Abstract
Background
The association of vitamin D deficiency with coronary artery disease (CAD) is controversial. This study seeks the association between vitamin D deficiency and acute myocardial infarction (MI) in Iraq.
Patients and methods
A total of 104 patients with acute MI and 104 healthy controls were studied throughout 2015. Their demographic, cardiovascular risk factors, and clinical characteristics were recorded. Serum vitamin D measurement was carried out for all patients.
Results
Vitamin D was more deficient in cases than controls; the number of cases was 60 (57.7%) and 53 (51%), respectively. However, a statistically significant difference (P=0.6) was not obtained. In the patient group, type 2 diabetes mellitus showed a strong association with vitamin D deficiency; there were 31 (81.6%) diabetic patients and 29 (43.9%) nondiabetic patients (P<0.001).
Conclusion
No statistical association between vitamin D deficiency and acute MI was found. Nevertheless, a strong association between vitamin D deficiency and acute MI with type 2 diabetes mellitus was seen.
Keywords: acute myocardial infarction, diabetes mellitus, vitamin D
Introduction
Association of vitamin D deficiency with coronary artery disease (CAD) has been reported in a number of studies and reviews recently 1–4. There are several mechanisms by which vitamin D may be associated with CAD including its effect on the rennin–angiotensin system, vessel compliance, blood pressure, parathyroid hormone level, and also glycemic control. In addition, vitamin D has anti-inflammatory effects 5,6.
Numerous recent studies have found high rates of cardiovascular diseases among patients with lower levels of vitamin D. According to the Framingham Offspring Study, in participants who were free of cardiovascular diseases at the baseline, the rate of major cardiovascular events was 53–80% higher among those with low vitamin D levels 4. This study aims to assess the vitamin D levels among patients of acute myocardial infarction (MI) and its relation with cardiovascular risk factors in Iraq.
Patients and methods
A case–control study was carried out at the Azadi Tertiary Teaching Hospital in Duhok, Kurdistan, Iraq during 2015. Overall, 104 patients and 104 controls were enrolled. After obtaining an informed consent, a complete questionnaire to determine the demographic and main cardiovascular risk factors of CAD including hypertension, type 2 diabetes mellitus (T2DM), dyslipidemia, smoking, and obesity was distributed among the participants.
At admission, venous blood samples were taken from patients, and the following laboratory parameters were analyzed: complete blood count, blood glucose, lipid profile, serum creatinine, blood urea, aminotransferase, alkaline phosphatase, serum bilirubin, serum albumin, serum troponin, creatine kinase-MB, and serum 25-hydroxy vitamin D3 [25(OH)D].
Serum [25(OH)D] was measured by an enzyme-linked immunosorbent assay test. We used the following cutoff values for classifying vitamin D status; a serum vitamin D level of less than 20 ng/ml was considered as vitamin D deficiency. A level between 20 and 30 ng/ml was regarded as an insufficient level. But a level higher than 30 ng/ml was considered a desirable level 7. Controls were age and sex matched to cases, and they needed to be free from previous cardiovascular events. Controls were recruited from the attendants or relatives of noncardiac patients from the noncardiac ward or patients attending noncardiac outpatient clinics for disorders unrelated to CAD.
Acute MI encompasses ST-elevation myocardial infarction (STEMI) and non-ST-elevation myocardial infarction (NSTEMI) and was diagnosed according to the 2014 AHA/ACC definitions 8. Cardiovascular risk factors including smoking, hypertension, T2DM, dyslipidemia, and obesity were checked and defined based on standard international definitions 9–12.
The inclusion criteria included all patients older than 25 years with diagnoses of acute MI. The exclusion criteria included patients with end-stage renal disease, malignancies, chronic liver disease, and patients receiving vitamin D and/or calcium supplements.
Statistical analyses
The Statistical Package for Social Sciences (version 18; SPSS Inc., Chicago, Illinois, USA) software was used for data analysis, and data were presented as mean±SD. The descriptive statistics of participants were obtained by determining frequency distributions of categorical data and weighted means and SEs of continuous variables such as age, sex, BMI, dyslipidemia, T2DM, hypertension, smoking, and serum vitamin D. Significant differences in categorical and continuous variables between the cases and control groups were analyzed using the χ2-test. The study was approved by the ethical committee at the Kurdistan Board of Medical Specialties in Erbil, Kurdistan, Iraq.
Results
The patients’ mean age was 60.12±12.22 ranging from 28 to 84 years. In all, 78 (75%) patients had STEMI and 26 (25%) patients had NSTEMI. Vitamin D deficient and insufficient numbers were 60 (57.7%) in cases and 53 (51%) in controls.
The patients had a higher prevalence of hypertension, T2DM, dyslipidemia, obesity, and smoking status. There was a significant difference in terms of the cardiovascular risk factors between the two groups (P<0.05) as shown in Table 1. With regard to vitamin D status, there was no significant difference in the distribution of vitamin D levels among cases and controls (P=0.6) as shown in Table 1 and Fig. 1.
Table 1.
Baseline characteristics of participants
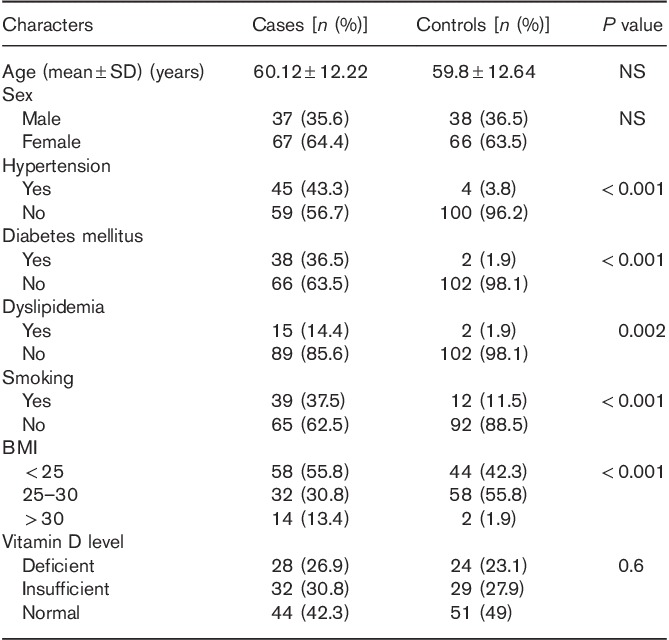
Fig. 1.
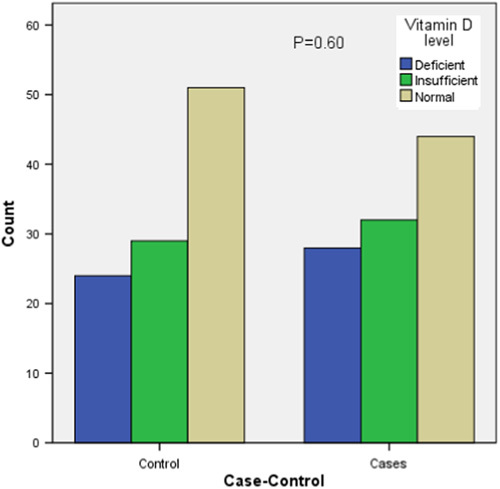
Distribution of vitamin D status among cases and controls.
Within the patients’ group, vitamin D deficiency and insufficiency were evident in 31 (81.6%) diabetic patients compared with 29 (43.9%) nondiabetic patients with a significant difference (P<0.001) as shown in Table 2. The vitamin D status among the types of acute MI (STEMI and NSTEMI) has been presented in Fig. 2. In addition, there was no significant difference between them (P=0.2).
Table 2.
Relation of characteristics of cases with vitamin D status
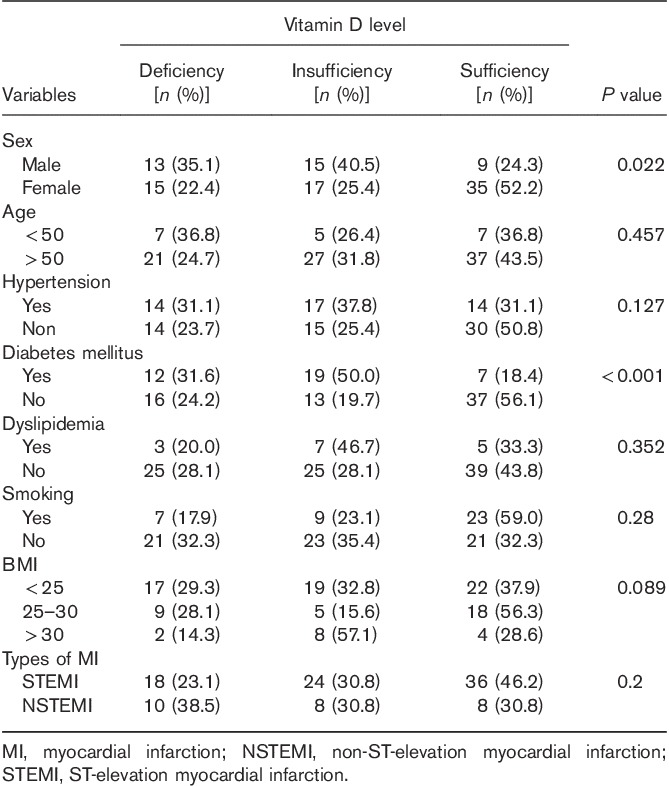
Fig. 2.
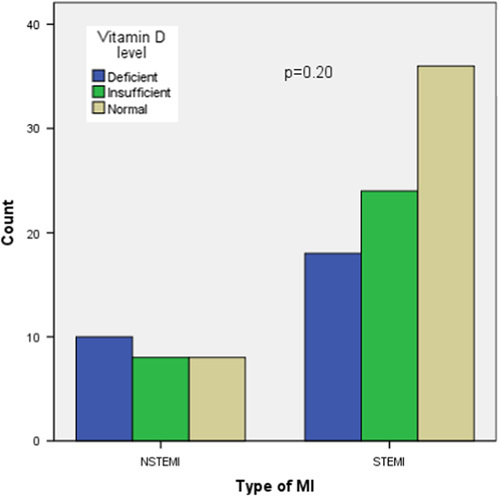
Vitamin D levels in STEMI and NSTEMI. MI, myocardial infarction; NSTEMI, non-ST-elevation myocardial infarction; STEMI, ST-elevation myocardial infarction.
Discussion
This study revealed that a high rate of vitamin D deficiency was prevalent in Iraq, and the rate of this deficiency was relatively higher in cases of acute MI compared with healthy controls. However, there was no statistical difference in the prevalence of vitamin D deficiency between patients with acute MI and healthy controls.
It has been observed in many studies that the risk of CAD and acute MI is higher in people with vitamin D deficiency 13–15. The possible mechanism between vitamin D insufficiency and cardiac events has been postulated to be associated with metabolic, procoagulant, and inflammatory events. This suggests that vitamin D insufficiency increases the risk of acute MI by promoting established risk factors that are predisposed to atherothrombosis 16.
Despite the higher numerical rates of vitamin D deficiency found among our cases, in agreement with the following studies including the studies by Rodriquez et al. 17, Ahbab et al. 18, and Messenger et al. 19, no statistically significant difference in the vitamin D levels between patients and healthy controls were found. Conversely, it was found that the high level of vitamin D might be associated with adverse cardiac events. Rajasree et al. 20 observed that a high level of vitamin D is arteriotoxic and suggested an association of high intake of vitamin D with an increased incidence of CAD. Besides, with regard to the types of acute MI, the present study found no difference in the vitamin D levels between STEMI and NSTEMI patients, and this is similar to the study by De Matrio et al. 21 from Italy.
An important observation in this study was a strong association between vitamin D deficiency and T2DM among cases with acute MI (P<0.001). Several studies like those by Cigolini et al. 3, Targherand et al. 4, and Pietschamn et al. 22 found an association between vitamin D deficiency and T2DM. However, the data are limited to the correlations between vitamin D deficiency and T2DM among cases of acute MI. It seems that vitamin D deficiency in diabetic patients is an additive risk factor, augmenting the occurrence of acute MI 3,4. Moreover, more studies are required to assess whether hypovitaminosis D is associated directly with acute MI among patients with T2DM and to investigate the clinical implications of this association in the prevention and management of cardiovascular events including the acute MI 3,23.
Although the significance of vitamin D deficiency in CAD is seen in many observational studies, the role of vitamin D supplementation on the risk of CAD is not clear. A sizeable trial carried out on the effect of vitamin D supplementation on cardiovascular events did not show any significant impact 24,25.
As the design of the study was case-controlled and only collected new, eligible cases of acute hospitalized MI, the sample size was relatively small, which in part could explain the nonstatistically significant difference in vitamin D levels between groups despite the higher clinical rate of vitamin D deficiency in acute MI cases.
On the basis of the association observed between vitamin D deficiency and T2DM among cases of acute MI, we do recommend measuring the serum vitamin D levels for all patients with T2DM, and to treat it if it was deficient to decrease the relative risk of acute MI. MI being such a risk is higher among T2DM patients with vitamin D deficiency compared with diabetic patients with normal vitamin D levels.
Acknowledgements
In addition to the Duhok Heart Center, the authors acknowledge the Azadi laboratory staff in Duhok for their help in carrying out this study.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Krause R, Bühring M, Hopfenmüller W, Holick MF, Sharma AM. Ultraviolet B and blood pressure. Lancet 1998; 352:709–710. [DOI] [PubMed] [Google Scholar]
- 2.Chiu KC, Chu A, Go VL, Saad MF. Hypovitaminosis D is associated with insulin resistance and beta cell dysfunction. Am J Clin Nutr 2004; 79:820–825. [DOI] [PubMed] [Google Scholar]
- 3.Cigolini M, Iagulli MP, Miconi V, Galiotto M, Lombardi S, Targher G. Serum 25-hydroxyvitamin D3 concentrations and prevalence of cardiovascular disease among type 2 diabetic patients. Diabetes Care 2006; 29:722–724. [DOI] [PubMed] [Google Scholar]
- 4.Targher G, Bertolini L, Padovani R, Zenari L, Scala L, Cigolini M, et al. Serum 25hydroxyvitamin D3concentrations and carotid artery intima media thickness among type 2 diabetic patients. Clin Endocrinol 2006; 65:593–597. [DOI] [PubMed] [Google Scholar]
- 5.Wang TJ, Pencina MJ, Booth SL, Jacques PF, Ingelsson E, Lanier K, et al. Vitamin D deficiency and risk ofcardiovascular disease. Circulation 2008; 117:503–511. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lee JH, O'keefe JH, Bell D, Hensrud DD, Holick MF. Vitamin D deficiency an important, common, and easily treatable cardiovascular risk factor? J Am Coll Cardiol 2008; 52:1949–1956. [DOI] [PubMed] [Google Scholar]
- 7.Hollis BW, Wagner CL. Normal serum vitamin D levels. N Engl J Med 2005; 352:515–516. [DOI] [PubMed] [Google Scholar]
- 8.Amsterdam EA, Wenger NK, Brindis RG, Casey DE, Jr, Ganiats TG, Holmes DR, Jr, et al. 2014 AHA/ACC Guideline for the Management of Patients with Non-ST-Elevation Acute Coronary Syndromes: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. J Am Coll Cardiol 2014; 64:e139–e228. [DOI] [PubMed] [Google Scholar]
- 9.Grundy SM, Cleeman JI, Bairey CN. For the coordinating Committee of theNational Cholesterol Education Program. Circulation 2004b; 110:227–239.15249516 [Google Scholar]
- 10.World Health Organization Definition and diagnosis of diabetes mellitus and intermediate hyperglycemia: report of a WHO/IDF consultation (PDF). Geneva: World Health Organization; 2006. 21. [Google Scholar]
- 11.Jellinger P, Smith D, Mehta A, Ganda O, Handelsman Y, Rodbard H, et al. American Association of Clinical Endocrinologists’ Guidelines for management of dyslipidemia and prevention of atherosclerosis. Endocrine Practice 2012; 18:1–78. [DOI] [PubMed] [Google Scholar]
- 12.Nuttall FQ. Body mass index: obesity, BMI, and health: a critical review. Nutr Today 2015; 50:117–128. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hosseinpanah F, Yarjanli M, Sheikholeslami F, Heibatollahi M, Eskandary PS, Azizi F. Associations between vitamin D and cardiovascular outcomes; Tehran Lipid and Glucose Study. Atherosclerosis 2011; 218:238–242. [DOI] [PubMed] [Google Scholar]
- 14.Giovannucci E, Liu Y, Hollis BW, Rimm EB. 25-hydroxyvitamin D and risk of myocardial infarction in men: a prospective study. Arch Intern Med 2008; 168:1174–1180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.De Boer IH, Kestenbaum B, Shoben AB, Michos ED, Sarnak MJ, Siscovick DS. 25-Hydroxyvitamin D levels inversely associate with risk for developing coronary artery calcification. J Am Soc Nephrol 2009; 20:1805–1812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Deleskog A, Piksasova O, Silveira A, Samnegård A, Tornvall P, Eriksson P, et al. Serum 25-hydroxyvitamin D concentration, established and emerging cardiovascular risk factors and risk of myocardial infarction before the age of 60 years. Atherosclerosis 2012; 223:223–229. [DOI] [PubMed] [Google Scholar]
- 17.Rodriguez G, Starr AZ, Czernuszewicz GZ, Manhas A, Alhariri A, Willerson JT, et al. Determinants of plasma vitamin D levels in patients with acute coronary syndromes. Eur J Clin Invest 2011; 41:1299–1309. [DOI] [PubMed] [Google Scholar]
- 18.Ahbab S, Avus BC, Kayas D, Cetin F, Ataoglu HE, Yenigun M. Acute coronary syndrome and plasma vitamin D levels in hypertensive patients. Turkey: Internal Medicine Clinic, Haseki Training Research Hospital. [Google Scholar]
- 19.Messenger W, Nielson CM, Beer T, Barrett-Connor E, Stone K, Shannon J. Serum and dietary vitamin D and cardiovascular disease risk in elderly men: a prospective cohort study. Nutr Metab Cardiovasc Dis 2012; 22:856–863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Rajasree S, Rajpal K, Kartha CC, Sarma PS, Kutty VR, Iyer CS, et al. Serum 25-hydroxyvitamin D3 levels are elevated in South Indian patients with ischemic heart disease. Eur J Epidemiol 2001; 17:567–571. [DOI] [PubMed] [Google Scholar]
- 21.De Metrio M, Milazzo V, Rubino M, Cabiati A, Moltrasio M, Marana I, et al. Vitamin D plasma levels and in-hospital and 1-year outcomes in acute coronary syndromes: a prospective study. Medicine (Baltimore) 2015; 94:857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Pietschmann P, Schernthaner G, Woloszczuk W. Serum osteocalcin levels in diabetes mellitus: analysis of the type of diabetes and microvascular complications. Diabetologia 1988; 31:892–895. [DOI] [PubMed] [Google Scholar]
- 23.Palomer X, González-Clemente JM, Blanco-Vaca F, Mauricio D. Role of vitamin D in thepathogenesis of type 2 diabetes mellitus. Diabetes Obes Metab 2008; 10:185–197. [DOI] [PubMed] [Google Scholar]
- 24.Nadir MA, Szwejkowski BR, Witham MD. Vitamin D and cardiovascular prevention. Cardiovasc Ther 2010; 28:5–12. [DOI] [PubMed] [Google Scholar]
- 25.Pilz S, Tomaschitz A, März W, Drechsler C, Ritz E, Zittermann A, et al. Vitamin D, cardiovascular disease and mortality. Clin Endocrinol 2011; 75:575–584. [DOI] [PubMed] [Google Scholar]


