. [PubMed] [Google Scholar]
- 29. Alosaimi FD, Alzain N, Asiri S, et al. Patterns of psychiatric diagnoses in inpatient and outpatient psychiatric settings in Saudi Arabia. Arch. Clin. Psychiatry 2017;44:77–83. 10.1590/0101-60830000000124 [DOI] [Google Scholar]
- 30. Mirghani HO, Elbadawi AS. Depression, anxiety, and daytime sleepiness among type 2 diabetic patients and their correlation with the diabetes control: A case-control study. J Taibah Univ Med Sci 2016;11:374–9. 10.1016/j.jtumed.2016.05.009 [DOI] [Google Scholar]
- 31. AlBekairy A, AbuRuz S, Alsabani B, et al. Exploring factors associated with depression and anxiety among hospitalized patients with type 2 diabetes mellitus. Med Princ Pract 2017;26:547–53. 10.1159/000484929 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Kiejna A, Piotrowski P, Adamowski T, et al. [The prevalence of common mental disorders in the population of adult Poles by sex and age structure - an EZOP Poland study]. Psychiatr Pol 2015;49:15–27. 10.12740/PP/30811 [DOI] [PubMed] [Google Scholar]
- 33. Volodina MN, Starostina EG, Moshnyaga EN, et al. Rasprostranennost' nepsihoticheskih psihicheskih rasstrojstv (NPR) pri saharnom diabete (SD). - V knige: Vzaimodejstvie specialistov v okazanii pomoshchi pri psihicheskih rasstrojstvah. Materialy obshcherossijskoj konferencii v ramkah Plenuma Pravleniya Rossijskogo obshchestva psihiatrov s uchastiem glavnyh psihiatrov i narkologov, rukovoditelej psihiatricheskih i narkologicheskih uchrezhdenij sub"ektov RF. - Otvetstvennyj redaktor Krasnov V.N 2009:13–14.
- 34. Starostina EG, Moshnyaga EN, Volodina MN, et al. Epidemiologiya naiboleye chastykh psikhicheskikh rasstroystv U bolnykh sakharnym diabetom. Almanakh klinicheskoy meditsiny 2014;32:17–23. [Google Scholar]
- 35. Lloyd CE, Nouwen A, Sartorius N, et al. Prevalence and correlates of depressive disorders in people with type 2 diabetes: results from the International prevalence and treatment of diabetes and depression (INTERPRET-DD) study, a collaborative study carried out in 14 countries. Diabet Med 2018;35:760–9. 10.1111/dme.13611 [DOI] [PubMed] [Google Scholar]
- 36. Lloyd CE, Sartorius N, Cimino LC, et al. The INTERPRET-DD study of diabetes and depression: a protocol. Diabet Med 2015;32:925–34. 10.1111/dme.12719 [DOI] [PubMed] [Google Scholar]
- 37. Sheehan DV, Lecrubier Y, Harnett Sheehan K, et al. The validity of the mini international neuropsychiatric interview (mini) according to the SCID-P and its reliability. European Psychiatry 1997;12:232–41. 10.1016/S0924-9338(97)83297-X [DOI] [Google Scholar]
- 38. Sheehan DV, Lecrubier Y, Sheehan KH, et al. The Mini-International neuropsychiatric interview (M.I.N.I.): the development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. J Clin Psychiatry 1998;59 Suppl 20:22–33. [PubMed] [Google Scholar]
- 39. IBM CR. Ibm SPSS statistics for windows, version 23.0. Armonk, NY: IBM Corp, 2015. [Google Scholar]
- 40. Li C, Barker L, Ford ES, et al. Diabetes and anxiety in US adults: findings from the 2006 behavioral risk factor surveillance system. Diabet Med 2008;25:878–81. 10.1111/j.1464-5491.2008.02477.x [DOI] [PubMed] [Google Scholar]
- 41. Thomas J, Jones G, Scarinci I, et al. A descriptive and comparative study of the prevalence of depressive and anxiety disorders in low-income adults with type 2 diabetes and other chronic illnesses. Diabetes Care 2003;26:2311–7. 10.2337/diacare.26.8.2311 [DOI] [PubMed] [Google Scholar]
- 42. Kessler RC, Angermeyer M, Anthony JC, et al. Lifetime prevalence and age-of-onset distributions of mental disorders in the world Health organization's world mental health survey initiative. World Psychiatry 2007;6:168–76. [PMC free article] [PubMed] [Google Scholar]
- 43. Trento M, Charrier L, Salassa M, et al. Depression, anxiety and cognitive function in patients with type 2 diabetes: an 8-year prospective observational study. Acta Diabetol 2015;52:1157–66. 10.1007/s00592-015-0806-0 [DOI] [PubMed] [Google Scholar]
- 44. Anderson RJ, Grigsby AB, Freedland KE, et al. Anxiety and poor glycemic control: a meta-analytic review of the literature. Int J Psychiatry Med 2002;32:235–47. 10.2190/KLGD-4H8D-4RYL-TWQ8 [DOI] [PubMed] [Google Scholar]
- 45. Zhang Y, Hu G, Yuan Z, et al. Glycosylated hemoglobin in relationship to cardiovascular outcomes and death in patients with type 2 diabetes: a systematic review and meta-analysis. PLoS One 2012;7:e42551 10.1371/journal.pone.0042551 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Iversen MM, Nefs G, Tell GS, et al. Anxiety and depressive symptoms as predictors of all-cause mortality among people with insulin-naïve type 2 diabetes: 17-year follow-up of the second Nord-Trøndelag health survey (HUNT2), Norway. PLoS One 2016;11:e0160861 10.1371/journal.pone.0160861 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Aschner P. New IDF clinical practice recommendations for managing type 2 diabetes in primary care. Diabetes Res Clin Pract 2017;132:170 10.1016/j.diabres.2017.09.002 [DOI] [PubMed] [Google Scholar]