Abstract
Objective
The aim of this study was to evaluate the behaviour and knowledge skill levels of Turkish orthopedic surgeons about fluoroscopy usage and radiation safety.
Methods
The questionnaire, consisting of nineteen questions, was sent to orthopaedic surgeons and requested by a total of 323 surgeons online. The questions were about personal information, training and behaviours related to radiation and fluoroscopy usage, and the use of protective equipment.
Results
A total of 277 individuals completed the questionnaire. The answers of 180 surgeons whose working duration was more than 1 year and also who participated in at least one fluoroscopy requiring operation per week, were analysed. 22 (12%) participants answered that they were trained on fluoroscopy usage. Sixty people (33.3%) reported that they did not use any protective equipment regularly. The most commonly used protection methods were lead aprons 123 (68.3%). Thyroid protectors were used by 92 participants (52.1%). There was no significant difference between the groups when comparing the use of protective equipment according to the academic title. Only 19 (10.6%) of the surgeons noted that they used dosimeter regularly, and 15 (83.3%) of them reported that they controlled their dosimeters.
Conclusion
In this study, Orthopedic surgeons were found not to be adequately trained about use and risks of fluoroscopy and also not to be equipped about methods for preventing radiation damage.
Keywords: Orthopedic surgery, Fluoroscopy, Radiation protection, C-arm, Operating room safety
Introduction
Radiation is currently used in the diagnosis and treatment of many diseases in medicine. In addition to the benefits of the use of ionizing radiation in medicine, health workers are exposed to radiation during health practise.1
Orthopedic surgeons also use fluoroscopy, which is an X-ray source, frequently.2 Despite frequent use in everyday practice, the inexperience of the use of fluoroscopy and radiation safety methods are leading harmful consequences of radiation exposure.3 Fundamentals of fluoroscopy use help to reduce exposure to radiation and therefore harmful effects.3
The purpose of this study is to determine behaviour and knowledge levels of Turkish orthopedic surgeons about fluoroscopy usage and radiation safety.
Material and methods
The questionnaire, consisting of nineteen questions, was sent to orthopedic surgeons and requested by a total of 323 surgeons online. The survey was about personal information, training and behaviours related to radiation and fluoroscopy usage, and the use of protective equipment.
All questions were answered with one option except the eighth question. This question was about which equipments were used during operation. So, eighth question was answered more than one choice, and it was predicted during analysing that the answers given to this question may be more than 100%.
The results were analysed using SPSS v.11.5.0 (SPSS Inc., Chicago, IL, USA) program. Pearson chi-square test, t-test, and Pearson correlation test were used for the analysis. p˂0.05 level was considered to be statistically significant.
Results
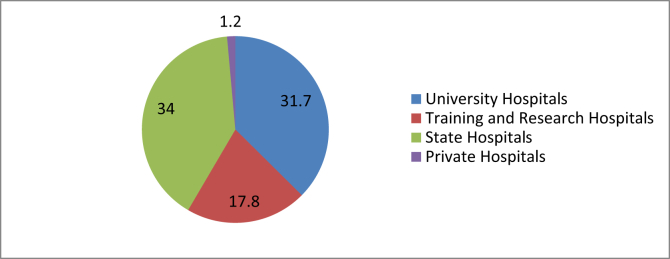
The questionnaire was sent to 323 orthopedic surgeons. 277 individuals completed the questionnaire, and 180 of these 277 surgeons’, whose working duration was more than 1 year and also who participated in at least one fluoroscopy requiring operation per week, answers were analysed. Of the participants, 84 (46,7%) were residents, 74 (41,1%) were specialist doctors, and 22 (12,2%) were associate professors and professors (Fig. 1). It was determined that 57 (31,7%) were working in university hospitals, 57 (31,7%) were in training and research hospitals, 32 (17,8%) were in state hospitals and 34 (18,8%) were in private hospitals(Fig. 2).
Fig. 1.
Distribution of participants according to academic title (%).
Fig. 2.
Distribution of participants according to their hospitals (%).
When participants were questioned about their training of fluoroscopy use, 22 (12%) of all participants were trained. It was found out that 8 (9,5%) of the residents, 10 (13,5%) of the specialist doctors and 4 (18,2%) of associate professors and professors were trained. The number of people who were not trained was statistically significantly higher. When these values were compared according to the academic title, no significant difference was found (p = 0.439).
While 47 (26,2%) participants used fluoroscopy in 6–10 operations per week, 65 (36,1%) participants stated that they used fluoroscopy in 2–5 operations and 68 (37,7%) participants used more than in 10 operations per week.
Seventy-two of 180 (40%) reported that the x-ray tube was positioned at the bottom and the image receptor at the top, 41 participants (22,8%) reported that the X-ray receiver was positioned at the bottom, the X-ray tube at the top. While 67 participants (37,2%) reported that they did not pay attention to the positions of the receiver and the tube(Table 1). No significant difference was found between the groups when the answers were evaluated according to the academic title (p = 0,170).
Table 1.
Position of the C-ARM device during the sequence.
| X-ray tube at the bottom, the X-ray receiver at the top | X-ray receiver at the bottom, the X-ray tube at the top | No attention to the position | ||||
|---|---|---|---|---|---|---|
| Residents | 38 | %45,2 | 16 | %19 | 30 | %35,7 |
| Specialist | 27 | %36,5 | 19 | %25,7 | 28 | %37,8 |
| Professor and As.Professor | 7 | %31,8 | 6 | %27,3 | 9 | %40,9 |
| Total | 72 | %40 | 41 | %22,8 | 67 | %37,2 |
While 106 participants (58,9%) were 1–2 steps away and 18 participants (10%) were 3 m away from fluoroscopy during the procedure; 56 participants (31,1%) were not careful about the distance from fluoroscopy. Considering these values, again, there was no significant difference between the academic title and distance to the device during shooting (Table 2).
Table 2.
Distance from Fluoroscopy in the sequence.
| 1-2 steps away | At least 3 m away | Not care | ||||
|---|---|---|---|---|---|---|
| Residents | 47 | %56 | 9 | %10,7 | 28 | %33,3 |
| Specialist | 47 | %63,5 | 4 | %5,4 | 23 | %31,1 |
| Professor and As.Professor | 12 | %54,5 | 5 | %22,7 | 5 | %22,7 |
| Total | 106 | %58,9 | 18 | %10 | 56 | %31,1 |
Sixty (33,3%) of the surgeons participating in the study said that they did not use protective equipment. The most commonly used protection methods were lead aprons 123 (68,3%). Thyroid protectors were used by 92 participants (52,1%) (Table 3). There was no significant difference between the groups when comparing the use of protective equipment according to the academic title (p = 0.178).
Table 3.
Use of protective equipment.
| The protective apron | Thyroid Gland Shields | Radio-Protective glasses | Radio-protective gloves | Never use | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Residents | 60 | %71,4 | 43 | %51,2 | 0 | %0 | 0 | %0 | 34 | %40,4 |
| Specialist | 48 | %64,9 | 37 | %50 | 3 | %4,1 | 1 | %1,4 | 26 | %35,1 |
| Professor and As.Professor | 15 | %68,2 | 12 | %54,5 | 0 | %0 | 0 | %0 | 0 | %0 |
| Total | 123 | %68,3 | 92 | %52,1 | 3 | %1,7 | 1 | %0,5 | 60 | %33,3 |
Although only 19 (10,6%) of the surgeons participating in the study that they used dosimeter regularly, 15 (83,3%) of these 19 surgeons were reported that they got controlled their dosimeters. Eleven participants (13,1%) of dosimeter users were residents, 6 participants (8,1%) of were specialists and 2 participants (9,1%) were professors.
One hundred fifty-seven participants (87,2%) were worried about radiation exposure, while 7 participants (3,9%) were not worried, and 16 participants were sometimes worried. There was no significant difference between the groups when they were evaluated between the academic title (p = 0,190).
The question asking the safety of the operating rooms was replied by thirty-four (18,9%) of the participants as the lead block was used. But 74 (41,1%) participants stated that lead block was not used and 72 (40%) participants did not know about this issue. In response to the question whether there was a warning sign on the door of the operating room, 40 responders (22,2%) answered that there was, 130 responders (72,2%) answered that there was not and 10 responders (5,6%) answered that they did not pay attention to this sign (Table 4).When the answers were evaluated according to the institution where the participants were working, almost all the physicians (34 of 180 participants) working in the private hospital stated that there were no warning signs on the door of the operating room. Twelve (21,1%) persons from university hospitals, seven (21,9%) persons from state hospitals and 21 (36,8%) persons from training and research hospitals indicated that there were warning signs in their hospitals’ operating rooms (Table 5).
Table 4.
Presence of lead block in the operating room.
| Yes | No | I don't care | ||||
|---|---|---|---|---|---|---|
| University Hospital | 9 | %15,8 | 27 | %47,4 | 21 | %36,8 |
| Research Hospital | 10 | %17,5 | 22 | %38,6 | 25 | %43,9 |
| State Hospital | 7 | %21,9 | 14 | %43,8 | 11 | %34,4 |
| Private Hospital | 8 | %23,5 | 11 | %32,4 | 15 | %44,1 |
| Total | 34 | %18,8 | 74 | %41,1 | 72 | %40 |
Table 5.
Presence of a warning sign at the door of the rooms where Fluoroscopy is used.
| Yes | No | I don't know | ||||
|---|---|---|---|---|---|---|
| University Hospital | 12 | %21,1 | 43 | %75,4 | 2 | %3,5 |
| Research Hospital | 21 | %36,8 | 30 | %52,6 | 6 | %10,5 |
| State Hospital | 7 | %21,9 | 24 | %75 | 1 | %3,1 |
| Private Hospital | 0 | %0 | 33 | %97,1 | 1 | %2,1 |
| Total | 40 | %22,2 | 130 | %72,2 | 10 | %5,6 |
Fifty-nine (32,8%) of orthopedic surgeons get help from radiology technicians, 96 (53,3%) of the surgeons get help from operating room personnel, and 25 (13,9%) of the surgeons get help from another orthopedic doctor for fluoroscopy shooting. All participants in state hospitals gave the same answer that the fluoroscopy was not taken by the doctor (Table 6).
Table 6.
Person using fluoroscopy.
| Radiology Technicians | Operating Room Staff | Doctor | ||||
|---|---|---|---|---|---|---|
| University Hospital | 20 | %35,1 | 32 | %56,1 | 5 | %8,8 |
| Research Hospital | 22 | %38,6 | 16 | %28,1 | 19 | %33,3 |
| State Hospital | 12 | %37,5 | 20 | %62,5 | 0 | %0 |
| Private Hospital | 5 | %14,7 | 28 | %82,4 | 1 | %2,9 |
| Total | 59 | %32.8 | 96 | %53.3 | 25 | %13.9 |
Discussion
The popularity of minimally invasive surgery among orthopedic surgeons and the widespread use of intramedullary nails have also increased the need for fluoroscopic imaging.4, 5 This, in turn, leads to more radiation exposure. In this study, we aimed to evaluate behaviour and knowledge levels of Turkish orthopedic surgeons about fluoroscopy use and radiation safety.
The results of this questionnaire showed both that the rules that must be followed to avoid harmful effects of radiation during fluoroscopy are not given sufficient importance and that the protection methods are not used sufficiently by orthopedic surgeons. It has come to the conclusion that the surgeons have not adequately fulfilled the measures that can be taken to reduce radiation exposure. It has come to the conclusion that physicians, independently of the academic title, have not adequately implemented the applications in order to reduce radiation exposure.
The areas that are likely to exceed the value of 1 mSv annually are considered as radiation field according to Radiation Safety Regulation which has posted on the Official Journal at 24/03/2003 based on Turkish Atomic Energy Agency law.6 However, since the use of dosimeters is not widespread, there is no definitive data on the average annual dose exposed in orthopedic operating rooms. Previously, in a survey conducted in Turkey, similar to our study, they reported that the dosimeter usage rate of about 10%.7
According to the Radiation Safety Regulations, warning signs must be found in areas that are likely to be exposed to radiation.6 In this study, only 22,2% of participants stated that there were warning signs in the operating room. Even, all participants who worked in private hospitals reported that were not warning signs. This data shows that inspections in this area are insufficient.
There are many studies in the literature about the precautions that should be taken to protect orthopedic surgeons from radiation and the radiation protection principles have been established. The most important of these are being at least 3 m away from fluoroscopy during shooting, use of protective equipment and presence of scoping technician.3, 5, 8 Mohiuddin and colleagues have found that the dose of radiation exposure seriously diminishes with the principles they determine.8
It has been reported that the X-ray tube located upper from the table will cause ten times more radiation exposure than underneath position during fluoroscopy shooting.5 In our study, it was determined that the surgeons did not pay enough attention to the fluoroscopic position, independently from the academic title. This suggests that the training on the use of fluoroscopy is inadequate and that this issue is not considered enough.
The more distant the patient is during the exposure, the less exposition to the radiation is.5 At the time of the shooting, stopping at 2–3 m away from the tube and from the patient reduces the exposure to radiation 4–10 times.5 Only 18 participants (10%) gave the answer that they stayed 3 m away from fluoroscopy, when we questioned the distance during the shooting sequence. This shows that orthopedists do not have enough knowledge of the technique of reducing radiation exposure.
The use of protective equipment during fluoroscopy has been reported to seriously reduce the exposure to radiation.9, 10 We found that lead protection was used by 68,3% of participants and thyroid shield was used by half of the participants as protective equipment. It was stated that only 3 (1.7%) of the participants used the protective eyewear and only 1 (0.6%) of the gloves were used by the participants. In a study conducted by Ismail and his colleagues,11 resident doctors were most exposed to radiation in the operating room, while orthopedic and urologic specialists were second. Again, in a study conducted in Turkey, the amount of radiation in the region where orthopaedic surgeons worked was found to be higher than the amount of radiation in the area where the anesthetist worked.12 But our study has shown that orthopedic surgeons do not adequately comply with the methods of protection. This suggests that we may face with radiation-induced problems.
The limitation of this study is the low participation rate when we consider that there are about 3500 orthopedic surgeons in Turkey. We think that more exact data can be obtained by a study with a larger sample. The strength of our work is that it is one of the few studies that have been done in our country about such an important issue.
Conclusion
In conclusion, according to the information we received from our limited numbers of colleague who agreed to participate in the survey, orthopedic surgeons did not take adequate measures to use fluoroscopy for radiation safety. Although certain methods of radiation protection have been developed, perhaps the most important part of preservation is the provision of education at certain intervals. Increased training in the use of fluoroscopy and awareness of the risks created by radiation can reduce the time and the amount of radiation exposure for both the patient and the surgeon. We think that this survey can be a guide on the programming of orthopedic and traumatology specialization training.
The Questionnaire
|
|
| |
| |
|
|
| |
| |
| |
|
|
| |
| |
| |
| |
| |
|
|
| |
| |
| |
|
|
| |
|
|
| |
|
|
| |
|
|
| |
| |
| |
| |
|
|
| |
| |
|
|
| |
|
|
| |
| |
|
|
| |
| |
|
|
| |
| |
|
|
| |
| |
|
|
| |
| |
|
|
| |
| |
|
|
| |
| |
|
|
| |
| |
|
|
|
Conflicts of interest
None declared.
Footnotes
Peer review under responsibility of Turkish Association of Orthopaedics and Traumatology.
Contributor Information
Fırat Fidan, Email: drfiratfidan@gmail.com.
Mehmet Ümit Çetin, Email: drumitcetin@gmail.com.
Cengiz Kazdal, Email: zzengizz@gmail.com.
Feyzi Kılıç, Email: drkilicfeyzi@gmail.com.
Ufuk Özkaya, Email: ufukozkaya2004@yahoo.com.
References
- 1.Dewey P., George S., Gray A. (i) Ionising radiation and orthopaedics. Curr Orthop. 2005;19(1):1–12. [Google Scholar]
- 2.Badman B.L., Rill L., Butkovich B., Arreola M., Griend R.A.V. Radiation exposure with use of the mini-C-arm for routine orthopaedic imaging procedures. J Bone Joint Surg Am. 2005;87(1):13–17. doi: 10.2106/JBJS.D.02162. [DOI] [PubMed] [Google Scholar]
- 3.Kaplan Daniel J., Patel Jay N., Liporaceand Frank A., Yoon Richard S. Intraoperative radiation safety in orthopaedics: a review of the ALARA (As low as reasonably achievable) principle Kaplan et al. Pat Safety Surg. 2016;10(1):27. doi: 10.1186/s13037-016-0115-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Singer G. Occupational radiation exposure to the surgeon. J Am Acad Orthop Surg. 2005;13(1):69–76. doi: 10.5435/00124635-200501000-00009. [DOI] [PubMed] [Google Scholar]
- 5.Hatzis C., Brilakis A.E., Efstathopoulos N. Practical rules for occupational radiation exposure protection in orthopaedic surgery. EEXOT Τόμος. 2012;63(1):41–46. [Google Scholar]
- 6.Radyasyon Güvenliği Yönetmeliği. Türkiye Cumhuriyeti Resmi gazetesi. 2003;3(23999):1–7. [Google Scholar]
- 7.Tuncer N., Kuyucu E., Sayar S., Polat G., Erdil I., Tuncay I. Orthopedic surgeons' knowledge regarding risk of radiation exposition: a survey analysis. SICOT J. 2017;3(3):1–4. doi: 10.1051/sicotj/2017008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Mohiuddin Mohd Jalal, Kumar Chinnala Srujan. A Study to determine the average Number of X-Rays taken during an Orthopaedic surgery and approximate amount of radiation exposure. Int J Adv Res. 2016;4(8):801–804. [Google Scholar]
- 9.Quinn A.D., Taylor C.G., Sabharwal T., Sikdar T. Radiation protection awareness in non-radiologists. Br J Radiol. 1997;70(289):102–106. doi: 10.1259/bjr.70.829.9059306. [DOI] [PubMed] [Google Scholar]
- 10.Rehani M.M., Ciraj-Bjelac O., Vañó E. Radiological protection in fluoroscopically guided procedures performed outside the imaging department. ICRP. 2010;40(6):1–102. doi: 10.1016/j.icrp.2012.03.001. [DOI] [PubMed] [Google Scholar]
- 11.Ismail S., Khan F.A., Sultan N., Naqvi M. Radiation exposure of trainee anaesthetists. Anaesthesia. 2006;61(1):9–14. doi: 10.1111/j.1365-2044.2005.04419.x. [DOI] [PubMed] [Google Scholar]
- 12.Cecen G.S., Gulabi D., Pehlivanoglu G., Bulut G., Bekler H., Asil K. Radiation in the orthopedic operating theatre. Acta Orthop Traumatol Turc. 2015;49(3):297–301. doi: 10.3944/AOTT.2015.14.0250. [DOI] [PubMed] [Google Scholar]