Dear Editor,
I am Dr. Sabiha Gungor Kobat, from the Department of Ophthalmology, Elazig Health Sciences University, Elazig, Turkey. I am writing to present an exceedingly rare case of two siblings, one of whom developed Bietti crystalline dystrophy (BCD) with choroidal neovascularization at the age of 13 years, and the other has asymptomatic BCD at 8 years old.
BCD, which was first described by Bietti[1] in 1937, is characterized by yellow-white deposits localized in the paralimbal cornea, and superficial and deeper retinal layers[2]–[3]. Inheritance is usually expressed as autosomal recessive but it can be found in autosomal dominant cases[4]. As this slowly progressing disease advances, atrophy, choroid sclerosis, and pigmental changes occur in the retinal pigment epithelium (RPE). These result in a decrease in visual acuity, night blindness, narrowing of the visual field, and central scotomas[2]–[3]. The development of choroidal neovascularization in BCD is quite rare[5]–[12]. The disease usually appears in the third decade of life, although cases have been reported in the first or second decades[2],[13]. The aim of this paper is to present an exceedingly rare case of two siblings, one of whom developed BCD with choridal neovascularization at 13 years old, while the other has asymptomatic BCD at 8 years old.
The report is in accordance with the Declaration of Helsinki Ethical Principles. The patient has given her consent for her images and related clinical information to be reported in this journal.
Case 1
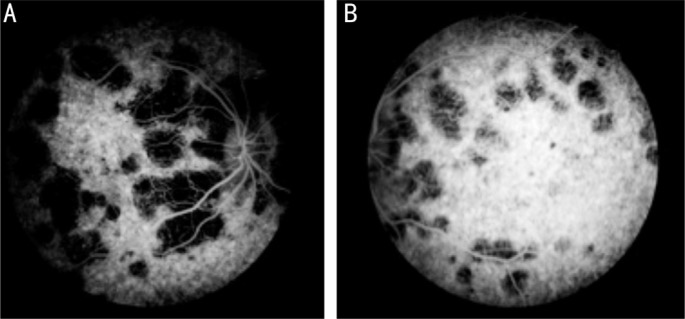
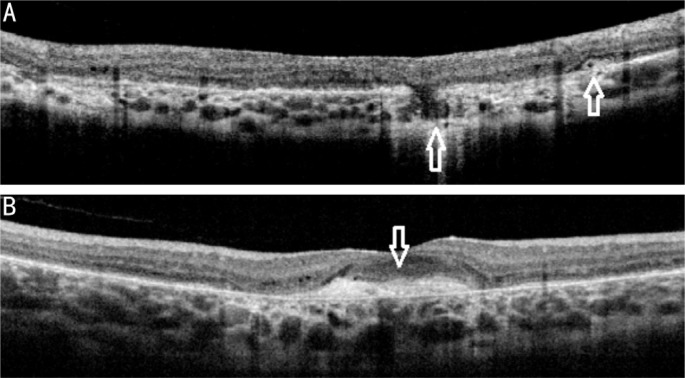
A 13-year-old girl was admitted to our outpatient clinic with complaints of visual impairment which had been ongoing for the last two years. Visual acuity was 0.4 (-3.00 D myopic correction) in the right eye and 0.05 in the left eye. There was no pathological finding in the anterior segment examination. Intaocular pressure was normal. Numerous white-yellow deposits, chorioretinal atrophic areas and pigment clusters in the bilateral retinal posterior poles were detected during examination (Figure 1). A foveal scar was determined in the left eye (Figure 1B). The fundus image suggested BCD, and so the cornea was re-examined but no corneal constriction was observed. Colored fundus photographs and fundus fluorescein angiography (FFA) were taken. FFA showed common chorioretinal atrophy in both eyes, and scar formation without leakage in the left eye (Figure 2). Optic coherence tomography (OCT) images showed high reflective crystalline deposits in the sensorineural retina and RPE, together with irregularity and increased reflectivity in RPE (Figure 3). Subretinal scarring possibly due to old choroidal neovascularization was observed in the juxta foveal area in the left eye (Figure 3B). There was no fluid in the lesion. In addition to crystals in the right eye, RPE defect and external retinal tubalization were observed (Figure 3A). No history of systemic disease or drug use history was present in the medical history of the patient. However, consanguinity was present as the parents were cousins. The entire family was examined and BCD was also detected in an 8-year old boy who was the youngest family member.
Figure 1. Color fundus pictures depicting the intraretinal crystals, foveal scar (white arrow) and pigment clusters (black arrow).

A: Right eye; B: Left eye.
Figure 2. Common areas of chorioretinal atrophy in fluorescein angiography.
A: Right eye; B: Left eye.
Figure 3. OCT of the right-left eye showing high reflective crystalline deposits in the sensorineural retina and RPE, irregularity and increased reflectivity in RPE.
A: Outer segment tabulation; B: Subretinal scarring possibly due to old choroidal neovascularization.
Case 2
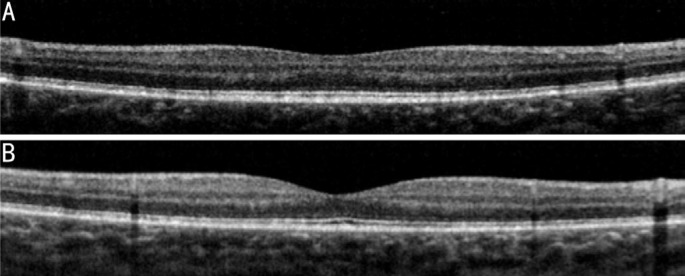
An 8-year-old male patient was examined, and visual acuity was evaluated as 1.0 in both eyes. Biomicroscopic examination of the anterior segment and intraocular pressure were normal. Numerous shiny white-yellow deposits were detected at the posterior pole (Figure 4). Color fundus photographs and OCT were taken. The OCT images showed high reflective crystalline deposits in the sensorineural retina (Figure 5).
Figure 4. Colour fundus images.
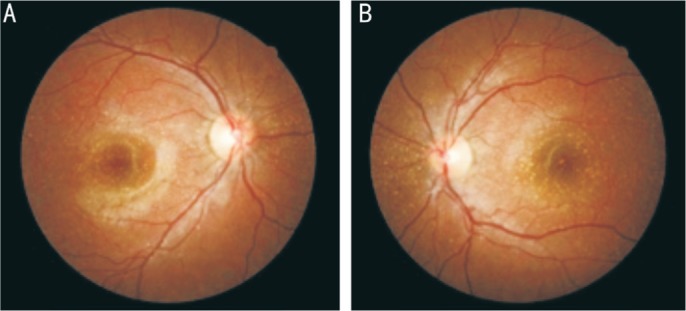
A: Right eye; B: Left eye.
Figure 5. OCT images.
A: Right eye; B: Left eye.
BCD is a rare, chorioretinal degeneration that is usually inherited through autosomal recessive CYP4V2 (cytochrome P450 family 4 subfamily V polypeptide 2) gene due to gene mutation. Usually dystrophy appears in the third decade of life, but it may also occasionally be seen in the first or second decades[2],[13]. BCD can result in legal blindness with decreasing visual acuity and narrowing of the visual field in the fifth or sixth decades. Choroidal neovascularization, cystoid macular edema, and macular hole have been reported in patients with BCD[5]–[12],[14]–[16]. Fuerst et al[12] treated a 34-year-old patient diagnosed with choroidal neovascularization using bevacizumab. Nachiappan et al[9] diagnosed BCD which was complicated with choroidal neovascular membrane (CNVM) in a 33-year-old male patient. The CNVM was treated with intravitreal ranibizumab, and it was thought that the CNVM development may have been due to crystalline irritation against the Bruch membrane[9]. Mamatha et al[8] also diagnosed BCD which was complicated with CNVM in a 31-year-old patient, and treated the CNVM with intravitreal ranibizumab. Atmaca et al[5] reported the case of a 13-year-old patient with CNVM in the peripapillary region and serous retinal detachment in the fovea. Gupta et al[6] diagnosed CNVM complicated by juxtafoveal CNVM in a 64-year-old male patient. The lesion was inactive so was not treated. The current patient was a 13-year-old girl. Numerous white-yellow deposits, chorioretinal atrophic areas, and scar formation were detected, which could have developed after CNVM. There were no findings of active CNVM such as hemorrhagia or subretinal fluid. The OCT images showed high reflective crystalline deposits in the sensorineural retina and RPE, and irregularity and increased reflectivity in RPE. Subretinal scarring possibly due to old choroidal neovascularization was detected in the left eye. There was no fluid in the lesion. Although early studies showed crystals in the cornea to be diagnostic criteria for BCD, later studies did not show corneal crystals in some patients. In the current patient, no corneal crystals were observed. The presence of common chorioretinal atrophy and scarring suggested that the disease had been present for a long time. The patient's mother and two siblings were also examined carefully. No signs of the disease in the 19-year-old sister of the patient whereas in the 8-year-old brother, crystals were detected in the retina but not in the cornea. To the best of our knowledge, there are no cases in literature of patients younger than this with BCD.
With careful ophthalmological examination, BCD can be easily diagnosed. Diagnosis can be supported by OCT and FFA findings. It was not possible to perform electrophysiological and genetic testing on these cases because of the lack of available facilities. The consanguinity of the parents of these patients suggests that the genetic transition may be inherited through autosomal recessive. This demonstrates that genetic transitions should be considered in consanguineous marriages and cases can be diagnosed at a much younger age by conducting health screening on all family members.
Acknowledgments
Conflicts of Interest: Kobat SG, None; Gul FC, None; Yusufoglu E, None.
REFERENCES
- 1.Bietti G. Su alcune forme atippiche o rare di degeneraziona retinica (degenerazioni tappeto-retiniche e quadri morbosi similari) Boli Oculist. 1937;16:1159–1244. [Google Scholar]
- 2.Wilson DJ, Weleber RG, Klein ML, Welch RB, Green WR. Bietti's crystalline dystrophy. A clinicopathologic correlative study. Arch Ophthalmol. 1989;107(2):213–221. doi: 10.1001/archopht.1989.01070010219026. [DOI] [PubMed] [Google Scholar]
- 3.Eldem B, Irkeç M. Bietti's crystal retinal and corneal dystrophy due to two cases. T Oft Gaz. 1989;19:602–607. [Google Scholar]
- 4.Richards BW, Brodstein DE, Nussbaum JJ, Ferencz JR, Maeda K, Weiss L. Autosomal dominant crystalline dystrophy. Ophthalmology. 1991;98(5):658–665. doi: 10.1016/s0161-6420(91)32237-1. [DOI] [PubMed] [Google Scholar]
- 5.Atmaca LS, Muftuoglu O, Atmaca-Sonmez P. Peripapillary choroidal neovascularization in Bietti crystalline retinopathy. Eye (Lond) 2007;21(6):839–842. doi: 10.1038/sj.eye.6702673. [DOI] [PubMed] [Google Scholar]
- 6.Gupta B, Parvizi S, Mohamed MD. Bietti crystalline dystrophy and choroidal neovascularisation. Int Ophthalmol. 2011;31(1):59–61. doi: 10.1007/s10792-010-9406-8. [DOI] [PubMed] [Google Scholar]
- 7.Li Q, Li Y, Zhang X, Xu Z, Zhu X, Ma K, She H, Peng X. Utilization of fundus autofluorescence, spectral domain optical coherence tomography, and enhanced depth imaging in the characterization of bietti crystalline dystrophy in different stages. Retina. 2015;35(10):2074–2084. doi: 10.1097/IAE.0000000000000592. [DOI] [PubMed] [Google Scholar]
- 8.Mamatha G, Umashankar V, Kasinathan N, Krishnan T, Sathyabaarathi R, Karthiyayini T, Amali J, Rao C, Madhavan J. Molecular screening of the CYP4V2 gene in Bietti crystalline dystrophy that is associated with choroidal neovascularization. Mol Vis. 2011;17:1970–1977. [PMC free article] [PubMed] [Google Scholar]
- 9.Nachiappan K, Krishnan T, Madhavan J. Ranibizumab for choroidal neovascular membrane in a rare case of Bietti's crystalline dystrophy: a case report. Indian J Ophthalmol. 2012;60(3):207–209. doi: 10.4103/0301-4738.95873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Le Tien V, Atmani K, Querques G, Massamba N, Souied EH. Ranibizumab for subfoveal choroidal neovascularization in Bietti crystalline retinopathy. Eye (Lond) 2010;24(11):1728–1729. doi: 10.1038/eye.2010.116. [DOI] [PubMed] [Google Scholar]
- 11.Yin H, Jin C, Fang X, Miao Q, Zhao Y, Chen Z, Su Z, Ye P, Wang Y, Yin J. Molecular analysis and phenotypic study in 14 Chinese families with Bietti crystalline dystrophy. PLoS One. 2014;9(4):e94960. doi: 10.1371/journal.pone.0094960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Fuerst NM, Serrano L, Han G, Morgan JI, Maguire AM, Leroy BP, Kim BJ, Aleman TS. Detailed functional and structural phenotype of Bietti crystalline dystrophy associated with mutations in CYP4V2 complicated by choroidal neovascularization. Ophthalmic Genet. 2016;37(4):445–452. doi: 10.3109/13816810.2015.1126616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bozkir DM, Ekinciler OF, Mirza E, Dogan H. TAO National Congress Bulletin İstanbul; 1991. Bietti's Crystalline Retinal dystrophy; pp. 178–183. [Google Scholar]
- 14.Saatci AO, Yaman A, Berk AT, Söylev MF. Macular hole formation in Bietti's crystalline retinopathy. A case report. Ophthalmic Genet. 1997;18(3):139–141. doi: 10.3109/13816819709057127. [DOI] [PubMed] [Google Scholar]
- 15.Saatci AO, Doruk HC, Yaman A. Cystoid macular edema in bietti's crystalline retinopathy. Case Rep Ophthalmol Med. 2014;2014:964892. doi: 10.1155/2014/964892. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Broadhead GK, Chang AA. Acetazolamide for cystoid macular oedema in Bietti crystalline retinal dystrophy. Korean J Ophthalmol. 2014;28(2):189–191. doi: 10.3341/kjo.2014.28.2.189. [DOI] [PMC free article] [PubMed] [Google Scholar]