Abstract
Introduction
Acetabulum fractures, though relatively uncommon, are associated with significant morbidity and mortality. These involve high energy trauma and due to their complex nature, the management requires understanding the relevant surgical anatomy, defining the injury via appropriate radiographic assessment and determining a suitable treatment plan. Literature is scarce for the demographic data, fracture patterns, associated injuries, management and early complications in the Indian scenario. These factors play a pivotal role in the ultimate recovery of the patients. Therefore this study was conceptualised to assess the epidemiology and evaluate the complications of these fractures. Furthermore the effects of various factors determining the quality of reduction in surgically treated patients were also assessed.
Methodology
This was a prospective observational study in which patients presenting to the advance trauma centre of our institute with acetabulum fractures were included. Demographical data of the patients, mechanisms of injuries, fractures morphologies, complications and radiological outcomes were recorded prospectively.
Results
116 patients with acetabular fractures were included in the study. 81% of these were males, with average age of 39.95 ± 15.87 years; with road traffic accidents being the predominant mode of injuries. Mortality was reported in 5 patients; 4 patients had deep venous thrombosis and sciatic nerve injuries were seen in 12 patients of which 4 were iatrogenic. 8 patients had some form of infection, out of which 4 required multiple debridements. 4 cases developed heterotrophic ossification while 2 cases had loss of reduction. The timing of surgery and other associated fractures had significant effect on the quality of reduction (p < 0.05); while age, gender, mode of injury or individual fracture patterns had no such effect.
Conclusions
Proper radiological assessment and evaluation of fracture configuration is important for management of acetabulum fractures. When indicated, this should be followed by early open reduction and internal fixation to achieve anatomical reduction, with management of associated injuries for better outcomes.
Keywords: Acetabulum fractures, Epidemiology, Indian population, Complications
1. Background
Acetabular fractures are relatively uncommon injuries constituting 0.3–6% of the total fractures seen annually.1 These are usually caused by high energy trauma, most commonly due to road traffic accidents.2 Epidemiological studies have reported a higher incidence in males and association with high - energy collisions, mainly vehicular accidents.2 There is documented evidence for coexistent lower limb fractures and head injuries as the commonest injuries.2–6
The incidence of associated injuries is a significant factor for ultimate outcome in acetabulum fractures. It has been reported that acetabular fractures associated with other injuries have a longer hospital stay, higher complication rates and re-admissions.7
Open anatomic reduction and internal fixation is the method of choice for displaced acetabulum fractures. The main indications for operative management, are fractures with hip incongruity, instability or involvement of the superior weight bearing dome. The aims of surgical management are anatomical reduction (defined as < 1 mm of residual displacement), along with hip joint congruity and stability.3 Thus, accurate reduction of intra-articular fracture fragments is critical for successful outcome, as is the maintenance of this reduction by optimal fixation. So the factors that determine the quality of reduction become even more critical for final outcomes.
Due to complex nature of these fractures, there is association of significant complications. Many factors including the patient's age, general medical condition, and associated injuries, must be considered before making definitive management decisions.2,4,5 Early surgical intervention done within the first 14 days of injury are more successful and fractures more than 14 days are considered old and associated with worse quality of reduction and outcomes.3,8
The study population in all the previous studies were Western and the relevant literature on acetabular fractures is scarce in the Indian population [Table 1]. The present study studied acetabular fractures in Indian scenario and identified the factors that determine the quality of reduction in surgically managed cases, which is crucial for better outcomes.
Table 1.
Epidemiological data and its comparison to other studies.
| Mean Age | Gender |
Mode Of Injury |
Side |
Associated Orthopaedic Injuries |
Associated Non-Orthopaedic Injuries |
Time to Surgery | Surgery Within 2 Weeks |
Duration Of Hospital Stay |
|
|---|---|---|---|---|---|---|---|---|---|
| Males (%) | RTA/Fall from height/Others (%) | Rt (%) | Dislocation/Head Femur/Pelvis/Limb | HI/BTA/BTC/Others | (%) | (Days) | |||
| Giannoudis2 | 38.6 ± 4.6 | 69.4 | 61/24/15 | NR | NR/NR/6.2/40.3 | 22/7.9/12/5.6 | 8.9 ± 2.9 | NR | NR |
| Ochs12 | 47.3 ± 20.1 | 78 | NR | NR | 32.4 overall | 17% overall | 6.3 ± 4.7 | 85.4 | NR |
| Dias4 | 39.6 ± 3.8 | 76.8 | 78/12.4/9.6 | 52 | 30/NR/8/16 | 21.7/17.4/39.1/NR | 11 | 78 | 23.6 |
| Kumar5 | 39.5 | 91 | 65/25/10 | 55.5 | 33/NR/5.5/25 | 1.3/5.5/16.6/NR | 11.7 | 80 | 26.5 |
| Our Study | 39.95 ± 15.87 | 81 | 72.4/21.6/6 | 62 | 17.5/3.3/25.8/43.3 | 15/12.5/6.7/3.3 | 8.32 | 72.8 | 15.12 |
(RTA: Road Traffic Accidents; HI: Head Injury; BTA: Blunt Trauma Abdomen; BTC: Blunt Trauma Chest; Rt: right; NR: Not Reported).
2. Materials and methods
A total of 130 patients presented with acetabulum fractures during the study period between 1 July 2015 to 30 June 2016. Of these, 5 patients were excluded as they were skeletally immature while complete data could not be collected in 9 cases. Thus the present study included 116 patients of which 4 cases had bilateral acetabular fractures. Demographic data, radiological fracture patterns, associated injuries and management, were all documented. Of the 116 patients, 70 acetabular fractures were operated by a senior surgeon at a single centre who were followed up to assess the complications and radiological outcomes as per Mata's criteria (anatomical, congruent and incongruent). The reduction was termed as anatomical when there was no fracture gap or step intra-operatively and all five anatomical lines (ilioinguinal, iliopectineal, anterior wall, posterior wall and dome) were restored post-operatively. The patients were followed up at 2 weeks, 6 weeks, 3 months, and 6 months.
3. Statistical analysis
We used SPSS software (version 20, SPSS Inc., Chicago, IL, USA). Chi-square test was used to assess the factors affecting quality of reduction. P value of less than 0.05 was considered statistically significant.
4. Results
There were 94 male patients comprising 81% of the total study group. The mean age of patients was 39.95 ± 15.87 years (18–85 years). A total of 62% of the patients were between age of 25–55 years, which is the socioeconomic productive age-group. Most common mode of injury was road traffic accidents (72.4%), followed by fall from height resulting in 21.6% of cases. 7 cases were caused by blunt trauma due to fall of object, while there was a single case who reported with bullet injury.
72 patients had fractures on the right side (62%) while 40 patients had left (34.5%) sided fractures. 4 patients reported with bilateral acetabulum fractures (3.5%). Out of the 120 acetabular fractures, 77 fractures were of elementary type while 43 were of associated type. 9 The most common type was posterior wall followed by transverse, bicolumnar, T-type and anterior column fractures. Associated anterior wall with posterior hemitransverse fractures were lowest in incidence [Table 2].
Table 2.
Types of fractures (Letournel classification). 9
| Fracture Pattern | Number of cases | |
|---|---|---|
| 1. | Posterior Wall | 34 |
| 2. | Posterior Column | 5 |
| 3. | Anterior Wall | 9 |
| 4. | Anterior Column | 13 |
| 5. | Transverse | 16 |
| 6. | Both Columns | 15 |
| 7. | Posterior wall + Transverse | 6 |
| 8. | T type | 14 |
| 9. | Anterior wall + Posterior Hemitransverse | 2 |
| 10. | Posterior Column + Wall | 6 |
| Total | 120 | |
Associated orthopaedics injuries were observed most commonly in the lower limbs, which were involved in 36 patients. Pelvic injuries were seen in 31 cases. 21 patients had an associated posterior dislocation of the hip while 4 patients had associated ipsilateral fractures of the femoral head. 16 patients had upper limb injuries. 27 of the 116 patients (23.3%) had an associated open fracture. Head injury was most common non orthopaedic injury with 18 cases, followed by blunt trauma abdomen (15 cases). 8 patients had associated blunt trauma chest.
70 patients underwent surgery, with 48 patients operated via the Kocher Langenbeck approach, 6 by the iliofemoral approach and 16 were operated by both.
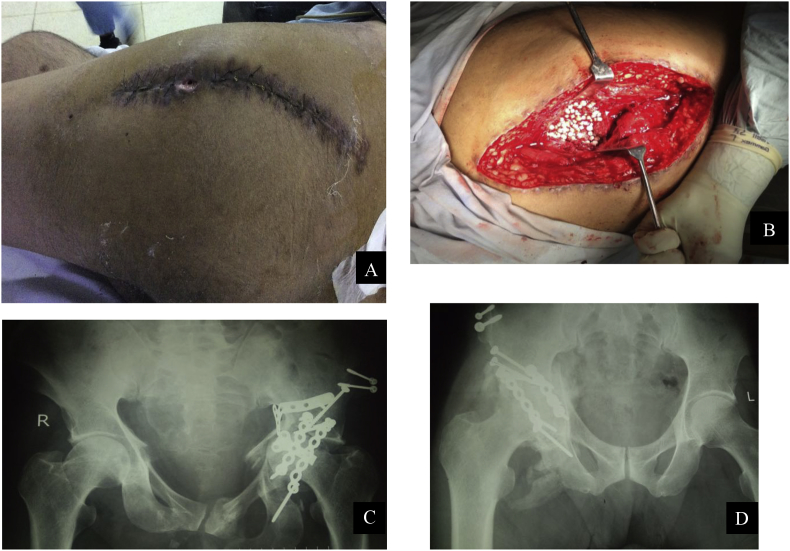
During the subsequent follow ups, the patients were evaluated for any complications associated with the fracture or the surgery. 37 patients (31.9%) reportedly had one or the other complications [Table 3] (see Fig. 1).
Table 3.
Complications observed in our study.
| Complication | Number |
|---|---|
| Sciatic Nerve Palsy (Pre Op/Post Op) | 8/4 |
| DVT/PE | 4/3 |
| Meralgia Paraesthetica | 10 |
| Infection | 8 |
| Heterotopic Ossification | 4 |
| Screw Placement Error | 1 |
| Loss Of Reduction | 2 |
| Mortality | 5 |
Fig. 1.
Images showing presence of surgical site infection (A) with use of bioabsorbable beads for the same patient (B). Image C shows loss of reduction and D shows heterotopic ossification.
Sciatic nerve palsy was seen in 8 patients at the time of injury and in 4 patients in the post-operative period. 4 patients were diagnosed with DVT on the basis of clinical picture and confirmation by compression ultrasound. Of these 3 patients had respiratory distress and were diagnosed with pulmonary embolism by CT Pulmonary Angiogram. 8 patients reported with early infection, out of whom, 4 patients improved with antibiotic course of one week as per culture/sensitivity. (Fig. 1A) Debridement and antibiotic beads were used in 2 patients). (Fig. 1B) On plain radiographs, one patient who reported with continuous anterior groin pain, was diagnosed with a broken anterior plate while there was loss of reduction in two patients. (Fig. 1C) Mortality was reported in 5 cases.
Heterotopic Ossification (HO) was reported in 4 patients in our study. (Fig. 1D) All these patients developed restriction in internal rotation. No excision was done for any of these patients.
No case of a vascular injury was reported. Complications such as AVN and osteoarthritic changes were not clearly evident as the follow up was only for 6 months and these changes are seen over a longer time period.
The average time of injury to presentation in our institute was 2.3 days. For patients being managed surgically, average time duration from injury to surgery was 8.3 days (1 - 60 days). The average duration of hospital stay was 15 days.
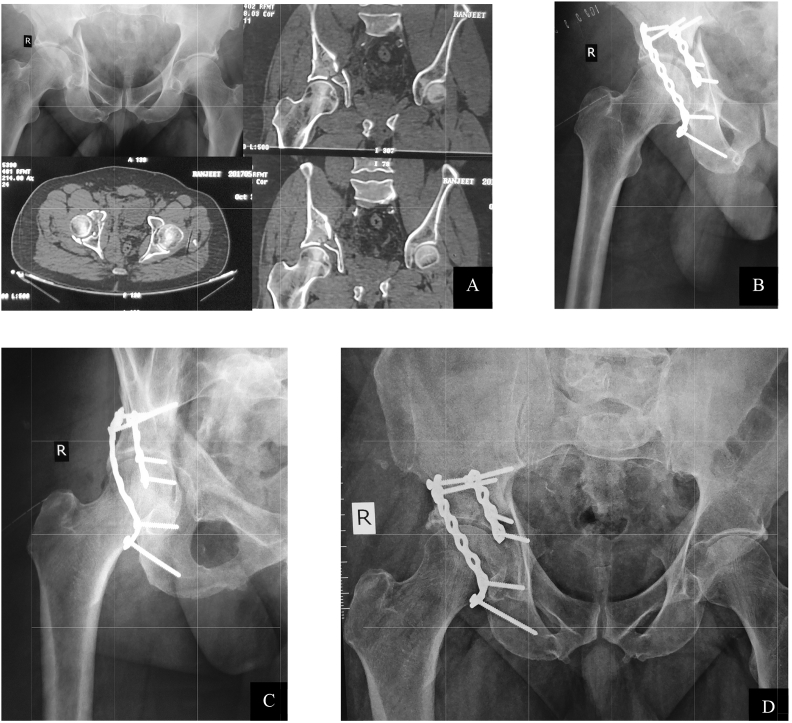
As per Mata's radiological criteria, we had 29 fractures with anatomical reduction (41.4%), 31 with congruent reduction (44.3%) and 10 with incongruent reduction (14.3%) [Table 4]. (see Fig. 2)
Table 4.
Quality of Reduction of individual fracture pattern.
| Type | Anatomical | Congruent | Incongruent | Total |
|---|---|---|---|---|
| Posterior Wall | 16 (66.67%) | 6 (25%) | 2 (8.33%) | 24 (34.2%) |
| Posterior Column | 0 (0%) | 2 (100%) | 0 (0%) | 2 (2.8%) |
| Anterior Wall | 1 (100%) | 0 (0%) | 0 (0%) | 1 (1.4%) |
| Anterior Column | 1 (33.3%) | 2 (66.7%) | 0 (0%) | 3 (4.2%) |
| Transverse | 4 (40%) | 5 (50%) | 1 (10%) | 10 (14.2%) |
| Both Column | 4 (36.3%) | 6 (54.5%) | 1 (9.2%) | 11 (15.7%) |
| Posterior Wall + Transverse | 0 (0%) | 3 (60%) | 2 (40%) | 5 (7.1%) |
| T Type | 2 (25%) | 4 (50%) | 2 (25%) | 8 (11.4%) |
| Anterior Wall + Posterior Hemitransverse | 0 (0%) | 2 (100%) | 0 (0%) | 2 (2.8%) |
| Posterior Column + Wall | 1 (25%) | 1 (25%) | 2 (25%) | 4 (5.7%) |
| Total | 29 | 31 | 10 | 70 |
Fig. 2.
61 yr male with history of RTA with fracture of the right acetabulum (A). Follow up X-rays at immediate post-op (B), 6 weeks (C) and 6 months (D) post operatively showing anatomic reduction.
Individual fracture patterns were evaluated with quality of reduction. Posterior wall fractures showed the best radiological outcome out of all the fracture patterns.
Significant factors associated with quality of reduction were timing of surgery, associated injuries and fracture patterns (elementary or associated types). No association was found with age, gender, mode of injury, or associated open injury. [Table 5]
Table 5.
Evaluation of factors affecting quality of reduction.
| Factor | Quality Of Reduction |
Total | P Value | |||
|---|---|---|---|---|---|---|
| Anatomical | Congruent | Incongruent | ||||
| Age | <55 yrs | 26 | 25 | 8 | 59 | 0.58 |
| >55 yrs | 3 | 6 | 2 | 11 | ||
| Gender | Male | 23 | 26 | 9 | 58 | 0.726 |
| Female | 6 | 5 | 1 | 12 | ||
| Timing Of Surgery | <2 weeks | 25 | 22 | 4 | 51 | 0.017 |
| >2 weeks | 4 | 9 | 6 | 19 | ||
| Associated Injury | Yes | 13 | 11 | 8 | 32 | 0.048 |
| No | 16 | 20 | 2 | 38 | ||
| Fracture Pattern | Elementary | 22 | 14 | 4 | 40 | 0.002 |
| Associated | 7 | 17 | 6 | 30 | ||
| Mode Of Injury | RTA | 19 | 27 | 7 | 53 | 0.13 |
| Others | 10 | 4 | 3 | 17 | ||
| Associated Open Injury | Yes | 3 | 6 | 3 | 12 | 0.33 |
| No | 26 | 25 | 7 | 58 | ||
5. Discussion
The incidence of acetabulum fractures is on the lower side, but being associated with high energy trauma with coexistent injuries, they result in high rates of morbidity and mortality. Therefore, the focus on these fractures has increased significantly over the past few decades. The present study reports an incidence of 4.7% which is similar to 0.3–6% fractures reported in literature in the Western population.1
These fractures are commonly seen in males, compared to the females. The most common mode of injury is vehicular accidents and the younger economically active population are affected the most.2,3 The conventional role of males being the working force in our society and non urban females being home makers, requires the former to travel far and wide, hence it could be a cause of them meeting more accidents.10 The increasing number of accidents could be due to increased number of vehicles and the poor conditions of roads. Also the practice of not wearing seat belts and lack of proper road sense prevails in our part of the world that could also be one of the reasons.11
Associated injuries have also been well documented, with various studies reporting lower limb fractures and head injuries as the commonest.2,4 Hip dislocations were seen in 21 of our patients which is similar to Giannoudis et al.2 Hip dislocation affects the eventual outcome by compromising vascularity of the femoral head and makes surgical reconstruction of the acetabulum more challenging.12 We found a high incidence of associated pelvic injuries with acetabular fractures. This can be attributed to the high energy of trauma in these injuries.
Though the patients in our study presented on an average of more than 2 days after injury, we operated them early, within 10 days in most of the cases. This allowed better reduction and outcome. Delay of more than 2 weeks tends to decrease the quality of reduction and could hamper the ultimate outcome and also could lead to early avascular necrosis.3
Sciatic nerve palsy is the most common nerve injury that occurs with acetabulum fractures. Pre-operative sciatic nerve injuries occur more commonly with hip dislocations with posterior wall fractures. Iatrogenic injuries occur mainly due to improper retractor placement or excessive traction during reduction. The rates of sciatic nerve palsies was comparable to that of other studies. [Table 6] Recovery of the nerve is more commonly seen with iatrogenic injuries which in majority of cases is due to stretching of the nerve. Only 1 patient with pre-operative injury showed signs of recovery, showing that traumatic nerve injuries are more commonly contusions. HO was seen in only 4 of our patients, who had Brooker type 1 or 2 ossification.13 None of them needed excision and the routine prophylaxis with Indomethacin which we give, could be the reason for this low incidence.
Table 6.
Comparison of complications to various studies in literature.
| Complications | Cases (No.) | Mortality (%) | DVT (%) | PE (%) | Sciatic Nerve Palsy (%) | Infection (%) | Failure Of Fixation (%) |
|---|---|---|---|---|---|---|---|
| Letournel and Judet9 | 569 | 2.3 | 3 | 2.1 | 12/6 | 4.2 | 1 |
| Matta3 | 259 | NR | NR | NR | 12 | 5 | 3 |
| Mears17 | 100 | 1 | 5 | 1 | 16/3 | 4 | 1 |
| Routt18 | 108 | NR | NR | 3 | 5 | 3 | NR |
| Helfet19 | 84 | 0 | 6 | 4 | 31/6 | 0 | 2 |
| Giannoudis2 | 3 | 4.3 | NR | 16.4/8 | 4.4 | NR | |
| Kumar6 | 72 | 0 | 0 | 0 | 1.4% | 4.1 | 1.4 |
| Gupta et al.5 | 63 | 0 | NR | NR | 3.1 | 7.93 | 1.5 |
| Our Study | 120 | 4.1 | 3.3 | 2.5 | 6.6/5.7 | 6.6 | 1 |
(DVT: Deep Vein Thrombosis; PE: Pulmonary Embolism).
Poorer results were seen in posterior wall + posterior column, T type and posterior wall + transverse patterns. This is similar to previous studies.14, 15, 16 These patterns are often associated with communition,cartilage damage, impaction and difficult reduction, which could be the reason for worse outcomes. The rate of infection in our study was slightly higher as compared to other studies [Table 6].2,3,5,6,9,17,18,19 4 patients who had deep infections had an associated open fracture. The relatively higher rate of infection in our study can thus be related to delay in surgery and associated open fracture. 2 of these patients had been operated via usage of indigenous implant, which could have been a confounding factor.
The quality of reduction was assessed as per Matta's radiological principle for reduction assessment: anatomical, congruent or incongruent. The quality of reduction according to the Matta's criteria, was comparable to a few studies in literature, while others showed varied differences. [Table 7].14, 20, 21, 22 This can be attributed to the varied number of cases in different studies and the complex pattern of injuries presenting to the hospital. Our hospital is a major tertiary care centre and receives a high number of complex injuries with associated injuries, which may result in lower rate of anatomical reductions.
Table 7.
Comparison of quality of reduction to various studies.
The quality of reduction was compared between fractures operated within and after 2 weeks and it was seen that fractures operated after 2 weeks had poorer outcome as compared to the former. This is comparable to other studies like Matta et al. who considered fractures more than 2 weeks as old and associated with compromised quality of reduction.2, 4
Since our study was done with short term follow up of 6 months, we assessed short term complications and radiology. The functional outcomes correlate well with radiographical outcomes. Thus it is expected that majority of the patients will have excellent to good results in the long term period with maintenance of optimal reduction. However, factors beyond the surgeons control, including muscle injury, associated cartilage damage or surgical morbidity could be detrimental.
The present study gives a clear idea about the demographic factors of acetabular fractures in North India and compares it to the western scenario. An important limitation of this study is that ours being a tertiary care centre, may not have had all the referrals from nearby areas, which could have affected the actual rate of prevalence. Another limitation is the non assessment of long term complications such as AVN and osteoarthritis which may lead to poor functional outcome and subsequent joint sacrificing surgeries. But the incidence is well documented and gives a good idea about the different aspects of acetabulum fractures and their complications in the Indian scenario.
6. Conclusion
Acetabulum fractures in Indian population are common in the economically productive males, most commonly due to road traffic accidents. Fractures of the posterior wall are most common, while associated injuries of the lower extremities, pelvis and head are common, and are associated with a longer hospital stay and influence the quality of reduction and thus the overall outcome. It is important that acetabulum fractures are referred to a dedicated centre at the earliest so that proper evaluation with radiology can be undertaken to understand the fracture pattern. Open reduction and internal fixation should be done as early as possible, with the aim of anatomical reduction in cases requiring surgery which depends on timing of surgery and fracture patterns. This results in satisfactory outcomes and lower complication rates.
Conflicts of interest
None.
Source of funding
Nil.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.jcot.2019.02.012.
Contributor Information
Karan Jindal, Email: karan.121@hotmail.com.
Sameer Aggarwal, Email: drsameer35@yahoo.co.in.
Prasoon Kumar, Email: drprasoonksingh@gmail.com.
Vishal Kumar, Email: drkumarvishal@gmail.com.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- 1.Gänsslen A., Pohlemann T., Paul C., Lobenhoffer P., Tscherne H. Epidemiology of pelvic ring injuries. Injury. 1996;27(Suppl. 1):S13–S20. [PubMed] [Google Scholar]
- 2.Giannoudis P.V., Grotz M.R.W., Papakostidis C., Dinopoulos H. Operative treatment of displaced acetabular fractures of the acetabulum: a meta-analysis. J Bone Joint Surg Br. 2005;87:2–9. [PubMed] [Google Scholar]
- 3.Matta J.M. Fractures of the acetabulum: accuracy of reduction and clinical results in patients managed operatively within three weeks after the injury. J Bone Joint Surg Am. 1996;78A:1632–1645. [PubMed] [Google Scholar]
- 4.Dias M., Goldsztajn F., Guimaraes J. Epidemiology of acetabulum fractures treated at the instituto nacional de traumatologia e ortopedia. Rev Bras Ortop. 2010 Sep-Oct;45(5):474–477. doi: 10.1016/S2255-4971(15)30438-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gupta R.K., Singh H., Dev B. Results of operative treatment of acetabular fractures from the Third World – how local factors affect the outcome. Int Orthop. 2009 Apr;33(2):347–352. doi: 10.1007/s00264-007-0461-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kumar A., Shah N.A., Kershaw S.A., Clayson A.D. Operative management of acetabular fractures: a review of 73 fractures. Injury. 2005;36(5):605–612. doi: 10.1016/j.injury.2004.11.022. [DOI] [PubMed] [Google Scholar]
- 7.Phruetthiphat O.A., Willey M., Karam M.D. Comparison of outcomes and complications of isolated acetabular fractures and acetabular fractures with associated non-acetabular injuries. J Orthop Trauma. 2016 Oct 5 doi: 10.1097/BOT.0000000000000720. [DOI] [PubMed] [Google Scholar]
- 8.VanOpdorp H., Lunen B.V., Swanson J. Fracture of the superomedial weight-bearing surface of the acetabulum in a division I field-hockey player: a case study. J Sport Rehabil. 2004;13(4):343–352. [Google Scholar]
- 9.Judet R., Judet J., Letournel E. Fractures of the acetabulum: classification and surgical approaches for open reduction. J Bone Joint Surg. 1964;46A:1615–1638. [PubMed] [Google Scholar]
- 10.Kumar P., Sen R.K., Aggarwal S., Jindal K. Common hip conditions requiring primary total hip arthroplasty and comparison of their postoperative functional outcomes, J Clin Orthopaed Trauma, 10.1016/j.jcot.2019.02.009. [DOI] [PMC free article] [PubMed]
- 11.Dakin G.J., Eberhardt A.W., Alonso J.E., Stannard J.P., Mann K.A. Acetabular fracture patterns: association with motor vehicle crash information. J Trauma. 1999:1063–1071. doi: 10.1097/00005373-199912000-00012. [DOI] [PubMed] [Google Scholar]
- 12.Ochs B.G., Marintschev I., Hoyer H. Changes in the treatment of acetabular fractures over 15 years: analysis of 1266 cases treated by the German pelvic multicentre study group (DAO/DGU) Injury. 2010;41:839–851. doi: 10.1016/j.injury.2010.04.010. [DOI] [PubMed] [Google Scholar]
- 13.Firoozabadi R., O'Mara T.J., Swenson A., Agel J., Beck J.D., Routt M. Risk factors for the development of heterotopic ossification after acetabular fracture fixation. Clin Orthop Relat Res. 2014;472(11):3383–3388. doi: 10.1007/s11999-014-3719-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Matta J., Mehne D., Raffi R. Fractures of the acetabulum: early results of a prospective study. Clin Orthop Relat Res. 1986;205:241–250. [PubMed] [Google Scholar]
- 15.Moed B.R., Yu P.H., Gruson K.I. Functional outcomes of acetabular fractures. J Bone Joint Surg Am. 2003;85-A:1879–1883. doi: 10.2106/00004623-200310000-00002. [DOI] [PubMed] [Google Scholar]
- 16.Murphy D., Kaliszer M., Rice J., McElwain J.P. Outcome after acetabular fracture: prognostic factors and their inter-relationships. Injury. 2003;34:512–517. doi: 10.1016/s0020-1383(02)00349-2. [DOI] [PubMed] [Google Scholar]
- 17.Mears D.C., Rubash H. Pelvic and acetabular fractures. J Bone Joint Surg. 1986;7:78–83. [Google Scholar]
- 18.Routt M.L.C., Jr., Swiontkowski M.F. Operative treatment of complex acetabular fractures: combined anterior and posterior exposures during the same procedure. J Bone Joint Surg. 1990;72-A:897–904. [PubMed] [Google Scholar]
- 19.Helfet D.L., Schmeling G.J. Management of acute, displaced acetabular fractures using indirect reduction techniques and limited approaches. Orthop Trans. 1991;15:833–834. [Google Scholar]
- 20.Stockle U., Hoffmann R., Sudkamp N., Reindl R., Haas N. Treatment of complex acetabular fractures through a modified extended iliofemoral approach. J Orthop Trauma. 2002 Apr;16(4):220–230. doi: 10.1097/00005131-200204000-00002. [DOI] [PubMed] [Google Scholar]
- 21.Hussain K., Kancheria N., Kanugula S., Patnala C. Analysis of displaced acetabular fracture in adults treated with open reduction and internal fixation. Int J Res Orthop. 2016 Sep;2(3):99–103. [Google Scholar]
- 22.Khadrawe T., Hammad A., Hassaan A. Indicators of outcome after internal fixation of complex acetabular fractures. Alexandria J Med. 2012 June;48(2):99–107. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.