Abstract
Objective:
Among patients with status epilepticus, we sought to determine the rate of endotracheal intubation, identify the physician specialties responsible for endotracheal intubation, and characterize the trend in use of endotracheal intubation over the last 20 years.
Methods:
We performed a cross-sectional study using data from 2 sources. First, we used inpatient claims between 2009 and 2015 from a nationally representative 5% sample of Medicare beneficiaries. Patients with status epilepticus were identified using International Classification of Diseases, 9th Revision, Clinical Modification (ICD-9-CM) codes, and those who underwent endotracheal intubation were identified based on Current Procedural Terminology codes. Medical specialties of providers performing intubation were identified based on Healthcare Provider Taxonomy Codes. Second, we used claims data from the National Inpatient Sample (NIS) to estimate the annual rates and trends of endotracheal intubation and tracheostomy among patients with status epilepticus from 1995 to 2014.
Results:
Among 1971 Medicare beneficiaries with status epilepticus, 566 (29%) patients underwent endotracheal intubation. 375 (66%) patients were intubated on admission. The most common medical providers performing intubation in patients with status epilepticus were emergency medicine physicians (50.4%), anesthesiologists (16.4%), and pulmonary medicine physicians (10.1%). Neurologists accounted for 1.7% of all intubations. Among individuals with status epilepticus identified in the NIS, 248 681 (41.7%) were intubated. The proportion of patients intubated increased from 29.5% (95% confidence interval [CI]: 27.8%-31.3%, P = .018) in 1995 to 50.8% (95% CI: 49.6%-52%, P = .012) in 2014. The proportion of patients with status epilepticus who underwent tracheostomy increased from 2.2% (95% CI: 1.7%-2.7%, P = .005) in 1995 to 3.4% (95% CI: 3%-3.9%, P = .004) in 2014.
Significance:
Approximately 1 in 3 patients with status epilepticus undergo endotracheal intubation. Over the last 20 years, the proportion of patients with status epilepticus undergoing endotracheal intubation has almost doubled. Neurologists perform a small percentage of these intubations.
Keywords: status epilepticus, mechanical ventilation, intubation, tracheostomy
Status epilepticus is a neurological emergency requiring rapid treatment. There are approximately 200 000 cases of status epilepticus in the United States each year with an associated mortality between 9% and 27%.1,2 In order to avoid permanent brain injury, guidelines recommend urgent seizure control in patients with status epilepticus. Respiratory failure is a common complication of both the disease itself and its treatments (ie, anesthetics) and as a result, endotracheal intubation is often performed to manage respiratory failure and maintain adequate ventilation and oxygenation.3–7 Prior randomized trials indicate that between 15% and 18% of all patients with status epilepticus undergo endotracheal intubation at the time of hospital admission, but the overall rate and timing of endotracheal intubation within the hospitalization for status epilepticus is uncertain.1,8 Among patients with status epilepticus, we sought to determine the rate of endotracheal intubation, identify the physician specialties responsible for endotracheal intubation, and characterize the trend in use of endotracheal intubation over the last 20 years. As guidelines for the treatment of status epilepticus have become more aggressive over time, with earlier recommended use of anesthetics and increased use of continuous electroencephalography monitoring, we hypothesized that the rate of endotracheal intubation is increasing in patients with status epilepticus and that neurologist are routinely involved in the care of these patients.
Methods
Study Design
We performed a cross-sectional retrospective cohort study using data from 2 different data sets. First, we used inpatient claims between 2009 and 2015 from a nationally representative 5% sample of Medicare beneficiaries. The US federal government’s Centers for Medicare and Medicaid Services provide health insurance to a large majority of US residents once they reach 65 years of age. Centers for Medicare and Medicaid Services makes available to researchers data on claims submitted by providers and hospitals in the course of Medicare beneficiaries’ clinical care. Claims data from hospitals include International Classification of Diseases, 9th Revision, Clinical Modification (ICD-9-CM) diagnosis and procedure codes and dates of hospitalization. Physician claims include Current Procedural Terminology (CPT) codes, the dates of service, and physicians’ specialty. Multiple claims for a given patient can be linked via a unique beneficiary identifier code, thus allowing for a comprehensive and longitudinal analysis of each beneficiary’s care over time.
Second, to evaluate trends in use of endotracheal intubation and tracheostomy in patients with status epilepticus, we used inpatient discharge data from the National Inpatient Sample (NIS) between 1994 and 2014. The NIS is a nationally representative, deidentified database that is funded by the Agency for Healthcare Research and Quality.9 It contains a 20% stratified sample of all inpatient hospitalizations annually from nonfederal hospitals across the United States.10
Standard Protocol Approval
The Weill Cornell Medical College institutional review board approved our analysis of these data. We adhered to the Report of Studies Conducted Using Observational Routinely Collected Health Data guidelines for studies using administrative claims data.11
Patient Population
Among our 5% sample of beneficiaries, we included only those ≥65 years of age who had continuous coverage in traditional fee-for-service Medicare (both parts A and B) for at least 1 year (or until death, if applicable) and no enrollment in a Medicare Advantage plan, as is standard in analysis of Medicare data.12 From this sample, we selected patients hospitalized between January 1, 2009 and September 30, 2015 for status epilepticus as defined by the ICD-9-CM code 345.3 in any discharge diagnosis position. This algorithm has been previously validated and found to have a sensitivity of 82% (95% confidence interval [CI]: 72%-92%) and specificity of 100%.13,14 The end date of September 30, 2015 was chosen because ICD-10 went into effect on October 1, 2015. We included all eligible hospitalizations for a given patient, and for each eligible hospitalization, we included all physician claims dated from the day of admission through the day of discharge.
In the NIS, we identified all patients hospitalized with status epilepticus using ICD-9-CM code 345.3 in any discharge diagnosis position. In a sensitivity analysis, we considered only patients with status epilepticus coded in the principal discharge diagnosis position.
Measurements
In our analysis of Medicare beneficiaries, our primary outcome was endotracheal intubation performed during the index hospitalization for status epilepticus. Endotracheal intubation was identified using the CPT code 31500. In addition, we identified the day on which endotracheal intubation was performed and the medical specialty of the provider (Healthcare Provider Taxonomy Code) who performed the intubation. We determined demographic characteristics including age, sex, and race, as reported by Medicare. In addition, a cumulative clinical severity score was calculated for each patient using the Charlson Comorbidity index.15,16
In the NIS, our primary outcome was endotracheal intubation or mechanical ventilation performed during the index hospitalization for status epilepticus using procedure codes 97.x and 96.7. As a secondary outcome, we evaluated trends in the use of tracheostomy, as defined by ICD-9-CM procedure codes 31.1, 31.2, 31.21, and 31.29.17–19
Statistical Analysis
Patients’ baseline characteristics were compared using the χ2 test and the t test, as appropriate. Crude rates were reported using descriptive statistics with exact 95% CI. Since we were interested in which medical specialty performed endotracheal intubation and when endotracheal intubation was performed, we created tabular lists of the top 10 physician specialties performing endotracheal intubation on the day of admission through day 3 of hospitalization. In our analysis of the NIS, we used survey weights to report annual rates of endotracheal intubation and variance-weighted linear least squares regression to test temporal trends between 1994 and 2013 in the NIS. All trend analyses were 2-tailed and statistical significance was defined as a P value <.05. Statistical analysis was performed using Stata (version 14.0, College Station, Texas).
Results
Medicare Beneficiaries
We identified 1971 Medicare beneficiaries with status epilepticus, of whom 566 (29%) underwent endotracheal intubation. Patients who underwent endotracheal intubation were slightly younger (75.5 vs 76.8 years) but were similar in terms of sex, race, or Charlson Comorbidity burden (Table 1). The majority of patients were intubated for status epilepticus on the day of admission (66%); the remainder of patients with status epilepticus were intubated between day 1 through 6 of the hospitalization.
Table 1.
Characteristics of a 5% Sample of Medicare Beneficiaries With Status Epilepticus, Stratified by Performance of Endotracheal Intubation.
| Characteristica | Intubation (N = 566) | No Intubation (N = 1405) |
|---|---|---|
| Age, mean (SD), years | 75.5 (0.3) | 76.8 (0.2) |
| Female | 320 (56.5) | 837 (59.8) |
| Race | ||
| White | 403 (71.2) | 994 (70.8) |
| Black | 139 (24.6) | 321 (22.9) |
| Other | 24 (4.2) | 90 (6.4) |
| Charlson Comorbidity Index, 95% CI | 3.1 (3-3.3) | 3.1 (3-3.2) |
Abbreviations: CI, confidence interval; SD, standard deviation.
aData are presented as number (%) unless otherwise specified.
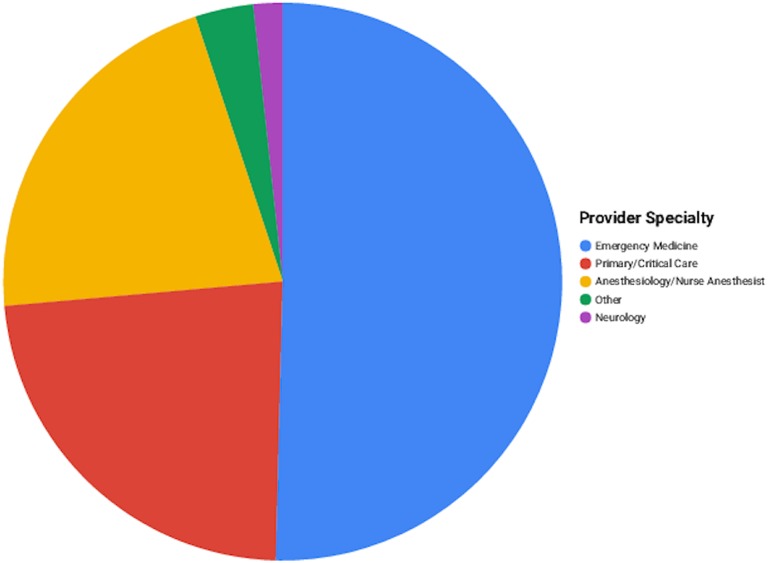
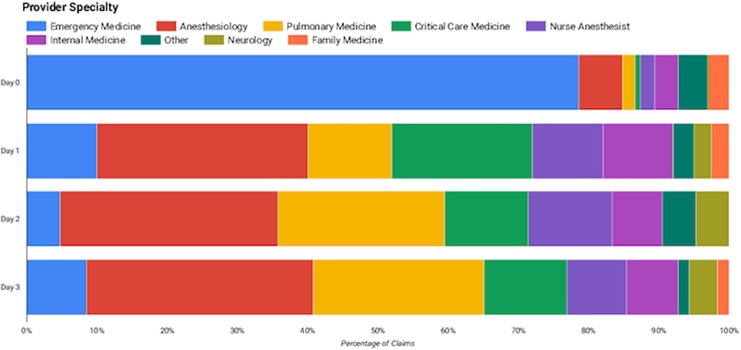
Emergency medicine physicians accounted for the majority of intubations (50.4%). The remaining claims for intubation were most commonly submitted by physicians trained in anesthesiology (16.4%) and pulmonary medicine (10.1%). Neurologists accounted for 1.7% of all intubation claims. When we broke down the analysis by day of hospitalization for status epilepticus, emergency medicine physicians accounted for the vast majority of claims from the day of admission (78.6%) followed by anesthesiologists (6.2%). Beyond the admission day, anesthesiologists accounted for the majority of claims for intubation: 30.0% on the second hospitalization day and 31.0% on third hospitalization day. Neurologists accounted for 2.5% of intubations on day 2 and 4.0% on day 3 of hospitalization (Figures 1 and 2).
Figure 1.
Distribution of specialties of physicians performing endotracheal intubation for status epilepticus. Emergency medicine physicians perform the majority of endotracheal intubations (50.4%). The remaining intubations were most commonly performed by anesthesiologists (16.4%) and pulmonary medicine physicians (10.1%). Neurologists accounted for 1.7% of all intubations.
Figure 2.
Distribution of specialties of physicians performing endotracheal intubations among patients with status epilepticus on the day of admission and subsequent hospitalization days. Emergency medicine physicians accounted for the majority of intubations on the day of admission (78.6%) followed by anesthesiologists (6.2%). Beyond the admission day, anesthesiologists accounted for the majority of all intubations: 30.0% on the second hospitalization day and 31.0% on third hospitalization day. Neurologists accounted for 2.5% of all intubations on day 2 and 4.0% on day 3 of hospitalization.
National Inpatient Sample Results
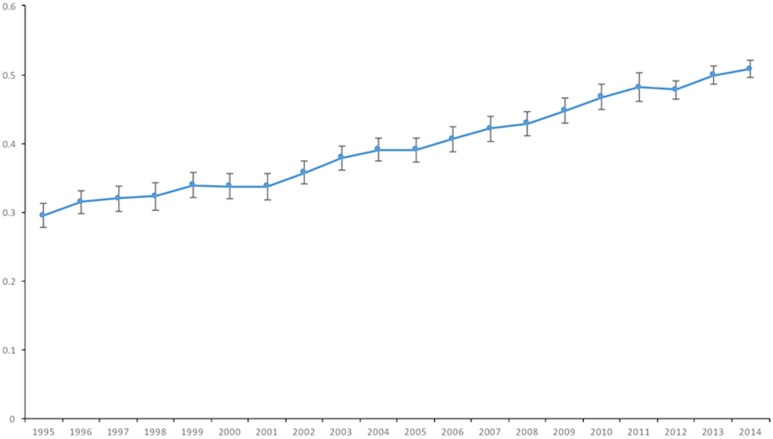
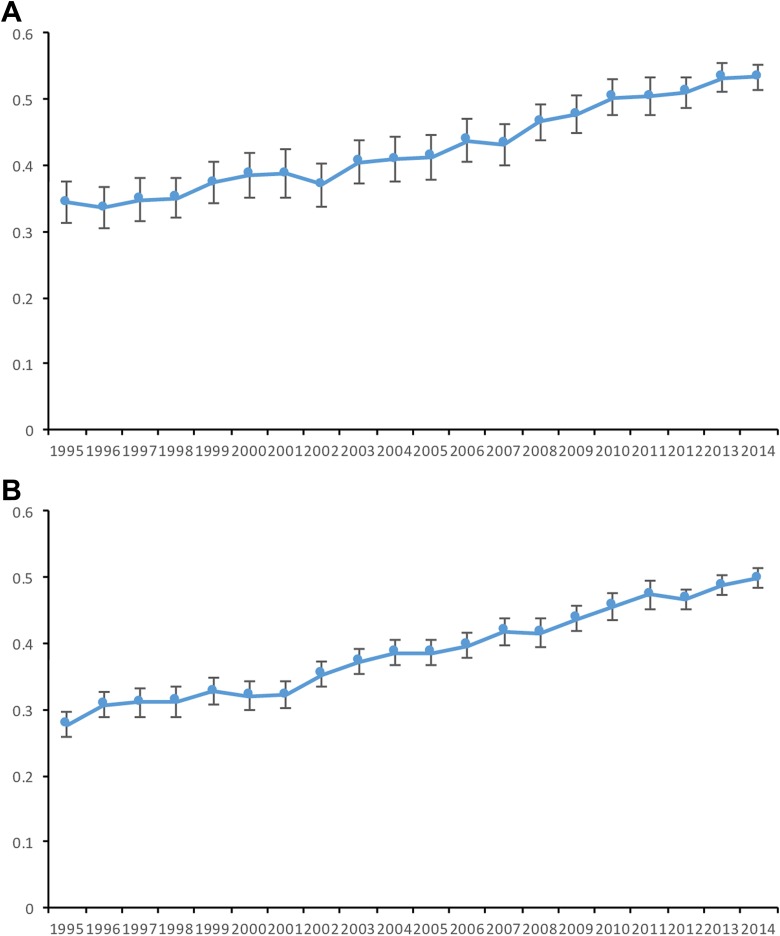
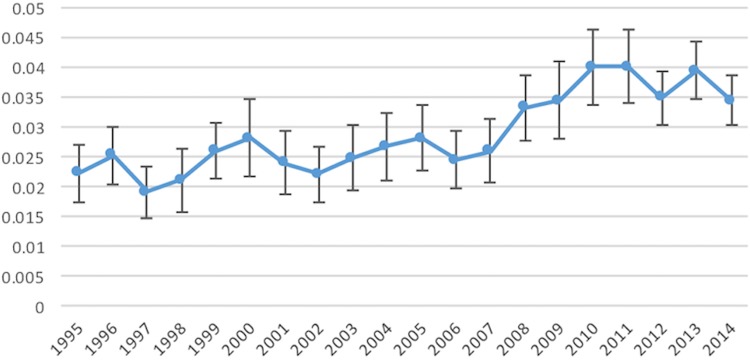
Between 1995 and 2014, 41.7% (95% CI: 41.2%-42.3%) of patients with status epilepticus received endotracheal intubation. The proportion of patients with status epilepticus who received endotracheal intubation increased from 29.5% (95% CI: 27.8%-31.3%) in 1995 to 50.8% (95% CI: 49.6%-52.0%) in 2014; these results were similar when we considered only patients with status epilepticus in the primary discharge diagnosis position: 23.9% (95% CI: 21.8%-25.9%) in 1995 and 39% (95% CI: 37.5%-40.5%) in 2014 (Figure 3). The rate of endotracheal intubation among patients with status epilepticus increased among patients <65 years old and ≥65 years between 1995 and 2014 (Figure 4). In addition, the use of tracheostomy in patients with status epilepticus increased from 2.2% (95% CI: 1.7%-2.7%) in 1995 to 3.4% (95% CI: 3.0%-3.9%) in 2014 (Figure 5; Table 2).
Figure 3.
Rate of intubation in patients with status epilepticus using data from the national inpatient sample from 1995 to 2014. The proportion of patients with status epilepticus who received endotracheal intubation increased from 29.5% (95% CI: 27.8%-31.3%) in 1995 to 50.8% (95% CI: 49.6%-52%) in 2014. Error bars indicate 95% confident interval.
Figure 4.
A, Rate of intubation in patients ≥65 years old with status epilepticus using data from the national inpatient sample from 1995 to 2014. The rate of intubation in ≥65 years old patients with status epilepticus increased from 34.4% (95% CI: 31.2%-37.6%) in 1995 to 53.3% (95% CI: 51.3%-55.3%) in 2014. Error bars indicate 95% confident interval. B, Rate of intubation in patients <65 years old with status epilepticus using data from the national inpatient sample from 1995 to 2014. The rate of intubation in <65 years old patients with status epilepticus increased from 27.7% (95% CI: 25.8%-29.6%) in 1995 to 49.9% (95% CI: 48.5%-51.3%) in 2014. Error bars indicate 95% confident interval.
Figure 5.
Rate of tracheostomy in patients with status epilepticus using data from the national inpatient sample from 1995 to 2014. The use of tracheostomy in patients with status epilepticus increased from 2.2% (95% CI: 1.7%-2.7%) in 1995 to 3.4% (95% CI: 3.0%-3.9%) in 2014. Error bars indicate 95% confident interval.
Table 2.
Characteristics of the National Inpatient Sample (NIS) Patients With Status Epilepticus, Stratified by Performance of Endotracheal Intubation.
| Characteristica | Intubation (N = 248 681) | No Intubation (N = 346 745) |
|---|---|---|
| Age, mean (SD), years | 45 (0.5) | 40 (0.5) |
| Female | 113 150 (45.5) | 172 700 (49.9) |
| Race | ||
| White | 118 732 (56.7) | 164 177 (57.6) |
| Black | 52 027 (24.8) | 67 482 (23.7) |
| Other | 38 795 (18.5) | 53 163 (18.7) |
| Charlson Comorbidity Index, 95% CI | 1.03 (1.00-1.06) | 0.69 (0.67-0.71) |
Abbreviations: CI, confidence interval; SD, standard deviation.
aData are presented as number (%) unless otherwise specified.
Discussion
In a large, nationally representative sample of Medicare beneficiaries, we found that approximately 1 in 3 patients with status epilepticus are intubated for status epilepticus. The proportion of patients with status epilepticus undergoing intubation has almost doubled in the last 20 years. Neurologists perform few of these intubations.
Previous randomized trials have reported that approximately 15% to 18% of patients with status epilepticus are intubated.1,8 Furthermore, there has been an increasing trend in the number of hospitalizations for status epilepticus between 1999 and 2010.20 Vohra et al demonstrated a higher mortality for intubated patients in their secondary analysis of the Rapid Anticonvulsant Medication Prior to Arrival Trial.21,22 Our study builds upon these prior studies by identifying the rate of endotracheal intubation in older patients with status epilepticus and by demonstrating an increasing trend in the use of intubation in patients with status epilepticus.
There are multiple possible explanations for the increased use of endotracheal intubation among patients with status epilepticus. First, the combination of the change in the practical definition of status epilepticus from 30 to 5 minutes of seizure activity and the change in guidelines that recommend early escalation of antiepileptic therapy in patients with status epilepticus may have led to a lower threshold for initiation of aggressive seizure control.23 As outcomes of patients with status epilepticus are strongly linked to the duration of status epilepticus, the American Epilepsy Society guidelines strongly support rapid escalation of antiepileptic therapy including anesthetics, which necessitate endotracheal intubation.23–26 Second, improved surveillance of seizures via increased use of continuous electroencephalography monitoring may have led to an increased detection of seizures and status epilepticus.20,27 Third, although an increase in the use of administrative claims codes may explain the observed increase in incidence of status epilepticus, this would have been unlikely to have affected the observed increase in the proportion of patients with status epilepticus that undergo endotracheal intubation.
Our results suggest that emergency medicine physicians and anesthesiologists accounted for the majority of endotracheal intubations in patients with status epilepticus. Neurologists accounted for a small percentage of endotracheal intubations. Although the field of neurocritical care continues to expand, neurologists performed <5% of endotracheal intubations that were performed after the admission day for status epilepticus (when the patients were unlikely to still be in the emergency department). Further data are necessary to evaluate whether these patients are primarily being taken care of by neurointensivists or by a consulting neurologist as the majority of hospitals do not have a dedicated neurological intensive care unit.
Our findings may have implications for future research in status epilepticus. As guidelines recommend early aggressive seizure control, endotracheal intubation is being more frequently used to provide third-line agents anesthetic agents.23 However, it remains unclear whether an increased use of anesthetics and endotracheal intubation among patients with status epilepticus is associated with better outcomes; endotracheal intubation is associated with respiratory infections, prolonged hospitalizations, and place patients at high risk for systemic complications. Future studies are therefore necessary to evaluate the benefit of endotracheal intubation for the use of anesthetics among patients with status epilepticus.”
Our study has several limitations. First, we lacked data regarding the severity, etiology, and medications used to treat status epilepticus. Similarly, we lacked electroencephalography data determining whether the seizures were clinical versus subclinical or generalized versus partial, and we lacked data regarding seizure semiology. Second, our study of Medicare beneficiaries >65 years of age may limit the generalizability of our results. However, we tried to circumvent this issue by also using the NIS, which has data on all patients over 18 years of age. Third, as our study relied on ICD-9-CM codes to identify patients with status epilepticus, study results may have misclassification bias. However, we used ICD-9-CM codes that were previously well-validated and utilized in prior studies characterizing patients with status epilepticus.13 Furthermore, we were unable to account for differences in coding practices, including variability based on geographical location or type of hospital (academic versus community). Fourth, as we only evaluated claims for endotracheal intubation that occurred within the hospitalization for status epilepticus, it is possible that we missed a number of patients with status epilepticus who were intubated en route to the hospital. However, data from the RAMPART trial evaluating out-of-hospital midazolam versus lorazepam suggest that more than 90% of all intubations in patients with status epilepticus are performed after arrival to the hospital.21
Conclusions
Among a large, heterogeneous group of Medicare beneficiaries, we found that approximately 1 in 3 patients with status epilepticus undergo intubation. The proportion of patients with status epilepticus undergoing intubation has almost doubled from 1995 to 2014. Neurologists perform a small percentage of intubations for patients with status epilepticus.
Footnotes
Authors’ Note: Acquisition of data by Alkhachroum and Chatterjee. Administrative, technical, or material support by Alkhachroum, Chatterjee, Chen, and Merkler. Analysis and interpretation of data by Alkhachroum, Rubinos, Chen, and Merkler. Ayham Alkhachroum had full access to all the data in the study and takes responsibility for the integrity of the data and the accuracy of the data analysis. Critical revision of the manuscript for important intellectual content by Rubinos, Chatterjee, Chen, Martin, Claassen, Murthy, and Merkler. Drafting of the manuscript by Alkhachroum. Statistical analysis by Chatterjee and Merkler. Study concept and design by Alkhachroum and Merkler. Study supervision by Merkler.
Declaration of Conflicting Interests: The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: Alexander Merkler is supported by NIH grant KL2TR0002385 and the Leon Levy Foundation in Neuroscience. Santosh Murthy is supported by the American Brain Foundation/American Academy of Neurology and the Leon Levy Foundation.
References
- 1. Alldredge BK, Gelb AM, Isaacs SM. et al. A comparison of lorazepam, diazepam, and placebo for the treatment of out-of-hospital status epilepticus. N Engl J Med. 2001;345:631–637. [DOI] [PubMed] [Google Scholar]
- 2. DeLorenzo RJ, Hauser WA, Towne AR. et al. A prospective, population-based epidemiologic study of status epilepticus in Richmond, Virginia. Neurology. 1996;46(4):1029–1035. [DOI] [PubMed] [Google Scholar]
- 3. Meldrum BS, Horton RW. Physiology of status epilepticus in primates. Arch Neurol. 1973;28(1):1–9. [DOI] [PubMed] [Google Scholar]
- 4. Meldrum BS, Brierley JB. Prolonged epileptic seizures in primates. Ischemic cell change and its relation to ictal physiological events. Arch Neurol. 1973;28(1):10–17. [DOI] [PubMed] [Google Scholar]
- 5. Meldrum BS, Vigouroux RA, Brierley JB. Systemic factors and epileptic brain damage. Prolonged seizures in paralyzed, artificially ventilated baboons. Arch Neurol. 1973;29(2):82–87. [DOI] [PubMed] [Google Scholar]
- 6. Varelas PN, Mirski MA. Status epilepticus. Curr Neurol Neurosci Rep. 2009;9:469–476. [DOI] [PubMed] [Google Scholar]
- 7. Brophy GM, Bell R, Claassen J. et al. Guidelines for the evaluation and management of status epilepticus. Neurocrit Care. 2012;17(1):3–23. [DOI] [PubMed] [Google Scholar]
- 8. Chamberlain JM, Okada P, Holsti M. et al. Lorazepam vs diazepam for pediatric status epilepticus: a randomized clinical trial. JAMA. 2014;311(16):1652–1660. [DOI] [PubMed] [Google Scholar]
- 9. Agency for Healthcare Research and Quality. NIS Overview [online]. https://www.hcup-us.ahrq.gov/nisoverview.jsp. [DOI] [PubMed]
- 10. Murthy SB, Merkler AE, Omran SS. et al. Outcomes after intracerebral hemorrhage from arteriovenous malformations. Neurology. 2017;88(20):1882–1888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Benchimol EI, Smeeth L, Guttmann A. et al. The REporting of studies Conducted using Observational Routinely-collected health Data (RECORD) statement. PLoS Med. 2015;12(10): e1001885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Walkey AJ, Hammill BG, Curtis LH, Benjamin EJ. Long-term outcomes following development of new-onset atrial fibrillation during sepsis. Chest. 2014;146(5):1187–1195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Urtecho J, Snapp M, Sperling M. et al. Hospital mortality in primary admissions of septic patients with status epilepticus in the United States*. Crit Care Med. 2013;41(8):1853–1862. [DOI] [PubMed] [Google Scholar]
- 14. Dham BS, Hunter K, Rincon F. The epidemiology of status epilepticus in the United States. Neurocrit Care. 2014;20(3):476–483. [DOI] [PubMed] [Google Scholar]
- 15. Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40(5):373–383. [DOI] [PubMed] [Google Scholar]
- 16. Deyo RA, Cherkin DC, Ciol MA. Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases. J Clin Epidemiol. 1992;45(6):613–619. [DOI] [PubMed] [Google Scholar]
- 17. Walcott BP, Kamel H, Castro B, Kimberly WT, Sheth KN. Tracheostomy after severe ischemic stroke: a population-based study. J Stroke Cerebrovasc Dis. 2014;23(5):1024–1029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. De Coster C, Li B, Quan H. Comparison and validity of procedures coded With ICD-9-CM and ICD-10-CA/CCI. Med Care. 2008;46(6):627–634. [DOI] [PubMed] [Google Scholar]
- 19. Lahiri S, Mayer SA, Fink ME. et al. Mechanical Ventilation for Acute Stroke: A Multi-state Population-Based Study. Neurocrit Care. 2015;23(1):28–32. [DOI] [PubMed] [Google Scholar]
- 20. Betjemann JP, Josephson SA, Lowenstein DH, Burke JF. Trends in Status Epilepticus-Related Hospitalizations and Mortality: redefined in US Practice Over Time. JAMA Neurol. 2015;72(6):650–655. [DOI] [PubMed] [Google Scholar]
- 21. Silbergleit R, Durkalski V, Lowenstein D. et al. Intramuscular versus intravenous therapy for prehospital status epilepticus. N Engl J Med. 2012;366:591–600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Vohra TT, Miller JB, Nicholas KS. et al. Endotracheal intubation in patients treated for prehospital status epilepticus. Neurocrit Care. 2015;23(1):33–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Glauser T, Shinnar S, Gloss D. et al. Evidence-based guideline: treatment of convulsive status epilepticus in children and adults: Report of the Guideline Committee of the American Epilepsy Society. Epilepsy Curr. 2016;16(1):48–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Logroscino G, Hesdorffer DC, Cascino GD, Annegers JF, Bagiella E, Hauser WA. Long-term mortality after a first episode of status epilepticus. Neurology. 2002;58(4):537–541. [DOI] [PubMed] [Google Scholar]
- 25. DeLorenzo RJ, Towne AR, Pellock JM, Ko D. Status epilepticus in children, adults, and the elderly. Epilepsia. 1992;33(Suppl 4): S15–S25. [DOI] [PubMed] [Google Scholar]
- 26. Neligan A, Shorvon SD. Prognostic factors, morbidity and mortality in tonic-clonic status epilepticus: a review. Epilepsy Res. 2011;93(1):1–10. [DOI] [PubMed] [Google Scholar]
- 27. Ney JP, van der Goes DN, Nuwer MR, Nelson L, Eccher MA. Continuous and routine EEG in intensive care: utilization and outcomes, United States 2005-2009. Neurology. 2013;81(23):2002–2008. [DOI] [PMC free article] [PubMed] [Google Scholar]