Abstract
Background/purpose
Clinically, PMMA resin is extensively used for fabricating provisional FPDs. However, fracture often occurs due to the unsatisfactory mechanical strength, especially within connectors of long-span provisional FPDs. The purpose of this study is to evaluate the fracture load of fiber-reinforced provisional FPDs with various pontic span lengths, and to identify the most suitable span length for fiber-reinforced long-span provisional FPDs.
Materials and methods
Fifty-six provisional FPDs with various pontic span lengths were fabricated. Seven samples from each group were reinforced with glass fibers. Unreinforced counterparts served as control. The samples were fixed on the abutments after thermocycling and then received a fatigue test. Subsequently, they were mechanically loaded until fracture, and the initial fracture load and fracture patterns were recorded. Statistical analysis, including two-sample t-test, one-way, two-way ANOVA, Tukey-Kramer HSD post hoc analysis and χ2 test were used to evaluate mechanical performance.
Results
The mean fracture load of FPDs with 14 mm pontic span length is significantly higher than the other lengths. The fracture load of each reinforced group is significantly higher than each counterpart control. There is no interaction between two variables, pontic span and fiber reinforcement. With fiber reinforcement, the fracture patterns were altered from catastrophic fracture to bent or partial fracture. But, the fracture patterns were not affected by pontic span.
Conclusion
The fracture load of acrylic FPDs decreases significantly when pontic span length is greater than 17 mm. Adding glass fibers into long-span provisional FPDs can significantly improve the fracture resistance and fracture patterns.
Keywords: Fiber-reinforced, Glass fiber, Pontic span length, Provisional fixed partial dentures
Introduction
Fracture often occurs in provisional fixed partial dentures (FPDs) made by Polymethyl Methacrylate (PMMA) due to its unsatisfactory mechanical strength.1, 2, 3 Although its transverse strength can be increased by embedding metal wire,4,5 pores often exist on the interface between metal and resin matrix.6 Substantially, it cannot increase ultimate strength and fatigue resistance.7
Carbon fiber effectively improves fatigue resistance,8 impact strength,9 and transverse strength of PMMA resin.10 But it also exhibits operational inconvenience, unsatisfactory aesthetics, and toxicity.8,10 Kevlar® fiber owns superior mechanical strength.11 However, the yellowish appearance jeopardize esthetics, and the rough surface causes difficulties in polishing.8,10 Ultra-High Molecular Weight Polyethylene (UHMWP) fiber features excellent ductility, superior esthetic color, low density, and good biocompatibility.12 Treating with plasma can improve its poor adhesion to resin matrix, but that needs cautious handling.13 With improved esthetics, biocompatibility, handling and mechanical properties, glass fiber has been widely used.9,14 Pre-impregnating silane-treated glass fiber can successfully adhere to resin matrix and enhance the fracture resistance.15,16
The position of fiber is crucial for reinforcing effect, more so than the length and the adhesion.17,18 Placing fibers in the tensile zone can effectively reinforce acrylic resin.2,3,18 To maximize the reinforcing effect, fibers should be oriented perpendicular to the force direction.1,19 Increasing the weight percentage of fiber increased the fracture load and impact strength.2,20 However, excessive fiber concentrations may produce the opposite effect.21 When the thickness of fibers exceeded 0.6 mm, the reinforcing effect becomes less significant.22
Previous studies show that the mean fracture resistance of the three-unit provisional FPDs is 614 N without fiber reinforcement and 659 N with fiber reinforcement.4 The mean masticatory force in the molar area is about 500 N–600 N.23 Therefore, the reinforcement for three-unit FPDs is not clinically required, while reinforcing four- or more-units provisional FPDs is necessary.17,18
The length/diameter ratio and span length influence the strength of fiber-reinforced composite resin.24 A previous study showed fiber-reinforced PEMA and PBMA FPDs with longer span length yielded superior reinforcement effects.2 However, the fiber position was not the same due to inadequate specimen preparation protocols.2 Moreover, glass fibers were only used in four-unit provisional FPDs of 17 and 19.5 mm span lengths, so the reinforcing effect for other span lengths was not evaluated. In another study, composite resin (Tagis/Vectris) and polyethylene fibers (Ribbond) were used to fabricate 3-, 4-, and 5-unit provisional FPDs (12, 19, and 30 mm span lengths, respectively). The reinforcing effect does not vary with span length while the surface treatment of fiber plays a more important role.25 The effect of span lengths on the fiber-reinforced provisional FPDs remains uncertain.
Fractures are often caused clinically by water sorption,26,27 thermal cycling,28 and repeated loading. The absorbed water acts as a plasticizer and reduces the strength of PMMA resin.27 The flexural strength of the composite resin was significantly reduced, by approximately 31%–41%, within the first 5000 thermal cycles at 4 °C–60 °C per min.28 The fatigue resistance of cylinders made by fiber-reinforced composite resin was evaluated with a constant-deflection of 1 mm.29 The resistance of acrylic denture reinforced with glass fibers and metal wires was evaluated using repeated loading of 180 N until fracture.7 However, evaluation of provisional FPDs’ mechanical performance under repeated loading is limited.
The aim of this investigation was to determine the influences of different pontic span lengths on the fracture load and fracture pattern of fiber-reinforced provisional FPDs, and to identify the most suitable span length for fiber-reinforced long-span provisional FPDs. The null hypothesis was that pontic span lengths or fiber reinforcement of provisional FPDs would not affect the fracture load and patterns.
Materials and methods
Multi-unit provisional FPDs with 14, 17, 20, and 24 mm span lengths, measured from the distal side of premolars to the mesial side of molars, were fabricated. Within each group, seven FPDs were reinforced with BisGMA-preimpregnated S2-glass fiber (FibreKor, Jeneric/Pentron, Wallingford, CT, USA), and the others without fiber reinforcement served as control. Fibers were placed close to the lower border of the connectors, horizontally aligned through each connector and pontic, and extended to both axial walls of the abutments. All samples were divided into eight groups (N = 7) according to their span lengths and whether reinforcing fibers were used or not.
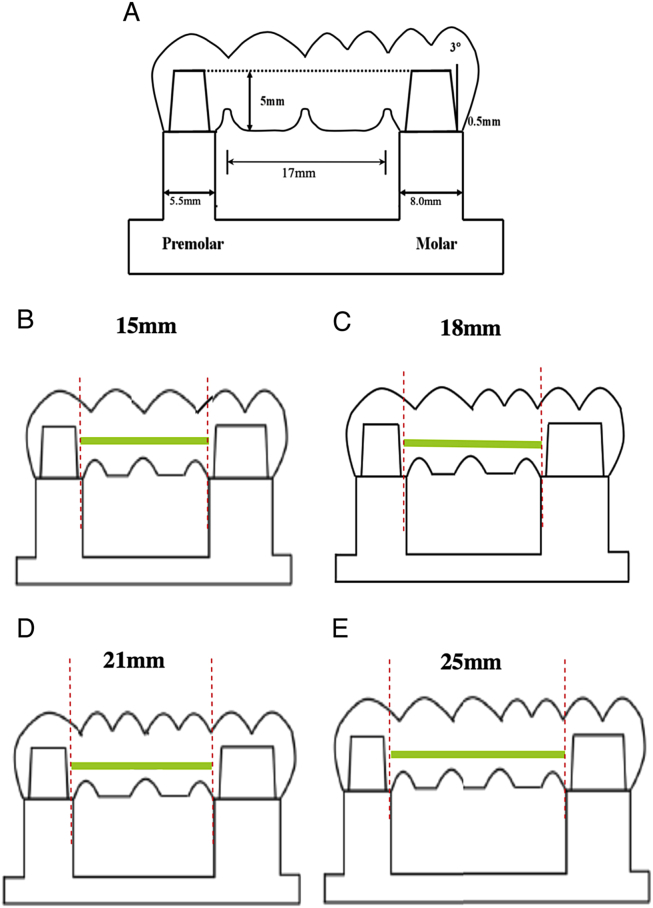
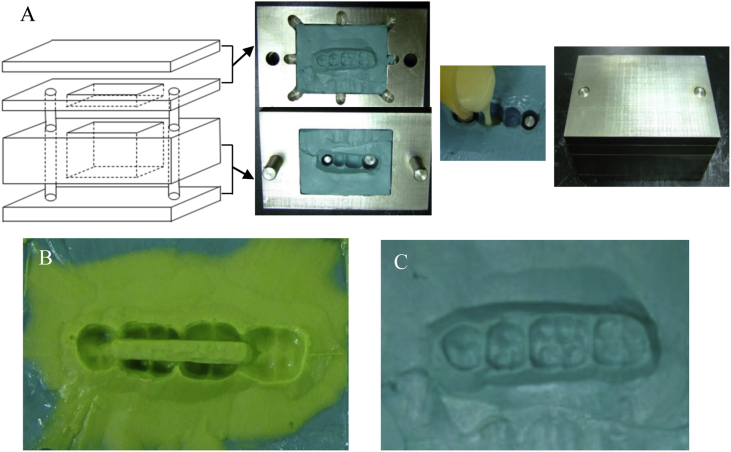
A stainless steel jig was made to simulate the edentulous condition of long-span mandibular multi-unit FPDs (Fig. 1). Each abutment was 5.0 mm in height with a total occlusal convergence of 6° and the shoulder margin was 0.5 mm in width. The wax pattern from each group was first made on a metal jig with inlay wax (Inlay wax, Hard, GC Corporation, Tokyo, Japan). To fabricate fiber-reinforced ones, a slot 3.0 mm wide by 4.0 mm deep with lengths of 15, 18, 21, and 25 mm were respectively prepared in FPDs of 14, 17, 20, and 24 mm using a flat-end tungsten carbide bur mounted on a milling machine (Bachmann milling unit model 82; Cendres & Metaux, Biel-Bienne, Switzerland). Subsequently, the impression was made to form two molds using polyvinylsiloxane putty (Take 1, Kerr, Orange, CA, USA) in a metal fixture (Fig. 2).
Figure 1.
(A) A cross-sectional view of a provisional FPD of 17 mm pontic span length, measured from the distal contact surface of the premolars to the mesial contact surface of the molars. The fiber length for each group was (B) 15 mm, (C) 18 mm, (D) 21 mm, (E) 25 mm.
Figure 2.
(A) Polyvinylsiloxane putty was placed in a metal fixture to duplicate the samples. (B) Polyvinylsiloxane mold for fabricating PMMA FPDs with fibers. (C) Polyvinylsiloxane mold for fabricating PMMA FPDs without fibers.
The molds were used to duplicate the FPDs. The PMMA resin (Tempron, GC Corporation, Tokyo, Japan) was poured into the molds to construct samples of various span lengths. Fibers were light-cured for 20 s and placed in the slots. Subsequently, the slots were filled with PMMA resin to the original contour. All samples were placed in a water bath at 50 ± 1 °C for 10 min for complete polymerization, and measured to ensure dimensional errors were less than 0.1 mm after finishing and polishing.
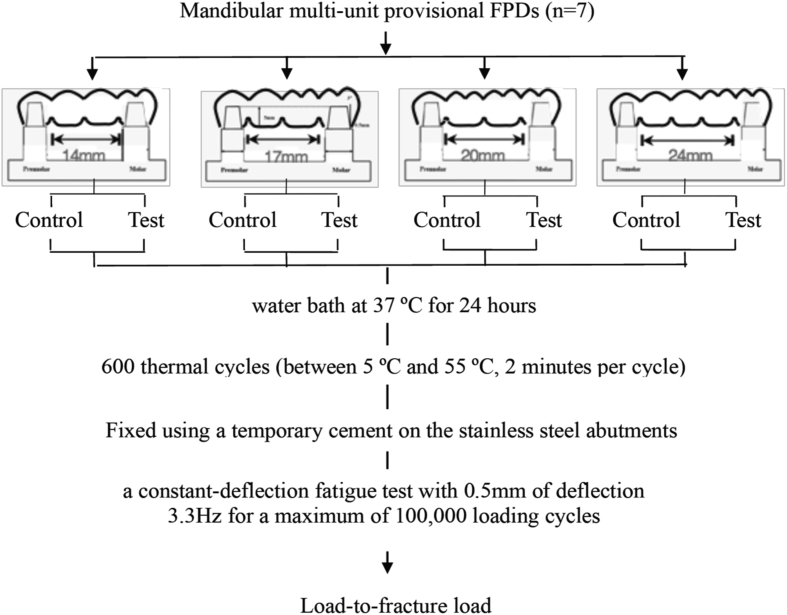
The flow chart was shown in Fig. 3. All FPDs were stored in distilled water at 37 ± 1 °C for 24 h, thermocycled for 600 cycles (5 °C/55 °C for 2 min per cycle), and air-dried for 24 h at room temperature. Then, they were installed on metal jigs with Polycarboxylate cement (Hy-Bond, Shofu Inc., Kyoto, Japan) and an object of 5 kg was placed on them for five minutes. A universal testing machine (858 Mini Bionix II, MTS) was used to perform fatigue testing under a constant deflection of 0.5 mm at 3.3 Hz for 100,000 times to simulate six-months’ chewing.30 Samples were loaded with a steel ball of 6 mm in diameter at the central region of the occlusal surface, and a 0.5-mm-thick aluminum foil was placed between them. After fatigue testing, they were loaded to fracture with a crosshead speed of 5.0 mm per minute. The initial fracture load was defined as when any two signs of the first declining point of the force-deflection curve appeared, the first audible cracking sound was heard, or the first visible crack appeared.31 In addition, the fracture patterns were examined under an optical microscope.
Figure 3.
A flow chart of the present study.
The fracture load and patterns were statistically analyzed using software (JMP 7.0, SAS Institute Inc., Cary, NC, USA). One-way ANOVA was used to evaluate the influence of span length on the final fracture load. The Tukey–Kramer method was adopted for performing post-hoc tests. A two-sample t-test was performed to examine the influence of fiber reinforcement on the mechanical performance. Two-way ANOVA was used to determine the interaction between fiber reinforcement and span length. The differences were considered statistically significant when the p-value is less than 0.05. Finally, a Chi-square (χ2) test was performed to analyze fracture patterns.
From each group, three samples were selected and spotted with gold particles for 180 s by using a vacuum metallizing machine (E-1010, Hitachi, Japan). Subsequently, the fracture surfaces were examined using a scanning electron microscope (SEM; EMAX, S-3000 N, Hitachi, Japan) with a magnification from 40× to 1500× at an accelerating voltage of 15 kV.
Results
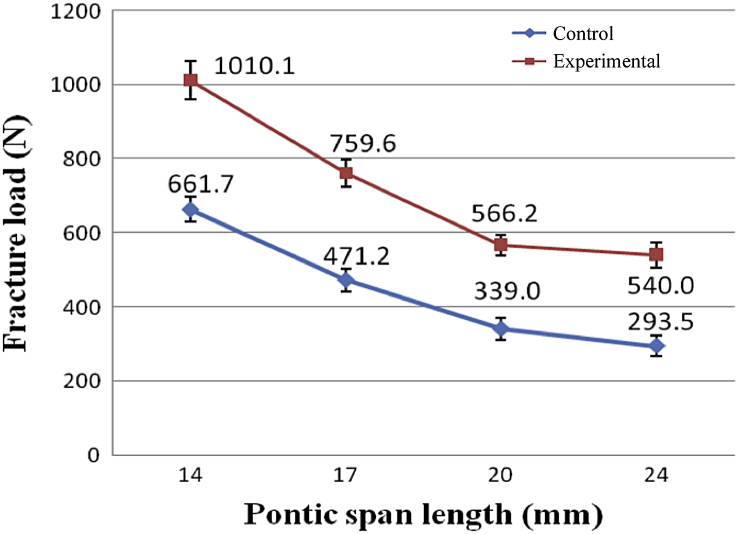
Fracture load
The mean fracture load of the control and experimental groups ranged from 661.7 N to 293.5 N and 1010.1 N–540.0 N. There is a significant difference among both groups and the post-hoc comparison showed that the FPDs with 14 mm span length have the highest mean fracture loads (Table 1). However, no significant difference was found between 20 mm and 24 mm. Both groups showed the similar trend (Fig. 4). The fracture loads of the FPDs with fiber reinforcement were significantly higher (Table 2). The mean fracture load was increased by 65.51%, 62.03%, 59.87% and 54.35%, respectively for those with 14, 17, 20, and 24 mm span lengths. The reinforcing effect was not significantly influenced by pontic span length and vice versa (Table 3).
Table 1.
Mean fracture load of provisional FPDs with various span lengths (n = 7).
| Pontic span length (mm) | Fracture load (N) Mean ± SD |
P-value of One-way ANOVA | Post hoc comparison | ||
|---|---|---|---|---|---|
| Control groups | |||||
| 14 | 661.7 ± 91.1 | <0.0001 | A | ||
| 17 | 471.2 ± 80.1 | B | |||
| 20* | 339.0 ± 77.2 | C | |||
| 24* | 293.5 ± 75.4 | C | |||
| Experimental groups | |||||
| 14 | 1010.1 ± 136.3 | <0.0001 | A | ||
| 17 | 759.6 ± 96.8 | B | |||
| 20* | 566.2 ± 73.3 | C | |||
| 24* | 540.0 ± 90.2 | C | |||
*Groups with the same letter do not significantly differ at P < 0.0001.
Figure 4.
Mean fracture loads of provisional FPDs with various span lengths from the experimental and control groups.
Table 2.
Comparisons between the mean fracture load of provisional FPDs with various span lengths.
| Group | Pontic span length (mm) |
|||
|---|---|---|---|---|
| 14 |
17 |
20 |
24 |
|
| Mean ± SD | Mean ± SD | Mean ± SD | Mean ± SD | |
| Experiment | 1010.1 ± 136.3 | 759.6 ± 96.8 | 566.2 ± 73.3 | 540.0 ± 90.2 |
| Control | 661.7 ± 91.1 | 471.2 ± 80.1 | 339.0 ± 77.2 | 293.5 ± 75.4 |
| P-value of 2-sample t-test | 0.0001 | <0.0001 | 0.0001 | 0.0001 |
Table 3.
Two-way ANOVA analysis regarding the effects of fiber reinforcement and pontic span length on the fracture load of provisional FPDs.
| Source | DF | Sum of squares | F ratio | P-value |
|---|---|---|---|---|
| Pontic span length | 3 | 1534912.9 | 60.3861 | <0.0001 |
| Fiber reinforcement | 1 | 1078836.9 | 127.3299 | <0.0001 |
| Pontic span length * Fiber reinforcement | 3 | 30248.8 | 1.1900 | 0.3235 |
Fracture pattern
Based on clinical observation and literature review, the fracture patterns of PMMA FPDs were classified into three types.1,17,32 The first was “catastrophic failure,” in which the pontics were broken into pieces. The second was “bent failure,” in which an observable gap was detected within the pontic region. Samples were, however, still held together. The third was “partial fracture,” in which the samples remained intact and only fracture lines can be detected.17 Among 28 samples from the control groups, 25 exhibited catastrophic fracture and 3 exhibited bent fracture, while from the experimental groups, 18 exhibited partial fracture and 10 exhibited bent fracture.
Table 4 showed no significant difference among the different groups of various span lengths for both the control and experimental groups, indicating that span length did not influence fracture pattern. However, a significant difference was found between the FPDs with or without fiber reinforcement, indicating that fracture pattern changed after fiber reinforcement.
Table 4.
Comparisons of the fracture patterns of provisional FPDs from various groups.
| Fracture pattern | Partial | Bent | Catastrophic | ||
|---|---|---|---|---|---|
| Effect of Pontic Span Length on Fracture Pattern of FPDs with or without Fiber Reinforcement | |||||
| Categories (Pontic span length) | χ2(df = 3) | Significance | |||
| Control groups | |||||
| 14 | 0 (0.00%) | 1 (14.29%) | 6 (85.71%) | 1.08 | P = 0.7819 |
| 17 | 0 (0.00%) | 1 (14.29%) | 6 (85.71%) | ||
| 20 | 0 (0.00%) | 1 (14.29%) | 6 (85.71%) | ||
| 24 | 0 (0.00%) | 0 (0.00%) | 7 (100.00%) | ||
| Experimental groups | |||||
| 14 | 5 (71.43%) | 2 (28.57%) | 0 (0.00%) | 1.80 | P = 0.6149 |
| 17 | 5 (71.43%) | 2 (28.57%) | 0 (0.00%) | ||
| 20 | 5 (71.43%) | 2 (28.57%) | 0 (0.00%) | ||
| 24 | 3 (42.86%) | 4 (57.14%) | 0 (0.00%) | ||
| Effect of Fiber Reinforcement on Fracture Pattern of FPDs with Various Span Lengths | |||||
| Categories (Fiber reinforcement) | χ2(df = 1) | Significance | |||
| 14 mm | |||||
| Control | 0 (0.00%) | 1 (14.29%) | 6 (85.71%) | 10.36 | P = 0.0013 |
| Experimental | 5 (71.43%) | 2 (28.57%) | 0 (0.00%) | ||
| 17 mm | |||||
| Control | 0 (0.00%) | 1 (14.29%) | 6 (85.71%) | 10.36 | P = 0.0013 |
| Experimental | 5 (71.43%) | 2 (28.57%) | 0 (0.00%) | ||
| 20 mm | |||||
| Control | 0 (0.00%) | 1 (14.29%) | 6 (85.71%) | 10.36 | P = 0.0013 |
| Experimental | 5 (71.43%) | 2 (28.57%) | 0 (0.00%) | ||
| 24 mm | |||||
| Control | 0 (0.00%) | 0 (0.00%) | 7 (100.00%) | 11.58 | P = 0.0007 |
| Experimental | 3 (42.86%) | 4 (57.14%) | 0 (0.00%) | ||
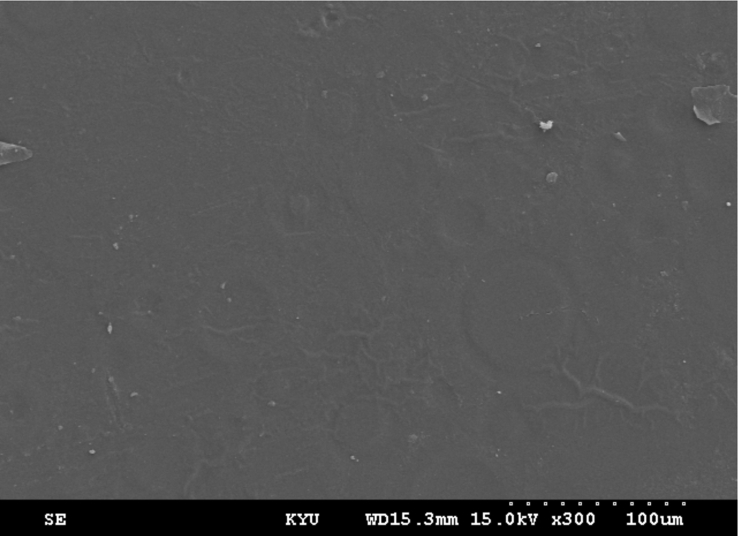
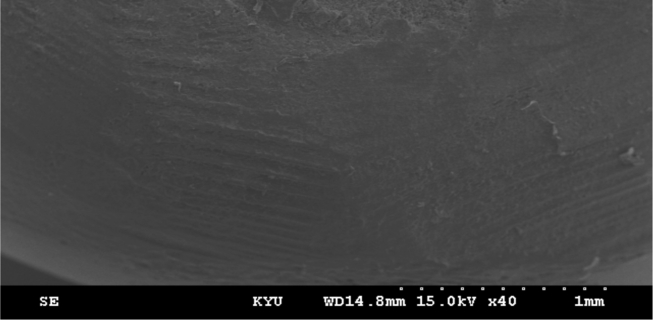
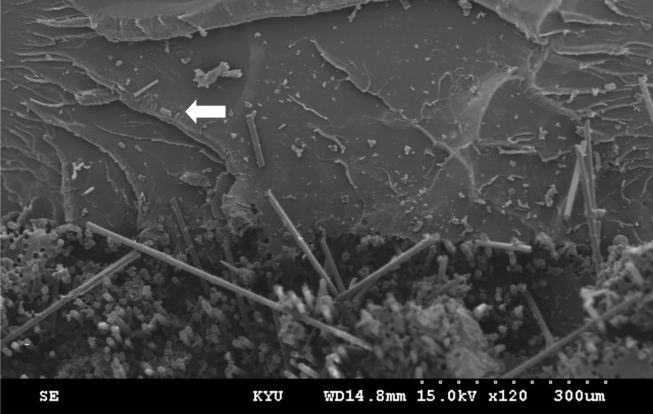
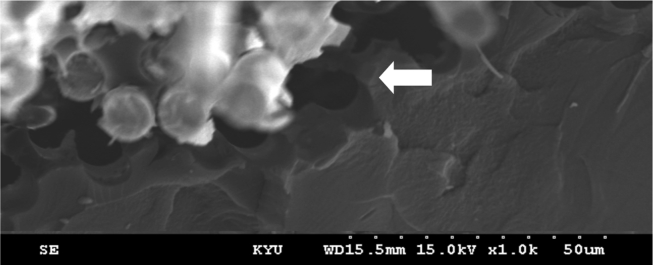
SEM observation
The smooth fractured surfaces of the control groups indicated brittle fracture (Fig. 5). Some fatigue marks caused by repeated loading were found under SEM (Fig. 6), similar to the previous study.7 Irregular roughness was found on the fractured surfaces of the experimental groups (Fig. 7). The outer layer of the glass fiber was delaminated from the resin, and it left a trace on the resin matrix (Fig. 8), also found in a previous study.20
Figure 5.
Fractured surface of a sample without fiber reinforcement (300× magnification). The smooth surface outlook demonstrates the characteristics of brittle fracture.
Figure 6.
The fractured surface of a sample without fiber reinforcement (40× magnification), showing fatigue marks caused by repeated loading.
Figure 7.
The fractured surface of a sample with fiber reinforcement (120× magnification). The arrow (⇦) indicates the irregularly fractured surface.
Figure 8.
The fractured surface of a sample with fiber reinforcement (1000× magnification). The outer layer of glass fiber separated from the resin (⇦) and left a mark on the resin matrix, indicating the excellent impregnation between the fiber and matrix.
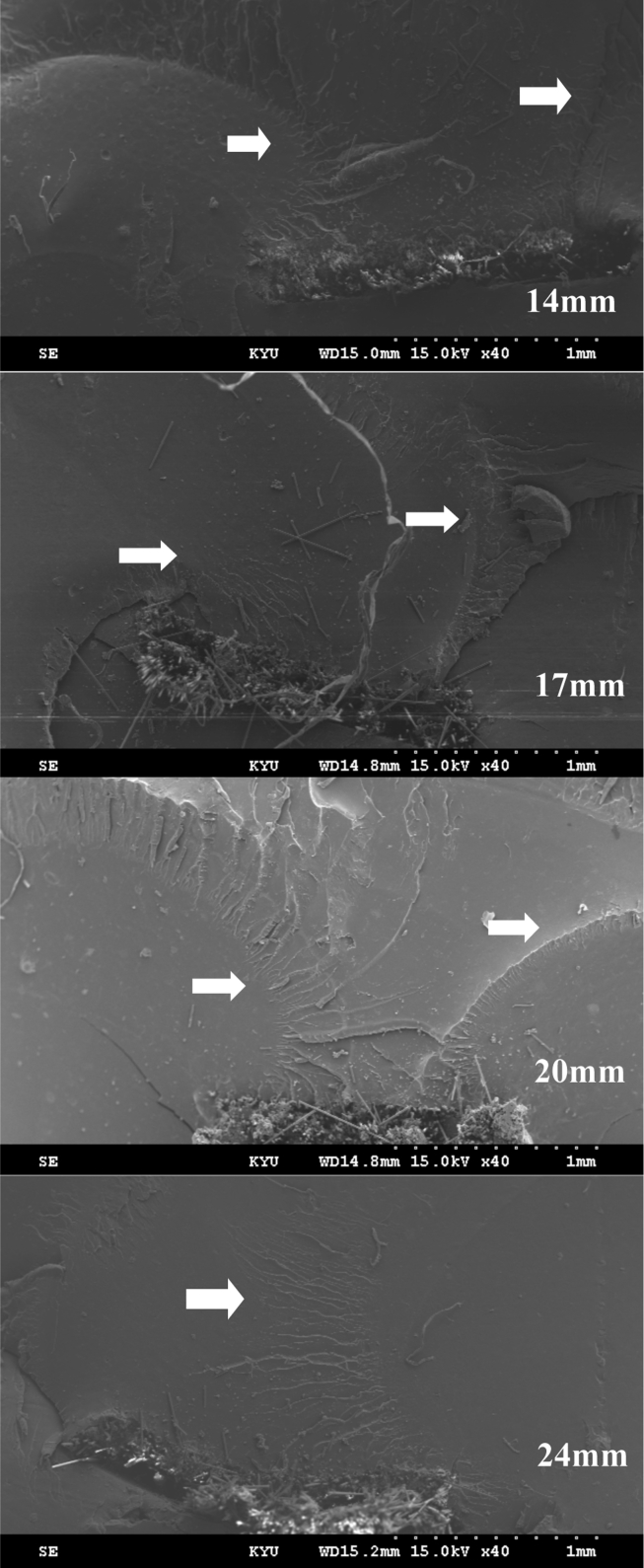
Cracks of the experimental groups of various span lengths first occurred on the tension side and extended to the pressure side. For samples exhibiting short span lengths, the cracks propagated to the buccal and lingual sides. As the pontic span increased, the cracks went through the fibers to the pressure side, although this phenomenon only occurred on the samples of 24 mm pontic span (Fig. 9).
Figure 9.
The fractured sample surfaces of various span lengths with fiber reinforcement (40× magnification). The white arrows indicate the locations of crack lines.
Discussion
Among all samples, FPDs with 14 mm span length has the highest mean fracture load and no significant difference between those with 20 mm and 24 mm span length. For the fracture pattern, no significant difference was found among various pontic span lengths within either the control or experimental groups. However, the existence of fiber reinforcement significantly changed the fracture patterns. Therefore, based on the above findings, the null hypothesis of the present study is rejected.
A span length of 17 mm or more significantly reduces fracture load (Table 1) and fiber reinforcement significantly increases fracture load (Table 2), similar to previous studies.2,33 The previous study concluded that fiber should be used to enhance the fracture resistance if longer pontic spans are considered, although the longest pontic span length was only 19.5 mm.2 It found that the reinforcing effect increased when span length became longer, which is contradictive to our study. The possible reason is that the proportion of fiber was decreased when the span length became longer. Pontic span and fiber reinforcement significantly influence the fracture load of long-span provisional FPDs, but the interaction effect was not significant (Table 3). It implies that the effect of pontic span length on fracture load was not influenced by fiber reinforcement.
The mean fracture loads measured in this study are lower than those in a previous study.2 This can be attributed to the thermal cycling and repeated loading. In addition, the fracture load for a span length of 17 mm was not different from our previous findings, in which cyclic loading was not considered. One possible reason is that thermal cycling can more significantly influence the strength of fiber-reinforced FPDs than cyclic loading.34
When the pontic span length is 17 mm or more, the mean fracture load of the control groups is significantly reduced and lower than 500 N (Fig. 4). The mean masticatory force in molar is 500–600 N.23 Reinforcing fiber should be applied when the span length exceeds 17 mm, representing the sum of the mesiodistal widths of a premolar and molar.
In this study, span length is not correlated with the fracture pattern, but it distinctly changed after fiber reinforcement. The control groups mostly exhibited catastrophic failure. Fiber-reinforced samples exhibited partial fracture, conversely. The fracture first initiated at the cervical third of a connector, then extended upward to the fiber-reinforced part, and was finally stopped spreading to the occlusal surface. However, not all fiber-reinforced samples behaved the same. Several samples presented bent fracture, where fracture went through the fiber-reinforced part without being completely stopped. The fracture bypassed the fiber and moved toward the occlusal surface. The percentage of the occurrence of bent fractures increased when span length became longer. A similar phenomenon of bent fracture was observed, and the bonding strength varied at different fiber locations.35
Three different resin-preimpregnated glass fibers (Stick®, EverStick®, and FibreKor®) yielded similar reinforcing results in transverse strength of denture base.32 However, the hydrolytic stability of glass fiber is correlated with the amount of B2O3. FibreKor®, used in this study contains only 0.1% B2O3, which is significantly less than the 6%–9% B2O3 contained in Stick®. The hydrolytic stability of FibreKor® is superior to that of Stick®. In terms of manipulation, FibreKor® is also easier than Stick®, because it can be photo-polymerized to the desired shape. Furthermore, FibreKor® is substantially thinner compared with Stick® and more suitable for clinical use. Therefore, FibreKor® was selected for this study.
An indirect method is used to control the fiber position in the tensile zone.2,3,18 To place fibers slightly away from the bottom of connectors avoids exposing and accumulating plaque.36 The interface between the acrylic was examined under SEM and found no significant flaw (Fig. 6). Fibers were not required to extend across the occlusal surfaces of both abutments because pontic and connector areas were highly stressed.17,22,25
Most studies evaluate provisional FPDs' survival for six months. Also provisional FPDs are required for complex cases such as full mouth reconstruction. Patients usually need to wear these provisional FPDs for six months or more. Based on previous studies, samples were stored in distilled water at 37 ± 1 °C for 24 h and thermocycled from 5 to 55 °C for 600 times to simulate six-month clinical use.12,17 However, limited studies on fiber-reinforced acrylic resin simulated cyclic loading. A fatigue testing machine with 0.5 mm of deflection at 3.3 Hz for 100,000 times was used to simulate six-months’ chewing in this study.30 Compared with our previous findings for samples not experiencing cyclic loading, more bent fracture occurred.
Owing to the limitations of this study, the samples were fabricated with PMMA resin and using different material can lead to different outcome. In addition, the load direction has the greatest impact on strength.33 Oblique occlusal force can be more detrimental and produces greater maximum principal stress than does axial force. Additional studies based on well-controlled randomized clinical trials will help us more comprehensively understand the mechanical performance of fiber-reinforced acrylic provisional FPDs.
The fracture loads of the long-span acrylic FPDs with fiber reinforcement were significantly higher than those without fiber reinforcement. The fracture load decreased significantly when pontic span length is greater than 17 mm. The reinforcing effect of fiber was not significantly influenced by pontic span length and vice versa. Span length did not influence fracture pattern. However, fracture pattern was improved after fiber reinforcement.
Conflicts of interest
None declared.
Acknowledgments
This research is partially supported and sponsored by the Ministry of Science and Technology, Taiwan, R.O.C. under Grant no. NSC98-2320-B-037-004-MY3.
Footnotes
Supplementary data related to this article can be found at https://doi.org/10.1016/j.jds.2018.11.008.
Contributor Information
Yung-Chung Chen, Email: yc_chen@mail.ncku.edu.tw.
Jen-Chyan Wang, Email: jechwz@kmu.edu.tw.
Appendix A. Supplementary data
The following is the supplementary data related to this article:
References
- 1.Samadzadeh A., Kugel G., Hurley E., Aboushala A. Fracture strengths of provisional restorations reinforced with plasma-treated woven polyethylene fiber. J Prosthet Dent. 1997;78:447–450. doi: 10.1016/s0022-3913(97)70058-1. [DOI] [PubMed] [Google Scholar]
- 2.Nohrström T.J., Vallittu P.K., Yli-Urpo A. The effect of placement and quantity of glass fibers on the fracture resistance of interim fixed partial dentures. Int J Prosthodont. 2000;13:72–78. [PubMed] [Google Scholar]
- 3.Hamza T.A., Rosenstiel S.F., El-Hosary M.M., Ibraheem R.M. Fracture resistance of fiber-reinforced PMMA interim fixed partial dentures. J Prosthodont. 2006;15:223–228. doi: 10.1111/j.1532-849X.2006.00110.x. [DOI] [PubMed] [Google Scholar]
- 4.Vallittu P.K. The effect of glass fiber reinforcement on the fracture resistance of a provisional fixed partial denture. J Prosthet Dent. 1998;79:125–130. doi: 10.1016/s0022-3913(98)70204-5. [DOI] [PubMed] [Google Scholar]
- 5.Vallittu P.K. A review of methods used to reinforce polymethyl methacrylate resin. J Prosthodont. 1995;4:183–187. doi: 10.1111/j.1532-849x.1995.tb00338.x. [DOI] [PubMed] [Google Scholar]
- 6.Vallittu P.K. Dimensional accuracy and stability of polymethyl methacrylate reinforced with metal wire or with continuous glass fiber. J Prosthet Dent. 1996;75:617–621. doi: 10.1016/s0022-3913(96)90246-2. [DOI] [PubMed] [Google Scholar]
- 7.Vallittu P.K. Comparison of the in vitro fatigue resistance of an acrylic resin removable partial denture reinforced with continuous glass fibers or metal wires. J Prosthodont. 1996;5:115–121. doi: 10.1111/j.1532-849x.1996.tb00285.x. [DOI] [PubMed] [Google Scholar]
- 8.Chen S.Y., Liang W.M., Yen P.S. Reinforcement of acrylic denture base resin by incorporation of various fibers. J Biomed Mater Res. 2001;58:203–208. doi: 10.1002/1097-4636(2001)58:2<203::aid-jbm1008>3.0.co;2-g. [DOI] [PubMed] [Google Scholar]
- 9.Uzun G., Hersek N., Tincer T. Effect of five woven fiber reinforcements on the impact and transverse strength of a denture base resin. J Prosthet Dent. 1999;81:616–620. doi: 10.1016/s0022-3913(99)70218-0. [DOI] [PubMed] [Google Scholar]
- 10.Jagger D., Harrison A., Jandt K. The reinforcement of dentures. J Oral Rehabil. 1999;26:185–194. doi: 10.1046/j.1365-2842.1999.00375.x. [DOI] [PubMed] [Google Scholar]
- 11.Berrong J.M., Weed R.M., Young J.M. Fracture resistance of Kevlar-reinforced poly (methyl methacrylate) resin: a preliminary study. Int J Prosthodont. 1990;3:391–395. [PubMed] [Google Scholar]
- 12.Kolbeck C., Rosentritt M., Behr M., Lang R., Handel G. In vitro study of fracture strength and marginal adaptation of polyethylene-fibre-reinforced-composite versus glass-fibre-reinforced-composite fixed partial dentures. J Oral Rehabil. 2002;29:668–674. doi: 10.1046/j.1365-2842.2002.00870.x. [DOI] [PubMed] [Google Scholar]
- 13.Ramos V., Runyan D.A., Christensen L.C. The effect of plasma-treated polyethylene fiber on the fracture strength of polymethyl methacrylate. J Prosthet Dent. 1996;76:94–96. doi: 10.1016/s0022-3913(96)90348-0. [DOI] [PubMed] [Google Scholar]
- 14.Hirajima Y., Takahashi H., Minakuchi S. Influence of a denture strengthener on the deformation of a maxillary complete denture. Dent Mater J. 2009;28:507–512. doi: 10.4012/dmj.28.507. [DOI] [PubMed] [Google Scholar]
- 15.Solnit G.S. The effect of methyl methacrylate reinforcement with silane-treated and untreated glass fibers. J Prosthet Dent. 1991;66:310–314. doi: 10.1016/0022-3913(91)90255-u. [DOI] [PubMed] [Google Scholar]
- 16.Vallittu P.K. The effect of void space and polymerization time on transverse strength of acrylic-glass fibre composite. J Oral Rehabil. 1995;22:257–261. doi: 10.1111/j.1365-2842.1995.tb00083.x. [DOI] [PubMed] [Google Scholar]
- 17.Chen W.-C., Hung C.-C., Huang Y.-C., Wang C.-K., Wang J.-C. Fracture load of provisional fixed partial dentures with long-span fiber-reinforced acrylic resin and thermocycling. J Dent Sci. 2009;4:25–31. [Google Scholar]
- 18.Eisenburger M., Riechers J., Borchers L., Stiesch-Scholz M. Load-bearing capacity of direct four unit provisional composite bridges with fibre reinforcement. J Oral Rehabil. 2008;35:375–381. doi: 10.1111/j.1365-2842.2008.01855.x. [DOI] [PubMed] [Google Scholar]
- 19.Dyer S.R., Lassila L.V., Jokinen M., Vallittu P.K. Effect of cross-sectional design on the modulus of elasticity and toughness of fiber-reinforced composite materials. J Prosthet Dent. 2005;94:219–226. doi: 10.1016/j.prosdent.2005.06.008. [DOI] [PubMed] [Google Scholar]
- 20.Fonseca R.B., de Almeida L.N., Mendes G.A.M., Kasuya A.V.B., Favarão I.N., de Paula M.S. Effect of short glass fiber/filler particle proportion on flexural and diametral tensile strength of a novel fiber-reinforced composite. J Prosthodont Res. 2016;60:47–53. doi: 10.1016/j.jpor.2015.10.004. [DOI] [PubMed] [Google Scholar]
- 21.Keyf F., Uzun G. The effects of glass fiber reinforcement at different concentrations on the transverse strength, deflection and modulus of elasticity of a provisional fixed partial denture resin. J Biomater Appl. 2001;16:149–156. doi: 10.1106/BGNY-V5DA-VMWB-TC2W. [DOI] [PubMed] [Google Scholar]
- 22.Ootaki M., Akikazu S.-Y., Harunori G., Akiyoshi S.-Y., Nakasone Y. Optimum design for fixed partial dentures made of hybrid resin with glass fiber reinforcement by finite element analysis: effect of vertical reinforced thickness on fiber frame. Dent Mater J. 2007;26:280–289. doi: 10.4012/dmj.26.280. [DOI] [PubMed] [Google Scholar]
- 23.Bonakdarchian M., Askari N., Askari M. Effect of face form on maximal molar bite force with natural dentition. Arch Oral Biol. 2009;54:201–204. doi: 10.1016/j.archoralbio.2008.11.009. [DOI] [PubMed] [Google Scholar]
- 24.Alander P., Lassila L.V., Vallittu P.K. The span length and cross-sectional design affect values of strength. Dent Mater. 2005;21:347–353. doi: 10.1016/j.dental.2004.05.009. [DOI] [PubMed] [Google Scholar]
- 25.Pfeiffer P., Grube L. In vitro resistance of reinforced interim fixed partial dentures. J Prosthet Dent. 2003;89:170–174. doi: 10.1067/mpr.2003.29. [DOI] [PubMed] [Google Scholar]
- 26.Uzun G., Keyf F. The effect of fiber reinforcement type and water storage on strength properties of a provisional fixed partial denture resin. J Biomater Appl. 2003;17:277–286. doi: 10.1177/0885328203017004003. [DOI] [PubMed] [Google Scholar]
- 27.Miettinen V.M., Vallittu P.K. Water sorption and solubility of glass fiber-reinforced denture polymethyl methacrylate resin. J Prosthet Dent. 1997;77:531–534. doi: 10.1016/s0022-3913(97)70147-1. [DOI] [PubMed] [Google Scholar]
- 28.Kawano F., Ohguri T., Ichikawa T., Matsumoto N. Influence of thermal cycles in water on flexural strength of laboratory-processed composite resin. J Oral Rehabil. 2001;28:703–707. doi: 10.1046/j.1365-2842.2001.00724.x. [DOI] [PubMed] [Google Scholar]
- 29.Narva K.K., Lassila L.V., Vallittu P.K. Fatigue resistance and stiffness of glass fiber-reinforced urethane dimethacrylate composite. J Prosthet Dent. 2004;91:158–163. doi: 10.1016/j.prosdent.2003.10.024. [DOI] [PubMed] [Google Scholar]
- 30.Kohal R.J., Klaus G., Strub J.R. Zirconia-implant-supported all-ceramic crowns withstand long-term load: a pilot investigation. Clin Oral Implant Res. 2006;17(5):565–571. doi: 10.1111/j.1600-0501.2006.01252.x. [DOI] [PubMed] [Google Scholar]
- 31.Dyer S.R., Sorensen J.A., Lassila L.V., Vallittu P.K. Damage mechanics and load failure of fiber-reinforced composite fixed partial dentures. Dent Mater. 2005;21:1104–1110. doi: 10.1016/j.dental.2005.03.001. [DOI] [PubMed] [Google Scholar]
- 32.Narva K.K., Lassila L.V., Vallittu P.K. The static strength and modulus of fiber reinforced denture base polymer. Dent Mater. 2005;21:421–428. doi: 10.1016/j.dental.2004.07.007. [DOI] [PubMed] [Google Scholar]
- 33.Kuo W.-C., Lin Y.-S., Lin C.-L., Wang J.-C. Biomechanical investigation of long-span glass-fiber-reinforced acrylic resin provisional fixed partial denture: a finite element analysis. J Med Biol Eng. 2012;32:357–364. [Google Scholar]
- 34.Lehmann F., Eickemeyer G., Rammelsberg P. Fracture resistance of metal-free composite crowns–effects of fiber reinforcement, thermal cycling, and cementation technique. J Prosthet Dent. 2004;92:258–264. doi: 10.1016/j.prosdent.2004.05.014. [DOI] [PubMed] [Google Scholar]
- 35.Lassila L.V., Tezvergil A., Dyer S.R., Vallittu P.K. The bond strength of particulate-filler composite to differently oriented fiber-reinforced composite substrate. J Prosthodont. 2007;16:10–17. doi: 10.1111/j.1532-849X.2006.00147.x. [DOI] [PubMed] [Google Scholar]
- 36.Tanner J., Vallittu P.K., Söderling E. Effect of water storage of E-glass fiber-reinforced composite on adhesion of Streptococcus mutans. Biomaterials. 2001;22:1613–1618. doi: 10.1016/s0142-9612(00)00314-8. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.