Abstract
Objective
The aim of this animal study was to investigate the short and long-term local histomorphologic effects and the utility of intra-articular application of ibuprofen.
Methods
Forty-six Wistar Albino rats were used in the study. The rats were randomized into 5 groups of 8 and a sham group of 6. The 40 rats in the study groups were anaesthetised with 60 mg/kg of ketamine, then 0.25 ml ibuprofen (25 mg) was injected to the right knee joint of each rat (ibuprofen group) and 0.25 ml 0.9% saline to the left knee joint as the control group. To the 6 rats in the sham group, only puncture was applied to both knee joints. The rats in each of the 5 study groups were sacrificed on days 1, 2, 7, 14 and 21 respectively. The histomorphologic changes were graded on a 6-point scale regarding inflammation of the synovia, cartilage tissue, and subchondral bone. Inflammation scores were compared using the Mann Whitney U-test and comparisons of the sacrifice day and drug used were evaluated with the Kruskal Wallis test. The p values below 0.05 were considered as significant.
Results
Statistically significant difference was found between the ibuprofen injected knees (10/40) and the saline injected (0/40) and sham knees (0/12) in respect of hematoma positivity (p = 0.002). Significantly higher inflammation scores were found in ibuprofen injected knees on the 1st, 2nd, 7th and 14th days compared to controls and sham (p < 0.05). Inflammation scores were similar in ibuprofen injected knees with and without hematoma (p > 0.05). Inflammation of the ibuprofen injected group was most severe on day one and the severity of inflammation reduced gradually throughout the 3 weeks.
Conclusion
Our results show that intra-articular injection of ibuprofen can cause intra-articular hematoma. It also leads to transient inflammation of the synovia that is more severe in the early period, which gradually recovers.
Keywords: Ibuprofen, Intra-articular, Knee, Synovium, Cartilage
Introduction
Inadequate pain control after orthopaedic knee surgery can lead to immobility-related complications and poor outcomes.1 Early mobilisation requires effective pain relief. Traditionally opioid analgesics have been the mainstay of postoperative analgesia. Side effects of opioids including respiratory depression, dependence, urinary retention, constipation, and nausea limit their use. Together with opioids, systemic non-steroid anti-inflammatory drugs (NSAIDs), periarticular, and intraarticular injection of opioids and local anaesthetics have been widely used for multimodal pain protocols.2, 3, 4, 5, 6 Intra-articular use of NSAIDs including, tenoxicam,7, 8 lornoxicam9 and ketorolac10, 11 have been investigated for the clinical management of orthopaedic surgery and osteoarthritis pain. Still, there are concerns about the short and long-term safety of intra-articular injection of NSAIDs. The intravenous form of ibuprofen has been recently approved for the treatment of mild to moderate pain, and for the treatment of moderate to severe pain as an augmentation to opioids.12
Local administration of any drug to the synovia may have significant consequences. Despite considered as a safe method,13, 14 there is little information with mixed results on the safety of intra-articular injection of various NSAIDs.15, 16, 17, 18, 19 To the best of our knowledge, there is no study in the literature which has assessed the effects of intra-articular injection of the newly-licensed intravenous form of ibuprofen on joint cartilage and synovia. We aimed to study local synovial inflammation after single intra-articular injection of ibuprofen and normal saline in rat knee joint.
Materials and methods
Total of forty-six adult albino male Wistar rats (250–300 g) was randomised and housed in groups of 8 (sham group 6), with water and food ad libitum, at a constant temperature of 22 °C and controlled lighting (12 h light/12 h dark cycle). Forty rats were used for ibuprofen and saline injection, 6 rats were used for the sham group. Experimental procedures were performed in accordance with Guide for the Care and Use of Laboratory Animals.20 The protocol was also reviewed and approved by the Ethical Committee of Research Centre of Experimental Medicine.
Intra-articular injection
Under ketamine anaesthesia (60 mg/kg of intraperitoneal ketamine), both knees were disinfected with povidone-iodine, intra-articular injection to the right knee joint of 0.25 ml standard commercial preparation of ibuprofen (25 mg) (Intrafen®, Gen ilac, Turkey) was performed with the use of a 1 ml syringe and a 26G needle. The animal received another similar injection to the left knee joint with 0.25 ml of 0.9% saline. Punction with a 26G needle was applied to both knee joints of the 6 rats in the sham group. Dose and volume of the injectates were based on previous rat studies with NSAID's.16, 19 Each knee received a single injection. The rats were returned to the cages for further care until sacrificed.
Tissue processing
The rats were sacrificed at certain time points according to their groups under ketamine anaesthesia. Rats of the study groups (n = 8) were sacrificed on the 1st, 2nd, 7th, 14th and 21st days after injection with ibuprofen and saline. Sham-treated animals (n = 6) were sacrificed on the 2nd day.
The knee joints of each rat were surgically dissected by making an incision from the distal tibia and proximal femur. The skin, subcutaneous tissues, and muscles were removed from the bone structures, preserving the integrity of the knee joint. After exposing the tissues without opening the capsule, the joint was macroscopically examined for the presence of a possible hematoma, and the findings were recorded. The explored knees of the study groups were labeled as ibuprofen injected right knee (IB-R), saline injected left knee (SL-L), right sham knee (SM-R) and left sham knee (SM-L). Knees in the injection groups were further labeled according to the day of sacrifice as 1, 2, 7, 14 and 21.
Histomorphologic examination
Tissue samples taken from labeled joints were fixed in 10% formaldehyde for two days, followed by decalcification in rapid decalcifier (20% formic acid) for one day. After decalcification, the samples were embedded in paraffin blocks, and serial sagittal histological sections (5 μm) were obtained using a Leica 2255 rotatory microtome. Sections were stained with haematoxylin/eosin. Stained sections were evaluated under a microscope Zeıss AXI0, Imager A1. The samples were evaluated in respect of oedema and inflammation in the joint and synovia, the presence of macrophages, neutrophil count, synoviocyte hyperplasia, fibrin exudate, joint surface erosion, and chondrocyte necrosis.
Inflammatory changes were graded on a 6-point scale:
- grade 0: no inflammation, - grade 1: minimal inflammation, mild congestion, and oedema, - grade 2: mild inflammation, erosion of joint surface, congestion and oedema and a small number of neutrophils, - grade 3: moderate inflammation, neutrophils, and macrophages, synoviocyte hyperplasia, - grade 4: severe inflammation, neutrophils and macrophages, synoviocyte hyperplasia and fibrin exudation, - grade 5: necrosis.
Statistical analysis
As the grade was an original variable, comparison of median values was made with the Kruskal Wallis test. In the evaluation of the obtained data, data showing normal distribution were evaluated with the Bonferroni (Dunn) test. In the comparison of the degree of inflammatory changes of the right and left knees within the same group, the Mann Whitney U-test was used. A value of p < 0.05 was accepted as statistically significant.
Results
Hematoma
Haematoma was present in 10/40 of ibuprofen injected knee joints. No haematoma was observed in any of the control (0/40) or sham (0/12) knee joints. Statistically significant difference was determined between the ibuprofen injected knees, and the saline injected and sham knees in respect of hematoma positivity (p = 0.002).
Scores of histomorphologic inflammatory changes
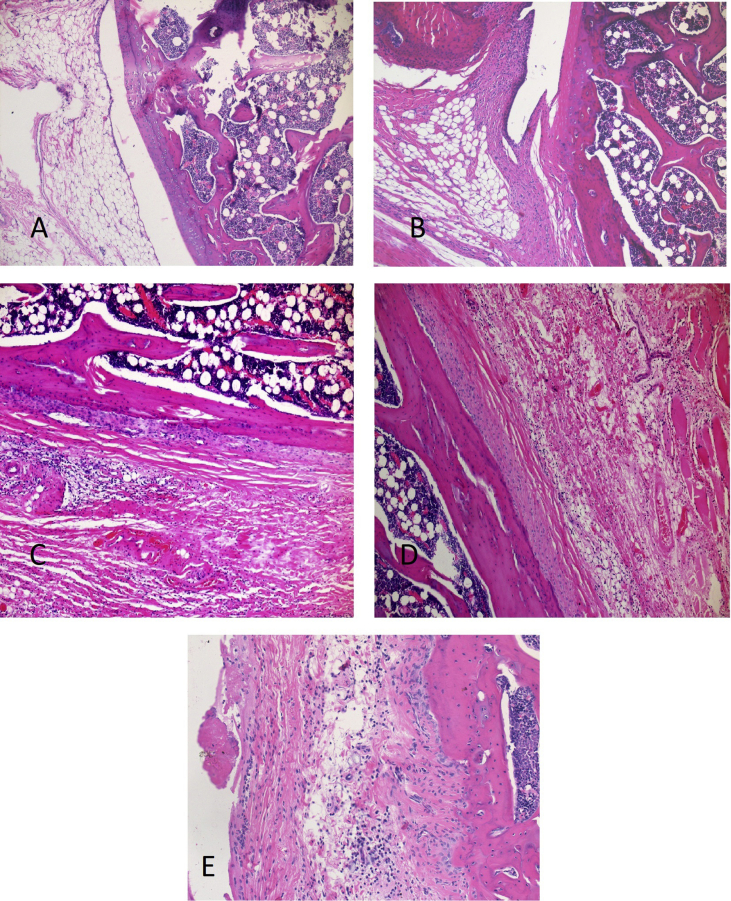
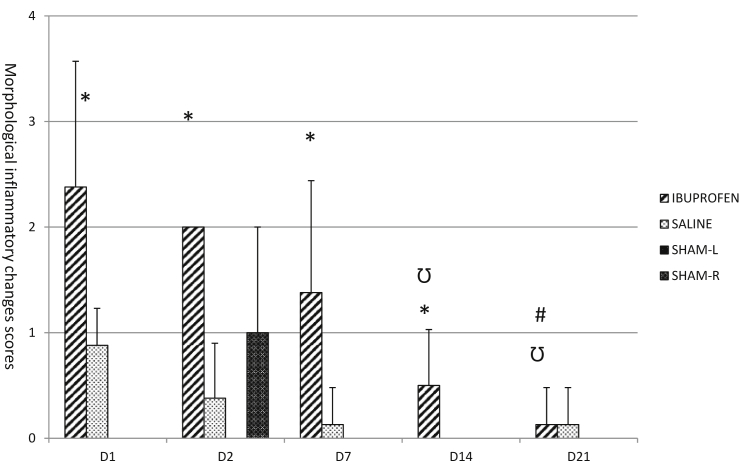
Examples of histomorphologic grades of inflammation are presented in Fig. 1. Significantly higher inflammation scores were seen in ibuprofen injected knees on the 1st, 2nd, 7th and 14th days compared to the saline-injected counterparts and sham groups (p < 0.05). Inflammation scores were similar between the ibuprofen and saline groups in rats sacrificed on the 21st day (p > 0.05). Scores of right and left knee sham injections were also similar (p > 0.05). Inflammation scores were similar in ibuprofen injected knees with and without hematoma (p > 0.05). When inflammation scores of knee joints of the ibuprofen injected group were compared as regard to time; inflammation was most severe on day one. Day one score was significantly higher than day 14 and day 21 scores (p < 0.05). Day two score was significantly higher than day 21 score. Throughout the three weeks, the severity of inflammation reduced gradually (Fig. 2).
Fig. 1.
Light microscopic views of rat knee joint. Haematoxylin-eosinn × 100. A: Degree 0 from group SR2; normal histological appearance. B: Degree 1 from group D4; minimal inflammation, mild congestion. C: Degree 2 from group D2; moderate inflammation, lymphocyte infiltration. D: Degree 3 from group D1; severe inflammation o,edema. E: Degree 4 from group D1; very severe inflammation.
Fig. 2.
D1: 1st daysacrificedd group that was injected ibuprofen in the right knee. D2: 2nd daysacrificedd group that was injected ibuprofen in the right knee. D7: 7th daysacrificedd group that was injected ibuprofen in the right knee. D14: 14th daysacrificedd group that was injected ibuprofen in the right knee. D21: 21st daysacrificedd group that was injected ibuprofen in the right knee. *p < 0.05 compared to saline and sham, Ʊ p < 0.05 ibuprofen group compared to day 1, #p < 0.05 compared to day.
Discussion
To the best of our knowledge, this is the first study on the local inflammatory effect on synovia of intra-articularly administered ibuprofen. Results of this animal study suggest that when injected into the synovia commercial ibuprofen leads to transient mild to moderate inflammation and possibly has an adverse effect on local coagulation.
Early clinical studies have demonstrated the efficacy of intra-articular NSAIDs in providing analgesia in patients undergoing arthroscopic knee surgery. Ketorolac, a non-selective COX1-COX2 inhibitor, when given intra-articular, provides better postoperative analgesia than an equal dose administered systemically.11, 21, 22
Previous studies regarding the potentially harmful effects of intra-articular injection of NSAIDs in animal models provided mixed results. In a study by Irwin et al., intra-articular ketorolac and saline were injected into rat knee joints and the histomorphologic changes were evaluated on the 1st, second and fifth days. On the 5th day, more inflammation was seen in the ketorolac group compared to the saline control group.16 Similarly, intra-articular injection of ketorolac into the healthy rabbit knee showed mild histomorphologic changes.15 Contrary to these results some studies claimed that injection of NSAIDs might be safe and even pose less threat to the local tissue after intra-articular administration. Intra-articular injection of ketorolac into the healthy rabbit knee showed no histological changes, and injection into the rabbit patellar tendon showed no detrimental biomechanical or histological changes.23 Riggin et al. showed that intra-articular injection of ketorolac or saline to the tibiofemoral joint resulted in no injury to the rat cartilage tissue.24 In a rabbit osteoarthritis model, Jiang et al. applied intra-articular injections of celecoxib, a selective COX2 inhibitor, hyaluronic acid and saline to 3 groups of 30 rabbits. Histologically, similar to the hyaluronic acid, celecoxib improved rabbit articular cartilage, much more than in the saline group.18 In an in vivo animal study, six weekly injections of bufexamac which inhibits class IIB histone deacetylases (HDAC6 and HDAC10) was shown to cause no systemic or local changes in healthy horse intercarpal joint articular cartilage from the histological analysis.25 In the present study, we observed a significant increase in inflammation scores at the first and second days after injection of ibuprofen, the scores decreased over time, and no significant inflammation was seen after the 14th day. Our results are consistent with the study by Özyuvaci et al. which histologically assessed the effects intra-articular tenoxicam, a non-selective COX inhibitor on rat cartilage. They similarly observed inflammation at the first and second days, but further on there were no signs of inflammation.19 On the contrary, our results differ from Saricaoglu et al., which investigated the effects of lornoxicam on the synovium and cartilage of the rat knee joint with a similar methodology.17 Their results showed no significant differences in inflammation between saline and lornoxicam. Our study design does not include the possible mechanisms of the inflammation which developed after ibuprofen injection. Hence we can only speculate that no local inflammation after lornoxicam injection may be attributed to the known better safety profile of lornoxicam compared to other NSAIDs.26, 27 Lornoxicam inhibits polymorphonuclear (PMN)-leukocyte migration; inhibits the release of superoxide from PMN-leukocytes; inhibits the release of platelet-derived growth factor (PDGF) from platelets and stimulates the synthesis of proteoglycans in cartilage in tissue culture.26
Although ibuprofen per se could have caused the inflammation, it is possible to speculate that pH of the standard preparation, arginine in the content of commercial ibuprofen or the high incidence of hematoma after the injection of ibuprofen could also be responsible. The ibuprofen solution has a neutral pH of 7.4. Therefore it is unlikely to cause inflammation. Arginine is a precursor to nitric oxide (NO). Osteoblasts, osteoclasts, macrophages, fibroblasts, neutrophils, and endothelial cells are capable of generating NO in the synovium. NO is considered to be involved in inflammation and mediate a number of processes including apoptosis and expression of proinflammatory cytokines.28 Arginine may have contributed to the inflammation caused by commercial ibuprofen injection. Further research is needed to assess the role of arginine in this inflammatory process.
The haematoma is unlikely to be the cause of inflammation based on the fact that the inflammation scores of ibuprofen injected knees with and without hematoma were statistically similar.
All NSAIDs including ibuprofen inhibit COX, an enzyme that converts arachidonic acid to prostaglandins, thereby mediating pain, inflammation, and fever.29 In the present study higher incidence of macroscopic haematoma observed in ibuprofen injected knees may be through reversible inhibition of COX-1 enzyme which decreases the conversion of arachidonic acid into prostaglandin endoperoxides including thromboxane and prostacyclin30. The COX-1 enzyme does not appear to be affected by the inflammatory process. Induction of COX-2 enzyme is associated with inflammation. The relative ratio of the COX1/COX2 inhibitory potential of each agent differs markedly. Ketorolac and ibuprofen inhibit both COX-1 and COX-2 with little selectivity. Their COX-1/COX-2 selectivity IC50 ratio is 0.13 and 0.50 respectively.31, 32 Inhibition of COX-1 suppresses the formation of pro-aggregatory thromboxane A2 in platelets. One of the major concerns in using intravenous ibuprofen in the acute care setting is the risk of bleeding.30 Oral ibuprofen is known to dose proportionally significantly inhibit the activity of thromboxane B2, platelet aggregation and prolong bleeding time compared with placebo.33, 34 Surprisingly previous studies with ketorolac which has higher COX-1 inhibitory activity, which employed similar methodology of injection to the rat joints fail to mention any hematoma after the injection of the drug.16, 24
The half-life of anti-inflammatory drugs in the joint cavity measured after intra-articular injection is unknown, but half-life after oral administration is known to be around 1–5 h.35 Due to lymphatic drainage of the joint cavity,36 effects of ibuprofen may be different if administered continuously or repeatedly in the long term. In a study by Orak et al., intra-articular tenoxicam, diclofenac, and methylprednisolone were administered to rats, and the long-term effects in the knee joint were evaluated. Histomorphologic changes were examined in the knee joints of the rats at 48 h, then at 1, 2, 4 and 8 weeks after the application of these 3 drugs. In the tenoxicam and diclofenac groups, increased fibroblast numbers and fibrosis levels were observed. They concluded that multiple intra-articular injections may be harmful to the knee.37 Human patients who received intra-articular ketorolac after knee arthroscopy demonstrated increased levels of glycerol, a marker of cell damage, in the synovial membrane, suggesting a potentially toxic effect of this NSAID on the joint soft tissues.38
There are several limitations to this study. The present study was conducted on healthy rats with healthy cartilage tissue. The safety of ibuprofen in human cartilage and synovia may be different. We evaluated the histology of a single dose of ibuprofen over a period of 21 days. Therefore, the results of the macroscopic examination and histological evaluation at early or a few time points after a single ibuprofen injection are provided. The clinical efficacy on joint functional properties, pain relief and effects of repeated injections were not assessed. Also, the study does not include the possible systemic effects and side effects of the drug.
In conclusion, a single intra-articular injection of commercial ibuprofen can cause intra-articular hematoma. It also leads to transient inflammation of the synovia that is more severe in the early period, which gradually recovers. Although this study does not assess pain scores, the observed inflammation and hematoma may lead to joint pain. This brings the need for further animal studies before any human research for intra-articular administration of ibuprofen.
Acknowledgement
In our study, financial support was provided by Selçuk University units of scientific research projects (BAP).
Footnotes
Peer review under responsibility of Turkish Association of Orthopaedics and Traumatology.
References
- 1.Lavie L.G., Fox M.P., Dasa V. Overview of total knee arthroplasty and modern pain control strategies. Curr Pain Headache Rep. 2016;20:1–5. doi: 10.1007/s11916-016-0592-6. [DOI] [PubMed] [Google Scholar]
- 2.Busch C.A., Shore B.J., Bhandari R. Efficacy of periarticular multimodal drug injection in total knee arthroplasty. A randomized trial. J Bone Joint Surg Am. 2006;88:959–963. doi: 10.2106/JBJS.E.00344. [DOI] [PubMed] [Google Scholar]
- 3.Altay M.A., Ertürk C., Altay N., Atbinici H. The effect of intraarticular local anaesthesia on postoperative pain in arthroscopic knee surgery. J Clin Exp Invest. 2010;1:86–90. [Google Scholar]
- 4.Jacobson E., Assareh H., Cannerfelt R., Anderson R.E., Jakobsson J.G. The postoperative analgesic effects of intra-articular levobupivacaine in elective day-case arthroscopy of the knee: a prospective, randomized, double-blind clinical study. Knee Surg Sports Traumatol Arthrosc. 2006;14:120–124. doi: 10.1007/s00167-005-0655-4. [DOI] [PubMed] [Google Scholar]
- 5.Joshi G.P., McCarroll S.M., McSwiney M., O'Rourke P., Hurson B.J. Effects of intraarticular morphine on analgesic requirements after anterior cruciate ligament repair. Reg Anesth. 1993;18:254–257. [PubMed] [Google Scholar]
- 6.Kızılcık N., Özler T., Menda F., Ç Uluçay, Köner Ö., Altıntaş F. The effects of intra-articular levobupivacain versus levobupivacain plus magnesium sulfate on postoperative analgesia in patients undergoing arthroscopic meniscectomy: a prospective randomized controlled study. Acta Orthop Traumatol Turc. 2017;51:104–109. doi: 10.1016/j.aott.2017.02.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Elhakim M., Fathy A., Elkott M., Said M.M. Intra-articular tenoxicam relieves post-arthroscopy pain. Acta Anaesthesiol Scand. 1996;40:1223–1226. doi: 10.1111/j.1399-6576.1996.tb05554.x. [DOI] [PubMed] [Google Scholar]
- 8.Talu G.K., Ozyalçin S., Koltka K. Comparison of efficacy of intraarticular application of tenoxicam, bupivacaine and tenoxicam: bupivacaine combination in arthroscopic knee surgery. Knee Surg Sports Traumatol Arthrosc. 2002;10:355–360. doi: 10.1007/s00167-002-0306-y. [DOI] [PubMed] [Google Scholar]
- 9.Eren M., Koltka K., Köknel Talu G., Aşik M., Ozyalçin S. Comparison of analgesic activity of Intraarticular lornoxicam, bupivacaine and saline after knee arthroscopy. Agri. 2008;20:17–22. [PubMed] [Google Scholar]
- 10.Richards M.M., Maxwell J.S., Weng L., Angelos M.G., Golzarian J. Intra-articular treatment of knee osteoarthritis: from anti-inflammatories to products of regenerative medicine. Phys Sports Med. 2016;44:101–108. doi: 10.1080/00913847.2016.1168272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Convery P.N., Milligan K.R., Quinn P., Scott K., Clarke R.C. Low-dose Intraarticular ketorolac for pain relief following arthroscopy of the knee joint. Anaesthesia. 1998;53:1125–1129. doi: 10.1046/j.1365-2044.1998.00582.x. [DOI] [PubMed] [Google Scholar]
- 12.Koh W., Nguyen K.P., Jahr J.S. Intravenous non-opioid analgesia for peri- and postoperative pain management: a scientific review of intravenous acetaminophen and ibuprofen. Korean J Anesthesiol. 2015;68:3–12. doi: 10.4097/kjae.2015.68.1.3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Fang R., Liu Z., Alijiang A. Efficacy of intra-articular local anesthetics in total knee arthroplasty. Orthopedics. 2015;38:e573–e581. doi: 10.3928/01477447-20150701-54. [DOI] [PubMed] [Google Scholar]
- 14.Zou Z., An M.M., Xie Q. Single dose intraarticular morphine for pain control after knee arthroscopy. Cochrane Database Syst Rev. 2016;5:1–93. doi: 10.1002/14651858.CD008918.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Dogan N., Erdem A.F., Gundogdu C., Kursad H., Kizilkaya M. The effects of ketorolac and morphine on articular cartilage and synovium in the rabbit knee joint. Can J Physiol Pharmacol. 2004;82:502–505. doi: 10.1139/y04-066. [DOI] [PubMed] [Google Scholar]
- 16.Irwin M.G., Cheung K.M., Nicholls J.M., Thompson N. Intra-articular injection of ketorolac in the rat knee joint: effect on articular cartilage and synovium. Br J Anaesth. 1998;80:837–839. doi: 10.1093/bja/80.6.837. [DOI] [PubMed] [Google Scholar]
- 17.Saricaoglu F., Dal D., Atilla P. Effect of intraarticular injection of lornoxicam on the articular cartilage & synovium in rat. Indian J Med Res. 2008;127:362–365. [PubMed] [Google Scholar]
- 18.Jiang D., Zou J., Huang L. Efficacy of intraarticular injection of celecoxib in a rabbit model of osteoarthritis. Int J Mol Sci. 2010;11:4106–4113. doi: 10.3390/ijms11104106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ozyuvaci H., Bilgic B., Ozyuvaci E., Altan A., Altug T., Karaca C. Intraarticular injection of tenoxicam in rats: assessment of the local effects on the articular cartilage and synovium. J Int Med Res. 2004;32:312–316. doi: 10.1177/147323000403200311. [DOI] [PubMed] [Google Scholar]
- 20.Institute for Laboratory Animal Research Division on Earth and Life Studies . 8th ed. The National Academies Press; Washington, DC: 2011. Guide for the Care and Use of Laboratory Animals. [Google Scholar]
- 21.Gupta A., Axelsson K., Allvin R. Postoperative pain following knee arthroscopy: the effects of intra-articular ketorolac and/or morphine. Reg Anesth Pain Med. 1999;24:225–230. doi: 10.1016/s1098-7339(99)90132-3. [DOI] [PubMed] [Google Scholar]
- 22.Reuben S.S., Connely N.R. Postoperative analgesia for outpatient arthroscopic knee surgery with Intraarticular bupivacaine and ketorolac. Anesth Analg. 1995;80:1154–1157. doi: 10.1097/00000539-199506000-00015. [DOI] [PubMed] [Google Scholar]
- 23.Shapiro P.S., Rohde R.S., Froimson M.I. The effect of local corticosteroid or ketorolac exposure on histologic and biomechanical properties of rabbit tendon and cartilage. Hand (NY) 2007;2:165–172. doi: 10.1007/s11552-007-9042-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Riggin C.N., Tucker J.J., Soslowsky L.J., Kuntz A.F. Intra-articular tibiofemoral injection of a nonsteroidal anti-inflammatory drug has no detrimental effects on joint mechanics in a rat model. J Orthop Res. 2014;32:1512–1519. doi: 10.1002/jor.22674. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Suominen M.M., Tulamo R.M., Anttila M.O. Effects of intra-articular injections of bufexamac suspension in healthy horses. Am J Vet Res. 2001;62:1629–1635. doi: 10.2460/ajvr.2001.62.1629. [DOI] [PubMed] [Google Scholar]
- 26.Pruss T.P., Stroissnig H., Radhofer-Welte S. Overview of the pharmacological properties, pharmacokinetics and animal safety assessment of lornoxicam. Postgrad Med J. 1990;66:S18–S21. [PubMed] [Google Scholar]
- 27.Garg Y., Singh J., Sohal H.S., Gore R., Kumar A. Comparison of clinical effectiveness and safety of newer nonsteroidal anti-inflammatory drugs in patients of osteoarthritis of knee joint: a randomized, prospective, open-label parallel-group study. Indian J Pharmacol. 2017;49:383–389. doi: 10.4103/ijp.IJP_245_16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Fermor B., Christensen S.E., Youn I., Cernanec J.M., Davies C.M., Weinberg J.B. Oxygen, nitric oxide and articular cartilage. Eur Cell Mater. 2007;13:56–65. doi: 10.22203/ecm.v013a06. [DOI] [PubMed] [Google Scholar]
- 29.Moore N., Pollack C.2, Butkerait P.2. Adverse drug reactions and drug-drug interactions with over-the-counter NSAIDs. Ther Clin Risk Manag. 2015;11:1061–1075. doi: 10.2147/TCRM.S79135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Bookstaver P.B., Miller A.D., Rudisill C.N., Norris L.B. Intravenous ibuprofen: the first injectable product for the treatment of pain and fever. J Pain Res. 2010;3:67–79. doi: 10.2147/jpr.s6993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Jett M.F., Ramesha C.S., Brown C.D. Characterization of the analgesic and anti-inflammatory activities of ketorolac and its enantiomers in the rat. J Pharmacol Exp Ther. 1999;288:1288–1297. [PubMed] [Google Scholar]
- 32.Hinz B., Brune K. Specific cyclooxygenase-2 inhibitors. Basis and options of a pharmacotherapeutic concept. Anaesthesist. 2000;49:964–971. doi: 10.1007/s001010070032. [DOI] [PubMed] [Google Scholar]
- 33.Evans A.M., Nation R.L., Sansom L.N., Bochner F., Somogyi A.A. Effect of racemic ibuprofen dose on the magnitude and duration of platelet cyclooxygenase inhibition: relationship between inhibition of thromboxane production and the plasma unbound concentration of S(+)-ibuprofen. Br J Clin Pharmacol. 1991;31:131–138. doi: 10.1111/j.1365-2125.1991.tb05500.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Van Hecken A., Schwartz J.I., Depré M. Comparative inhibitory activity of rofecoxib, meloxicam, diclofenac, ibuprofen, and naproxen on COX-2 versus COX-1 in healthy volunteers. J Clin Pharmacol. 2000;40:1109–1120. [PubMed] [Google Scholar]
- 35.Larsen C., Ostergaard J., Larsen S.W. Intraarticular depot formulation principles: role in the management of postoperative pain and arthritic disorders. J Pharm Sci. 2008;97:4622–4654. doi: 10.1002/jps.21346. [DOI] [PubMed] [Google Scholar]
- 36.Netter P., Bannwarth B., Royer-Morrot M.J. Recent findings on the pharmacokinetics of non-steroidal anti-inflamatory drugs in synovial fluid. Clin Pharmacokinet. 1989;17:145–162. doi: 10.2165/00003088-198917030-00002. [DOI] [PubMed] [Google Scholar]
- 37.Orak M.M., Ak D., Midi A., Laçin B., Purisa S., Bulut G. Comparison of the effects of chronic intra-articular administration of tenoxicam, diclofenac, and methylprednisolone in healthy rats. Acta Orthop Traumatol Turc. 2015;49:438–446. doi: 10.3944/AOTT.2015.14.0312. [DOI] [PubMed] [Google Scholar]
- 38.Stalman A., Tsai J.A., Segerdahl M., Dungner E., Arner P., Fellander-Tsai L. Ketorolac but not morphine exerts inflamatory and metabolic effects in synovial membrane after knee arthroscopy: a double-blind randomized prospective study using the microdialysis technique. Reg Anesth Pain Med. 2009;34:557–564. doi: 10.1097/aap.0b013e3181bfbd9f. [DOI] [PubMed] [Google Scholar]