Abstract
Malignant glomus tumors (MGTs) are exceptional but pose diagnostic and therapeutic challenges. Wide resection is the recommended treatment method, however, no data are available concerning adjuvant therapies.
We present an exceptional case of extradigital deep-seated MGT of the forearm, with an exceptional bone infiltration. Despite being treated with wide resection, the patient had an optimal functional outcome, no functional loss, no motor or sensitive deficits and has returned to his full daily activity.
Keywords: Glomangioma, Malignant glomus tumor, Wide resection, Literature review, Forearm
Introduction
Glomus tumors (GTs) are rare neoplasms originating from the glomus body.1 Glomus tumors are classified into common or solid form, glomangioma, and glomangiomyoma according to histological features.1, 2 Overall, GTs account for about 1.5% of soft tissue tumors, being mostly located in the forearm and the subungual area of the digits,1, 3, 4 and multiple GTs account for 25% of the cases.5 The average duration of symptoms is reported to be between 7 and 11 years before diagnosis, and a wide excision is generally required.1 Despite the fact that GTs are commonly considered benign, malignancy should be considered if they are deep-seated (under muscular fascia), larger than 2 cm, or in the presence of specific histologic features such as nuclear atypia, necrosis, or mitotic activity.6 Fatal cases with distant metastases are occasionally reported, comprising less than 1% of all glomus tumors. Both malignant glomus tumors and glomus tumors of uncertain malignant potential are rarely diagnosed (2.9% and 3.6%, respectively).6 At the moment, few data are available for either therapeutic strategies for malignant glomus tumors, or adjuvant therapies.
We present an exceptional case of extradigital deep-seated MGT of the forearm, with an exceptional bone infiltration. Despite being treated with wide resection, the patient had an optimal functional outcome, no functional loss, no motor or sensitive deficits and has returned to his full daily activity.
Case report
A 46-year-old male patient presented to our clinic due to a mass he discovered on the right forearm five years ago, which was kept under control with periodically performed echo sonographies. He did not have any pain-related symptoms. The patient was only able to use his right arm due to a not well-defined cerebral ischemic event he had during his childhood which ended in paralysis of the left upper limb. Images on echography between controls were usually superimposable until a certain growth of that mass was detected. The patient stated that the radiologists described the mass as a benign cyst which had to be followed up once a year. Unfortunately, we neither have written documentation of those years nor the images of the ultrasounds performed. Five months before, the patient was advised by his primary care physician to undergo an MRI of the right forearm for a visible growth of the neoplasm coupled with the onset of an inflammatory pain on the wrist. A large mass (7 × 1.5 × 1.2 cm), which showed a hypersignal on T2-weighted images and an intermediate signal on T1-weighted images and full-contrast enhancement was detected. The lobulated mass which infiltrated the ulna was located anteriorly to the tendon of the ulnar carpal extensor and posteriorly to the ulnar carpal flexor. It had a necrotic area near to the distal ulna, infiltrated at a depth of 0.5 cm and with a length of 1.6 cm (Fig. 1, Fig. 2, Fig. 3). The core specimen biopsy detected a glomangioma with no histological signs of malignancy (Fig. 4). We performed a wide resection of the neoplasm, including the right distal ulna (the size of the tumor was 6 × 3 × 1 cm). Histological analysis of the resected mass confirmed specimen findings as glomangioma and wide margins of resection (Fig. 5, Fig. 6, Fig. 7) We followed up our patient clinically and radiologically at 3-month intervals (Fig. 8). During the 24th month of the follow-up, he underwent MRIs of the forearm and radiographs of the chest. Despite the wide resection, the patient had an optimal functional outcome, no functional loss, no motor or sensitive deficits and has returned to his full daily activity. No signs of recurrence or metastases were reported.
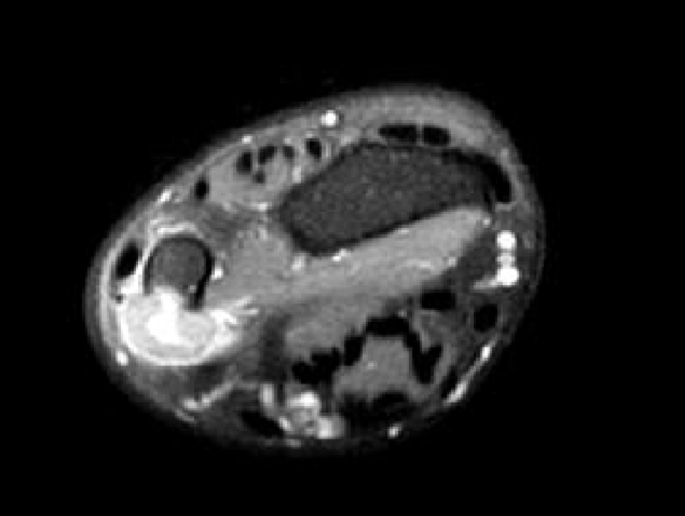
Fig. 1.
Axial STIR image. Infiltration into the right ulna can be seen.
Fig. 2.
Proximal to distal extension of the GT in the coronal plane on T1-weighted image.
Fig. 3.
Plain radiograph showing the bone erosion of the right ulna.
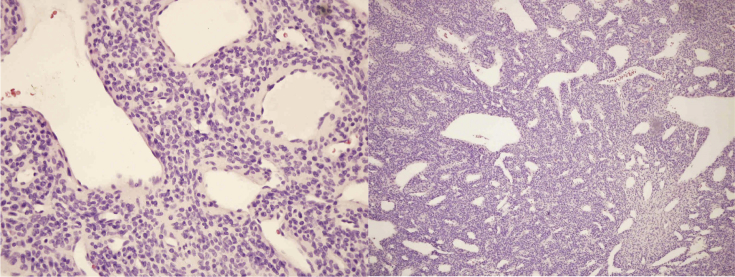
Fig. 4.
Core biopsy specimen (H&E staining;×40 and ×10 magnification). The tumor is composed of small round and uniform cells with a round nucleus and an amphophilic to lightly-eosinophilic cytoplasm. Nests of glomus cells surrounding capillary-sized vessels. Hemangiopericytoma-like vasculature is present.
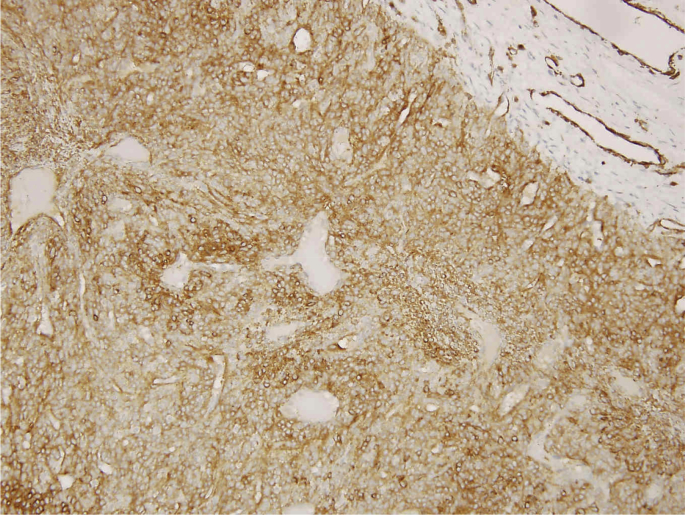
Fig. 5.
Resected specimen including bone margins (×40 magnification). Immunohistochemistry confirmed strong reactivity for SMA.
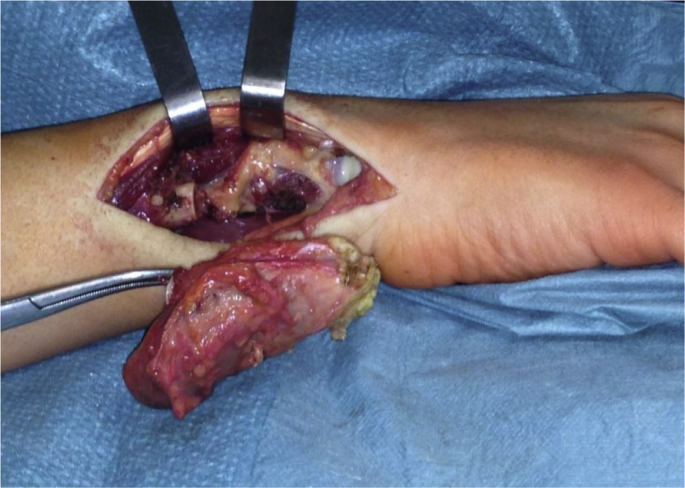
Fig. 6.
Intraoperative photograph showing resection.
Fig. 7.
Postoperative radiograph showing resection.
Fig. 8.
Postoperative photograph of the forearm.
Discussion
We reviewed 40 cases of forearm glomangiomas or malignant glomus tumors described in 13 case reports, one case report review and three retrospective single center studies from 1982 to 2016. The mean size of all the tumors we reviewed was 1.37 cm. The biggest forearm glomus neoplasm was 14 cm in length, but had an intravascular growth in the venous system.7 In one study, an intraosseous growth of a small GT, as in osteoid osteoma, was treated with bone excision, but neither bone erosion nor infiltration was reported.8 One malignant and one atypical GT reported in two other studies9, 10 were treated with surgical excision without adjuvant therapy. However, little data about the follow-up were available since the follow-ups usually had a short duration or did not even take place (Table 1). Glomus tumors, as a very rare group of neoplasms pose diagnostic and therapeutic challenges. Extradigital tumors comprise 27% of the GTs, with the forearm being the most common location. The tumors have an average size of 0.66 cm, ranging from 0.1 to 3 cm.1, 3 On MRI, these neoplasms show an intermediate signal on T1-weighted and a high signal on T2-weighted images with homogeneous contrast enhancement; and larger masses can be lobulated. On echography, glomus tumors present as circumscribed, solid hypoechoic masses that may show small cystic-shaped spaces. Marked blood flow within the masses has been observed on power Doppler and color Doppler ultrasonography.12, 13 Malignant GTs account for 2.9% of all GTs and little data is available about their treatment and follow-up. Mainly all data about MGTs are included in a small retrospective study or in few case reports. Our case was about a glomus tumor with exceptional characteristics. The mass had unusual dimensions; one of the biggest reported in the literature. This neoplasm showed also bone infiltration in the forearm, which was never reported. Although histological characteristics showed no signs of malignancy on biopsy and surgical specimens, we considered our case as an MGT. As Folpe et al6 suggested, its big dimensions and deep position were considered as the markers of malignancy. We performed wide resection, prioritizing the survival of the patient rather than achieving a functional outcome, although our patient had neurological disability. We set a radiological and clinical follow-up each three months for the first two years after surgery since we expected a high risk of recurrence. The criteria to distinguish MGTs derive from a retrospective study of 52 unusual cases, whose conclusions are not supported by strong statistical analysis, and the statistical analysis in estimating the relative risks of malignancy lacked confidence interval and significance due to the small sample size. In such a scenario, the surgeon's experience plays a fundamental role in treatment planning. There is also no significant data about adjuvant treatments. Oncological reference hospitals should share their data and plan for trials to have more information about the diagnosis, classification and treatment of unusual and malignant GTs.
Table 1.
Literature review.
| Title | Authors | Type | Bone erosion | Malignancy | Adjuvant therapy | Year | Dimensions |
|---|---|---|---|---|---|---|---|
| Acquired Solitary Glomangiomyoma on the Forearm: A Rare Case Report | Deger et al18 | Case report | No | No | No | 2016 | 0.5 cm |
| Intravascular extra-digital glomus tumor of the forearm | Muneer et al17 | Case report | No | No | No | 2016 | 2 cm |
| Malignant Glomus Tumor Arising in a Long Standing Precursor Lesion | Damavandy et al9 | Case report | N/A | Yes | N/A | 2016 | N/A |
| The value of diagnostic ultrasonography in the assessment of a glomus tumor of the subcutaneous layer of the forearm mimicking a hemangioma: a case report | Lee et al13 | Case report | No | No | No | 2015 | 0.8 cm |
| Intravascular glomus tumor of the forearm causing chronic pain and focal tenderness | Lee et al15 | Case report | No | No | No | 2014 | 0.5 cm |
| Extradigital glomus tumor: A case report | Chun et al16 | Case report | No | No | No | 2014 | 0.9 cm |
| Painful forearm mass in a 75-year-old man | Schoenleber et al14 | Case report | No | No | No | 2014 | 0.7 cm |
| Atypical venous glomangioma causing chronic compression of the radial sensory nerve in the forearm. A case report and review of the literature | Jiga et al10 | Case report | No | No | No | 2012 | 0.4 cm |
| Intraosseous glomus tumor of the ulna: a case report with radiographic findings and a review of the literature | Urakawa et al8 | Case report | N/A | No | No | 2008 | N/A |
| Glomus tumor--the report of a case in an adult Nigerian | Yakubu et al20 | Case report | No | No | No | 2005 | N/A |
| Giant intravenous glomus tumor | Acebo et al7 | Case report | No | No | No | 1997 | 14 cm |
| Intravenous glomus tumor of the forearm | Googe and Griffin19 | Case report | N/A | N/A | N/A | 1993 | N/A |
| Glomus tumor: a clinicopathologic and electron microscopic study | Tsuneyoshi and Enjoji11 | Case report review | No | No | No | 1982 | 0.75 cm |
| Imaging features of glomus tumors | Glazebrook et al12 | Retrospective study, single center | No | No | No | 2011 | 0.75 cm |
| Extradigital glomus tumors: a 20-year experience | Schiefer et al1 | Retrospective study, single center | No | No | No | 2006 | 0.6 cm |
| Atypical and malignant glomus tumors: analysis of 52 cases, with a proposal for the reclassification of glomus tumors | Folpe et al6 | Retrospective study, single center | N/A | N/A | No | 2001 | 2 cm |
N/A: Data not available.
In conclusion, planning therapeutic strategies for this rare case is challenging. The literature usually consists of case reports but very few reviews. Considering the increase in the number of case reports on GTs in recent years, we should find a standardized way to collect all data in the case reports. Having more standardized data should help in planning better therapeutic strategies.
Footnotes
Peer review under responsibility of Turkish Association of Orthopaedics and Traumatology.
References
- 1.Schiefer T.K., Parker W.L., Anakwenze O.A., Amadio P.C., Inwards C.Y., Spinner R.J. Extradigital glomus tumors: a 20-year experience. Mayo Clin Proc. 2006;81:1337–1344. doi: 10.4065/81.10.1337. [DOI] [PubMed] [Google Scholar]
- 2.Mravic M., LaChaud G., Nguyen A., Scott M.A., Dry S.M., James A.W. Clinical and histopathological diagnosis of glomus tumor: an institutional experience of 138 cases. Int J Surg Pathol. 2015;23:181–188. doi: 10.1177/1066896914567330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lee D.W., Yang J.H., Chang S. Clinical and pathological characteristics of extradigital and digital glomus tumours: a retrospective comparative study. J Eur Acad Dermatol Venereol. 2011;25:1392–1397. doi: 10.1111/j.1468-3083.2011.03979.x. [DOI] [PubMed] [Google Scholar]
- 4.Kransdorf M.J. Benign soft-tissue tumors in a large referral population: distribution of specific diagnoses by age, sex, and location. AJR Am J Roentgenol. 1995;164:395–402. doi: 10.2214/ajr.164.2.7839977. [DOI] [PubMed] [Google Scholar]
- 5.Maxwell G.P., Curtis R.M., Wilgis E.F. Multiple digital glomus tumors. J Hand Surg Am. 1979;4:363–367. doi: 10.1016/s0363-5023(79)80076-3. [DOI] [PubMed] [Google Scholar]
- 6.Folpe A.L., Fanburg-Smith J.C., Miettinen M., Weiss S.W. Atypical and malignant glomus tumors: analysis of 52 cases, with a proposal for the reclassification of glomus tumors. Am J Surg Pathol. 2001;25:1–12. doi: 10.1097/00000478-200101000-00001. [DOI] [PubMed] [Google Scholar]
- 7.Acebo E., Val-Bernal J.F., Arce F. Giant intravenous glomus tumor. J Cutan Pathol. 1997;24:384–389. doi: 10.1111/j.1600-0560.1997.tb00808.x. [DOI] [PubMed] [Google Scholar]
- 8.Urakawa H., Nakashima H., Yamada Y., Tsushima M., Ohta T., Nishio T. Intraosseous glomus tumor of the ulna: a case report with radiographic findings and a review of the literature. Nagoya J Med Sci. 2008;70:127–133. [PubMed] [Google Scholar]
- 9.Damavandy A.A., Anatelli F., Skelsey M.K. Malignant glomus tumor arising in a long standing precursor lesion. Am J Dermatopathol. 2016;38:384–387. doi: 10.1097/DAD.0000000000000481. [DOI] [PubMed] [Google Scholar]
- 10.Jiga L.P., Rata A., Ignatiadis I., Geishauser M., Ionac M. Atypical venous glomangioma causing chronic compression of the radial sensory nerve in the forearm. A case report and review of the literature. Microsurgery. 2012;32:231–234. doi: 10.1002/micr.20983. [DOI] [PubMed] [Google Scholar]
- 11.Tsuneyoshi M., Enjoji M. Glomus tumor: a clinicopathologic and electron microscopic study. Cancer. 1982;50:1601–1607. doi: 10.1002/1097-0142(19821015)50:8<1601::aid-cncr2820500823>3.0.co;2-5. [DOI] [PubMed] [Google Scholar]
- 12.Glazebrook K.N., Laundre B.J., Schiefer T.K., Inwards C.Y. Imaging features of glomus tumors. Skeletal Radiol. 2011;40:855–862. doi: 10.1007/s00256-010-1067-1. [DOI] [PubMed] [Google Scholar]
- 13.Lee D.Y., Hwang S.C., Jeong S.T. The value of diagnostic ultrasonography in the assessment of a glomus tumor of the subcutaneous layer of the forearm mimicking a hemangioma: a case report. J Med Case Rep. 2015;9:191. doi: 10.1186/s13256-015-0672-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Schoenleber S.J., Rosenberg A.E., Temple H.T. Painful forearm mass in a 75-year-old man. Clin Orthop Relat Res. 2014;472:776–780. doi: 10.1007/s11999-013-3409-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lee S.K., Song D.G., Choy W.S. Intravascular glomus tumor of the forearm causing chronic pain and focal tenderness. Case Rep Orthop. 2014;2014:619490. doi: 10.1155/2014/619490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Chun J.S., Hong R., Kim J.A. Extradigital glomus tumor: a case report. Mol Clin Oncol. 2014;2(2):237–239. doi: 10.3892/mco.2013.219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Muneer M., Alkhafaji A., El-Menyar A., Al-Hetmi T., Al-Basti H., Al-Thani H. Intravascular extra-digital glomus tumor of the forearm. J Surg Case Rep. 2016;2016(7):1–3. doi: 10.1093/jscr/rjw124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Deger A.N., Deger H., Tayfur M., Balcioglu M.G., Kadioglu E. Acquired solitary glomangiomyoma on the forearm: a rare case report. J Clin Diagn Res. 2016;10:ED10–ED11. doi: 10.7860/JCDR/2016/19062.8195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Googe P.B., Griffin W.C. Intravenous glomus tumor of the forearm. J Cutan Pathol. 1993;20:359–363. doi: 10.1111/j.1600-0560.1993.tb01276.x. [DOI] [PubMed] [Google Scholar]
- 20.Yakubu A.A., Mohammed A.Z., Edino S.T., Sheshe A.A. Glomus tumour--the report of a case in an adult Nigerian. Niger J Med. 2005;14:97–99. doi: 10.4314/njm.v14i1.37145. [DOI] [PubMed] [Google Scholar]