Abstract
Over the last three decades, trials of coronary revascularization have taken into account whether populations did or did not have diabetes. What has not been considered is whether or not patients with diabetes in these studies have type 1 or type 2 diabetes. ‘Diabetes’ appears to be largely used as a synonym for type 2 diabetes. The number of patients with type 1 diabetes has not been reported in most trials. Many questions remain unanswered. Do patients with type 1 diabetes have the same response to various modes of revascularization as those with type 2 diabetes? We know type 2 diabetes affects coronary endothelial function and the coronary artery wall but to what extent does type 1 diabetes affect these? Any response to revascularization does not just depend on the coronary artery but also on the myocardium. How does type 1 diabetes affect the myocardium? To what extent do patients with type 1 diabetes have viable or ischaemic myocardium or scar? What does ‘diabetic cardiomyopathy’ refer to in the context of type 1 diabetes? This manuscript reviews the evidence for revascularization in type 1 diabetes. We conclude that there has been a near absence of investigation of the pros and cons of revascularization in this population. Investigations to establish both the nature and extent of coronary and myocardial disease in these populations are necessary. Clinical trials of the pros and cons of revascularization in type 1 diabetes are necessary; many will declare that these will be too challenging to perform.
Keywords: coronary, diabetes, revascularization
Introduction
Much attention has been paid to the relative merits of coronary artery bypass grafting (CABG) and percutaneous intervention in patients with ‘diabetes’. The term ‘diabetes’ however appears to have been used as a synonym for type 2 diabetes. Type 1 diabetes is widely recognized to have very different pathophysiology, natural history and associated comorbidities from type 2 diabetes 1. This manuscript reviews the extent of the literature concerning type 1 diabetes and revascularization.
Type 1 diabetes and clinical trials of revascularization strategies
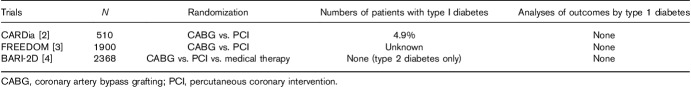
Trials including only patients with diabetes
Three trials of revascularization strategies have solely included patients with diabetes (Table 1). The largest of these, Bypass Angioplasty Revascularization Investigation 2 Diabetes (BARI-2D) 4, specifically excluded patients with type 1 diabetes (i.e. included only those with type 2 diabetes). The second largest, Future Revascularization Evaluation in Patients with Diabetes Mellitus: Optimal Management of Multivessel Disease (FREEDOM) 3, did not report how many patients had type 1 diabetes. The only other trial, Coronary Artery Revascularization in Diabetes (CARDia) 2, was the only trial to report the numbers with type 1 diabetes (4.9%). None of these trials reported subanalyses of the pros and cons of randomized strategies in type 1 diabetes. There will be those who suggest that trials specifically in patients with type 1 diabetes are too difficult to recruit because of the lower prevalence of type 1 versus type 2 diabetes. Caution should be used when extrapolating these results to guide the management of patients with type 1 diabetes until specific evidence in this population is available.
Table 1.
Revascularization trials including patients with diabetes only
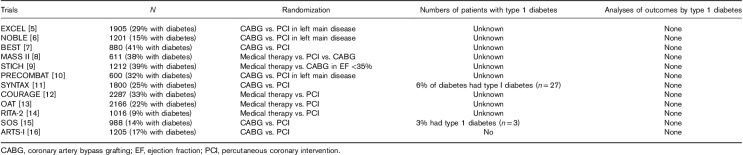
Trials with subgroup analyses of subgroups of patients with diabetes
Of the large trials with diabetes subgroups, only two stated how many patients had type 1 diabetes (Table 2). The Synergy between Percutaneous Coronary Intervention with Taxus and Cardiac Surgery trial 11 and Stent or Surgery trial 15 included a combined total of 30 patients with type 1 diabetes.
Table 2.
Revascularization trials with subgroup analyses of patients with diabetes
Type 1 diabetes and studies of revascularization strategies
In the absence of clinical trials, there are now emerging nonrandomized analyses attempting to shed some light on the relative merits of revascularization strategies in type 1 diabetes. In the largest to date (2546 patients with type 1 diabetes in Swedish Web-system for Enhancement and Development of Evidence-based care in Heart disease Evaluated According to Recommended Therapies, SWEDE-HEART), CABG was associated with better outcomes than percutaneous coronary intervention 17.
International clinical practice guidelines and type 1 diabetes
The most recent international guidelines for revascularization (2018 guidelines on behalf of the European Society of Cardiology and European Association for Cardio-Thoracic Surgery) have several sections on ‘diabetes’ but make no mention of type 1 diabetes 18. The lack of evidence is not acknowledged in the ‘gaps in evidence’ section. No previous international practice guideline has offered guidance on how revascularization in type 1 diabetes might be approached.
Coronary artery disease in type 1 diabetes
Coronary artery disease in diabetes is known to be characterized by endothelial dysfunction and extensive atherosclerotic changes 1. These studies of coronary disease in diabetes have investigated patients with type 2 diabetes. Type 1 diabetes is anecdotally known to be associated with coronary artery disease but the prevalence and extent of disease is as yet unstudied. It is conceivable that patients with type 1 diabetes have very different coronary artery characteristics than those with type 2 diabetes in the context of the differing prevalence of comorbidities and presenting at different ages. The role of microvascular disease in coronary disease in patients with type 1 diabetes is unstudied.
Complications of percutaneous coronary intervention and coronary artery bypass grafting in type 1 diabetes
Patients with diabetes have a higher rate of one of the scourges of percutaneous coronary intervention: in-stent restenosis 19. No study has reported on the rates of restenosis in type 1 diabetes with the vast majority of studies failing to report the proportion of patients with type 1 or type 2 diabetes. Similarly, patients with diabetes have a higher rate of graft occlusion following CABG 20. ‘Diabetes’ in these studies has been used to mean type 2 diabetes. The rate of graft occlusion in patients with type 1 diabetes is unknown. Other unknowns regarding type 1 diabetes and percutaneous coronary intervention include the relative merits of dual antiplatelet therapy and rates of major and minor bleeding. Other unknowns with respect to CABG include the length of intensive care stay and sternal healing.
Myocardium and type 1 diabetes
In patients with type 2 diabetes and coronary artery disease, it is not only the coronary arteries that determine the pros and cons of revascularization but also the extent of disease of the myocardium. Myocardial disease in type 1 diabetes is largely unstudied. The prevalence of scar, ischaemia and viability is unknown. A very recent report from the DCCT has found that some patients with type 1 diabetes have cardiac autoantibodies 21. Patients with elevated levels of these autoantibodies have a higher risk of subsequent cardiovascular events than those who do not. Findings such as this illustrate the unique nature of the cardiovascular disease in type 1 diabetes and emphasize that type 1 diabetes should be studied as a distinct entity. ‘Diabetic cardiomyopathy’ is a term that has been used to describe the effects of diabetes on the myocardium. As yet this term has primarily been used in the context of type 2 diabetes with very little debate or discussion as to how the myocardial changes of type 1 diabetes might sit within this construct 22.
The rising recognition of the pre-eminence of cardiovascular disease in diabetes
Diabetes and cardiology communities have been stirred to the opportunities of improving the outcomes of patients with diabetes following the remarkable reduction in cardiovascular events seen with sodium-glucose cotransporter 2 inhibitors and glucagon-like peptide-1 receptor agonists 23. These trials have included patients with type 2 diabetes. The potential role of novel pharmacological strategies in type 1 diabetes is being considered. This enthusiasm should be expanded into improving the outcomes of patients with type 1 diabetes and coronary artery disease.
Type 1 diabetes is not the same as insulin-requiring diabetes
Some analyses of large clinical trials of revascularization in diabetes have presented results by insulin-requiring versus non-insulin-requiring diabetes. Not only is this a poor surrogate for type 1 diabetes, but it also fails to recognize those other forms of insulin-requiring diabetes including monogenic and secondary diabetes, and as such we recommend case report forms for clinical trials should be developed to explicitly capture whether the patient has type 1 or type 2 diabetes at baseline according to the American Diabetes Association criteria 24. Inclusion and exclusion criteria should also be clear as to whether or not patients with type 1 diabetes are to be included.
The future
Future registries, clinical trials and international guidelines must address the large evidence gap in revascularization in type 1 diabetes. Diabetologists have appreciated for years that these two diseases are separate entities. Diabetes and cardiovascular communities need to come together to design achievable and informative clinical trials.
Acknowledgements
Conflicts of interest
There are no conflicts of interest.
References
- 1.Paneni F, Beckman JA, Creager MA, Cosentino F. Diabetes and vascular disease: pathophysiology, clinical consequences, and medical therapy: part I. Eur Heart J 2013; 34:2436–2443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kapur A, Hall RJ, Malik IS, Qureshi AC, Butts J, de Belder M, et al. Randomized comparison of percutaneous coronary intervention with coronary artery bypass grafting in diabetic patients. 1-year results of the CARDia (Coronary Artery Revascularization in Diabetes) trial. J Am Coll Cardiol 2010; 55:432–440. [DOI] [PubMed] [Google Scholar]
- 3.Farkouh ME, Domanski M, Sleeper LA, Siami FS, Dangas G, Mack M, et al. Strategies for multivessel revascularization in patients with diabetes. N Engl J Med 2012; 367:2375–2384. [DOI] [PubMed] [Google Scholar]
- 4.BARI 2D Study Group, Frye RL, August P, Brooks MM, Hardison RM, Kelsey SF, et al. A randomized trial of therapies for type 2 diabetes and coronary artery disease. N Engl J Med 2009; 360:2503–2515. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Stone GW, Sabik JF, Serruys PW, Simonton CA, Généreux P, Puskas J, et al. Everolimus-eluting stents or bypass surgery for left main coronary artery disease. N Engl J Med 2016; 375:2223–2235. [DOI] [PubMed] [Google Scholar]
- 6.Mäkikallio T, Holm NR, Lindsay M, Spence MS, Erglis A, Menown IBA, et al. Percutaneous coronary angioplasty versus coronary artery bypass grafting in treatment of unprotected left main stenosis (NOBLE): a prospective, randomised, open-label, non-inferiority trial. Lancet (London, England) 2016; 388:2743–2752. [DOI] [PubMed] [Google Scholar]
- 7.Park S-J, Ahn J-M, Kim Y-H, Park D-W, Yun S-C, Lee J-Y, et al. Trial of everolimus-eluting stents or bypass surgery for coronary disease. N Engl J Med 2015; 372:1204–1212. [DOI] [PubMed] [Google Scholar]
- 8.Lima EG, Hueb W, Garcia RMR, Pereira AC, Soares PR, Favarato D, et al. Impact of diabetes on 10-year outcomes of patients with multivessel coronary artery disease in the Medicine, Angioplasty, or Surgery Study II (MASS II) trial. Am Heart J 2013; 166:250–257. [DOI] [PubMed] [Google Scholar]
- 9.Velazquez EJ, Lee KL, Jones RH, Al-Khalidi HR, Hill JA, Panza JA, et al. Coronary-artery bypass surgery in patients with ischemic cardiomyopathy. N Engl J Med 2016; 374:1511–1520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Park S-J, Kim Y-H, Park D-W, Yun S-C, Ahn J-M, Song HG, et al. Randomized trial of stents versus bypass surgery for left main coronary artery disease. N Engl J Med 2011; 364:1718–1727. [DOI] [PubMed] [Google Scholar]
- 11.Banning AP, Westaby S, Morice M-C, Kappetein AP, Mohr FW, Berti S, et al. Diabetic and nondiabetic patients with left main and/or 3-vessel coronary artery disease: comparison of outcomes with cardiac surgery and paclitaxel-eluting stents. J Am Coll Cardiol 2010; 55:1067–1075. [DOI] [PubMed] [Google Scholar]
- 12.Boden WE, O’Rourke RA, Teo KK, Hartigan PM, Maron DJ, Kostuk WJ, et al. Optimal medical therapy with or without PCI for stable coronary disease. N Engl J Med 2007; 356:1503–1516. [DOI] [PubMed] [Google Scholar]
- 13.Hochman JS, Lamas GA, Buller CE, Dzavik V, Reynolds HR, Abramsky SJ, et al. Coronary intervention for persistent occlusion after myocardial infarction. N Engl J Med 2006; 355:2395–2407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Henderson RA, Pocock SJ, Clayton TC, Knight R, Fox KAA, Julian DG, et al. Seven-year outcome in the RITA-2 trial: coronary angioplasty versus medical therapy. J Am Coll Cardiol 2003; 42:1161–1170. [DOI] [PubMed] [Google Scholar]
- 15.Booth J, Clayton T, Pepper J, Nugara F, Flather M, Sigwart U, et al. Randomized, controlled trial of coronary artery bypass surgery versus percutaneous coronary intervention in patients with multivessel coronary artery disease: six-year follow-up from the Stent or Surgery Trial (SoS). Circulation 2008; 118:381–388. [DOI] [PubMed] [Google Scholar]
- 16.Abizaid A, Costa MA, Centemero M, Abizaid AS, Legrand VM, Limet RV, et al. Clinical and economic impact of diabetes mellitus on percutaneous and surgical treatment of multivessel coronary disease patients: insights from the Arterial Revascularization Therapy Study (ARTS) trial. Circulation 2001; 104:533–538. [DOI] [PubMed] [Google Scholar]
- 17.Nyström T, Sartipy U, Franzén S, Eliasson B, Gudbjörnsdottir S, Miftaraj M, et al. PCI versus CABG in patients with type 1 diabetes and multivessel disease. J Am Coll Cardiol 2017; 70:1441–1451. [DOI] [PubMed] [Google Scholar]
- 18.Neumann F-J, Sousa-Uva M, Ahlsson A, Alfonso F, Banning AP, Benedetto U, et al. 2018. ESC/EACTS Guidelines on myocardial revascularization. Eur Heart J 2019; 40:87–165. [Google Scholar]
- 19.Kirtane AJ, Patel R, O’Shaughnessy C, Overlie P, McLaurin B, Solomon S, et al. Clinical and angiographic outcomes in diabetics from the ENDEAVOR IV trial: randomized comparison of zotarolimus- and paclitaxel-eluting stents in patients with coronary artery disease. JACC Cardiovasc Interv 2009; 2:967–976. [DOI] [PubMed] [Google Scholar]
- 20.Deb S, Singh SK, Moussa F, Tsubota H, Une D, Kiss A, et al. The long-term impact of diabetes on graft patency after coronary artery bypass grafting surgery: a substudy of the multicenter Radial Artery Patency Study. J Thorac Cardiovasc Surg 2014; 148:1246–1253; (discussion 1253). [DOI] [PubMed] [Google Scholar]
- 21.Sousa GR, Pober D, Galderisi A, Lv H, Yu L, Pereira AC, et al. Glycemic control, cardiac autoimmunity, and long-term risk of cardiovascular disease in type 1 diabetes mellitus: a DCCT/EDIC cohort-based study. Circulation 2018; 148:730–743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lee MMY, McMurray JJV, Lorenzo-Almorós A, Kristensen SL, Sattar N, Jhund PS, et al. Diabetic cardiomyopathy. Heart 2019; 105:337–345. [DOI] [PubMed] [Google Scholar]
- 23.Sattar N, Petrie MC, Zinman B, Januzzi JL. Novel diabetes drugs and the cardiovascular specialist. J Am Coll Cardiol 2017; 69:2646–2656. [DOI] [PubMed] [Google Scholar]
- 24.American Diabetes Association. 2. Classification and diagnosis of diabetes: standards of medical care in diabetes. Diabetes Care 2019; 42 (Suppl 1): S13–S28. [DOI] [PubMed] [Google Scholar]