Abstract
There is conflicting evidence as to whether military populations (i.e., veteran and active-duty military service members) demonstrate a poorer response to psychotherapy for posttraumatic stress disorder (PTSD) compared to civilians. Existing research may be complicated by the fact that treatment outcomes differences could be due to the type of trauma exposure (e.g., combat) or population differences (e.g., military culture). This meta-analysis evaluated PTSD treatment outcomes as a function of trauma type (combat v. assault v. mixed) and population (military v. civilian). Unlike previous meta-analyses, we focused exclusively on manualized, first-line psychotherapies for PTSD as defined by expert treatment guidelines. Treatment outcomes were large across trauma types and population; yet differences were observed between trauma and population subgroups. Military populations demonstrated poorer treatment outcomes compared to civilians. The combat and assault trauma subgroups had worse treatment outcomes compared to the mixed trauma subgroup, but differences were not observed between assault and combat subgroups. Higher attrition rates predicted poorer treatment outcomes, but did not vary between military populations and civilians. Overall, manualized, first-line psychotherapies for PTSD should continue to be used for civilians and military populations with various trauma types. However, greater emphasis should be placed on enhancing PTSD psychotherapies for military populations and on treatment retention across populations based on findings from this meta-analysis.
Keywords: Meta-Analysis, Posttraumatic stress disorder, First-Line Treatments, Trauma type, Military, Veterans, Civilians
1. Introduction
Posttraumatic stress disorder (PTSD) is a debilitating condition that leads to relationship dysfunction, physical health issues, greater health care utilization, increased work sick days, substance abuse, and elevated suicidality risk (Hoge, Terhakopian, Castro, Messer, & Engel, 2007; Taft, Watkins, Stafford, Street, & Monson, 2011; Thomas et al., 2010). Research has shown particularly high rates of PTSD in military populations (13–30%; Thomas et al., 2010; Kok, Herrell, Thomas & Hoge, 2012) compared to the general population (6–8%; Kessler, Berglund, Demler, Jin, & Walters, 2005). Given that almost 3 million U.S. military personnel have deployed to the Middle East and surrounding territories since 2001, the demand for effective treatments for veterans and active-duty service members, hereinafter referred to as military populations, is critical.
Evidence based psychotherapies for PTSD exist and the positive effects of evidence-based psychotherapies in civilian and military populations are well-established (Bisson et al., 2007; Bradley, Greene, Russ, Dutra & Western, 2005; Cusack et al., 2016; Goodson, Helstrom, Halpern, Ferenschack, & Gillihan, 2011; Kline, Cooper, Rytwinksi, & Feeny, 2018; Powers, Halpern, Ferenshak, Gilliahn, & Foa, 2010; Steenkamp, Litz, Hoge, & Marmar, 2015). However, several meta-analyses have reported smaller effect sizes among treatment studies with a greater proportion of veterans and combat samples (Bisson et al., 2007; Bradley et al., 2005; Sloan, Feinstein, Gallagher, Beck, & Keane, 2013; Watts, et al., 2013). These findings suggest military populations experience less benefit from psychotherapies for PTSD compared to civilians (Litz et al., 2009; Sifferlin, 2015; Steenkamp et al., 2015). Yet, existing meta-analyses have been limited in evaluating treatment response differences among military and civilian populations in several ways. For example, Bisson et al. (2007) only evaluated two studies of Vietnam veterans. Sloan et al. (2013) found that group interventions for PTSD were not significantly superior to active control conditions (d = 0.09); however, they did not include individual interventions. Watts et al. (2013) found that studies with more women, or fewer veterans, had larger effect sizes, but the authors were unable to disentangle whether this finding was due to gender or veteran status. Additionally, Watts et al. (2013) included psychotherapies that were considered to be first-line and non-first-line treatments according to PTSD treatment recommendation guidelines, which may have confounded results (American Psychological Association [APA], 2017; Department of Veterans Affairs and Department of Defense [VA/DoD], 2017; Foa, Keane, Friedman, & Cohen, 2009; Institute of Medicine [IOM], 2008; International Society for Traumatic Stress Studies [ISTSS], 2018). Similarly, Bradley et al. (2005) included all psychotherapies in their meta-analysis. They also reported that trauma type was a predictor of treatment effect size, but only reported an omnibus test of differences across three groups (combat v. mixed v. assault). This study did not test whether the combat group, which demonstrated the smallest effect size, was significantly different from the other groups.
There is also meta-analytic evidence to suggest that military populations benefit equally well from PTSD treatments compared to civilians. In a recent meta-analysis, Kline et al. (2018) demonstrated that population type (i.e., military v. civilian) was unrelated to effect sizes at long-term follow-up. However, this meta-analysis also included non-first-line psychotherapy treatments and only examined effect sizes at long-term follow-up, excluding studies that did not provide follow-up data. Thus, whether or not military populations demonstrate a poorer treatment response from first-line PTSD psychotherapies in comparison to their civilian counterparts remains an open and important question.
Conflicting findings in the existing research literature among military and civilian populations may be complicated by differences in the nature of the trauma exposure (e.g., combat v. assault) or differences in the patient population (i.e., characteristics of military v. civilian populations). Research has shown that military populations experience traumatic events at a greater frequency, these events are often combat-related, and are often more severe and diverse compared to civilian populations (Green et al., 2015; Stein et al., 2012). All of these factors have also been identified as variables that may contribute to PTSD symptom severity and treatment outcomes (Steenkamp et al., 2015). Additionally, active-duty service members remain in relatively dangerous situations during deployment, which places them at greater risk for repeated trauma exposure.
Discrepant findings on whether military populations benefit less from first-line PTSD psychotherapies may also be because, to our knowledge, previous meta-analyses have not separated military sexual trauma (MST) and combat-related trauma type in military populations. Research has found symptom presentation differences between MST victims and military populations with non-MST related PTSD (Carroll et al., 2018; Sexton et al., 2018). It is possible that MST is more akin to civilian sexual assault than to combat trauma, which in turn may impact treatment outcomes. Alternatively, it is possible that the impact of MST differs from that of civilian sexual assault, especially when perpetrated by a fellow service member with whom the victim may have continued contact and on whom the victim’s continued safety may depend (e.g., in combat). Early research is mixed regarding treatment outcome differences between MST and non-sexual assault military traumas (Tiet, Leyva, Blau, & Turchik, 2015; Voelkel, Pukay-Martin, Walter, & Chard, 2015; Zalta et al., 2018). Therefore, separating military population studies by trauma type could provide an explanation for previous conflicting results regarding population and trauma type differences.
It is also important to consider that treatment outcome differences may not be impacted by the type of trauma, but rather characteristics that differ between military and civilian populations. For example, prior research has noted approximately 87% of treatment seeking military veterans with PTSD also meet criteria for at least one additional psychiatric comorbidity (Magruder et al., 2005). Military culture has also been identified as a factor that may interfere with optimal treatment response. Research has indicated that mental health stigma in the military may impact treatment seeking behavior and treatment dropout (Sharp et al., 2015). Mental health stigma beliefs may also result in treatment dropout and poor treatment attendance, which has been linked to worse PTSD treatment outcomes (Bush, Sheppard, Fantelli, Bell, & Reger, 2013; Tarrier, Sommerfield, Pilgrim, & Faragher, 2000). Military training is another factor that may interfere with treatment response by promoting hyperarousal PTSD symptoms, such as hypervigiliance and anger, as key strategies for survival (Yehuda, Vermetten, McFarlane, & Lehrner, 2014). It is also possible that other systemic factors, such as service connection disability claims and secondary gain, may impede treatment gains (Guina, Welton, Broderick, Correll, & Peirson, 2016; McNally & Frueh, 2013). Although mental health stigma, cultural norms about the benefits of hypervigilance and avoidance, and disability claims are not entirely absent in civilian populations, they appear to be more prevalent in military populations.
The goal of this meta-analysis is to evaluate PTSD treatment outcomes as a function of trauma type and population. Specifically, we aim to evaluate whether military populations demonstrate a poorer treatment response from first-line PTSD psychotherapy interventions in comparison to civilians. Based on the existing evidence, we hypothesized that: (a) first-line treatments would result in treatment benefits across trauma types and population types; (b) combat traumas would yield smaller treatment benefits compared to other trauma types; and (c) military populations would report poorer treatment outcomes compared to civilian populations.
2. Methods
A systematic review of the literature was conducted to identify psychotherapy treatment outcome trials for PTSD from PsycINFO, PILOTS, and MEDLINE databases from January 1, 1980 to December 31, 2017. The rationale for selecting this start date was based on the formal introduction of PTSD as codified clinical diagnosis in the American Psychiatric Association Diagnostic and Statistical Manual, 3rd ed, which was published in 1980 (American Psychiatric Association, 1980). We used subject headings and keywords, when appropriate, for the following search terms, “(ptsd or post traumatic stress disorder or posttraumatic stress disorder or post-traumatic stress disorder) and (cognitive behavior* therapy or cbt or cognitive-behavio* therapy) or (cognitive processing therapy or CPT) or (prolonged exposure or prolonged exposure therapy or PE) or (eye movement desensitization and reprocessing or emdr) and (Adult*).” Additional inclusion criteria were that manuscripts were peer reviewed and published in English. Potential papers for inclusion were also identified through hand-searching published PTSD reviews, PTSD meta-analyses, and the references of retrieved articles.
2.1. Inclusion criteria
We included PTSD psychotherapy treatment outcome trials (controlled and uncontrolled studies) for adults with a diagnosis of PTSD. Studies that included participants with sub-threshold PTSD were excluded from the meta-analysis. Selection of included intervention types was based on the International Society for Traumatic Stress Studies (ISTSS) PTSD treatment recommendation guidelines (ISTSS, 2018). Based on the ISTSS guidelines, we included studies that utilized at least one of four manualized, first-line psychotherapy treatments for PTSD: Prolonged Exposure (PE), Cognitive Processing Therapy (CPT), Eye Movement Desensitization and Reprocessing (EMDR), and Ehlers and Clark’s (2005) Cognitive Therapy (CT) for PTSD.
The rationale to include only these four interventions was to mitigate treatment type confounds (e.g., first-line vs. non-first-line treatment options). Studies that utilized components of these interventions, implemented the interventions in a manner that was inconsistent with the standard protocol, or included an additive treatment component were excluded from the meta-analysis. For example, if a study only used imaginal exposure, combined PE with another intervention, or implemented components of PE in a manner that was inconsistent with the protocol, that study was excluded. When a trial involved multiple condition arms and one of the arms was consistent with our inclusion criteria, we extracted the data for that condition alone and excluded the other treatment arms. For example, if a trial compared EMDR alone v. EMDR combined with medication, we extracted the data from the first condition and excluded the second condition.
Studies that utilized individual, face-to-face weekly or biweekly interventions in an outpatient setting were included in the meta-analysis. Although PTSD treatments using a group treatment modality, teletherapy/virtual options, daily (massed) delivery, and administration in a residential/inpatient setting have demonstrated positive treatment outcomes, these formats can include additional components that deviate from the initial protocol design or remain categorized as a non-first-line treatment option (ISTSS, 2018). For instance, residential PTSD treatments often include additional supplementary components (e.g., skills-based therapy, art therapy, etc.) that are not often utilized in conjunction with a first-line PTSD treatment delivered in an individual outpatient therapy format. We also excluded trials that focused on dual diagnosis treatment for PTSD and a comorbid issue because the primary focus of this meta-analysis was PTSD treatment outcomes alone. We did not exclude studies where participants endorsed a comorbid secondary condition as long as the aim of the study was PTSD treatment alone. Based on expert guidelines, studies with a protocol that was at least 4 sessions in length were eligible for inclusion (Foa et al., 2009).
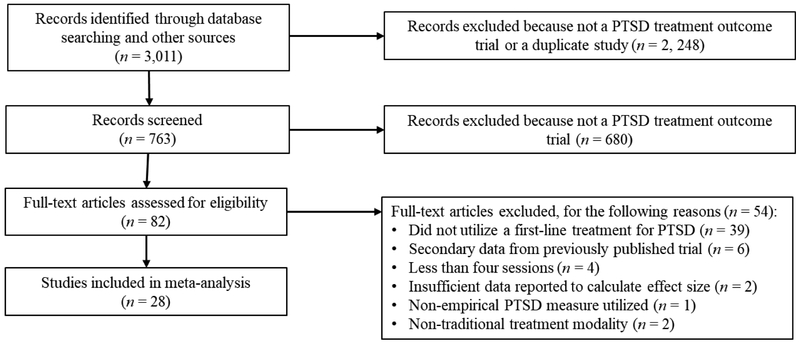
Additional criteria for inclusion were that studies utilized an established PTSD outcome measure and an established PTSD diagnostic measure. The rationale for all of the listed exclusion decisions was to mitigate potential variables that may impact treatment outcomes and confound our primary analyses. When insufficient information was available to calculate an effect size, the primary study author was contacted to obtain the required information (i.e., Duffy, Gillespie, & Clark, 2007; Lee, Gavriel, Drummond, Richards, & Greenwald, 2002; Monson et al., 2006; Nacash et al., 2011; Popiel, Zawadzki, Pragiowska, & Teichman, 2015; Rauch et al., 2009; Schnurr et al., 2007; Thorp et al., 2012). Studies were excluded from analyses if the author could not be contacted or was unable to provide data. Based on the criteria outlined above, 28 studies were included. See Figure 1 for a flow chart of included studies.
Figure 1.
PRISMA Flow Chart of Included Studies.
2.2. Coding procedures and definitions
Outcome variables of interest were PTSD symptom severity mean scores at pre and posttreatment and the proportion of participants who no longer met criteria for PTSD at posttreatment. Additionally, study sample characteristics and study methodology was coded for each study to evaluated potential covariates that may predict treatment outcomes (see Table 1). Sample descriptive variables included percentage of participants that were female, mean participant age in years, and percentage of the sample who dropped out of treatment (attrition). Study methodology variables included intervention type (EMDR, CPT, PE, CT), PTSD treatment outcome/diagnostic measure used, method of PTSD measure administration (self-report v. clinical interview), statistical analysis method (intent to treat v. completer), study year, and trial type (randomized clinical trial [RCT], clinical comparative trial [CCT], and uncontrolled clinical trial [UCT]). Intervention type coding included four categories of EMDR, CPT, PE, or CT. Coding for PTSD measures was based on the reported diagnostic and outcome-based measures used in the study. Effect sizes based on intent to treat were selected over effect sizes based on completers when both methods were reported in the study. For type of trial, there was one instance of a quasi-randomization that was coded as “Quasi” (i.e., Thorpe, Stein, Jeste, Patterson, & Loebach-Wethell, 2012). This study was excluded from the trial type covariate analysis
Table 1.
Study Characteristics
| Study Name | n | Intervention Type | PTSD Measure | Trauma Type | Population | Trial Type | Age (M) | Female (%) | Attrition (%) | Dx (%) | SAM |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Asukai et al. 2010 | 12 | PE | CAPS, IES-R | Mixed (Assault, Accident) | Civilian | RCT | 29 | 87 | 25 | NR | ITT |
| Capezzani et al. 2013 | 21 | EMDR | IES-R | Mixed (Cancer) | Civilian | CCT | 53 | 90 | 0 | 95 | ITT |
| Carlson et al. 1998 | 10 | EMDR | MS-Com, IES | Combat | Military | RCT | 53 | 0 | 0 | 78 | CA |
| Chard et al. 2010 | 104 | CPT | CAPS, PCL-S | Combat | Military | UCT | 45 | 0 | 31 | 51 | ITT |
| Devilly and Spence 1999 | 11 | EMDR | MS-Civ, IES, PSS, PTSD-I | Mixed (Sexual/Physical Assault, Accident, Disaster, War Zone) | Civilian | CCT | 40 | 72 | 55 | 36 | CA |
| Ehlers et al. 2005 | 14 | CT | PSS, CAPS | Mixed (Accident, Assault, Witnessed Death) | Civilian | RCT | 55 | 37 | 0 | 71 | ITT |
| Ehlers et al. 2014 | 61 | CT | CAPS, PSS | Mixed (Assault, Accident, Disaster, Witnessed Death, Other) | Civilian | RCT | 39 | 59 | 3 | 71 | ITT |
| Feske 2008 | 9 | PE | PSS | Assault | Civilian | RCT | 43 | 100 | 31 | NR | CA |
| Foa et al. 1991 | 10 | PE | PSS | Assault | Civilian | RCT | 32 | 100 | 29 | 40 | CA |
| Foa et al. 1999 | 23 | PE | PSS | Assault | Civilian | RCT | 35 | 100 | 8 | 60 | CA |
| Foa et al. 2005 | 79 | PE | PSS | Assault | Civilian | RCT | 31 | 100 | 34 | NR | ITT |
| Forbes et al. 2012 | 30 | CPT | CAPS, PCL-S | Combat | Military | RCT | 53 | 4 | 30 | 38 | ITT |
| Galovski et al. 2012 | 53 | CPT | PSS, CAPS | Assault | Civilian | RCT | 40 | NR | 26 | 92 | ITT |
| Hӧgberg et al. 2007 | 12 | EMDR | IES | Mixed (Accident, Assault) | Civilian | RCT | 43 | 21 | 0 | 67 | CA |
| Lee et al. 2002 | 12 | EMDR | SIP-I, IES | Mixed (Assault, Accident, Combat, and Witnessed Death) | Civilian, Militaryd | RCT | 34 | NR | 8 | 83 | CA |
| Monson et al. 2006 | 30 | CPT | CAPS, PCL-S | NRa | Military | RCT | 54 | 10 | 20 | 40 | ITT |
| Nacash et al. 2010 | 15 | PE | PSS | Mixedc (Combat,Terror-related) | Military | RCT | 34 | NR | 13 | NR | ITT |
| Nijdam et al. 2012 | 70 | EMDR | SIP-I, IES-R | Mixed (Assault, Accident, Disaster, War-related, Other) | Civilian | CCT | 38 | 51 | 36 | 66 | ITT |
| Popiel et al. 2015 | 114 | PE | PSS-SR | Mixed (Accident) | Civilian | CCT | 40 | 21 | 18 | 66 | ITT |
| Power et al. 2002 | 27 | EMDR | SIP-SR, IES | Mixed (Accident, Assault, Traumatic Death, Real or Implied Physical Threat, Other) | Civilian | RCT | 39 | 42 | 31 | NR | CA |
| Rauch et al. 2009 | 10 | PE | PSS | Mixedb (Combat; MST/Assault) | Military | UCT | 39 | 20 | 0 | NR | ITT |
| Rauch et al. 2015 | 11 | PE | CAPS | Combat | Military | CCT | 32 | 8 | 39 | NR | CA |
| Resick et al. 2002 | 124 | PE, CPT | CAPS, PSS | Assault | Civilian | RCT | 32 | 100 | 27 | 53 | ITT |
| Resick et al. 2008 | 100 | CPT | PSS, CAPS | Assault | Civilian | CCT | 35 | 100 | 24 | 60 | ITT |
| Schnurr et al. 2007* | 141 | PE | CAPS, PCL-S | Mixedc (Assault, Combat, Other) | Military | RCT | 44 | 100 | 38 | 39 | ITT |
| Surís et al. 2013 | 52 | CPT | CAPS, PCL-S | MST/Assault | Military | RCT | 46 | 85 | 35 | NR | ITT |
| Thorp et al. 2012 | 8 | PE | CAPS, IES-R | Mixedb (Combat; MST; Accident) | Military | Quasi | 63 | 0 | 0 | 88 | CA |
| Tuerk et al. 2011 | 65 | PE | PCL-M | Combat | Military | UCT | 32 | 11 | 34 | 49 | ITT |
Note. Total N = 1,228; PTSD = posttraumatic stress disorder; RCT = randomized controlled trial; UCT = uncontrolled trial; CCT = comparative clinical trial; Quasi = quasi-randomized controlled trial; M = mean; % = percentage; Dx = PTSD diagnosis at posttreatment; SAM= statistical analysis method; ITT = intent to treat; CA = completer; PE = prolonged exposure; CPT = cognitive processing therapy; CT = cognitive therapy; EMDR = eye movement desensitization reprocessing; CAPS = Clinician Administered PTSD Scale; IES(-R) = Impact of Events Scale (-Revised); MS (-Com or -Civ) = Mississippi Scale for PTSD (-Combat or -Civilian); PCL (-S or -M) = Posttraumatic Stress Disorder Checklist (-Specific or -Military); PSS (-SR) = Posttraumatic Stress Scale Interview (-Self Report); PTSD-I = PTSD Interview; SIP (-I or -SR) = Structured Interview for PTSD (-Interview or -Self Report); NR = not reported.
The study sample was excluded from trauma type analysis because trauma type was not indicated and author did not respond through correspondence.
The study sample included some participants with non-combat traumas, but only the participants with combat trauma were included in the trauma type analysis due to small n in other trauma type categories (Rauch et al., 2009: n = 8; Thorp et al., 2012: n = 5);
The study sample was separated by trauma type in analysis for reasons described in the Methods section; studies with a trauma type category defined as “Mixed” without a superscript were not separated by trauma type in trauma type analysis.
Denotes the study sample was separated by population type for population analysis.
study was identified as an outlier based on SAM-D statistic.
The first moderator variable of interest was trauma type. A minimum of three studies were required to establish a trauma type to maximize the number of identified trauma categories in the least restrictive manner. Based on this method, we defined and coded trauma type into three categories: a) combat, b) assault, or c) mixed. The combat trauma category was defined as a traumatic experience that occurred in the context of a combat-related event. The assault trauma category was defined as physical or sexual assault, and included one military sexual trauma study (i.e., Surís et al., 2013). The mixed trauma category included studies with various trauma types reported or a specific trauma type that did not have at least three studies to establish a specific trauma type subgroup. For example, Ehlers et al. (2014) included individuals with PTSD related to assault, accidents, disaster, and witnessing death. Alternatively, the sample in Capezzani et al. (2013) was composed of individuals with oncology-related PTSD, but this was the only study entirely composed of individuals with this trauma type. Based on the coding methods, both studies were assigned to the mixed category.
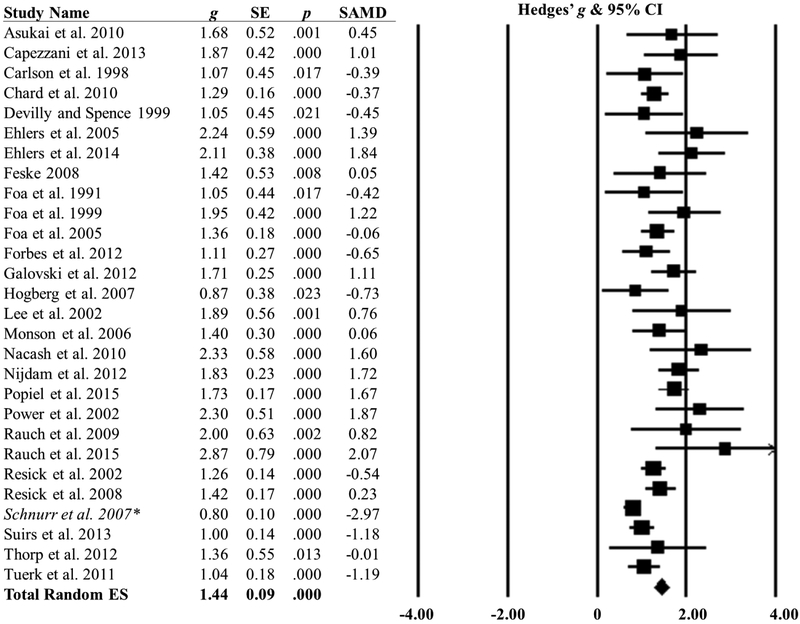
Four military population studies included participants with various trauma types (i.e., Nacash et al., 2011; Rauch et al., 2009; Schnurr et al., 2007; Thorp et al., 2012). For these studies, we contacted the primary author to request sub-sample effect size information for specific trauma types. Schnurr et al. was a military population sample that included participants with exposure to combat, assault (MST and non-military related assault), and other types of trauma types (e.g., accidents). Therefore, the Schnurr et al. study participants were separated into three groups for sub-group analyses by trauma type: combat (n = 7), assault (n = 74), and mixed (n = 30). Nacash et al. included a military population sample that included participants with exposure to combat (n = 10) and terror-related trauma types (n = 5). Participants with exposure to terror-related trauma were assigned to the mixed trauma category because this was the only study that included terror-related trauma. Studies by Rauch et al. (2009) and Thorp et al. (2012) also reported combat, assault, and mixed trauma type categories. However, only the combat trauma participants were included for these two studies because of small sample size (n < 3) in the other trauma categories (see Figure 3). Comprehensive Meta-Analysis will not calculate an effect size for samples this small. One military population study was not included in trauma type analyses, but was included in population analyses because the author could not be reached to provide information on trauma type (i.e., Monson et al., 2006).
Figure 3.
Repeated Measures Trauma Type Subgroup Analysis. g = Hedges’ g; SE = Standard Error; ES = effect size. Three studies were separated by trauma type for trauma type analyses. Two studies included some participants with non-combat traumas, but only the participants with combat trauma were included in the trauma type analysis due to small n in other trauma type categories (i.e., Rauch et al., 2009: n = 8; Thorp et al., 2012: n = 5). One study was separated by trauma type in trauma type analysis as follows: Nacash et al. (2011; n = 10) = Combat, Nacash et al. (2011; n = 5) = Mixed.
The second moderator variable of interest was population type. Study population was coded as either military or civilian. A majority of the included military population studies were comprised of veterans and only one military study was made up of active-duty military service members (i.e., Thorp et al., 2012). When a study sample was composed of military and civilian participants, we contacted the author to request sub-sample effect size information by population type (e.g., Lee et al., 2002).
2.3. Data analytic plan
In order to evaluate treatment outcome differences as a function of trauma type and population, we used random mixed-effects models with repeated measures, with time (pre-post treatment) as the within group variable and trauma type or population type as the between group variable. Hedges’ g was used as a measure of the weighted effect size for within group PTSD symptom severity outcomes (Hedges & Olkin, 1985). PTSD remission rate was also evaluated as a secondary outcome and as a measure of clinically meaningful improvement. PTSD remission was defined as the sample proportion that no longer met diagnostic criteria for PTSD at posttreatment as indicated by an evidence-based diagnostic instrument. Event rates analyses were used to evaluate PTSD remission rates at posttreatment in the total sample. Cochran’s Q was utilized to test group differences in symptom severity and PTSD remission. When appropriate, post-hoc testing was performed using a partitioned chi-square analysis to evaluate groups of three or greater. The partitioned method allows for analysis of k-1 group comparisons that should sum to the total degrees of freedom in the omnibus chi-square. Informal interpretation of general difference across subgroup effect-size estimates were utilized to inform the specified contrast tests.
In this study, a positive effect size sign denotes symptom reduction scores from pretreatment to posttreatment. In instances where a study included multiple outcomes (e.g., PCL and CAPS) or multiple interventions (e.g., PE and CPT), a combined study effect size was calculated (e.g., Resick, Nishith, Weaver, Astin, & Feuer, 2002). Of note, a majority of studies did not report a pre-post score correlation coefficient which is a component of the repeated measures Hedges’ g effect size formula. It is recommended to conduct a sensitivity analysis utilizing a range of plausible correlations when this occurs (Borenstein et al., 2009). However, Borenstein et al. (2009) do not provide specific sensitivity analysis estimates. Therefore, we used Cohen’s (1988) recommended conventional interpretation of a small (.10), medium (.30), and large (.50) correlation coefficients. This provided a range of plausible correlations with a varying degree of impact on pre-post change scores. Overall, findings based on these three correlation coefficients were not meaningfully different. Therefore, a medium pre-post score correlation (.30) was used across studies.
2.4. Preliminary analyses
Prior to evaluating the main hypotheses, we conducted outlier and publication bias analyses. We also evaluated treatment outcome differences across study methodology and descriptive factors to identify any variables that may impact treatment outcomes. We identified potential outlier studies utilizing the sample adjusted-meta-analytic deviance (SAMD) statistic (Huffcutt & Arthur, 1995). The SAMD statistic is based on the difference-in-fit standardized (DFFITS) statistic, which calculates a value approximate to a t distribution with and without that observation included. Values greater than 2.00 are considered large (Huffcutt & Arthur, 1995). However, we selected a cutoff of 2.25, which maximizes the ability to explore group differences (Beal, Corey, & Dunlap, 2000). If a study was identified as an outlier, this study was removed from the primary model analyses. As the methods for the identification and management of outliers is not universally accepted, findings with potential outlier studies are also reported (Aguinis, Gottfredson, & Joo, 2013).
2.4.1. Publication bias analyses.
Fail-safe N analysis and trim and fill plot procedures were utilized to evaluate publication bias (Rosenthal, 1979; Duval & Tweedie, 2000). The fail-safe N calculates the robustness of significant meta-analytic findings by estimating the number of hypothesized missing studies required to nullify the summary effect. As the number of hypothesized missing studies required to result in null findings increases, there is less reason for concern regarding missing studies. The trim and fill approach estimates an adjusted effect size based on imputed estimates that result in a more symmetrical, unbiased funnel plot. Duval and Tweedie (2000) recommend this method as a sensitivity analysis with an emphasis on identifying how the effect size may change if missing studies exist.
2.4.2. Study and descriptive preliminary analyses.
A series of mixed-effects models and meta-regression analyses were also conducted prior to the main analyses to identify potential influential variables that may impact treatment outcomes and confound our primary aims. We evaluated differences between intervention type, PTSD measure used for diagnosis and outcome, method of PTSD measure administration, statistical analysis method, study year, trial type, gender, attrition, and publication year (see Table 1). When a study did not report specific descriptive information, that study was excluded from that analysis and the missing information was denoted with “NR = not reported” in Table 1. Multiple studies used self-report and clinician interview measures to assess PTSD. We evaluated outcome differences between these two methods prior to creating a combined composite score to rule out measure administration type confounds. We excluded one study (Resick et al., 2002) from the treatment type analysis because this study included both PE and CPT intervention arms.
2.4.3. Heterogeneity statistics.
Heterogeneity of the summary effect size was examined using the Cochran’s Q statistic and I2 index. The Q statistic is based on a chi square distrubution that tests if the observed distribution is significantly larger than expected as indicated by the within group error. As noted previously, the Q statistic can also be used to test group differences in subgroup analyses (Borenstein et al., 2009). Higgins and Thompson (2002) proposed the use of the I2 statistic as a method of determing heterogeneity based on the ratio of true variance to total variance. I2 can be understood as the percentage of between-studies variablitity in the effect esimates. Higgins and Thompson (2002) developed a classification system of I2 values to interpret magnitude. I2 = 25%, I2 = 50%, and I2 = 75% are classified as small, medium, and high cut-off benchmarks, respectively.
Analyses were conducted using Comprehensive Meta-Analysis. The SAMD estimates were calculated based on the recommended formulas (Huffcutt & Arthur, 1995). All studies were included in analyses unless otherwise specified in the text or indicated in tables and figures as missing or excluded.
3. Results
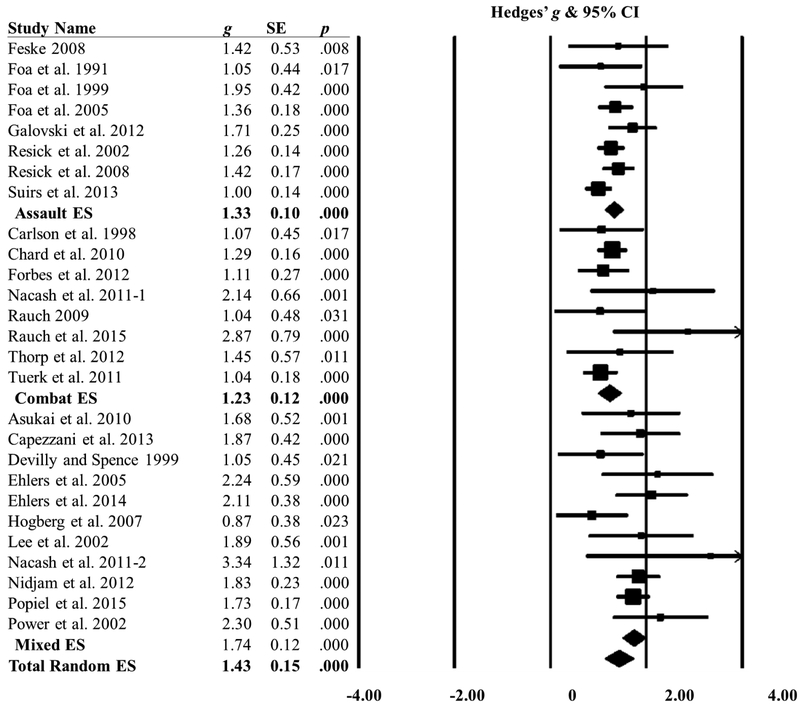
3.1. Total effect size analyses
Study characteristics are displayed in Table 1. The n across studies ranged from 8 to 141 and there was a total of 1,228 participants. Results yielded a large repeated measure total effect size across all studies, g = 1.44, SE = .09, p < .001. The total summary repeated measure effect size information is presented in Figure 2. Heterogeneity analyses of the summary effect with all included studies suggested there was not a common effect size across studies, and mixed effect subgroup analysis was warranted, Q (27) = 75.49, p < .001, I2 = 64.23.
Figure 2.
Repeated Measures Treatment Effect Sizes with SAMD. N = 1,228; g = Hedges’ g; SE = Standard Error; SAMD = sample adjusted-meta-analytic deviance; ES = effect size.
*The study was identified as an outlier based n the SAMD statistic > 2.25. The total random effect size increased, g = 1.46, SE = .08 , p < .001, with the outlier study (Schnurr et al., 2007) removed from the model.
3.2. Preliminary analyses
Prior to examining trauma type and population, a series of outlier and publication bias analyses were conducted. We also ran a series of mixed-effects models to identify any methodological or descriptive study variables that may impact PTSD treatment outcomes.
3.2.1. SAMD statistic results.
SAMD outlier analyses are presented in Figure 2, and indicate one outlier study (Schnurr et al., 2007; SAMD = −2.97), which was therefore excluded from primary analyses. As exclusion of outliers is not a universally recommended method (Aguinis et al., 2013) and Schnurr et al. was a methodologically rigorous study, we also report outcomes with Schnurr et al. included in the model. Of note, heterogeneity statistics of the total summary effect with Schnurr et al. excluded from the model remained statistically significant (p < .001).
3.2.2. Fail-safe N and trim and fill analyses.
The fail-safe N analysis demonstrated that 5,251 missing studies with no effect of PTSD treatment were necessary to result in a non-significant p value. The funnel plot was slightly asymmetrical in favor of treatment effects. The trim-and fill analysis imputed seven studies opposed to the treatment effect (right) and zero studies in support of the treatment effect. Consideration of the imputed studies resulted in a small decrease (gdiff = −0.13) between the observed effect size (g = 1.44) and imputed effect size (g = 1.31).
3.2.3. Mixed-effects and meta-regression.
A series of preliminary analyses were conducted to evaluate treatment outcomes across descriptive and study methodology variables. Meta-regression analyses indicated that attrition rate was the only variable associated with treatment outcomes, B = −1.121, SE = .57, Z = −1.96, p = .05. Specifically, higher rates of attrition were related to worse treatment effects. All other study methodology and descriptive variables were found to be statistically null, p > .05.
3.3. Treatment outcomes as a function of trauma type and population
Two mixed-effects analyses were performed to evaluate PTSD treatment outcomes as a function of trauma type and population type (see Figures 3 & 4). A significant difference was found between trauma subgroups, Q (2) = 10.07, p = .006. The mixed subgroup demonstrated the largest effect size, g = 1.74, SE = 0.12, p < .001, followed by the assault trauma subgroup, g = 1.33, SE = 0.09, p < .001, and the combat trauma subgroup, g = 1.23, SE = 0.13 p < .001. Post-hoc analyses utilizing a partioned chi-square contrast method were implemented to evaluate differences between groups. Because the mixed trauma group appeared to be different compared to the other two trauma type subgroups, we first evaluated differences between the mixed trauma subgroup and the combined assault and combat subgroups. The second contrast evaluated differences between the assault v. combat subgroups. Findings indicated that the treatment outcome effect in the mixed trauma subgroup was significantly larger than the combined assault/combat comparison, Q (1) = 9.71, p = .002. There was not a statistically significant difference in pre-post change scores between the assault and combat subgroups, Q (1) = 0.36, p = .56.
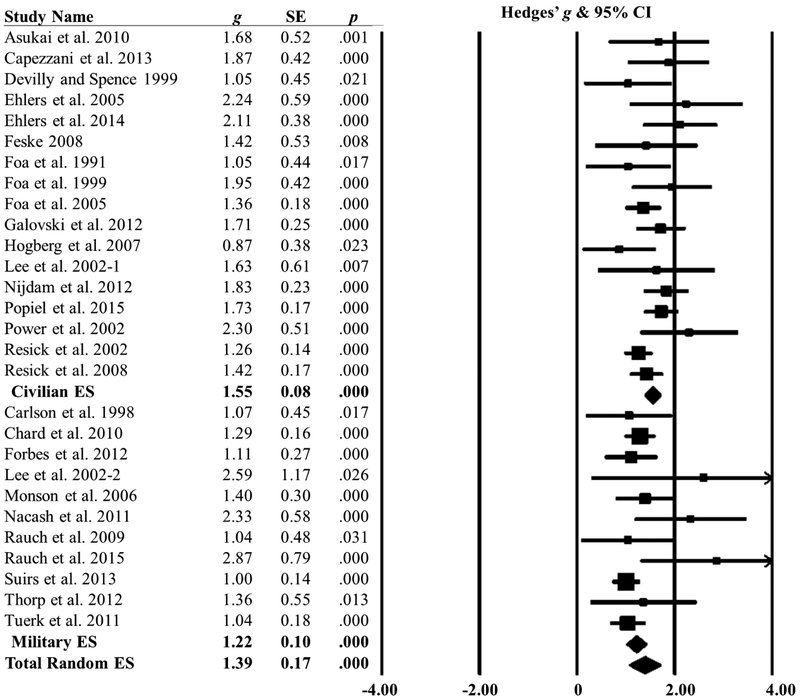
Figure 4.
Repeated Measures Population Type Subgroup Analysis. g = Hedges’ g; SE = Standard Error; ES = effect size. One study included military and civilian participants and therefore was separated by population for population type analyses. Lee et al. (2002) was separated by population type as follows: Lee et al. (2002-1; n = 4) = Military, Lee et al. (2002-2; n = 8) = Civilian.
Population type analyses revealed significant differences in treatment outcomes between civilian and military populations, Q (1) = 6.19, p = .01. Specifically, the military population subgroup, g = 1.22, SE = .10, p < .001 demonstrated a smaller treatment response in comparison to the civilian subgroup, g = 1.55, SE = 0.08, p < .001.
Given that attrition rate was a significant predictor of treatment outcomes, we also evaluated whether there were population differences in attrition rates. Lee et al. (2002) was excluded from analyses as this study was comprised of military and civilians participants. The total sample across studies demonstrated an omnibus attrition rate of approximately 26%. Subgroup analysis indicated there was not a significant difference in attrition between populations, Q (1) = 0.28, p = .60. Both groups had a similar attrition rate, with the military subgroup, 28%, CI (0.21, 0.36), demonstrating a slightly higher rate of attrition compared to civilians, 25%, CI (0.20, 0.31). Trauma type differences in attrition rates were not conducted because attrition information was not available by trauma type for studies that were separated as described (see Section 2.2. Coding Procedures and Definitions).
3.4. PTSD remission rate as a measure of clinically meaningful change
Approximately 59% of participants across studies no longer met criteria for PTSD at posttreatment. Population subgroup analysis were also conducted to evaluate PTSD diagnostic remission differences between military and civilian subgroups. Lee et al. (2002) was excluded from this analyses because this study included military and civilian subgroups. Subgroup analysis indicated that military populations demonstrated poorer rates of PTSD remission at posttreatment compared to civilians, Q (1) = 4.39, p = .04. Specifically, 50%, CI (0.39, 0.62), of the military population subgroup no longer met criteria for PTSD at posttreatment, while 65%, CI (0.57, 0.72), of the civilian population subgroup no longer met criteria for PTSD at posttreatment.
3.5. Results with the outlier study included in models
All analyses were re-evaluated with the Schnurr et al. (2007) outlier study included in the model.1 Preliminary analyses evaluating study and descriptive variables maintained similar patterns and significance levels with Schnurr et al. (2007) included in models. That is, attrition was the only variable that was predictive of treatment outcomes (p < .05). Treatment outcomes did not vary by, nor were treatment outcome predicted by, any other study methodological or descriptive variable (p > .05).
When including the outlier study, trauma type no longer impacted treatment outcome, Q (2) = 3.24, p = .20. Specifically, the mixed trauma subgroup retained the largest effect size, but slightly decreased in magnitude compared to the first model, g = 1.64, SE = 0.18, p < .001; gdiff = −0.10. The combat trauma subgroup went from having the weakest effect in the first model to having the second largest effect in the second model, g = 1.30, SE = 0.20, p < .001; gdiff = 0.07. The assault trauma subgroup demonstrated the poorest treatment effect with the outlier study included in the model, g = 1.22, SE = 0.18, p < .001; gdiff = - 0.11. In contrast, treatment outcome differences as a function of population remained significant when Schnurr et al. (2007) was included in the model, Q (1) = 9.14, p = .003. The civilian subgroup maintained a larger treatment effect size, g = 1.56, SE = 0.09, p < .001; gdiff = 0.00, compared to the military subgroup, g = 1.14, SE = 0.10, p < .001; gdiff = −0.13.
The pattern of PTSD remission rates was essentially unchanged when including the outlier study. That is, 57% of participants no longer met criteria for PTSD at posttreatment. Population differences in PTSD remission rates at posttreatment remained significant, Q (1) = 7.44, p = .006. With Schnurr et al. (2007) included in the model, 48%, CI (0.38, 0.58), of the military population subgroup no longer met criteria for PTSD, whereas 65%, CI (0.58, 0.72), of the civilian population subgroup no longer met criteria for PTSD at posttreatment.
4. Discussion
The primary aim of this meta-analysis was to evaluate PTSD treatment outcomes as a function of trauma type and population. Overall, there were large treatment effect sizes across studies and subgroups, indicating that first-line psychotherapy treatments for PTSD result in significant treatment benefits. Additionally, we evaluated PTSD remission rate as a measure of clinically meaningful change and, on average, 59% of the sample demonstrated PTSD remission at posttreatment. These findings provide additional support for the effectiveness of manualized, first-line psychotherapy treatments for PTSD that are strongly recommended among experts in the field (ISTSS, 2018).
Consistent with our second hypothesis, the combat subgroup benefitted less from treatment than did the mixed trauma subgroup. However, treatment response in the combat trauma subgroup was not different from the assault subgroup. These findings may be because the nature of assault and combat trauma events can be thought of as more severe compared to other trauma events, such as accidents, illness, and disasters. Additionally, assault and combat trauma events can be more chronic or repeated, although this is not always the case. Thus, these findings indicate that manualized, first-line PTSD psychotherapy treatments, although quite effective across trauma types, may be less effective in assault and combat trauma type categories relative to other trauma types.
This outcome is consistent with prior meta-analyses that have also found treatment outcomes variations as a function of trauma type (Bradley et al., 2005; Bisson et al., 2007; Sloan et al., 2013). Although Bradley et al. and Bisson et al. did not conduct specific subgroup test comparisons, both meta-analyses reported smaller treatment effect sizes among combat-related studies. Sloan et al (2013) carried out specific subgroup tests in a sample of group-based PTSD interventions and found that the mixed trauma subgroup demonstrated the largest treatment effect size in comparison to other trauma subgroups, such as combat-related trauma types. This meta-analysis extends this pattern of treatment outcome differences to individual treatments and incorporates assault trauma events.
Trauma type findings in this meta-analysis should be interpreted with consideration of how the outlier impacted results. Variations in trauma type results with the outlier study included v. excluded in the model can potentially be explained by two possibilities. First, the variability in trauma type findings may bring into question the relative importance of trauma type with regard to treatment outcomes. Prior meta-analyses have emphasized difficulties in disentangling trauma type as a factor that impacts treatment outcomes in military populations (Bisson et al., 2007; Bradley et al., 2005; Sloan et al., 2013; Watts et al., 2013). Differences in the statistical stability of trauma type v. population type when the outlier study was included in the model provides a possible indication that population may be a more influential variable.
A second possibility for variations in trauma type analysis with the outlier study included in the model is potentially related to the uniqueness of the Schnurr et al. (2007) study sample. The women in this sample reported varying trauma types including combat, assault, and mixed traumas. Across these three trauma types, women with assault appeared to have particularly poor outcomes (g = 0.26) compared to women with mixed (g = 0.82) and combat (g = 1.16) traumas. Military women in this study endorsed high levels of PTSD symptom severity and a high number of lifetime traumatic exposures (Mtraumas = 10). It is likely that the comparatively smaller effect size (0.80), in this study reflects the high severity of trauma symptoms, the deleterious effects of a high rate of traumatic life events, the unique components of female military populations, and possibly the nature of MST.
Although there is some evidence to suggest that veterans who report MST as their index trauma have poorer PTSD treatment outcomes compared to veterans with combat-related index traumas (Zalta et al., 2018), unlike the Schnurr et al. (2007) subsample, those with MST-related index traumas still demonstrated large treatment effects in our meta-analysis (i.e., Surís et al., 2013). Moreover, there is also evidence indicating negligible difference in treatment outcomes for those with v. without MST (Tiet et al., 2015; Voelkel et al., 2015), which is similar to findings from this meta-analysis related to combat and assault-related traumas. Notably, all of these studies comparing those with MST v. combat trauma evaluated residential and intensive treatment programs. To our knowledge, there are no studies directly comparing treatment outcomes of weekly, first-line psychotherapy treatment for those with and without MST as their index trauma. Unfortunately, we were not able to examine MST as a separate trauma type category from assault in this meta-analysis. It is possible that the rudimentary trauma type categorization coding entirely masked the true effects of trauma type on treatment outcomes. Thus, the impact of trauma type on treatment outcomes warrants further evaluation and remains an empirical question. Future studies should explore how symptom presentation differences between combat-related PTSD and MST impact treatment outcomes.
The military population subgroup demonstrated a poorer treatment response compared to civilians as indicated by effect size differences and PTSD remission rates at posttreatment. This is consistent with our hypothesis and in line with prior meta-analytic results that have highlighted that military populations do not benefit from PTSD psychotherapy treatment to the same degree as civilians (Bisson et al., 2007; Bradley et al., 2005; Sloan et al., 2013; Steenkamp et al., 2015; Watts et al., 2013). Individual factors (e.g., psychiatric comorbidities) and systemic factors (e.g., mental health stigma and secondary gain) have been identified as important variables for consideration with regard to treatment engagement and outcomes in military populations (Bush et al., 2013; Guina et al., 2016; Magruder et al., 2005; McNally & Frueh, 2013 Tarrier et al., 2000). Although prior research has highlighted the importance of considering these factors in psychotherapy treatment, minimal research has evaluated these issues. Therefore, the direct influence of these variables on treatment outcomes remains an empirical question.
Although pre-post treatment effects were large for all trauma and population types, across all groups, more than 40% of individuals continued to meet criteria for PTSD at posttreatment. This was even greater among military populations, half of whom still had PTSD after treatment. These findings are generally consistent with prior literature (Steenkamp et al., 2015), and highlight the dire need to develop ways to improve treatment outcomes even though existing treatments yield large improvements on average. Further, this meta-analysis extends previous PTSD remission rate findings by directly comparing differences between military and civilian populations PTSD remission rates.
Higher rate of attrition was predictive of poorer treatment gains based on exploratory analyses, which is consistent with previous meta-analytic findings (Bradley et al., 2005; Sloan et al., 2013). Factors related to attrition may be different in civilian and military samples. For example, military culture factors, such as mental health stigma and career impact, could affect treatment seeking and attrition in military populations (Bush et al., 2013; Sharp et al., 2015). However, there was not a significant difference in attrition rates between civilians and military subgroups. An absence of attrition rate differences supported previous research showing that attrition rates with first-line psychotherapy treatments for PTSD are a concern across populations (Garcia, Kelley, Rentz, & Lee, 2011; Imel, Laska, Jakcupcak, & Simpson, 2013; Steenkamp et al., 2015). Nonetheless, it is imperative that future research identify and be mindful of specific cultural factors that may lead to attrition across military and civilian populations.
We found no differences in treatment outcomes as a function of gender or age. The absence of gender effects in this study differs from previous PTSD treatment outcome reviews that suggest women experience greater symptom reductions than men (Wade et al., 2016; Watts et al., 2013). This discrepancy with previous research may potentially be explained by our decision to include only manualized, first-line psychotherapy treatments whereas previous meta-analyses included a more liberal criteria. The null findings for age effects were consistent with previous research demonstrating the effectiveness of PTSD treatment across age groups (Clapp & Beck, 2012; Cook, McCarthy, & Thorp, 2017). Taken together, findings from this meta-analysis provide additional support that first-line psychotherapy treatments for PTSD are effective regardless of age or gender.
A final point for discussion is consideration of publication bias. Fail-safe N analyses revealed minimal concerns for publication bias based on the number of studies required to produce a null effect, whereas trim and fill analysis found a slightly asymmetrical funnel plot suggestive of minor publication bias. Although trim and fill analysis produced a slightly asymmetrical funnel plot, the difference between the imputed effect size and the observed effect size was relatively trivial. Additionally, an asymmetrical funnel plot can indicate publication bias, but asymmetry may also be due to different causes other than publication bias, such as heterogeneity (Egger, Davey-Smith, Schneider, & Minder, 1997; Sterne, Egger, & Davey-Smith, 2001). Therefore, the presence of heterogeneity in this meta-analysis is a plausible explanation for the asymmetrical funnel plot. While publication bias was present to a degree in this study, and is an important consideration across meta-analyses, the presence of symmetry and small effect size difference between observed and imputed estimates provides an increased degree of confidence in findings from this meta-analysis.
4.1. Limitations
Several limitations should be noted from this review. First, there were a limited number of trials that utilized a first-line, manualized psychotherapy treatment for PTSD and provided information on specific trauma types that yielded effect size data. Review of the literature suggested that specific trauma type information was not consistently provided across trials and typically only a brief description of trauma type was provided, with insufficient information to parse apart trauma type by outcome effects. This trend was present across trauma types included in this study and resulted in utilizing broad categories (e.g., Mixed) to develop an adequate number of trauma type subgroups. The use of broad, generalized trauma categories may have masked treatment outcomes effects by trauma type and may also explain variations in trauma type findings discussed above. Additionally, there were challenges in defining trauma type in military-related studies. A number of studies utilized the term military-related trauma which was representative of a variety of trauma types, such as MST, combat trauma, training accidents, and in some cases traumas that may have occurred outside of the military. We directly contacted authors to parse apart trauma differences in military studies. However, there were limitations in data availability, which in turn resulted in a slightly rudimentary categorization of study samples. Additionally, individuals were categorized into specific trauma groups based on their presenting trauma event (i.e., index event); however, it is likely many individuals across studies had experienced multiple traumas in their lifetime that were representative of different trauma categories. All these factors may have impacted trauma type results and findings should be interpreted within the context of these limitations. This meta-analysis highlights the challenges of evaluating trauma type based on how this information is reported in the literature. The question as to whether treatment outcomes vary as a function of trauma type requires further investigation.
Another limitation is that we were unable to evaluate potential differences between active-duty military and veteran populations because the military sample in this meta-analysis was almost entirely composed of veterans. We were also unable to evaluate various systemic and individual factors that may impact psychological treatment among active-duty military service members v. veterans. Indeed, previous research has identified individual and systemic differences between active-duty and veteran populations, such as stigma, career threat, avoidance of deployment, and secondary gain (Guina et al., 2016; McNally & Frueh, 2013). These factors may result in symptom minimization or exaggeration, influence motivation to seek or to benefit from treatment, and may vary across active-duty and veteran populations. Future research should evaluate such potential differences between active-duty military and veteran populations.
A final limitation to note is the generalizability of findings to alternative treatment types, treatment modalities, and treatment settings that were excluded from this meta-analysis, such as teletherapy, group therapy, and residential treatment settings. Our rationale to include only select interventions was to mitigate confounding variables and focus exclusively on highly recommended PTSD treatments. Although such interventions were excluded from this study, these methods have displayed positive evidence for military populations (e.g., Zalta et al., 2018). Findings should be interpreted within the context of the included treatment types, treatment modalities, and treatment settings. Moreover, future research should explore whether alternative methods of treatment delivery can help to improve treatment response for military populations.
4.2. Conclusions
Overall, first-line, manualized psychotherapies for PTSD appear to be very effective in ameliorating symptoms of PTSD across populations and trauma types. Despite the effectiveness of these treatments, military populations demonstrated worse treatment outcomes compared to civilians, and these differences appear to be robust. In contrast, specific trauma types that may be more severe in nature (e.g., assault and combat) were associated with poorer treatment response compared to other trauma types. Trauma type appeared to be a less robust finding and the inclusion of one outlier study resulted in trauma type differences becoming non-significant. Hence, the impact of trauma type warrants further investigation. Finally, a large minority of individuals across all groups did not achieve remission, and this number was particularly large in the military group. Together, these data highlight the necessity of continued efforts to improve treatment outcomes.
Declarations of Interest:
Alyson Zalta is supported by a career development award from the National Institute of Mental Health (K23 MH103394). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Submission Declaration: This manuscript has not been published previously and is not under consideration for publication elsewhere. This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Footnotes
All analyses were also evaluated with only the RCT studies included in the model (with and without the outlier study). Effect size statistics and the pattern of results were essentially unchanged (gdiff = ± 0.01) in comparison to the results reported in text.
References marked with an asterisk denote studies included in the meta-analysis.
References2
- Aguinis H, Gottfredson RK, & Joo H (2013). Best-practice recommendations for defining, identifying, and handling outliers. Organizational Research Methods, 16, 270–301. [Google Scholar]
- American Psychological Association (APA). (2017). Clinical practice guidelines for the treatment of PTSD in adults. Retrieved from: https://www.apa.org/ptsd-guideline/index
- American Psychiatric Association. (1980). Diagnostic and statistical manual of mental disorders (3rd ed.). Washington, DC: American Psychiatric Association. [Google Scholar]
- *.Asukai N, Saito A, Tsuruta N, Kishimoto J, Nishikawa T (2010). Efficacy of exposure therapy for Japanese patients with posttraumatic stress disorder due to mixed traumatic events: A randomized controlled study. Journal of Traumatic Stress, 23, 744–50. [DOI] [PubMed] [Google Scholar]
- Beal DJ, Corey DM, & Dunlap WP (2002). On the bias of Huffcutt and Arthur’s (1995) procedure for identifying outliers in the meta-analysis of correlations. The Journal of Applied Psychology, 87(3), 583–89. [DOI] [PubMed] [Google Scholar]
- Bisson J, Ehlers A, Matthews R, Piling S, Richards D, & Turner S (2007). Psychological treatments for chronic post-traumatic stress disorder: Systematic review and meta-analysis. The British Journal of Psychiatry, 190, 97–104. [DOI] [PubMed] [Google Scholar]
- Borenstein M, Hedges LV, Higgins JP, & Rothstein HR (2009). Introduction to meta-analysis. Hoboken, NJ: Wiley. [Google Scholar]
- Bradley R, Greene J, Russ E, Dutra L, & Westen D (2005). A multidimensional meta-analysis of psychotherapy for PTSD. The American Journal of Psychiatry, 162, 214–27. [DOI] [PubMed] [Google Scholar]
- Bush NE, Sheppard SC, Fantelli E, Bell KR, & Reger MA (2013). Recruitment and attrition issues in military clinical trials and health research studies. Military Medicine, 178, 1157–63. [DOI] [PubMed] [Google Scholar]
- *.Capezzani L, Ostacoli L, Cavallo M, Carletto S, Fernandez I, Solomon R, … & Cantelmi T (2013). EMDR and CBT for cancer patients: Comparative study of effects on PTSD, anxiety, and depression. Journal of EMDR Practice and Research, 7, 134–43. [Google Scholar]
- *.Carlson JG, Chemtob CM, Rusnak K, Hedlund NL, & Muraoka MY (1998). Eye movement desensitization and reprocessing (EMDR) treatment for combat-related posttraumatic stress disorder. Journal of Traumatic Stress, 11, 3–24. [DOI] [PubMed] [Google Scholar]
- Carroll KK, Lofengren AM, Weaver DC, Held P, Klassen BJ, Smith DL, … & Zalta AK (2018). Negative posttraumatic cognitions among military sexual trauma survivors. Journal of Affective Disorders, 238, 88–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Chard K, Schumm JA, Owens GP, & Cottingham SM (2010). A comparison of OEF and OIF and Vietnam veterans receiving outpatient cognitive processing therapy. Journal of Traumatic Stress, 23, 25–32. [DOI] [PubMed] [Google Scholar]
- Clapp JD, & Beck JG (2012). Treatment of PTSD in older adults: Do cognitive-behavioral interventions remain viable? Cognitive and Behavioral Practice, 19, 126–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen J (1988). Statistical power analysis for the behavioral sciences (2nd ed.). Hillsdale, NJ: Lawrence Earlbaum Associates. [Google Scholar]
- Cook JM, McCarthy E, & Thorp SR (2017). Older adults with PTSD: Brief state of research and evidence-based psychotherapy case illustration. American Journal of Geriatric Psychiatry, 25, 522–30. [DOI] [PubMed] [Google Scholar]
- Cusack K, Jonas DE, Forneris CA, Wines C, Sonis J, Cook-Middleton J, … & Gaynes BN (2016). Psychological treatments for adults with posttraumatic stress disorder: A systematic review and meta-analysis. Clinical Psychology Review, 43, 128–41. [DOI] [PubMed] [Google Scholar]
- *.Devilly GJ, & Spence SH (1999). The relative efficacy and treatment distress of EMDR and a cognitive-behavior trauma treatment protocol in the amelioration of posttraumatic stress disorder. Journal of Anxiety Disorders, 13, 131–57. [DOI] [PubMed] [Google Scholar]
- Duffy M, Gillespie K, Clark DM (2007). Post-traumatic stress disorder in the context of terrorism and other civil conflict in Northern Ireland: Randomised controlled trial. British Medical Journal, 334, 1147–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duval S, & Tweedie R (2000). Trim and fill: A simple funnel-plot-based method of testing and adjusting for publication bias in meta-analysis. Biometrics, 56, 455–63. [DOI] [PubMed] [Google Scholar]
- Egger M, Davey-Smith G, Schneider M, & Minder C (1997). Bias in meta-analysis detected by a simple, graphical test. British Medical Journal, 315, 629–634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Ehlers A, Clark DM, Hackman A, McManus F, & Fennell M (2005). Cognitive therapy for post-traumatic stress disorder: Development and evaluation. Behaviour Research and Therapy, 43, 413–31. [DOI] [PubMed] [Google Scholar]
- *.Ehlers A, Hackman A, Grey N, Wild J, Liness S, Albert I, … & Clark DM (2014). A randomized controlled trial of 7-day intensive and standard weekly cognitive therapy for PTSD and emotion-focused supportive therapy. The American Journal of Psychiatry, 171, 294–304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Feske U (2008). Treating low-income and minority women with posttraumatic stress disorder: A pilot study comparing prolonged exposure and treatment as usual conducted by community therapists. Journal of Interpersonal Violence, 23, 1027–40. [DOI] [PubMed] [Google Scholar]
- *.Foa EB, Dancu CV, Hembree EA, Jaycox LH, Meadows EA, & Street GP (1999). A comparison of exposure therapy, stress inoculation training, and their combination for reducing posttraumatic stress disorder in female assault victims. Journal of Consulting and Clinical Psychology, 67(5), 194–200. [DOI] [PubMed] [Google Scholar]
- *.Foa EB, Hembree EA, Cahill SP, Rauch SA, Riggs DS, Feeny NC, & Yadin E (2005). Journal of Consulting and Clinical Psychology, 73(5), 953–64. [DOI] [PubMed] [Google Scholar]
- Foa EB, Keane TM, Friedman MJ, & Cohen JA (Eds.). (2009). Effective treatments for PTSD (2n ed.). New York, NY: Guilford Press. [Google Scholar]
- *.Foa EB, Rothbaum BO, Riggs DS, & Murdock TB (1991). Treatment of posttraumatic stress disorder in rape victims: A comparison between cognitive-behavioral procedures and counseling. Journal of Consulting and Clinical Psychology, 59(5), 715–23. [DOI] [PubMed] [Google Scholar]
- *.Forbes D, Lloyd D, Nixon RD, Elliott P, Varker T, Perry D, … & Creamer M (2012). A multisite randomized controlled effectiveness trial of cognitive processing therapy for military-related posttraumatic stress disorder. Journal of Anxiety Disorder, 26, 442–52. [DOI] [PubMed] [Google Scholar]
- *.Galovski TE, Blain LM, Mott JM, Elwood L, & Houle T (2012). Manualized therapy for PTSD: Flexing the structure of cognitive processing therapy. Journal of Consulting and Clinical Psychology, 80, 968–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garcia HA, Kelley LP, Rentz TO, & Lee S (2011). Pretreatment predictors of dropout from cognitive behavioral therapy for PTSD in Iraq and Afghanistan war veterans. Psychological Services, 8, 1–11. [Google Scholar]
- Goodson J, Helstrom A, Halpern J, Ferenschack MP, Gillihan SJ, & Powers MB (2011). Treatment of posttraumatic stress disorder in U.S. Combat veterans: A meta-analytic review. Psychological Reports, 109, 573–99. [DOI] [PubMed] [Google Scholar]
- Green JD, Bovin MJ, Erb SE, Lachowicz M, Gorman KR, Rosen RC, … & Marx BP (2015). The effect of enemy combat tactics on PTSD prevalence rates: A comparison of Operation Iraqi Freedom deployment phases in a sample of male and female veterans. Psychological Trauma Theory, Research, Practice, and Policy, 8, 634–40. [DOI] [PubMed] [Google Scholar]
- Guina J, Welton RS, Broderick PJ, Correll TL, & Peirson RP (2016). DSM-5 criteria and its implication for diagnosing PTSD and military service members and veterans. Current Psychiatry Reports, 18, 43. [DOI] [PubMed] [Google Scholar]
- Hedges LV, & Olkin I (1985). Statistical methods for meta-analysis. Orlando, FL: Academic Press. [Google Scholar]
- Higgins JP, & Thompson SG (2002). Quantifying heterogeneity in a meta-analysis. Statistics in Medicine, 21, 1539–58. [DOI] [PubMed] [Google Scholar]
- *.Hӧgberg G, Pagani M, Ӧrjan S, Soares J, Åberg-Wistedt, Tӓrnell B, & Hӓllstrӧm T (2007). On treatment with eye movement desensitization and reprocessing of chronic post-traumatic stress disorder in public transportation workers: A randomized controlled trial. Nordic Journal of Psychiatry, 61, 54–61. [DOI] [PubMed] [Google Scholar]
- Hoge CW, Terhakopian A, Castro CA, Messer SC, & Engel CC (2007). Association of posttraumatic stress disorder with somatic symptoms, health care visits, and absenteeism among Iraq War Veterans. The American Journal of Psychiatry, 164, 150–53. [DOI] [PubMed] [Google Scholar]
- Huffcutt AI, & Arthur W (1995). Development of a new outlier statistic for meta-analytic data. The Journal of Applied Psychology, 80, 327–334. [Google Scholar]
- Imel ZE, Laska K, Jakcupcak M, & Simpson T (2013). Meta-analysis of dropout in treatments for posttraumatic stress disorder. Journal of Consulting and Clinical Psychology, 81, 394–404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Institute of Medicine (IOM). 2008. Treatment of posttraumatic stress disorder: An assessment of the evidence. Washington, DC: The National Academies Press. [Google Scholar]
- International Society for Traumatic Stress Studies (ISTSS). 2018. Posttraumatic stress disorder prevention and treatment guidelines: Methodology and recommendations. Retrieved from: http://www.istss.org/treating-trauma/new-istss-prevention-and-treatment-guidelines.aspx [DOI] [PubMed]
- Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, & Walters EE (2005) Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Archives of General Psychiatry, 62, 593–602. [DOI] [PubMed] [Google Scholar]
- Kline AC, Cooper AA, Rytwinksi NK, & Feeny NC (2018). Long-term efficacy of psychotherapy for posttraumatic stress disorder: A meta-analysis of randomized controlled trials. Clinical Psychology Review, 59, 30–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kok BC, Herrell RK, Thomas JL, & Hoge CW (2012). Posttraumatic stress disorder associated with combat service in Iraq or Afghanistan: Reconciling prevalence differences between studies. The Journal of Nervous and Mental Disease, 200, 444–50. [DOI] [PubMed] [Google Scholar]
- *.Lee C, Gavriel H, Drummond P, Richards J, & Greenwald R (2002). Treatment of ptsd: Stress inoculation training with prolonged exposure compared to EMDR. Journal of Clinical Psychology, 58, 1071–89. [DOI] [PubMed] [Google Scholar]
- Litz B, Stein N, Delaney E, Lebowitz L, Nash WP, Silva C, & Maguen S (2009). Moral injury and moral repair in war veterans: A preliminary model and intervention strategy. Clinical Psychology Review, 29, 695–06. [DOI] [PubMed] [Google Scholar]
- Magruder KM, Frueh BC, Knapp RG, Davis L, Hamner MB, Martin RH, … Arana GW (2005). Prevalence of posttraumatic stress disorder in Veterans Affairs primary care clinics. General Hospital Psychiatry, 27, 169–79. [DOI] [PubMed] [Google Scholar]
- McNally RJ, & Frueh BC (2013). Why are Iraq and Afghanistan War veterans seeking PTSD disability compensation at unprecedented rates? Journal of Anxiety Disorder, 27, 520–26. [DOI] [PubMed] [Google Scholar]
- *.Monson CM, Schnurr PP, Resick PA, Friedman MJ, YoungXu Y, & Stevens SP (2006). Cognitive processing therapy for veterans with military-related posttraumatic stress disorder. Journal of Consulting and Clinical Psychology, 74, 898–907. [DOI] [PubMed] [Google Scholar]
- *.Nacash N, Foa EB, Huppert JD, Tzur D, Fostick L, Dinstein Y, … & Zohar J (2011). Prolonged exposure therapy for combat- and terror-related posttraumatic stress disorder: A randomized control comparison with treatment as usual. The Journal of Clinical Psychiatry, 72, 1174–80. [DOI] [PubMed] [Google Scholar]
- *.Nijdam MJ, Gersons BPR, Reitsma JB, de Jongh A, & Olff M (2012). Brief eclectic psychotherapy v. Eye movement desensitisation and reprocessing therapy for post-traumatic stress disorder: Randomised controlled trial. The British Journal of Psychiatry, 200, 224–31. [DOI] [PubMed] [Google Scholar]
- *.Power K, McGoldrick T, Brown K, Buchanan R, Sharp D, Swanson V, & Karatzias A (2002). A controlled comparison of eye movement desensitization and reprocessing versu exposure plus cognitive restructuring versus waiting list in the treatment of post-traumatic stress disorder. Clinical Psychology and Psychotherapy, 9, 299–318. [Google Scholar]
- *.Popiel A, Zawadzki B, Pragiowska E, & Teichman Y (2015). Prolonged exposure, paroxetine, and the combination in the treatment of PTSD following a motor vehicle accident. A randomized clinical trial – The “TRAKT” study. Journal of Behavior Therapy and Experimental Psychiatry, 48, 17–26. [DOI] [PubMed] [Google Scholar]
- Powers MB, Halpern JM, Ferenshak MP, Gilliahn SJ, & Foa EB (2010). A meta-analytic review of prolonged exposure for posttraumatic stress disorder. Clinical Psychology Review, 30, 635–41. [DOI] [PubMed] [Google Scholar]
- *.Rauch SAM, Defever E, Favorite T, Duroe A, Garrity C, Martis B, & Liberzon (2009). Prolonged exposure for PTSD in a veterans health administration PTSD clinic. Journal of Traumatic Stress, 22, 60–64. [DOI] [PubMed] [Google Scholar]
- *.Rauch SAM, King AP, Abelson J, Tuerk PW, Smith E, Rothbaum BO, … & Liberzon I (2015). Biological and symptom changes in posttraumatic stress disorder treatment: A randomized clinical trial. Depression and Anxiety, 32, 204–12. [DOI] [PubMed] [Google Scholar]
- *.Resick PA, Galovski TE, Uhlmansiek MO, Scher CD, Clum GA, & Young-Xu Y (2008). A randomized clinical trial to dismantle components of cognitive processing therapy for posttraumatic stress disorder in female victims of interpersonal violence. Journal of Consulting and Clinical Psychology, 76, 243–58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Resick PA, Nishith P, Weaver TL, Astin MC, & Feuer CA (2002). A comparison of cognitive-processing therapy with prolonged exposure and a waiting condition for the treatment of chronic posttraumatic stress disorder in female rape victims. Journal of Consulting and Clinical Psychology, 70, 867–79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosenthal R (1979). The ‘file drawer problem’ and tolerance for null results. Psychological Bulletin, 86, 638–41. [Google Scholar]
- *.Schnurr PP, Friedman MJ, Engel CC, Foa EB, Shea MT, Chow BK, … & Bernardy N (2007). Cognitive behavioral therapy for posttraumatic stress disorder in women: A randomized controlled trial. Journal of the American Medical Association, 297, 820–30. [DOI] [PubMed] [Google Scholar]
- Sexton MB, Davis MT, Bennett DC, Morris DH, & Rauch SAM (2018). A psychometric evaluation of the Posttraumatic Cognitions Inventory with Veterans seeking treatment following military trauma exposure. Journal of Affective Disorder, 226, 232–38. [DOI] [PubMed] [Google Scholar]
- Sharp M, Fear NT, Rona RJ, Wessely S, Greenburg N, Jones N, & Goodwin L (2015). Stigma as a barrier to seeking health care among military personnel with mental health problems. Epidemilogic Reviews, 37, 144–62. [DOI] [PubMed] [Google Scholar]
- Sifferlin A (2015, August). How effective are PTSD treatments for veterans? Retrieved from: http://time.com/3982440/ptsd-veterans/
- Sloan DM, Feinstein BA, Gallagher MW, Beck JG, & Keane TM (2013). Efficacy of group treatment for posttraumatic stress symptoms: A meta-analysis. Psychological Trauma Theory, Research, Practice, and Policy, 5, 176–83. [Google Scholar]
- Steenkamp MM, Litz BT, Hoge CW, & Marmar CR (2015). Psychotherapy for military-related PTSD: A review of randomized clinical trials. Journal of the American Medical Association, 314, 489–500. [DOI] [PubMed] [Google Scholar]
- Stein NR, Mills MA, Arditte K, Mendoza C, Borah AM, Resick PA, Litz BT, & the STRONG STAR Consortium. (2012). A scheme for categorizing traumatic military events. Behavior Modification, 36, 785–805. [DOI] [PubMed] [Google Scholar]
- Sterne JA, Egger M, & Davey-Smith G (2001). Investigating and dealing with publication and other biases in meta-analysis. British Medical Journal, 323, 101–105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- *.Surís A, Link-Malcolm J, Chard K, Ahn C, & North C (2013). A randomized clinical trial of cognitive processing therapy for veterans with PTSD related to military sexual trauma. Journal of Traumatic Stress, 26, 28–37. [DOI] [PubMed] [Google Scholar]
- Taft CT, Watkins LE, Stafford J, Street AE, & Monson CM (2011). Posttraumatic stress disorder and intimate relationship problems: A meta-analysis. Journal of Consulting and Clinical Psychology, 79, 22–33. [DOI] [PubMed] [Google Scholar]
- Tarrier N, Sommerfield C, Pilgrim H, & Faragher B (2000). Factors associated with outcome of cognitive–behavioural treatment of chronic post-traumatic stress disorder. Behaviour Research and Therapy, 38, 191–202. [DOI] [PubMed] [Google Scholar]
- Thomas JL, Wilk JE, Riviere LA, McGurk D, Castro CA, & Hoge CW (2010). Prevalence of mental health problems and functional impairment among active component and National Guard soldiers 3 and 12 months following combat in Iraq. Archives of General Psychiatry, 67, 614–23. [DOI] [PubMed] [Google Scholar]
- *.Thorp SR, Stein MB, Jeste DV, Patterson TL, & Wetherell JL (2012). Prolonged exposure therapy for older veterans with posttraumatic stress disorder: A pilot study, American Journal of Geriatric Psychiatry, 20(3), 276–80. [DOI] [PubMed] [Google Scholar]
- Tiet QQ, Leyva YE, Blau K, Turchik JA, & Rosen CS (2015). Military sexual assault, gender, and PTSD treatment outcomes of US Veterans. Journal of Traumatic Stress, 28, 92–101. [DOI] [PubMed] [Google Scholar]
- *.Tuerk PW, Yoder M, Grubaugh A, Myrick H, Hamner M, & Acierno R (2011). Prolonged exposure therapy for combat-related posttraumatic stress disorder: An examination of treatment effectiveness for veterans of the wars in Afghanistan and Iraq. Journal of Anxiety Disorders, 25, 397–403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- U.S. Department of Veterans Affairs, Department of Defense. VA/DOD clinical practice guideline for the management of posttraumatic stress disorder and acute stress disorder The Management of Posttraumatic Stress Disorder Work Group with support from The Office of Quality, Safety and Value, VA, Washington, DC: & Office of Evidence Based Practice, U.S. Army Medical Command; Version 3.0 – 2017. [Google Scholar]
- Voelkel E, Pukay‐Martin ND, Walter KH, & Chard KM (2015). Effectiveness of cognitive processing therapy for male and female US veterans with and without military sexual trauma. Journal of Traumatic Stress, 28, 174–82. [DOI] [PubMed] [Google Scholar]
- Wade D, Varker T, Kartal D, Hetrick S, O’Donnell M, & Forbes D (2016). Gender difference in outcomes following trauma-focused interventions for posttraumatic stress disorder: Systematic review and meta-analysis. Psychological Trauma Theory, Research, Practice, and Policy, 8, 356–64. [DOI] [PubMed] [Google Scholar]
- Watts BV, Schnurr PP, Mayo L, Young-Xu Y, Weeks WB, & Friedman MJ (2013). Meta-analysis of the efficacy of treatments for posttraumatic stress disorder. The Journal of Clinical Psychiatry, 74, 541–50. [DOI] [PubMed] [Google Scholar]
- Yehuda R, Vermetten E, McFarlane AC, & Lehrner A (2014). PTSD in the military: Special considerations for understanding prevalence, pathophysiology and treatment following deployment. European Journal of Psychotraumatology, 5, 1–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zalta AK, Held P, Smith DL, Klassen BJ, Lofgreen AM, Normand PS, … & Karnik NS (2018). Evaluating patterns and predictors of symptom change during a three-week intensive outpatient treatment for veterans with PTSD. BMC Psychiatry, 18, 242. [DOI] [PMC free article] [PubMed] [Google Scholar]