The impetus for our 1996 milbank quarterly article “Organizing Care for Patients With Chronic Illness”1 was the disturbing evidence of inadequate care among patients with common chronic illnesses. Why were well‐trained, hard‐working clinicians (like us) unable to deliver proven services reliably or achieve targeted levels of blood pressure, HbA1c, or other disease control indicators for our patients? Our reliance on sporadic, physician‐dominated office visits with competing agendas and multipound paper records wasn't doing the job. Pioneers in health care quality improvement, such as Don Berwick and Paul Batalden, helped us to see that we were working in poorly designed systems of care, which had evolved ages ago to respond to acute illnesses and injuries. In other words, our “system” for delivering care to our patients “was perfectly designed to achieve the [mediocre] results it achieves.”2
We looked in the literature for changes to traditional care systems that would improve care. Three findings influenced our future course. First, the interventions that improved care and outcomes consistently fell into four categories: changes to the way care is delivered, changes to the education and support for patients, interventions to educate or remind providers, and changes to information systems. In the model shown in Figure 1 of the Milbank Quarterly article and reprinted here, these four categories were labeled Practice Redesign, Patient Education, Expert System, and Information, respectively. Second, the relevant research almost invariably involved patients with a particular chronic disease such as diabetes or asthma. This raised a critical question—would the system changes that improved care and outcomes vary substantially from condition to condition? Our literature review strongly suggested that similar interventions in the four categories improved care across different chronic conditions. Third, further literature reviews found that more multifaceted interventions with components from all four categories resulted in the largest improvements in care and outcomes.3
Figure 1.
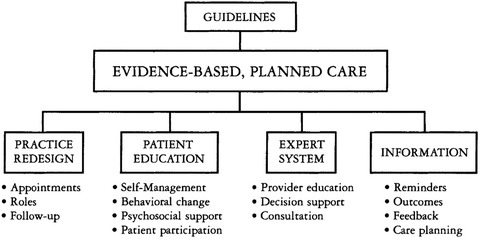
Improving Outcomes in Chronic Illnessa
aReproduced from The Milbank Quarterly 1
We then began a series of activities to improve and refine the Milbank article model, and to study its validity and utility. Contemporaneous research encouraged us to rethink the names and content of the “Patient Education” and “Expert System” categories in the original model. Evidence was mounting that collaborative, goal‐oriented, self‐management programs changed patient health behaviors and improved disease outcomes, while traditional didactic patient education had minimal impact. This led us to change the category's name to “Self‐management Support.” Dr. Russell Glasgow, lead author of a related paper in this issue of the Quarterly,4 was instrumental in helping us to understand and present effective approaches to enabling patients to become more competent self‐managers. Also, provider reminders and alerts proved far more successful in changing provider behavior than traditional continuing education. “Expert System” became “Decision Support” in the final Chronic Care Model (CCM).
To assess the validity of the evolving CCM, we asked 75 experts in chronic illness management to review the model. This group included researchers, practicing clinicians, nurses, and other health professionals, health administrators, and patient advocates. Their comments guided a major revision of the CCM. The changes included:
Visually placing the medical practice in its surrounding community and adding two new related intervention categories: “Community Resources and Policies” and “Health Care Organization.”
Showing the mechanisms by which the recommended changes would improve patient outcomes. Effective self‐management support and linkage to relevant community services help to create “Informed, Activated Patients.” Interventions in “Health Care Organization,” “Delivery System Design,” “Decision Support,” and “Information Systems” categories help to ensure “Prepared, Proactive Practice Teams.”
Evidence‐based care and better disease control result from “Productive Interactions” between more engaged patients and well‐organized practice teams.
The revised CCM was first published in 1998,5 and is shown in Figure 2.
Figure 2.
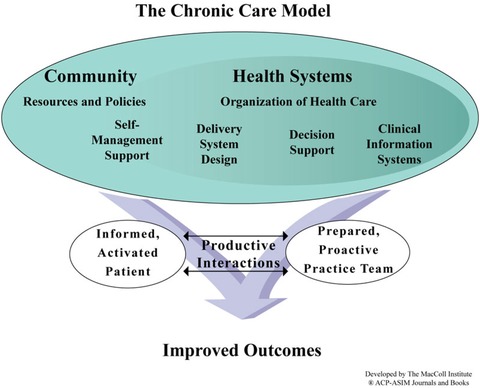
The Chronic Care Model [Color figure can be viewed at wileyonlinelibrary.com]
While the experts largely endorsed the revised CCM, many questioned whether front‐line providers would be willing or able to make such sweeping changes to their practices. To test the acceptability and effectiveness of the CCM, we searched for a realistic approach to practice transformation that would give busy practices the necessary guidance and support over time. The best option was the Institute for Healthcare Improvement's (IHI) Breakthrough Series Collaboratives. We and IHI jointly conducted five collaboratives between 1999 and 2002 that collectively involved several hundred primary care practices. In general, the evaluations showed that a majority of practices could make relevant changes, care became more consistent with evidence‐based guidelines, and patient outcomes improved.6 Watching busy practices wrestle with our largely hypothetical recipe for better care was instructive. We learned that practice change was difficult, and especially so for practices that lacked effective leadership, clearly defined provider panels, robust measurement of clinical quality, or effective clinical teams. And the CCM didn't directly address those issues.
Between 1999 and 2007, references to and use of the CCM in primary care quality improvement, research, and policy planning rapidly increased. During this same interval, American primary care appeared to many to be mired in an existential crisis—dissatisfied patients, burnt‐out physicians, uneven quality of care, and fewer and fewer US medical students choosing primary care as their specialty. In response, the major American primary care professional societies proposed in 2007 a new model of primary care—the Patient‐Centered Medical Home (PCMH)—that hopefully would better meet patient needs, and rejuvenate the primary care workforce.7
The proposed PCMH model essentially combined the elements of the CCM with the Pediatric Patient‐Centered Medical Home model. The latter reaffirmed the importance of the defining features of primary care: continuity of care with a personal physician, comprehensive care, care coordination, and enhanced access. Since 2007, our practice improvement activities have focused on PCMH transformation because:
the components of the CCM are incorporated in PCMH definitions and standards;
recognition as a PCMH often has financial advantages for practices; and
the PCMH model emphasizes foundational practice capacities, such as effective leadership, team‐building, empanelment, and performance measurement that are essential for CCM implementation.
Since 2007, thousands of practices have been involved in PCMH practice transformation programs. It has been estimated that nearly one‐half of American primary care physicians are now practicing in a PCMH. Despite its rapid dissemination and multiplicity of evaluations, evidence of PCMH impacts on quality and cost continues to be disappointingly mixed.8
Thus far, there have been no convincing explanations for the variability of PCMH evaluation results. In our CCM collaboratives, successful practices substantially changed care delivery by increasing the involvement of nonphysician staff in clinical care. Building effective teams that have the trust of the providers may be critical, but has proven to be a major hurdle for many practices. In 2012, we launched a national program, The Primary Care Team: Learning from Effective Ambulatory Practices, whose goal was to help primary care practices develop more effective primary care teams using insights, examples, and resources gleaned from 30 innovative, high‐performing practices across the United States, 80% of which were certified PCMHs. All 30 practices had well‐developed practice teams and work processes that enabled these practices to deliver care consistent with the CCM (see www.improvingprimarycare.org). A survey of physicians and staff in these practices found high percentages expressing satisfaction with their work.
Twenty‐three years after publication of our Milbank article, we know much more about the design of care systems that can reliably deliver evidence‐based care, engage and satisfy patients, and achieve better control of chronic diseases. Nevertheless, helping busy practices to transform into effective care systems still remains a formidable challenge.
Acknowledgments
The body of work described in this article would not have been possible without the many contributions of my MacColl Center colleagues, especially my 1996 Milbank Quarterly coauthors, Brian Austin and Michael Von Korff, and the enduring encouragement and support of the Robert Wood Johnson Foundation.
References
- 1. Wagner EH, Austin BT, Von Korff M. Organizing care for patient with chronic illness. Milbank Q. 1996;74(4):511‐544. [PubMed] [Google Scholar]
- 2. Berwick DM. A Primer on leading the improvement of systems. BMJ. 1996;314:1564‐5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Bodenheimer T, Wagner EH, Grumbach K. Improving primary care for patients with chronic illness, part 2. JAMA. 2002;288:1775‐1779. [DOI] [PubMed] [Google Scholar]
- 4. Glasgow RE, Huebschmann AG, Krist AH, DeGruy FV. An Adaptive, Contextual, Technology‐Aided Support (ACTS) System for Chronic Illness Self‐Management [published online August 2019]. Milbank Q. 10.1111/1468-0009.12412 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Wagner EH. Chronic disease management: what will it take to improve care for chronic illness? Effective clinical practice: 1998, Vol. 1(1), p. 2‐4. [PubMed] [Google Scholar]
- 6. Coleman K, Austin BT, Brach C, Wagner EH. Evidence on the chronic care model in the new millennium. Health Aff. 2009;28:75‐85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Joint Principles of the Patient‐centered Medical Home , American Academy of Family Practice website. https://www.aafp.org/dam/AAFP/documents/practice_management/pcmh/initiatives/PCMHJoint.pdf. Accessed July 7, 2019.
- 8. Sinaiko AD, Landrum MB, Meyers DJ, et al. Synthesis of research on patient‐centered medical homes brings systematic differences into relief. Health Aff. 2017;36:500‐508. [DOI] [PMC free article] [PubMed] [Google Scholar]


