Abstract
Objective:
Incarcerated individuals have high rates of trauma exposure. IPT reduces posttraumatic stress disorder (PTSD) symptoms in non-incarcerated adults, but has not been examined in prison populations. Moreover, little is known about the mechanisms through which IPT reduces PTSD symptoms. The current study investigated the direct and indirect effects of IPT on PTSD symptoms. We hypothesized that IPT would decrease PTSD symptoms by enhancing social support and decreasing loneliness (theorized IPT mechanisms).
Method:
A sub-sample of trauma-exposed participants (n = 168) were drawn from a larger randomized trial (n = 181) of IPT for major depressive disorder among prisoners. We examined a series of mediation models using non-parametric bootstrapping procedures to evaluate the indirect effect of IPT on PTSD symptoms.
Results:
Contrary to hypotheses, the relation between IPT and PTSD symptoms was significantly mediated through improvements in hopelessness and depressive symptoms (mechanisms of cognitive behavioral interventions), rather than through social support and loneliness. Increased social support and decreased loneliness were associated with decreased PTSD symptoms, but IPT did not predict changes in social support or loneliness.
Conclusions:
IPT may reduce PTSD symptoms in depressed prisoners by reducing hopelessness and depression. (ClinicalTrials.gov number NCT01685294)
Keywords: Interpersonal Psychotherapy, Trauma, PTSD, Prison, Intervention
Approximately 50% of incarcerated men and women in America experience at least one traumatic event prior to detainment (Bloom, Owen & Covington, 2003; Briere, Agee & Dietrich, 2016; Sacks, 2004; Wolff, Shi & Siegle, 2009), and nearly half of all inmates report being the victim of an assault or other crime while in custody (Wolff et al., 2009; Wooldredge, 1998). Unsurprisingly, rates of posttraumatic stress disorder (PTSD) in incarcerated populations in the U.S. are elevated (Baranyi, Cassidy, Fazel, Priebe & Mundt, 2018). One recent study suggested that 48% of individuals in prison met criteria for PTSD compared to less than 4% of the general population (Briere et al., 2016; Prins, 2014). Incarcerated individuals with PTSD are also significantly more likely to also experience other forms of psychopathology, specifically Major Depressive Disorder (MDD) (Zlotnick, 1997). Prisoners with co-occurring PTSD and MDD may be at elevated risk for a host of negative outcomes, including increased suicidal behaviors (Oquendo et al., 2005) and greater functional impairment (Campbell et al., 2007) Considered together, this suggests a critical need for interventions that can be effectively delivered in a prison setting to address PTSD symptoms among depressed individuals.
Most interventions for PTSD have focused on cognitive behavioral approaches utilizing exposure modalities. These treatments, including Prolonged Exposure and Cognitive Processing Therapy, are widely used and shown to be efficacious in reducing PTSD symptoms by decreasing hopelessness and distress (Gallagher, 2017; Gallagher & Resick, 2011). However, clinical and practical factors have somewhat limited the utility of this approach in certain populations. For instance, both clients and therapists report discomfort taking part in exposure exercises and research suggests that exposure-based interventions evidence higher rates of attrition (Zeyfert, DeViva, Becker, Pike, Gillock, & Hayes, 2005; Goetter, Bui, Ojserkis, Zakarian, Brendel & Simon, 2015), while less than half of clients demonstrate clinically meaningful improvement across treatment (Mendes, Mello, Passarela, Venture & Mari, 2008). Furthermore, these interventions have not been tested among incarcerated populations because they required highly trained mental health providers, which may be in short supply in many of these settings (Johnson et al., 2016).
In contrast to this approach, an emerging literature suggests the efficacy of interpersonal therapy (IPT) for reducing PTSD symptoms in the general population. Originally developed to treat depressive disorders, IPT is guided by the assumption that psychological symptoms emerge in response to difficulties in interpersonal interactions. IPT focuses on improving social interactions and strengthening important relationships. This approach may be especially relevant for individuals with PTSD, as the disorder is associated with social isolation (Rosen, Adler & Tiet, 2013) and impaired interpersonal functioning (Olatunji, Cisler & Tolin, 2007). Lack of social support and higher rates of loneliness have been found to increase PTSD following exposure to trauma (Hofman, Hahn, Tirabassi & Gaher, 2016; Ozer, Best, Lipsey & Weiss, 2008; Smith, Benight, & Cieslak, 2013), whereas enhanced social support may buffer the impact of traumatic experiences (Paul et al., 2015; Stanley et al., 2018). Given robust evidence to suggest IPT is effective in treating depressive symptoms (de Mello, de Jesus, Bacaltchuk, Verdeli & Neugebauer, 2005), IPT is also well-suited for treating depressed individuals exposed to trauma, relative to exposure-based methods that primarily evidence benefits for anxiety symptoms only. Furthermore, IPT has already been found to be feasible and acceptable for use in prison settings (Johnson & Zlotnick, 2008, 2012; Johnson, Williams & Zlotnick, 2015), and has been effectively delivered by trained nonspecialist providers (Johnson et al., 2016), increasing its ability to be disseminated in justice settings.
Both individual (Bleiberg & Markowitz, 2005) and group-based IPT (Campanini et al., 2010; Krupnik et al., 2008) trials for trauma-exposed adults have demonstrated significant PTSD symptom reduction and improvements in interpersonal functioning following treatment. Research comparing IPT with exposure-based approaches have found comparable symptom outcomes and higher retention rates in the IPT condition than in the exposure conditions (Krupnick, Melnikoff & Reinhard, 2016; Markotwitz et al., 2015). Although initial results are promising, these studies have been largely preliminary and limited by their use of small sample sizes or lack of comparison conditions. Moreover, little attention has been paid to mechanisms of change that may be specifically relevant to PTSD symptoms and the majority of this research was conducted on community-based samples, limiting the generalizability of these findings to vulnerable prison populations.
The current study sought to address these limitations by examining the efficacy of IPT for treating PTSD symptoms in an incarcerated population and identifying specific mechanisms of change. Participants who reported experiencing at least one traumatic life event (n = 168) were drawn from a larger randomized controlled trial (n = 181) of IPT for MDD among prisoners. We hypothesized that IPT would be effective in reducing PTSD symptoms over a 12-week period. Additionally, we hypothesized that improvements in social support and loneliness would mediate the relation between IPT and decreases in PTSD symptoms, in contrast to exposure-based interventions which have traditionally targeted reducing PTSD by decreasing general distress and hopelessness.
Method
Participants and Procedures.
The current study is a secondary analysis of data from a randomized control trial examining the efficacy of implementing IPT for prisoners with MDD, described in detail in Johnson et al., 2019. Participants in the original study included 181 incarcerated individuals recruited from five minimum and medium security prisons in the New England region of the United States. Flyers, announcements, and prison provider referrals were used to identify individuals potentially interested in the study. Interested individuals provided written consent and were then screened privately and individually by study personnel using the Structured Clinical Interview for the Diagnostic and Statistical Manual-IV (SCID; First, 1997). Participants were selected for inclusion based on meeting specific criteria, including (1) meeting DSM-IV-TR criteria for a primary diagnosis of MDD, (2) being incarcerated (and substance use free) for at least 4 weeks, and (3) likely to stay at the facility for at least six months. Exclusion criteria included: (1) an inability to understand English well enough to understand the consent process and participate in group therapy and (2) meeting criteria for lifetime bipolar or primary psychotic disorder. Following randomization, participants completed assessment measures at pre-intervention (T1) and post-intervention which was approximately 12 weeks later (T2).
Individuals were included in the current analysis if they reported being exposed to at least one lifetime physical or sexual trauma on an abbreviated version of the Trauma History Questionnaire (Carlson et al., 2011) at the pre-intervention assessment. Rates of exposure by trauma type varied; however the most widely endorsed items included: “having things thrown at you to scare or hurt you” (71.8%), “having someone try to take something directly from you by force” (57.5%), “having someone attack you with a gun/knife/weapon” (56.9%), and “having a family member beat or push you hard enough to cause injury” (55.8%). Of the 181 individuals participating in the larger study, 168 reported trauma exposure and were included in the current data analyses, 160 of whom also completed the post-intervention assessment battery. The sample ranged in age from 20 to 61 years old (Mage = 39.61, SDage = 10.45), was predominantly male (67.3% male), and reflected the racial/ethnic diversity of the larger incarcerated population, with 61.9% identifying as White, 23.2% identifying as Black/African-American, and 14.9% identifying as another race/ethnicity. In our secondary analysis sample, participants were randomized to receive either treatment as usual (TAU) + IPT (n = 87), or TAU alone (n = 81).
Participants received $10 deposited into their inmate account for completing post-intervention assessment measures. All assessments were completed at the prison and administered by study research assistants who were blinded to treatment condition.
Protocols were approved by the Brown University Institutional Review Board, registered on www.clinicaltrials.gov (NCT01685294), and followed national and international guidelines regarding the ethical conduct of research.
Nine study therapists conducted the IPT sessions. All therapists were employed within the prison at the time of the study; five were mental health clinicians and four were nonspecialist counselors (working in various other roles within the prison system, such as discharge planners and education specialists). All therapists had earned a bachelor’s degree and had at least one year of experience working with incarcerated populations. Therapists were trained and supervised by the last author (Johnson), a certified IPT supervisor (see Johnson et al., 2019 for further details).
Intervention Conditions.
Because of the real-world setting of this trial, participants were randomized to receive IPT plus prison treatment as usual (IPT + TAU) or prison TAU alone for MDD. All met criteria for MDD at baseline, despite the fact that 78% were already receiving some other kind of mental health treatment (including group and/or individual therapy, or medications) at baseline.
IPT plus TAU.
The active intervention condition consisted of manualized, group-based IPT (see Weissman, Markowitz & Klerman, 2000; Wilfley, MacKenzie, Welch, Ayres & Weissman, 2000) as well as any standard treatments traditionally delivered within the prison setting. IPT centers on helping individuals to identify specific interpersonal stressors in their lives and to build interpersonal skills to address the distress associated with these stressors. Interpersonal skills include improving communication, changing expectations around certain relationships, and fostering an effective social support network. Consistent with IPT approaches for the general population, incarcerated participants received 20 90-minute group IPT sessions over the course of 10 weeks as well as four individual sessions. The individual sessions took place before the beginning of group, mid-way through group treatment, at the conclusion of group, and four weeks following the end of group therapy. The content of the individual session focused on helping participants effectively engage in the group sessions and identify appropriate interpersonal goals. Information regarding fidelity is presented elsewhere (see Johnson et al., 2019). Participants were also able to access standard care in the prison (described below).
TAU alone.
Participants in the TAU condition were given referrals to existing mental health resources currently available in the facility. These primarily consisted of psychotropic medication evaluations and treatment. Limited psychosocial treatments, including brief mental health counseling, psychoeducational groups, and residential substance use treatment, were available in some facilities. See Johnson et al., 2019 for more information regarding the frequency of each level of care received. Outside of the current study, IPT was not offered at any participating facility.
Measures.
Perceived Social Support.
The Multidimensional Scale of Perceived Social Support (MSPSS; Zimet, Dahlem, Zimet, & Farley, 1988) was used to measure perceived social support among participants from three sources: family, friends, and significant other. Participants are asked to rate each of 12-items on a Likert scale from (1) very strongly disagree to (7) very strongly agree. Sample items include “I have friends with whom I can share my joys and sorrows” and “my family is willing to help me make decisions.” Higher summed scale scores indicate greater perceived social support. The measure is widely used and evidences strong reliability and validity (Kazarian & McCabe, 1991; Zimet et al., 1988). The coefficient alpha in the current study was 0.93 at both T1 and T2.
Loneliness.
The UCLA Loneliness Scale (Russell, Peplau, & Cutrona, 1980) was used to measure loneliness and isolation. The brief, 10-item version asks participants to respond to items on a rating scale ranging from (0) “I never feel this way” to (4) “I often feel this way.” Items include feeling “unhappy doing so many things alone” and feeling “shut out and excluded by others.” Items are summed to create a total score, with higher scores reflecting more loneliness. The brief version of the scale demonstrates strong psychometric properties in adult populations (Russell, 1996). In the current study, coefficient alpha was 0.85 at T1 and 0.88 at T2.
Hopelessness.
The Beck Hopelessness Scale (BHS; Beck, Weissman, Lester, & Trexler, 1974) consists of 20 yes or no items measuring feelings of hopelessness in the past week. Sample items include “I look forward to the future with hope and enthusiasm” and “the future seems vague and uncertain to me.” Scores range from 0–20 with higher scores indicating greater feelings of hopelessness. The BHS has demonstrated strong psychometric properties in prison populations (e.g. Horon et al., 2013). Coefficient alpha was 0.93 at both T1 and T2.
Depressive Symptoms.
The intereviewer-administered Hamilton Depression Rating Scale (HAM-D; Hamilton, 1960) consists of 21 items assessing depression symptoms. Participants are asked to report the presence of 11 symptoms of depression, including depressed mood and thoughts of suicide, on a five-point rating scale ranging from (0) not present to (4) severe, and nine additional symptoms, including somatic symptoms and diurnal variations, on a scale from (0) absent to (2) severe. The HAM-D is considered the “gold standard” for assessing depression (Worboys, 2013), with higher scores reflecting greater depressive symptomology. In the current study, the coefficient alpha was 0.73 at T1 and 0.88 at T2.
Posttraumatic Stress Disorder Symptoms.
The PTSD Checklist - Civilian Version (PCL-C; Weathers et al., 1991, 1993) is a 17-item measure used to assess DSM-IV symptoms of PTSD in the previous month. Respondents are asked to report the frequency they experienced specific symptoms on a five-point rating scale ranging from (1) not at all to (5) extremely. Sample items include: “repeated, disturbing memories, thoughts, or images, of a stressful experience from the past” and “avoid thinking about or talking about the stressful event.” Items are summed to create a total score, with higher scores indicating greater PTSD. In the current sample, PTSD symptoms ranged from 21 to 85, suggesting all participants reported one or more trauma-related symptoms. The PCL-C demonstrates strong psychometric properties across populations (Wilkins, Lang & Norman, 2011) and the co-efficient alpha in the current study was 0.88 at T1 and 0.94 at T2.
Data Analytic Plan.
First, we evaluated the data for patterns of missing data and univariate normality. Means, standard deviations and bivariate correlations among key study variables were calculated. Using an established minimal clinically important difference (MCID) criterion (Stefanovics, Rosenheck, Jones, Huang, & Krystal, 2017), we also assessed the percent of participants in each condition who reported clinically significant improvements in PTSD symptoms over the course of the intervention. In order to examine our first hypothesis that IPT would predict decreases in PTSD, we evaluated the effect of treatment condition on changes in PTSD symptoms over the course of the 12-week IPT treatment using linear regression analyses. Specifically, we regressed PTSD symptoms at post-intervention onto treatment condition, controlling for pre-intervention PTSD symptoms. Next, we examined our two hypothesized mediators of the relation between treatment and PTSD symptomology: perceived social support and loneliness (see Figure 1). Given research suggesting changes in hopelessness and general distress predicted decreases in PTSD symptoms in CBT-based treatment approaches, two alternative mediators (hopelessness and depressive symptoms, a proxy for general distress) were also evaluated. For each mediation model, post-intervention PTSD symptoms were regressed onto one of the hypothesized mediators. Research utilizing incarcerated samples suggests positive relations between PTSD symptoms and being female (Bebbington et al., 2017), white (Teplin, Abram & McClelland, 1996), and from an older age group (Teplin et al., 1996); thus, we also included participant’s sex, age and race/ethnicity as covariates in all models. No data was missing at T1; missing data at T2 ranged from 4 – 7%. Cases with missing data were listwise deleted by model.
Figure 1.
Proposed Mediation Model
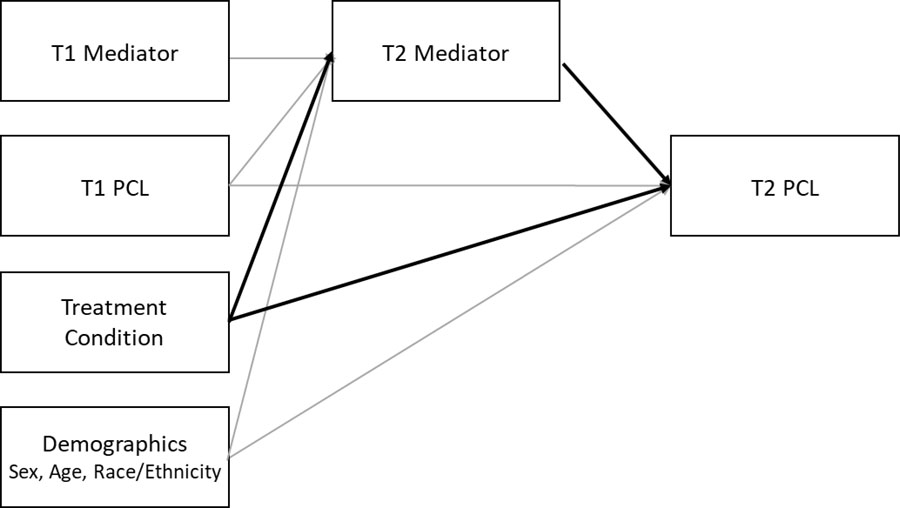
Note. T1 = pre-intervention; T2 = post-intervention. PCL = PTSD Checklist
We utilized non-parametric bootstrapping procedures to evaluate the indirect effect of treatment condition on PTSD symptoms via its relation to our proposed mediators in four separate analyses. Non-parametric bootstrapping utilizes repeated, random sampling with replacement in order to estimate the sampling distribution around the indirect effect. Unlike hypothesis testing based on parametric statistics, bootstrapping procedures do not assume that the indirect effect is normally distributed (Preacher & Hayes, 2008). An indirect effect with a bootstrapped confidence interval that does not contain zero would indicate a statistically significant indirect effect of treatment on PTSD symptoms through each mediator. We utilized the PROCESS Macro in SPSS Version 24 to conduct all mediation analyses with 5,000 bootstrapped samples as recommended by Hayes (2009).
Results
Preliminary Analyses.
Missing data patterns were assessed among all key study variables by examining correlations between baseline variables and treatment completion. Consistent with research suggesting women tend to have shorter sentences than men and were therefore more likely to be released early (Doerner & Demuth, 2010; Stacey & Spohn, 2006), correlation analyses suggest that being female was associated with having missing data at post-treatment (r = .35). There was also a small, but significant, relation between perceived social support and post-treatment study assessment drop-out (r = −.16) indicating that participants with higher perceived support were less likely to complete the post-treatment follow-up assessment.
Next, data were examined for univariate normality; all variables were found to be within acceptable ranges for skew and kurtosis (≤ 3.0). Utilizing PCL clinical cut-offs recommended by Weathers et al. (1993), we found that 53.0% and 33.3% of the sample met criteria for clinically significant levels of PTSD symptoms at pre-treatment and post-treatment, respectively. Means, standard deviations, and correlations between variables are reported in Table 1. Being female was associated with higher levels of perceived social support at both pre- and post-treatment and lower levels of loneliness at post-treatment only. Younger age was also associated with greater perceived social support at post-treatment only.
Table 1.
Means, SDs, and Intercorrelations of Key Study Variables
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | ||
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. | Age | 1.00 | |||||||||
| 2. | Sex (female) | −.20** | 1.00 | ||||||||
| 3. | Race (white) | .12 | .10 | 1.00 | |||||||
| 4. | Condition (IPT) | −.04 | .00 | .06 | 1.00 | ||||||
| 5. | T1 PCL | −.06 | −.00 | −.01 | .08 | 1.00 | |||||
| 6. | T2 PCL | −.06 | −.02 | −.01 | −.04 | .56** | 1.00 | ||||
| 7. | T1 MSPSS | −.10 | .28** | −.02 | −.16* | −.22** | −.24** | 1.00 | |||
| 8. | T2 MSPSS | −.16* | .20** | −.00 | −.02 | −.21** | −.35** | .60** | 1.00 | ||
| 9. | T1 BHS | .12 | −.18* | .08 | .04 | .37** | .42** | −.50** | −.39 ** | 1.00 | |
| 10. | T2 BHS | −.01 | −.08 | −.01 | −.21** | .37** | .65** | −.29** | −.41** | .60** | 1.00 |
| 11. | T1 Ham-D | −.07 | −.08 | −.07 | −.01 | .49** | .48** | −.29** | −.30** | .49** | .43** |
| 12. | T2 Ham-D | .06 | .06 | −.04 | −.13 | .33** | .67** | −.19* | −.30** | .35** | .59** |
| 13. | T1 UCLA | .01 | −.14 | .03 | .11 | .26** | .30** | −.46** | −.28** | .43** | .30** |
| 14. | T2 UCLA | .02 | −.17 | −.12 | −.00 | .33** | .52** | −.37** | −.41** | .44** | .44** |
| Mean (SD) | 39.36 (10.40) | 1.35 (.48) | .62 (.49) | .50 (.50) | 45.71 (12.86) | 39.30 (15.27) | 52.85 (18.73) | 55.21 (17.89) | 7.72 (5.88) | 5.40 (5.37) | |
| N | 168 | 168 | 168 | 168 | 168 | 159 | 168 | 160 | 166 | 160 |
Note. T1 = pre-intervention; T2 = post-intervention. IPT = Interpersonal Therapy; PCL = PTSD Checklist; MSPSS = Multidimensional Scale of Perceived Social Support; BHS = Beck Hopelessness Scale; Ham-D = Hamilton Depression Rating Scale.
p < .05
p < .01
We then examined the percent of participants in each condition who evidenced a change in standardized PCL scores of 0.48 or greater, reflective of a clinically meaningful improvement in symptomology across the intervention (Stefanovics et al., 2017). Results suggest that 27.6% of participants receiving TAU and 38.6% of participants receiving IPT + TAU reported clinically meaningful improvement in PTSD symptoms.
Impact of IPT on PTSD symptoms.
First, we assessed whether there was a direct effect of IPT on changes in PTSD symptoms. We found that only previous levels of PTSD symptoms significantly predicted post-intervention PTSD symptomology: β= .56; p < .001. There was a non-significant trend for individuals in the IPT treatment to report lower levels of post-intervention PTSD symptoms: β= −.12; p = .088.
Indirect effects of perceived social support.
In order to examine our mediation hypotheses, we first evaluated social support as a mediator of the relationship between IPT and post-intervention PTSD symptoms, controlling for baseline levels of social support, PTSD symptoms, sex, age, and race/ethnicity. We found that changes in perceived social support had a significant direct effect on changes in PTSD symptoms (est. = −.16, SE = 0.07, p = .025), suggesting that larger increases in social support were associated with larger decreases in PTSD symptoms. IPT, however, was not associated with changes in perceived social support (est. = 2.37, SE = 2.50, p = .345). Inconsistent with hypotheses, results indicated that there was not a significant indirect effect of treatment on PTSD symptoms through social support (IE = −0.39, SE = 0.49; Bias-Corrected 95% CI = −1.92 to 0.25).
Although findings did not support differential changes in social support between treatment conditions (i.e. IPT + TAU was not associated with greater increases in social support relative to TAU), post-hoc exploratory analyses were conducted to examine changes in social support in the total sample. We evaluated a paired-samples t-test evaluating mean-level differences changes in social support (collapsing across conditions) and found that there was a significant increase in perceived social support in the total sample from pre-intervention (M = 51.80, SD = 18.34) to post-intervention (M = 54.73, SD = 18.05): t(159) = −2.21, p = 0.029. These findings indicate that social support increased in the whole sample, regardless of treatment condition.
Indirect effects of loneliness
Next, we examined loneliness as a mediator of the effect of IPT on post-intervention PTSD symptoms, including all covariates. Results suggest that decreases in loneliness were significantly associated with decreases in PTSD symptoms (est. = 0.45,.SE = 0.21 p = .033). However, IPT was not a significant predictor of reduced loneliness (est. = 0.32, SE = 0.86, p = .708). Moreover, and in contrast to hypotheses, results indicated that there was not a significant indirect effect of IPT on PTSD symptoms (IE = −0.39, SE = 0.49; Bias-Corrected 95% CI = −1.92 to 0.25).
Given results suggesting that treatment condition did not differentially predict changes in loneliness, we conducted additional post-hoc analyses to examine whether there were changes in loneliness across the total sample. We found significant decreases in loneliness from pre-intervention (M = 29.92, SD = 6.06) to post-intervention (M = 27.77, SD = 6.78): t(158) = 4.72, p < 0.001 for both the IPT + TAU and TAU conditions.
Indirect effects of hopelessness
We then examined hopelessness as a mediator of treatment on post-intervention PTSD symptoms, controlling for specified covariates. Findings indicate that decreases in hopelessness were associated with decreases in PTSD symptoms (est. = 0.60, SE = 0.12 p < .001) and that IPT predicted decreases in hopelessness (est. = −2.84,.SE = 1.37 p = .041). Results also suggest a significant indirect effect of IPT on PTSD symptoms via its relation with hopelessness (IE = −1.69, SE = 0.91; Bias-Corrected 95% CI = −3.83 to −0.22). In other words, IPT decreased hopelessness which, in turn, decreased PTSD symptoms1.
Indirect effects of depressive symptoms
Finally, we examined depressive symptoms as a mediator of the relation between IPT and post-intervention PTSD symptoms. Results suggested that decreases in depressive symptoms were significantly related to decreases in PTSD symptoms (est. = 0.88,.SE = 0.10 p < .001) and that IPT predicted decreases in depressive symptoms (est. = −2.99,.SE = 1.32 p = .026). Moreover, findings indicated a significant indirect effect from IPT to post-intervention PTSD symptoms through changes in depressive symptoms (IE = −2.64, SE = 1.24; Bias-Corrected 95% CI = −5.29 to −0.40). Stated differently, IPT was associated with decreases in PTSD symptoms via its impact on decreasing depressive symptoms2.
Discussion
The current study examined the effect of IPT on PTSD symptoms and mechanistic links between treatment and symptom reduction in a sample of incarcerated adults. We found that IPT in conjunction with prison mental health TAU had a marginally significant direct effect on PTSD symptoms relative to prison TAU alone. Inconsistent with hypotheses, however, results suggest that hopelessness and depressive symptoms (a proxy for general distress), rather than perceived social support and loneliness, mediated the relation between treatment and PTSD symptomology. These novel findings suggest that IPT influences posttraumatic symptoms in incarcerated populations through the same mechanisms as CBT, rather than through the anticipated interpersonal mechanisms of increasing social support and decreasing loneliness. In this trial, increased social support and decreased loneliness were associated with decreased PTSD symptoms, but IPT did not predict changes in social support or loneliness.
Our first mediation hypothesis postulated that improvements in interpersonal variables (including perceived social support and loneliness) would drive changes in PTSD symptoms for individuals in IPT + TAU therapy, given extent research indicating that IPT directly improves relationships (Lipsitz & Markowitz, 2013) and that these changes are, in turn, related to decreases in other forms of psychopathology (e.g. depression, Bernecker, 2012; Toth et al., 2013; c.f. Bernecker, Constantino, Pazzaglia, Ravitz & McBride, 2014). This mediation hypothesis was not supported because IPT + TAU did not increase social support or reduce loneliness relative to TAU alone (though it did reduce depressive symptoms and hopelessness differentially). Post-hoc exploratory analyses suggest that, in fact, social support and loneliness significantly improved in the total sample. While it is unclear what drove increases in social support and loneliness in the prison mental health TAU group (see Johnson et al., 2019 for discussion), our results suggested that significant improvements in social support and loneliness were linked to decreases in PTSD symptoms across condition. While it is important to note that the current analyses examined concurrent changes in interpersonal variables and PTSD symptoms and it is not possible to disentangle the temporal precedence of these relations, these findings are consistent with extant literature using general (non-incarcerated) populations that suggest poor interpersonal relationships are one of the strongest predictors of PTSD following trauma exposure (Brewin, Andrews & Valentine, 2000; Ozer, Best, Lipsey & Weiss, 2003). Importantly, recent research suggests these relations may be bi-directional, such that improvements in PTSD symptoms may also drive improved social support (Nickerson et al., 2017). Future research should examine the temporal precedence of changes in symptomology relative to improvement in peer and family relationships.
Unexpectedly, findings indicate that the effect of IPT effects on hopelessness and depressive symptoms appeared were associated with changes in PTSD symptoms over time. While future work examining the temporal ordering of these effects is needed, these preliminary findings are similar to mediation analyses examining the effects of CBT-based approaches on changes in PTSD (e.g. Foa & Kozak, 1986; Gallagher, 2017). Other research utilizing longitudinal methods to directly compare mechanisms of change in IPT and cognitive therapy for depressed adults also found no differences in pathways between treatment and symptom remediation between these approaches; both interventions worked via similar pathways (Lemmens et al., 2017). Lemmens and colleagues (2017) reported that participants in both conditions demonstrated improvement across both cognitive and interpersonal domains, regardless of treatment assignment. The authors theorized that changes in one domain are likely closely associated with changes in other domains; for instance, enhancing interpersonal relationships likely leads to associated improvements in dysfunctional attitudes related to relationships (a hypothesized mediator in cognitive therapy), and that methodological limitations fail to allow researchers to tease apart these micro-level processes.
Other studies have found that improvement in general distress, depression, and hopelessness is associated with subsequent decreases in PTSD symptoms, including decreased avoidance and improved modulation of arousal (Gallagher & Resick, 2012; Gilman, Shumm & Chard, 2012; Glass et al., 2009; Irving et al., 2004). Indeed, increasing levels of hope (regardless of treatment modality) and decreasing distress have been found to be associated with reduced avoidance, hyperarousal and improved emotion regulation among trauma-exposed adults (Bluett, Zoellner & Feeny, 2014; Ford, Grasso, Greene, Slivinsky & DeViva, 2018). Therefore, the improvements observed in depression and hopelessness because of IPT found in this and other studies (e.g. Jiang et al., 2014; Talbot et al., 2005) may be driving some of IPT’s effects on PTSD symptoms. IPT’s emphasis on going over triggering loss or grief experiences in detail may be considered a form of exposure and therefore also related to improvement in PTSD symptoms (see Johnson et al., 2016). Further research taking a more fine-grained and longer-term approach may help elucidate the relative roles of psychological and interpersonal factors in improving symptomology for trauma-exposed incarcerated adults.
While a larger percentage of participants in the IPT + TAU condition evidenced clinically significant changes in PTSD symptomology relative to indiviudals receiving TAU alone, our findings did not suggest a direct effect of the intervention on improving PTSD symptoms. This may reflect a need for future, larger-scale, studies as the tests of the direct path have relatively low power (Kenny & Judd, 2014). It may also point to the need for future research to consider moderators of treatment outcomes. Understanding which interventions work better for whom would allow for more targeted treatment approaches and individualized care.
Strengths, limitations, and future directions
The current study makes a number of unique contributions to the literature by examining specific pathways by which IPT may improve PTSD symptomology in an incarcerated population. First, identifying mechanisms of treatment efficacy is critical to improving our understanding of how specific interventions bring about change (Kazdin, 2007, 2008). Second, the current research utilized a particularly vulnerable sample that is often underrepresented in treatment research: incarcerated adults. Existing evidence on treatment research in correctional settings is largely limited to treatment of serious mental illnesses and substance use disorders (Chandler, Fletcher, & Volkow, 2009; Lynch et al., 2014). Third, our use of a randomized control trial and longitudinal design improved upon existing research (Johnson & Zlotnick, 2012; Zlotnick, Najavits, Rohsenow, & Johnson, 2003) and allowed for evaluating treatment-specific changes in symptomology and the examination of the temporal ordering of these relations.
Limitations to the current study also point to important avenues for future research. First, we were limited to using only two time points of data to assess longitudinal mediation. This did not allow us to consider alternative hypotheses, such as changes in PTSD symptoms driving improvements in interpersonal constructs. Future studies should examine more time points and longer follow-up periods to assess sustained changes in symptoms. Second, participants were selected for inclusion in the current study due to meeting criteria for MDD. Although research suggests approximately half of all individuals with PTSD also report co-occurring depression (Campbell et al., 2007; O’Donnell, Creamer, & Pattison, 2004), there is a need for additional research to understand whether these relations hold for a non-depressed sample. Third, measures of key constructs used in the current study were self-report; therefore, responses may be influenced by social desirability bias or response-shift bias (Rosenman, Tennekoon, & Hill, 2011). Future studies should consider objective and clinician-administered measures of changes specifically in interpersonal domains (such as improved relationships with family members and friends). Fourth, our measure of loneliness (the UCLA Loneliness Scale), although commonly used in the literature, lacks a time frame for response (e.g., past week, past month). The measure would be stronger if a timeframe were provided. Finally, our sub-sample is composed of individuals reporting trauma exposure rather than diagnostic levels of PTSD. This approach allowed us to examine greater variability in symptomology and consider changes in sub-clinical symptoms; however, more research is needed to replicate these findings in adults diagnosed with PTSD.
Conclusions and Clinical Implications
The current study is the first, to our knowledge, to examine specific mechanisms of change in the relation between IPT and PTSD symptoms. Findings indicated that decreases in hopelessness, depressive symptoms, and loneliness and increases in social support were each associated with reductions in PTSD symptoms. However, IPT + TAU reduced hopelessness and depressive symptoms relative TAU alone in this sample, and did not have differential effects on social support or loneliness. This work contributes to clarifying how IPT improves posttraumatic functioning, especially among incarcerated adults with major depression, a psychosocially complex population with numerous psychiatric and physical comorbidities. The effects of IPT on depression and hopelessness may result in improvements in PTSD symptoms. Moreover, IPT is a relatively straightforward intervention to deliver and can be effectively disseminated by Master’s level clinicians, who are typically first line treatment providers in jail and prison settings. Thus, IPT for major depressive disorder may be feasibly and efficaciously delivered in incarcerated populations to produce additional benefits for PTSD symptom reduction.
Acknowledgments
This work was supported in part by the National Institute of Mental Health under Grant R01MH095230 (PI: Jennifer E. Johnson).
Footnotes
The authors report no conflict of interest to report.
Given evolving conceptualizations of PTSD factors, we conducted a series of exploratory analyses using the 5-factor model of PTSD suggested by Reddy et al. 2013. We examined five separate mediation models in which treatment predicted hopelessness which, in turn, predicted each of the five symptom clusters (re-experiencing, anxiety, numbing, dysphoric arousal, and anxious arousal). All models were significant in the same direction as the results presented above utilizing the total score.
We conducted additional parallel exploratory analyses examining depressive symptoms as a mediator of the relation between treatment and each of five PTSD symptom clusters (Reddy et al., 2013). We found the same pattern of relations (reported above) across all models.
References
- Baranyi G, Cassidy M, Fazel S, Priebe S, & Mundt AP (2018). Prevalence of posttraumatic stress disorder in prisoners. Epidemiologic reviews, 40(1), 134–145. 10.1176/appi.ps.201300166 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bebbington P, Jakobowitz S, McKenzie N, Killaspy H, Iveson R, Duffield G, & Kerr M (2017). Assessing needs for psychiatric treatment in prisoners: 1. Prevalence of disorder. Social Psychiatry and Psychiatric Epidemiology, 52(2), 221–229. doi: 10.1007/s00127-016-1311-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beck AT, Weissman A, Lester D, & Trexler L (1974). The measurement of pessimism: the hopelessness scale. Journal of consulting and clinical psychology, 42(6), 861. doi: 10.1037/h0037562 [DOI] [PubMed] [Google Scholar]
- Bernecker SL (2012). How and for whom does interpersonal psychotherapy for depression work. Psychotherapy Bulletin, 47(2), 13–17. doi: 10.1016/j.cpr.2017.07.001 [DOI] [Google Scholar]
- Bernecker SL, Constantino MJ, Pazzaglia AM, Ravitz P, & McBride C (2014). Patient interpersonal and cognitive changes and their relation to outcome in interpersonal psychotherapy for depression. Journal of clinical psychology, 70(6), 518–527. doi: 10.1002/jclp.22038 [DOI] [PubMed] [Google Scholar]
- Bleiberg KL, & Markowitz JC (2005). A pilot study of interpersonal psychotherapy for posttraumatic stress disorder. American Journal of Psychiatry, 162(1), 181–183. doi: 10.1176/appi.ajp.162.1.181 [DOI] [PubMed] [Google Scholar]
- Bloom B, Owen BA, & Covington S (2003). Gender-responsive strategies: Research, practice, and guiding principles for women offenders Washington, DC: US Department of Justice, National Institute of Corrections. doi: 10.1037/e409682005-001 [DOI] [Google Scholar]
- Briere J, Agee E, & Dietrich A (2016). Cumulative trauma and current posttraumatic stress disorder status in general population and inmate samples. Psychological Trauma: Theory, Research, Practice, and Policy, 8(4), 439. doi: 10.1037/tra0000107 [DOI] [PubMed] [Google Scholar]
- Bluett EJ, Zoellner LA, & Feeny NC (2014). Does change in distress matter? Mechanisms of change in prolonged exposure for PTSD. Journal of behavior therapy and experimental psychiatry, 45(1), 97–104. doi: 10.1016/j.jbtep.2013.09.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Campanini RF, Schoedl AF, Pupo MC, Costa ACH, Krupnick JL, & Mello MF (2010). Efficacy of interpersonal therapy‐group format adapted to post‐traumatic stress disorder: an open‐label add‐on trial. Depression and anxiety, 27(1), 72–77. doi: 10.1002/da.20610 [DOI] [PubMed] [Google Scholar]
- Campbell DG, Felker BL, Liu C-F, Yano EM, Kirchner JE, Chan D, . . . Chaney EF (2007). Prevalence of depression–PTSD comorbidity: Implications for clinical practice guidelines and primary care-based interventions. Journal of General Internal Medicine, 22(6), 711–718. doi: 10.1007/s11606-006-0101-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Caruana EJ, Roman M, Hernández-Sánchez J, & Solli P (2015). Longitudinal studies. Journal of Thoracic Disease, 7(11), E537–E540. doi: 10.3978/j.issn.2072-1439.2015.10.63 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chandler RK, Fletcher BW, & Volkow ND (2009). Treating drug abuse and addiction in the criminal justice system: Improving public health and safety. JAMA, 301(2), 183–190. doi: 10.1001/jama.2008.976 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Charuvastra A, & Cloitre M (2008). Social bonds and posttraumatic stress disorder. Annu. Rev. Psychol, 59, 301–328. doi: 10.1146/annurev.psych.58.110405.085650 [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Mello MF, de Jesus Mari J, Bacaltchuk J, Verdeli H, & Neugebauer R (2005). A systematic review of research findings on the efficacy of interpersonal therapy for depressive disorders. European Archives Of Psychiatry And Clinical Neuroscience, 255(2), 75–82. doi: 10.1007/s00406-004-0542-x [DOI] [PubMed] [Google Scholar]
- Doerner JK, & Demuth S (2010). The independent and joint effects of race/ethnicity, gender, and age on sentencing outcomes in US federal courts. Justice Quarterly, 27(1), 1–27. doi: 10.1080/07418820902926197 [DOI] [Google Scholar]
- Dumont DM, Brockmann B, Dickman S, Alexander N, & Rich JD (2012). Public health and the epidemic of incarceration. Annual Review of Public Health, 33, 325–339. doi: 10.1146/annurev-publhealth-031811-124614 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Foa EB, & Kozak MJ (1986). Emotional processing of fear: exposure to corrective information. Psychological bulletin, 99(1), 20. doi: 10.1037//0033-2909.99.1.20 [DOI] [PubMed] [Google Scholar]
- Ford JD, Grasso DJ, Greene CA, Slivinsky M, & DeViva JC (2018). Randomized clinical trial pilot study of prolonged exposure versus present centred affect regulation therapy for PTSD and anger problems with male military combat veterans. Clinical psychology & psychotherapy doi: 10.1002/cpp.2194 [DOI] [PubMed]
- Gallagher K, & Rodricks DJ (2017). Hope despite hopelessness: Race, gender, and the pedagogies of drama/applied theatre as a relational ethic in neoliberal times. Youth Theatre Journal, 31(2), 114–128. doi: 10.1080/08929092.2017.1370625 [DOI] [Google Scholar]
- Gallagher MW, & Resick PA (2012). Mechanisms of change in cognitive processing therapy and prolonged exposure therapy for PTSD: Preliminary evidence for the differential effects of hopelessness and habituation. Cognitive therapy and research, 36(6), 750–755. doi: 10.1037/e533652013-169 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gilman R, Schumm JA, & Chard KM (2012). Hope as a change mechanism in the treatment of posttraumatic stress disorder. Psychological Trauma: Theory, Research, Practice, and Policy, 4(3), 270. doi: 10.1037/a0024252 [DOI] [Google Scholar]
- Glass SJ, & Newman JP (2009). Emotion processing in the criminal psychopath: the role of attention in emotion-facilitated memory. Journal of abnormal psychology, 118(1), 229. doi: 10.1037/a0014866 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grinstead O, Faigeles B, Bancroft C, & Zack B (2001). The financial cost of maintaining relationships with incarcerated African American men: A survey of women prison visitors. Journal of African American Men, 6(1), 59–69. doi: 10.1007/s12111-001-1014-2 [DOI] [Google Scholar]
- Goetter EM, Bui E, Ojserkis RA, Zakarian RJ, Brendel RW, & Simon NM (2015). A systematic review of dropout from psychotherapy for posttraumatic stress disorder among Iraq and Afghanistan combat veterans. Journal of traumatic stress, 28(5), 401–409. doi: 10.1002/jts.22038 [DOI] [PubMed] [Google Scholar]
- Hayes AF (2009). Beyond Baron and Kenny: Statistical mediation analysis in the new millennium. Communication monographs, 76(4), 408–420. doi: 10.1080/03637750903310360 [DOI] [Google Scholar]
- Hofman NL, Hahn AM, Tirabassi CK, & Gaher RM (2016). Social Support, Emotional Intelligence, and Posttraumatic Stress Disorder Symptoms. Journal of Individual Differences doi: 10.1027/1614-0001/a000185 [DOI]
- Horon R, McManus T, Schmollinger J, Barr T, & Jimenez M (2013). A study of the use and interpretation of standardized suicide risk assessment: Measures within a psychiatrically hospitalized correctional population. Suicide and Life-Threatening Behavior, 43(1), 17–38. doi: 10.1111/j.1943-278x.2012.00124.x [DOI] [PubMed] [Google Scholar]
- Irving LM, Snyder CR, Cheavens J, Gravel L, Hanke J, Hilberg P, et al. (2004). The relationships between hope and outcomes at the pretreatment, beginning, and later phases of psychotherapy. Journal of Psychotherapy Integration, 14, 419–443. doi: 10.1037/1053-0479.14.4.419 [DOI] [Google Scholar]
- Jiang RF, Tong HQ, Delucchi KL, Neylan TC, Shi Q, & Meffert SM (2014). Interpersonal psychotherapy versus treatment as usual for PTSD and depression among Sichuan earthquake survivors: a randomized clinical trial. Conflict and health, 8(1), 14. doi: 10.1186/1752-1505-8-14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson JE, Miller TR, Stout RL, Zlotnick C, Cerbo L, Andrade J, Wiltsey-Stirman S (2016). Study protocol: Hybrid Type I cost-effectiveness and implementation study of interpersonal psychotherapy (IPT) for men and women prisoners with major depression. Contemporary Clinical Trials, 47, 266–274. doi: 10.1016/j.cct.2016.01.013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson JE, Price AB, Kao JC, Fernandes K, Stout RL, Gobin R, & Zlotnick C (2016). Interpersonal psychotherapy (IPT) for major depression following perinatal loss: A pilot randomized controlled trial. Archives of Women’s Mental Health, 19(5), 845–859. doi: 10.1007/s00737-016-0625-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson JE, Stout RL, Miller TR, Zlotnick C, Cerbo LA, Andrade JT, ... & Wiltsey-Stirman S (2019). Randomized cost-effectiveness trial of group interpersonal psychotherapy (IPT) for prisoners with major depression. Journal of consulting and clinical psychology doi: 10.1037/ccp0000379 [DOI] [PMC free article] [PubMed]
- Johnson JE, Williams C, & Zlotnick C (2015). Development and feasibility of a cell phone- based transitional intervention for women prisoners with comorbid substance use and depression. The Prison Journal, 95(3), 330–352. doi: 10.1177/0032885515587466 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Johnson JE, & Zlotnick C (2008). A pilot study of group interpersonal psychotherapy for depression in substance abusing female prisoners. Journal of Substance Abuse Treatment, 34, 371–377. doi: 10.1016/j.jsat.2007.05.010 [DOI] [PubMed] [Google Scholar]
- Johnson JE, & Zlotnick C (2012). Pilot study of treatment for major depression among women prisoners with substance use disorder. Journal of psychiatric research, 46(9), 1174–1183. doi: 10.1016/j.jpsychires.2012.05.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kazarian SS, & McCabe SB (1991). Dimensions of social support in the MSPSS: Factorial structure, reliability, and theoretical implications. Journal of Community psychology, 19(2), 150–160. doi: [DOI] [Google Scholar]
- Kazdin AE (2007). Mediators and mechanisms of change in psychotherapy research. Annu. Rev. Clin. Psychol, 3, 1–27. doi: 10.1146/annurev.clinpsy.3.022806.091432 [DOI] [PubMed] [Google Scholar]
- Kazdin AE (2008). Evidence-based treatment and practice: new opportunities to bridge clinical research and practice, enhance the knowledge base, and improve patient care. American Psychologist, 63(3), 146. doi: 10.1037/0003-066x.63.3.146 [DOI] [PubMed] [Google Scholar]
- Keilson J, & Servi LD (1988). A distributional form of Little’s law. Operations Research Letters, 7(5), 223–227. doi: 10.1016/0167-6377(88)90035-1 [DOI] [Google Scholar]
- Kenny DA, & Judd CM (2014). Power anomalies in testing mediation. Psychological Science, 25(2), 334–339. doi: 10.1177/0956797613502676 [DOI] [PubMed] [Google Scholar]
- Krupnick JL, Green BL, Stockton P, Miranda J, Krause E, & Mete M (2008). Groupinterpersonal psychotherapy for low-income women with posttraumatic stress disorder. Psychotherapy Research, 18(5), 497–507. doi: 10.1080/10503300802183678 [DOI] [PubMed] [Google Scholar]
- Krupnick JL, Melnikoff E, & Reinhard M (2016). A pilot study of interpersonal psychotherapy for PTSD in women veterans. Psychiatry, 79(1), 56–69. doi: 10.1080/00332747.2015.1129873 [DOI] [PubMed] [Google Scholar]
- Kubiak SP (2004). The effects of PTSD on treatment adherence, drug relapse, and criminal recidivism in a sample of incarcerated men and women. Research on Social Work Practice, 14(6), 424–433. doi: 10.1177/1049731504265837 [DOI] [Google Scholar]
- Lemmens LH, Galindo-Garre F, Arntz A, Peeters F, Hollon SD, DeRubeis RJ, & Huibers MJ (2017). Exploring mechanisms of change in cognitive therapy and interpersonal psychotherapy for adult depression. Behaviour research and therapy, 94, 81–92. doi: 10.1016/j.brat.2017.05.005 [DOI] [PubMed] [Google Scholar]
- Lipsitz JD, & Markowitz JC (2013). Mechanisms of change in interpersonal therapy (IPT). Clinical psychology review, 33(8), 1134–1147. doi: 10.1016/j.cpr.2013.09.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whalley E (2014). A multisite study of the prevalence of serious mental illness, PTSD, and substance use disorders of women in jail. Psychiatric Services, 65(5), 670–674. doi: 10.1176/appi.ps.201300172 [DOI] [PubMed] [Google Scholar]
- Markowitz JC, Petkova E, Neria Y, Van Meter PE, Zhao Y, Hembree E, ... & Marshall RD (2015). Is exposure necessary? A randomized clinical trial of interpersonal psychotherapy for PTSD. American Journal of Psychiatry, 172(5), 430–440. doi: 10.1176/appi.ajp.2014.14070908 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Massoglia M, & Warner C (2011). The consequences of incarceration. Criminology & Public Policy, 10(3), 851–863. doi: 10.1111/j.1745-9133.2011.00754.x [DOI] [Google Scholar]
- Mendes DD, Mello MF, Venture P, Passarela C,M, & Mari JJ (2008). A systematic review on the effectiveness of cognitive behavioural therapy for posttraumatic stress disorder. International Journal of Psychiatry in Medicine, 38(3), 241–259. doi: 10.2190/pm.38.3.b [DOI] [PubMed] [Google Scholar]
- Nickerson A, Creamer M, Forbes D, McFarlane AC, O’Donnell ML, Silove D, & ... Bryant RA (2017). The longitudinal relationship between post-traumatic stress disorder and perceived social support in survivors of traumatic injury. Psychological Medicine, 47(1), 115–126. doi: 10.1017/S0033291716002361 [DOI] [PubMed] [Google Scholar]
- Nietlisbach G, & Maercker A (2009). Social cognition and interpersonal impairments in trauma survivors with PTSD. Journal of Aggression, Maltreatment & Trauma, 18(4), 382–402. doi: 10.1080/10926770902881489 [DOI] [Google Scholar]
- O’Donnell ML, Creamer M, & Pattison P (2004). Posttraumatic stress disorder and depression following trauma: understanding comorbidity. American Journal of Psychiatry, 161(8), 1390–1396. doi: 10.1176/appi.ajp.161.8.1390 [DOI] [PubMed] [Google Scholar]
- Olatunji BO, Cisler JM, & Tolin DF (2007). Quality of life in the anxiety disorders: a meta-analytic review. Clinical psychology review, 27(5), 572–581. doi: 10.1016/j.cpr.2007.01.015 [DOI] [PubMed] [Google Scholar]
- Oquendo M, Brent DA, Birmaher B, Greenhill L, Kolko D, Stanley B, & ... Mann J (2005). Posttraumatic Stress Disorder Comorbid With Major Depression: Factors Mediating the Association With Suicidal Behavior. The American Journal Of Psychiatry, 162(3), 560–566. doi: 10.1176/appi.ajp.162.3.560 [DOI] [PubMed] [Google Scholar]
- Ozer EJ, Best SR, Lipsey TL, & Weiss DS (2008). Predictors of posttraumatic stress disorder and symptoms in adults: A meta-analysis. Psychological Trauma: Theory, Research, Practice, and Policy, S (1), 3–36. doi: 10.1037/1942-9681.s.1.3 [DOI] [PubMed] [Google Scholar]
- Paul LA, Felton JW, Adams ZW, Welsh K, Miller S, & Ruggiero KJ (2015). Mental health among adolescents exposed to a tornado: the influence of social support and its interactions with sociodemographic characteristics and disaster exposure. Journal of traumatic stress, 28(3), 232–239. doi: 10.1002/jts.22012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Preacher KJ, & Hayes AF (2008). Asymptotic and resampling strategies for assessing and comparing indirect effects in multiple mediator models. Behavior research methods, 40(3), 879–891. doi: 10.3758/brm.40.3.879 [DOI] [PubMed] [Google Scholar]
- Prins SJ (2014). Prevalence of mental illnesses in U.S. state prisons: A systematic review. Psychiatric Services, 65(7), 862–872. 10.1176/appi.ps.201300166 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reddy MK, Anderson BJ, Liebschutz J, & Stein MD (2013). Factor structure of PTSD symptoms in opioid-dependent patients rating their overall trauma history. Drug And Alcohol Dependence, 132(3), 597–602. doi: 10.1016/j.drugalcdep.2013.04.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosen C, Adler E, & Tiet Q (2013). Presenting concerns of veterans entering treatment for posttraumatic stress disorder. Journal of traumatic stress, 26(5), 640–643. doi: 10.1002/jts.21841 [DOI] [PubMed] [Google Scholar]
- Rosenman R, Tennekoon V, & Hill LG (2011). Measuring bias in self-reported data. International Journal of Behavioural and Healthcare Research, 2(4), 320–332. doi: 10.1504/ijbhr.2011.043414 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Russell DW (1996). UCLA Loneliness Scale (Version 3): Reliability, validity, and factor structure. Journal of personality assessment, 66(1), 20–40. doi: 10.1207/s15327752jpa6601_2 [DOI] [PubMed] [Google Scholar]
- Russell D, Peplau LA, & Cutrona CE (1980). The revised UCLA Loneliness Scale: Concurrent and discriminant validity evidence. Journal of personality and social psychology, 39(3), 472. doi: 10.1037//0022-3514.39.3.472 [DOI] [PubMed] [Google Scholar]
- Sacks JY (2004). Women with co‐occurring substance use and mental disorders (COD) in the criminal justice system: a research review. Behavioral Sciences & the Law, 22(4), 449–466. doi: 10.1002/bsl.597 [DOI] [PubMed] [Google Scholar]
- Smith AJ, Benight CC, & Cieslak R (2013). Social support and postdeployment coping self-efficacy as predictors of distress among combat veterans. Military Psychology, 25(5), 452–461. doi: 10.1037/mil0000013 [DOI] [Google Scholar]
- Stacey AM, & Spohn C (2006). Gender and the social costs of sentencing: An analysis of sentences imposed on male and female offenders in three US district courts. Berkeley J. Crim. L, 11, 43. doi: 10.15779/Z38F32G [DOI] [Google Scholar]
- Stanley IH, Hom MA, Chu C, Dougherty SP, Gallyer AJ, Spencer-Thomas S, ... & Sachs-Ericsson NJ (2018). Perceptions of belongingness and social support attenuate PTSD symptom severity among firefighters: A multistudy investigation. Psychological services doi: 10.1037/ser0000240 [DOI] [PMC free article] [PubMed]
- Stefanovics EA, Rosenheck RA, Jones KM, Huang G, & Krystal JH (2017). Minimal clinically important differences (mcid) in assessing outcomes of post-traumatic stress disorder. Psychiatric Quarterly, doi:http://dx.doi.org.proxy2.cl.msu.edu/10.1007/s11126-017-9522-y [DOI] [PubMed]
- Talbot NL, Conwell Y, O’hara MW, Stuart S, Ward EA, Gamble SA,… Tu X (2005). Interpersonal psychotherapy for depressed women with sexual abuse histories: a pilot study in a community mental health center. The Journal of nervous and mental disease, 193(12), 847–850. doi: 10.1097/01.nmd.0000188987.07734.22 [DOI] [PubMed] [Google Scholar]
- Tang TC, Jou SH, Ko CH, Huang SY, & Yen CF (2009). Randomized study of school‐based intensive interpersonal psychotherapy for depressed adolescents with suicidal risk and parasuicide behaviors. Psychiatry and Clinical Neurosciences, 63(4), 463–470. doi: 10.1111/j.1440-1819.2009.01991.x [DOI] [PubMed] [Google Scholar]
- Teplin LA, Abram KM, & McClelland GM (1996). Prevalence of psychiatric disorders among incarcerated women: I. Pretrial jail detainees. Archives of general psychiatry, 53(6), 505–512. doi: 10.1001/archpsyc.1996.01830060047007 [DOI] [PubMed] [Google Scholar]
- Toth SL, Rogosch FA, Oshri A, Gravener-Davis J, Sturm R, & Morgan-López AA (2013). The efficacy of interpersonal psychotherapy for depression among economically disadvantaged mothers. Development and psychopathology, 25(4pt1), 1065–1078. doi: 10.1017/s0954579413000370 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weathers F, Huska J, & Keane T (1991). The PTSD checklist military version (PCL- M) Boston, MA: National Center for PTSD, 42. doi: 10.1037/t05198-000 [DOI] [Google Scholar]
- Weathers LR (1993). U.S. Patent No. 5,219,322 Washington, DC: U.S. Patent and Trademark Office. doi: 10.1016/0172-2190(93)90019-s [DOI] [Google Scholar]
- Weismann MM, Markowitz JC, & Klerman GL (2000). Comprehensive guide to interpersonal psychotherapy New York: Basic Books. doi: 10.1093/med:psych/9780195309416.001.0001 [DOI] [Google Scholar]
- Welch R, Mills M, & Wilfley D(2012-03). Interpersonal Psychotherapy for Group (IPT-G). In Casebook of Interpersonal Psychotherapy New York, NY: Oxford University Press. doi: 10.1093/med:psych/9780199746903.003.0020 [DOI] [Google Scholar]
- Wilkins KC, Lang AJ, & Norman SB (2011). Synthesis of the psychometric properties of the PTSD checklist (PCL) military, civilian, and specific versions. Depression and anxiety, 28(7), 596–606. doi: 10.1002/da.20837 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wolff N (2005). Community reintegration of prisoners with mental illness: A social investment perspective. International journal of law and psychiatry, 28, 43–58. doi: 10.1016/j.ijlp.2004.12.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wolff N, & Draine J (2004). Dynamics of social capital of prisoners and community reentry: Ties that bind? Journal of Correctional Health Care, 10(3), 457–490. doi: 10.1177/107834580301000310 [DOI] [Google Scholar]
- Wolff N, Shi J, & Siegel J (2009). Understanding physical victimization inside prisons: Factors that predict risk. Justice Quarterly, 26(3), 445–475. doi: 10.1080/07418820802427858 [DOI] [Google Scholar]
- Wolff N, Shi J, & Siegel JA (2009). Patterns of victimization among male and femaleinmates: Evidence of an enduring legacy. Violence and victims, 24(4), 469. doi: 10.1891/0886-6708.24.4.469 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wooldredge JD (1998). Inmate lifestyles and opportunities for victimization. Journal of research in crime and delinquency, 35(4), 480–502. doi: 10.1177/0022427898035004006 [DOI] [Google Scholar]
- Worboys M (2013). The Hamilton Rating Scale for Depression: The making of a “gold standard” and the unmaking of a chronic illness, 1960–1980. Chronic illness, 9(3), 202–219. doi: 10.1177/1742395312467658 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zayfert C, DeViva JC, Becker CB, Pike JL, Gillock KL, & Hayes SA (2005). Exposure utilization and completion of cognitive behavioral therapy for PTSD in a “real world” clinical practice. Journal of traumatic stress, 18(6), 637–645. doi: 10.1002/jts.20072 [DOI] [PubMed] [Google Scholar]
- Zimet GD, Dahlem NW, Zimet SG, & Farley GK (1988). The multidimensional scale of perceived social support. Journal of personality assessment, 52(1), 30–41. doi: 10.1207/s15327752jpa5201_2 [DOI] [PubMed] [Google Scholar]
- Zlotnick C (1997). Posttraumatic stress disorder (PTSD), PTSD comorbidity, and childhood abuse among incarcerated women. Journal Of Nervous And Mental Disease, 185(12), 761–763. doi: 10.1097/00005053-199712000-00007 [DOI] [PubMed] [Google Scholar]
- Zlotnick C, Najavits LM, Rohsenow DJ, & Johnson DM (2003). A cognitive-behavioral treatment for incarcerated women with substance abuse disorder and posttraumatic stress disorder: Findings from a pilot study. Journal of Substance Abuse Treatment, 25(2), 99–105. doi: 10.1016/s0740-5472(03)00106-5 [DOI] [PubMed] [Google Scholar]


