Abstract
Chronic periapical abscess drains through a sinus tract either intraorally or extraorally. However, intraoral drainage is more common than extraoral in both dentitions. Nevertheless, the simultaneous presentation of extraoral and intraoral sinus tract is very rarely reported in primary dentition. This case report discussed the management of a girl aged 7 years with a chronic periapical abscess of tooth no. 85 with both non-healing extraoral and intraoral sinus tract having multiple stomata. Non-vital pulpectomy using calcium hydroxide paste intracanal dressing was performed initially until 2 weeks without remarkable healing; then antibiotic dressing consisting of a mixture of ciprofloxacin, metronidazole and clindamycin was placed as an intracanal medicament for 1 week, which shows uneventful healing of both intraoral and extraoral sinus tract. This case report clearly indicates about how history, correct diagnosis and appropriate treatment of endodontic infection associated with sinus tract can be conservatively healed with endodontic treatment alone.
Keywords: dentistry and oral medicine, infections
Background
The drainage of sinus tract either intraorally or extraorally depends on various factors such as the location of the involved tooth, position of the tooth’s apex to muscular attachments, virulence of the bacteria, decreased immunity of the host and least resistance provided by the structures underlying it.1
The chronic endodontic infection that will drain through an intraoral communication to the gingival surface is known as intraoral sinus tract. Surface opening of the sinus tract is known as stomata.2 Intraoral sinus tract usually has a single stoma. However, multiple draining sinuses either intraorally or extraorally apart from dental infection can also be seen in case of chronic suppurative osteomyelitis.3
Sinus tracts of odontogenic origin occurring extraorally presents a diagnostic challenge because of their distant location from the underlying source of infection and absence of any dental symptoms.4 These cutaneously discharging sinuses can appear as a papule or nodule with purulent discharge and their common site of location is on the chin, cheek, submandibular area and on rare occasion in the nasal region with mandibular teeth as more common source of infection than maxillary teeth.5–7 All of which further makes the diagnosis difficult for the clinician.
Furthermore, the chronicity of the lesion has often been worsened by the misdiagnosis, which could create significant effects on the facial aesthetics due to undesirable treatment such as frequent biopsies and antibiotics use resulting in the scarring of the skin.8 9 Therefore, thorough dental examination must be carried out for proper evaluation of all chronic draining sinus tracts of orofacial region.
Maintenance of primary teeth before normal exfoliation is necessary for the development of arch form, aesthetics, function, mastication and normal eruption of permanent teeth. Primary molars with a chronic discharging sinus can be preserved by carrying out a non-vital pulpectomy procedure. Pulpectomy is a procedure indicated for primary tooth that involves creation of an access to the root canal system followed by thorough cleaning, shaping and disinfection of the root canals, and then finally obturating the root canals using a resorbable root filling material.10 11 Once the causative factors related to the formation of the sinus tract are removed, the stoma and the sinus tract will close within several days.2
The following case report describes successful management of primary molar with both intraoral and extraoral sinus tracts by pulpectomy using calcium hydroxide paste initially for two consecutive weeks followed by use of an antibiotic dressing consisting of a mixture of ciprofloxacin, metronidazole and clindamycin as an intracanal medicament before obturation with resorbable sealer.
Case presentation
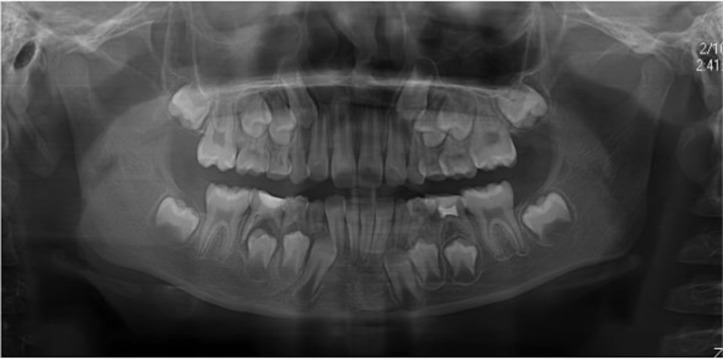
A girl aged 7 years reported to the Conservative Dentistry and Endodontics Department of Bangabandhu Sheikh Mujib Medical University (BSMMU) with the chief complaint of non-healing extraoral draining sinus on lower right cheek for 1 year. She gave history of multiple systemic antibiotic regimens along with curettage of the extraoral sinus tract. She had no significant medical history. On extraoral examination, an erythematous area of approximately 1.8×1 cm in diameter was found along the inferior right border of the mandible approximating the angle of mandible (figure 1A and B). The opening of the lesion was found closed by scab formation with no discharge of pus on palpation. On intraoral examination, the presence of a deep carious lesion on tooth no. 85 along with swelling and intraoral sinus tract draining through multiple stomata was found (figure 1C). Tooth no. 85 was found slightly sensitive to percussion and palpation with no mobility. She had also caries on teeth no. 74 and 75.
Figure 1.

(A) Extraoral cutaneous sinus tract. (B) Unhealthy granulation tissue, two stomata and erythematous surrounding skin clearly visible at the angle of jaw extraorally. (C) Tooth no. 85 showing large carious lesion and intraoral sinus tract with double stomata (arrow marked). (D) Healed intraoral sinus tract. (E) Healed extraoral sinus tract at 3 months follow-up visit. (F) Healed sinus with surrounding normal skin extraorally after 6 months, only scar mark is present.
Investigations
Intraoral periapical radiograph: it revealed the presence of diffuse inter-radicular radiolucency extending periapically in relation to tooth no. 85.
Sinus tract tracing using gutta-percha (GP): the source of the lesion (sinus) was determined radiographically using a GP point (figure 2A). The radiograph showed a GP point extending into the furcation area of tooth no. 85 and confirmed it as the source of draining sinus. The lesion in the furcation area might have occurred due to extension of infection from the pulp chamber into the inter-radicular bone either via furcation canals and lateral canals or through the porosities of the dentin and cementum of the pulpal floor.
Figure 2.
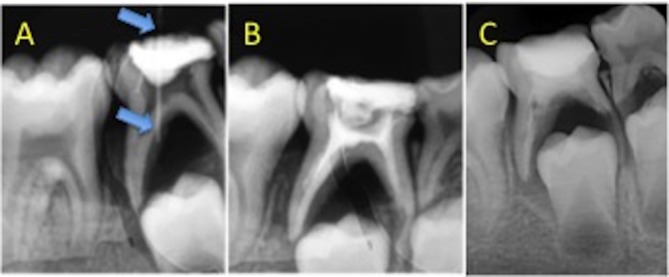
(A) Intraoral periapical X-ray showing intraoral sinus tract, traced with Gutta-percha (GP), arrow indicating the radiographic image of inserted GP reaching up to furcal area. (B) Postobturation radiograph. (C) Follow-up X-ray after 1 year with complete healing of periapical bone.
Differential diagnosis
Furuncle, chronic osteomyelitis.
Treatment
A treatment plan of a non-vital pulpectomy procedure was made which was explained to the parents. After getting consent from the parents, endodontic treatment was initiated without giving local anaesthesia considering the tooth as a non-vital. A straight line access cavity was made. The canals were negotiated followed by the establishment of the working length. Initially, coronal flaring of each canal was done with universal ProTaper Sx file. Then, cleaning and shaping of the root canals were done up to #40 K-file followed by copious irrigation with the alternate use of normal saline and 1% sodium hypochlorite (NaOCl). A high vacuum suction device with special type of suction tip, which can be inserted directly into the access cavity thereby preventing the overflow, was used for irrigation throughout the procedure (figure 3A, B and C). The canals were dried using paper points followed by application of calcium hydroxide (Ca(OH)2) dressing. Sealing of the access cavity was done with zinc oxide eugenol cement. Patient was advised for follow-up after 2 weeks. After 2 weeks there was no remarkable healing. Further biomechanical preparation was started at that appointment where each of the canals was instrumented up to size #60 H-file with copious irrigation using normal saline and 1% NaOCl. After drying the canals with paper points, antibiotic dressing consisting of a mixture of ciprofloxacin, metronidazole and clindamycin was made and placed inside the canals using lentulospiral. Again sealing of the access cavity was done with zinc oxide eugenol cement. In the subsequent appointment after 1 week, healing of intraoral sinus tract was evident with no symptoms. At this appointment, the antibiotic paste was washed out from the canals followed by drying of the canals using paper points. Finally, the canals were obturated using zinc oxide eugenol sealer followed by placement of glass ionomer restoration (figure 2B).
Figure 3.
(A) Commercially available microsuction device used for irrigation purpose. (B) Microsuction constructed by adapting a needle onto the saliva ejector. (C) Magnified view of adapted microsuction tip used for suctioning irrigating solution directly from pulp chamber/canals.
Outcome and follow-up
The patient was advised for recall visit after 3, 6 and 12 months interval. Proper healing was observed at 3 months follow-up visit (figure 1D and E) and finally, further 1-year follow-up revealed no recurrence (figure 2C and 4).
Figure 4.
Follow-up OPG X-ray after 1 year with complete healing of periapical bone.
Discussion
Chronic periapical abscess in primary dentition commonly drains via the intraoral sinus tract. However, occasionally a necrosed primary tooth can drain via extraoral cutaneous sinus tract.12 13 Chronic periapical abscess in primary dentition draining simultaneously through intraoral and extraoral sinus tract is a very rare condition which is until now not reported by any study. Thus, abscess draining through extraoral and intraoral sinus along with expression of pus through multiple stomata intraorally made the present case extremely atypical.
The presence of simultaneous presentation of both intraoral and extraoral sinus tract, in this case, is thought to be due to previous antibiotic therapy and surgical curettage, which could have partially blocked the drainage pathways through partial healing and thus finally making intraoral drainage pathways with multiple patent stomata.
Whenever a draining lesion is seen on the skin of the face, consider an endodontic origin in the differential diagnosis. Also include chronic periapical abscess, furuncle, osteomyelitis, congenital fistula, pyogenic granuloma, salivary gland fistula, deep mycotic infection and infected cyst in the differential diagnosis.14 While the cause of intraoral sinus tracts can be detected easily, incorrect diagnosis is more common in extraoral sinus tracts. One of the reasons for incorrect diagnosis is the patient’s initial presentation to a general surgeon or dermatologist, instead of a dental practitioner. Misdiagnosis, unnecessary antibiotic treatment and surgical interventions are commonly seen due to such conditions,15 especially due to failure to take advice and consultation from appropriate specialist or general dental practitioners, no matter dental symptoms are present or absent.16 In the present case, a differential diagnosis of furuncle and chronic osteomyelitis were considered. The diagnosis of furuncle was excluded considering the lesion as painless; absence of red, inflamed and tender bump with no history of spontaneous remission, fever and lymphadenopathy.17 Also, considering the patient’s medical fitness with no history of fever and regional lymphadenopathy along with the absence of any bony sequestra in the mandible as seen in preoperative intraoral radiograph and postoperative orthopantomograph (OPG) after 1 year (figure 4) helps to exclude the diagnosis of chronic osteomyelitis.3
Previously, these sinus tracts were thought to be lined by epithelium and therefore there was concept for using surgical intervention apart from endodontic treatment.18 However, recent studies suggested it to be lined by granulation tissue and not epithelium, which means that non-surgical endodontic treatment as supported by the success of the present case study will be the treatment of choice for draining sinuses either intraorally or extraorally.19
Pulpectomy is a procedure similar to root canal procedure indicated for primary teeth with irreversibly inflamed or necrotic pulp tissue either due to caries or trauma.
The prognosis of pulpectomy depends on the amount of remaining supporting bone. Extraction should be opted as an alternative if in case there is remarkable bone loss and root resorption. Although the case presented here shows large inter-radicular bone loss, the presence of intact surrounding bone and minimal resorption of distal root with less than half resorption of mesial root made this case preferable to pulpectomy rather than for extraction. Furthermore, besides the consideration of age and need for preserving the primary tooth before normal exfoliation time, the availability of better irrigants and intracanal medicaments which increases the success of pulpectomy by providing a better means of canal disinfection also helps to choose pulpectomy as a treatment of choice over extraction for this case.2 11 20
The endodontic treatment’s success depends on through cleaning, shaping, disinfection and three-dimensional filling of the root canals. Until now among the various available irrigating solution, NaOCl is considered as the primary irrigating solution because of its tissue dissolving property and potent antimicrobial activity.11 So NaOCl was chosen as an irrigating solution to achieve better cleaning and disinfection of the primary molar tooth root canals where many pulpal ramifications such as intercommunicating canals, lateral canals and accessory canals are present, which cannot be reached mechanically.2 Nevertheless, irrigation throughout the procedure was performed with 1% NaOCl using high vacuum suction device with special type of suction tip, which can be inserted directly into the access cavity thereby preventing the overflow.21 Moreover, diluting the NaOCl solution to 1%, and application of side venting needle and avoiding forceful injection of NaOCl, all were the precautions taken to prevent the risk of damage both the surrounding soft tissues as well as underlying permanent tooth germ by diffusing through the apex.2 11
Various medicaments are available to be used as intracanal medicament in primary teeth such as formocresol, Ca(OH)2 and triple antibiotic paste. Formocresol though having excellent antimicrobial property tends to have toxic effects on the body through diffusion of its vapour beyond the apex. Furthermore, due to carcinogenic nature of these medicaments, the use of these chemicals is contraindicated in modern paediatric endodontic treatment.22 Ca(OH)2 is the preferred intracanal medicament for disinfection of endodontic pathogens for both dentitions because it possesses broad-spectrum antibacterial activity, better stability for long periods, good biocompatibility and can dissolve necrotic tissue remnants and bacteria and their by-products. However, Ca(OH)2 is found not effective against Enterococcus faecalis and Candida albicans.2 11 Alternative to Ca(OH)2, the triple antibiotic paste consisting of mixture of ciprofloxacin, metronidazole and minocycline has been advocated as the intracanal medicament, which is found to have exceptional antimicrobic activity including E. faecalis and C. albicans. 23–25
Niigata University School of Dentistry, Japan suggested the first use of triple antibiotic paste in the management of chronic infected primary molar as lesion sterilisation and tissue repair (LSTR) therapy, which has been proved to attain 100% sterility in the root canal system.26–29 This technique involves only debriding the pulp chamber of chronically infected primary teeth and placing medicament (ciprofloxacin, metronidazole and minocycline) near the root orifice without preparing the radicular portion. The efficiency of medicament depends on the type of vehicle used such as macrogol and propylene glycol (3MIX-MP). These vehicles carry the medicament deep into the dentinal tubules, thus aid in effective eradication of bacteria.30 Present case report in contrast to LSTR technique involves complete cleaning and shaping of the root canals followed by the placement of antibiotic paste containing mixture of ciprofloxacin, metronidazole and clindamycin paste as an intracanal dressing for 1 week before obturation. The symptoms were resolved after 1 week of its application. Metronidazole was chosen as the first choice among the antibacterial drugs as obligate anaerobes are found in the deep layers of the infected dentine of the root canal wall. According to study, it has been demonstrated that metronidazole can penetrate the deep layers of carious lesions and disinfect the lesions in vivo and diffuse throughout the dentine.31 32 As the root canal with a periradicular lesion consists of complex nature of bacterial flora, metronidazole alone cannot kill all bacteria necessitating the need for other drugs to sterilise the infected root dentine. Thus, ciprofloxacin and clindamycin, in addition to metronidazole were required to sterilise the infected root dentine. Ciprofloxacin is effective against Gram-negative organisms with bacteriocidal mode of action.33 Clindamycin shows excellent antimicrobial activity against Gram-positive organisms, including anaerobes and β-lactamase-producing strains; and can achieve high levels in bone, gingival crevicular fluid and saliva. Moreover, clindamycin can also inhibit bacterial toxins, proteins, enzymes and cytokines.34 35 Using a combination of antibiotics is also believed to decrease the chance of development of microbial resistance.30 36 Thus, achievement of excellent clinical results37 can be expected as was found in this case report by using the combination of antibiotics.
Learning points.
Periapical abscess in primary tooth can rarely be present with both intraoral and extraoral sinus tract.
Even though there are various causes of extraoral cutaneous sinus tract, the medical practitioner must be alert about its dental aetiology.
Establishment of a good communication between the medical practitioner and the dental surgeon is very much essential for appropriate diagnosis and treatment of such rare cases.
Cleaning, shaping and combination of antibiotics as an intracanal medicament before obturation can heal the persistent sinus tract.
Footnotes
Contributors: AKMB, KA and GKC were involved in conception and design, acquisition of data or analysis, interpretation of data and drafting of the article. AR contributed actively in revising it critically for important intellectual content and final approval of the version along with the other coauthors.
Funding: The authors have notdeclared a specific grant for this research from any funding agencyin the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Patient consent for publication: Obtained.
References
- 1. Pasternak-Júnior B, Teixeira CS, Silva-Sousa YT, et al. . Diagnosis and treatment of odontogenic cutaneous sinus tracts of endodontic origin: three case studies. Int Endod J 2009;42:271–6. 10.1111/j.1365-2591.2008.01519.x [DOI] [PubMed] [Google Scholar]
- 2. Hargreaves KM, Berman LH. Cohen’s pathways of the pulp. 11th edition: Elsevier, 2016:12–13. [Google Scholar]
- 3. Malik NA. Textbook of Oral and Maxillofacial Surgery. 3rd edition New Delhi 110 002, India: Jaypee Brothers Medical Publishers Limited, 2012. [Google Scholar]
- 4. Mittal N, Gupta P. Management of extra oral sinus cases: a clinical dilemma. J Endod 2004;30:541–7. 10.1097/00004770-200407000-00019 [DOI] [PubMed] [Google Scholar]
- 5. Heling I, Rotstein I. A persistent oronasal sinus tract of endodontic origin. J Endod 1989;15:132–4. 10.1016/S0099-2399(89)80135-9 [DOI] [PubMed] [Google Scholar]
- 6. Mishra R, Khan TS. Cutaneous sinus tract in association with traumatic injury to the teeth. Int J Clin Pediatr Dent 2013;6:205–7. 10.5005/jp-journals-10005-1220 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. McWalter GM, Alexander JB, del Rio CE, et al. . Cutaneous sinus tracts of dental etiology. Oral Surg Oral Med Oral Pathol 1988;66:608–14. 10.1016/0030-4220(88)90384-2 [DOI] [PubMed] [Google Scholar]
- 8. Cantatore JL, Klein PA, Lieblich LM. Cutaneous dental sinus tract, a common misdiagnosis: a case report and review of the literature. Cutis 2002;70:264–5. [PubMed] [Google Scholar]
- 9. Badole GP, Kubde R, Gunwal M, et al. . Nonsurgical Management of Cutaneous Sinus Tract of Odontogenic Origin: A Case Report. Global Journal of Medical Research: J Dentistry and Otolaryngology 2014;14:23–5. [Google Scholar]
- 10. Welbury R, Duggal MS, Hosey MT. Paediatric Dentistry. 4th edition: Oxford university press, 2012:138–9. [Google Scholar]
- 11. Ingle JI, Slavkin HC, Milledge JT. Endodontic therapy for primary teeth Ingle’s Endodontics. 6th edition Canada: Hamilton, OntarioBC Decker, 2008:1400–30. [Google Scholar]
- 12. Uppal A, Thakur S, Chauhan D, et al. . Extraoral cutaneous sinus tracts of dental origin: A report of two pedodontic cases. International Dental & Medical Journal of Advanced Research - VOLUME 2015 2017;3:1–4. 10.15713/ins.idmjar.71 [DOI] [Google Scholar]
- 13. Nikhilraj SP, Chatra L, Veena KM, et al. . Dentoalvolar abscess with extra oral sinus in a pediatric patient: a case report. Pacific journal of medical sciences 2014;13:36–40. [Google Scholar]
- 14. Abuabara A, Schramm CA, Zielak JC, et al. . Dental infection simulating skin lesion. An Bras Dermatol 2012;87:619–21. 10.1590/S0365-05962012000400017 [DOI] [PubMed] [Google Scholar]
- 15. Salamat K, Rezai RF. Nonsurgical treatment of extraoral lesions caused by necrotic nonvital tooth. Oral Surg Oral Med Oral Pathol 1986;61:618–23. 10.1016/0030-4220(86)90107-6 [DOI] [PubMed] [Google Scholar]
- 16. Deepa C, Srinath KS, Roopa KS. Conservative management of cutaneous facial sinus tract of odontogenic origin: a case report. J Evol Med Dent Sci 2013;2:5728–32. [Google Scholar]
- 17. Habif TP. Furuncles and carbuncles Clinical Dermatology: A Color Guide to Diagnosis and Therapy. 4th edition Mosby: Philadelphia PA. [Google Scholar]
- 18. Thoma KH, Surgery O. St Louis. 4th edn USA: Mosby, 1963:733. [Google Scholar]
- 19. Grossman LI. Endodontic Practice. 10th edn Philadelphia, PA: Lea and Febiger, 1981:84–111. [Google Scholar]
- 20. Guideline on Pulp Therapy for Primary and Immature Permanent Teeth. American Association of Paediatric Dentistry. 37, 1991:244–52. [PubMed] [Google Scholar]
- 21. Hülsmann M. Prevention and management of problems during root canal treatment – A problem-based approach to root canal treatment Part I. ENDO 2016;10:127–40. [Google Scholar]
- 22. Deshpande A, Sudani U. Intracanal medicament in Pediatric Endodontics: A Literature Review. J Adv Med Dent Scie Res 2015;3:63–8. [Google Scholar]
- 23. Reddy GA, Sridevi E, Sai Sankar AJ, et al. . Endodontic treatment of chronically infected primary teeth using triple antibiotic paste: An in vivo study. J Conserv Dent 2017;20:405–10. 10.4103/JCD.JCD_161_17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Kaur M, Kendre S, Gupta P, et al. . Comparative Evaluation of Anti Microbial effects of Triple Antibiotic Paste and Amox and its derivatives against E. Faecalis: An in vitro study. J ClinExp Dent 2017;9(6:e799–e804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Shaik J, Garlapati R, Nagesh B, et al. . Comparative evaluation of antimicrobial efficacy of triple antibiotic paste and calcium hydroxide using chitosan as carrier against Candida albicans and Enterococcus faecalis: An in vitro study. J Conserv Dent 2014;17:335–9. 10.4103/0972-0707.136444 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Nakornchai S, Banditsing P, Visetratana N. Clinical evaluation of 3Mix and Vitapex as treatment options for pulpally involved primary molars. Int J Paediatr Dent 2010;20:214–21. 10.1111/j.1365-263X.2010.01044.x [DOI] [PubMed] [Google Scholar]
- 27. Takushige T, Cruz EV, Asgor Moral A, et al. . Endodontic treatment of primary teeth using a combination of antibacterial drugs. Int Endod J 2004;37:132–8. 10.1111/j.0143-2885.2004.00771.x [DOI] [PubMed] [Google Scholar]
- 28. Hoshino E, Kurihara-Ando N, Sato I, et al. . In-vitro antibacterial susceptibility of bacteria taken from infected root dentine to a mixture of ciprofloxacin, metronidazole and minocycline. Int Endod J 1996;29:125–30. 10.1111/j.1365-2591.1996.tb01173.x [DOI] [PubMed] [Google Scholar]
- 29. Divya S, Retnakumari N. Lesion sterilisation and tissue repair in primary teeth with periapical pathosis – A case series. IOSR J Dent Med Sci 2014;13:7–11. [Google Scholar]
- 30. Cruz EV, Kota K, Huque J, et al. . Penetration of propylene glycol into dentine. Int Endod J 2002;35:330–6. 10.1046/j.1365-2591.2002.00482.x [DOI] [PubMed] [Google Scholar]
- 31. Goomer P, Jain RL. Non-surgical endodontic treatment of extraoral sinus with triple antibiotic paste and mineral trioxide aggregate obturation. Indian Journal of Oral Sciences 2013;4:95–8. 10.4103/0976-6944.119934 [DOI] [Google Scholar]
- 32. Taneja S, Kumari M, Parkash H. Nonsurgical healing of large periradicular lesions using a triple antibiotic paste: A case series. Contemp Clin Dent 2010;1:31–5. 10.4103/0976-237X.62519 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Vijayaraghavan R, Mathian VM, Sundaram AM, et al. . Triple antibiotic paste in root canal therapy. J Pharm Bioallied Sci 2012;4:230–3. 10.4103/0975-7406.100214 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Shweta PSK. Dental abscess: A microbiological review. Dental Research Journal 2013;10:585–91. [PMC free article] [PubMed] [Google Scholar]
- 35. Gemmell CG, Amir MKA. Effect of certain antibiotics on the formation of cellular antigens and extracellular products by group A streptococci Parker MT, Pathogenic streptococci. Chertsey: Reed Books, 1979:67–8. [Google Scholar]
- 36. Sato I, Ando-Kurihara N, Kota K, et al. . Sterilization of infected root-canal dentine by topical application of a mixture of ciprofloxacin, metronidazole and minocycline in situ. Int Endod J 1996;29:118–24. 10.1111/j.1365-2591.1996.tb01172.x [DOI] [PubMed] [Google Scholar]
- 37. Manuel ST, Parolia A, Kundabala M, et al. . Non-surgical endodontic therapy using triple-antibiotic paste. Kaen Dent J 2010;33:2. [Google Scholar]