Abstract
Objective
The aim of this study was to compare the complication rates and clinical results of labral repair with two suture anchors and capsular plication, and labral repair with three suture anchor fixation in artroscopic Bankart surgery.
Methods
Sixty-nine patients (60 males, 9 females; mean age: 28.2 ± 7.8 years (range: 16–50)) who had undergone arthroscopic repair of a labral Bankart lesion were evaluated. Group A underwent an arthroscopic Bankart repair with three knotless suture anchors, while group B underwent a modified arthroscopic Bankart repair with two knotless suture anchors and an additional capsular plication procedure. The mean follow-up was 52.5 months. Constant Shoulder Score (CSS), Rowe Score (RS), modified UCLA Shoulder Score (mUSS) and range of motion (ROM) were used as outcome measures.
Results
In both groups, a significant improvement was detected in functional outcomes at postoperative last follow-up compared to the preoperative period. No statistically significant difference was found (p > 0.05) in clinical scores (CSS; Group A: 89.7, Group B: 80.2) (RS; Group A: 88.2, Group B: 80.2) (mUSS; Group A: 26.3, Group B: 25.7) external rotation loss (At neutral; Group A: 4.5°, Group B: 5.2°. At abduction; Group A: 4.3°, Group B: 5.7°) and recurrence rates (Group A: 13.3%, Group B: 20.8%). Although the difference was not statistically significant, the recurrence rate was higher in group B (20.8%), compared to group A (13.3%), despite the shorter average follow-up time of group B (p = 0.417).
Conclusions
Arthroscopic repair of labral Bankart lesions with both techniques showed good functional outcomes and stability at the latest follow-up. Higher recurrence rate despite the shorter average follow-up of group B suggests that two anchor usage might not be sufficient for Bankart repair in terms of better stability and less recurrence risk.
Level of evidence
Level III, Therapeutic Study.
Keywords: Traumatic recurrent anterior shoulder instability, Labral Bankart lesion, Arthroscopic repair, Anchor number, Capsular plication, Surgical outcome
Introduction
The repair of labrum with the help of suture anchors has been the standard treatment in patients without significant bone loss. Additional procedures such as capsular shift and plication are defined to reduce joint volume and achieve a more stable joint.1 In the literature, the recurrence rates between 4% and 30% were reported in arthroscopically repaired anteroinferior labral lesions.2, 3, 4, 5
There is no consensus in the literature about the number of minimum suture anchor required in an arthroscopic Bankart repair for better stability. While some authors reported that there is no difference between one, two or three suture anchor repair in terms of stability,6 some others claim that in the treatment of labral Bankart lesions, at least three suture anchors should be used for repair to achieve satisfying stability.7, 8 In this study we hypothesized that addition of capsular plication to a two suture anchor labral Bankart repair can increase the stability by increasing the capsular tension and provide good functional outcome comparable to a three suture anchor repair, in case of three suture anchor repair is not possible due to access problems.
Material and methods
Patient selection
After obtaining the approval of the local Ethics Committee (06-06-2017/A-20), 87 patients (87 consecutive shoulders) who underwent arthroscopic labral Bankart repair surgery due to traumatic recurrent anterior shoulder instability between January 2009 and July 2015 were retrospectively investigated. The patients, who have completed at least 24 months follow-up, were included in the study. All patients had similar size of labral Bankart tear anteroinferiorly, between 3 and 6 o'clock position of the glenoid. The patients with greater tears were not included in the study. The patients with bony Bankart lesion, capsular laxity, SLAP lesion, engaging Hill-Sachs lesion requiring an additional intervention like remplissage procedure, rheumatologic disease, multidirectional shoulder instability, joint laxity, glenohumeral arthrosis, rotator cuff tear, more than 20% glenoid defect, neurological deficit, previous cervical or shoulder surgery and the patients with recurrent instability due to a major trauma after primary surgery were excluded from the study.
Study design
Patients were divided into two groups according to the surgical technique. The patients in group A underwent arthroscopic Bankart repair with three knotless suture anchors, between January 2009 and April 2014. In group B, the patients underwent arthroscopic Bankart repair with two knotless suture anchors and additional capsular plication procedure was performed, between April 2014 and July 2015. The reason behind the change in the surgical technique was the restriction on the number of suture anchors by national health-care insurance regulations of government. After April 2014, National Social Security Administration, which manages national health insurance plan, restricted the maximum applicable number of suture anchors to two, for each Bankart repair operations. We considered this restriction as a compromise for the stability of our repair and we added capsular plication after each labral Bankart repair with two suture anchors to secure our repair and achieve a more stable shoulder joint.
Clinical evaluation
The patients were evaluated preoperatively and postoperatively using the Constant Shoulder Score (CSS), Rowe Score (RS) and modified UCLA Shoulder Score (mUSS).9, 10 The satisfaction component of USS was removed from the questionnaire since it prevents the usage of USS preoperatively. Range of motion (ROM) of the operated shoulders was also recorded. All preoperative evaluations and surgical intervention were performed by the first author. A different surgeon completed the postoperative examinations. The data collection was made prospectively during routine follow-ups, and the clinical outcomes were investigated retrospectively according to the surgical technique.
Preoperative imaging
In all patients, preoperative radiographs of the shoulder were obtained to determine if any bony lesions or arthritis were present. All instability patients were routinely evaluated by magnetic resonance imaging (MRI) before surgery to identify labral Bankart lesion and diagnose concomitant abnormalities.
Surgical technique
All operations were performed in the beach chair position under general anaesthesia by the first author. The standard arthroscopic portals including posterior, anterosuperior, and anteroinferior were established. Diagnostic arthroscopy was performed to assess any intraarticular pathology. The capsulolabral tissue was mobilized from the anterior glenoid surface with an elevator and light decortication was performed in the anterior glenoid neck using arthroscopic rasp to promote healing. Knotless Polyetheretherketone (PEEK) anchors were used in all cases.
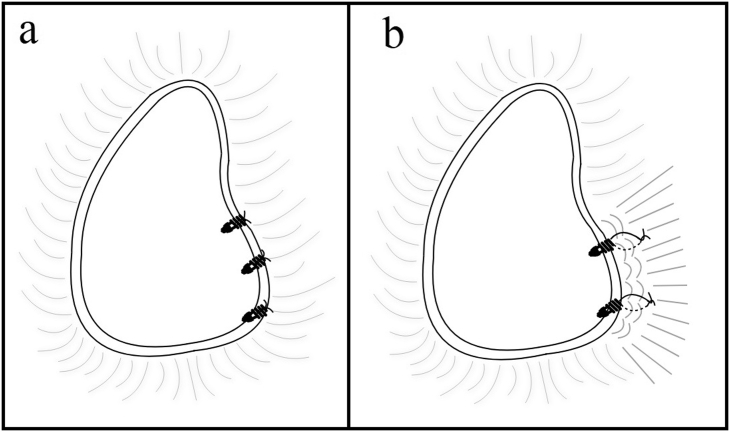
In group A, labrum was penetrated at the most inferior position with a 45° curved suture passing device (Suture Lasso®; Arthrex, Naples, USA or Accupass®, Smith & Nephew, Memphis, USA) through the anteroinferior portal. No:2 non-absorbable suture (FiberWire®, Arthrex, Naples, USA or Ultrabraid®, Smith & Nephew, Memphis, USA) was then pulled through the capsulolabral complex and the other end of the suture was also retrieved through anteroinferior portal. Anchor holes were created on the glenoid surface using a drill at an angle of 50–70 to the plane of the glenoid and 1–2 mm from the glenoid rim. Both ends of the suture were passed through the distal ring of the knotless suture anchor (PushLock® 3.5 mm, Arthrex, Naples, USA in 30 cases & Bioraptor® 2.9 mm, Smith & Nephew, Memphis, USA in 15 cases), which was then inserted and tapped into a drill hole to the desired depth. The other two anchors were inserted appropriately in sequence from inferior to superior. In group A, three knotless suture anchors were used in all cases (Fig. 1).
Fig. 1.
Demonstration of two surgical techniques used in the study. a. Group A underwent an arthroscopic Bankart repair with three knotless suture anchors. b. Group B underwent a modified arthroscopic Bankart repair with two knotless suture anchor and additional capsular plication (Illustration was made using Pages software, version 6.1.1).
In group B, after penetrating the labrum with a suture passing device (Accupass®, Smith & Nephew, Memphis, USA), two knotless suture anchors (Bioraptor® 2.9 mm, Smith & Nephew, Memphis, USA in all cases) were inserted with the same method in sequence from inferior to superior. After anchor insertion, one free end of the inserted anchor was carried to anterosuperior portal. Suture passer was inserted from anteroinferior portal. The capsular tissue was penetrated at 10 mm anterior to the glenoid rim. Both ends of the non-absorbable No:2 suture (Ultrabraid®, Smith & Nephew, Memphis, USA) were taken to anteroinferior portal and tied to each other providing capsular plication. In group B, two knotless suture anchors were used in all cases (Fig. 1). This technique is similar to the technique Sanchez et al described in which they plicated 2–3 mm of the capsule by the help of sutures passing through the anchors for posterior labral repair.11
Then a careful examination with a probe was made in all patients to make sure that the repair is successful, capsulolabral complex is stabile and the labral hump is restored. Routine closure of the portals was performed.
Postoperative rehabilitation
The patients were discharged on the same day or the day after the surgery. A standard postoperative rehabilitation protocol was followed for all patients. The arm was maintained in a simple arm sling for three weeks. Pendulum exercises were started the day after surgery. External rotation exercises and self-assisted active strengthening exercises were started at six weeks after surgery. Non-contact sports were allowed at four months and contact sports were permitted eight months after the operation. Heavy manual work and over-head activities were restricted until postoperative eighth month.
Statistical analyses
The data were analyzed with the SPSS program. Preoperative and postoperative scores were assessed statistically by paired samples t-test, score differences between groups were statistically evaluated by ANCOVA (Analysis of Covariance) method, ROM losses were compared statistically by independent samples t-test and recurrence & revision rates were compared by Pearson's chi-squared test. A p-value < 0.05 was considered statistically significant. Statistical analyses were performed using SPSS program, version 22.0 (SPSS Inc.). Standard Deviation (SD) was used as a measure of dispersion.
Results
Among 84 patients who underwent labral Bankart repair during the study period, 69 patients (60 males, 9 females) met the inclusion criteria and returned for follow-up. 7 patients were lost to follow-up and 8 patients didn't meet the inclusion criteria. The mean patient age was 28.2 years (range: 16–50 years, SD ± 7.8 years). The mean follow-up was; 52.5 months (range: 24–96 months, SD ± 20.6). No superficial or deep infection or intra and postoperative neuro-vascular complications were experienced.
Group A consisted of 45 patients (39 males, 6 females). The mean age was; 28.2 years (SD ± 7.6 years). The mean follow-up was 64.6 months (range: 37–96 months, SD ± 14.7 months). Group B consisted of 24 patients (21 males, 3 females). The mean age was 28.3 years (SD ± 8.2 years). The mean follow-up was 29.8 months (range: 24–38 months, SD ± 4.9 months).
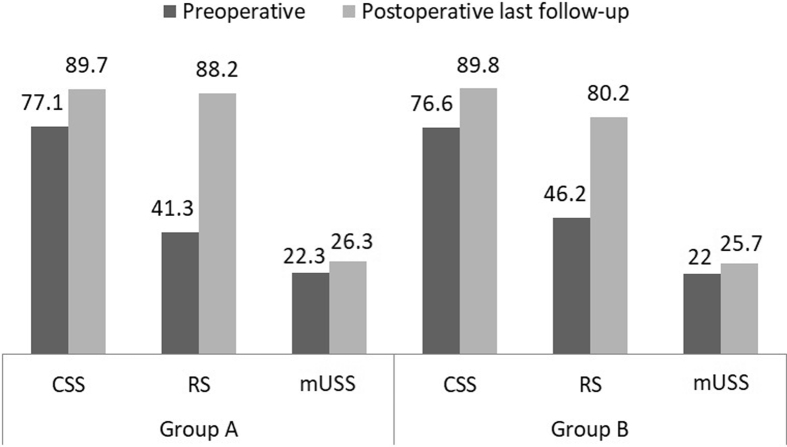
When the treatment groups were compared within themselves in terms of scores before and after surgery, both groups had significant CSS (Group A & B: p < 0.001), RS (Group A & B: p < 0.001) and mUSS (Group A: p < 0.001, Group B: p = 0.012) increase at last follow-up compared to preoperative period (Table 1) (Fig. 2). When the comparison was made between the treatment groups, CSS and mUSS increases were similar, but RS increase was 12.9 points higher in Group A. Although, it was not statistically significant (CSS: p = 0.948, RS: p = 0.138, mUSS: p = 0.590) (Table 2).
Table 1.
Preoperative and postoperative last follow-up scores of the groups with their statistical comparison by ANCOVA (analysis of covariance) method and the associated p-values.
| Preoperative (±SD) | Postoperative last follow-up (±SD) | p Value | ||
|---|---|---|---|---|
| Group A | CSS | 77.1 (±12.6) | 89.7 (±10.6) | <0.001* |
| RS | 41.3 (±10.4) | 88.2 (±20.6) | <0.001* | |
| mUSS | 22.3 (±4.4) | 26.3 (±3.9) | <0.001* | |
| Group B | CSS | 76.6 (±13.4) | 89.8 (±9.7) | <0.001* |
| RS | 46.2 (±10.9) | 80.2 (±24.6) | <0.001* | |
| mUSS | 22 (±4.5) | 25.7 (±4.2) | 0.012* | |
All scores including CSS, RS and mUSS were increased significantly in both groups at last follow-up (p < 0.05) (CSS, Constant Shoulder Score; RS, Rowe Score; mUSS, modified UCLA Shoulder Score) (*) Statistically significant result.
Fig. 2.
Preoperative and postoperative last follow-up scores of the groups. All scores including CSS, RS and mUSS were increased significantly in both groups at last follow-up (p < 0.05) (CSS, Constant Shoulder Score; RS, Rowe Score; mUSS, modified UCLA Shoulder Score).
Table 2.
The score increases of patients between preoperative period and postoperative last follow-up according to the groups with their statistical comparison by paired samples t-test and the associated p-values.
| Mean score increase (±SD) |
p-Value |
||
| Group A | Group B | ||
| CSS | 12.5 (±14.6) | 13.1 (±16.2) | 0.948 |
| RS | 46.8 (±22.3) | 33.9 (±26.6) | 0.138 |
| mUSS | 3.9 (±5.8) | 3.7 (±6.7) | 0.590 |
The score increase differences between groups were not statistically significant (p < 0.05) (CSS, Constant Shoulder Score; RS, Rowe Score; mUSS, modified UCLA Shoulder Score).
In Group A, six patients had recurrent subluxation or dislocation; while in Group B, five patients had recurrence. In Group B, all recurrences developed during first two years after surgery but in Group A, one recurrence developed later than first two years after surgery. When the groups were compared, Group B had higher rate of recurrence but this was not statistically significant (p > 0.05) (Table 3). External rotation losses were compared between two groups. In Group B, external rotation loss was 0.7° higher at neutral position and 1.4° higher at abduction. But these differences were not statistically significant (p > 0.05) (Table 4).
Table 3.
Recurrence rates according to groups with their statistical comparison by Pearson's chi-squared test and the associated p-value.
| Number of cases (%) |
p Value | |||
| Group A | Group B | Total | ||
| Recurrent subluxation or dislocation | 6 (13.3%) | 5 (20.8%) | 11 (15.9%) | 0.417 |
The recurrence rate was higher in Group B but it was not statistically significant (p < 0.05).
Table 4.
Average external rotation loss degrees according to groups [mean degree (range, ±SD)] with their statistical comparison by independent paired t-test and the associated p-value.
| Group A (range, SD) | Group B (range, SD) | p-Value | |
|---|---|---|---|
| ER loss (at neutral) | 4.5 (0–20, ±6.0) | 5.2 (0–23, ±6.2) | 0.646 |
| ER loss (at abduction) | 4.3 (0–21, ±6.1) | 5.7 (0–24, ±7.0) | 0.410 |
The external rotation loss was higher in group B but it was not statistically significant (p < 0.05) (ER, external rotation).
Discussion
In this study, statistically significant clinical improvement was found in patients with labral Bankart lesion repaired arthroscopically by both classical and modified methods, while the comparison of change in functional outcome between the two treatment groups was not statistically significant. External rotation losses were small and not noteworthy functionally. Although the functional scores of both techniques have similar results, the recurrence rate was higher in group B compared to group A. The strength of two anchor repair with capsular plication was not found sufficient in terms of stability and the risk of recurrence.
Generally, arthroscopic Bankart repair is a standard method for most of the traumatic recurrent anterior shoulder instabilities. Some surgeons prefer adding capsular plication or shift to the arthroscopic Bankart repair, to reduce capsular volume and to achieve a more stable shoulder.12, 13, 14, 15, 16 In recent series with arthroscopic labral Bankart repair, recurrence rates are ranging from 4% to 30% but the effect of additional capsular intervention to outcomes is still unclear.3, 4, 17, 18, 19 This is due to the diverse patient groups, concomitant pathologies, different arthroscopic techniques and different criteria for selection of appropriate surgical method. In our retrospective study, we found a recurrence rate of 15.9% in total patient cohort (Group A: 13.3%, Group B: 20.8%) which is consistent with the rates reported in the recent literature. We achieved satisfactory outcomes with both surgical techniques.
Bankart repairs were made with knotless anchors and no complication was experienced due to knotless anchor usage. Knotless suture anchor technique in arthroscopic Bankart repair was defined by Thal.20 Some advantages of this technique include; no need for knot tying, no bulky tied knot in the joint, less time consuming repair and better capsular shift capability.20, 21 In a biomechanical cadaveric study of anterior Bankart repair, Nho et al didn't detect any difference between knotless and conventional suture anchors in terms of single load to failure.22 Garofalo et al and Hayashida et al reported satisfactory clinical results after Bankart repair with knotless anchors.21, 23 Also, in two prospective comparative study by Zhaowen et al and Kocaoglu et al, no difference was found between knot-tying and knotless anchors in terms of clinical outcomes.24, 25
Different techniques were defined for capsular plication procedure to reduce capsular volume and reduce capsular redundancy. The direction of the plication can differ based on the direction of instability and surgeon's preference but anterior plication is mostly preferred when the aim is reducing the anterior redundancy of the capsule in anterior shoulder instabilities. In a recent biomechanical cadaveric study, Mayer et al reported that 10-mm plication restores anterior translation closest to baseline when compared to 5-mm and 15-mm plication.26 Sodl et al also claimed that 10-mm anterior capsular plication reduces glenohumeral range of motion back to the intact state in cadaveric shoulder instability models.27 The capsular plication technique in our study also involved 10-mm of the capsule which is consistent with these biomechanical studies.26, 27
External rotation losses were reported after capsular interventions in several biomechanical and clinical studies.15, 28, 29 In a biomechanical study by Bohnsack et al, anterior capsular shift caused a significant decrease in external rotation.15 Kim et al also found a decrease in only external rotation of the patients who underwent capsular shift surgery.28 Castagna et al reported no external rotation loss with their posteroinferior capsular plication but they determined a loss in the range of forward flexion.29 However, a group of studies reported that capsular plication or shift doesn't affect the range of motion in any direction.30, 31 In a series of 105 patients, Park et al found no significant ROM loss in patients who underwent anterior capsular shift in addition to arthroscopic Bankart repair compared to the patients who underwent arthroscopic Bankart repair only.30 Levy et al also didn't determine any significant external rotation loss with their posteroinferior capsular plication.31 In our study, no significant external rotation loss was found also.
In our study, group B, in which two suture anchors and capsular plication were used for repair due to restrictions by National Social Security Administration, had higher recurrence rates (20.8%) compared to Group A (13.3%), in which three suture anchors were used for repair. In the literature, there is no consensus about the optimum quantity of suture anchors for Bankart repair. In a biomechanical cadaveric study, Martetschlager et al reported that fourth suture anchor does not add strength to three suture anchor repair.32 Witney-Lagen et al claimed that the number of suture anchor doesn't influence the outcome of Bankart repairs.6 In their cohort of 114 patients, they found no difference in outcomes of the patients who underwent Bankart repair with one, two or three suture anchors. They concluded that the important part of the surgery is superomedial shift of the torn capsulolabral tissue, rather than the number of anchors. But also there are some studies reporting that the usage of fewer suture anchors in Bankart repair compromises the stability of the shoulder and might increase the risk of recurrence.7, 8 In their series of 88 patients with Bankart lesion, Kim et al found higher recurrence rates in patients who had anchor number less than three.8 In a study about possible risk factors for recurrence of shoulder instability, Boileau et al also discovered higher recurrence rates in patients who had three anchors or fewer for arthroscopic Bankart repair.7 Even though our result was not statistically significant, when the shorter follow-up times of group B were considered, it might be a valuable result pointing out a similar conclusion with preceding reports which claim fewer suture anchor usage might be related to increased risk of recurrence. If we could have a similar average follow-up time for group B, the recurrence rate could be higher than the existing rate, making this difference statistically significant.
Our study has several strengths. All surgeries were performed by the same surgeon in similar groups of patients with no additional lesions or interventions, which reduced the possible variability in clinical outcomes due to the surgeon skills, patient characteristics or additional pathologies. Prospective data collection makes the results of this study reliable.
This study also has several limitations. The number of patients in Group B was smaller than Group A and the average follow-up time for Group B was shorter than Group A. Disproportionate number of shoulders and follow-up times between two groups might have led to incorrect comparisons between the two groups. Although the clinical data had been collected prospectively, retrospective design of our study is a limitation. Preoperative and postoperative examinations were completed by single but different surgeons, which might have caused inter-observer variability in clinical evaluations. Even though the operations were made by the same surgeon, the all patients in group A underwent surgery before the all patients in group B. It means that the surgeon was more experienced at the time interval which the group B underwent surgery. This is a limitation for our study but actually it makes the results of this study more powerful since the group B has worse functional outcome, suggesting that it could be lower if they were operated at the same time interval with group A. Finally, using two different brand materials with different sizes might have caused variability related to mechanical characteristics of the implants.
Conclusion
Statistically significant clinical improvement was observed in patients with both arthroscopic Bankart repair techniques. The comparison of two different surgical techniques didn't show statistically significant difference regarding clinical outcomes including CSS, RS, mUSS and external rotation loss. Recurrence rate was higher in the group who underwent two anchor repair with capsular plication. Although it was not statistically significant, the higher recurrence rate despite the shorter follow-up of this patient group might suggest that two anchor repair does not provide sufficient stability compared to three anchor repair. Addition of capsular plication might be considered when two suture anchors can be used instead of three due to reasons beyond surgeon's control but more than two anchors should be preferred when available in favour of better shoulder stability and decreased risk of recurrence.
Conflicts of interest
None.
Acknowledgements
Not applicable.
Footnotes
Peer review under responsibility of Turkish Association of Orthopaedics and Traumatology.
Contributor Information
Nuri Aydin, Email: nuriaydin@hotmail.com.
Bedri Karaismailoglu, Email: bedrikio@hotmail.com.
Emir Harbiyeli, Email: emirharbiyeli@hotmail.com.
Mahmut Kursat Ozsahin, Email: drmkursatozsahin@yahoo.com.
References
- 1.Ahmed I., Ashton F., Robinson C.M. Arthroscopic Bankart repair and capsular shift for recurrent anterior shoulder instability. J Bone Joint Surg Am. 2012;94(14):1308–1315. doi: 10.2106/JBJS.J.01983. [DOI] [PubMed] [Google Scholar]
- 2.Burkhart S.S., De Beer J.F. Traumatic glenohumeral bone defects and their relationship to failure of arthroscopic Bankart repairs: significance of the inverted-pear glenoid and the humeral engaging Hill-Sachs lesion. Arthroscopy. 2000;16(7):677–694. doi: 10.1053/jars.2000.17715. [DOI] [PubMed] [Google Scholar]
- 3.Kim S.-H., Ha K., Cho Y.-B., Ryu B., Oh I. Arthroscopic anterior stabilization of the shoulder: two to six-year follow-up. J Bone Joint Surg Am. 2003;85-A(8):1511–1518. [PubMed] [Google Scholar]
- 4.Koss S., Richmond J.C., Woodward J.S., Jr. Two- to five-year followup of arthroscopic Bankart reconstruction using a suture anchor technique. Am J Sport Med. 1997;25(6):809–812. doi: 10.1177/036354659702500613. [DOI] [PubMed] [Google Scholar]
- 5.Çiçek H., Tuhanioğlu Ü., Oğur H.U., Seyfettinoğlu F., Çiloğlu O., Beyzadeoğlu T. Single anterior portal: a better option for arthroscopic treatment of traumatic anterior shoulder instability? Acta Orthop Traumatol Turc. 2017;51(4):298–302. doi: 10.1016/j.aott.2017.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Witney-Lagen C., Perera N., Rubin S., Venkateswaran B. Fewer anchors achieves successful arthroscopic shoulder stabilization surgery: 114 patients with 4 years of follow-up. J Shoulder Elbow Surg. 2014;23(3):382–387. doi: 10.1016/j.jse.2013.08.010. [DOI] [PubMed] [Google Scholar]
- 7.Boileau P., Villalba M., Héry J.Y., Balg F., Ahrens P., Neyton L. Risk factors for recurrence of shoulder instability after arthroscopic Bankart repair. J Bone Joint Surg Am. 2006;88(8):1755–1763. doi: 10.2106/JBJS.E.00817. [DOI] [PubMed] [Google Scholar]
- 8.Kim S.-H., Ha K.-I., Kim S.-H. Bankart repair in traumatic anterior shoulder instability: open versus arthroscopic technique. Arthroscopy. 2002;18(7):755–763. doi: 10.1053/jars.2002.31701. [DOI] [PubMed] [Google Scholar]
- 9.Constant C.R., Murley A.H. A clinical method of functional assessment of the shoulder. Clin Orthop Relat Res. 1987;214(1):160–164. [PubMed] [Google Scholar]
- 10.Amstutz H.C., Sew Hoy A.L., Clarke I.C. UCLA anatomic total shoulder arthroplasty. Clin Orthop Relat Res. 1981;155(2):7–20. https://doi.org/0009-921X/81/0300/007 [PubMed] [Google Scholar]
- 11.Sanchez G., Kennedy N.I., Ferrari M.B., Mannava S., Frangiamore S.J., Provencher M.T. Arthroscopic labral repair in the setting of recurrent posterior shoulder instability. Arthrosc Tech. 2017;6(5):e1789–e1794. doi: 10.1016/j.eats.2017.06.055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gartsman G.M., Roddey T.S., Hammerman S.M. Arthroscopic treatment of bidirectional glenohumeral instability: two- to five-year follow-up. J Shoulder Elbow Surg. 2001;10(1):28–36. doi: 10.1067/mse.2001.109324. [DOI] [PubMed] [Google Scholar]
- 13.Savoie F.H., Field L.D. Thermal versus suture treatment of symptomatic capsular laxity. Clin Sports Med. 2000;19(1):63–75. doi: 10.1016/S0278-5919(05)70296-9. [DOI] [PubMed] [Google Scholar]
- 14.Tibone J.E., McMahon P.J., Shrader T.A., Sandusky M.D., Lee T.Q. Glenohumeral joint translation after arthroscopic, nonablative, thermal capsuloplasty with a laser. Am J Sports Med. 1998;26(4):495–498. doi: 10.1177/03635465980260040301. [DOI] [PubMed] [Google Scholar]
- 15.Bohnsack M., Bartels B., Ostermeier S. Biomechanical stability of an arthroscopic anterior capsular shift and suture anchor repair in anterior shoulder instability: a human cadaveric shoulder model. Knee Surg Sport Traumatol Arthrosc. 2009;17(12):1493–1499. doi: 10.1007/s00167-009-0843-8. [DOI] [PubMed] [Google Scholar]
- 16.Alberta F.G., Elattrache N.S., Mihata T., McGarry M.H., Tibone J.E., Lee T.Q. Arthroscopic anteroinferior suture plication resulting in decreased glenohumeral translation and external rotation. Study of a cadaver model. J Bone Joint Surg Am. 2006;88(1):179–187. doi: 10.2106/JBJS.D.02974. [DOI] [PubMed] [Google Scholar]
- 17.Porcellini G., Campi F., Pegreffi F., Castagna A., Paladini P. Predisposing factors for recurrent shoulder dislocation after arthroscopic treatment. J Bone Joint Surg Am. 2009;91(11):2537–2542. doi: 10.2106/JBJS.H.01126. [DOI] [PubMed] [Google Scholar]
- 18.Flinkkilä T., Hyvönen P., Ohtonen P., Leppilahti J. Arthroscopic Bankart repair: results and risk factors of recurrence of instability. Knee Surg Sport Traumatol Arthrosc. 2010;18(12):1752–1758. doi: 10.1007/s00167-010-1105-5. [DOI] [PubMed] [Google Scholar]
- 19.Voos J.E., Livermore R.W., Feeley B.T. Prospective evaluation of arthroscopic Bankart repairs for anterior instability. Am J Sports Med. 2010;38(2):302–307. doi: 10.1177/0363546509348049. [DOI] [PubMed] [Google Scholar]
- 20.Thal R. A knotless suture anchor: technique for use in arthroscopic Bankart repair. Arthroscopy. 2001;17(2):213–218. doi: 10.1053/jars.2001.20666. [DOI] [PubMed] [Google Scholar]
- 21.Hayashida K., Yoneda M., Mizuno N., Fukushima S., Nakagawa S. Arthroscopic Bankart repair with knotless suture anchor for traumatic anterior shoulder instability: results of short-term follow-up. Arthroscopy. 2006;22(6):620–626. doi: 10.1016/j.arthro.2006.03.006. [DOI] [PubMed] [Google Scholar]
- 22.Nho S.J., Frank R.M., Van Thiel G.S. A biomechanical analysis of anterior Bankart repair using suture anchors. Am J Sports Med. 2010;38(7):1405–1411. doi: 10.1177/0363546509359069. [DOI] [PubMed] [Google Scholar]
- 23.Garofalo R., Mocci A., Moretti B. Arthroscopic treatment of anterior shoulder instability using knotless suture anchors. Arthroscopy. 2005;21(11):1283–1289. doi: 10.1016/j.arthro.2005.08.033. [DOI] [PubMed] [Google Scholar]
- 24.Ng D.Z., Kumar V.P. Arthroscopic Bankart repair using knot-tying versus knotless suture anchors: is there a difference? Arthroscopy. 2014;30(4):422–427. doi: 10.1016/j.arthro.2014.01.005. [DOI] [PubMed] [Google Scholar]
- 25.Kocaoglu B., Guven O., Nalbantoglu U., Aydin N., Haklar U. No difference between knotless sutures and suture anchors in arthroscopic repair of Bankart lesions in collision athletes. Knee Surg Sport Traumatol Arthrosc. 2009;17(7):844–849. doi: 10.1007/s00167-009-0811-3. [DOI] [PubMed] [Google Scholar]
- 26.Mayer S.W., Kraszewski A.P., Skelton A., Kontaxis A., Warren R. What are the effects of capsular plication on translational laxity of the glenohumeral joint: a study in cadaveric shoulders. Clin Orthop Relat Res. 2018 Jul;476(7):1526–1536. doi: 10.1097/01.blo.0000534681.21276.14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Sodl J.F., McGarry M.H., Campbell S.T., Tibone J.E., Lee T.Q. Biomechanical effects of anterior capsular plication and rotator interval closure in simulated anterior shoulder instability. Knee Surg Sport Traumatol Arthrosc. 2016;24(2):365–373. doi: 10.1007/s00167-014-2878-8. [DOI] [PubMed] [Google Scholar]
- 28.Kim D.W., Kim C.K., Jung S.W. An arthroscopic pleated capsular shift for recurrent anterior dislocation of the shoulder. Knee Surg Sport Traumatol Arthrosc. 2012;20(12):2579–2584. doi: 10.1007/s00167-012-1943-4. [DOI] [PubMed] [Google Scholar]
- 29.Castagna A., Borroni M., Delle Rose G. Effects of posterior-inferior capsular plications in range of motion in arthroscopic anterior Bankart repair: a prospective randomized clinical study. Knee Surg Sport Traumatol Arthrosc. 2009;17(2):188–194. doi: 10.1007/s00167-008-0650-7. [DOI] [PubMed] [Google Scholar]
- 30.Park J.-Y., Chung S.W., Kumar G. Factors affecting capsular volume changes and association with outcomes after Bankart repair and capsular shift. Am J Sports Med. 2015;43(2):428–438. doi: 10.1177/0363546514559825. [DOI] [PubMed] [Google Scholar]
- 31.Levy D.M., Gvozdyev B.V., Schulz B.M., Boselli K.J., Ahmad C.S. Arthroscopic anterior shoulder stabilization with percutaneous assistance and posteroinferior capsular plication. Am J Orthop (Belle Mead NJ) 2014;43(8):364–369. [PubMed] [Google Scholar]
- 32.Martetschläger F., Michalski M.P., Jansson K.S., Wijdicks C.A., Millett P.J. Biomechanical evaluation of knotless anterior and posterior Bankart repairs. Knee Surg Sports Traumatol Arthrosc. 2014;22(9):2228–2236. doi: 10.1007/s00167-013-2602-0. [DOI] [PubMed] [Google Scholar]