Abstract
Background
Proper patellar tracking is one of the most important aspect of TKA to ensure good functional outcome. A patellar tracking problem noted intraoperatively serves as a warning sign and should prompt the surgeon to reassess position of each component. Various tests are there to assess lateral retinaculum tightness viz. "No thumb test", "Towel clip test". A new test "Vertical patella test" is described to assess lateral retinaculum tightness. A study was conducted to assess the effectiveness, correlation and validity of two techniques.
Materials & Methods
Patients >50 years of age and with diagnosis of Osteoarthritis knee having less than 30 varus and flexion deformity going in for primary TKA were selected with a sample size of 100 knees in a tertiary care centre. Revision cases or patients with flexion contracture more than 30, complex knee surgery; with pre existing patellar tilt were excluded from study.
Results
Results of both tests were found to correlate in 75% of case with sensitivity of 96.65% and specificity of 75.00%. Kappa came out to be 0.634 which shows good agreement of vertical patella test and towel clip test. Result was computed using excel and SPSS and was found to be significant with p value< 0.05. Lateral retinaculum release was done in 8 knees.
Conclusions
Vertical patella test correlates with towel clip test, is easy to perform and saves time. The limitation of our study was small sample size.
Keywords: Total knee arthroplasty, Patellar tracking, Vertical patella test, Towel clip test
1. Introduction
Proper patella tracking is one of the most important aspect of Total Knee Arthroplasty to ensure good functional outcome.
Patellar maltracking can result in increase pressure on the prosthesis which in turn leads to excessive wear of patellar components and patellar tilt or dislocation. Intraoperative assessment of patellar tracking is therefore of critical importance. A patellar-tracking problem noted intraoperatively serves as a warning sign 1,2 and should prompt the surgeon to reassess position of each component. When the components of the arthroplasty are well placed and a tendency for tilt or subluxation of the patella still persists, then it implies that lateral retinaculum is tight and it requires release of lateral retinaculum to improve patellofemoral tracking. Many tests have been described in literature to assess lateral retinaculum tightness by assessing the tracking of patella in Total knee arthroplasty (TKA) viz: “No thumb test”, “Towel clip test” etc. Recently, another test has been described “Vertical patella test” by Nitin Goyal et al 3 which is very simple, less time consuming.
It would be of great importance to know whether any positive correlation exists between “Towel clip test” and “Vertical patella test” to assess lateral retinaculum tightness.
Therefore, a prospective study was done to study the effectiveness, correlation and validity of these two techniques for assessing lateral retinaculum tightness.
2. Subjects and methods
A prospective comparative study was carried out in a tertiary care hospital in New Delhi from Oct.2015– March 2017 after clearance from ethical committee with sample size of 100 knees. All patients >50 years with OA knee having less than 30° varus and flexion deformity going in for primary TKA were included in this study. Patients with flexion contracture more than 30°; previous complex knee surgery; retained metal hardware at the hip and Knee; ankylosis of ipsilateral hip, knee or ankle were excluded from this study.
2.1. Operative techniques
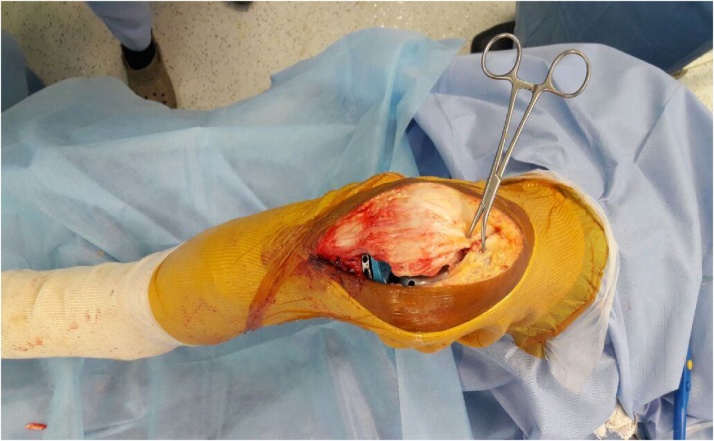
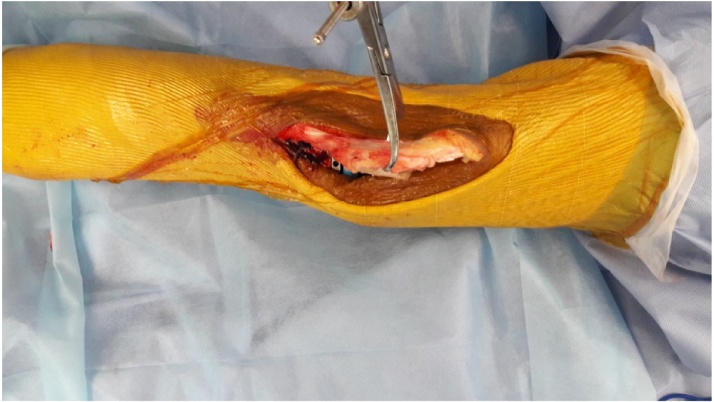
Standard operating techniques for TKR were used. Patellar tracking was checked by “Towel clip” and “Vertical Patella Test” to assess lateral retinaculum tightness. The “Towel clip test” is done by re-approximating the vastus medialis and medial retinaculum to the medial border of the patella using a towel clip or a stitch.4 The knee is again taken through a range of motion. Any elevation of the medial edge of the patella is considered a positive test. Fig. 1. For “Vertical patella test” the patella is initially everted to 90° in relation to the femoral component. It is then translated medially so that its lateral border is past the middle of the intercondylar groove of the femoral component while still in the everted position. The inability to translate it past the midpoint of the intercondylar groove of the femoral component while everted constitutes a positive test suggesting tight lateral retinaculum (Fig. 2).3
Fig. 1.
Towel clip test.
Fig. 2.
Vertical patella test - superior view.
In case of discrepancy between the two tests, decision to do lateral retinaculum releases was based on towel clip test which is the most acceptable test as of now and not on Vertical Patella Test, so there was no conflict.
3. Results
The majority of the patients in whom TKR was done belonged to age group of 61–65 years. The youngest patient for whom TKR was done was 51 years of age and the oldest patient was 75 years. Mean age at the time of surgery was 62.3 years. There was female predominance in this group accounting for 62% of the patients.
Even though our study was to assess intraoperative lateral retinaculum tightness, we routinely followed up patients at 2 weeks, 1month, 3 months, 6 months and then annually after surgery. Maximum duration of follow up was 21 months, and minimum was 6 months. Mean period of follow up was 1 year. Sensitivity of the test is 95.65% and specificity is 75% (Table 1).
Table 1.
Cross table of towel clip test and vertical patella test.
| TOWEL CLIP |
Total | P value | Kappa | |||
|---|---|---|---|---|---|---|
| NORMAL | ABNORMAL | |||||
| VPT | Normal | 88 (88.00 %) |
2 (2.00%) |
90 (90.00%) |
0.007 | 0.634 |
| Abnormal | 4 (4.00%) |
6 (6.00%) |
10 (10.00%) |
|||
| Total | 92 (92.00%) |
8 (8.00%) |
100 (100.00%) |
|||
P value of VPT IS 0.007 and this result is statistically significant. Kappa which is strength of agreement is 0.634.In our study, significant good agreement was seen between VPT with Towel Clip Test.
Out of 8 Positive towel clip test, Vertical patella test was positive in 6 cases. Therefore, there is 75% correlation of results of Vertical patella test with Towel clip test.
In our study Lateral retinacular release rate was 8% and this was done on the basis of “towel clip test” which is the most accepted test in literature to assess the lateral retinaculum tightness.
4. Discussion
Proper patellar tracking is crucial for a total knee arthroplasty to function well.5 Proper patellar tracking is attributable to a combination of static and dynamic factors. Among the former are the position of the patellar implant on the bone, the position and alignment of the femoral component, the configuration of the prosthetic trochlear groove, and most importantly, the soft tissue balance. The dynamic factors include the direction and magnitude of the quadriceps action.6 Abnormal patellar tracking can lead to diminished range of motion, anterior knee pain, and abnormal implant wear.5 Optimizing patellar tracking in total knee arthroplasty is a surgical priority.7 Traditional teaching has emphasized the need for importance of doing a lateral retinacular release in a maltracking patella in a well positioned implant. The mechanical success of a total knee replacement demands stable patellar tracking without subluxation.8
However, lateral retinacular release have been shown to include diminished blood supply to the patella 9,10 compromised wound healing11 and symptomatic subluxation of the soft tissue defect over the femoral component.12 The additional dissection and retinacular incision can result in increased blood loss and lead to wound healing complications.11 With these potential complications, the identification of appropriate indications for this procedure is critical. Therefore, we need a good test to identify lateral retinaculum tightness during surgery. Various tests have been described in literature to assess lateral retinaculum tightness viz. “No thumb test”, “Towel clip test”13 etc. Till now, towel clip test is considered as the most acceptable. Recently a novel technique has been described in literature by Nitin Goyal et al 3 to assess lateral retinaculum tightness i.e. “Vertical patella test”.
4.1. Lateral retinaculum release rate
Patellar maltracking14 in TKA can cause a range of postoperative problems such as chronic pain, restricted ROM, and can hamper ambulation with frank dislocation. The incidence of patellar-related issues complicating knee arthroplasty varies between 4% and 10%. Patellar maltracking can be dealt with in several ways at surgery. Lateral release of the tight lateral retinaculum is one well-described option in the literature and has been reported as being performed in 3.8%–45% of patients. Lateral release of a tight lateral retinaculum is performed to correct patellar maltracking.
Lateral retinacular release of the patella is a useful resource for knee surgeries and may be performed in disorders of the extensor apparatus, whether or not associated with other procedures.15 The theoretic basis of this technique is the imbalance of the extension mechanism caused by excessive tension of the lateral retinaculum, which contributes to patellofemoral disorders, such as anterior knee pain, acute or chronic instability, patellar chondropathy, and patellofemoral osteoarthrosis (OA).
Intraoperative lateral retinacular release performed during primary total knee arthroplasty (TKA) can improve patellar tracking. A study by Kusuma et al 16 compares the outcomes of patients who did and did not have lateral retinacular release during primary TKA. One thousand one hundred eight consecutive primary TKAs were reviewed. Lateral release was performed on 314 patients; 794 patients did not undergo release. Comparisons of range of motion, Knee Society Score, and postoperative complications were made between the 2 groups. At an average follow-up of 4.7 years, no statistically significant difference in range of motion, Knee Society Score, or postoperative complications of patella fracture, subluxation, postoperative manipulation, or wound complications was demonstrated.
Optimal patellar tracking and component alignment are important in achieving a well-functioning total knee arthroplasty.17 The patella is constrained partly by design of the prosthetic trochlear groove, and patellar tracking is governed by a combination of static and dynamic factors. Maltracking may result from excessive or unbalanced tension in the surrounding soft tissues.
Indications for lateral retinaculum release are patellar maltracking, patellofemoral instability, patellofemoral subluxation and retinacular tightness and pain. Archibeck and colleagues4 in 2003 compared the rule of “no thumb test” with the “towel clip test” in determining the need for lateral retinacular release in 200 consecutive primary TKR. The “towel clip test” was positive in 13 knees (6.5%) and “no thumb test “was positive in 78 knees (39%). He concluded that the “no thumb test” had a high rate of false positives which over predicts the need for retinacular release. They advocated the” towel clip test” to determine the need for lateral retinacular release. They reported a lateral retinaculum release rate of 6.5%.
Richard W. Westerman et al 18 in April 2015 conducted a study to assess intraoperative PFJ kinematics using both “no thumb technique” and “towel clip test” and found “towel clip test” created a significant medialization of patella by a mean of 5.5 mm when compared with the traditional” no thumb technique”. Towel clip test markedly improves patellar tracking generating a mean medialization of 15%.
In a study conducted by Richard S. Laskin6, lateral release rate was 6% using towel clip test in 178 patients undergoing TKR. Fetto et al 19 in a study where they did soft tissue balancing procedure during TKR found lateral retinaculum release rate to be 5.5%. Fithian and co-workers 20conducted a scientific study amongst experience knee surgeons and reports a 2% rate of lateral retinacular release. Kusuma and associates16 reported a 28% lateral retinacular rate on 1108 TKA. Ritter et al 21 in a study found lateral retinaculum release rate to be 3.7%. Thus Lateral release rate varies from a low of1.4% to a high of 28%.
In our study, Lateral retinaculum release rate (LRRR) was 8%. This is little on higher side but could be due to low sample size (Table 2).
Table 2.
Lateral retinaculum release rates in various studies.
| AUTHOR | NUMBER OF PATINETS | LRRR (%) |
|---|---|---|
| Archibeck | 200 | 6.5 |
| Kusuma et al | 1108 | 28 |
| Ritter et al | 1146 | 3.7 |
| Fithian et al | – | 2 |
| Fetto | 100 | 5.5 |
| Richard S. Laskin | 178 | 6 |
| Yoon | 365 | 1.4 |
| Our study | 100 | 8 |
4.2. Correlation of vertical patella test with towel clip test
Nitin Goyal et al 3 conducted an index study and described “Vertical patella test” as a novel technique to assess the adequacy of patellar tracking during TKA. They did a study on 820 consecutive primary TKAs using posterior cruciate substituting total knee prosthesis. In these operations, a” towel clip test “was used in conjunction with the “vertical patella test “to assess the patellar tracking. In nearly all cases where the “towel clip test” demonstrated tilting of the patellar edge or subluxation (i.e., a positive test or abnormal), the “vertical patella test “also was positive. In the 21 cases with a positive “towel clip test,” the “vertical patella test “was positive in 86% (18 of 21), indicating a high correlation. They concluded that “Vertical patella test”, is a novel technique to assess the lateral retinaculum tightness which should be used in addition to the currently used “no thumb” and “towel clip” tests. They felt that the VPT may be more specific to lateral retinacular tightness. According to their method may also aid in the diagnosis and correction of patellar maltracking during revision TKA in situations when the exact cause of the patellar subluxation is often unclear. They have also felt the need for further prospective comparative studies to validate this technique.
We have done a similar study on 100 knees using Posterior Stabilized knees. In our study, towel clip test revealed 8 knees in which patella tilted or subluxated laterally whereas in vertical patella test 10 knees tilted or subluxated laterally. Using towel clip test as the most acceptable test, only in 8 cases lateral retinaculum release was done using an “inside out” technique.
We found there is good correlation of results of “Vertical patella test “with “Towel clip test “and both the tests can be used intraoperatively.
We have gone a step further by doing a detailed statistical analysis to validate these two techniques.
As lateral retinaculum release has sometimes serious repercussions, the patient should be selected carefully. This selection becomes easier for the operating surgeon if both the tests are employed, as VPT validates the results of Towel clip test and gives more confidence to surgeon about patellar tracking.
5. Conclusion
We conclude that results of Vertical patella test correlates with towel clip test. However, a large cohort of patients is required to conclusively prove or disprove efficacy of “vertical patella test” in relation to Towel clip test.
Contributor Information
Anjul Verma, Email: vermaanjul08@gmail.com.
Rajesh Lalchandani, Email: rlchandani@yahoo.com.
References
- 1.Pagnano M.W., Kelly M.A. The intraoperative assessment of patellar tracking. In: Scuderi G.R., Tria J.A., editors. Surgical techniques in total knee arthroplasty. Springer; New York: 2002. pp. 317–325. [Google Scholar]
- 2.Johnson D., Eastwood D. Lateral patellar release in knee arthroplasty: effect on wound healing. J Arthroplasty. 1992;7:427–431. doi: 10.1016/s0883-5403(07)80035-0. [DOI] [PubMed] [Google Scholar]
- 3.Goyal N., Matar W.Y., Parvizi J. Assessing patellar tracking during total knee arthroplasty:a technical note. Am J Orthop. 2012;41(10):450–451. [PubMed] [Google Scholar]
- 4.Archibeck M., Camarata D., Trauger J., Allman J., White R. Indications for lateral retinacular release in total knee replacement. Clin Orthop Relat Res. 2003;414:157–161. doi: 10.1097/01.blo.0000079260.91782.96. [DOI] [PubMed] [Google Scholar]
- 5.Grace J.N., Rand J.A. Patellar instability after total knee arthroplasty. Clin Orthop Relat Res. 1988;237(7):184–189. [PubMed] [Google Scholar]
- 6.Laskin R. Lateral release rates after total knee arthroplasty. Clin Orthop Relat Res. 2001;392(November):88–93. doi: 10.1097/00003086-200111000-00011. [DOI] [PubMed] [Google Scholar]
- 7.Clinical Biomechanics Clin Biomech (Bristol, Avon) 2008;23(August (7)):900–910. doi: 10.1016/j.clinbiomech.2008.04.001. Epub 2008 Jun 5. [DOI] [PubMed] [Google Scholar]
- 8.Miller M.C., Zhang A.X., Petrella A.J., Berger R.A., Rubash H.E. The effect of component placement on knee kinetics after arthroplasty with an unconstrained prosthesis. J Orthop Res. 2001;19:614–620. doi: 10.1016/S0736-0266(00)00043-7. [DOI] [PubMed] [Google Scholar]
- 9.Mcmahon M.S., Scuderi G.R., Glashow J.L. Scintigraphic determination of patellar viability after excision of infrapatellar fat pad and/or lateral retinacular release in total knee arthroplasty. Clin Orthop Rel Res. 1990;(260):10–16. [PubMed] [Google Scholar]
- 10.Ritter M.A., Keating E.M., Faris P.M. Clinical, roentgenographic, and scintigraphic results after interruption of the superior lateral genicular artery during total knee arthroplasty. Clin Orthop Rel Res. 1989;(248):145–151. [PubMed] [Google Scholar]
- 11.Johnson D.P., Eastwood D.M. Lateral patellar release in knee arthroplasty effect on wound healing. J Arthroplasty. 1992;7:427–431. doi: 10.1016/s0883-5403(07)80035-0. [DOI] [PubMed] [Google Scholar]
- 12.Engh G.A., Holt B.T., Parks N.L. A midvastus muscle-splitting approach for total knee arthroplasty. J Arthroplasty. 1997;12(3):322–331. doi: 10.1016/s0883-5403(97)90030-9. [DOI] [PubMed] [Google Scholar]
- 13.Rae P., Noble J., Hodgkinson J. Patellar resurfacing in total condylar knee arthroplasty. The Journal Arthroplasty. 1990;5(3):259–265. doi: 10.1016/s0883-5403(08)80081-2. [DOI] [PubMed] [Google Scholar]
- 14.Maniar R.N., Singhi T., Rathi S.S., Baviskar J.V., Nayak R.M. Surgical technique: lateral retinaculum release in knee arthroplasty using a stepwise, outside-in technique. Clin Orthop Relat Res. 2012;470(10):2854–2863. doi: 10.1007/s11999-012-2420-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.da Fonseca L.P.R.M., Kawatake E.H., de Pochini A.C. Lateral patellar retinacular release: changes over the last ten years. Revista Brasileira De Ortopedia. 2017;52(4):442–449. doi: 10.1016/j.rboe.2017.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kusuma S.K., Puri N., Lotke P.A. Lateral retinacular release during primary total knee arthroplasty. J Arthroplasty. 2009;24(April (3)):383–390. doi: 10.1016/j.arth.2007.11.004. [DOI] [PubMed] [Google Scholar]
- 17.Strachan R., Merican A., Devadasan B., Maheshwari R., Amis A. A technique of staged lateral release to correct patellar tracking in total knee arthroplasty. J Arthroplasty. 2009;24(5):735–742. doi: 10.1016/j.arth.2008.02.005. [DOI] [PubMed] [Google Scholar]
- 18.Bhangoo N., James P., Westerman R. When and How Is Patella Tracking Best Assessed in Total Knee Arthroplasty Surgery? Journal of Knee Surgery. 2015;29(04):337–340. doi: 10.1055/s-0035-1554924. [DOI] [PubMed] [Google Scholar]
- 19.Fetto J.F., Hadley S., Leffers K.J., Leslie C.J., Schwarzkopf R. Electronic measurement of soft-tissue balancing reduces lateral releases in total knee arthroplasty. Bull NYU Hosp Jt Dis. 2011;69(4):285–288. [PubMed] [Google Scholar]
- 20.Fithian D.C., Paxton E.W., Post W.R., Panni A.S. Lateral retincular release: a survey of the International patellofemoral study group. Arthroscopy. 2004;20(May (5)):463–468. doi: 10.1016/j.arthro.2004.03.002. [DOI] [PubMed] [Google Scholar]
- 21.Ritter M.A., Pierce M.J., Zhou H. Patellar complications(total knee arthroplasty). Effect of lateral release and thickness. Clin Orthop Relat Res. 1999;367(October):149–157. [PubMed] [Google Scholar]