Abstract
In direct-to-consumer telemedicine, physicians treat patients through real-time, audio-visual conferencing for common conditions such as acute respiratory infections. Early studies had mixed findings on the quality of care provided during direct-to-consumer telemedicine and were limited by small sample sizes and narrow geographic scopes. Using 2015–16 claims data from a large national commercial insurer, we examined the quality of antibiotic management in adults with acute respiratory infection diagnoses at 38,839 direct-to-consumer telemedicine visits compared to 942,613 matched primary care office visits and 186,016 matched urgent care visits. In the matched analyses, we found clinically similar rates of antibiotic use, broad-spectrum antibiotic use, and guideline-concordant antibiotic management. However, direct-to-consumer telemedicine visits had less appropriate streptococcal testing and higher frequency of follow-up visits. These results suggest specific opportunities for improvement in direct-to-consumer telemedicine quality.
Through real-time direct-to-consumer telemedicine, patients can use their own telephones or computers to access care 24 hours a day, 7 days a week from remote providers employed by national, commercial companies. In the US, the direct-to-consumer telemedicine market is dominated by three commercial telemedicine companies: American Well, TelaDoc, and Doctor on Demand.(1) Use of direct-to-consumer telemedicine is rapidly growing with an estimated 7 million users in 2018.(2) Among large employers, 96% have added some telemedicine as a covered benefit,(3) and many large national insurers have contracted for services with specific direct-to-consumer telemedicine companies. Employers hope that direct-to-consumer telemedicine coverage will result in less time away from work, increased access to those in underserved communities, and potential savings when direct-to-consumer telemedicine is used as a lower-cost alternative to emergency department (ED) or urgent care visits.(4)
While use of direct-to-consumer telemedicine continues to rise, physician groups have raised concerns about the quality of care provided. Commercial direct-to-consumer telemedicine physicians do not generally have ongoing relationships with patients, access to past records, or ability to obtain certain lab tests. The care is also limited by the extent of the physical exams that can take place through telephone or personal computer. Some visits are audio-only, and visits that do incorporate video are still limited in clinical evaluation capabilities compared to other telemedicine models, which may incorporate peripheral devices, such as tele-stethoscopes, to enhance exam capabilities.(5) Limited continuity of care and examination capabilities could increase clinical uncertainty, which may foster inappropriate antibiotic management, even for commonly treated illnesses such as acute respiratory infections. Early studies of direct-to-consumer telemedicine visit quality had mixed findings regarding use of antibiotics and appropriate testing,(6, 7) but these studies were limited by narrow geographic scope, small sample sizes, and data from the initial expansion of direct-to-consumer telemedicine. Therefore, the current quality of care during direct-to-consumer telemedicine visits remains unknown.
To address this knowledge gap, we used 2015–16 commercial claims data from a large national insurer to compare the quality of acute respiratory infection care at nearly 40 thousand direct-to-consumer telemedicine visits to matched primary care physician (PCP) and urgent care visits. We focused on acute respiratory infection visits such as acute otitis media, sinusitis, and viral pharyngitis because these are the most common conditions treated at direct-to-consumer telemedicine.(8) We compared direct-to-consumer telemedicine visits to both PCP and urgent care visits because these are two common alternative sites of care for acute respiratory infections. Quality of care was assessed via five measures: antibiotic use, broad-spectrum antibiotic use, guideline concordance of antibiotic management, appropriate streptococcal testing, and frequency of follow-up visits.
Study Data And Methods
Study Population.
We conducted a retrospective cohort study using claims data from 2015–16 from a large national commercial insurer that provided coverage for beneficiaries for real-time audio and audio-visual direct-to-consumer telemedicine visits. Our analyses were limited to adults between 18 to 64 years old who had pharmaceutical coverage at the time of their visit.
Defining Acute Respiratory Infection Episodes.
Based on prior work,(9–11) acute respiratory infection visits were defined using the International Classification of Diseases, 9th Revision, Clinical Modification (ICD-9-CM) diagnosis codes. ICD-10 codes were converted back into ICD-9 codes using a modified crosswalk from the Centers for Medicare and Medicaid Services.(12) A comparison of diagnoses before and after ICD-10 implementation is shown in online Appendix Exhibit A1.(13) Consistent with previous studies,(9–11, 14, 15) we categorized each acute respiratory infection diagnosis into one of two broad groups: diagnoses where antibiotics may be indicated (sinusitis [461.X], streptococcal pharyngitis [034.X], and otitis media [382.X]), and diagnoses where antibiotics are not indicated (bronchitis/bronchiolitis [490.X, 466.X] and “other viral acute respiratory infections”, which included non-suppurative otitis [381.X], acute nasopharyngitis [460.X], pharyngitis [462.X], tonsillitis [463.X], laryngitis [464.X], acute URI [465.X], and viral pneumonia [480.x]). Visits for bacterial pneumonia [481.X-483.X, 485.X-486.X] were excluded because of the small number of direct-to-consumer telemedicine visits (n=109).
We identified new acute respiratory infection episodes by identifying “index” acute respiratory infection visits.(7, 16) Index acute respiratory infection visits were visits with no acute respiratory infection visits in the preceding 21 days (see Appendix Exhibit A2, for a flow diagram of included visits)(13). Additional acute respiratory infection visits in the 21 days after an index visit were counted as follow-up visits. We removed episodes in which the initial visit included competing acute diagnoses (e.g., urinary tract infection) or chronic comorbidities (e.g., chronic obstructive pulmonary disease) that might impact antibiotic management decisions (n=109,363; 7.5%)(9,11) (See Appendix Exhibit A3 for a complete list of diagnoses.)(13). Acute respiratory infection episodes with multiple visits to different settings on the index visit date (n=892; <0.1%) were excluded because we were unable to determine which visit occurred first. Episodes with an inpatient visit on the day of or the day after the index visit (n=1,195; 0.1%) were excluded due to our interest in outpatient antibiotic management. Finally, we excluded 15,290 visits (1.1%) with missing demographic data.
Determining Setting of Care.
We focused on index visits to direct-to-consumer telemedicine, PCP, or urgent care. Using previously published methods,(17) we identified visits to direct-to-consumer telemedicine and urgent care through place of service codes, provider specialty codes, Current Procedural Terminology (CPT) codes, organizational national provider identifiers, and billing and servicing tax identification numbers (TIN). Among identified telemedicine visits, we specifically limited analyses to commercial direct-to-consumer telemedicine companies, identified through TINs (listed in Appendix Exhibit A4)(13). PCP visits were identified with both outpatient CPT codes (such as 99201–99205, 99211–99215) and specialty codes indicating a primary care physician, nurse practitioner, or physician assistant (such as internal medicine, family practice, general practice, or general pediatrics). Acute respiratory infection episodes with index visits to other settings (such as EDs, retail clinics, or specialty physician offices) were not included.
Measuring Quality of Antibiotic Management.
We focused on three measures of antibiotic management: any antibiotic use, broad-spectrum antibiotic use, and guideline-concordant antibiotic management.
We examined pharmaceutical claims filled on the day of the index visit and the subsequent two days, and linked these to the index visit.(7, 18, 19) We included systemic (e.g., oral, intramuscular) antibiotic pharmaceutical claims, but excluded topical, ophthalmic, or otic antibiotics in order to examine antibiotic concordance with guidelines for systemic antibiotic use []. Prior studies are not entirely consistent in their definition of broad-spectrum antibiotics.(7, 20–25) Based on prior studies and guidelines for included diagnoses, broad-spectrum antibiotics were defined as macrolides (excluding erythromycin), fluoroquinolones, and non-first-generation cephalosporins. Our measures of any antibiotic use and broad-spectrum antibiotic use were assessed regardless of diagnosis, making these measures agnostic to given diagnosis. In contrast, guideline concordance was assessed in relation to diagnoses given at each visit.
To assess guideline concordance of antibiotic management, we built off prior research (11, 26) and professional society guidelines.(27–31) Visits with diagnoses where antibiotics may be indicted (sinusitis, streptococcal pharyngitis, otitis media) were categorized into three groups: guideline-concordant antibiotic use, guideline non-concordant antibiotic use, or no antibiotic use.(11, 26) Guideline non-concordant antibiotic use was defined as receipt of systemic antibiotic other than guideline-concordant antibiotics appropriate for the given diagnosis (see Appendix Exhibit A5 for further details of visit categorization)(13). Visits for diagnoses where antibiotic are not indicated (bronchitis/bronchiolitis, other viral acute respiratory infections) were categorized into unnecessary antibiotic use or guideline-concordant non-use of antibiotics (i.e. the appropriate lack of antibiotic prescriptions).(31) Building on previous studies(11, 26) and specific guidelines, antibiotic management for each visit was classified as guideline-concordant as follows: guideline-concordant antibiotic use for the diagnosis of streptococcal pharyngitis;(27) guideline-concordant antibiotic use or no antibiotic use for diagnoses of sinusitis or acute otitis media;(28, 29) or appropriate non-use of antibiotics for bronchitis or other viral URIs.
When an index visit included a diagnosis that may require antibiotics along with a viral diagnosis (e.g., acute otitis media and upper respiratory infection), guideline concordance was determined based on the diagnosis that may require antibiotics. Additionally, 1.0% of acute respiratory infection index visits had more than one diagnosis that may require antibiotics (e.g., sinusitis and streptococcal pharyngitis). In this situation, we considered the visit to have guideline-concordant antibiotic management if the visit had guideline-concordant antibiotic use for at least one of the diagnoses. For visits with diagnoses of both sinusitis and acute otitis media, no antibiotic use was also considered guideline-concordant antibiotic management.
Measuring streptococcal testing and follow up visits.
As secondary outcomes, we examined the occurrence of streptococcal testing within 2 days of index visits with a streptococcal pharyngitis diagnosis,(27) and follow-up visits within 2 and 21 days of the index visit.(8, 32, 33)
Patient and visit characteristics.
We identified patient sex, age, and participation in high-deductible health plans (HDHP versus non-HDHP) from insurance medical claims. Based on ZIP code of residence, we categorized the level of urbanicity into metropolitan, micropolitan, and small town/rural.(34) Geographic regions (Northeast, South, Midwest, and West) were also determined from ZIP code data. Presence versus absence of a chronic medical condition was determined by applying the Charlson Comorbidity Index, which identifies several specific chronic conditions.
Matching.
To address potential selection biases among patients and conditions across these three settings, we matched direct-to-consumer telemedicine visits to PCP and urgent care visits using coarsened-exact matching.(35) Visits were matched on age category, sex, presence/absence of chronic conditions, state, urbanicity of ZIP code, high-deductible health plan status, and diagnosis category (e.g., sinusitis, bronchitis/bronchiolitis). Through coarsened-exact matching, each direct-to-consumer telemedicine visit was matched to multiple PCP and urgent care visits, and each visit in these sets was weighted such that each set had the same weight.
Statistical analysis.
We first described patient and diagnosis characteristics in the unmatched and the matched weighted sample. Using chi-square tests, we compared direct-to-consumer telemedicine visits to PCP visits and separately to urgent care visits for each of the three main outcomes: antibiotic use, broad-spectrum antibiotic use, and guideline-concordant antibiotic management. We also compared these outcomes by diagnosis across the three care settings. Finally, we compared streptococcal testing rates and follow-up visit rates for direct-to-consumer telemedicine visits to PCP and urgent care visits.
As a sensitivity analysis, we used an alternative definition for guideline-concordant antibiotic management, now including only guideline-concordant antibiotic use among visits where antibiotics may be appropriate and guideline-concordant antibiotic non-use among visits where antibiotics are not indicated. Because it can often be guideline-concordant to not treat sinusitis and otitis media with antibiotics,(28, 29) we considered no antibiotic use to be guideline-concordant for these diagnoses in our main analysis, but not in this sensitivity analysis.
We used SAS, version 9.4 for analyses (SAS Institute, Inc., Cary, North Carolina) with 2-sided p values <0.05 considered significant. This study was reviewed by our institution’s Institutional Review Board and determined to be exempt.
Limitations.
Because this analysis used administrative data, we do not have additional sociodemographic or clinical data, such as race/ethnicity and illness severity. We used coarsened-exact matching to address differences in observed characteristics, but differences in other unobserved characteristics could influence antibiotic management across settings. Additionally, our data did not include information on drug allergies, which could render alternative antibiotics appropriate. For example, if individuals with antibiotic allergies preferentially saw PCPs, this may bias our comparison of guideline concordance between direct-to-consumer telemedicine and PCP visits. We also note that retail clinics, which have different antibiotic use than either PCP or urgent care facilities(15) were not included in this analysis. Our analysis focused on antibiotic use during reimbursed visits within a commercially insured population; results for other populations, such as those covered by Medicaid or those paying out of pocket for care, may differ. Similarly, claims data do not include antibiotics that are paid for out of pocket. This may bias our results if patients self-pay for antibiotics differentially across studied settings.
Study Results
From 2015 to 2016, there were 39,974 direct-to-consumer telemedicine visits, 1,084,056 PCP visits, and 212,837 urgent care visits in the unmatched acute respiratory infection sample (Exhibit 1). Patients treated at direct-to-consumer telemedicine visits were more likely to be younger, enrolled in a high-deductible health plan, and live in the South compared to patients visiting a PCP. Compared to patients at PCP or urgent care, direct-to-consumer telemedicine patients were more likely to receive a diagnosis of sinusitis (42% vs 31% PCP visits, 29% urgent care, p<0.001, both comparisons), and less likely to receive a diagnosis of an “other” viral acute respiratory infection (in which antibiotics are not indicated) (40% vs 45% PCP visits, 44% urgent care, p<0.001, both).
Exhibit 1:
Acute Respiratory Infections Visits to Direct to Consumer Telemedicine, Primary Care Providers, and Urgent Care Facilitites in the Unmatched and Matched Samples, 2015–16
| Unmatched Visitsd | Matched Visitse | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| DTC Telemedicine | PCP | Urgent Care | DTC Telemedicine | PCP | Urgent Care | |||||||
| Overall (N) | 39,974 | 1,084,056 | 212,837 | 38,839 | 942,613 | 186,016 | ||||||
| Age Category | ||||||||||||
| 18–34 years old | 12,979 | 32 | 360,129 | 33 | 92,369 | 43 | 12,752 | 33 | 309,488 | 33 | 61,075 | 33 |
| 35–44 years old | 12,637 | 32 | 248,321 | 23 | 53,185 | 25 | 12,289 | 32 | 298,251 | 32 | 58,857 | 32 |
| 45–54 years old | 9,213 | 23 | 250,865 | 23 | 39,714 | 19 | 8,848 | 23 | 214,739 | 23 | 42,377 | 23 |
| 55–64 years old | 5,145 | 13 | 224,741 | 21 | 27,569 | 13 | 4,950 | 13 | 120,135 | 13 | 23,708 | 13 |
| Gender | ||||||||||||
| Female | 25,271 | 63 | 680,629 | 63f | 130,061 | 61 | 24,627 | 63 | 597,691 | 63 | 117,949 | 63 |
| Male | 14,703 | 37 | 403,427 | 37 f | 82,776 | 39 | 14,212 | 37 | 344,922 | 37 | 68,067 | 37 |
| Chronic Illness Presencea | ||||||||||||
| No Chronic Illness | 30,730 | 77 | 751,140 | 69 | 161,572 | 76 | 30,029 | 77 | 728,796 | 77 | 143,821 | 77 |
| Chronic Illness | 9,244 | 23 | 332,916 | 31 | 51,265 | 24 | 8,810 | 23 | 213,817 | 23 | 42,195 | 23 |
| Rural/Urban | ||||||||||||
| Metropolitan | 37,407 | 94 | 981,430 | 91 | 198,974 | 93 | 37,007 | 95 | 898,151 | 95 | 177,242 | 95 |
| Micropolitan | 1,615 | 4 | 61,633 | 6 | 9,783 | 5 | 1,316 | 3 | 31,939 | 3 | 6,303 | 3 |
| Small Town/Rural | 952 | 2 | 40,993 | 4 | 4,080 | 2 | 516 | 1 | 12,523 | 1 | 2,471 | 1 |
| Region | ||||||||||||
| Northeast | 6,840 | 17 | 329,122 | 30 | 20,304 | 10 | 6,725 | 17 | 163,214 | 17 | 32,209 | 17 |
| Midwest | 6,518 | 16 | 166,804 | 15 | 32,375 | 15 | 6,117 | 16 | 148,458 | 16 | 29,297 | 16 |
| South | 20,278 | 51 | 407,724 | 38 | 102,100 | 48 | 19,799 | 51 | 480,517 | 51 | 94,826 | 51 |
| West | 6,338 | 16 | 180,406 | 17 | 58,058 | 27 | 6,198 | 16 | 150,424 | 16 | 29,685 | 16 |
| High Deductible Health Plan | ||||||||||||
| No | 34,050 | 85 | 1,015,954 | 94 | 199,059 | 94 | 33,555 | 86 | 814,372 | 86 | 160,709 | 86 |
| Yes | 5,924 | 15 | 68,102 | 6 | 13,778 | 6 | 5,284 | 14 | 128,241 | 14 | 25,307 | 14 |
| Diagnosis Categoryb | ||||||||||||
| Sinusitis | 16,628 | 42 | 338,656 | 31 | 62,699 | 29 | 16,168 | 42 | 392,393 | 42 | 77,435 | 42 |
| Streptococcal Pharyngitis | 747 | 2 | 32,203 | 3 | 12,649 | 6 | 669 | 2 | 16,236 | 2 | 3,204 | 2 |
| Otitis Media | 647 | 2 | 60,081 | 6 | 14,894 | 7 | 603 | 2 | 14635 | 2 | 2,888 | 2 |
| Bronchitis/Bronchiolitis | 5,792 | 14 | 172,837 | 16 | 31,212 | 15f | 5547 | 14 | 134624 | 14 | 26,567 | 14 |
| Other Viral ARIsc | 16,160 | 40 | 490,839 | 45 | 94,092 | 44 | 15852 | 41 | 384724 | 41 | 75,922 | 41 |
Source: Authors’ analysis of data from 2015-2016 claims from a large national insurer.
Notes: DTC is direct-to-consumer. HDHP is high deductible health plan. PCP is primary care provider. ARI is acute respiratory infection.
Presence or absence of patient’s chronic medical conditions was determined using the Charlson Comorbidity Index.
A small percentage (1.0%) of visits had more than one of these diagnoses, so the percentages of the diagnosis categories may sum up to be greater than 100%.
The other viral ARIs category consists of diagnoses where antibiotics are not indicated (e.g., viral upper respiratory infection, viral pharyngitis, and non-suppurative otitis), with the exception that bronchitis/bronchiolitis is separately categorized.
All categories in the unmatched sample have a p value that is <0.001, expect when otherwise indicated.
All categories in the matched sample have a p value that is equal to 1. Counts within categories in the matched sample may exceed column total because of weighted frequencies are rounded to whole numbers.
The indicated estimate did not differ significantly from DTC telemedicine estimates (p>0.05).
In the unmatched sample, compared to PCP patients, direct-to-consumer telemedicine patients were 2% more likely to receive an antibiotic (52% vs 50% PCP, p<0.001) and 1% more likely to receive guideline-concordant care (62% vs 61% PCP, p<0.001) (Exhibit 2). A breakdown of antibiotic use, broad-spectrum antibiotic use, and guideline-concordant antibiotic management by diagnosis category in the unmatched sample is shown in Appendix Exhibit A6(13).
Exhibit 2:
Antibiotic Use, Broad-Spectrum Antibiotic Use, and Guideline-Concordant Antibiotic Management across Settings in the Unmatched and Matched Sample, 2015–2016
| Unmatched Visits | Matched Visits | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| DTC Telemedicine | PCP | Urgent Care | DTC Telemedicine | PCP | Urgent Care | |||||||
| Overall (N) | 39,974 | 1,084,056 | 212,837 | 38,839 | 942,613 | 186,016 | ||||||
| Any Antibiotic Usea | 20,839 | 52 | 544,105 | 50*** | 113,769 | 53*** | 20,231 | 52 | 497,941 | 53** | 105,048 | 56*** |
| Broad-Spectrum Antibiotics Useb | 10,932 | 27 | 302,020 | 28* | 54,829 | 26*** | 10,627 | 27 | 273,628 | 29*** | 52,985 | 28*** |
| Guideline-Concordant Antibiotic Managementc | 24,767 | 62 | 660,582 | 61*** | 128,731 | 60*** | 24,055 | 62 | 568,949 | 60*** | 110,095 | 59*** |
Source: Authors’ analysis of data from 2015-2016 claims from a large national insurer.
Notes: Abbreviations: DTC, direct to consumer; PCP, primary care provider.
Visits with antibiotic use include those categorized as guideline-concordant use, guideline non-concordant use, and unnecessary antibiotic use.
Broad-spectrum antibiotics were defined as macrolides (excluding erythromycin), fluoroquinolones, and non-first-generation cephalosporins.
Visits with guideline-concordant antibiotic management include those categorized as guideline-concordant antibiotic use, guideline-concordant non-use of antibiotics, or, for visits with a diagnosis of acute otitis media or sinusitis, no antibiotic use. Hypothesis testing performed using chi-square tests, comparing DTC telemedicine visits to PCP visits and to urgent care visits
p<0.05;
p<0.01;
p<0.001
Antibiotic use among matched visits.
The matched, weighted sample included 38,839 direct-to-consumer telemedicine, 942,613 PCP, and 186,016 urgent care visits (Exhibit 1) with good balance across observed characteristics (Appendix Exhibit A7)(13). In the matched sample, visits in each setting were primarily by individuals from metropolitan areas (95%, all), the South (51%, all), and for either sinusitis (42%) or other viral acute respiratory infections (41%).
Across matched acute respiratory infection visits, patients at direct-to-consumer telemedicine visits received 1% fewer antibiotics than patients at PCP visits (52% vs 53% PCP, p<0.01) and 4% fewer antibiotics than patients at urgent care visits (52% vs. 56% urgent care, p <0.001) (Exhibit 2). Broad-spectrum antibiotic use was 1–2% lower for patients at direct-to-consumer telemedicine visits compared to PCP and urgent care visits (27% vs 29% PCP, 28% urgent care, p <0.001, both). Azithromycin accounted for 90% of broad-spectrum antibiotics received by patients at direct-to-consumer telemedicine visits, compared to 70% at PCP visits and 71% at urgent care visits (p<0.001, both) (results not shown).
Guideline-concordant antibiotic management was 2–3% higher for patients at direct-to-consumer telemedicine compared to PCP and urgent care (62% versus 60% PCP, 59% urgent care, p<0.001, both)(Exhibit 2). Comparisons of specific categories of guideline concordance (e.g., guideline non-concordant antibiotic use) are shown in Appendix Exhibit A8(13).
Within diagnoses, we found that direct-to-consumer telemedicine antibiotic measures were not consistently superior or inferior to other settings (Exhibit 3). For example, among patients diagnosed with bronchitis, those at direct-to-consumer telemedicine visits were more likely to receive guideline-concordant antibiotic management than those at PCP or urgent care visits (43% v 40% PCP, 36% urgent care, p<0.001, both). On the other hand, among patients with streptococcal pharyngitis, those at direct-to-consumer telemedicine visits were more likely to receive broad spectrum antibiotics than patients at PCP or urgent care visits (23% v 17% PCP, 18% urgent care, p<0.01).
Exhibit 3:
Antibiotic Use, Broad-spectrum Antibiotic Use, and Guideline-Concordant Antibiotic Management in DTC Telemedicine, Primary Care Providers, and Urgent Care by Diagnosis Category in the Matched Sample, 2015–2016
| Matched Visits | ||||||
|---|---|---|---|---|---|---|
| DTC Telemedicine | PCP | Urgent Care | ||||
| Overall (N) | 38,839 | 942,613 | 186,016 | |||
| Diagnosis Categories | ||||||
| Antibiotics May Be Indicated | ||||||
| Sinusitis | ||||||
| Any Antibiotic Use | 9,932 | 61 | 252,871 | 64*** | 52,596 | 68*** |
| Broad-Spectrum Antibiotics Use | 4,509 | 28 | 118,378 | 30*** | 21,314 | 28 |
| Guideline-Concordant Antibiotic Management | 11,344 | 70 | 257,347 | 66*** | 52,219 | 67*** |
| Streptococcal Pharyngitis | ||||||
| Any Antibiotic Use | 461 | 69 | 10,937 | 67 | 2,284 | 71 |
| Broad-Spectrum Antibiotics Use | 151 | 23 | 2,784 | 17*** | 561 | 18** |
| Guideline-Concordant Antibiotic Management | 270 | 40 | 6,149 | 38 | 1,393 | 43 |
| Otitis Media | ||||||
| Any Antibiotic Use | 420 | 70 | 9,449 | 65* | 2,041 | 71 |
| Broad-Spectrum Antibiotics Use | 130 | 22 | 3,444 | 24 | 714 | 25 |
| Guideline-Concordant Antibiotic Management | 460 | 76 | 10,788 | 74 | 2,120 | 73 |
| Antibiotics Not Indicated | ||||||
| Bronchitis/Bronchiolitis | ||||||
| Any Antibiotic Use | 3,161 | 57 | 81,360 | 60*** | 16,956 | 64*** |
| Broad-Spectrum Antibiotics Use | 2,552 | 46 | 65,979 | 49*** | 13,523 | 51*** |
| Guideline-Concordant Antibiotic Management | 2,386 | 43 | 53,264 | 40*** | 9,611 | 36*** |
| Other Viral ARI | ||||||
| Any Antibiotic Use | 6,257 | 39 | 143,324 | 37*** | 31,170 | 41*** |
| Broad-Spectrum Antibiotics Use | 3,285 | 21 | 83,043 | 22** | 16,873 | 22*** |
| Guideline-Concordant Antibiotic Management | 9,595 | 61 | 241,400 | 63*** | 44,752 | 59*** |
Source: Authors’ analysis of data from 2015-2016 claims from a large national insurer.
Notes: Abbreviations: DTC, direct to consumer; PCP, primary care provider. Hypothesis testing performed using chi-square tests, comparing DTC telemedicine visits to PCP visits and to urgent care visits
p<0.05;
p<0.01;
p<0.001
Streptococcal testing and follow-up visits.
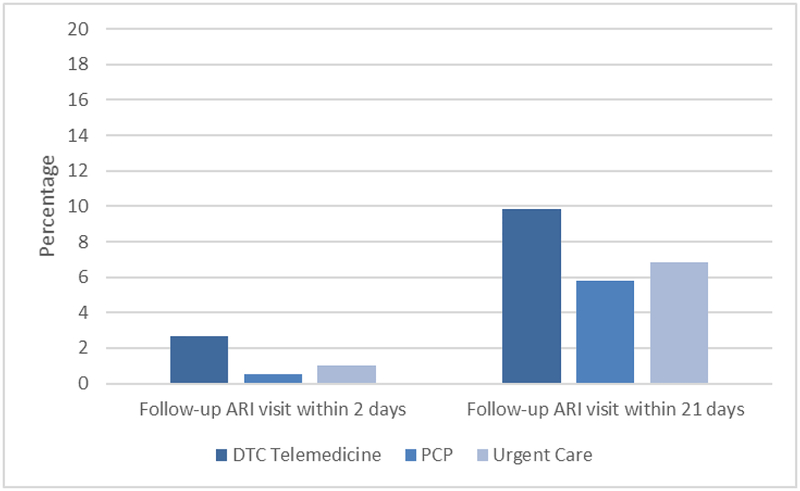
Among visits with a streptococcal pharyngitis diagnosis in the matched sample, direct-to-consumer telemedicine patients received a streptococcal testing 1% of the time compared to 67% of patients at PCP and 78% at urgent care visits (p<0.001 both comparisons, results not shown). Among all acute respiratory infection visits in the matched, weighted sample, we found a higher frequency of follow-up visits for patients in the subsequent 2 days and 21 days after direct-to-consumer telemedicine index visits compared to PCP or urgent care index visits (21 day follow-up visits: 10% vs 6% PCP, 7% urgent care, p<0.001, both)(Exhibit 4). After direct-to-consumer telemedicine index visits, the location of the first follow-up visit was divided between a 2nd direct-to-consumer telemedicine visit (42%) and a PCP visit (41%) (results not shown). After PCP index visits, follow-up visit location was primarily PCPs (91%). After an urgent care index visit, follow-up visit locations were divided between a 2nd urgent care visit (49%) and a PCP visit (45%).
Exhibit 4: Follow-up Visit Rate across DTC Telemedicine, Primary Care Providers, and Urgent Care in the Matched Sample, 2015–2016.
Source: Authors’ analysis of data from 2015-2016 claims from a large national insurer.
Notes: Abbreviations: DTC, direct to consumer; PCP, primary care provider. Hypothesis testing performed using chi-square tests, comparing DTC telemedicine visits to PCP visits and to urgent care visits. All comparisons have a p value that is <0.001.
Sensitivity analysis.
When employing our alternative definition of guideline-concordant antibiotic management, rates of guideline-concordant antibiotic management were not different across direct-to-consumer telemedicine, PCP, and urgent care patients (45% direct-to-consumer telemedicine vs 45% PCP [p=0.12], 45% urgent care [p=0.91])(Appendix Exhibit A9)(13).
Discussion
While patients may benefit from the access and convenience of direct-to-consumer telemedicine, one ongoing concern has been the quality of care provided. In our unmatched and matched analyses, compared to PCP visits, quality at direct-to-consumer telemedicine visits was within 1–2 percentage points for measures of antibiotic use, broad spectrum antibiotic use, and guideline-concordant antibiotic management. Though most of these differences are statistically significant due to the large sample size, the small size of these differences and the inconsistent direction of differences in diagnosis-specific analysis suggest that these differences may not be clinically meaningful. On other quality metrics, we find that direct-to-consumer telemedicine has less appropriate streptococcal testing and more frequent follow-up visits.
Small studies examining early experiences with direct-to-consumer telemedicine reported some concerns regarding antibiotic management during acute respiratory infection visits, including 10% more inappropriate antibiotic use for bronchitis compared to physician’s offices(6) and significantly higher use of broad-spectrum antibiotics.(7) In contrast with these earlier findings, we found that antibiotic use after direct-to-consumer telemedicine visits for adults with acute respiratory infections appears on par with PCP and urgent care visits. In recent years, many direct-to-consumer telemedicine companies began initiatives to enhance antibiotic stewardship,(36, 37) and such efforts may explain the differences between earlier and current findings.
While antibiotic measures were similar, the low streptococcal testing rate and higher follow-up rate highlight areas in need of ongoing attention. Direct-to-consumer telemedicine companies have been working with lab diagnostic companies to better integrate and streamline lab testing into their visits.(38, 39) However, given the minimal amount of streptococcal testing performed following direct-to-consumer telemedicine visits where this diagnosis is made, more work is needed to bring care for streptococcal pharyngitis via direct-to-consumer telemedicine in line with guidelines.(27)
In addition, the higher follow-up visit rates could indicate that there was a misdiagnosis or that patients’ needs were not adequately addressed at the initial visit, requiring additional unplanned care. An alternative explanation is that direct-to-consumer telemedicine providers recommended follow-up visits at a higher rate than PCP or urgent care providers, perhaps to confirm a suspected diagnosis with in-person evaluation or to monitor status some interval after the initial visit. Whether these follow-up visits were planned or unplanned cannot be determined from the claims data. Future research could compare outcomes across different direct-to-consumer telemedicine models (with and without personal in-home devices for ear exams; with and without access to the patient’s primary care records) or via randomization to site of care (to address potential self-selection biases) to better understand specific aspects of the direct-to-consumer telemedicine model contributing to these differences in follow-up visits.
Another important finding is the differential mix of acute respiratory infection diagnoses across settings. Providers at direct-to-consumer telemedicine visits were more likely to diagnose bacterial conditions that may warrant antibiotics, while PCPs and urgent care were more likely to diagnose viral conditions. This has both clinical and methodological implications. This could represent a true difference in the presenting illnesses at each setting due to patient self-selection. Alternatively, direct-to-consumer telemedicine providers may be swayed (consciously or subconsciously) towards making diagnoses that may warrant antibiotics, perhaps due to clinical uncertainty or perceived patient expectations. This diagnosis pattern could also be an unintended consequence of company attention to antibiotic stewardship(37, 40): pressure to improve the concordance of antibiotic management could unintentionally incentivize providers to increase coding of diagnoses that may warrant antibiotics. Methodologically, because acute respiratory infection diagnosis is partially subjective,(41) we included analysis of both matched and unmatched samples. Many prior studies of acute respiratory infection antibiotic management do not adjust for diagnoses for this reason.(9, 11)
While our analysis was designed to examine differences between direct-to-consumer telemedicine, PCP, and urgent care visits, we note that antibiotic management was poorly concordant with guidelines across all settings, consistent with other recent studies.(14, 15) Outpatient antibiotic stewardship has been successful in driving improvement(42–47) and may need to be more aggressively applied to all of these settings.
Policy Implications
Policy statements of organizations such as the American College of Physicians state that the quality of care during telemedicine should be comparable to in-person visits.(48) Our results imply that direct-to-consumer telemedicine antibiotic management quality is clinically similar to that at PCP and urgent care, but that completion of streptococcal testing remains much lower among visits where the diagnosis of streptococcal pharyngitis is made. As noted above, direct-to-consumer telemedicine companies have sought to enhance their ability to incorporate laboratory testing into their care.(38, 39) Our results emphasize the need for more work in this area. Additionally, diagnoses of otitis media via direct-to-consumer telemedicine raise questions about adherence to in-person standards, given that patients rarely have the tele-otoscopy equipment needed to transmit an image of the tympanic membrane. Thus, it appears that direct-to-consumer telemedicine visits are clinically similar to in-person visits in adherence to acute respiratory infection antibiotic management guidelines, but that ongoing attention is needed to adherence to acute respiratory infection diagnosis guidelines and standards.
Health plans and employers that help pay for direct-to-consumer telemedicine visits could play a more active role in monitoring and improving the quality of care provided by direct-to-consumer telemedicine providers, including a focus on the appropriate reasons to use direct-to-consumer telemedicine and appropriate diagnoses that can be conclusively made during direct-to-consumer telemedicine visits. For example, payers may wish to partner with direct-to-consumer telemedicine companies to reduce visits where diagnoses are made and treated with inadequate exams or evaluations (e.g., diagnosis of otitis media without visualizing the tympanic membrane). In recent work, one such partnership succeeded at dramatically reducing “inappropriate” direct-to-consumer telemedicine visits.(36) Additionally, these payers could be more direct in fostering and facilitating partnership between direct-to-consumer telemedicine providers and lab diagnostic companies.
In conclusion, adult patients with acute respiratory infection diagnosis at direct-to-consumer telemedicine visits have clinically similar rates of antibiotic use, broad-spectrum antibiotic use, and guideline-concordant antibiotic management compared to matched patients at PCP and urgent care visits. However, direct-to-consumer telemedicine patients had lower appropriate streptococcal testing and increased frequency of follow-up visits.
Supplementary Material
References
- 1.Tahir D Telehealth services surging despite questions about value. Mod Healthc. 2015 February 21, 2015. [PubMed] [Google Scholar]
- 2.Global Telehealth Market Set to Expand Tenfold by 2018. El Segundo: IHS Markit; 2014. January 17. [Google Scholar]
- 3.National Business Group on Health. Large US employers project health care benefit costs to surpass $14000 per employee in 2018, National Business Group on Health survey finds [press release]: National Business Group on Health; [updated August 8, 2017. Available from: https://www.businessgrouphealth.org/news/nbgh-news/press-releases/press-release-details/?ID=334. [Google Scholar]
- 4.Ladika S Tuning in to Telemedicine 2015. Available from: https://www.managedcaremag.com/archives/2015/7/tuning-telemedicine. [PubMed]
- 5.Weinstein RS, Krupinski EA, Doarn CR. Clinical Examination Component of Telemedicine, Telehealth, mHealth, and Connected Health Medical Practices. Med Clin North Am. 2018;102(3):533–44. [DOI] [PubMed] [Google Scholar]
- 6.Uscher-Pines L, Mulcahy A, Cowling D, Hunter G, Burns R, Mehrotra A. Access and Quality of Care in Direct-to-Consumer Telemedicine. Telemedicine journal and e-health : the official journal of the American Telemedicine Association. 2016;22(4):282–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Uscher-Pines L, Mulcahy A, Cowling D, Hunter G, Burns R, Mehrotra A. Antibiotic prescribing for acute respiratory infections in direct-to-consumer telemedicine visits. JAMA Intern Med. 2015;175(7):1234–5. [DOI] [PubMed] [Google Scholar]
- 8.Uscher-Pines L, Mehrotra A. Analysis of Teladoc use seems to indicate expanded access to care for patients without prior connection to a provider. Health Affairs. 2014;33(2):258–64. [DOI] [PubMed] [Google Scholar]
- 9.Mehrotra A, Gidengil CA, Setodji CM, Burns RM, Linder JA. Antibiotic prescribing for respiratory infections at retail clinics, physician practices, and emergency departments. Am J Manag Care. 2015;21(4):294–302. [PubMed] [Google Scholar]
- 10.Grijalva CG, Nuorti JP, Griffin MR. Antibiotic prescription rates for acute respiratory tract infections in US ambulatory settings. JAMA. 2009;302(7):758–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Gidengil CA, Mehrotra A, Beach S, Setodji C, Hunter G, Linder JA. What drives variation in antibiotic prescribing for acute respiratory infections? J Gen Intern Med. 2016;31(8):918–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Roth J CMS ICD-9-CM to and from ICD-10-CM and ICD-10-PCD Crosswalk or General Equivalence Mappings: The National Bureau of Economic Research; [Available from: http://www.nber.org/data/icd9-icd-10-cm-and-pcs-crosswalk-general-equivalence-mapping.html. [Google Scholar]
- 13.To access the Appendix, click on the Details tab of the article online.
- 14.Fleming-Dutra KE, Hersh AL, Shapiro DJ, Bartoces M, Enns EA, File TM Jr, et al. Prevalence of inappropriate antibiotic prescriptions among us ambulatory care visits, 2010–2011. JAMA. 2016;315(17):1864–73. [DOI] [PubMed] [Google Scholar]
- 15.Palms DL, Hicks LA, Bartoces M, et al. Comparison of antibiotic prescribing in retail clinics, urgent care centers, emergency departments, and traditional ambulatory care settings in the united states. JAMA Intern Med. 2018;178(9):1267–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mehrotra A, Paone S, Martich GD, Albert SM, Shevchik GJ. A comparison of care at e-visits and physician office visits for sinusitis and urinary tract infection. JAMA Intern Med. 2013;173(1):72–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Poon SJ, Schuur JD, Mehrotra A. Trends in visits to acute care venues for treatment of low-acuity conditions in the united states from 2008 to 2015. JAMA Intern Med. 2018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ashwood J, Mehrotra A, Cowling D, Uscher-Pines L. Direct-To-Consumer Telehealth May Increase Access To Care But Does Not Decrease Spending. Health Affairs. 2017;36(3):485–91. [DOI] [PubMed] [Google Scholar]
- 19.Mehrotra A, Paone S, Martich GD, Albert SM, Shevchik GJ. Characteristics of Patients Who Seek Care via eVisits Instead of Office Visits. Telemedicine journal and e-health : the official journal of the American Telemedicine Association. 2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Silverman MA, Konnikova L, Gerber JS. Impact of antibiotics on necrotizing enterocolitis and antibiotic-associated diarrhea. Gastroenterol Clin North Am. 2017;46(1):61–76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Steinman MA, Landefeld CS, Gonzales R. Predictors of broad-spectrum antibiotic prescribing for acute respiratory tract infections in adult primary care. JAMA. 2003;289(6):719–25. [DOI] [PubMed] [Google Scholar]
- 22.Shapiro DJ, Hicks LA, Pavia AT, Hersh AL. Antibiotic prescribing for adults in ambulatory care in the USA, 2007–09. J Antimicrob Chemother. 2014;69(1):234–40. [DOI] [PubMed] [Google Scholar]
- 23.Lee GC, Reveles KR, Attridge RT, Lawson KA, Mansi IA, Lewis JS 2nd, et al. Outpatient antibiotic prescribing in the United States: 2000 to 2010. BMC Med. 2014;12:96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Sarpong EM, Miller GE. Narrow- and Broad-Spectrum Antibiotic Use among U.S. Children. Health Services Research. 2015;50(3):830–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Gerber JS, Ross RK, Bryan M, Localio AR, Szymczak JE, Wasserman R, et al. Association of Broad- vs Narrow-Spectrum Antibiotics With Treatment Failure, Adverse Events, and Quality of Life in Children With Acute Respiratory Tract Infections. JAMA. 2017;318(23):2325–36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Gidengil CA, Linder JA, Beach S, Setodji CM, Hunter G, Mehrotra A. Using Clinical Vignettes to Assess Quality of Care for Acute Respiratory Infections. INQUIRY: The Journal of Health Care Organization, Provision, and Financing. 2016;53:0046958016636531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Shulman ST, Bisno AL, Clegg HW, Gerber MA, Kaplan EL, Lee G, et al. Clinical Practice Guideline for the Diagnosis and Management of Group A Streptococcal Pharyngitis: 2012 Update by the Infectious Diseases Society of America. Clin Infect Dis. 2012;55(10):e86–e102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Chow AW, Benninger MS, Brook I, Brozek JL, Goldstein EJC, Hicks LA, et al. Executive Summary: IDSA Clinical Practice Guideline for Acute Bacterial Rhinosinusitis in Children and Adults. Clin Infect Dis. 2012;54(8):1041–5. [DOI] [PubMed] [Google Scholar]
- 29.Lieberthal AS, Carroll AE, Chonmaitree T, Ganiats TG, Hoberman A, Jackson MA, et al. The Diagnosis and Management of Acute Otitis Media. Pediatrics. 2013;131(3):e964–e99. [DOI] [PubMed] [Google Scholar]
- 30.Wong DM, Blumberg DA, Lowe LG. Guidelines for the Use of Antibiotics in Acute Upper Respiratory Tract Infections. Am Fam Physicians. 2006;74(6):956–66. [PubMed] [Google Scholar]
- 31.Centers for Disease Control and Prevention. Adult Treatment Recommendations In: Centers for Disease Control and Prevention, editor. Atlanta: National Center for Emerging and Zoonotic Infectious Diseases (NCEZID); 2017. [Google Scholar]
- 32.Fu TL, Natalie M, James GW. Virtual Visits for Upper Respiratory Tract Infections in Adults Associated with Positive Outcome in a Cox Model. Telemedicine and e-Health. 2017;23(3):200–4. [DOI] [PubMed] [Google Scholar]
- 33.Gordon AS, Adamson WC, DeVries AR. Virtual Visits for Acute, Nonurgent Care: A Claims Analysis of Episode-Level Utilization. Journal Of Medical Internet Research. 2017;19(2):e35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.US Department of Agriculture Economic Research Service. Rural-Urban Commuting Area Codes 2016 [updated October 12 2016. Available from: https://www.ers.usda.gov/data-products/rural-urban-commuting-area-codes/.
- 35.Iacus SM, King G, Porro G. Causal Inference Without Balance Checking: Coarsened Exact Matching. Political Analysis. 2012;20(1):1–24. [Google Scholar]
- 36.Gali K, Faiman M, Romm S. Ensuring Clinical Quality in Telemedicine. New Engl J Med Catalyst. 2018. [Google Scholar]
- 37.Pedulli L Teladoc and Doctor on Demand CEOs share their vision for telehealth 2014. Available from: https://www.clinical-innovation.com/topics/mobile-telehealth/teladoc-and-doctor-demand-ceos-share-their-vision-telehealth.
- 38.HITC Staff. Doctor On Demand Integrates With LabCorp & Quest Diagnostics for Patient Lab Results 2017. Available from: https://hitconsultant.net/2017/05/05/doctor-demand-integrates-lab/.
- 39.Analyte Health and Teladoc Announce Partnership 2017. Available from: https://www.teladoc.com/news/2017/01/09/analyte-health-and-teladoc-announce-partnership/.
- 40.Beck M Where does it hurt? log on. the doctor is in; telemedicine sector attracts funding, but some physician groups worry about quality of care. Wall Street Journal (Online) [Internet]. 2014. Available from: https://www.wsj.com/articles/where-does-it-hurt-log-on-the-doctor-is-in-1399589901. [Google Scholar]
- 41.Gerber JS, Prasad PA, Russell Localio A, Fiks AG, Grundmeier RW, Bell LM, et al. Variation in Antibiotic Prescribing Across a Pediatric Primary Care Network. Journal of the Pediatric Infectious Diseases Society. 2015;4(4):297–304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Sanchez GV, Fleming-Dutra KE, Roberts RM, Hicks LA. Core Elements of Outpatient Antibiotic Stewardship. MMWR Recomm Rep. 2016;65(6):1–12. [DOI] [PubMed] [Google Scholar]
- 43.Gerber JS, Prasad PA, Fiks AG, Localio AR, Grundmeier RW, Bell LM, et al. Effect of an outpatient antimicrobial stewardship intervention on broad-spectrum antibiotic prescribing by primary care pediatricians: a randomized trial. JAMA. 2013;309(22):2345–52. [DOI] [PubMed] [Google Scholar]
- 44.McDonagh M, Peterson K, Winthrop K, Cantor A, Holzhammer B, Buckley DI. Improving Antibiotic Prescribing for Uncomplicated Acute Respiratory Tract Infections. AHRQ Comparative Effectiveness Reviews. 2016(Report No.: 15(16)-EHC033-EF). [PubMed] [Google Scholar]
- 45.Tonkin-Crine SKG, Tan PS, van Hecke O, Wang K, Roberts NW, McCullough A, et al. Clinician-targeted interventions to influence antibiotic prescribing behaviour for acute respiratory infections in primary care: an overview of systematic reviews. Cochrane Database of Systematic Reviews. 2017(9). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Linder JA, Meeker D, Fox CR, et al. Effects of behavioral interventions on inappropriate antibiotic prescribing in primary care 12 months after stopping interventions. JAMA. 2017;318(14):1391–2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Meeker D, Linder JA, Fox CR, et al. Effect of behavioral interventions on inappropriate antibiotic prescribing among primary care practices: A randomized clinical trial. JAMA. 2016;315(6):562–70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Daniel H, Sulmasy L, for the Health and Public Policy Committee of the American College of Physicians. Policy recommendations to guide the use of telemedicine in primary care settings: An American College of Physicians position paper. Annals of Internal Medicine. 2015;163(10):787–9. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.