Abstract
Objective:
Although patient satisfaction is increasingly used to rate hospitals, it is unclear how patient satisfaction is associated with health outcomes. We sought to define the relationship of self-reported patient satisfaction and health outcomes.
Design:
Retrospective cross-sectional analysis using regression analyses and generalized linear modeling.
Setting:
Utilizing the Medical Expenditure Panel Survey Database (2010-2014), patients who had responses to survey questions related to satisfaction were identified.
Participants:
Among the 9166 patients, representing 106 million patients, satisfaction was rated as optimal (28.2%), average (61.1%), and poor (10.7%). Main Outcome Measures: We sought to define the relationship of self-reported patient satisfaction and health outcomes.
Results:
Patients who were younger, male, black/African American, with Medicaid insurance, as well as patients with lower socioeconomic status were more likely to report poor satisfaction (all P < .001). In the adjusted model, physical health score was not associated with an increased odds of poor satisfaction (1.42 95% confidence interval [CI]: 0.88-2.28); however, patients with a poor mental health score or ≥2 emergency department visits were more likely to report poor overall satisfaction (3.91, 95% CI: 2.34-6.5; 2.24, 95% CI: 1.48-3.38, respectively).
Conclusion:
Poor satisfaction was associated with certain unmodifiable patient-level characteristics, as well as mental health scores. These data suggest that patient satisfaction is a complex metric that can be affected by more than provider performance.
Keywords: patient satisfaction, health-care outcomes, provider performance
Introduction
Published in 2001 by the Institute of Medicine, Crossing the Quality Chasm: A New Health System for the 21st Century developed a framework including 6 goals that encouraged health systems to provide safe, effective, patient-centered, timely, efficient, and equitable care (1). Although there are a variety of ways to interpret and assess patient-centered care, the goal of patient “centeredness” has led to the widespread mandatory introduction of patient satisfaction surveys. For example, the Hospital Consumer Assessment of Healthcare Providers and Systems (HCAHPS) survey has been introduced as part of hospital value–based purchasing and is tied to hospital reimbursement (2). Additionally, public reporting of satisfaction is advocated to help patients choose where to obtain their health care (3). In fact, patient satisfaction data have increasingly been used by patients and payors both in the United States and abroad as a metric to assess hospital quality and rate hospital performance (2 –6).
Patient satisfaction is increasingly used as a method to rate, rank, and compare hospitals. Several studies across a wide variety of medical specialties have reported that a multitude of factors influence patients’ perception of their care (4 –6). It is unclear, however, how patient satisfaction is associated with health outcomes and how patient-level factors affect patient satisfaction. Kaye et al noted a possible relationship between high patient satisfaction and improved outcomes in some patient populations (7). In a separate study, Cowen et al suggested a potential interrelationship between patient mortality risk and patient satisfaction and outcomes (8). However, few studies have specifically examined the association of self-reported patient satisfaction scores with a broad range of health outcome metrics. In addition, little data exist on the relationship between baseline patient-level characteristics (eg, sex, education level, socioeconomic status, etc), health-care outcomes (eg, physical and mental health, emergency room utilization, expenditures, etc), and self-reported satisfaction. Information on the underlying factors associated with patient satisfaction may allow for a more targeted approach to improving the patient experience. As such, we sought to define the relationship of self-reported patient satisfaction and health outcomes in a large, nationally representative cohort of patients. In addition, we sought to characterize how patient-level factors impact patient reported satisfaction and, in turn, health-care outcomes.
Methods
The Medical Expenditure Panel Survey
Data were obtained from the Medical Expenditure Panel Survey (MEPS) data sets, which are sponsored by the Agency for Healthcare Research and Quality (AHRQ). The Household Component (MEPS-HC), one of the major components of the MEPS, is reported annually and is based on that entire year’s results. Following data collection, person weights and variance estimation stratum as recommended by the AHRQ were applied to represent an estimate of people on the US population level. Each individual is uniquely identified by a combination of person number and dwelling units generated by the AHRQ. The full-year consolidated file, the medical conditions file, and prescribed medicines file from the MEPS-HC were merged using the unique person-level identifiers for each year from 2010 to 2014. This study was considered exempt by institutional review board of The Ohio State Wexner Medical Center.
Study Population
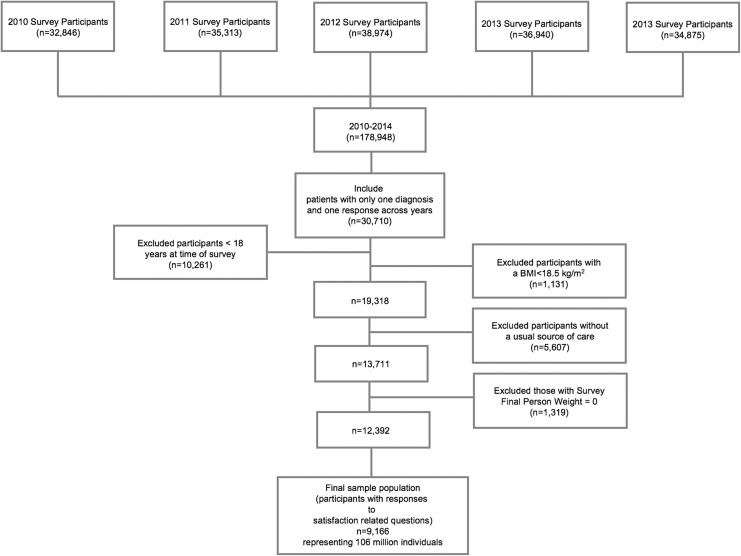
Data from 2010 to 2014 in MEPS were reviewed. Eligible individuals included patients who had a diagnosis of psychiatric, hepato-pancreato-biliary (HPB), gastrointestinal (GI; including malignancy of GI tract), cardiovascular, endocrine/metabolic, pulmonary, renal/genitourinary (GU)/gynecology (GYNE), or hematologic (including hematologic malignancy) diseases. Clinical classifications were categorized based on International Classification of Diseases, Ninth Revision condition and V codes, which were then collated to create 8 groups of disease categories (Supplemental Table 1). Individuals who were <18 years old, had a body mass index <18.5 kg/m2, lacked a usual source of care, and had a final survey person weight ≤0 or missing were excluded (Figure 1). Only patients who had responses to the satisfaction/overall rating of health-care providers were retained in the final analytic cohort. No institutional review board approval was required for this study as MEPS is a deidentified, publicly available data set.
Figure 1.
Flowchart of study participant selection process.
Study Outcomes
The influence of patient satisfaction was analyzed relative to a broad range of health outcomes, including the patient-reported health outcomes collected from responses to questions on Short-Form 12 version 2, quality of care indicators, utilization of health-care resources, and annual health-care costs.
The MEPS full-year consolidated file provides a summary mental health score (MHS) and physical health score (PHS), from the worst health status (0) to the best health status (100). These summary scores were divided into quartiles and stratified with the lowest quartile categorized as poor MHS/PHS. Utilization of health-care resources pooled from the MEPS full-year consolidated file was represented by several variables, including the number of emergency room visits, the number of inpatient hospital stays, and the annual health-care expenditures. An increased utilization of health-care resource was defined as ≥2 emergency room visits or ≥2 hospital discharges (1). Both annual health-care expenditure and out-of-pocket expenditure, obtained from the MEPS full-year consolidated file, were summed across the calendar year. Annual health-care expenditure was defined as total payments, including both out-of-pocket payments and payments made on behalf of the patient by insurance companies or other payer groups. Out-of-pocket expenditure was the amount of money paid by patients themselves.
Independent Variables (Satisfaction/Overall Rating of Health-Care Providers)
A satisfaction score was obtained from patient responses to the question assessing satisfaction. The question employed to derive a satisfaction score was “rating of health care from all doctors and other health providers” ranging from the worst health-care possible (0) to the best health-care possible (10). The overall satisfaction score was categorized as “poor” (0-6 total points), “average” (7-9 total points), and “optimal” (10 total points).
Statistical Analysis
A survey-based analysis approach was used to represent the nationwide estimates of the US civilian noninstitutionalized adult population after accounting for person weights and variance estimations. The χ2 test was used to estimate robustly the relative differences in sociodemographic factors across satisfaction categories among the eligible population. Unadjusted and adjusted logistic regression models were used to adjust for age, gender, race/ethnicity, clinical disease categories, insurance, level of education, level of income, region, and the modifiable risk factors for the final model. Level of income was categorized by using the proportion of the federal poverty level as poor (<125%), low (125%-200%), middle (200%-400%), and high income (≥400%). Smoking status, obesity (body mass index ≥30 kg/m2), diabetes, high blood pressure, and high cholesterol, as well as whether the participant reported a half hour or more in moderate to vigorous physical activity at least 3 to 5 times a week, were also analyzed. Two-part logistic regression models were employed to estimate the mean annual health-care expenditure and out-of-pocket expenditure. Data were reported using 95% confidence intervals (CIs), odds ratios (ORs), and 2-sided P values <.05 to assess for significance. All statistical analysis was performed with STATA 14.0 software.
Results
Cohort Characteristics
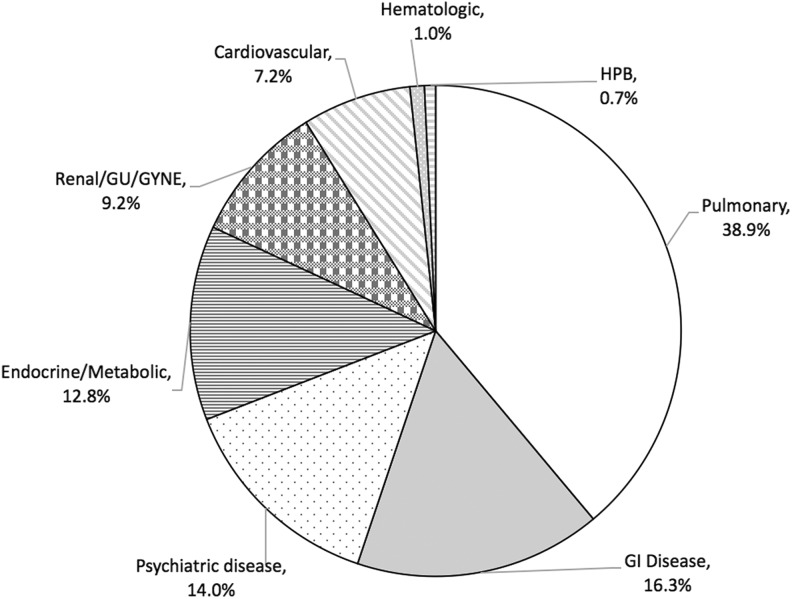
The total cohort consisted of 9166 participants representing 106 million noninstitutionalized US adults. The median age of the participants was 48 ± 17 years, and most patients were female (55%). The majority of patients were white (71.2%), followed by Hispanic (11.2%), black/African American (10.3%), Asian (5%), and others (2.5%). The most frequent diagnosis was pulmonary disease (38.9%) followed by GI disease (16.3%), psychiatric disease (14.0%), endocrine/metabolic disease (12.8%), renal/GU/GYNE (9.2%), cardiovascular (7.2%), hematologic (1.0%), and HPB (0.7%; Figure 2). Overall, 47.3% of the study participants were categorized as high income, while 12.1% were categorized as poor. Most patients had private insurance (76.5%), while 6.7%, 6.1%, and 10.5% patients had no insurance, Medicaid, or Medicare, respectively. Most participants had an associate/bachelor degree (45.4%), whereas 10.6% patients reported no high school diploma.
Figure 2.
Distribution of eligible patients with one diagnosis from 2010 to 2014 across the United States.
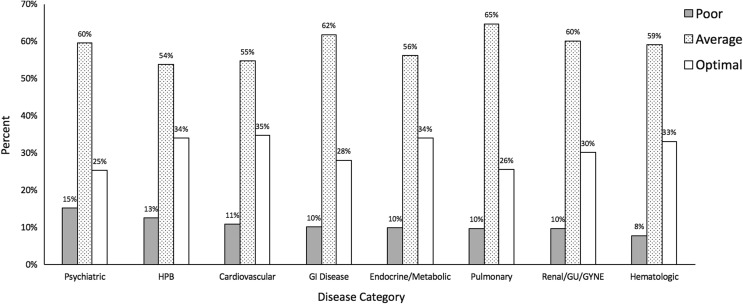
Overall patient characteristics across different patient satisfaction level are described in Table 1. In assessing self-reported satisfaction, 10.7% of patients reported satisfaction as poor, while 61.1% and 28.2% patients reported satisfaction as average or optimal, respectively. Patients who were younger (12.5%), poorer (17.5%), black/African American (14.4%), male patients (11.3%), with Medicaid (21.9%) and individuals with no degree (13.8%) were more likely to report poor satisfaction (all P < .001). Patients with psychiatric disease were also most likely to report poor satisfaction (15.2%), followed by patients with HPB (12.5%) and cardiovascular (10.8%) diseases (Figure 3).
Table 1.
Weighted Sample Characteristics of US Patients Aged 18 Years and Older.
| Variable | Satisfaction | |||
|---|---|---|---|---|
| Optimal | Average | Poor | P Value | |
| N | 2640 | 5407 | 1119 | |
| Weighted sample | 29 780 958 | 64 532 650 | 11 286 538 | |
| Age groups, years (%) | ||||
| 18-39 | 22.8 | 64.7 | 12.5 | <.001 |
| 40-64 | 26.3 | 62.9 | 10.8 | |
| ≥65 | 42.9 | 50.2 | 7.0 | |
| Sex (%) | ||||
| Male | 25.1 | 63.6 | 11.3 | <.001 |
| Female | 30.7 | 59.1 | 10.2 | |
| Race/ethnicity (%) | ||||
| White/Caucasian | 28.1 | 62.2 | 9.7 | <.001 |
| Black/African American | 30.6 | 55.0 | 14.4 | |
| Asian/Pacific Islander | 17.7 | 69.9 | 12.5 | |
| Hispanic | 31.4 | 56.2 | 12.4 | |
| Other | 26.9 | 69.4 | 13.7 | |
| Insurance status (%) | ||||
| Uninsured | 23.3 | 55.7 | 21.0 | <.001 |
| Private | 26.7 | 64.5 | 8.9 | |
| Medicaid | 27.4 | 50.7 | 21.9 | |
| Medicare | 43.1 | 46.5 | 10.5 | |
| Others (public only) | 10.2 | 56.2 | 33.6 | |
| Level of income (%) | ||||
| Poor | 29.9 | 52.6 | 17.5 | <.001 |
| Low income | 32.2 | 52.4 | 15.5 | |
| Middle income | 28.8 | 60.4 | 10.8 | |
| High income | 26.5 | 65.8 | 7.8 | |
| Region (%) | ||||
| Northeast | 28.8 | 61.1 | 10.1 | .416 |
| Midwest | 28.1 | 61.2 | 10.8 | |
| South | 29.5 | 59.6 | 10.9 | |
| West | 25.9 | 63.2 | 10.8 | |
| Education (%) | ||||
| No degree | 34.4 | 51.8 | 13.8 | <.001 |
| GED/high school diploma | 32.1 | 55.6 | 12.2 | |
| Associate degree/bachelor | 24.3 | 66.1 | 9.7 | |
| Above bachelor | 28.4 | 63.7 | 7.9 | |
| Disease category (%) | ||||
| Psychiatric | 25.3 | 59.5 | 15.2 | <.001 |
| HPB | 33.9 | 53.7 | 12.5 | |
| Cardiovascular | 34.7 | 54.6 | 10.8 | |
| Gastrointestinal disease (including malignancy of GI tract) | 28.1 | 61.7 | 10.1 | |
| Endocrine/metabolic | 33.9 | 56.1 | 9.9 | |
| Pulmonary | 25.5 | 64.7 | 9.8 | |
| Renal/GU/GYNE | 30.1 | 60.1 | 9.8 | |
| Hematologic (including hematologic malignancy) | 33.1 | 59.0 | 7.9 | |
Abbreviations: GI, gastrointestinal; GU, genitourinary; GYNE, gynecology; GED, General Education Diploma.
Bold shows values of statistical significance.
Figure 3.
Distribution of satisfaction across disease categories.
Patient-Specific Factors Associated With Self-Reported Satisfaction Scores
Patients who had a poor PHS or MHS were more likely to self-report poor satisfaction. In fact, 18.1% patients who had a poor PHS reported poor satisfaction (poor PHS vs non-poor PHS: 18.1% vs 10.4%), while 40.1% with a poor MHS rated their satisfaction as poor (poor MHS vs non-poor MHS: 40.1% vs 10.2%; both P <.001). Patients with poor satisfaction were also more likely to report a poor PHS (5.2%) and a poor MHS (5.6%) compared with patients who reported optimal satisfaction (both P < .001; Table 2). On both unadjusted and adjusted regression analyses, self-reported poor satisfaction was associated with an increased likelihood of a poor MHS (adjusted OR: 3.91, 95% CI: 2.34-6.51). However, there was no association between self-reported quality of satisfaction and the physical health status of patients (OR: 1.42, 95% CI: 0.88-2.28; Table 3). Older patients were more likely to report their physical health component as poor (OR [40-64]: 3.62, 95% CI: 1.11-5.89; OR [≥65]: 3.42, 95% CI: 1.53-7.65). Similarly, there was a consistent inverse relationship between the level of income and poor self-reported physical health status (OR of poor vs high income: 1.79, 95% CI: 1.10-2.91). Compared with participants who had private insurance, individuals with Medicaid (OR: 2.43, 95% CI: 1.30-4.56) or Medicare (OR: 3.32, 95% CI: 1.94-5.66) were more likely to have a poor PHS (Table 4).
Table 2.
Variation in Health-Reported Outcomes Across Satisfaction Responses Among US Adults Aged 18 Years and Older With Established Diseases.
| Variable | Satisfaction | |||
|---|---|---|---|---|
| Optimal | Average | Poor | P Value | |
| Patient-reported outcomes | ||||
| SF-12 physical health score (poor), % (95% CI) | 3.4 (2.6-4.5) | 2.5 (2.1-3.1) | 5.2 (3.8-7.1) | <.001 |
| SF-12 mental health score (poor % [95% CI]) | 1.0 (0.7-1.5) | 1.0 (0.7-1.3) | 5.6 (4.2-7.4) | <.001 |
| Health-care resource utilization | ||||
| ≥2 emergency department visits (yes % [95% CI]) | 2.3 (1.8-3.0) | 2.3 (1.8-2.8) | 5.8 (4.2-7.9) | <.001 |
| ≥2 inpatient hospital stays (yes % [95% CI]) | 1.0 (0.7 -1.7) | 0.9 (0.6 -1.2) | 0.6 (0.3 -1.1) | .339 |
| Annual healthcare expenditure | ||||
| Unadjusted mean annual health-care expenditures in dollars (95% CI) | $4 867 ($4,226-$5,507) |
$4 290 ($3,994-$4,585) |
$4 467 ($3 774-$5,161) |
.241 |
| Annual out-of-pocket expenditure | ||||
| Unadjusted mean cost in dollars (95% CI) | $677 ($609-$745) |
$739 ($682-$797) |
$748 ($589-$906) |
.493 |
Abbreviation: CI, confidence interval.
$ represents US$. Bold shows values of statistical significance.
Table 3.
Odds Ratios for Health Outcomes Using Satisfaction and Other Covariates as Explanatory Variables Among US Adults Aged 18 Years and Older With Established Diseases, Medical Expenditure Panel Survey 2010 to 2014.
| Variable | Satisfaction | ||
|---|---|---|---|
| Optimal | Average | Poor | |
| Patient-reported outcomes | |||
| SF-12 physical health score (OR of poor PHS [95% CI]) | |||
| Model 1 | Ref | 0.73 (0.53-1.01) | 1.55 (1.01-2.36) |
| Model 2 | Ref | 1.06 (0.76 -1.49) | 1.42 (0.88-2.28) |
| SF-12 mental health score (OR of poor MHS [95% CI]) | |||
| Model 1 | Ref | 0.97 (0.61-1.54) | 5.77 (3.48-9.55) |
| Model 2 | Ref | 1.00 (0.63-1.61) | 3.91 (2.34-6.51) |
| Health-care resource utilization | |||
| OR of ≥2 emergency department visits (95% CI) | |||
| Model 1 | Ref | 0.97 (0.68-1.40) | 2.66 (1.70-3.93) |
| Model 2 | Ref | 1.17 (0.80-1.71) | 2.24 (1.48-3.38) |
| OR of ≥2 inpatient hospital stay (95% CI) | |||
| Model 1 | Ref | 0.81 (0.45-1.43) | 0.50 (0.21-1.17) |
| Model 2 | Ref | 0.99 (0.56-1.77) | 0.54 (0.24-1.24) |
Abbreviations: CI, confidence interval; OR, odds ratio.
Bold shows values of statistical significance.
Note: Model 1 is the unadjusted model. In the adjusted analysis (Model 2), we included age, gender, region, race/ethnicity, income level, education, insurance status, disease category and modifiable risk factors (smoking status, obesity (BMI ≥30 kg/m2), diabetes, high blood pressure, and high cholesterol, as well as whether the participant spends a half hour or more in moderate to vigorous physical activity at least three to five times a week).
Table 4.
Odds Ratios for Patient-Reported Physical Health Status by Patient Characteristics Among US Adults Aged 18 Years and Older With Established Diseases, Medical Expenditure Panel Survey 2010 to 2014.a
| PHS Rated as Poor | ||
|---|---|---|
| Odds Ratio | 95% CI | |
| Level of satisfaction | ||
| Optimal | Reference | Reference |
| Average | 1.06 | 0.76-1.49 |
| Poor | 1.42 | 0.88-2.28 |
| Age groups, years | ||
| 18-39 | Reference | Reference |
| 40-64 | 3.62 | 2.22-5.89 |
| ≥65 | 3.42 | 1.53-7.65 |
| Sex | ||
| Male | Reference | Reference |
| Female | 0.97 | 0.73 -1.29 |
| Race/ethnicity | ||
| White/Caucasian | Reference | Reference |
| Black/African American | 1.02 | 0.69 -1.51 |
| Asian/Pacific Islander | 0.9 | 0.50 -1.65 |
| Hispanic | 0.69 | 0.45 -1.05 |
| Other | 0.72 | 0.30 -1.72 |
| Insurance status | ||
| Private | Reference | Reference |
| Uninsured | 1.14 | 0.56-2.30 |
| Medicaid | 2.43 | 1.30-4.56 |
| Medicare | 3.32 | 1.94-5.66 |
| Income status | ||
| High income | Reference | Reference |
| Middle income | 1.29 | 0.88 -1.88 |
| Low income | 2.25 | 1.32-3.83 |
| Poor | 1.79 | 1.10-2.91 |
| Region | ||
| Northeast | Reference | Reference |
| Midwest | 0.88 | 0.52 -1.49 |
| South | 0.76 | 0.49 -1.18 |
| West | 1.3 | 0.49 -1.18 |
| Education | ||
| No degree | Reference | Reference |
| GED/high school diploma | 1.01 | 0.73-1.41 |
| Associate degree/bachelor | 0.69 | 0.45-1.05 |
| Above bachelor | 0.76 | 0.40-1.44 |
| Disease category | ||
| HPB | Reference | Reference |
| Psychiatric | 0.51 | 0.08-3.24 |
| GI (including malignancy of GI tract) | 0.49 | 0.08-3.16 |
| Cardiovascular | 0.77 | 0.12-4.97 |
| Endocrine/metabolic | 0.55 | 0.08-3.84 |
| Pulmonary | 0.43 | 0.07-2.76 |
| Renal/GU/GYNE | 0.44 | 0.06-3.03 |
| Hematologic (including hematologic malignancy) | 0.56 | 0.08-3.84 |
Abbreviations: HPB, hepato-pancreato-biliary; GI, gastrointestinal; GU, genitourinary; GYNE, gynecology; PHS, SF-12 physical health score; GED, General Education Diploma.
Bold shows values of statistical significance.
aWe also adjusted for disease category and modifiable risk factors (smoking status, obesity with body mass index (BMI) ≥30 kg/m2, diabetes, high blood pressure, and high cholesterol, as well as whether the participant spends a half hour or more in moderate to vigorous physical activity at least 3 to 5 times a week).
Satisfaction level was not associated with health-care utilization factors, with the exception of emergency room use, as 5.8% of participants with poor satisfaction reported 2 or more emergency department visits (P < .001). Furthermore, patients with poor satisfaction were more likely to report 2 or more emergency department visits after adjusting for other covariates (OR: 2.24, 95% CI: 1.48-3.38; Table 2). Patients with a poor satisfaction were not, however, more likely to report 2 or more inpatient stays in the survey year (OR: 0.54, 95% CI: 0.24-1.24; Table 3). Inpatient hospital stay was associated with clinical diagnosis (Table 5). For example, compared with patients who had an HPB diagnosis, individuals diagnosed with psychiatric (OR: 0.11, 95% CI: 0.02-0.51), GI (OR: 0.12, 95% CI: 0.03-0.55), endocrine/metabolic (OR: 0.06, 95% CI: 0.01-0.42), pulmonary (OR: 0.04, 95% CI: 0.01-0.21), or renal (OR: 0.11, 95% CI: 0.02-0.57) diseases were less likely to report an increased utilization of inpatient hospital stay. Moreover, the quality of satisfaction was not associated with either overall annual health-care expenditure or out-of-pocket expenditure (both P > .05). The average annual health-care expenditure was USD$4,471 per year and average out-of-pocket expenditure was USD$735 per year across 2010 to 2014 (Table 2).
Table 5.
Odds Ratios for Inpatient Hospital Stay by Patient Characteristics Among US Adults Aged 18 Years and Older With Established Diseases, Medical Expenditure Panel Survey 2010 to 2014.
| Variable | ≥2 Inpatient Hospital Stay | |
|---|---|---|
| Odds Ratio | 95% CI | |
| Level of satisfaction | ||
| Optimal | Reference | Reference |
| Average | 0.99 | 0.56 -1.77 |
| Poor | 0.54 | 0.24 -1.24 |
| Age groups, years | ||
| 18-39 | Reference | Reference |
| 40-64 | 0.95 | 0.49 -1.83 |
| ≥65 | 1.28 | 0.47-3.47 |
| Sex | ||
| Male | Reference | Reference |
| Female | 0.74 | 0.41 -1.33 |
| Race/ethnicity | ||
| White/Caucasian | Reference | Reference |
| Black/African American | 1.01 | 0.52 -1.96 |
| Asian/Pacific Islander | 1.83 | 0.63-5.36 |
| Hispanic | 1.07 | 0.51-2.24 |
| Other | 3.87 | 1.56-9.60 |
| Insurance status | ||
| Private | Reference | Reference |
| Uninsured | 0.4 | 0.11 -1.50 |
| Medicaid | 1.42 | 0.61-3.30 |
| Medicare | 1.34 | 0.53-3.35 |
| Income status | ||
| High income | Reference | Reference |
| Middle income | 1.69 | 0.79-3.61 |
| Low income | 1.61 | 0.74-3.49 |
| Poor | 1.51 | 0.68-3.36 |
| Region | ||
| Northeast | Reference | Reference |
| Midwest | 1.08 | 0.51-2.27 |
| South | 1.13 | 0.54-2.36 |
| West | 0.88 | 0.43 -1.81 |
| Education | ||
| No degree | Reference | Reference |
| GED/high school diploma | 0.9 | 0.38-2.13 |
| Associate degree/bachelor | 0.61 | 0.23 -1.60 |
| Above bachelor | 0.62 | 0.19-2.00 |
| Disease category | ||
| HPB | Reference | Reference |
| Psychiatric | 0.11 | 0.02-0.51 |
| GI (including malignancy of GI tract) | 0.12 | 0.03-0.55 |
| Cardiovascular | 0.39 | 0.09 -1.78 |
| Endocrine/metabolic | 0.06 | 0.01-0.42 |
| Pulmonary | 0.04 | 0.01-0.21 |
| Renal/GU/GYNE | 0.11 | 0.02-0.57 |
| Hematologic (including hematologic malignancy) | 0.24 | 0.02-2.65 |
Abbreviations: BMI, body mass index; CI, confidence interval; HPB, hepato-pancreato-biliary; GI, gastrointestinal; GU, genitourinary; GYNE, gynecology; GED, General Education Diploma.
aWe also adjusted for disease category and modifiable risk factors (smoking status, obesity with body mass index (BMI) ≥30 kg/m2, diabetes, high blood pressure, and high cholesterol, as well as whether the participant spends a half hour or more in moderate to vigorous physical activity at least 3 to 5 times a week).
Discussion
Patient satisfaction has been recognized as an important metric of health-care quality.(9,10) In fact, the HCAHPS survey is now a part of hospital value–based purchasing and is tied to hospital reimbursement.(11) Furthermore, in some institutions, provider-specific HCAHPS survey data are used to assess and measure individual physician “quality,” as well as in some circumstances, determine quality-based bonuses. Public reporting of provider and institution satisfaction data is often utilized by patients and referral networks to choose where to obtain health care.(3) Information on how self-reported satisfaction tracks with patient-level factors, as well as patient health-care outcome metrics, has, however, been lacking. The current study is important because it examined the association of self-reported satisfaction with baseline patient-level characteristics (eg, sex, education level, socioeconomic status, etc), as well as health-care outcomes (eg, physical and mental health, emergency department utilization, expenditures, etc). Of note, several baseline patient characteristics were associated with an increased odds of poor patient satisfaction including age, race, level of income, insurance, and education status. In addition, while satisfaction was not associated with PHS, patients with poor satisfaction were more likely to report a poor MHS and increased emergency department utilization.
Patient satisfaction is often proposed as measure of provider performance (10). However, data from the current study would strongly suggest that patient-specific characteristics that are independent of provider performance also impact satisfaction.
For example, self-reported patient satisfaction was strongly associated with “fixed” patient characteristics such as age, sex, race, and socioeconomic status as these factors were related to the satisfaction level that patients reported. Specifically, there was an incremental increase in patient satisfaction associated with increased socioeconomic status and education level. Interestingly, age was also associated with the odds of reporting poor patient satisfaction—with younger patients being more likely to report poor satisfaction. Although the reasons for these patient-level differences are likely multifactorial, variations in self-reported satisfaction may be related to different patient expectations and perceptions of care. To this point, several theories have been proposed to conceptualize the concept of patient satisfaction (12 –14). For example, the fulfillment theory defines satisfaction as the perceived difference between what is expected and what is received (15). In contrast, the equity and social comparison theory conceptualizes satisfaction as perceived equity—that is, a direct comparison of the care a patient received relative to their perception of the care delivered to others (15). As such, patient-level factors such as age/generation, race/culture, and education level may directly and meaningfully impact perceptions of satisfaction based on how “satisfaction” may be conceptualized differently among certain patient populations. In turn, results of patient satisfaction surveys such as HCAHPS need to be interpreted not only in light of provider performance but also the specific patient population being served.
Patients with poor satisfaction were more likely to report a poor MHS. Previous studies have similarly highlighted the important interplay between mental health and self-reported patient satisfaction. In particular, some providers of psychiatric care have expressed skepticism about the validity and utility of satisfaction surveys among patients with mental health concerns (16 –18). It is possible that patients with poor MHS may be generally less satisfied with matters both related and unrelated to health care. In addition, varying levels of insight into one’s own care may complicate the measurement of self-reported satisfaction (18 –20). Although mental health status may impact how data on self-reported satisfaction are interpreted, it doesn’t invalidate these data. Rather, there is evidence that satisfaction surveys are still applicable to patients with low MHS as patients are still able to articulate if and to what extent they are satisfied (21). Poor insight, though, may frequently prevent these patients from identifying why they are satisfied or articulating a coherent rationale for their satisfaction ratings (20). Collectively, the data serve to highlight that—in addition to baseline patient demographic characteristics—other patient-level factors such as mental health status can directly impact patient self-reported satisfaction scores. In turn, when interpreting data on patient satisfaction, information on patient mental status also needs to be assessed to provide the appropriate context.
Given the rising cost of health care, there has been considerable interest in better understanding and identifying the drivers of overall health-care utilization. Although the impact of patient satisfaction on health-care utilization has not been well studied, several studies have suggested an association (22 –24). Of note, patient satisfaction was based on responses to 5 survey questions including one related directly to patient satisfaction and 4 related to a patient’s evaluation of patient–provider communication. In the current study, we similarly noted that patient satisfaction was associated with emergency department utilization. Specifically, patients who rated their satisfaction as poor were more than twice as likely to report 2 or more emergency department visits a year. Of note, even after adjusting for other covariates, the association of patient satisfaction and emergency department utilization remained. One plausible explanation could be that patients who are dissatisfied with their health-care providers end up seeking medical care in the emergency department rather than in the outpatient clinic. Of note, in contrast to the study by Fenton et al.,(6) we did not note an association of patient satisfaction and inpatient stay or overall health-care expenditures. These disparate results may be related to differences in how patient satisfaction was defined, as well as variations in statistical modeling.
Several limitations should be considered when interpreting data from the current study. Given that patient satisfaction was based on the MEPS survey, the data were subject to recall bias. Patients included in the MEPS database were also not tracked longitudinally over time. Additionally, the MEPS database contains limited variables and some variables that might have had an impact on patient satisfaction and outcomes, such as patient comorbidities contributing to mortality risk, were not included (8). Data were also exclusively derived from patients in the United States who were noninstitutionalized. Therefore, data from the current study cannot necessarily be generalized to other populations. It is important to note, however, that the MEPS database is generally accepted as the “best” source of patient-reported data on their health-care experience.
In conclusion, up to 1 in 10 patients self-reported satisfaction with their health-care experience as poor. Poor satisfaction was associated with certain unmodifiable patient-level characteristics such as age, sex, and race. Other baseline characteristics such as socioeconomic status and education level also impacted the odds of a patient rating their satisfaction as poor. In addition, MHS similarly was associated with the odds of patient self-reporting a poor satisfaction score. These data strongly suggest that patient satisfaction is a complex metric that can be dramatically affected by more than provider performance. The rating, ranking, and comparison of providers and hospitals using satisfaction scores need to be considered in light of these data. Other metrics such as patient activation and patient engagement will need to be incorporated into future assessments of the patient–provider experience to better assess and evaluate patient “centeredness” in the clinical setting.
Supplemental Material
Supplemental_Table_1_(1) for The Association Between Patient Satisfaction and Patient-Reported Health Outcomes by Qinyu Chen, Eliza W Beal, Victor Okunrintemi, Emily Cerier, Anghela Paredes, Steven Sun, Griffin Olsen and Timothy M Pawlik in Journal of Patient Experience
Author Biographies
Qinyu Chen, MHS, is a biostatistician at the Ohio State University Wexner Medical Center in the Division of Surgical Oncology, Department of General Surgery.
Eliza W Beal, MD, MS, obtained her BS at the University of Michigan and MD and MS at the Ohio State University. She is a general surgery resident and postdoctoral research fellow in the Division of Surgical Oncology, Department of Surgery, The Ohio State University Wexner Medical Center.
Victor Okunrintemi, MD, MPH, was born and raised in Nigeria. He attended medical school at Usmanu Danfodiyo University, Sokoto, Nigeria. He received his MPH from Johns Hopkins and completed a 2 year postdoctoral research fellowship at Baptist Health South Florida. He is currently an internal medicine resident at East Carolina University.
Emily Cerier, BS, MD, is a general surgery resident at Northwestern University.
Anghela Paredes, MD, is a general surgery resident and postdoctoral research fellow in the Division of Surgical Oncology, Department of Surgery, The Ohio State University Wexner Medical Center.
Steven Sun, MD, completed his undergraduate education at Washington University and medical school at the University of Michigan. He is a general surgery resident and postdoctoral research fellow in the Division of Surgical Oncology, Department of Surgery, The Ohio State University Wexner Medical Center.
Griffin Olsen, BA, MD, is a general surgery resident at UT Southwestern.
Timothy M. Pawlik, MD, MPH, PhD, is the Urban Meyer III and Shelley Meyer Chair for Cancer Research and Division of Surgical Oncology, Health Services Management and Policy as well as the Chair of the Department of Surgery at the Ohio State University Wexner Medical Center.
Footnotes
Authors’ Note: Qinyu Chen and Eliza W. Beal contributed equally to this work.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Supplemental Material: Supplemental material for this article is available online.
References
- 1. Committee on Quality Health Care in America IoM. Crossing the Quality Chasm: a New Health System for the 21st Century. Washington DC: National Academy Press; 2001. [Google Scholar]
- 2. Centers for Medicare & Medicaid Services (CMS), HHS. Medicare Program: Hospital Outpatient Prospective Payment and Ambulatory Surgical Center Payment Systems and Quality Reporting Programs; Organ Procurement Organization Reporting and Communication; Transplant Outcome Measures and Documentation Requirements; Electronic Health Record (EHR) Incentive Programs; Payment to Nonexcepted Off-Campus Provider-Based Department of a Hospital; Hospital Value-Based Purchasing (VBP) Program; Establishment of Payment Rates Under the Medicare Physician Fee Schedule for Nonexcepted Items and Services Furnished by an Off-Campus Provider-Based Department of a Hospital . Final rule with comment period and interim final rule with comment period. Fed Regist. 2016;81:79562–892. PubMed PMID: 27906530.eng. [PubMed] [Google Scholar]
- 3. Services CfMaM. Hospital Consumer Assessment of Healthcare Providers and Systems. Patients’ Perspectives of Care Survey. 2014. Retrieved September 25, 2014, from: https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/HospitalQualityInits/HospitalHCAHPS.html.
- 4. Kennedy GD, Tevis SE, Kent KC. Is there a relationship between patient satisfaction and favorable outcomes? Ann Surg. 2014;260:592–8; discussion 8–600. PubMed PMID:25203875. PMCID: PMC4159721. eng. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Kane RL, Maciejewski M, Finch M. The relationship of patient satisfaction with care and clinical outcomes. Med Care. 1997;35:714–30. PubMed PMID: 9219498. eng. [DOI] [PubMed] [Google Scholar]
- 6. Fenton JJ, Jerant AF, Bertakis KD, Franks P. The cost of satisfaction: a national study of patient satisfaction, health care utilization, expenditures, and mortality. Arch Intern Med. 2012;172:405–11. PubMed PMID: 22331982. [DOI] [PubMed] [Google Scholar]
- 7. Kaye DR, Richardson CR, Ye Z, Herrel LA, Ellimoottil C, Miller DC. Association between patient satisfaction and short-term outcomes after major cancer surgery. Ann Surg Oncol. 2017;24:3486–93. PubMed PMID: 28819930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Cowen ME, Czerwinski J, Kabara J, Blumenthal DU, Kheder S, Simmons S. The risk-outcome-experience triad: mortality risk and the Hospital Consumer Assessment of Healthcare Providers and systems survey. J Hosp Med. 2016;11:628–35. PubMed PMID: 27251217. [DOI] [PubMed] [Google Scholar]
- 9. Cleary PD, McNeil BJ. Patient satisfaction as an indicator of quality care. Inquiry. 1988;28:25–36. [PubMed] [Google Scholar]
- 10. Al-Abri R, Al-Balushi A. Patient satisfaction survey as a tool towards quality improvement. Oman Med J. 2014;29:3–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. HCAHPS: Patients’ Perspectives of Care Survey. Hospital Quality Initiative, Centers for Medicare & Medicaid Services. 2017. Available from: https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/HospitalQualityInits/HospitalHCAHPS.html. Accessed January 1, 2018.
- 12. Gill L, White L. A critical review of patient satisfaction. Leadership Health Ser. 2009;22:8–19. [Google Scholar]
- 13. Wagner D, Bear M. Patient satisfaction with nursing care: a concept analysis within a nursing framework. J Adv Nurs. 2009;65:692–701. [DOI] [PubMed] [Google Scholar]
- 14. Turris SA. Unpacking the concept of patient satisfaction: a feminist analysis. J Adv Nurs. 2005;50:293–8. [DOI] [PubMed] [Google Scholar]
- 15. Jaipaul CK, Rosenthal GE. Are older patients more satisfied with hospital care than younger patients? J Gen Intern Med. 2003;18:23–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Ortiz G. Examining patients’ perceptions of care to identify opportunities for quality improvement in psychiatric inpatient hospitals. Patient. 2014;7:301–12. [DOI] [PubMed] [Google Scholar]
- 17. Shipley K, Hilborn B, Hansell A, Tyrer J, Tyrer P. Patient satisfaction: a valid index of quality of care in a psychiatric service. Acta Psychiatr Scand. 2000;101:330–3. [PubMed] [Google Scholar]
- 18. Eisen SV, Wilcox M, Idiculla T, Speredelozzi A, Dickey B. Assessing consumer perceptions of inpatient psychiatric treatment: the perceptions of care survey. Jt Comm J Qual Improv. 2002;28:510–26. [DOI] [PubMed] [Google Scholar]
- 19. Nordon C, Rouillon F, Barry C, Gasquet I, Falissard B. Determinants of treatment satisfaction of schizophrenia patients: results from the ESPASS study. Schizophr Res. 2012;139:211–7. [DOI] [PubMed] [Google Scholar]
- 20. Bell M, Fiszdon J, Richardson R, Lysaker P, Bryson G. Are self-reports valid for schizophrenia patients with poor insight? Relationship of unawareness of illness to psychological self-report instruments. Psychiatry Res. 2007;151:37–46. [DOI] [PubMed] [Google Scholar]
- 21. Cort D, Sugarbaker D, Zeller S. What’s Driving Patient Satisfaction in Inpatient Hospitals? March 16 2015 https://www.psychiatryadvisor.com/practice-management/whats-driving-patient-satisfaction-in-inpatient-hospitals/article/403746/2/. Accessed January 1, 2018.
- 22. Greene J, Hibbard JH. Why does patient activation matter? An examination of the relationships between patient activation and health-related outcomes. J Gen Intern Med. 2012;27:520–6. PubMed PMID: 22127797. PMCID: PMC3326094. eng. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Greene J, Hibbard JH, Sacks R, Overton V, Parrotta CD. When patient activation levels change, health outcomes and costs change, too. Health Aff (Millwood). 2015;34:431–7. PubMed PMID: 25732493. eng. [DOI] [PubMed] [Google Scholar]
- 24. Hibbard JH, Greene J. What the evidence shows about patient activation: better health outcomes and care experiences; fewer data on costs. Health Aff (Millwood). 2013;32:207–14. PubMed PMID: 23381511. eng. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental_Table_1_(1) for The Association Between Patient Satisfaction and Patient-Reported Health Outcomes by Qinyu Chen, Eliza W Beal, Victor Okunrintemi, Emily Cerier, Anghela Paredes, Steven Sun, Griffin Olsen and Timothy M Pawlik in Journal of Patient Experience