Abstract
The capsaicin receptor transient receptor potential V1 (TRPV1; also known as vanilloid receptor 1) is a sensory neuron-specific ion channel that serves as a polymodal detector of pain-producing chemical and physical stimuli. It has been reported that extracellular ATP potentiates the TRPV1 currents evoked by capsaicin or protons and reduces the temperature threshold for its activation through metabotropic P2Y receptors in a PKC-dependent pathway, suggesting that TRPV1 activation could trigger the sensation of pain at normal body temperature in the presence of ATP. Here, we show that ATP-induced thermal hyperalgesia was abolished in mice lacking TRPV1, suggesting the functional interaction between ATP and TRPV1 at a behavioral level. However, thermal hyperalgesia was preserved in P2Y1 receptor-deficient mice. Patch-clamp analyses using mouse dorsal root ganglion neurons indicated the involvement of P2Y2 rather than P2Y1 receptors. Coexpression of TRPV1 mRNA with P2Y2 mRNA, but not P2Y1 mRNA, was determined in the rat lumbar DRG using in situ hybridization histochemistry. These data indicate the importance of metabotropic P2Y2 receptors in nociception through TRPV1.
Keywords: pain, thermal hyperalgesia, capsaicin receptor, P2Y receptor, ATP, UTP
Introduction
The sensation of pain allows us to recognize injury and triggers appropriate protective responses. A specific population of primary afferent neurons called nociceptors are known to be involved in the detection of noxious thermal, mechanical, or chemical stimuli and can be distinguished by their sensitivity to capsaicin, the pungent ingredient in hot chili peppers (Szallasi and Blumberg, 1999; Wood and Perl, 1999; Woolf and Salter, 2000). The capsaicin receptor transient receptor potential V1 (TRPV1; also known as vanilloid receptor 1), a member of the transient receptor potential ion channel superfamily (Minke and Cook, 2002), is a nonspecific cation channel with six transmembrane domains expressed predominantly in unmyelinated C fibers and activated not only by capsaicin but also by noxious heat (>43°C) or protons (acidification), both of which cause pain in vivo (Caterina et al., 1997; Tominaga et al., 1998; Caterina and Julius, 2001). Recently, TRPV1 has been reported to respond to anandamide (Zygmunt et al., 1999), lipoxygenase products (Hwang et al., 2000), and N-arachidonoyl-dopamine (Huang et al., 2002). Furthermore, analyses of mice lacking TRPV1 have shown that TRPV1 is essential for selective modalities of pain sensation and for tissue injury-induced thermal hyperalgesia, further suggesting a critical role for TRPV1 in the detection or modulation of pain (Caterina et al., 2000; Davis et al., 2000).
Tissue damage associated with infection, inflammation, or ischemia produces an array of chemical mediators that activate or sensitize nociceptor terminals to elicit or exacerbate pain at the site of injury in addition to the release of the mediators from the nociceptor terminals themselves. One of the important components of this acute proalgesic response is ATP released from the cytosol of the damaged or ruptured cells and sensory neurons (Sawynok and Sweeney, 1989; Lazarowski et al., 2000; Dunn et al., 2001). Extracellular ATP excites nociceptor endings (Cook and McCleskey, 2002), evoking a sensation of pain (Sawynok and Sweeney, 1989; Dunn et al., 2001). In these neurons, the most widely studied targets of extracellular ATP have been ionotropic ATP (P2X) receptors (North and Barnard, 1997; Ralevic and Burnstock, 1998; Dunn et al., 2001). Indeed, several P2X receptor subtypes have been identified in sensory neurons, including one (P2X3) whose expression is primarily confined to these cells (Chen et al., 1995; Lewis et al., 1995). In contrast, possible roles for metabotropic ATP (P2Y) receptors in nociceptive signalings have received limited attention (von Kugelgen and Wetter, 2000). However, there is increasing evidence that P2Y receptors are involved in nociception (Lang et al., 2002; Molliver et al., 2002; Zimmermann et al., 2002). Furthermore, ATP has been found recently to potentiate the TRPV1 currents evoked by capsaicin or protons through metabotropic P2Y1 receptor activation in a protein kinase C-dependent pathway (Tominaga et al., 2001). In the presence of extracellular ATP, the temperature threshold for TRPV1 activation was reduced from 42 to 35°C, such that normal body temperature is capable of activating TRPV1, which might cause pain sensation. Bradykinin has also been reported to reduce the temperature threshold for TRPV1 activation through a PKC-dependent pathway (Sugiura et al., 2002). These data suggest that phosphorylation of TRPV1 by PKC changes the agonist sensitivity of this ion channel. Indeed, direct phosphorylation of TRPV1 by PKC has been proven biochemically, and two serine residues as substrates for PKC-dependent phosphorylation have been identified (Numazaki et al., 2002).
Despite these findings, the involvement of metabotropic P2Y receptors in nociception has not yet been investigated in live animals. To address this question, we performed behavioral, electrophysiological, and histochemical analyses to explore the expression and function of P2Y subtypes in wild-type mice and mice lacking TRPV1. We observed a loss of ATP-induced thermal hyperalgesia in TRPV1 knock-out mice and found that P2Y2 receptors, but not P2Y1 receptors, could be the targets of extracellular ATP in TRPV1-mediated thermal hyperalgesia.
Materials and Methods
Primary cultures prepared from male adult C57BL/6 strain (wild-type) (20 gm body weight; Japan SLC, Shizuoka, Japan) or P2Y1-deficient mice (obtained from Dr. Gachet, Institut National de la Santé et de la Recherche Médicale, Strasbourg, France) (Leon et al., 1999) dorsal root ganglion neurons were incubated in medium containing nerve growth factor (100 ng/ml). Whole-cell patch-clamp recordings were performed 1 d after preparation of DRG neurons as described previously (Caterina et al., 1997). Standard bath solution contained (in mm): 140 NaCl, 5 KCl, 2 MgCl2, 5 EGTA, 10 HEPES, and 10 glucose, pH 7.4 (adjusted with NaOH). Pipette solution contained (in mm): 140 KCl, 5 EGTA, and 10 HEPES, pH 7.4 (adjusted with KOH). All patch-clamp experiments were performed at room temperature.
Male C57BL/6 strain mice, P2Y1-deficient mice, or TRPV1-deficient mice (obtained from Dr. D. Julius, University of California, San Francisco, San Francisco, CA) were used for behavioral analyses. After 1 hr of adaptation, ATP (100 nmol), α,β-methylene ATP (αβmeATP) (20 nmol), or UTP (100 nmol) was injected intraplantarly into one hindpaw of each mouse, and response latencies to a radiant paw heating were measured as described previously (Caterina et al., 2000). In some experiments, mice were pretreated with 2′,3′-O-(2,4,6-trinitrophenyl) (TNP)–ATP (50 nmol) or saline (control) 10 min before αβmeATP or UTP injection. All procedures involving the care and use of mice and rats were performed in accordance with Mie University and Hyogo College of Medicine institutional guidelines and the National Institutes of Health Guide for the Care and Use of Laboratory Animals.
Total RNA was isolated from male adult C57BL/6 strain mice and reverse transcribed using Superscript II (Invitrogen, Gaithersburg, MD). The gene-specific primers (5′-GTTCAATTTGGCTCTGGCCG-3′ and 5′-CTGATAGGTGGCATAAACCC-3′forP2Y1;5′-CTTCAACGAGGACTTCAAGTACGTGC-3′ and 5′-CATGTTGATGGCGTTGAGGGTGTGG-3′ for P2Y2) were designed from mouse P2Y1 and P2Y2 sequences. PCR was performed with 35 cycles of the following protocol: 94°C, 10 sec; 55°C (for P2Y1) or 60°C (for P2Y2), 30 sec; and 68°C, 45 sec. Precise amplification of the expected fragment was confirmed by sequencing.
For in situ hybridization, L5 DRGs of four male Sprague Dawley rats were quickly removed and frozen in powdered dry ice. Sections (5 μm thick) were cut with a cryostat, thaw-mounted onto Matsunami adhesive silane-coated slides (Matsunami, Osaka, Japan), fixed in phosphate-buffered 4% formaldehyde for 20 min, and treated with 5 μg/ml proteinase-K in 50 mm Tris-HCl and 5 mm EDTA for 3 min. The sections were acetylated with 0.25% acetic anhydride in 0.1 m triethanolamine, dehydrated in ascending ethanol series, and air dried. Two 35S-labeled RNA probes were prepared by in vitro transcription of P2Y1 cDNA (GenBank accession number U22830, nucleotides 653–980) fragment and P2Y2 cDNA (GenBank accession number L46865, nucleotides 493–868) in linearized pGEM-T Easy vector (Promega, Madison, WI) by using T7 or SP6 RNA polymerase (Promega) and 35S-UTP (PerkinElmer Life Sciences, Natick, MA), giving a specific activity of 1.0–1.5 × 109 cpm/μg. A digoxigenin (DIG)-labeled RNA antisense probe was prepared by in vitro transcription of TRPV1 cDNA (GenBank accession number AF029310, nucleotides 149–486) fragment in linearized pGEM-T Easy vector by using a DIG RNA labeling Kit SP6/T7 (Roche Diagnostics, Mannheim, Germany). The procedures for hybridization, washing, and visualization using DAB reaction and autoradiography have been described previously (Hashimoto et al., 2001). In brief, sections were hybridized overnight at 55°C in humidified boxes with each of 35S-labeled RNA probes (3 × 106 cpm) and with a DIG-labeled probe (300 ng) in 300 μl of the hybridization buffer. All of these sections were rinsed in 5× SSC and 5 mm DTT for 30 min at 58°C and then washed in high-stringency buffer for 30 min at 58°C. Quantification of the labeled neurons was performed using randomly selected tissue profiles with bright-field illumination for DAB-stained neurons or dark-field illumination for silver grains over 35S-labeled neurons (Fukuoka et al., 2001). At least 200 neurons from an L5 DRG section of each of four rats were measured.
All the chemicals were obtained from Sigma (St. Louis, MO).
Results
To confirm the interaction between ATP and TRPV1 in the context of ATP-induced hyperalgesia in vivo, we performed a behavioral analysis using wild-type mice and TRPV1-deficient mice. Nociceptive responses such as licking and biting lasted for ∼2 min after ATP injection in wild-type mice. After cessation of the responses induced by intraplantar ATP injection, mice were subjected to radiant paw heating. A significant reduction in paw withdrawal latency was observed for 5–30 min after ATP injection in wild-type mice. In contrast, TRPV1-deficient mice developed no such thermal hypersensitivity in response to ATP injection, suggesting a functional interaction between ATP and TRPV1 (Fig. 1A). Next, we injected αβmeATP to examine the possibility that P2X receptors are involved in ATP-induced thermal hyperalgesia (Fig. 1B). Interestingly, thermal hyperalgesia was also observed after injection of αβmeATP. However, the αβmeATP-induced thermal hyperalgesia appeared and disappeared more rapidly than ATP and was blocked by TNP–ATP, a blocker of P2X receptors (Tsuda et al., 1999). Furthermore, we examined the effect of αβmeATP in TRPV1-deficient mice. Small but significant thermal hypersensitivity was observed only 5 min after αβmeATP injection (Fig. 1B), suggesting that TRPV1 does not mediate primarily αβmeATP-induced thermal hyperalgesia. In addition, TNP–ATP failed to inhibit the ATP-induced thermal hyperalgesia (Fig. 1C). These results suggest that both P2X and P2Y receptors are involved in ATP-induced thermal hyperalgesia, although P2Y receptors seem to be involved more predominantly and contribute to the protracted component of the ATP-induced thermal hyperalgesia. A pharmacological analysis of ATP-induced potentiation of TRPV1 currents evoked by capsaicin in human embryonic kidney 293 (HEK293) cells expressing TRPV1 suggested the involvement of the P2Y1 subtype of metabotropic ATP receptors (Tominaga et al., 2001). Therefore, we extended our behavioral analyses to P2Y1-deficient mice, which were reported to show defective platelet aggregation and increased resistance to thrombosis (Leon et al., 1999). Surprisingly, after ATP injection, mice lacking P2Y1 exhibited a reduction in heat-evoked withdrawal latency similar to that observed in wild-type mice, indicating that P2Y1 receptors are not involved in ATP-induced thermal hyperalgesia in mice (Fig. 1A).
Figure 1.
TRPV1 is essential for the development of ATP-induced thermal hypersensitivity in vivo, and P2Y receptors are predominantly involved. A, Wild-type (•), TRPV1 -/- (○), or P2Y1-/- mice (□) were injected intraplantarly with ATP (100 nmol), and the response latency to radiant heating of the hindpaw was measured at various time points after injection. Values are expressed as mean ± SE; n = 6 for each group. *p < 0.05 and **p < 0.01 versus wild-type and P2Y1-/- mice; two-tailed unpaired t test. B, Behavioral analyses in response to αβ meATP (20 nmol) injection similar to A in wild-type (•,▴) or TRPV1 -/- mice (○). In some experiments, mice were pretreated with TNP–ATP (50 nmol) (▴). Values are expressed as mean ± SE; n = 6 for each group. *p < 0.05 and **p < 0.01 versus wild type without TNP–ATP pretreatment; two-tailed unpaired t test. C, Behavioral analyses in response to ATP (100 nmol) injection similar to A in wild-type mice pretreated with TNP–ATP (50 nmol) (▵) or saline (•). Values are expressed as mean ± SE; n = 6 for each group.
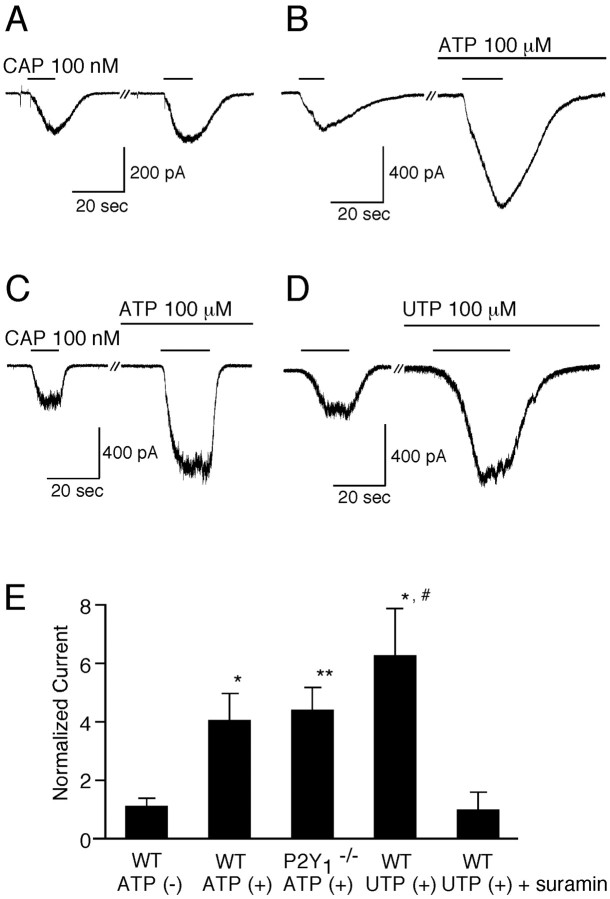
To explore the identity of the P2Y subtypes responsible for ATP-induced thermal hyperalgesia in mice, we first examined the effects of ATP on the capsaicin (low-dose)-evoked response in isolated mouse DRG neurons. In DRG neurons of wild-type mice, extracellular ATP caused significant increases in low-dose capsaicin-evoked currents, as observed in rat DRG neurons (1.07-fold ± 0.26-fold increase for controls vs 4.01-fold ± 0.92-fold increase with ATP; p < 0.05) (Fig. 2A,B,E) (Tominaga et al., 2001). In some of the DRG neurons examined, rapidly desensitized inward currents at -60 mV were observed after ATP application, indicative of activation of P2X receptors (data not shown). DRG neurons without such ATP-evoked currents were used to examine the effects of ATP on capsaicin-evoked responses to simplify the pathway involved, although the ATP-induced potentiation of the capsaicin-evoked responses was also observed in the cells showing ATP-evoked inward currents (data not shown). Similar potentiation of capsaicin-evoked currents was observed in P2Y1-deficient mice (4.37-fold ± 0.74-fold; p < 0.01 vs control) (Fig. 2C,E), suggesting lack of involvement of P2Y1 receptors in mouse DRG neurons, consistent with our behavioral analyses (Fig. 1A). We subsequently examined the effect of another ATP-related molecule, UTP, because this molecule is thought to be a relatively selective agonist of P2Y2 and P2Y4 receptors (Ralevic and Burnstock, 1998). UTP potentiated the capsaicin-evoked current responses to an extent similar to that seen for ATP (6.24-fold ± 1.59-fold; p < 0.05 vs control) (Fig. 2D,E), suggesting the involvement of P2Y2 or P2Y4 subtypes. Finally, the fact that suramin, which blocks P2Y2 but not P2Y4, abolished the potentiation by UTP (0.95-fold ± 0.57-fold; p < 0.05 vs UTP in wild type) implicates P2Y2 as the most likely P2Y subtype involved in the potentiation of capsaicin-evoked current responses in mouse DRG neurons.
Figure 2.
Extracellular ATP or UTP potentiates capsaicin-evoked currents in DRG neurons from wild-type or P2Y1-deficient mice. A–C, Representative traces of increases in the capsaicin (CAP)-activated currents by extracellular ATP (100 μm) in DRG neurons from wild-type (WT) (B) or P2Y1-deficient (C) mice. A shows a control trace without ATP pretreatment. Holding potential was -60 mV. D, A representative trace of increases in the capsaicin-activated currents by UTP (100 μm) in DRG neurons from wild-type mice. E, Effects of ATP, UTP, or UTP plus suramin (50 μm) on the capsaicin-activated currents. Currents were normalized to the currents initially evoked by capsaicin (100 nm) in the absence of the additives. Normalized currents in the absence of ATP in wild-type mice, in the presence of ATP in wild-type mice, in the presence of ATP in P2Y1-deficient mice, in the presence of UTP in wild-type mice, or in the presence of UTP plus suramin in wild-type mice were 1.07 ± 0.26 (n = 3), 4.01 ± 0.92 (n = 8), 4.37 ± 0.74 (n = 4), 6.24±1.58 (n = 4), or 0.95 ± 0.57 (n = 3), respectively. *p < 0.05 and **p < 0.01 versus absence of ATP in wild type; #p < 0.05 versus presence of UTP and suramin in wild type; two-tailed unpaired t test. WT, Wild type.
To examine the functional importance of P2Y2 receptors, we next investigated the expression of P2Y2 mRNA. A reverse transcriptase-PCR study showed that P2Y2 as well as P2Y1 mRNA expression in mouse DRG neurons (Fig. 3A) was consistent with the pharmacological analyses described above. To further support the functional relationship of P2Y receptors with TRPV1 in the patch-clamp experiments, we examined the coexpression of P2Y1 receptor mRNA and P2Y2 receptor mRNA with TRPV1 mRNA in the rat lumbar DRG using in situ hybridization histochemistry. In this experiment, 23.5 ± 4.3, 22.5 ± 2.5, and 44.6 ± 5.2% of rat DRG neurons expressed P2Y1, P2Y2, and TRPV1 mRNAs, respectively. Coexpression of P2Y1 mRNA and TRPV1 mRNA was quite rare (Fig. 3B). Thus, most of the 35S-labeled P2Y1 mRNA-expressing neurons were not stained by DAB (2.6 ± 2.0% of P2Y1 mRNA-expressing cells were TRPV1 mRNA-positive) (Fig. 3B, a,b, arrowheads) and vice versa (1.6 ± 1.4% of TRPV1 mRNA-expressing cells were P2Y1 mRNA-positive). However, a significant population of DRG neurons coexpressed P2Y2 mRNA and TRPV1 mRNA (33.6 ± 10.7% of P2Y2 mRNA-expressing cells were TRPV1 mRNA-positive and 15.9 ± 5.2% of TRPV1 mRNA-expressing cells were P2Y2 mRNA-positive) (Fig. 3B, c,d, arrows). These data clearly suggest that P2Y2 receptors, but not P2Y1 receptors, can functionally interact with TRPV1 in DRG neurons.
Figure 3.

P2Y2 mRNA, but not P2Y1 mRNA, is coexpressed with TRPV1 mRNA in DRG. A, PCR amplification of P2Y1 (a) and P2Y2 (b) cDNA fragments from the RNAs of mouse DRG neurons. The expected sizes of the DNA fragments for mouse P2Y1 and P2Y2 are 651 and 781 bp, respectively. N, Negative control. B, Coexpression of TRPV1 mRNA with P2Y1 and P2Y2 mRNAs in rat DRG neurons. Double in situ hybridization histochemistry was performed on the sections. b and d are dark-field photomicrographs of a and c, respectively. The TRPV1 mRNA-expressing neurons were hybridized by a DIG-labeled antisense probe and visualized as DAB staining (brown cells in a and c). The P2Y1 mRNA-expressing (b) and P2Y2 mRNA-expressing (d) neurons were hybridized by the appropriate 35S-labeled antisense probe and visualized as clusters of silver grains. p, Positively labeled neurons. Arrowheads indicate P2Y1 mRNA-expressing neurons that do not express TRPV1 mRNA, whereas arrows indicate the neurons expressing both TRPV1 and P2Y2 mRNAs.
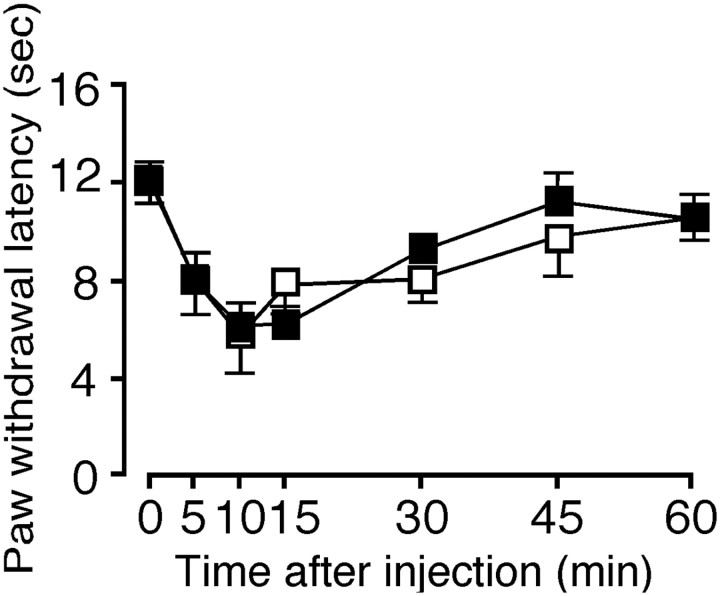
To confirm this P2Y2 receptor involvement, we examined the effect of UTP in mice (Fig. 4). UTP was found to cause thermal hyperalgesia with a time course similar to that observed in ATP injection. Furthermore, TNP–ATP could not prevent the UTP-induced thermal hyperalgesia, suggesting that P2Y2 receptors are involved in ATP-induced thermal hyperalgesia in mice.
Figure 4.
UTP induces thermal hyperalgesia in mice. Behavioral analyses in response to UTP (100 nmol) injection similar to Figure 1 in wild-type mice pretreated with TNP–ATP (50 nmol) (□) or saline (•). Values are expressed as mean ± SE; n = 6 for each group.
Discussion
In this study, we demonstrate the in vivo interaction of ATP with TRPV1. ATP could be involved in TRPV1-mediated thermal hyperalgesia through both P2X and P2Y receptors. However, P2Y receptors seem to be involved more predominantly, because the hyperalgesia was little affected by the P2X receptor inhibitor TNP–ATP. The existence of such a mechanism between P2Y receptors and TRPV1 is consistent with the observation that ATP-evoked nociceptive behavior in mice is only partially reduced by disruption of the P2X3 gene (Cockayne et al., 2000; Souslova et al., 2000). It has been well documented that signaling by ATP through sensory neuron-specific P2X3 and P2X2/3 receptors mediates an acute nociceptive pathway contributing to the pain of tissue damage (North and Barnard, 1997; Ralevic and Burnstock, 1998; Tsuda et al., 2000; Dunn et al., 2001). ATP could act on both ionotropic and metabotropic receptors to initiate and maintain the nociceptive responses in concert.
In TRPV1-transfected HEK293 cells, pharmacological studies have concluded that P2Y1 receptors are predominantly involved in ATP-induced potentiation or sensitization of TRPV1 (Tominaga et al., 2001). Our present results indicated that P2Y2 rather than P2Y1 receptors are likely to mediate the ATP-induced potentiation of capsaicin-evoked responses in mouse DRG neurons and in ATP-induced thermal hypersensitivity in vivo. Consistent with this hypothesis, P2Y2 mRNA, but not P2Y1 mRNA, is coexpressed with TRPV1 mRNA in rat DRG neurons (Fig. 3), and UTP injection causes thermal hyperalgesia in mice (Fig. 4). Together, these data suggest that P2Y2 receptors mediate ATP-induced hypersensitivity in mammals. A behavioral analysis with P2Y2-deficient mice would confirm our conclusion. P2Y2 receptor activation leads to TRPV1 potentiation in a relatively short time course. In addition, ATP and UTP have been reported recently to cause cAMP response element-binding protein (CREB) phosphorylation, which is likely to activate gene expression through P2Y2 receptor activation (Molliver et al., 2002). P2Y2 receptor activation could increase intracellular Ca2+ levels, leading to various outcomes including CREB phosphorylation, activation of phospholipase A2, and the consequent liberation of arachidonic acid, the rate-limiting step in prostaglandin formation (Molliver et al., 2002; Zimmermann et al., 2002). This Ca2+ mobilizing process could occur more slowly than the effects on TRPV1. Both fast and slow signals downstream of P2Y2 receptor activation might exist in native cells and contribute coordinately to hyperalgesia.
P2Y2 receptors confer responsiveness to UTP and ATP to a similar extent, suggesting a possible role for UTP as an important component of proalgesic response in the context of tissue injury. UTP has been reported to be released from ruptured cells (Anderson and Parkinson, 1997; Lazarowski et al., 2000). In addition to non-neuronal cells, ATP can be released from a subset of small primary afferent nerves in response to capsaicin (Sawynok and Sweeney, 1989), suggesting possible autocrine and paracrine mechanisms for the exacerbation of pain. A similar context can be imagined for the action of UTP in tissue damage. Therefore, UTP as well as ATP should be taken into account when purinergic contributions through P2Y receptors to pain sensation are examined.
Footnotes
This work was supported by grants from the Ministry of Education, Culture, Sports, Science and Technology of Japan, The Japan Health Sciences Foundation, and The Sumitomo Foundation. We thank Dr. D. Julius (University of California, San Francisco, San Francisco, CA) for supplying TRPV1-deficient mice and M. J. Caterina (Johns Hopkins University, Baltimore, MD) for his critical reading of this manuscript.
Correspondence should be addressed to M. Tominaga, Department of Cellular and Molecular Physiology, Mie University School of Medicine, Tsu, Mie 514-8507, Japan. E-mail: tominaga@doc.medic.mie-u.ac.jp
Copyright © 2003 Society for Neuroscience 0270-6474/03/236058-05$15.00/0
References
- Anderson CM, Parkinson FE ( 1997) Potential signaling roles for UTP and UDP: sources, regulation and release of uracil nucleotides. Trends Pharmacol Sci 18: 387–392. [DOI] [PubMed] [Google Scholar]
- Caterina MJ, Julius D ( 2001) The vanilloid receptor: a molecular gateway to the pain pathway. Annu Rev Neurosci 24: 487–517. [DOI] [PubMed] [Google Scholar]
- Caterina MJ, Schumacher MA, Tominaga M, Rosen TA, Levine JD, Julius D ( 1997) The capsaicin receptor: a heat-activated ion channel in the pain pathway. Nature 389: 816–824. [DOI] [PubMed] [Google Scholar]
- Caterina MJ, Leffler A, Malmberg AB, Martin WJ, Trafton J, Petersen-Zeitz KR, Koltzenburg M, Basbaum AI, Julius D ( 2000) Impaired nociception and pain sensation in mice lacking the capsaicin receptor. Science 288: 306–313. [DOI] [PubMed] [Google Scholar]
- Chen CC, Akopian AN, Sivilotti L, Colquhoun D, Burnstock G, Wood JN ( 1995) A P2X purinoceptor expressed by a subset of sensory neurons. Nature 377: 428–431. [DOI] [PubMed] [Google Scholar]
- Cockayne DA, Hamilton SG, Zhu QM, Dunn PM, Zhong Y, Novakovic S, Malmberg AB, Cain G, Berson A, Kassotakis L, Hedley L, Lachnit WG, Burnstock G, McMahon SB, Ford AP ( 2000) Urinary bladder hyporeflexia and reduced pain-related behaviour in P2X3-deficient mice. Nature 407: 1011–1015. [DOI] [PubMed] [Google Scholar]
- Cook SP, McCleskey EW ( 2002) Cell damage excites nociceptors through release of cytosolic ATP. Pain 95: 41–47. [DOI] [PubMed] [Google Scholar]
- Davis JB, Gray J, Gunthorpe MJ, Hatcher JP, Davey PT, Overend P, Harries MH, Latcham J, Clapham C, Atkinson K, Hughes SA, Rance K, Grau E, Harper AJ, Pugh PL, Rogers DC, Bingham S, Randall A, Sheardown SA ( 2000) Vanilloid receptor-1 is essential for inflammatory thermal hyperalgesia. Nature 405: 183–187. [DOI] [PubMed] [Google Scholar]
- Dunn PM, Zhong Y, Burnstock G ( 2001) P2X receptors in peripheral neurons. Prog Neurobiol 65: 107–134. [DOI] [PubMed] [Google Scholar]
- Fukuoka T, Kondo E, Dai Y, Hashimoto N, Noguchi K ( 2001) Brain-derived neurotrophic factor increases in the uninjured dorsal root ganglion neurons in selective spinal nerve ligation model. J Neurosci 21: 4891–4900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hashimoto N, Yamanaka H, Fukuoka T, Obata K, Mashimo T, Noguchi K ( 2001) Expression of hepatocyte growth factor in primary sensory neurons of adult rats. Brain Res Mol Brain Res 97: 83–88. [DOI] [PubMed] [Google Scholar]
- Huang SM, Bisogno T, Trevisani M, Al-Hayani A, De Petrocellis L, Fezza F, Tognetto M, Petros TJ, Krey JF, Chu CJ, Miller JD, Davies SN, Geppetti P, Walker JM, Di Marzo V ( 2002) An endogenous capsaicin-like substance with high potency at recombinant and native vanilloid VR1 receptors. Proc Natl Acad Sci USA 99: 8400–8405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hwang SW, Cho H, Kwak J, Lee SY, Kang CJ, Jung J, Cho S, Min KH, Suh YG, Kim D, Oh U ( 2000) Direct activation of capsaicin receptors by products of lipoxygenases: endogenous capsaicin-like substances. Proc Natl Acad Sci USA 97: 6155–6160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lang PM, Tracey DJ, Irnich D, Sippel W, Grafe P ( 2002) Activation of adenosine and P2Y receptors by ATP in human peripheral nerve. Naunyn Schmiedebergs Arch Pharmacol 366: 449–457. [DOI] [PubMed] [Google Scholar]
- Lazarowski ER, Boucher RC, Harden TK ( 2000) Constitutive release of ATP and evidence for major contribution of ecto-nucleotide pyrophosphatase and nucleoside diphosphokinase to extracellular nucleotide concentrations. J Biol Chem 275: 31061–31068. [DOI] [PubMed] [Google Scholar]
- Leon C, Hechler B, Freund M, Eckly A, Vial C, Ohlmann P, Dierich A, LeMeur M, Cazenave JP, Gachet C ( 1999) Defective platelet aggregation and increased resistance to thrombosis in purinergic P2Y1 receptor-null mice. J Clin Invest 104: 1731–1737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lewis C, Neldhart S, Holy C, North RA, Buell G, Surprenant A ( 1995) Coexpression of P2X2 and P2X3 receptor subunits can account for ATP-gated currents in sensory neurons. Nature 377: 432–435. [DOI] [PubMed] [Google Scholar]
- Minke B, Cook B ( 2002) TRP channel proteins and signal transduction. Physiol Rev 82: 429–472. [DOI] [PubMed] [Google Scholar]
- Molliver DC, Cook SP, Carlsten JA, Wright DE, McCleskey EW ( 2002) ATP and UTP excite sensory neurons and induce CREB phosphorylation through the metabotropic receptor, P2Y2. Eur J Neurosci 16: 1850–1860. [DOI] [PubMed] [Google Scholar]
- North AN, Barnard EA ( 1997) Nucleotide receptors. Curr Opin Neurobiol 7: 346–357. [DOI] [PubMed] [Google Scholar]
- Numazaki M, Tominaga T, Toyooka H, Tominaga M ( 2002) Direct phosphorylation of capsaicin receptor VR1 by PKCϵ and identification of two target serine residues. J Biol Chem 277: 13375–13378. [DOI] [PubMed] [Google Scholar]
- Ralevic V, Burnstock G ( 1998) Receptors for purines and pyrimidines. Pharmacol Rev 50: 413–492. [PubMed] [Google Scholar]
- Sawynok J, Sweeney MI ( 1989) The role of purines in nociception. Neuroscience 32: 557–569. [DOI] [PubMed] [Google Scholar]
- Souslova V, Cesare P, Ding Y, Akopian AN, Stanfa L, Suzuki R, Carpenter K, Dickenson A, Boyce S, Hill R, Nebenuis-Oosthuizen D, Smith AJ, Kidd EJ, Wood JN ( 2000) Warm-coding deficits and aberrant inflammatory pain in mice lacking P2X3 receptors. Nature 407: 1015–1017. [DOI] [PubMed] [Google Scholar]
- Sugiura T, Tominaga M, Katsuya H, Mizumura K ( 2002) Bradykinin lowered the threshold temperature for heat activation of vanilloid receptor 1. J Neurophysiol 88: 544–548. [DOI] [PubMed] [Google Scholar]
- Szallasi A, Blumberg PM ( 1999) Vanilloid (capsaicin) receptors and mechanisms. Pharmacol Rev 51: 159–211. [PubMed] [Google Scholar]
- Tominaga M, Caterina MJ, Malmberg AB, Rosen TA, Gilbert H, Skinner K, Raumann BE, Basbaum AI, Julius D ( 1998) The cloned capsaicin receptor integrates multiple pain-producing stimuli. Neuron 21: 531–543. [DOI] [PubMed] [Google Scholar]
- Tominaga M, Wada M, Masu M ( 2001) Potentiation of capsaicin receptor activity by metabotropic ATP receptors as a possible mechanism for ATP-evoked pain and hyperalgesia. Proc Natl Acad Sci USA 98: 6951–6956. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tsuda M, Ueno S, Inoue K ( 1999) In vivo pathway of thermal hyperalgesia by intrathecal administration of α,β-methylene ATP in mouse spinal cord: involvement of the glutamate-NMDA receptor system. Br J Pharmacol 127: 449–456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tsuda M, Koizumi S, Kita A, Shigemoto Y, Ueno S, Inoue K ( 2000) Mechanical allodynia caused by intraplantar injection of P2X receptor agonist in rats: involvement of heteromeric P2X2/3 receptor signaling in capsaicin-insensitive primary afferent neurons. J Neurosci 20:RC90( 1–5). [DOI] [PMC free article] [PubMed] [Google Scholar]
- von Kugelgen I, Wetter A ( 2000) Molecular pharmacology of P2Y-receptors. Naunyn Schmiedebergs Arch Pharmacol 362: 310–323. [DOI] [PubMed] [Google Scholar]
- Wood JN, Perl ER ( 1999) Pain. Curr Opin Genet Dev 9: 328–332. [DOI] [PubMed] [Google Scholar]
- Woolf CJ, Salter MW ( 2000) Neuronal plasticity: increasing the gain in pain. Science 288: 1765–1768. [DOI] [PubMed] [Google Scholar]
- Zimmermann K, Reeh PW, Averbeck B ( 2002) ATP can enhance the proton-induced CGRP release through P2Y receptors and secondary PGE2 release in isolated rat dura mater. Pain 97: 259–265. [DOI] [PubMed] [Google Scholar]
- Zygmunt PM, Petersson J, Andersson DA, Chuang H, Sorgard M, Di Marzo VD, Julius D, Hogestatt ED ( 1999) Vanilloid receptors on sensory nerves mediate the vasodilator action of anandamide. Nature 400: 452–457. [DOI] [PubMed] [Google Scholar]