Abstract
Background:
Forty-five percent of U.S. births are unintended, and the costs of unintended pregnancy and birth are substantial. Clinical and policy interventions that increase access to the most effective reversible contraceptive methods, intrauterine devices and contraceptive implants, have potential to generate significant cost savings. Evidence of cost savings for these interventions is needed.
Objective:
To conduct a cost savings analysis of the Contraceptive CHOICE Project, which provided counseling and no-cost conception, to demonstrate the value of investment in enhanced contraceptive care to the Missouri Medicaid program.
Study Design:
The CHOICE Project was a prospective cohort study of 9,256 reproductive-age women, enrolled between 2007 and 2011 and followed until October 2013. This analysis includes 5,061 CHOICE Project participants who were current Missouri Medicaid beneficiaries or uninsured and reported household incomes less than 201% of the federal poverty line. We created a simulated comparison group of women receiving care through the Missouri Title X program and modeled the contraception and pregnancy outcomes that would have occurred in the absence of the CHOICE Project. Data about contraceptive use for the comparison group (N=5,061) were obtained from the Missouri Title X program and adjusted based on age, race, ethnicity, and income. To make an accurate comparison accounting for difference in the two populations, we used our simulation model to estimate total CHOICE Project costs and total comparison group costs. We reported all costs in $2013 to account for inflation.
Results:
Among the CHOICE Project participants included, the uptake of intrauterine devices and implants was 76.1% compared to 4.8% among the comparison group. The estimated contraceptive cost for the simulated CHOICE Project group was $4.0 million versus $2.3 million for the comparison group. The estimated numbers of unintended pregnancies and births averted among the simulated CHOICE Project group compared to the comparison group were 927 and 483 respectively, representing a savings in pregnancy and maternity care of $6.7 million. We estimated that the total cost savings for the state of Missouri attributable to the CHOICE Project was $5.0 million (40.7%) over the project duration.
Conclusions:
A program providing counseling and no-cost contraception yields substantial cost savings due to increased uptake of highly effective contraception and consequent averted unintended pregnancy and birth.
Keywords: contraceptive counseling, contraceptive implant, cost savings analysis, intrauterine device, long-acting reversible contraception, return on investment
Introduction
Unintended pregnancy carries significant public health costs including reduced maternal quality of life, adverse maternal behaviors, and poorer infant outcomes.1,2 Societal costs are also large, including reduced educational attainment, employment opportunities, and economic stability as well as greater dependence on public assistance.3 The economic costs of unintended pregnancy and birth are substantial, and U.S. taxpayers pay roughly $11 billion each year in costs associated with unintended pregnancy.4
The Contraceptive CHOICE Project was a prospective study of 9,256 reproductive-age women that provided comprehensive contraceptive counseling, no-cost contraception, and reduced barriers to reversible contraception. These barriers included provider misconceptions,5 high out-of-pocket cost, 6 and multiple visits requirements for initiation of long-acting reversible contraception (LARC; intrauterine devices (IUDs) and implants).7,8 CHOICE participants had a high uptake of LARC and subsequent reductions in unintended and teen pregnancy.9,10 Multiple studies have demonstrated that provision of contraception, including LARC, results in economic savings.11,12 One cost effectiveness analysis found that although LARC is associated with higher upfront costs, these methods generate cost savings after approximately two years of use.13
The objective of this analysis was to estimate the cost savings the CHOICE Project contributed to the Missouri Medicaid program over the study period. Our secondary objective was to estimate potential public cost savings if the CHOICE Project model were scaled up to Missouri Medicaid beneficiaries statewide.
Materials and Methods
Model design and population
Participants in the Contraceptive CHOICE Project were enrolled between 2007 and 2011 and followed for two or three years through October 2013.14 Inclusion criteria for the CHOICE Project included age 14–45 years, not currently using a reversible contraceptive method or willing to start a new method, did not desire pregnancy for the next 12 months, sexually active with a male partner, and resided in the St. Louis area. We limited inclusion in this analysis to women who reported receipt of Medicaid or had incomes less than 201% of the federal poverty level (FPL), which is the income eligibility threshold for Missouri’s family planning waiver program, the Women’s Health Services Program (MO-WHSP), as well as pregnancy-related Medicaid. The time horizon for the analysis was 45 months which included the 36-month study period plus an additional 9 months to account for any births resulting from conception that occurred during the study period.
To create a comparison group for the analysis, we estimated the contraceptive method distribution that women would have selected in the absence of the CHOICE Project. We used data regarding the contraceptive method chosen by women receiving care at Missouri health centers participating in the Title X program between 2008 and 2012. Women who were currently pregnant, seeking pregnancy, or had a prior sterilization were excluded, as they were from the CHOICE Project. Given the demographic differences between the CHOICE cohort and the Title X program participants (shown in Table 1), we used multinomial logistic regression to obtain probabilities that a CHOICE participant, in the absence of the study intervention, would have selected each method. Contraceptive outcomes were categorized as follows: (1) IUD or implant; (2) injectable contraception; (3) oral contraceptive pills (OCPs), contraceptive patch, or vaginal ring; (4) condoms, other barriers methods, withdrawal, or fertility awareness; and (5) no method. Adjustment was limited to four demographic characteristics due to the available MO Title X data: age (19 years and under, 20–29, and 30 and above), race (white, black, and other race), Hispanic identity (non-Hispanic and Hispanic), and federal poverty level (less than 101% of the FPL and 101–200% of the FPL). This group formed the basis for a counterfactual simulation of the actual CHOICE participants’ experience in the absence of the CHOICE Project, thereby creating a comparison group with the CHOICE participant demographics but whose contraceptive choices were based upon the MO Title X population.
Table 1.
Demographic Characteristics of the Contraceptive CHOICE Project Participants and Missouri Title X Family Planning Patients.
|
Characteristic |
Contraceptive CHOICE Project (n=5,061) |
MO Title X Family Planning Clinics, (n=404,352) |
P value |
|---|---|---|---|
| Age Category | <0.0001 | ||
| 15–19 years | 15.0% | 1.4% | |
| 20–29 years | 65.7% | 55.0% | |
| 30–45 years | 19.3% | 43.7% | |
| Race | <0.0001 | ||
| Black | 60.7% | 29.3% | |
| White | 31.5% | 68.3% | |
| Other | 7.7% | 2.5% | |
| Ethnicity | |||
| Hispanic | 6.4% | 5.6% | 0.015 |
| Non-Hispanic | 93.6% | 94.4% | |
| Current Insurance | |||
| Uninsured (or unknown coverage) |
71.5% | 72.8% | 0.033 |
| Public insurance or family planning waiver program |
28.5% | 27.2% | |
| Income | <0.0001 | ||
| At or below 100% FPL | 83.7% | 70.0% | |
| 101%−200% of FPL | 16.3% | 30.0% | |
Abbreviations: FPL, Federal Poverty Level
Percentages may not add to 100% due to rounding.
For each woman in the comparison group, we conducted a Monte Carol simulation of outcomes and associated costs by executing 1,000 draws from the contraceptive distribution given by evaluating the multinomial logistic regression equation using the CHOICE participant’s specific demographic profile. For each draw, we simulated the month-to-month occurrence of pregnancy as well as all possible outcomes (using assumptions discussed in detail below) and tallied associated costs, averaged over 1,000 draws to smooth cost estimates. This generated two sets of simulated results: (1) those for the CHOICE population as predicted by our simulation, and (2) those for the comparison group. The simulated results for the CHOICE Project helped to test the accuracy and reasonableness of the assumptions entered into the simulation. All analyses were performed in SAS 9.4 (SAS Institute, Cary, NC) and STATA 14 (StataCorp, College Station, TX).
Utilization of contraceptive methods
For CHOICE participants, the assigned contraceptive method was the method chosen by the participant at study enrollment. For the comparison group, the method was assigned probabilistically using the MO Title X health center data described above. Methods were grouped into five the same contraceptive categories described above. To account for contraceptive discontinuation among women who chose an IUD or implant at baseline, we used published CHOICE Project continuation rates at one year and two years using a linear trend to estimate monthly continuation rates.15 In case of discontinuation, we assumed the same contraceptive distribution as the comparison group at baseline.
Costs of contraceptive methods
To estimate the contraceptive costs across both the CHOICE and comparison populations, we used Missouri Medicaid reimbursement rates for IUDs, implants, and injectable contraception, and the retail acquisition costs for OCPs, patch, and ring for years 2007 through 2011. These method-specific costs were incorporated into the simulation each time a particular method was drawn. Sensitivity of our results to these values was assessed by running the simulation using annual averaged contraceptive costs estimated by Laliberte et al which used Medicaid claims data for 11 million women across multiple states (including Missouri) between 2004 and 2010.16 Using the averaged contraceptive costs showed minimal difference in the estimated cost savings. See Supplementary Materials for sensitivity analysis results.
Cost of contraceptive initiation
Because the CHOICE Project involved additional programmatic costs due primarily to provision of evidence-based, comprehensive contraceptive counseling by trained non-clinician counselors, we computed the cost of contraceptive initiation using actual costs from the CHOICE Project. Annual salaries and fringe benefits for a full-time nurse practitioner, a half-time registered nurse, and a full-time contraceptive counselor were averaged over the number of CHOICE participants to approximate cost depending on enrollment year. We added 30% to the cost of salaries to account for overhead costs such as rent, utilities, and supplies.17 Since approximately twice the clinician time is required for LARC insertion, the per-participant nurse practitioner cost was calculated as a weighted average, with visits including LARC insertion weighted twice as much as those for non-LARC methods. For IUDs and implants, method and initiation costs were assumed to occur in year 1 only as the maximum duration of study participation was 3 years, therefore, no method replacement due to expiration was necessary.
Contraceptive initiation costs for the comparison group were estimated using Missouri Medicaid reimbursement rates. The estimated cost of initiation of OCPs, patch, ring, and injectable methods was the reimbursement amount for a new patient Level III office visit with a clinician. For initiation costs of IUDs and implant, the reimbursement for a new patient Level III and the method insertion were summed with the weighted by the percent of individuals who chose each type of IUD or the implant. We also calculated CHOICE Project costs using these rates within our simulation in order to capture the likely cost of a large-scale version of the project. See Supplementary Materials Tables 1A–3A for a summary of costs and supporting data sources.
Costs of unintended pregnancy-related events
In order to determine the number of unintended pregnancies, we incorporated previously published “typical use” contraceptive failure rates into the simulation model.18 The simulated CHOICE Project unintended pregnancy and birth outcomes were calibrated to exactly match the actual number of unintended pregnancies and births observed in the CHOICE Project. This calibration occurred within the bounds of parameter ranges suggested by the literature and was chosen deliberately to ensure that the cost calculations would be accurate for the actual CHOICE Project.
Five possible outcomes for unintended pregnancy were considered: live birth, induced abortion covered by Medicaid, induced abortion not covered by Medicaid, miscarriage, and ectopic pregnancy. We used a combination of CHOICE Project data as well as 2010 estimates for the percentages of unintended pregnancies that result in live birth, miscarriage, or abortion in Missouri.19 Additional detail is provided in the Supplementary Materials. The percent of pregnancies ending in an ectopic pregnancy was assumed using methods described by Trussell et al and subtracted from the miscarriage rate.13 The majority of induced abortions were assumed to have zero cost to the state, as Missouri Medicaid does not cover abortion except in cases of maternal life endangerment, rape, and incest. We estimated these to account for approximately one percent of induced abortions.20 Based upon this fact, we separated induced abortions into two categories: abortions covered by Missouri Medicaid and abortions not covered by Missouri Medicaid.
Costs associated with birth outcomes were drawn from multiple sources. We used data for the cost of birth and first year of life to Missouri Medicaid for fiscal years 2009 through 2011 which was obtained from Missouri’s Evaluations of the MO-WHSP from 2011 and 2012.21,22 The costs for miscarriage, induced abortions covered by Medicaid, and ectopic pregnancy were estimated using statistics reported by Trussell et al.13
All costs were adjusted to 2013 dollars for the final estimates to account for inflation. We did not discount costs as the cost savings analysis was conducted from a state budgetary perspective and there were minimal changes in MO Medicaid reimbursement over the time period.
Scaling Up Cost Savings to Approximate Savings for the Missouri Medicaid Populations
To calculate the cost savings from a statewide “scale-up” of the program, we applied our CHOICE Project simulation model to individual data from the 2009–13 American Community Survey (ACS),23 which we limited to all Missouri women aged 18 to 45 who reported receipt of Medicaid or whose household income and uninsured status made them eligible for the MO-WHSP. This approach provides an estimation of the outcomes in a different population (i.e. Missouri women) controlling for age, race, ethnicity, and income as described above. ACS survey weights were used to scale the savings of Missouri ACS respondents to state population level savings. We used estimates of 20 to 40% LARC uptake to calculate a possible range of cost savings that might occur in a statewide scale-up.
Results
Estimated Contraceptive Mix for the CHOICE Project and Comparison Group
Table 2 shows the contraceptive distribution for both groups. Women in the CHOICE Project were more likely to choose an IUD or implant than women in the comparison group, even after adjusting for baseline demographic differences between the groups. Women in the comparison group were more likely to choose OCPs, injectable contraception, condoms, or no contraceptive method.
Table 2.
Contraceptive Distribution for the Contraceptive CHOICE Project and Comparison Group.
| Contraceptive Method |
Contraceptive CHOICE Project (n=5,061) |
Comparison Group a (n=5,061) |
Percentage Point Difference |
|---|---|---|---|
| N (%) | N (%) | ||
| Intrauterine device | 2831(55.9) | 182 (3.6) | + 52.3% |
| Implant | 1036 (20.5) | 61 (1.2) | + 19.3% |
| Injectable | 439 (8.7) | 1731 (34.2) | − 25.5% |
| Oral contraceptive pills | 406 (8.0) | 2059 (40.7) | − 32.7% |
| Contraceptive patch | 102 (2.0) | 76 (1.5) | + 0.5% |
| Vaginal ring | 246 (4.9) | 142 (2.8) | + 2.1% |
| Natural family planning | 0.0 | 10 (0.2) | − 0.2% |
| Male condom | 0.0 | 577 (11.4) | − 11.4% |
| No method | 0.0 | 172 (3.4) | − 3.4% |
| Other method | 0.0 | 51 (1.0) | − 1.0% |
| Total | 100 | 100 | 100 |
The contraceptive distribution for the simulated comparison group is based on MO Title X Family Planning Health Center data adjusted for age, race, ethnicity and income.
Percentages may not add to 100% due to rounding.
Estimated number of unintended pregnancies averted in the CHOICE Project
Table 3 shows the simulated unintended pregnancy and birth outcomes and cost savings for the CHOICE participants and comparison group. There were 475 unintended pregnancies among the CHOICE Project cohort and an estimated 1,402 unintended pregnancies in the comparison group for a total of 927 unintended pregnancies averted. There were 247 unintended births in the CHOICE Project and an estimated 730 unintended births in the comparison group for 483 unintended births averted. The simulated CHOICE outcome of 247 unintended births was calibrated slightly to match the actual CHOICE outcome of 247 unintended births.
Table 3.
Comparison of Pregnancy and Cost Outcomes Between CHOICE Project and Simulated Comparison Group.
| Simulated CHOICE Project (1) |
Simulated Comparison Group (2) |
Difference (1–2) |
|
|---|---|---|---|
| Number of Unintended Pregnancies | 474.8 | 1401.7 | −926.9 |
| Unintended Pregnancy Rate (per 1,000 reproductive age women) |
37.7 | 116.1 | |
| Number of Unintended Births | 246.9 | 729.6 | −482.7 |
| Unintended Birth Rate (per 1,000 reproductive age women) | 19.6 | 60.4 | |
| Total Cost | $7,261,838 | $12,246,296 | −$4,984,458 |
| Contraceptive Costs | $4,019,056 | $2,343,820 | $1,675,236 |
| Pregnancy-Related Costs | $3,242,782 | $9,902,476 | −$6,659,694 |
| Annualized Cost | $2,858,991 | $4,821,376 | −$1,962,385 |
Estimated Costs Savings Resulting from the CHOICE Project for Missouri Medicaid
Table 3 also shows the estimated cost savings to Missouri Medicaid due to the CHOICE Project. Not surprisingly, the CHOICE Project was associated with higher contraceptive costs compared to the comparison group, because more women in the CHOICE Project chose IUDs and implants. Most of these costs occurred early in the study period when most women were initiating IUDs and implants as shown in Figure 1. The pregnancy-related costs, however, are lower in the CHOICE Project than in the comparison group, both in absolute terms and the annual average, due to the higher number of pregnancies averted. Because of the timeline of the CHOICE Project, approximately half of women were observed for two rather than three years.15 For this reason, Table 3 reports an overall sum of costs and savings as well as an annualized average that is adjusted to account for the variation in follow-up time. Thus, total costs in the comparison group are estimated to be $12.2 million compared to $7.3 million for the CHOICE Project group, which is a 40.7% reduction in costs related to contraception, unintended pregnancy, and birth.
Figure 1:
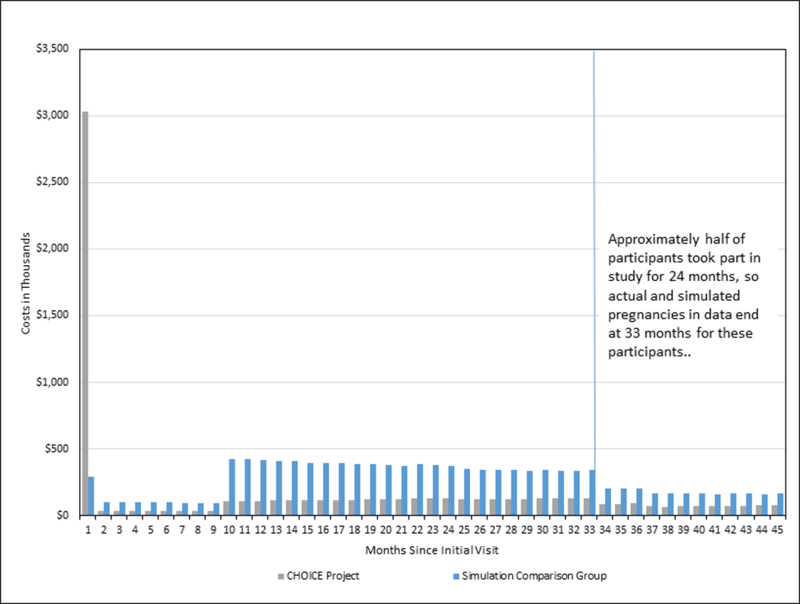
Monthly Cost Expenditure over Contraceptive CHOICE Project Period.
Figure 1 compares monthly costs over time for the simulated CHOICE Project and comparison groups. Higher up-front costs due to the use of IUDs and implants a lead to lower costs occurring during the two to three-year study follow-up period; we extended the comparison nine months beyond the study end to account for pregnancies in which conception occurred during study participation but the outcome (i.e. birth) did not occur until after the study ended, since these costs are also attributable to the study period.
Estimated Cost Savings Scaled Up to Missouri Medicaid Statewide
ACS data show that 132,058 women of reproductive age received Missouri Medicaid annually. During 2011, the average enrollment in the Women’s Health Services Program was 61,297.27 A scale-up of the CHOICE Project could save an estimated $79.7 million if 20% of female, reproductive-age, Medicaid beneficiaries chose LARC, increasing to $156.8 million if 40% chose LARC. The cost savings for the MO-WHSP range from an estimated $29.3 to $75.3 million, respectively. Using ACS data, we also estimated that a total of 123,571 women were actually eligible for the MO-WHSP; if all these eligible women were to enroll, the estimated cost savings for this group would range from $59.0 to $151.9 million. These data are shown in Table 4.
Table 4.
Estimated Cost Savings Associated with Statewide Scale Up of the Contraceptive CHOICE Project Model.
| Percent Using a LARC Method | |||
|---|---|---|---|
| 20% | 30% | 40% | |
| Women aged 18–45 who are current MO Medicaid beneficiaries (n=132,058)a | |||
| Unintended pregnancies avoided | 10,431 | 16,250 | 19,978 |
| Unintended births avoided | 6,903 | 10,695 | 13,518 |
| Estimated cost savings, 2013$ | $79,712,958 | $123,788,762 | $156,769,168 |
| Women enrolled in MO Women’s Health Services Program in 2011(n=61,297) | |||
| Unintended pregnancies avoided | 4,199 | 6,813 | 9,833 |
| Unintended births avoided | 2,653 | 4,536 | 6,469 |
| Estimated cost savings, 2013$ | $29,289,520 | $52,563,031 | $75,339,232 |
| Women aged 18–45 eligible for MO Women’s Health Services Program in 2011 (n=123,571)a | |||
| Unintended pregnancies avoided | 8,466 | 13,375 | 19,823 |
| Unintended births avoided | 5,348 | 9,145 | 13,040 |
| Estimated cost savings, $2013 | $59,045,880 | $105,963,854 | $151,879,280 |
LARC, Long-Acting Reversible Contraceptive
Estimated using data from the 2009–13 Annual Community Survey
Comment
In this analysis, we found the CHOICE Project generated a $5.0 million cost savings for Missouri Medicaid due to unintended births averted among women who had Medicaid or who would be eligible for expanded Medicaid in the case of a pregnancy, a 41% reduction in costs for the cohort over the time period. The cost savings in our analysis are consistent with those estimated by other studies. A statewide initiative in Colorado serving about 50,000 women annually found that increased provision of LARC resulted in an estimated cost savings of approximately $52 million to the state Medicaid program. 24,25 A national study of publicly supported family planning services to 8.9 million women found a $10.5 billion cost savings due to unintended pregnancies averted.26 It is important to note that our cost savings analysis was conducted for a cohort of 5,000 women and estimated only the direct health costs of unintended pregnancies averted over the study period, not indirect economic and social costs affecting mothers and children.
Strengths of this study include use of a comparison group of Missouri women seeking care at Title X health centers to estimate the contraceptive distribution in absence of the CHOICE Project. We used the actual unintended pregnancy and birth rates from CHOICE to inform the simulation and estimate the number of pregnancies averted by the CHOICE Project. The Monte Carlo simulation approach also allowed us to demonstrate the robustness of our findings to a range of assumptions. Lastly, we were able to obtain Missouri Medicaid level data for the costs of birth and first year of life to create a more precise estimate of costs associated with unintended birth, which is the largest contributor to pregnancy-related costs.
There are some limitations to our study. First, women in both the CHOICE Project and the comparison group were presenting for contraceptive care and therefore may not reflect contraceptive use among the general population. Furthermore, women in the CHOICE Project may have self-selected into the study specifically because they desired LARC and, as result, may not be generalizable to other populations. However, a prior analysis comparing CHOICE participants’ with National Survey of Family Growth and Missouri Behavioral Risk Factor Surveillance System respondents found that while demographic and contraceptive characteristics did differ, the absolute differences were small.27 In addition, other programs have demonstrated LARC uptake substantially higher than the national estimates.24,28,29 Therefore, it is unlikely that the difference in LARC use between CHOICE participants and MO Title X patients is attributable mainly to selection bias. In addition, due to limited data for the MO Title X patients, we were only able to control for a small number of the demographic characteristics which may influence contraceptive preferences. Lastly, this analysis did not take into account contraceptive switching or discontinuation for any method other than IUDs and implants. Not capturing the costs associated with initiating a new method may underestimate contraceptive costs and overestimate the cost savings slightly. We also assumed that women who discontinued an IUD or implant, chose a new method based on the distribution of the comparison group. However, women in the CHOICE Project group may have been more likely to choose another IUD or implant which would underestimate cost savings.
Multiple barriers to LARC continue to exist, including requirements for preauthorization, multiple visits for initiation, insurance access, and cost.30,31 Furthermore, the U.S. federal government is actively working to weaken the contraceptive guarantee and the Title X program.32,33 However, there are also concerns that “promotion” of LARC may result in coercive practices.34,35 We emphasize that any interventions to increase access to LARC be patient-centered, respect women’s autonomy, and include the full range of contraceptive options, while also removing barriers to care.
Our results demonstrate that increased provision of IUDs and implants can reduce public healthcare spending. The potential cost savings of scaling up a model of care similar to the CHOICE Project are large; thus state Medicaid programs looking at budget priorities should focus on removal of barriers to all contraceptive methods.
Supplementary Material
AJOG at a Glance:
We conducted this cost savings analysis to estimate the cost savings to Missouri Medicaid due to the high uptake of intrauterine devices and implants in the Contraceptive CHOICE Project and subsequent unintended pregnancies averted.
In this cost savings analysis of 5,061 reproductive-age women provided with no-cost contraception, Missouri Medicaid saved an estimated $5.0 million due to 483 unintended births averted.
These results provide important data about the public cost savings that may result from the increased uptake of intrauterine devices and implants. These data have implications for broader policies aimed at reducing unintended pregnancies as well as healthcare costs.
Acknowledgements
We thank Missouri Family Health Council (organization) for their generous sharing of data on contraceptive use on Missouri Title X clients (no compensation provided). We would also like to thank Linda Li, MPH (employment Washington University Brown School, no compensation) for her assistance with preparation of this manuscript.
Funding: This study was supported in part by: 1) an anonymous foundation; and 2) award number K23HD070979 from the Eunice Kennedy Shriver National Institute of Child Health & Human Development (NICHD). The funders had no role in the identification, design, conduct, and reporting on this analysis. The content is solely the responsibility of the authors and does not necessarily represent the official view of NICHD.
Footnotes
Conflicts of Interest: T.M. serves on a data safety monitoring board for phase 4 safety studies of Bayer contraceptive products. J.F.P. receives research funding from Bayer Healthcare Pharmaceuticals and Merck & Co, Inc. and serves on an advisory board for TEVA Pharmaceuticals and Watson/Activis. T.D.M. serves on a health policy advisory committee for Centene Corporation. The other authors have no potential conflicts of interest to disclose.
Condensation: A program providing counseling and no-cost contraception yields substantial cost savings due to increased uptake of highly effective contraception and averted unintended pregnancy and birth.
References
- 1.Schwarz EB, Smith R, Steinauer J, Reeves MF, Caughey AB. Measuring the effects of unintended pregnancy on women’s quality of life. Contraception. 2008;78(3):204–210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Hellerstedt WL, Pirie PL, Lando HA, et al. Differences in preconceptional and prenatal behaviors in women with intended and unintended pregnancies. Am J Public Health. 1998;88(4):663–666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Sonfield A, H K, M.L. K, Anderson R The Social and Economic Benefits of Women’s Ability To Determine Whether and When to Have Children. New York: Guttmacher Institute;2013. [Google Scholar]
- 4.Sonfield A, Kost K, Gold RB, Finer LB. The public costs of births resulting from unintended pregnancies: national and state-level estimates. Perspect Sex Reprod Health. 2011;43(2):94–102. [DOI] [PubMed] [Google Scholar]
- 5.Luchowski AT, Anderson BL, Power ML, Raglan GB, Espey E, Schulkin J. Obstetrician-gynecologists and contraception: practice and opinions about the use of IUDs in nulliparous women, adolescents and other patient populations. Contraception. 2014;89(6):572–577. [DOI] [PubMed] [Google Scholar]
- 6.Broecker J, Jurich J, Fuchs R. The relationship between long-acting reversible contraception and insurance coverage: a retrospective analysis. Contraception. 2016;93(3):266–272. [DOI] [PubMed] [Google Scholar]
- 7.Bergin A, Tristan S, Terplan M, Gilliam ML, Whitaker AK. A missed opportunity for care: two-visit IUD insertion protocols inhibit placement. Contraception. 2012;86(6):694–697. [DOI] [PubMed] [Google Scholar]
- 8.Biggs MA, Arons A, Turner R, Brindis CD. Same-day LARC insertion attitudes and practices. Contraception. 2013;88(5):629–635. [DOI] [PubMed] [Google Scholar]
- 9.Peipert JF, Madden T, Allsworth JE, Secura GM. Preventing unintended pregnancies by providing no-cost contraception. Obstet Gynecol. 2012;120(6):1291–1297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Secura GM, Madden T, McNicholas C, et al. Provision of no-cost, long-acting contraception and teenage pregnancy. N Engl J Med. 2014;371(14):1316–1323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cleland K, Peipert JF, Westhoff C, Spear S, Trussell J. Family planning as a cost-saving preventive health service. N Engl J Med. 2011;364(18):e37. [DOI] [PubMed] [Google Scholar]
- 12.Foster DG, Biggs MA, Malvin J, Bradsberry M, Darney P, Brindis CD. Cost-savings from the provision of specific contraceptive methods in 2009. Womens Health Issues. 2013;23(4):e265–271. [DOI] [PubMed] [Google Scholar]
- 13.Trussell J, Henry N, Hassan F, Prezioso A, Law A, Filonenko A. Burden of unintended pregnancy in the United States: potential savings with increased use of long-acting reversible contraception. Contraception. 2013;87(2):154–161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Secura GM, Allsworth JE, Madden T, Mullersman JL, Peipert JF. The Contraceptive CHOICE Project: reducing barriers to long-acting reversible contraception. Am J Obstet Gynecol. 2010;203(2):115 e111–117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.O’Neil-Callahan M, Peipert JF, Zhao Q, Madden T, Secura G. Twenty-four-month continuation of reversible contraception. Obstet Gynecol. 2013;122(5):1083–1091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Laliberte F, Lefebvre P, Law A, et al. Medicaid spending on contraceptive coverage and pregnancy-related care. Reprod Health. 2014;11(1):20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lairsona D, Chana W, Y C, del Juncob D, Vernona S. Cost-Effectiveness of Targeted vs. Tailored Interventions to Promote Mammography Screening Among Women Military Veterans in the United States. Eval Program Plann.34(2):97–104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sundaram A, Vaughan B, Kost K, et al. Contraceptive Failure in the United States: Estimates from the 2006–2010 National Survey of Family Growth. Perspect Sex Reprod Health. 2017;49(1):7–16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Finer LB, Kost K. Unintended pregnancy rates at the state level. Perspect Sex Reprod Health. 2011;43(2):78–87. [DOI] [PubMed] [Google Scholar]
- 20.Finer LB, Frohwirth LF, Dauphinee LA, Singh S, Moore AM. Reasons U.S. women have abortions: quantitative and qualitative perspectives. Perspect Sex Reprod Health. 2005;37(3):110–118. [DOI] [PubMed] [Google Scholar]
- 21.State of Missouri Department of Social Services. Evaluation of the Women’s Health Services Program: Section 1115 Demonstration Project. Evaluation Year 3: October 1, 2009-September 30, 2010. Washington, DC: Alicia Smith & Associates;2011. [Google Scholar]
- 22.State of Missouri Department of Social Services. Evaluation of the Women’s Health Services Program: Section 1115 Demonstration Project. Evaluation Year 4: October 1, 2010-September 30, 2011. Washington, DC: Alicia Smith & Associates;2012. [Google Scholar]
- 23.American Community Survey: 2009–2013 ACS 5-YEAR PUMS FILES. 2015; https://factfinder.census.gov/faces/tableservices/jsf/pages/productview.xhtml?pid=ACS_pums_csv_2009_2013&prodType=document.
- 24.Ricketts S, Klingler G, Schwalberg R. Game change in Colorado: widespread use of long-acting reversible contraceptives and rapid decline in births among young, low-income women. Perspect Sex Reprod Health. 2014;46(3):125–132. [DOI] [PubMed] [Google Scholar]
- 25.Colorado Department of Public Health and Environment; Taking the Unintended Out of Pregnancy: Colorado’s Success with Long-Acting Reversible Contraception; Denver, CO: 2017. [Google Scholar]
- 26.Frost JJ, Zolna MR, Frohwirth L. Contraceptive needs and services, 2010. New York: Guttmacher Institute; 2013. [Google Scholar]
- 27.Kittur ND, Secura GM, Peipert JF, Madden T, Finer LB, Allsworth JE. Comparison of contraceptive use between the Contraceptive CHOICE Project and state and national data. Contraception. 2011;83(5):479–485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Cohen R, Sheeder J, Kane M, Teal SB. Factors Associated With Contraceptive Method Choice and Initiation in Adolescents and Young Women. J Adolesc Health. 2017;61(4):454–460. [DOI] [PubMed] [Google Scholar]
- 29.Harper CC, Rocca CH, Thompson KM, et al. Reductions in pregnancy rates in the USA with long-acting reversible contraception: a cluster randomised trial. Lancet. 2015;386(9993):562–568. [DOI] [PubMed] [Google Scholar]
- 30.Wood S, Beeson T, Bruen B, et al. Scope of family planning services available in Federally Qualified Health Centers. Contraception. 2014;89(2):85–90. [DOI] [PubMed] [Google Scholar]
- 31.Politi MC, Estlund A, Milne A, Buckel CM, Peipert JF, Madden T. Barriers and facilitators to implementing a patient-centered model of contraceptive provision in community health centers. Contracept Reprod Med. 2016;1:21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.White House Acts to Roll Back Birth-Control Mandate for Religious Employers. New York TImes. May/29/17. [Google Scholar]
- 33.Trump Rule Could Deny Birth Control Coverage to Hundreds of Thousands of Women. New York Times. June/1/17, 2017. [Google Scholar]
- 34.Gomez AM, Fuentes L, Allina A. Women or LARC first? Reproductive autonomy and the promotion of long-acting reversible contraceptive methods. Perspect Sex Reprod Health. 2014;46(3):171–175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Gubrium AC, Mann ES, Borrero S, et al. Realizing Reproductive Health Equity Needs More Than Long-Acting Reversible Contraception (LARC). Am J Public Health. 2016;106(1):18–19. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


