Abstract
Recent research shows that blunted cardiovascular and cortisol reactions to acute psychological stress are associated with adverse behavioural and health outcomes: depression, obesity, bulimia, and addictions. These outcomes may reflect suboptimal functioning of the brain’s fronto-limbic systems that are needed to regulate motivated behaviour in the face of challenge. In support of this, brain imaging data demonstrate fronto-limbic hypoactivation during acute stress exposure. Those demonstrating blunted reactions also show impairments of motivation, including lower cognitive ability, more rapid cognitive decline, and poorer performance on motivation-dependent tests of lung function. Persons exhibiting blunted stress reactivity display well established temperament characteristics, including neuroticism and impulsivity, characteristic of various behavioural disorders. Notably, the outcomes related to blunted stress reactivity are similar to those that define Reward Deficiency Syndrome. Accordingly, some individuals may be characterised by a broad failure in cardiovascular and cortisol responding to both stress and reward, reflecting fronto-limbic dysregulation. Finally, we proffer a model of blunted stress reactivity, its antecedents and sequelae, and identify future research priorities.
Keywords: Behaviour, Cognitive ability, Cardiovascular activity, Cortisol, Blunted stress reactivity, Health, Neural hypoactivation
1. Introduction
Most stressful encounters are short-lived, lasting seconds, minutes, hours at most, and what is now clear is that such acute stress exposures activate the sympatho-medullary (SAM) system, perturbing cardiovascular activity, and the hypothalamic pituitary-adrenal (HPA) axis, altering cortisol levels. Under optimal conditions, specific brain structures assess the threat and develop an adaptive pattern of autonomic and endocrine outflow to support the physiological and behavioural responses needed to meet the present homeostatic challenge (Lovallo, 2016; McEwen and Gianaros, 2011). Sympathetic nervous system responses to stress engage the cardiovascular system and adrenal medulla to produce a coordinated preparation for fight-or-flight efforts. Along with this, the hypothalamic-pituitary-adrenocortical system produces a significant rise in circulating cortisol which aids in liberation of stored energy and also helps to regulate the stress response in both the periphery and in the central nervous system. Stress responses resolve when the challenge has been eliminated. Autonomic, and endocrine control over stress responses may be altered in persons with particular genotypes or exposed to early-life adversity (Lovallo, 2016; McEwen and Gianaros, 2011). In such persons, physiological, behavioural, and cognitive processes may be altered, health behaviours biased toward maladaptive practices, and health outcomes worsened. More recent research has shown that, along with autonomic and endocrine modifications, early stress exposure may change the regulation of inflammatory processes with consequences for brain function, peripheral regulation of the stress response, and the ability of the system to manage immune system responses and tissue inflammation (Gianaros et al., 2014, 2013). The normal regulation of these stress responsive systems has been described in detail elsewhere (Lovallo, 2016; McEwen and Stellar, 1993). The goal of the present paper is to discuss the health and behavioural consequences of blunted cardiovascular and cortisol reactivity to stress.
As indicated, it is clear that individuals differ markedly in their cardiovascular and cortisol reactions to acute psychological stress. This biological variability has proved fertile territory for researchers over the years. For the most part, research, at least in the realm of cardiovascular stress reactions, has been guided by the reactivity hypothesis (Obrist, 1976) which argues compellingly that those who consistently show exaggerated cardiovascular reactions to acute stress will be at increased risk of subsequent cardiovascular disease. There is now substantial evidence in favour of this, with population studies attesting to a link between heightened cardiovascular reactions to laboratory stress exposures and hyper-tension (e.g., Carroll et al., 2011, 2003), atherosclerosis (e.g., Barnett et al., 1997), increased left ventricular mass (e.g., Kapuku et al., 1999), and even increased cardiovascular disease mortality (Carroll et al., 2012a). Qualitative reviews (e.g., Treiber et al., 2003) confirm the contention that exaggerated cardiovascular reactivity presages poorer cardiovascular health, although it should be conceded that effect sizes from the latter are generally small. By implication, low or blunted cardiovascular reactivity has long been presumed to be benign or even protective. However, recent evidence strongly indicates that this is far from the case. Blunted cardiovascular, as well as cortisol, stress reactivity is implicated in a range of adverse behavioural and health outcomes.
The perspective we are advancing is based on the critical role that normal stress responsivity plays in adaptive responses to the constant demands the environment places on survival. In this view, stress responses represent a systems-level response to threats to homeostasis. By extension, optimal responses to those threats require appropriate integration of the system at multiple levels including peripheral physiology, the brainstem and hypothalamus, and the cortex and limbic system. From this perspective, physiological responses to stress should occur within the normal range for a given homeostatic threat. By definition, deviations from a normative response may signal poor systems integration and therefore diminished homeostatic control. We consider that exaggerated stress responses have negative consequences for health, as described above. However, similarly blunted stress responses may also signal poor homeostatic regulation, with a different set of consequences for health and behaviour.
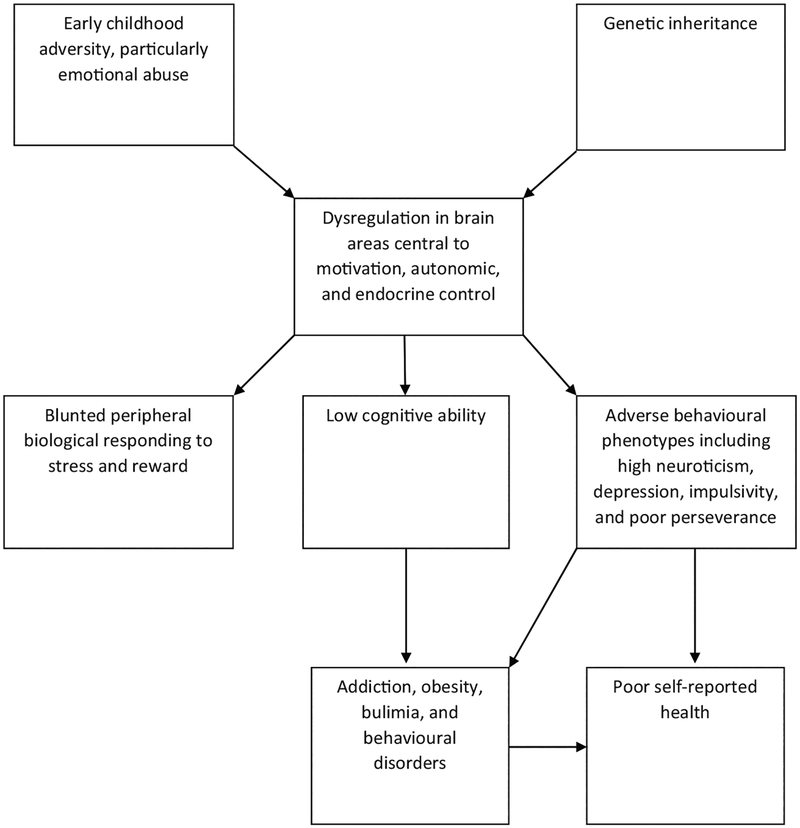
In this review, we also move toward a tentative model of blunted stress reactivity, by: first, enumerating its seemingly diverse behavioural and health corollaries, such as addiction, obesity, and poor self-reported health; second, by discussing the possible origins of blunted stress reactivity in genetic polymorphic variation and early life adversity; third, by suggesting possible pathways that link genetic inheritance and early adversity through sub-optimal functioning of brain areas central to both motivation and autonomic regulation to other more proximal corollaries of blunted stress reactions, such as relative poor cognitive ability and adverse behavioural phenotypes including depression, neuroticism, and poor impulse control; fourth, by considering these as increasing the risk of the more distal outcomes such as addiction, obesity, behaviour disorders, and poor self-reported health. This model regards blunted cardiovascular and cortisol stress reactivity, not as a cause, but rather as a marker of motivational dysregulation which, we propose, is the ultimate psychological determinant of the adverse health and behavioural outcome. This model is outlined in Fig. 1.
Fig. 1.
Provisional model of blunted biological stress reactivity; from this perspective, blunted reactivity is regarded as a marker rather than a cause of endpoint behavioural and health outcomes.
1.1. A tale of two cohort studies
Two large scale community studies have contributed much to our understanding of the corollaries of blunted stress reactivity and, accordingly, merit more than a cursory description.
1.1.1. The West of Scotland Twenty-07 Study
The first is the West of Scotland Twenty-07 Study (Ford et al., 1994). Established in 1987, its principal mission was to investigate the processes that generate and maintain socio-demographic differences in health. Participants, all from the Glasgow area, were chosen randomly with the probability proportional to the overall population of the same age within a postcode area. Thus, the sample was selected as a clustered, random, stratified sample of three narrow age cohorts who were 15, 35, and 55 years old at entry to the study; the achieved sample sizes in 1987 were 1009, 985, and 1042 for the three age cohorts, respectively. There was a fairly even gender split and an approximately equal number of manual and non-manual occupational households. However, the sample was predominantly Caucasian, reflecting the demographics of the West of Scotland population from which it was drawn. In all, there were five waves of data collection. Stress testing was undertaken at wave 3, in 1995/6, and consisted of exposure to the paced auditory serial addition test (PASAT), a test that requires attention and memory as well as simple arithmetic. Blood pressure and heart rate were recorded prior to and during the PASAT. The sample at this time point comprised 592 24-year olds, 624 44-year olds, and 431 63-year olds. Aside from yielding data on cardiovascular reactions to acute stress, the study also included detailed socio-demographic, anthropometric and health assessments (including self-reported smoking, self-rated health, forced expiratory volume in one second (FEV1), and symptoms of depression and anxiety), as well as measures of cognitive ability throughout.
1.1.2. The Dutch Famine Birth Cohort Study
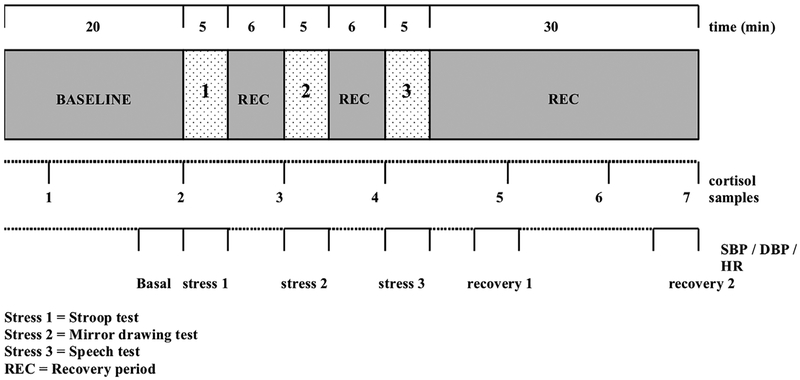
The second study of importance is the Dutch Famine Birth Cohort Study (Ravelli et al., 1998). It was established to investigate the subsequent health consequences of in utero exposure to severe maternal nutritional deprivation. Participants, 2414 men and women, were selected from among those born in Amsterdam between November 1943 and February 1947. In the winter of 1944/45, the Netherlands, in the densely populated western areas, including Amsterdam, was exposed to famine, known in Dutch as the Hongerwinter. The famine was the result of a German blockade which had cut off food and fuel shipments from rural areas to the towns and cities. It is estimated that some 22,000 Dutch citizens died as a result. The Dutch Famine Birth Cohort Study has, to date, comprised four waves of data collection: 1995/7, 2002/4, 2008/9 and 2012/3. During the second wave, participants were exposed to a battery of three commonly used stress tasks: the Stroop test, mirror drawing, and public speaking, and cardiovascular activity and cortisol were measured. The protocol is depicted in Fig. 2. Members of the cohort, 1423, who lived in the Netherlands and whose address was known in 2002, were invited to the clinic; 740 attended. Serendipitously, the other measures available in the West of Scotland Study were also taken as part of the Dutch Famine Birth Cohort Study, frequently using identical instruments.
Fig. 2.
Schematic representation of the psychological stress protocol in the Dutch Famine Birth Cohort study.
1.1.3. Exaggerated cardiovascular reactivity and hypertension in the West of Scotland and Dutch Studies
It is perhaps worth pointing out that in both the West of Scotland Study and the Dutch Famine Birth Cohort Study exaggerated blood pressure reactions to acute stress exposures are associated prospectively with hypertension prevalence (Carroll et al., 2012b, 2011). Thus, one of these studies’ outcomes is very much in line with the main proposition of the original reactivity hypothesis.
2. The behavioural and health corollaries of blunted stress SAM and HPA reactivity
2.1. Addiction
Smokers (e.g., al’Absi, 2006; al’Absi et al., 2005; Ginty et al., 2014; Phillips et al., 2009b) and those with alcohol (Lovallo, 2006; Panknin et al., 2002) and other substance dependencies (Brenner and Beauchaine, 2011; Lovallo et al., 2000) have been found consistently to have blunted cardiovascular and/or cortisol reactions to acute psychological stress.
Pathological gamblers (Paris et al., 2010) and those identified as exercise dependent (Heaney et al., 2011) also show relatively attenuated cardiovascular and cortisol stress reactions. This suggests that the link between addiction and blunted stress reactivity does not primarily reflect the chronic or acute effects of ingested toxins on autonomic function. This is reinforced in the case of smoking by the results of recent analyses of data from the Dutch Famine Birth Cohort Study confirming that smokers were characterised by blunted cardiovascular and cortisol stress reactivity compared to both ex-smokers and never smokers; however, there was no association, among smokers and ex-smokers, between packs per day × number of years smoked and stress reactivity, nor for current smokers between number of cigarettes presently smoked per day and reactivity (Ginty et al., 2014). It is also unlikely that the association between smoking and cardiovascular and cortisol reactions to acute stress is an artifact of nicotine’s acute effects on physiology attributable to the temporary abstinence enforced by a laboratory stress testing protocol (Roy et al., 1994). Blunted cardiovascular and cortisol reactions have been observed during laboratory stress exposure in both smokers who abstained from smoking and smokers who were permitted to smoke ad libitum (al’Absi et al., 2003). Further, blunted cardiovascular stress reactions have been reported in smokers who wore a nicotine patch throughout the stress exposure (Girdler et al., 1997). Along with the finding that blunted stress reactivity is also typical of the adolescent offspring of alcoholics, who are not themselves alcohol users and/or abusers, the data strongly imply that blunted stress reactivity may predate dependencies and, indeed, may be a marker of susceptibility (Lovallo, 2006). The observation that those with blunted cortisol stress reactions are more likely to relapse from a smoking cessation programme (al’Absi et al., 2006) conforms to the contention above and also suggests that blunted stress reactivity may have considerable prognostic value.
2.2. Adiposity and obesity
Turning now to adiposity and obesity, data from the West of Scotland Study indicated that blunted heart rate reactions to stress were also negatively associated with body mass index (BMI) and waist hip ratio, as well as being characteristic of those who were obese; in prospective analyses, low heart rate reactivity also predicted who was to remain or become obese five years later. These results were supported and extended by outcomes from the Dutch Famine Birth Cohort Study. Those with a greater BMI, waist hip ratio, and those categorized as obese again exhibited attenuated heart rate stress reactivity; they also displayed reduced cortisol stress reactivity, and, once again, blunted reactivity was associated with an increased likelihood of remaining or becoming obese four to seven years later (Phillips et al., 2012). As before, the cross-sectional and prospective associations emerging from the two studies withstood correction for a range of possible confounders, including in this case symptoms of depression. Other researchers have also observed a negative association between obesity and heart rate stress reactivity (e.g., Burch and Allen, 2014; Jones et al., 2012).
2.3. Disordered eating and bulimia
Blunted stress reactivity has also been found to characterize bulimia and disordered eating behaviour consistent with bulimia. In a study that compared controls and individuals with a diagnosis of bulimia, the latter showed significantly attenuated heart rate and blood pressure reactions to acute stress (Koo-Loeb et al., 1998). In a more recent study, women with marked symptoms of disordered eating, including self-induced vomiting, and the same number of healthy controls were selected from extensive questionnaire screening. Those reporting disordered eating behaviour showed attenuated heart rate and cortisol stress reactions compared to the controls (Ginty et al., 2012a). Inpatients with eating disorders show blunted cortisol and alpha-amylase, a proposed marker of sympathetic activation, in response to a socially demanding stress task (Het et al., 2015).
2.4. Poor self-reported health
Self-reported health predicts all-cause mortality, independently of objective medical status and behavioural risk factors (e.g., Idler and Benyamini, 1997). Since both exaggerated and blunted SAM and HPA reactions to acute stress exposure would appear to be associated with adverse health outcomes the question arises as to which has the greater implications for subjective well-being and perceived health. The health outcomes related to exaggerated reactivity, such as hypertension, tend to be somewhat covert and occult, whereas those associated with blunted reactivity, e.g., addiction and obesity, are much more overt and self-evident to the individual. Accordingly, it might be hypothesised that poorer self-reported health would tend to be associated with blunted rather than exaggerated stress reactions. Both the West of Scotland Study and the Dutch Famine Birth Cohort Study examined this issue. In the former, self-reported health was assessed with a single question, “Would you say that for someone your age your health is ....excellent, good, fair, poor?”. Since very few participants reported that their health was poor or excellent, the excellent and good categories were collapsed, as were the fair and poor, to yield a binary variable. Those reporting that their health was only fair or poor showed smaller cardiovascular reactions to the acute stress exposure (Phillips et al., 2009a). In the Dutch study, subjective health was measured by participants’ choice of excellent, very good, good, fair, or poor to the question, “How do you rate your health in general?” Again, because the self-report data were skewed, a binary good/poor variable was created. As above, it was blunted, not exaggerated, cardiovascular stress reactivity that was related to relatively poor subjective health; in addition, relatively poor self-reported health was also associated with blunted cortisol stress reactions (De Rooij and Roseboom, 2010). In both studies, these associations survived statistical adjustments for the usual range of potential confounders. Finally, in the West of Scotland study, self-reported health was also measured, using the same instrument, five years later. Blunted cardiovascular stress reactions were again linked to poorer self-reported health at this later time point and continued to predict subsequent poorer subjective health, even taking into account subjective health at the earlier time point; i.e., those who showed blunted stress reactions were more likely to experience deterioration in perceived health over time.
2.5. Depression
As some of the evidence linking depression and blunted stress reactions has been reviewed elsewhere (Carroll et al., 2009; Phillips, 2011), we can be reasonably brief. The West of Scotland analyses embarked from the expectation that symptoms of depression would be associated with exaggerated cardiovascular stress reactivity. This was based on a meta-analysis of a number of small scale studies. The authors reported a positive association between depression and reactivity, although none of the aggregate effects were statistically significant (Kibler and Ma, 2004). However, in the West of Scotland study depression scores on the Hospital Anxiety and Depression Scale (HADS: Zigmond and Snaith, 1983) were negatively related to both heart rate and systolic blood pressure reactivity; i.e., symptoms of depression were associated with blunted rather than exaggerated stress reactions (Carroll et al., 2007). The same direction of association for cardiovascular reactivity and symptoms of depression also emerged from analyses of data from the Dutch Famine Birth Cohort Study, again using the HADS (de Rooij et al., 2010); in addition, it was lower not higher cortisol reactivity that was related to higher depression symptoms. Both studies adjusted statistically for a broad range of possible confounders including antihypertensive and antidepressant medication. Further, in both studies similar associations were observed for symptoms of anxiety. Contemporary with and subsequent to these analyses, a number of other studies have now reported negative associations between symptoms of depression and stress reactivity in a range of samples (Brindle et al., 2013; Franzen and Brinkmann, 2015; Schwerdtfeger and Rosenkaimer, 2011; York et al., 2007), as well as between major depressive disorder and reactivity (Rottenberg et al., 2007; Salomon et al., 2009, 2013). Cross sectional associations between blunted stress reactivity and symptoms of anxiety have also been reported by others (Souza et al., 2015). Finally, in a prospective analysis of data from the West of Scotland Study, blunted heart rate reactions were associated with more symptoms of depression five years later, even when controlling for symptoms at the earlier time point, i.e., blunted heart rate reactivity was associated with any subsequent deterioration in symptoms of depression (Phillips et al., 2011b). Overall, the associations between blunted stress reactivity and outcomes such as depression, obesity, addiction, and bulimia would all appear to be largely independent of one another.
2.6. Personality and negative behavioural traits
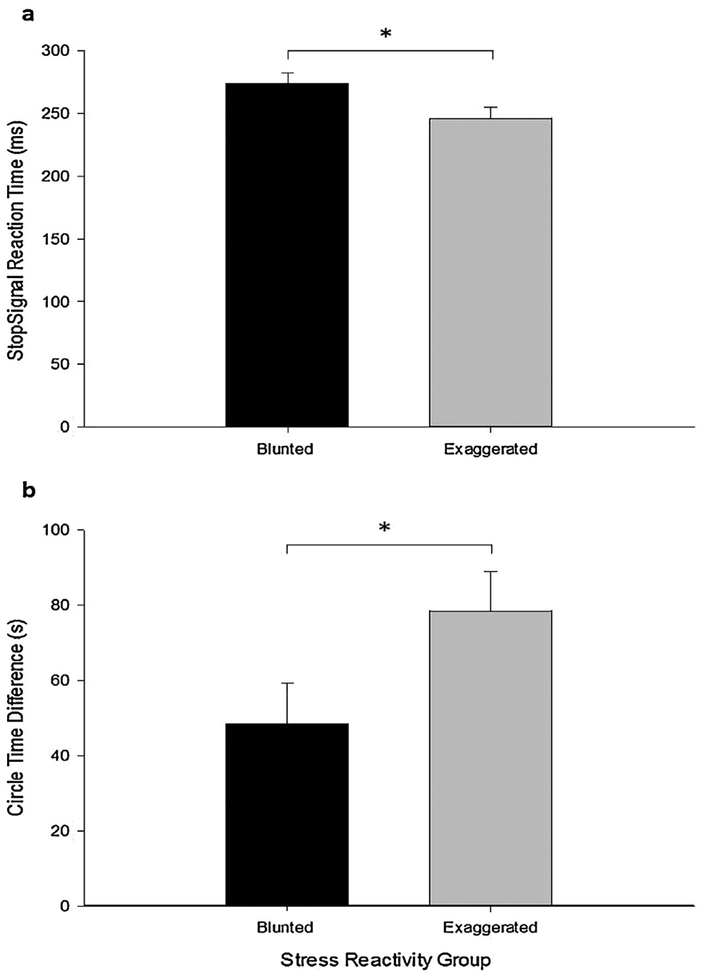
There is emerging evidence that blunted cardiovascular and/or cortisol reactions to acute stress may be typical of particular personality traits and stable behavioural characteristics. For example, in an analysis of data from the Dutch Famine Birth Cohort Study we found that those high in neuroticism and low in openness were characterised by blunted cardiovascular and cortisol reactions to the stress task battery, even though they reported experiencing greater levels of stress (Bibbey et al., 2013). Further, higher levels of impulsivity, measured via questionnaires, have also been related to diminished heart rate responses to acute psychological stress (Allen et al., 2009). In a study of pre-adolescent children, impulsivity, assessed by two standard behavioural inhibition tasks (one where participants were asked to draw a circle at their natural pace and then as slowly as possible, and a Go-NoGo task where they had to inhibit pre-potent responses), and maternal self-report was associated with blunted heart rate reactions to a mental arithmetic stress (Bennett et al., 2014). It is also worth pointing out that the self-perceived stressfulness of the stress task was not related to any of the measures of impulsivity. This result has recently been replicated in a study of undergraduates where blunted and exaggerated heart rate reactors were selected from stress testing a large screening sample, again using a standard mental arithmetic challenge (Bibbey et al., 2016). Selected participants were subsequently exposed to inhibitory control (stop signal) and motor impulsivity (circle drawing) tasks, analogous to those used in the earlier study of school children. Blunted stress reactors showed greater impulsivity on both behavioural assessments (see Fig. 3). Self-reported stressfulness, self-reported stress task engagement, and mental arithmetic performance did not differ between the stress reactor groups.
Fig. 3.
Mean (SE) (a) stop signal reaction time, and (b) circle time difference for the blunted and exaggerated stress reactivity groups.
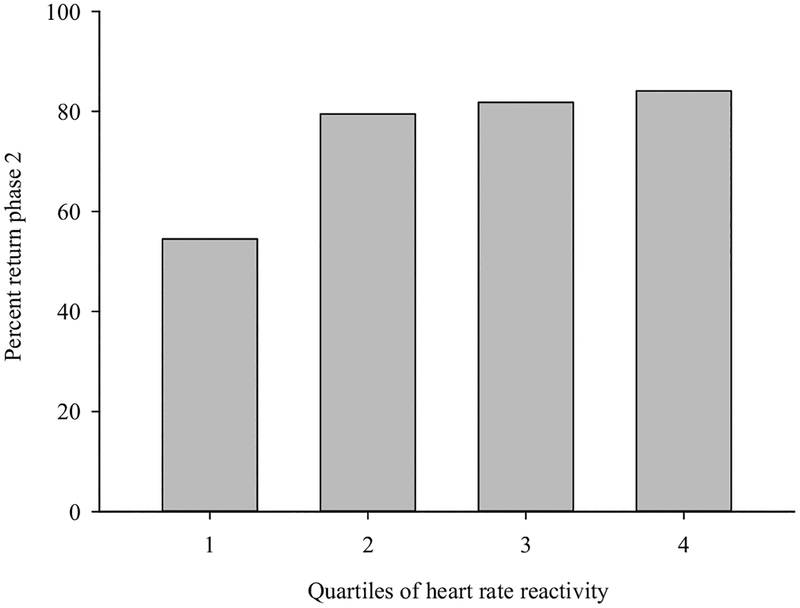
Perseverance is another characteristic that could conceivably be associated with the blunted stress reactivity phenotype. As indicated above, smokers who display the most blunted stress reactions are most likely to relapse in smoking cessation programmes. This was examined further in a study of 176 high school students who were stress-tested, using a mental arithmetic task, and cardiac reactivity recorded; a year later, when they were at university, all participants were contacted to complete a simple and undemanding on-line assessment (Ginty et al., 2015). Twenty-five percent of participants failed to complete the on-line assessment despite repeated prompts from the same researcher who had conducted the original stress testing session. Crucially, the non-completers were characterised by blunted heart rate and cardiac output reactions to the earlier stress task exposure (see Fig. 4, which illustrates the findings for heart rate reactivity). It is again worth stating that the association was independent of stress task performance. These results add to the idea that individual differences in stress reactivity may have implications for likely completion of multi-session intervention programmes, as well as for selection bias in longitudinal stress reactivity studies, as loss to follow-up would not appear to be arbitrary, but rather skewed towards those with blunted stress responses, with all the attendant adverse health and behavioural corollaries. Finally, there is also accumulating evidence that blunted stress reactions typify individuals who consistently display antisocial behaviour (e.g., De Vries-Bouw et al., 2011), have a conduct disorder (Fairchild et al., 2008), or have been diagnosed with attention deficit hyperactivity disorder (e.g., Pesonen et al., 2011)).
Fig. 4.
Percentage study completion rate by quartiles of heart rate reactivity.
2.7. Cognitive ability
In the Dutch Famine Birth Cohort Study, cognitive ability was assessed using the Alice Heim-4 test, a measure of general verbal and numerical ability, and two memory tasks, one requiring immediate recall and the other involving delayed recall. Blunted cardiovascular and cortisol stress reactivity was associated with poorer performance in all three tasks (Ginty et al., 2012b). In the West of Scotland Study, cognitive ability, again measured independently of the stress task, was assessed five and 12 years after the stress testing session, using the Alice Heim-4 and choice reaction time. Heart rate reactivity was again positively associated with performance on both tasks. Choice reaction time lengthened between the five and 12 year follow-ups in the oldest cohort in this study. Blunted heart reactivity was associated with a more rapid decline over time in choice reaction time speed in these older participants (Ginty et al., 2011, 2012b). Given, the imperative of predicting susceptibility to age-related cognitive decline, the size of the latter association clearly recommends further scrutiny of blunted stress reactivity in this context. Both the cross-sectional and longitudinal results described above have received more recent confirmation. Low heart rate reactivity has been reported to be associated with poorer fluid intelligence and perceptual reasoning in children (Gao et al., 2015). Cognitive ability was assessed at a 23-year follow-up of a cohort originally stress tested as young adults. Lower systolic, but not diastolic, blood pressure stress reactions were consistently associated with poorer subsequent cognitive performance (Yano et al., 2016).
2.8. FEV1
The most commonly applied test of lung function is forced expiratory volume in one second (FEV1). Aside from lung function per se, a major contributor to FEV1 is intrinsic motivation (Crim et al., 2011). The West of Scotland analyses yielded a positive association between FEV1 and heart rate reactions in middle-aged men and women; those with smaller cardiovascular stress reactions achieved significantly lower FEV1 scores, even after adjusting for smoking (Carroll et al., 2012c, 2013). It is also worth pointing out that in addition to smoking, statistical adjustment was undertaken for a range of demographic and health behaviour variables including those already known to be associated with blunted stress reactivity e.g., baseline cardiovascular activity, age, sex, socio-economic status, BMI, depression, and anti-hypertensive medication. The same result emerged from the Dutch Famine Birth Cohort Study; in addition, cortisol reactivity was also found to be positively associated with FEV1 (Carroll et al., 2013). Again, the findings survived adjustment for the same broad range of potential confounders, including stress task engagement and impact, suggesting again that low FEV1 was not simply a reflection of participants’ conscious unwillingness to expend effort.
3. The origins of blunted stress reactivity
In examining the sources of altered stress reactivity, we may consider that the response to a homeostatic challenge is conditioned by mechanisms at three ascending levels in the system: (a) peripheral physiology, (b) the hypothalamus and brainstem, and (c) the limbic system and prefrontal cortex (Lovallo, 2011; Lovallo and Gerin, 2003). At the peripheral level, alterations in outflow via the autonomic nervous system or at the target tissues could result in either exaggerated or diminished response magnitudes. For example, diabetics have deficient sympathetic nervous system communication to target tissues due to peripheral autonomic neuropathy. Similarly, the hypothalamus and brainstem may respond more or less actively to any set of signals calling on homeostatic adjustments to counter potential threats to well-being. For example, borderline hypertensives in a resting state are nonetheless hyper-reactive to a novel laboratory environment (al’Absi and Lovallo, 1993). Finally, the limbic system and pre-frontal cortex operate as a unit in evaluating the nature of external events, forming response strategies, and enacting these responses in behavioural adjustments and in the physiological adjustments needed to support those behaviours. This higher level of integration is the primary concern of the present paper and a logical place to consider reactivity in the face of psychological stressors.
The amygdala is a key structure in forming acute psychological stress responses (Davis, 2000), and it is essential for normal reactions to sensory inputs and is indispensable in creating Pavlovian conditioned responses (Campeau and Davis, 1995; Rolls, 1972, 1992). As such, the amygdala is needed for both innate and acquired motivational responses to external events and for building up a repertoire of adaptive responses in the service of survival. The amygdala sends downward projections to the brainstem and hypothalamus (Davis, 1997) and, in relation to the present discussion, upward to what we may refer to as the limbic-prefrontal junction, a functional region including the convergence of the bed nuclei of the stria terminalis, nucleus accumbens, medial pre-frontal cortex, and anterior cingulate gyrus (Amaral, 1992; Halgren, 1992; Swanson, 2000). At this junction, bottom-up inputs from the amygdala interact with top-down signals from the dorsolateral pre-frontal cortex, an area that is engaged in working memory and online conscious evaluation of events (Goldman-Rakic, 1996). As such, the limbic-prefrontal junction becomes a point in the system where external events are invested with emotional significance and motivational properties capable of integrating feeling states, physiological outflow, and behavioural motivation (Drevets et al., 1997; Phillips et al., 2003). Extensive clinical evidence illustrates the devastating effects of damage to these areas or disruption of their inputs (Anderson et al., 1999; Damasio et al., 1994) in which cases, patients become unable to make decisions or form adaptive responses to motivationally significant situations.
Although it seems reasonable to conclude that the limbic system affords a key neural platform, the reasons why some individuals show blunted reactions to acute stress exposures remains to be fully determined. Nevertheless, on the basis of preliminary evidence we can usefully speculate on two broad classes of cause worthy of further scrutiny: genotype and early childhood adversity. A meta-analysis of twin studies of cardiovascular stress reactivity (Wu et al., 2010) revealed pooled heritability estimates ranging from 0.26 to 0.43, indicating a far from negligible contribution from our genes. However, as the authors plaintively observed, “..in spite of significant heritability emerging from twin studies, independently and consistently replicated gene variants that explain this heritability are still at large” (Wu et al., 2010, p. 66). The most likely polymorphisms are those involved in the regulation of neurotransmitters, such as noradrenalin, serotonin, monoamine oxidase, and dopamine. We have briefly reviewed their candidature elsewhere (Carroll et al., 2009), and, although promising, substantial further concerted research is required before definitive pronouncements can be made. Nevertheless, let us elaborate a little on dopamine release at the nucleus accumbens, which accompanies attention to reward stimuli and enactment of approach and avoidance behaviours (Jackson and Moghaddam, 2001; Stevenson and Gratton, 2003). Genetic variations in dopamine regulation have received extensive study for individual differences in responses to environmental inputs and motivated behaviour. One such genetic polymorphism (Val158Met, rs4680) increases the activity of the enzyme catechol-o-methyltransferase, thereby increasing the breakdown of dopamine at the synapse. This results in a lifelong variation in dopaminergic signaling that has an impact on behaviour (Axelrod, 1957; Matsumoto et al., 2003; Smolka et al., 2005). The Val158Met (rs4680) polymorphism appears to underlie individual differences in behaviours that depend on the striatum and prefrontal cortex (Akil et al., 2003; Egan et al., 2001). Val/Val homozygotes may differ from Met/Met homozygotes in affective temperament (Drabant et al., 2006), stress reactivity (Bouma et al., 2012), cognition (Malhotra et al., 2002), regulation of behaviour (Barnett et al., 1997; Schulz et al., 2012), and processing of reward stimuli (Tunbridge et al., 2012), all of which have potential implications for health behaviour and health outcomes (Goldman et al., 2005). In addition to genetically driven individual differences in the limbic-prefrontal junction, this same region is highly sensitive to the impact of early life experience (Brenhouse et al., 2013; Seamans and Yang, 2004). For example, recent evidence indicates that the Val158Met (rs4680) polymorphism contributes to diminished cortisol reactivity to stress in children exposed to early life adversity (Lovallo et al., 2016), and others found hypocortisolism among children experiencing adverse early care (Koss et al., 2016). The foregoing indicates that genetic polymorphisms and early life experience may both modify stress reactivity in ways that can condition behavioural dispositions and health outcomes.
Perhaps the most persuasive evidence implicating early life adversity comes from the Oklahoma Family Health Patterns Project (e.g., Lovallo, 2013). The project’s participants comprised a cohort of 426 healthy young adults with or without a family history of alcoholism. Regardless of family history, participants who had experienced high levels of psychological adversity before the age of 16 showed blunted heart rate and cortisol reactions to mental arithmetic and public speaking stress. They also showed poorer cognitive ability, higher behavioural impulsivity, and greater antisocial tendencies. A model is proposed whereby early adversity affects fronto-limbic function, which in turn is manifest in reduced stress reactivity, lower cognitive ability, and unstable affect regulation; this then increases the likelihood of impulsivity and risk taking, which in turn contributes to unhealthy behaviour and addiction risk. While promising, the model is yet to encompass all the corollaries of blunted stress reactivity, such as depression, which again has been strongly linked to childhood adversity. Supportive results come from studies in both the Netherlands and England. In the former, the cardiac stress reactions to public speaking was assessed in a large sample of adolescents; those who had experienced serious adversities between the ages of 0 and 15 displayed greater antisocial behaviour at 16 and also exhibited blunted cardiac reactions to the stress task (Sitjtsema et al., 2015). In the English study, exposure to traumatic events and cortisol stress reactivity were measured in 400 8 to 11-year old children. At an earlier time point when the children were 3-years old, the sort of parenting they were exposed to was assessed during home visits. Those children who had experienced more traumatic events and had been exposed to harsh, non-responsive parenting showed blunted cortisol stress reactions. Still other research illustrates the damaging impact of early institutional care on brain development and behaviour (Silvers et al., 2016; Tottenham, 2012). A common theme is that early adversity often results in maladaptive behavioural repertoires in adulthood and in modifications of physiological function that may converge on poor health outcomes.
Finally, in this context, it is worth briefly considering the issue of developmental trajectories of stress response patterns. Central here are the concepts of allostasis and allostatic load. The former refers to the processes by which the body attempts to maintain homeostasis in the face of environmental perturbations, whereas the latter refers to the wear and tear that results from either over exposure to stress and/or excessive or prolonged responding (McEwen, 2007). From this perspective, it is possible that the blunted stress reactivity phenotype emerges from allostatic load and initial excessive stress reactivity. On the other hand, others have argued that stress physiology is set early in life (Matthews and Phillips, 2010). Studies of stress responding across childhood could help resolve matters.
4. Motivational dysregulation and blunted stress reactivity
The association between exaggerated stress reactivity and adverse cardiovascular health outcomes is conceptually plausible and, in retrospect, even self-evident, given mechanisms such as metabolic uncoupling, auto-regulation, and shear stress. Much less intuitively obvious is the link between blunted stress reactivity and the diverse behavioural and health outcomes summarized above. In an attempt at reconciliation, what we have previously proposed is that these various outcomes in their different ways reflect motivational dysregulation, by which we mean impaired functioning of areas of the brain essential for motivation and behavioural regulation (Carroll et al., 2009; Lovallo, 2011). If this notion is anywhere close to correct, we would expect to observe associations between activities that perceptibly rely on intact motivation for optimal performance and blunted stress reactions. It was for this reason that we purposively examined the association between blunted stress reactivity and both cognitive ability and FEV1 in the West of Scotland and Dutch studies. From our perspective, then, blunted cardiovascular and cortisol stress reactions are markers of suboptimal functioning in key fronto-limbic brain systems when individuals are exposed to acute psychological stress. Tellingly, those fronto-limbic brain areas that are concerned with motivated behaviour are also implicated in autonomic regulation.
However, it is worth considering at what level this motivational deficit is operating. A fairly parsimonious explanation of the link between the outcomes discussed above and low stress reactivity is that it reflects attenuated conscious psychological engagement with the stress task by the depressed, obese or otherwise dysfunctional participants, which in turn results in reduced biological responding. Evidence in favour of this comes from studies examining reactivity and stress task difficulty (e.g., Richter et al., 2008). Essentially, within-subject cardiovascular reactivity rises with increasing task difficulty but eventually decreases when the task becomes so difficult that success is impossible; this is attributed to conscious disengagement. However, in our studies and those of others, we have adjusted for subjective stress, self-reported stress task engagement and/or objective task performance or have found no differences between high and low reactors in these variables. Indeed, in two analyses of data from the Dutch Famine Birth Cohort Study, we found a complete dissociation between ratings of stressfulness and cardiovascular and cortisol stress reactivity; participants high in neuroticism and low on openness and those with depression and/or anxiety in the Dutch Famine Birth Cohort Study showed blunted cardiovascular and cortisol reactions to the battery of stress tasks but rated themselves as significantly more stressed by the experience (Bibbey et al., 2013). It would appear, then, that blunted stress reactivity may reflect something more nuanced: perhaps an unconscious physiological disengagement in the face of acute stress exposures.
5. Blunted stress reactions and neural hypoactivation
Neuroimaging studies measuring both cardiovascular and neural stressor-evoked responses have largely been focused on understanding how the brain is a central mediator of exaggerated reactions to stress and how such associations confer risk for future cardiovascular disease (Gianaros and Wager, 2015). Recent reviews and meta-analyses (e.g., Gianaros and Wager, 2015; Muscatell and Eisenberger, 2012; Myers, 2016; Shoemaker and Goswami, 2015; Thayer et al., 2012) have highlighted that functional divisions of the anterior cingulate cortex (ACC), medial prefrontal cortex (mPFC), insula, hippocampus, and amygdala are core, although not exclusive, components of a network of forebrain systems involved in mediating stressor-evoked cardiovascular activity (e.g., Gianaros and Wager, 2015; Myers, 2016; Shoemaker and Goswami, 2015). Similarly, several studies have demonstrated that cardiovascular changes (e.g., heart rate and blood pressure) in response to stress are associated with activity changes in these areas of the brain, consistent with invasive animal work and patient lesion studies on central cardiovascular, autonomic, and neuroendocrine control (Critchley et al., 2000; Oppenheimer and Cechetto, 2016; Shoemaker and Goswami, 2015). Typically, higher cardiovascular activity during stress is associated with greater neural activity in these areas. For example, it has been demonstrated that higher blood pressure reactivity to stress was associated with more amygdala activation in response to the stress exposure (Gianaros et al., 2008). In a recent study, we shifted the focus to unambiguously blunted cardiovascular reactors as an explicit comparison of their neural reactions to a standard stress exposure with those who were unambiguously exaggerated cardiovascular reactors (Ginty et al., 2013). Blunted and exaggerated cardiac stress reactors were selected from previous studies, on the basis of being at least two standard deviations below and above the mean heart rate and cardiac output reactivity for their respective cohorts. Neural activity, using fMRI, and heart rate were recorded at baseline and during exposure to a standard laboratory stress task, as well as to a non-stressful control task. For blunted reactors, the heart rate change from baseline did not differ between the stress and control tasks, whereas for exaggerated reactors the heart rate change was substantially and significantly greater during the stress than the control condition. Blunted reactors also exhibited reduced activation in the anterior mid-cingulate cortex and insula, as well as a greater deactivation in the amygdala and posterior cingulate. These outcomes are not substantially dissimilar from the results of earlier less focused studies.
The same areas of the brain involved in autonomic regulation of stress also comprise a network vital for motivated behavioural responses and adaptation to acute stress exposure (Gianaros et al., 2012). Therefore, it is not surprising that a number of functional magnetic imaging (fMRI) studies afford evidence that many of the outcomes associated with blunted stress reactivity are also associated with relatively reduced activation in the frontal and sub-cortical limbic regions (e.g., (Stice et al., 2008)). For example, a relatively recent neuroimaging study reported that those with major depressive disorder had reduced heart rate and neural (amygdala, hippocampus, anterior cingulate cortex) responses to an acute psychological stress task (Holsen et al., 2011). Accordingly, the results of this study are in line with our contention that blunted stress reactivity may be a marker of the under-recruitment of pertinent brain systems during stress exposures that require motivated action. Similarly, individuals with a history of early life stress and/or trauma have diminished stressor-evoked neural responses (Yang et al., 2015). Although, more research simultaneously examining stressor evoked neural and cardiovascular responses along with behavioural outcomes discussed in this review is still required before firm conclusions can be drawn, but the early indications are not inconsistent with our thesis.
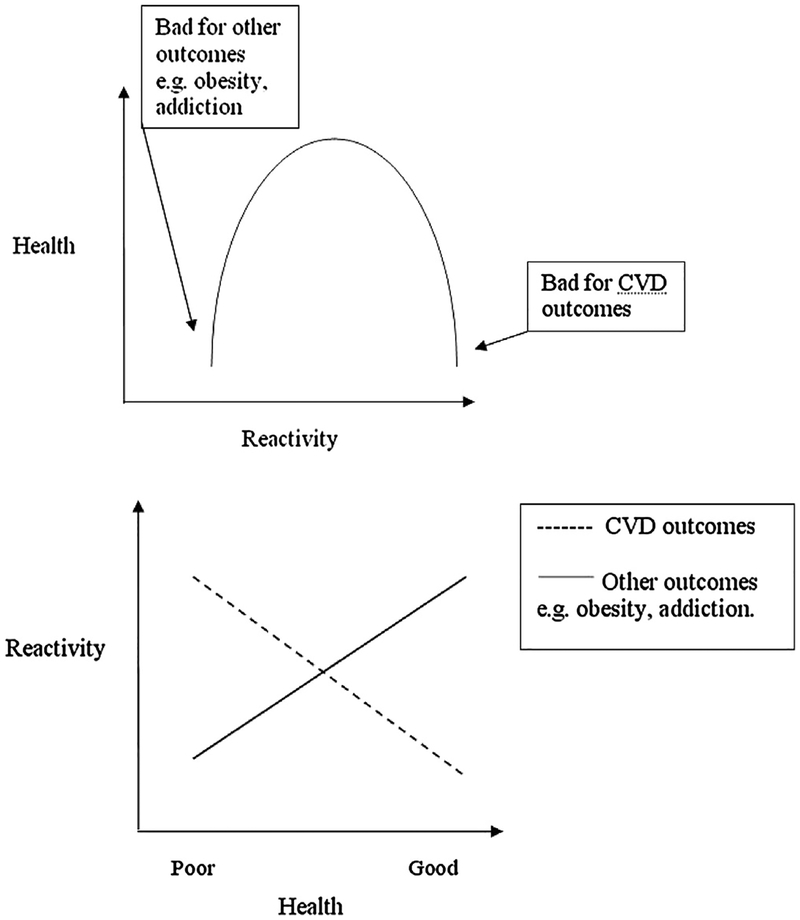
6. The reactivity hypothesis revisited: inverted-U or orthogonal processes
The reactivity hypothesis has shown remarkable resilience and durability. As indicated, its primary postulate is that exaggerated cardiovascular reactions to acute psychological stress will contribute to the subsequent development of hypertension and, by implication, other manifestations of end-point cardiovascular disease. Fairly few circumspect hypotheses in the biobehavioural sciences have generated such a volume of empirical and conceptual interest over the last 40 years. However, it is now becoming clear that the reactivity hypothesis warrants revision and extension. Although, it is now beyond contention that exaggerated cardiovascular reactions to stress predict future cardiovascular pathology, it is now equally apparent that blunted cardiovascular, and cortisol, reactions to stress are associated with a range of adverse health and behavioural outcomes, from depression and obesity to addiction and behavioural disorders to poorer cognitive ability. How might we re-conceptualise the reactivity hypothesis? The data conform to an inverted-U model where high and low reactivity can be considered maladaptive depending on the outcome in question. The inverted-U has a substantial pedigree in psychology. Originally characterised as the Yerkes-Dodson law (Yerkes and Dodson, 1908), the inverted-U proposed to describe the relationship between motivation and performance on one hand and physiological arousal on the other, such that there is an optimal mid-point in the arousal continuum where performance is best served. Accordingly, by conceiving of stress reactivity in terms of a unitary system that for some operates in a biased state, either over-responding or under-responding, we may simply be putting a few new clothes on a much loved but rather old doll. Nevertheless, as we indicate in the Introduction, the idea of bi-directional departures from appropriate homeostatic adjustments has a certain appeal at this stage.
On the other hand, a model which conceives of continuous positive associations between stress reactivity and some outcomes and continuous negative associations between reactivity and other outcomes can also fit the results. Indeed, increasingly this model has much to commend it. For the most part, the negative associations between stress reactivity and adverse health and behavioural outcomes involve blunted cardiac and cortisol reactions. There are exceptions, but very few consistent negative associations emerge for blood pressure reactivity, particularly for diastolic blood pressure reactivity. In contrast, the positive relationships between cardiovascular stress reactivity and cardiovascular pathology are largely confined to associations involving exaggerated blood pressure responding. We might speculate that the former involve impaired parasympathetic withdrawal and/or insufficient β-adrenergic drive (Brindle et al., 2014), whereas the latter are more vascular in origin, relying on enhanced α-adrenergic activation. We depict these two models in Fig. 5; time will tell which best serves revision of the reactivity hypothesis.
Fig. 5.
Alternative models, inverted-U and distinct mechanisms, linking stress reactivity to health and behavioural outcomes.
7. Biological disengagement: a wider phenomenon
Research on the antecedents and consequences of blunted cardiovascular and cortisol reactions to acute psychological stress is still in its infancy, but is gathering momentum. On the other hand, research into blunted biological responses to reward has a much longer pedigree. What is initially striking is that individuals differ markedly in their peripheral biological and central neural responses to reward, with some showing blunted responding. Further, what really catches the eye is that the behavioural and health correlates of deficient reward responses are remarkably similar to those associated with blunted stress responding: depression, obesity, bulimia, addiction including gambling addiction, attention deficit hyperactive disorder, and antisocial behaviour. Table 1 indicates the commonalities. Further, the neural mechanisms proposed to underlie blunted stress reactivity and what has come to be called Reward Deficiency Syndrome (RDS) (Blum et al., 2000) are noticeably similar; as with our notion of central motivational dysregulation, RDS would seem to be a manifestation of hypoactivation to reward stimuli in the same fronto-limbic network. In addition, RDS has been attributed to a dopaminergic deficiency, specifically at the D2 receptor. The dopaminergic system has also been attributed a key role in regulating autonomic activity, as well as in motivated behaviour and stimulus processing (Lovallo, 2011). A much fuller account of the parallels and their implications can be found elsewhere (Ginty, 2013); the present account is necessarily brief. However, the major implication is that blunted stress reactivity and RDS may be two sides of the same coin and both may reflect a more general failure of responding to both stress and reward, reflecting suboptimal functioning in motivational and emotional processing systems.
Table 1.
Disorders and behavioural manifestations associated with blunted physiological responses to both stress and reward.
| Manifestation | Reward | Stress |
|---|---|---|
| Depression | Brinkmann et al. (2009) | Brindle et al.(2013) |
| Pizzagalli et al. (2009) | Schwerdtfeger and Rosenkaimer(2011) | |
| Obesity | Stice et al. (2008) | Torres et al. (2014) |
| Batterink et al. (2010) | Carroll et al. (2008) | |
| Addiction | Brenner and Beauchaine (2011) | Lovallo et al. (2000) |
| al’Absi et al. (2003) | ||
| Bulimia | Bohen and Stice (2011) | Ginty et al. (2012a,b) |
| Koo-Loeb et al. (1998) | ||
| Gambling addiction | Reuter et al.(2005) | Paris et al. (2010) |
| Gourdiaan et al. (2006) | ||
| ADHD | Crowell et al. (2006) | Pesonen et al.(2011) |
| Iaboni et al.(1997) | Hirvikoski et al. (2011) | |
| Antisocial behaviour | Beauchaine et al. (2013) | Ortiz and Raine (2004) |
| Osterlaan et al. (2006) | De Vries-Bouw et al. (2011) | |
| Impulsivity | Hariri et al. (2006) | Bennett et al. (2014) |
| Allen et al. (2009) |
8. Concluding remarks and future directions
It is broadly accepted that exaggerated cardiovascular reactions to acute psychological stress are implicated in cardiovascular pathology. What has proved more contentious until lately is the notion that low or blunted cardiovascular and cortisol stress responding might also be associated with adverse behavioural and health outcomes. However, the strength and consistency of the empirical findings are now compelling, and blunted stress reactivity has been linked to depression, obesity, substance and non-substance addiction, bulimia, impulsivity and behavioural disorders, and poorer cognitive ability. Our thesis is that what links these diverse outcomes is that they all reflect, either directly or indirectly, suboptimal functioning in those fronto-limbic systems in the brain that are normally engaged during acute stress exposures, requiring motivation and adaptation. Those same systems are also involved in autonomic regulation, suggesting that blunted stress reactivity may be a marker of more central dysfunction. The available fMRI research tends to support this contention, but specifically-focussed studies are relatively scarce and more research that simultaneously examines peripheral autonomic and central neural reactions to acute stress is warranted. What we also require is a model fitting together the various pieces of what is becoming quite a complex jigsaw. The antecedents of central motivational dysregulation are likely to be found in genes and in childhood exposures. Although twin studies strongly implicate heredity, the precise polymorphisms involved have yet to be definitively determined. We would argue that genes involved in neurotransmission, particularly dopamine transmission, would be a good starting point. Although preliminary evidence is emerging, there needs to be much more focus on the association between blunted stress responding and early life adversity, particularly emotional neglect and abuse. Downstream from central neural dys-function are stable behavioural and emotional characteristics such as neuroticism, impulsivity, lack of perseverance, depression, and low cognitive ability. These in turn increase the likelihood of addiction and other unhealthy outcomes such as obesity and bulimia. Additionally, although beyond the scope of the present review, it should be noted many of these outcomes or behaviours are also associated with inflammation, such as low cognitive ability (Phillips et al., 2011a), obesity (Toni et al., 2004), and depression (Miller and Cole, 2012). This suggests that it would be fruitful to study the association between cardiovascular and cortisol stress reactivity and systemic inflammation, as well as acute inflammatory responses to psychological stress exposure.
This is the barest outline of a model based on current data, and is illustrated in Fig. 1; however, much more has to be done by way of confirmation and refinement. The parallels between blunted stress reactivity and the RDS also need further investigation; it is an essential next step to establish whether those who under-react to stress also under-react to reward both peripherally and centrally. Given the prognostic importance of cognitive decline for states of dementia, further attention needs to be paid to the association between blunted stress reactivity and age-related deterioration in cognitive ability. It is probably important to articulate a caveat; the studies we discuss in this review are largely observational studies. Thus, we cannot definitively establish the direction of causality, even when the evidence is derived from prospective studies. Although our model suggests particular pathways, others cannot be wholly discounted. For example, although we judge that the evidence favours our view that blunted cardiovascular and cortisol stress reactions, by reflecting central motivational dysregulation, is a risk marker for smoking, it remains possible that the association we and others observe also reflects a possible degradation of the autonomic nervous system by the toxins in cigarette smoke. Similarly, it remains possible that blunted reactivity may be a consequence of depression rather than a risk marker of it. Clarification in these instances can only come from cessation and treatment studies, respectively. Finally, almost all of the corollaries of blunted stress responding are targets for intervention; we would argue that stress testing and the detection of blunted reactivity could be informative in identifying participants likely to require more aggressive treatment.
References
- Akil M, Kolachana BS, Rothmond DA, Hyde TM, Weinberger DR, Kleinman JE, 2003. Catechol-O-methyltransferase genotype and dopamine regulation in the human brain. J. Neurosci 23, 2008–2013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- al’Absi M, 2006. Hypothalamic-pituitary-adrenocortical responses to psychological stress and risk for smoking relapse. Int. J. Psychophysiol 59, 218–227. [DOI] [PubMed] [Google Scholar]
- al’Absi M, Lovallo WR, 1993. Cortisol concentrations in serum of borderline hypertensive men exposed to a novel experimental setting. Psychoneuroendocrinology 18, 355–363. [DOI] [PubMed] [Google Scholar]
- al’Absi M, Wittmers LE, Erickson J, Hatsukami D, Crouse B, 2003. Attenuated adrenocortical and blood pressure responses to psychological stress in ad libitum and abstinent smokers. Pharmacol. Biochem. Behav 74, 401–410. [DOI] [PubMed] [Google Scholar]
- al’Absi M, Hatsukami D, Davis GL, 2005. Attenuated adrenocorticotropic responses to psychological stress are associated with early smoking relapse. Psychopharmacology (Berl.) 181, 107–117. [DOI] [PubMed] [Google Scholar]
- al’Absi M, Devereux RB, Rao DC, Kitzman D, Oberman A, Hopkins P, Arnett DK, 2006. Blood pressure stress reactivity and left ventricular mass in a random community sample of African-American and caucasian men and women. Am. J. Cardiol 97 (240–244), 10.1016/j.amjcard.2005.07.134, S0002–9149(05)01756-X [pii]. [DOI] [PubMed] [Google Scholar]
- Allen MT, Hogan AM, Laird LK, 2009. The relationships of impulsivity and cardiovascular responses: the role of gender and task type. Int. J. Psychophysiol 73, 369–376, 10.1016/j.ijpsycho.2009.05.014. [DOI] [PubMed] [Google Scholar]
- Amaral DG, 1992. Anatomical organization of the primate amygdaloid complex In: Aggleton JP (Ed.), The Amygdala: Neurobiological Aspects of Emotion, Memory, and Mental Dysfunction. Wiley, New York, pp. 1–66. [Google Scholar]
- Anderson SW, Bechara A, Damasio H, Tranel D, Damasio AR, 1999. Impairment of social and moral behavior related to early damage in human prefrontal cortex. Nat. Neurosci 2, 1032–1037, 10.1038/14833. [DOI] [PubMed] [Google Scholar]
- Axelrod J, 1957. O-methylation of epinephrine and other catechols in vitro and in vivo. Science 126, 400–401. [DOI] [PubMed] [Google Scholar]
- Barnett PA, Spence JD, Manuck SB, Jennings JR, 1997. Psychological stress and the progression of carotid artery disease. J. Hypertens 15, 49–55. [DOI] [PubMed] [Google Scholar]
- Batterink L, Yokum S, Stice E, 2010. Body mass correlates inversely with inhibitory control in response to food among adolescent girls: an from study. Neuroimage 52, 1703–1969. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beauchaine TP, Gatzke-Kopp L, Neuhaus E, Chipman J, Reid MJ, Webster-Stratton C, 2013. Sympathetic- and parasympathetic-linked cardiac function and prediction of externalizing behavior, emotion regulation, and prosocial behavior among preschoolers treated for ADHD. J. Consult. Clin. Psychol 81, 481–493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bennett C, Blissett J, Carroll D, Ginty AT, 2014. Rated and measured impulsivity in children is associated with diminished cardiac reactions to acute psychological stress. Biol. Psychol 102, 68–72, 10.1016/j.biopsycho.2014.07.009, S0301–0511(14)00156–2 [pii]. [DOI] [PubMed] [Google Scholar]
- Bibbey A, Carroll D, Roseboom TJ, Phillips AC, de Rooij SR, 2013. Personality and physiological reactions to acute psychological stress. Int. J. Psychophysiol 90, 28–36, 10.1016/j.ijpsycho.2012.10.018. [DOI] [PubMed] [Google Scholar]
- Bibbey A, Ginty AT, Brindle RC, Phillips AC, Carroll D, 2016. Blunted cardiac stress reactors exhibit relatively high levels of behavioural impulsivity. Physiol. Behav 159, 40–44, 10.1016/j.physbeh.2016.03.011. [DOI] [PubMed] [Google Scholar]
- Blum K, Braverman ER, Holder JM, Lubar JF, Monastra VJ, Miller D, Lubar JO, Chen TJ, Comings DE, 2000. Reward deficiency syndrome: a biogenetic model for the diagnosis and treatment of impulsive, addictive, and compulsive behaviors. J. Psychoact. Drugs 32 (Suppl. i–iv), 1–112. [DOI] [PubMed] [Google Scholar]
- Bohen C, Stice E, 2011. Reward abnormalities among women with full sub threshold bulimia nervosa: a functional magnetic resonance imaging study. Int. J. Eat. Disord 44, 585–595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bouma EM, Riese H, Doornbos B, Ormel J, Oldehinkel AJ, 2012. Genetically based reduced MAOA and COMT functioning is associated with the cortisol stress response: a replication study. Mol. Psychiatry 17, 119–121, 10.1038/mp.2011.115. [DOI] [PubMed] [Google Scholar]
- Brenhouse HC, Lukkes JL, Andersen SL, 2013. Early life adversity alters the developmental profiles of addiction-related prefrontal cortex circuitry. Brain Sci 3, 143–158, 10.3390/brainsci3010143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brenner SL, Beauchaine TP, 2011. Pre-ejection period reactivity and psychiatric comorbidity prospectively predict substance use initiation among middle-schoolers: a pilot study. Psychophysiology 48, 1588–1596, 10.1111/j.1469-8986.2011.01230. [DOI] [PubMed] [Google Scholar]
- Brindle RC, Ginty AT, Conklin SM, 2013. Is the association between depression and blunted cardiovascular stress reactions mediated by perceptions of stress? Int. J. Psychophysiol 90, 66–72, 10.1016/j.ijpsycho.2013.06.003. [DOI] [PubMed] [Google Scholar]
- Brindle RC, Ginty AT, Phillips AC, Carroll D, 2014. A tale of two mechanisms: a meta-analytic approach toward understanding the autonomic basis of cardiovascular reactivity to acute psychological stress. Psychophysiology 51, 964–976, 10.1111/psyp.12248. [DOI] [PubMed] [Google Scholar]
- Brinkmann K, Schubach L, Joye IA, Gendolla GH, 2009. Anehdonia and effort mobilization in dysphoria: reduced cardiovascular response to reward and punishment. Int. J. Psychophysiol 74, 250–258. [DOI] [PubMed] [Google Scholar]
- Burch AE, Allen MT, 2014. Stress task specific impairments of cardiovascular functioning in obese participants. Int. J. Psychophysiol 94, 1–8, 10.1016/j.ijpsycho.2014.07.002. [DOI] [PubMed] [Google Scholar]
- Campeau S, Davis M, 1995. Involvement of the central nucleus and basolateral complex of the amygdala in fear conditioning measured with fear-potentiated startle in rats trained concurrently with auditory and visual conditioned stimuli. J. Neurosci 15, 2301–2311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carroll D, Ring C, Hunt K, Ford G, Macintyre S, 2003. Blood pressure reactions to stress and the prediction of future blood pressure: effects of sex, age, and socioeconomic position. Psychosom. Med 65, 1058–1064, 10.1097/01.PSY.0000097330.58739.26. [DOI] [PubMed] [Google Scholar]
- Carroll D, Phillips AC, Hunt K, Der G, 2007. Symptoms of depression and cardiovascular reactions to acute psychological stress: evidence from a population study. Biol. Psychol 75, 68–74. [DOI] [PubMed] [Google Scholar]
- Carroll D, Phillips AC, Lovallo WR, 2009. Are large physiological reactions to acute psychological stress always bad for health? Soc. Pers. Compass (Health Sect.) 3, 725–743. [Google Scholar]
- Carroll D, Phillips AC, Der G, Hunt K, Benzeval M, 2011. Blood pressure reactions to acute mental stress and future blood pressure status: data from the 12-year follow-up of the West of Scotland Study. Psychosom. Med 73, 737–742, 10.1097/PSY.0b013e3182359808 (PSY.0b013e3182359808 [pii]). [DOI] [PubMed] [Google Scholar]
- Carroll D, Ginty AT, Der G, Hunt K, Benzeval M, Phillips AC, 2012a. Increased blood pressure reactions to acute mental stress are associated with 16-year cardiovascular disease mortality. Psychophysiology 49, 1444–1448, 10.1111/j.1469-8986.2012.01463.x. [DOI] [PubMed] [Google Scholar]
- Carroll D, Ginty AT, Painter RC, Roseboom TJ, Phillips AC, de Rooij SR, 2012b. Systolic blood pressure reactions to acute stress are associated with future hypertension status in the Dutch Famine Birth Cohort Study. Int. J. Psychophysiol 85, 270–273, 10.1016/j.ijpsycho.2012.04.001. [DOI] [PubMed] [Google Scholar]
- Carroll D, Phillips AC, Der G, Hunt K, Bibbey A, Benzeval M, Ginty AT, 2012c. Low forced expiratory volume is associated with blunted cardiac reactions to acute psychological stress in a community sample of middle-aged men and women. Int. J. Psychophysiol, 10.1016/j.ijpsycho.2012.10.005, S0167–8760(12)00619–8 [pii]. [DOI] [PubMed] [Google Scholar]
- Carroll D, Phillips AC, Der G, Hunt K, Bibbey A, Benzeval M, Ginty AT, 2013. Low forced expiratory volume is associated with blunted cardiac reactions to acute psychological stress in a community sample of middle-aged men and women. Int. J. Psychophysiol 90, 17–20, 10.1016/j.ijpsycho.2012.10.005. [DOI] [PubMed] [Google Scholar]
- Crim C, Celli B, Edwards LD, Wouters E, Coxson HO, Tal-Singer R, Calverley PM, 2011. Respiratory system impedance with impulse oscillometry in healthy and COPD subjects: ECLIPSE baseline results. Respir. Med 105, 1069–1078, 10.1016/j.rmed.2011.01.010, S0954–6111(11)00025–4 [pii]. [DOI] [PubMed] [Google Scholar]
- Critchley HD, Corfield DR, Chandler MP, Mathias CJ, Dolan RJ, 2000. Cerebral correlates of autonomic cardiovascular arousal: a functional neuroimaging investigation in humans. J. Physiol 523 (Pt 1), 259–270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crowell SE, Beauchaine TP, Gatzke-Kopp L, Sylvers P, Mead H, Chipman-Chacon J, 2006. Autonomic correlates of attention-deficit/hyperactivity disorder and oppositional defiant disorder in preschool children. J. Abnorm. Psychol 115, 174–178. [DOI] [PubMed] [Google Scholar]
- de Rooij SR, Schene AH, Phillips DI, Roseboom TJ, 2010. Depression and anxiety: associations with biological and perceived stress reactivity to a psychological stress protocol in a middle-aged population. Psychoneuroendocrinology 35, 866–877, 10.1016/j.psyneuen.2009.11.011, S0306–4530(09)00354–0 [pii]. [DOI] [PubMed] [Google Scholar]
- Damasio H, Grabowski T, Frank R, Galaburda AM, Damasio AR, 1994. The return of Phineas Gage: clues about the brain from the skull of a famous patient. Science 264, 1102–1105. [DOI] [PubMed] [Google Scholar]
- Davis M, 1997. Neurobiology of fear responses: the role of the amygdala. J. Neuropsychiatry Clin. Neurosci 9, 382–402, 10.1176/jnp.9.3.382. [DOI] [PubMed] [Google Scholar]
- Davis M, 2000. The role of the amygdala in unconditioned fear and anxiety In: Aggleton JP (Ed.), The Amygdala: A Functional analysis. Oxford University Press, Oxford, pp. 213–287. [Google Scholar]
- De Rooij SR, Roseboom TJ, 2010. Further evidence for an association between self-reported health and cardiovascular as well as cortisol reactions to acute psychological stress. Psychophysiology 47, 1172–1175, 10.1111/j.1469-8986.2010.01023.x, PSYP1023 [pii]. [DOI] [PubMed] [Google Scholar]
- De Vries-Bouw M, Popma A, Vermeiren R, Doreleijers TA, Van De Ven PM, Jansen LM, 2011. The predictive value of low heart rate and heart rate variability during stress for reoffending in delinquent male adolescents. Psychophysiology 48, 1597–1604, 10.1111/j.1469-8986.2011.01233.x. [DOI] [PubMed] [Google Scholar]
- Drabant EM, Hariri AR, Meyer-Lindenberg A, Munoz KE, Mattay VS, Kolachana BS, Egan MF, Weinberger DR, 2006. Catechol O-methyltransferase val158met genotype and neural mechanisms related to affective arousal and regulation. Arch. Gen. Psychiatry 63, 1396–1406, 10.1001/archpsyc.63.12.1396. [DOI] [PubMed] [Google Scholar]
- Drevets WC, Price JL, Simpson JR Jr., Todd RD, Reich T, Vannier M, Raichle ME, 1997. Subgenual prefrontal cortex abnormalities in mood disorders. Nature 386, 824–827, 10.1038/386824a0. [DOI] [PubMed] [Google Scholar]
- Egan MF, Goldberg TE, Kolachana BS, Callicott JH, Mazzanti CM, Straub RE, Goldman D, Weinberger DR, 2001. Effect of COMT Val108/158 Met genotype on frontal lobe function and risk for schizophrenia. Proc. Natl. Acad. Sci. U. S. A 98, 6917–6922, 10.1073/pnas.111134598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fairchild G, van Goozen SH, Stollery SJ, Brown J, Gardiner J, Herbert J, Goodyer IM, 2008. Cortisol diurnal rhythm and stress reactivity in male adolescents with early-onset or adolescence-onset conduct disorder. Biol Psychiatry 64, 599–606, 10.1016/j.biopsych.2008.05.022, S0006–3223(08)00685–9 [pii]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ford G, Ecob R, Hunt K, Macintyre S, West P, 1994. Patterns of class inequality in health through the lifespan: class gradients at 15, 35 and 55 years in the west of Scotland. Soc. Sci. Med 39, 1037–1050. [DOI] [PubMed] [Google Scholar]
- Franzen J, Brinkmann K, 2015. Blunted cardiovascular reactivity in dysphoria during reward and punishment anticipation. Int. J. Psychophysiol 95, 270–277, 10.1016/j.ijpsycho.2014.11.007. [DOI] [PubMed] [Google Scholar]
- Gao Y, Borlam D, Zhang W, 2015. The association between heart rate reactivity and fluid intelligence in children. Biol. Psychol 107, 69–75, 10.1016/j.biopsycho.2015.03.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gianaros PJ, Wager TD, 2015. Brain-body pathways linking psychological stress and physical health. Curr. Dir. Psychol. Sci 24, 313–321, 10.1177/0963721415581476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gianaros PJ, Sheu LK, Matthews KA, Jennings JR, Manuck SB, Hariri AR, 2008. Individual differences in stressor-evoked blood pressure reactivity vary with activation, volume, and functional connectivity of the amygdala. J. Neurosci 28, 990–999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gianaros PJ, Onyewuenyi IC, Sheu LK, Christie IC, Critchley HD, 2012. Brain systems for baroreflex suppression during stress in humans. Hum. Brain Mapp 33, 1700–1716, 10.1002/hbm.21315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gianaros PJ, Marsland AL, Sheu LK, Erickson KI, Verstynen TD, 2013Inflammatory pathways link socioeconomic inequalities to white matter architecture. Cereb. Cortex 23, 2058–2071, 10.1093/cercor/bhs191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gianaros PJ, Marsland AL, Kuan DC, Schirda BL, Jennings JR, Sheu LK, Hariri AR, Gross JJ, Manuck SB, 2014. An inflammatory pathway links atherosclerotic cardiovascular disease risk to neural activity evoked by the cognitive regulation of emotion. Biol. Psychiatry 75, 738–745, 10.1016/j.biopsych.2013.10.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ginty AT, Phillips AC, Der G, Deary IJ, Carroll D, 2011. Cognitive ability and simple reaction time predict cardiac reactivity in the West of Scotland Twenty-07 Study. Psychophysiology 48, 1022–1027, 10.1111/j.1469-8986.2010.01164.x. [DOI] [PubMed] [Google Scholar]
- Ginty AT, Phillips AC, Higgs S, Heaney JL, Carroll D, 2012a. Disordered eating behaviour is associated with blunted cortisol and cardiovascular reactions to acute psychological stress. Psychoneuroendocrinology 37, 715–724, 10.1016/j.psyneuen.2011.09.004, S0306–4530(11)00274–5 [pii]. [DOI] [PubMed] [Google Scholar]
- Ginty AT, Phillips AC, Roseboom TJ, Carroll D, Derooij SR, 2012b. Cardiovascular and cortisol reactions to acute psychological stress and cognitive ability in the Dutch Famine Birth Cohort Study. Psychophysiology 49, 391–400, 10.1111/j.1469-8986.2011.01316.x. [DOI] [PubMed] [Google Scholar]
- Ginty AT, Gianaros PJ, Derbyshire SWG, Phillips AC, Carroll D, 2013. Blunted cardiac stress reactivity relates to neural hypoactivation. Psychophysiology 50, 219–229. [DOI] [PubMed] [Google Scholar]
- Ginty AT, Jones A, Carroll D, Roseboom TJ, Phillips AC, Painter R, de Rooij SR, 2014. Neuroendocrine and cardiovascular reactions to acute psychological stress are attenuated in smokers. Psychoneuroendocrinology 48, 87–97, 10.1016/j.psyneuen.2014.05.023, S0306–4530(14)00209–1 [pii]. [DOI] [PubMed] [Google Scholar]
- Ginty AT, Brindle RC, Carroll D, 2015. Cardiac stress reactions and perseverance: diminished reactivity is associated with study non-completion. Biol. Psychol 109, 200–205, 10.1016/j.biopsycho.2015.06.001. [DOI] [PubMed] [Google Scholar]
- Ginty AT, 2013. Blunted responses to stress and reward: reflections on biological disengagement? Int. J. Psychophysiol 90, 90–94, 10.1016/j.ijpsycho.2013.06.008. [DOI] [PubMed] [Google Scholar]
- Girdler SS, Jamner LD, Jarvik M, Soles JR, Shapiro D, 1997. Smoking status and nicotine administration differentially modify hemodynamic stress reactivity in men and women. Psychosom. Med 59, 294–306. [DOI] [PubMed] [Google Scholar]
- Goldman D, Oroszi G, Ducci F, 2005. The genetics of addictions: uncovering the genes. Nat. Rev. Genet 6, 521–532. [DOI] [PubMed] [Google Scholar]
- Goldman-Rakic PS, 1996. The prefrontal landscape: implications of functional architecture for understanding human mentation and the central executive. Philos. Trans. R. Soc. Lond. B Biol. Sci 351, 1445–1453, 10.1098/rstb.1996.0129. [DOI] [PubMed] [Google Scholar]
- Gourdiaan AE, Oosterlaan J, de Beurs E, van den Brink W, 2006. Psychophysiological determinants and concomitants of deficient decision making in pathological gamblers. Drug Alcohol Depend. 84, 231–239. [DOI] [PubMed] [Google Scholar]
- Halgren E, 1992. Emotional neurophysiology of the amygdala within the context of human cognition In: Aggleton JP (Ed.), The Amygdala: Neurobiological Aspects of Emotion, Memory, and Mental Dysfunction. Wiley, New York, pp. 191–228. [Google Scholar]
- Hariri AR, Brown SM, Williamson DE, Flory JD, de Wit H, Manuck SB, 2006. Preference for immediate over delayed rewards is associated with magnitude of ventral stratal activity. J. Neurosci 26, 13213–13217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heaney JLJ, Ginty AT, Carroll D, Phillips AC, 2011. Preliminary evidence that exercise dependence is associated with blunted cardiac and cortisol reactions to acute psychological stress. Int. J. Psychophysiol 79, 323–329, 10.1016/j.ijpsycho.2010.11.010, S0167–8760(10)00756–7 [pii]. [DOI] [PubMed] [Google Scholar]
- Het S, Vocks S, Wolf JM, Hammelstein P, Herpertz S, Wolf OT, 2015. Blunted neuroendocrine stress reactivity in young women with eating disorders. J. Psychosom. Res 78, 260–267, 10.1016/j.jpsychores.2014.11.001. [DOI] [PubMed] [Google Scholar]
- Hirvikoski T, Olsson EM, Nordenstrom A, Lindholm T, Nordstrom AL, Lajic S, 2011. Deficient cardiovascular stress reactivity predicts poor executive functions in adults with attention-deficit/hyperactivity disorder. J. Clin. Experimen. Neuropsychol 33, 63–73. [DOI] [PubMed] [Google Scholar]
- Holsen LM, Spaeth SB, Lee JH, Ogden LA, Klibanski A, Whitfield-Gabrieli S, Goldstein JM, 2011. Stress response circuitry hypoactivation related to hormonal dysfunction in women with major depression. J. Affect. Disord 131, 379–387, 10.1016/j.jad.2010.11.024, S0165–0327(10)00721–4 [pii]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Iaboni F, Douglas VI, Ditto B, 1997. Psychophysiological responses of ADHD chidlren to reward and extinction. Psychophysiology 34, 116–123. [DOI] [PubMed] [Google Scholar]
- Idler EL, Benyamini Y, 1997. Self-rated health and mortality: a review of twenty-seven community studies. J. Health Soc. Behav 38, 21–37. [PubMed] [Google Scholar]
- Jackson ME, Moghaddam B, 2001. Amygdala regulation of nucleus accumbens dopamine output is governed by the prefrontal cortex. J. Neurosci 21, 676–681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones A, McMillan MR, Jones RW, Kowalik GT, Steeden JA, Deanfield JE, Pruessner JC, Taylor AM, Muthurangu V, 2012. Adiposity is associated with blunted cardiovascular, neuroendocrine and cognitive responses to acute mental stress. PLoS One 7, e39143, 10.1371/journal.pone.0039143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kapuku GK, Treiber FA, Davis HC, Harshfield GA, Cook BB, Mensah GA, 1999. Hemodynamic function at rest, during acute stress, and in the field: predictors of cardiac structure and function 2 years later in youth. Hypertension 34, 1026–1031. [DOI] [PubMed] [Google Scholar]
- Kibler JL, Ma M, 2004. Depressive symptoms and cardiovascular reactivity to laboratory behavioral stress. Int. J. Behav. Med 11, 81–87. [DOI] [PubMed] [Google Scholar]
- Koo-Loeb JH, Pedersen C, Girdler SS, 1998. Blunted cardiovascular and catecholamine stress reactivity in women with bulimia nervosa. Psychiatry Res 80, 13–27, S0165–1781(98)00057–2 [pii]. [DOI] [PubMed] [Google Scholar]
- Koss KJ, Mliner SB, Donzella B, Gunnar MR, 2016. Early adversity, hypocortisolism, and behavior problems at school entry: a study of internationally adopted children. Psychoneuroendocrinology 66, 31–38, 10.1016/j.psyneuen.2015.12.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lovallo WR, Gerin W, 2003. Psychophysiological reactivity: mechanisms and pathways to cardiovascular disease. Psychosom. Med 65, 36–45. [DOI] [PubMed] [Google Scholar]
- Lovallo WR, Dickensheets SL, Myers DA, Thomas TL, Nixon SJ, 2000. Blunted stress cortisol response in abstinent alcoholic and polysubstance-abusing men. Alcohol. Clin. Exp. Res 24, 651–658. [PubMed] [Google Scholar]
- Lovallo WR, Enoch MA, Acheson A, Cohoon AJ, Sorocco KH, Hodgkinson CA, Vincent AS, Goldman D, 2016. Early-life adversity interacts with FKBP5 genotypes: altered working memory and cardiac stress reactivity in the Oklahoma Family Health Patterns Project. Neuropsychopharmacology 41, 1724–1732, 10.1038/npp.2015.347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lovallo WR, 2006. Cortisol secretion patterns in addiction and addiction risk. Int. J. Psychophysiol 59, 195–202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lovallo WR, 2011. Do low levels of stress reactivity signal poor states of health? Biol. Psychol 86, 121–128, 10.1016/j.biopsycho.2010.01.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lovallo WR, 2013. Early life adversity reduces stress reactivity and enhances impulsive behavior: implications for health behaviors. Int. J. Psychophysiol 90, 8–16, 10.1016/j.ijpsycho.2012.10.006, S0167–8760(12)00622–8 [pii]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lovallo WR, 2016. Stress and Health: Biological and Psychological Interactions, 3rd edn Sage Publications, Los Angeles, CA. [Google Scholar]
- Malhotra AK, Kestler LJ, Mazzanti C, Bates JA, Goldberg T, Goldman D, 2002. A functional polymorphism in the COMT gene and performance on a test of prefrontal cognition. Am. J. Psychiatry 159, 652–654, 10.1176/appi.ajp.159.4.652. [DOI] [PubMed] [Google Scholar]
- Matsumoto M, Weickert CS, Akil M, Lipska BK, Hyde TM, Herman MM, Kleinman JE, Weinberger DR, 2003. Catechol O-methyltransferase mRNA expression in human and rat brain: evidence for a role in cortical neuronal function. Neuroscience 116, 127–137. [DOI] [PubMed] [Google Scholar]
- Matthews SG, Phillips DI, 2010. Minireview: transgenerational inheritance of the stress response: a new frontier in stress research. Endocrinology 151, 7–13, 10.1210/en.2009-0916. [DOI] [PubMed] [Google Scholar]
- McEwen BS, Gianaros PJ, 2011. Stress- and allostasis-induced brain plasticity. Annu. Rev. Med 62, 431–445, 10.1146/annurev-med-052209-100430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McEwen BS, Stellar E, 1993. Stress and the individual: mechanisms leading to disease. Arch. Int. Med 153, 2093–2101. [PubMed] [Google Scholar]
- McEwen BS, 2007. Physiology and neurobiology of stress and adaptation: central role of the brain. Physiol. Rev 87, 873–904, 10.1152/physrev.00041.2006. [DOI] [PubMed] [Google Scholar]
- Miller GE, Cole SW, 2012. Clustering of depression and inflammation in adolescents previously exposed to childhood adversity. Biol. Psychiatry 72, 34–40, 10.1016/j.biopsych.2012.02.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muscatell KA, Eisenberger NI, 2012. A social neuroscience perspective on stress and health. Soc. Pers. Psychol. Compass 6, 890–904, 10.1111/j.1751-9004.2012.00467.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Myers B, 2016. Cortico-limbic regulation and cardiovascular responses to stress. Physiol. Behav, in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Obrist PA, 1976. The cardiovascular-behavioral interaction—as it appears today. Psychophysiology 13, 95–107. [DOI] [PubMed] [Google Scholar]
- Oppenheimer S, Cechetto D, 2016. The insular cortex and the regulation of cardiac function. Compr. Physiol 6, 1081–1133, 10.1002/cphy.c140076. [DOI] [PubMed] [Google Scholar]
- Ortiz J, Raine A, 2004. Heart rate level and antisocial behavior in children and adolescents: a meta-analysis. J. Am. Acad. Child Adolesc. Psychiatry 43, 154–162. [DOI] [PubMed] [Google Scholar]
- Panknin TL, Dickensheets SL, Nixon SJ, Lovallo WR, 2002. Attenuated heart rate responses to public speaking in individuals with alcohol dependence. Alcohol. Clin. Exp. Res 26, 841–847. [PubMed] [Google Scholar]
- Paris JJ, Franco C, Sodano R, Frye CA, Wulfert E, 2010. Gambling pathology is associated with dampened cortisol response among men and women. Physiol. Behav 99, 230–233, 10.1016/j.physbeh.2009.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pesonen AK, Kajantie E, Jones A, Pyhala R, Lahti J, Heinonen K, Eriksson JG, Strandberg TE, Raikkonen K, 2011. Symptoms of attention deficit hyperactivity disorder in children are associated with cortisol responses to psychosocial stress but not with daily cortisol levels. J. Psychiatr. Res 45, 1471–1476, 10.1016/j.jpsychires.2011.07.002. [DOI] [PubMed] [Google Scholar]
- Phillips ML, Drevets WC, Rauch SL, Lane R, 2003. Neurobiology of emotion perception I: the neural basis of normal emotion perception. Biol. Psychiatry 54, 504–514. [DOI] [PubMed] [Google Scholar]
- Phillips AC, Der G, Carroll D, 2009a. Self-reported health and cardiovascular reactions to psychological stress in a large community sample: cross-sectional and prospective associations. Psychophysiology 46, 1020–1027, 10.1111/j.1469-8986.2009.00843.x, PSYP843 [pii]. [DOI] [PubMed] [Google Scholar]
- Phillips AC, Der G, Hunt K, Carroll D, 2009b. Haemodynamic reactions to acute psychological stress and smoking status in a large community sample. Int. J. Psychophysiol 73, 273–278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Phillips AC, Batty GD, van Zanten JJ, Mortensen LH, Deary IJ, Calvin CM, Carroll D, 2011a. Cognitive ability in early adulthood is associated with systemic inflammation in middle age: the Vietnam experience study. Brain Behav. Immun 25, 298–301, 10.1016/j.bbi.2010.09.022, S0889–1591(10)00503–9 [pii]. [DOI] [PubMed] [Google Scholar]
- Phillips AC, Hunt K, Der G, Carroll D, 2011b. Blunted cardiac reactions to acute psychological stress predict symptoms of depression five years later: evidence from a large community study. Psychophysiology 48, 142–148, 10.1111/j.1469-8986.2010.01045.x, PSYP1045 [pii]. [DOI] [PubMed] [Google Scholar]
- Phillips AC, Roseboom TJ, Carroll D, de Rooij SR, 2012. Cardiovascular and cortisol reactions to acute psychological stress and adiposity: cross-sectional and prospective associations in the Dutch Famine Birth Cohort Study. Psychosom. Med 74, 699–710, 10.1097/PSY.0b013e31825e3b91, PSY.0b013e31825e3b91 [pii]. [DOI] [PubMed] [Google Scholar]
- Phillips AC, 2011. Blunted cardiovascular reactivity relates to depression, obesity, and self-reported health. Biol. Psychol 86, 106–113, 10.1016/j.biopsycho.2010.03.016. [DOI] [PubMed] [Google Scholar]
- Pizzagalli DA, Holmes AJ, Dillon DG, Goetz EL, Birk JL, Bogdan R, Dougherty DD, Iosifescu DV, Rauch SL, Fava M, 2009. Reduced caudate and nucleus accumbens resposne to rewards in unmedicated individuals with major depressive disorder. Am. J. Psychiatry 166, 702–710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ravelli AC, van der Meulen JH, Michels RP, Osmond C, Barker DJ, Hales CN, Bleker OP, 1998. Glucose tolerance in adults after prenatal exposure to famine. Lancet 351, 173–177, S0140673697072449 [pii]. [DOI] [PubMed] [Google Scholar]
- Reuter J, Raedler T, Rose M, Hand I, Galscher J, Buchel C, 2005. Pathological gambling is linked to reduced activation of the mesolimbic reward system. Nat. Neurosci 8, 147–148. [DOI] [PubMed] [Google Scholar]
- Richter M, Friedrich A, Gendolla GH, 2008. Task difficulty effects on cardiac activity. Psychophysiology 45, 869–875, 10.1111/j.1469-8986.2008.00688.x, PSYP688 [pii]. [DOI] [PubMed] [Google Scholar]
- Rolls ET, 1972. Activation of amygdaloid neurones in reward, eating and drinking elicited by electrical stimulation of the brain. Brain Res 45, 365–381. [DOI] [PubMed] [Google Scholar]
- Rolls ET, 1992. Neurophysiology and functions of the primate amygdala In: Aggleton JP (Ed.), The Amygdala: Neurobiological Aspects of Emotion, Memory, and Mental Dysfunction. Wiley, New York, pp. 143–165. [Google Scholar]
- Rottenberg J, Chambers AS, Allen JJ, Manber R, 2007. Cardiac vagal control in the severity and course of depression: the importance of symptomatic heterogeneity. J. Affect. Disord 103, 173–179, 10.1016/j.jad.2007.01.028, S0165–0327(07)00048–1 [pii]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roy MP, Steptoe A, Kirschbaum C, 1994. Association between smoking status and cardiovascular and cortisol stress responsivity in healthy young men. Int. J. Behav. Med 1, 264–283. [DOI] [PubMed] [Google Scholar]
- Salomon EA, Mimiaga MJ, Husnik MJ, Welles SL, Manseau MW, Montenegro AB, Safren SA, Koblin BA, Chesney MA, Mayer KH, 2009. Depressive symptoms, utilization of mental health care, substance use and sexual risk among young men who have sex with men in EXPLORE: implications for age-specific interventions. AIDS Behav 13, 811–821, 10.1007/s10461-008-9439-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salomon K, Bylsma LM, White KE, Panaite V, Rottenberg J, 2013. Is blunted cardiovascular reactivity in depression mood-state dependent? A comparison of major depressive disorder remitted depression and healthy controls. Int. J. Psychophysiol 90, 50–57, 10.1016/j.ijpsycho.2013.05.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schulz S, Arning L, Pinnow M, Wascher E, Epplen JT, Beste C, 2012. When control fails: influence of the prefrontal but not striatal dopaminergic system on behavioural flexibility in a change detection task. Neuropharmacology 62, 1028–1033, 10.1016/j.neuropharm.2011.10.012. [DOI] [PubMed] [Google Scholar]
- Schwerdtfeger A, Rosenkaimer AK, 2011. Depressive symptoms and attenuated physiological reactivity to laboratory stressors. Biol. Psychol 87, 430–438, 10.1016/j.biopsycho.2011.05.009, S0301–0511(11)00144-X [pii]. [DOI] [PubMed] [Google Scholar]
- Seamans JK, Yang CR, 2004. The principal features and mechanisms of dopamine modulation in the prefrontal cortex. Prog. Neurobiol 74, 1–58, 10.1016/j.pneurobio.2004.05.006. [DOI] [PubMed] [Google Scholar]
- Shoemaker JK, Goswami R, 2015. Forebrain neurocircuitry associated with human reflex cardiovascular control. Front. Physiol 6, 240, 10.3389/fphys.2015.00240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Silvers JA, Lumian DS, Gabard-Durnam L, Gee DG, Goff B, Fareri DS, Caldera C, Flannery J, Telzer EH, Humphreys KL, Tottenham N, 2016. Previous institutionalization is followed by broader amygdala-hippocampal-PFC network connectivity during aversive learning in human development. J. Neurosci 36, 6420–6430, 10.1523/JNEUROSCI.0038-16.2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smolka MN, Schumann G, Wrase J, Grusser SM, Flor H, Mann K, Braus DF, Goldman D, Buchel C, Heinz A, 2005. Catechol-O-methyltransferase val158met genotype affects processing of emotional stimuli in the amygdala and prefrontal cortex. J. Neurosci 25, 836–842, 10.1523/JNEUROSCI.1792-04.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Souza GG, Mendonca-de-Souza AC, Duarte AF, Fischer NL, Souza WF, Coutinho ES, Figueira I, Volchan E, 2015. Blunted cardiac reactivity to psychological stress associated with higher trait anxiety: a study in peacekeepers. BMC Neurosci 16, 81, 10.1186/s12868-015-0216-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stevenson CW, Gratton A, 2003. Basolateral amygdala modulation of the nucleus accumbens dopamine response to stress: role of the medial prefrontal cortex. Eur. J. Neurosci 17, 1287–1295. [DOI] [PubMed] [Google Scholar]
- Stice E, Spoor S, Bohon C, Veldhuizen MG, Small DM, 2008. Relation of reward from food intake and anticipated food intake to obesity: a functional magnetic resonance imaging study. J. Abnorm. Psychol 117, 924–935. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Swanson LW, 2000. Cerebral hemisphere regulation of motivated behavior. Brain Res 886, 113–164. [DOI] [PubMed] [Google Scholar]
- Thayer JF, Ahs F, Fredrikson M, Sollers JJ 3rd, Wager TD, 2012. A meta-analysis of heart rate variability and neuroimaging studies: implications for heart rate variability as a marker of stress and health. Neurosci. Biobehav. Rev 36, 747–756, 10.1016/j.neubiorev.2011.11.009. [DOI] [PubMed] [Google Scholar]
- Toni R, Malaguti A, Castorina S, Roti E, Lechan RM, 2004. New paradigms in neuroendocrinology: relationships between obesity, systemic inflammation and the neuroendocrine system. J. Endocrinol. Invest 27, 182–186, 10.1007/BF03346266. [DOI] [PubMed] [Google Scholar]
- Torres SJ, Turner AI, Jayashinghe SU, Reynolds J, Nowson CA, 2014. The effect overweight/obesity on cardiovascular responses to acute psychological stress in men aged 50–70 years. Obesity Facts 7, 339–350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tottenham N, 2012. Risk and developmental heterogeneity in previously institutionalized children. J. Adolesc. Health 51, 529–533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Treiber FA, Kamarck T, Schneiderman N, Sheffield D, Kapuku G, Taylor T, 2003. Cardiovascular reactivity and development of preclinical and clinical disease states. Psychosom. Med 65, 46–62. [DOI] [PubMed] [Google Scholar]
- Tunbridge EM, Huber A, Farrell SM, Stumpenhorst K, Harrison PJ, Walton ME, 2012. The role of catechol-O-methyltransferase in reward processing and addiction. CNS Neurol. Disord. Drug Targets 11, 306–323. [DOI] [PubMed] [Google Scholar]
- Wu T, Snieder H, de Geus E, 2010. Genetic influences on cardiovascular stress reactivity. Neurosci. Biobehav. Rev 35, 58–68, 10.1016/j.neubiorev.2009.12.001. [DOI] [PubMed] [Google Scholar]
- Yang H, Spence JS, Briggs RW, Rao U, North C, Devous MD Sr., Xiao H, Adinoff B, 2015. Interaction between early life stress and alcohol dependence on neural stress reactivity. Addict. Biol 20, 523–533, 10.1111/adb.12135. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yano Y, Ning H, Reis JP, Lewis CE, Launer LJ, Bryan RN, Yaffe K, Sidney S, Albanese E, Greenland P, Lloyd-Jones D, Liu K, 2016. Blood pressure reactivity to psychological stress in young adults and cognition in midlife: The Coronary Artery Risk Development in Young Adults (CARDIA) Study. J. Am. Heart Assoc 5, 10.1161/jaha.115.002718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yerkes RM, Dodson JD, 1908. The relation of strength of stimulus to rapidity of habit-hyphen formation. J. Comp. Neurol. Psychol 18, 459–482. [Google Scholar]
- York KM, Hassan M, Li Q, Li H, Fillingim RB, Sheps DS, 2007. Coronary artery disease and depression: patients with more depressive symptoms have lower cardiovascular reactivity during laboratory-induced mental stress. Psychosom. Med 69, 521–528. [DOI] [PubMed] [Google Scholar]
- Zigmond AS, Snaith RP, 1983. The hospital anxiety and depression scale. ActaPsychiatr. Scand 67, 361–370. [DOI] [PubMed] [Google Scholar]