Abstract
Diabetes mellitus (DM) and atherosclerotic cardiovascular disease (ASCVD) both increase the risk for a major adverse cardiac event, and are therefore considered priority conditions clinically. Although guidelines encourage clinicians to treat them similarly, many researchers do not consider DM an ASCVD risk-equivalent. However, from a healthcare system standpoint it is more important to determine whether DM is an economic burden equivalent to ASCVD. Using data from the Household Component of the 2010–2013 Medical Expenditure Panel Survey, we determined that the diagnosis of DM yields significantly lower healthcare expenditures and resource utilization when compared with ASCVD. In fact, the healthcare cost associated with DM alone is almost $1000 less than ASCVD. That being said, the cost and resource utilization was highest among those individuals diagnosed with ASCVD+DM, underscoring the importance of primary and secondary prevention to help detect individuals early and initiate proper lifestyle and aggressive therapeutic managements.
Keywords: atherosclerotic cardiovascular disease, cardiovascular prevention, cost-effectiveness, diabetes mellitus
Introduction
In contrast to previous notion 1, contemporary emerging data suggest that not all individuals with diabetes mellitus (DM) should be unconditionally assumed as a risk equivalent of those with prior atherosclerotic cardiovascular disease (ASCVD) 2. From a healthcare delivery perspective, both are priority conditions as they are associated with significant healthcare costs, however specific quantitative information on the relative impact of each condition with regard to direct medical expenditure and resource utilization is scarce. Given this gap in knowledge, and the importance of understanding the economic burden of DM as its prevalence continues to increase, we evaluated and compared the healthcare costs and resource utilization for individuals across the spectrum of ASCVD and DM in a nationally representative US adult population.
Methods
Data for this study was extracted from the Medical Expenditure Panel Survey (MEPS), 2010–2013. The MEPS, led by the Agency for Healthcare Research and Quality, is a set of large-scale, national surveys about individuals and families, their medical providers, and their employers. The Household Component of the MEPS collects data about health services used, their frequency and cost, charges, source of payment, income, employment, as well as ample data on insurance used by, and available to, US workers 3. The MEPS respondents are enrolled for 2 years of data collection, with a new panel beginning each year. The sampling frame for the MEPS-Household Component is drawn from respondents to the National Health Interview Survey, with a design that includes sampling weights, stratification, and clustering. The MEPS sampling weights incorporate adjustment for the complex sample design and reflect survey nonresponse and population totals from the Current Population Survey 3.
Different files from the Household Component were utilized for this project: full-year consolidated data files, medical conditions files, and event files. The full-year consolidated data files include most demographics on a person-level, whereas the medical conditions files include each diagnosis a person has, which after being transcribed verbatim at each survey, are translated into International Classification of Diseases, 9th ed., Clinical Modification (ICD-9-CM) by professional coders. Modifiable risk factor profile was ascertained using self-reported and/or ICD-9-CM codes (when applicable), where individuals with presence of one or more of: hypertension (ICD-9-CM code: 401), dyslipidemia (ICD-9-CM code: 272), lack of physical exercise (defined as not participating in moderate–vigorous physical activity, ≥30 min, ≥5 times per week), smoking, and/or obesity (BMI≥30 kg/m2, a constructed variable using self-reported weight and height), were included. On the basis of the presence of these individual cardiovascular (CV) risk factors, survery participants were profiled as ‘Poor‘ (≥4 CV risk factors), ‘Average’ (2–3 CV risk factors), or ‘Optimal’ (0–1 CV risk factors).
Finally, each event file denotes healthcare resource utilization per person; including hospitalizations, emergency room visits, and outpatient clinic/office-based visits. All yearly files were linked together to determine accurate results for each individual, and data from 2010 to 2013 was combined to achieve a more robust study population. As MEPS data are publicly available, this study was exempt of Institutional Review Board (IRB) approval. We limited our study population to noninstitutionalized US adults of at least 18 years of age, and ascertained diagnoses of ASCVD (coronary artery disease, stroke, and peripheral artery disease) and DM using ICD-9-CM or self-report. Because MEPS collapses ICD-9-CM codes into three-digit codes, our code for DM includes individuals with type 1 and type 2 DM, though it is likely that the majority suffer from type 2 DM. Total annual direct medical expenditures were calculated for each person. Data for this variable included overall healthcare expenditures (HCE), including those from specific healthcare utilization types, such as hospitalizations, prescribed medications, outpatient visits, emergency department (ED) visits and other expenditures (dental visits, vision aid, home healthcare, and other medical supplies). Two-part models were utilized to study cost data; after taking into consideration the probability of having an expenditure (first model), a generalized linear model with gamma distribution, and link log (second model) was used to assess the mean per capita expenditures. Individuals were classified into four mutually exclusive categories: ‘DM (−), ASCVD (−)’, ‘DM (+)’, ‘ASCVD (+)’, or ‘DM (+), ASCVD (+)’.
Results
The total population included 87 665 participants (mean age: 47 years; 49% male), of which 82.6% had no DM or ASCVD, 7.2% had only DM, 7.0% had only ASCVD, and 3.2% had both DM and ASCVD. This represents weighted national estimates of over 225 million US adults (~16 million with only DM, ~16 million only with ASCVD). When comparing individuals with only DM and only ASCVD, a greater percentage of those with only DM had a poor modifiable risk factor profile, but also lower percentages across the three subsets of Modified Charlson Comborbidity Index (without CV components). Additional demographic and socioeconomic information comparing the four subgroups is available in Table 1.
Table 1.
Baseline characteristics from US adults, with and without diabetes mellitus and atherosclerotic cardiovascular disease, from the 2010–2013 Medical Expenditure Panel Survey
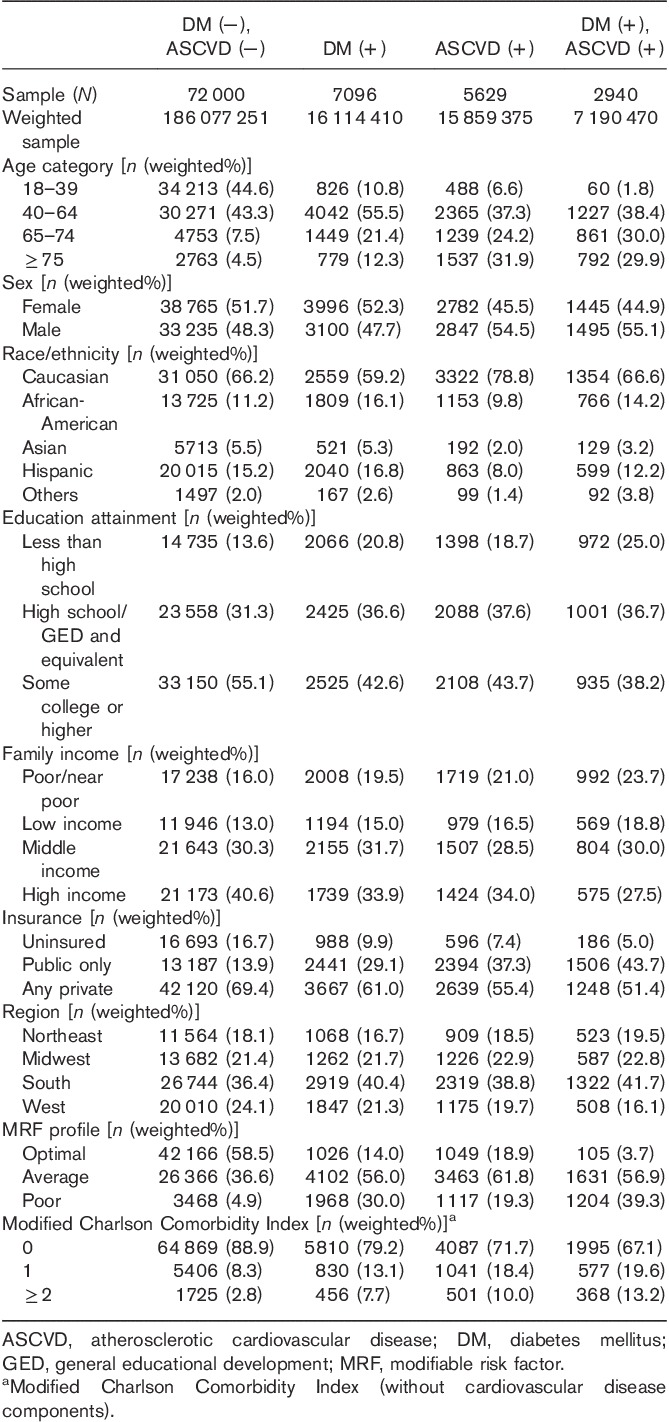
Figure 1 (top) shows the multivariate adjusted average total per capita healthcare expenditures by DM and ASCVD status. For each bar, the proportion of cost due to prescriptions medications, hospitalizations, ED visits, and outpatient visits is illustrated. Total average per capita healthcare cost was highest among those with both DM and ASCVD ($10 172). In multivariate adjusted models, as compared with those without DM and ASCVD, incremental annual HCE for (a) DM alone was $2694; (b) ASCVD alone was $3494; and (c) DM+ASCVD was $6043 (all P<0.001), respectively. In addition, the healthcare expenditures of those with only DM ($6823) was significantly lower (difference: $800, P=0.04) than those with only ASCVD ($7623).
Fig. 1.
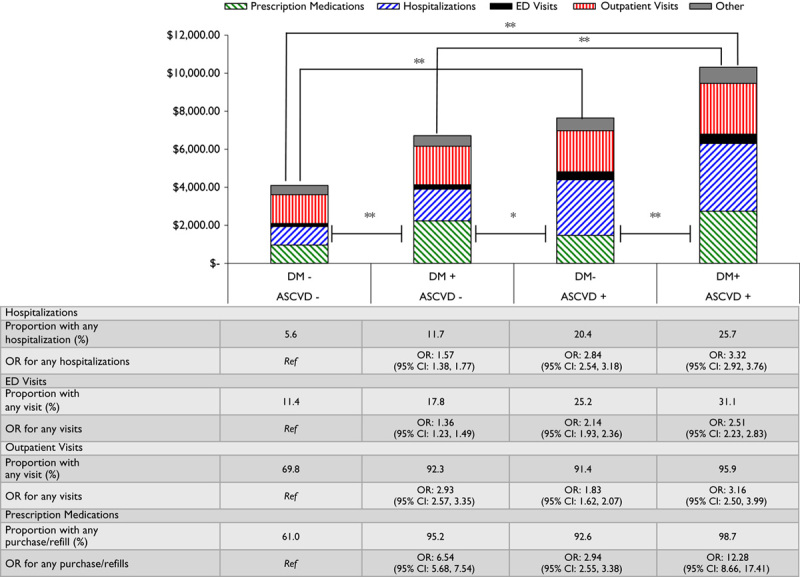
Average healthcare expenditures and resource utilization by DM and atherosclerotic cardiovascular disease status, from the 2010–2013 Medical Expenditure Panel Survey. Multivariate analysis for ORs and expenditures were adjusted for age, sex, modifiable risk factor profile, family income, race/ethnicity, insurance type, geographic region and Modified Charlson Comorbidity Index (without cardiovascular disease components). **P<0.001/*P<0.05. ASCVD, atherosclerotic cardiovascular disease; CI, confidence interval; DM, diabetes mellitus; ED, emergency department; OR, odds ratio.
Similar trends of higher resource utilization among participants with ASCVD versus DM alone were also noted, most notably regarding hospitalizations [odds ratio (OR)=2.8 vs. 1.6, respectively] and ED visits (OR=2.1 vs. 1.4, respectively) (Fig. 1, bottom). For those with a diagnosis of only ASCVD or ASCVD+DM, hospitalizations and ED visits accounted for 44 and 40% of the total healthcare expenditures, respectively. In comparison, for individuals with the diagnosis of only DM, hospitalizations and ED visits accounted for 28% of the total healthcare expenditures. In those individuals with only DM, the likelihood of filling a prescription medication was more than two times that of individuals with only ASCVD (OR=6.5 vs. 2.9, respectively).
Discussion
In summary, within a US nationally representative population, we observed significantly lower healthcare costs and resource utilization among those with only DM as compared with those with only ASCVD. Our results have important implications given the recent insights from Rana et al. 2, that showed a significantly lower 10-year risk among individuals with DM alone versus those with heart disease alone. As a result, individuals with only DM are not only considered a lower risk subgroup, but they also have statistically significant lower healthcare expenditures, driven primarily by less frequent hospitalizations and ED visits.
Currently in the USA, hospitalizations make up one-third of all healthcare expenditures, totaling an estimated $1 trillion 4. In addition, up to 10% of all visits to the ED end in admission to the hospital 5. Although hospitalizations are the single largest contributor to the overall healthcare expenditure total, physician visits and prescription drugs also play a role; yet in combination still account for a smaller percentage than hospitalizations (~20 and 10%, respectively) 4.
Our data are consistent with the current breakdown of medical expenditures in the USA, with large contributions to healthcare spending from hospitalizations and ED visits among those with these priority conditions. Moreover, hospitalizations and ED visits were significantly more common among individuals with only ASCVD compared with those with only DM, which appears to be reflective in differences in overall as well as specific healthcare expenditures. Although those individuals with only DM utilize prescription medications more often, it can be concluded that the lower upfront cost yields lower downstream cost in the form of hospitalizations and ED visits, underscoring the importance for early identification and management of those with DM and other ASCVD risk factors. Given that established ASCVD leads to twofold higher medical cost independent of CV risk factor profile and DM status 6, the value of primary prevention among those without established ASCVD, especially in high-risk groups such as those with DM, cannot be understated. In addition, future studies are needed to elucidate important differences that exist when individuals with DM are further classified using specific characteristics, including (but not limited to): type 1 versus type 2, controlled versus uncontrolled, duration of disease, the presence of end-organ damage, and/or insulin requirements.
There are several limitations of our analysis. First, as DM and ASCVD were self-reported or on the basis of ICD-9 codes, underestimation of the true national prevalence is likely, as has been previously described, especially with chronic conditions 7. Without accurate measurement of blood glucose or glycated hemoglobin at the time of enrollment, we cannot account for those individuals with undiagnosed DM. Second, other analyses have found that MEPS data tend to underestimate total medical expenditures 8. However, this limitation would lead to a likely underestimation of the actual associated cost and saving estimates from primordial prevention strategies. Third, as a cross-sectional analysis, differentiation between incident versus prevalent DM/ASCVD cases was not feasible, which might affect expenditure behavior. Fourth, generalizability outside the US noninstitutionalized adult population is limited. Finally, even after adjusting for important variables, the risk of residual confounding cannot be eliminated.
Conclusion
Although our data are not intended to inform the risk examination between DM and ASCVD, it does indicate that presence of DM alone does not translate into an ASCVD ‘economic burden’ equivalent. Our study finds an important trend that mirrors the current landscape of healthcare spending in the USA, which is that increased total number of prescription drugs and physician visits does not yield higher cost. In fact, to adequately reduce the economic burden of these priority conditions on the healthcare system, clinicians must maximize the positive effect and reduced cost of more frequent follow-up and proper management. If clinicians can more effectively intervene by encouraging targeted lifestyle interventions and adherence to guideline recommended treatment regimens, the higher rates of hospitalizations and ED visits in those individuals with ASCVD can be reduced and lead to lower overall healthcare spending. Ultimately, this may lead to greater upfront spending, but on the basis of the results of this data will return significant value by eliminating more costly visits to the hospitals and emergency room.
Acknowledgements
Conflicts of interest
Dr Nasir is on the advisory board for Quest Diagnostic and Consultant for Regeneron. For the remaining authors there are no conflicts of interest.
Footnotes
*David I. Feldman and Javier Valero-Elizondo contributed equally to the writing of this article.
References
- 1.Grundy SM. Diabetes and coronary risk equivalency. Diabetes Care 2006; 29:457–460. [DOI] [PubMed] [Google Scholar]
- 2.Rana JS, Liu JY, Moffet HH, Jaffe M, Karter AJ. Diabetes and prior coronary heart disease are not necessarily risk equivalent for future coronary heart disease events. J Gen Intern Med 2016; 31:387–393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Medical Expenditure Panel Survey. Survey background. Available at: http://meps.ahrq.gov/mepsweb/about_meps/survey_back.jsp. [Accessed 23 July 2016].
- 4.National Center for Health Statistics. Health, United States, 2015: with special feature on racial and ethnic health disparities. Hyattsville, MD: National Center for Health Statistics; 2016. [PubMed] [Google Scholar]
- 5.Rui P, Kang K, Albert M. National Hospital Ambulatory Medical Care Survey: 2013 Emergency Department Summary Tables. Available at: http://www.cdc.gov/nchs/data/ahcd/nhamcs_emergency/2013_ed_web_tables.pdf. [Accessed 19 February 2018].
- 6.Valero-Elizondo J, Salami JA, Ogunmoroti O, Osondu CU, Aneni EV, Malik R, et al. Favorable cardiovascular risk profile is associated with lower healthcare costs and resource utilization: the 2012 Medical Expenditure Panel Survey. Circ Cardiovasc Qual Outcomes 2016; 9:143–153. [DOI] [PubMed] [Google Scholar]
- 7.Gregg EW, Zhuo X, Cheng YJ, Albright AL, Venkat Narayan KM, Thompson TJ. Trends in lifetime risk and years of life lost due to diabetes in the USA, 1985–2011: a modeling study. Lancet Diabetes Endocrinol 2014; 2:867–874. [DOI] [PubMed] [Google Scholar]
- 8.Trogdon JG, Murphy LB, Khavjou OA, Li R, Maylahn CM, Tangka FK, et al. Costs of chronic diseases at the state level: the chronic disease cost calculator. Prev Chronic Dis 2015; 12:E140. [DOI] [PMC free article] [PubMed] [Google Scholar]


