Abstract
Accumulation of classical monocytes is imperative for the progression of atherosclerosis. Hence, therapeutic interference with mechanisms of lesional monocyte recruitment, the primary mechanism controlling macrophage accumulation, may allow for targeting atheroprogression and its clinical complications. Here, we review the important role of classical monocytes in atheroprogression as well as their routes of arterial recruitment. We specifically highlight the role of cell adhesion molecules as well as of platelet-derived chemokines and neutrophil-borne alarmins.
Key Words: Monocyte, Neutrophil, Platelet, Recruitment, Atherosclerosis
Introduction
Cardiovascular events are the main cause of morbidity and mortality in western societies. Clinical manifestations such as myocardial infarction and stroke mainly rely on the development and progression of atherosclerosis. Understanding of the pathophysiology of atherosclerosis has improved during recent years and we now know that atherosclerosis is a chronic inflammatory disease of the arterial wall, which in early stage is characterized by an endothelial dysfunction. Activation of endothelium leads to the upregulation of adhesion molecules and the release of cytokines and chemokines, all of which orchestrate leukocyte adhesion and transmigration. Among all leukocytes, monocytes are appreciated to be the most abundant subset to enter atherosclerotic lesions already in early stage and also during the course of lesion progression [1]. Hence, lesion growth and differentiation is primarily sustained by constant monocyte influx [2]. Once monocytes have entered the lesion, they differentiate into macrophages and, after uptake of oxidized low-density lipoprotein, into foam cells. Such processes could be limited by prevention of continued monocyte influx [3], premature macrophage apoptosis [4] or egress of such cells [5], the latter being a mechanism with debated significance. Thus, recruitment, apoptosis and egress of monocytes/macrophages may all three serve as targets for therapeutic intervention to limit atherosclerosis.
This review will summarize the importance of classical monocytes in atherogenesis and especially focus on the recruitment of those cells to sites of atherosclerosis. Besides the well-described direct mechanisms of adhesion, activation and transmigration, we will particularly highlight the importance of cell to cell interactions exerted by platelets or neutrophils promoting classical monocyte recruitment in atherosclerosis. However, most of the findings reviewed here stem from animal models making a direct translation into the human situation difficult. Thus, more research needs to be done to clearly prove if such mechanistic assumptions hold true in human pathogenesis.
Monocyte and Macrophage Subsets in Atherosclerosis
About 25 years ago, monocytes were proven to be present in both human plaques and lesions obtained from animal models [6, 7]. Direct evidence of the relevance of monocytes in atherogenesis could be demonstrated in a study where depletion of monocytes reduced plaque formation in rabbits [8]. However, a more recent study concentrated on the question whether depletion of monocytes and macrophages during early or later stages differentially impacts on atherosclerosis [9]. Although employing the diphtheria toxin receptor-mediated conditional cell ablation of all CD11b+ cells which may affect various myeloid cell subsets, depletion during early stages led to decreased plaque size accompanied by reduced macrophage numbers, collagen content and necrotic core within the lesion, whereas depletion during later stages did not have any of those effects, suggesting the importance of monocytes during early stages of atherogenesis [9]. The protective effect of monocytes during later stages of atherosclerosis may relate to their scavenger function clearing apoptotic cells, which protects from inflammatory processes exerted by secondary necrotic cells [10].
Two principal monocyte subsets exist in humans and mice [11, 12]. In humans, monocytes can be differentiated based on the expression of CD14 and CD16 [13, 14]. Classical monocytes are defined as CD14+CD16-, whereas non-classical monocytes are CD14lowCD16+. In mice, CD115+ monocyte subsets are discriminated based on the expression of lymphocyte antigen 6C (Ly6C). Ly6C+ monocytes are CX3CR1lowCCR2+ and thought to correspond to human classical monocytes. In contrast, murine Ly6C- monocytes CX3CR1highCCR2- are phenotypic equivalents of human non-classical monocytes [15]. However, the relative distribution of these subsets among total monocyte counts differs between human and mouse (90:10 vs. 50:50). Nevertheless, they widely exhibit similar expression patterns for a variety of adhesion molecules, chemokine receptors and other markers indicating comparable functional characteristics in both species (table 1) [16]. Murine classical monocytes are primarily recruited to inflamed tissue and lymph nodes in vivo, produce high levels of tumor necrosis factor (TNF)-α and interleukin (IL)-1 during infection or tissue damage, and therefore, are also termed ‘inflammatory monocytes’ [12, 17, 18].
Table 1.
Adhesion molecules, chemokine receptors and other markers in humans and mice
| Subset | Human |
Mouse |
||
|---|---|---|---|---|
| classical | non-classical | classical | non-classical | |
| Adhesion molecules | ||||
| CD62L | + + | – | + + | – |
| PSGL-1 | + + | + | + + | + |
| CD44 | n.d. | n.d. | + | + |
| CD11a | n.d. | n.d. | + | + + |
| CD11b | + + | + + | + + | + + |
| CD49b | n.d. | n.d. | + | – |
| Chemokine receptors | ||||
| CCR1 | + | – | + + | + |
| CCR2 | + + | – | + + | + |
| CCR5 | + | + | + | + |
| CX3CR1 | + | + + | + | + + |
| Others | ||||
| F4/80 | n.d. | n.d. | + | + |
| Gr1 | n.d. | n.d. | + | – |
| CD115 | + + | + + | + + | + + |
| MHCII | + | + + | – | – |
| CD68 | + + | + + | + | + |
n.d. = Not defined.
During the last years, it became evident that hyperlipidemia, an important risk factor for atherosclerosis, induces expansions of classical but not non-classical monocytes [19]. Subsequently, apolipoprotein E (ApoE) on hematopoietic stem and multipotential progenitor cells (HSPCs) has been identified as part of an ABC transporter-mediated cholesterol efflux pathway and suppressor of HSPC proliferation, providing a mechanistic link between hypercholesterolemia, leukocytosis and the subsequent development of atherosclerotic lesions in mice [20, 21, 22]. Moreover, a more recent study describes that cholesterol efflux via ABC transporters prevents from HSPC mobilization and extramedullary proliferation [23] which might be of high interest as the spleen has previously been identified to be a reservoir of classical monocytes which can be readily mobilized during inflammation [24]. In accordance with this finding, splenectomized mice failed to develop monocytosis under acute inflammatory conditions [24], and splenic monocytes give rise to lesional macrophages [25] and infiltrate the myocardium after infarction [26].
Circulating classical monocyte counts directly correlate with the extent of atherosclerotic lesion formation [19, 27, 28], and hence, mechanisms maintaining monocyte homeostasis are of interest in the discussion of arterial monocyte accumulation. By employing a combinatory depletion and resubstitution strategy for whole leukocytes and classical monocytes, we could recently demonstrate that classical rather than non-classical monocytes drive atheroprogression [28]. Homeostasis of classical monocytes is tightly regulated by the MCP-1/CCR2 axis with mice deficient in CCR2 having very much reduced counts of circulating classical monocytes. Thus, under acute inflammatory conditions, murine classical monocytes are massively mobilized from bone marrow in a CCL2/CCR2- and CCL7/CCR2-dependent fashion [29, 30]. However, in the context of atherosclerosis, this axis seems to be of minor relevance as plasma concentrations of CCL2 and CCL7 do not increase in Apoe−/− mice fed a high-fat diet [28]. Additionally, although mice deficient in CCR2 display a markedly reduced number of circulating classical monocytes under steady-state conditions, monocyte counts still increase under hypercholesterolemia [28]. Although, the before mentioned findings exclusively stem from mouse models, the importance of human monocyte subsets has further been proved in recent studies, clearly indicating a correlation between classical monocyte counts and the occurrence of cardiovascular events. Hence, classical rather than non-classical monocytes have been identified as possible prediction markers in human [31, 32].
Once recruited to sites of inflammation, classical monocytes are supposed to preferentially differentiate to M1 macrophages or TNF-α-producing Tip-DCs [17]. In contrast, extravasated non-classical monocytes initiate a typical macrophage differentiation program by expression and upregulation of markers characteristic for alternatively activated macrophages [33], also termed ‘M2-like macrophages’ [34, 35]. However, such simplified classification seems not to be applicable in atherosclerosis as M1 or M2 macrophages within the lesion could not be proved to descend from the one or the other monocyte subset, so far. M1 as well as M2 macrophages are both detectable within human and murine atherosclerotic lesion sites [36, 37]. Of note, based on their inflammatory characteristics, M1 macrophages are expected to promote atherosclerosis development, while M2 macrophages in general may be considered to be protective in this regard [38]. Both subsets have been shown to be able to undergo a switch from one macrophage phenotype to the other depending on the stage-dependent environment within atherosclerotic lesions [36]. Thus, suggesting a preferential role of the cytokine microenvironment within the lesion rather than the cellular origin in M1-macrophage polarization [39]. However, the specific cytokine milieu might be primarily sustained by TNFα and IL-1-secreting classical monocytes continuously infiltrating the lesion. This is further corroborated by a recent finding that IL-13 decreases vascular endothelial cell adhesion molecule 1 (VCAM-1)-mediated recruitment of classical monocytes which not only resulted in reduced macrophage accumulation but also induced alternatively activated M2 macrophages [40]. Furthermore, depletion of classical but not non-classical monocytes increased the fraction of M2 macrophages within lesions from aortic roots (unpublished data), indicating that classical monocytes secrete cytokines to suppress polarization towards alternatively activated M2 macrophages. In human, macrophage heterogeneity in atherosclerosis was demonstrated early on, characterizing centrally located macrophages as being more mature and differentiated compared to their counterparts within the superficial layer [41]. Although specific markers for M1 as well as M2 macrophages are present within human carotid atherosclerotic lesions [37], functional associations are rare. However, CD163 a marker typical for M2 macrophages could be related to intra-plaque hemorrhage [42]. This finding was further corroborated by another study demonstrating that M1 macrophages dominate the rupture-prone shoulder of atherosclerotic plaques whereas M2 specific markers were detectable in vascular adventitial tissue and stable plaques [43]. All of these findings highlight the importance of classical monocytes in atheroprogression. Therefore, a detailed understanding of classical monocyte recruitment to atherosclerotic lesions is essential for the identification of new therapeutic options.
Monocyte Recruitment - The Role of Adhesion Molecules and Chemokines
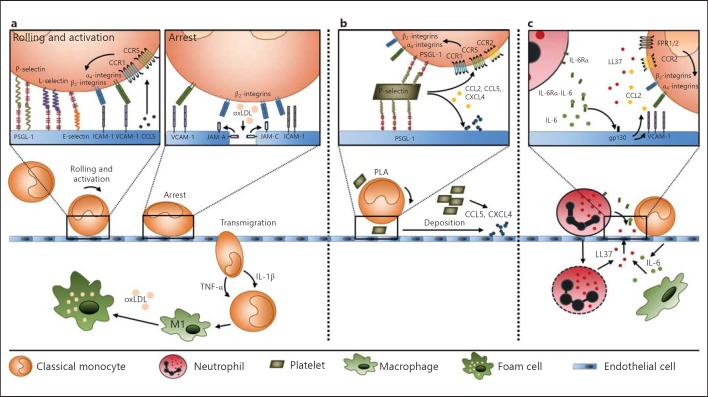
The classical leukocyte adhesion cascade is characterized by rolling, which is mediated by selectins, by activation, which is mediated by chemokines, and by integrin-mediated arrest [44]. However, progress has been made in defining additional steps such as capture (or tethering), slow rolling, adhesion strengthening and spreading, intravascular crawling, and paracellular and transcellular transmigration, which is mediated by integrins and junctional molecules (fig. 1) [44]. P-selectin, for example, which is expressed on monocytes, neutrophils and lymphocytes [15], is upregulated in human atherosclerotic plaques whereas it is not expressed on non-inflamed endothelium [45]. Mice deficient in P-selectin displayed lower macrophage numbers in the plaque and developed smaller atherosclerotic lesions [46] indicating reduced influx of classical monocytes. Similar effects on plaque development were observed in E-selectin-deficient mice [47]. The involvement of selectins and cell adhesion molecules in general has traditionally been investigated for the whole monocyte population, whereas recent data indicate distinct engagement patterns of these receptors for monocyte subsets [15]. For instance, P-selectin glycoprotein ligand 1 (PSGL-1), the high-affinity counter-receptor for P-selectin, has been demonstrated to be expressed at higher levels on classical monocytes and is hence crucially involved in the interaction of these cells with the atherosclerotic endothelium [48]. Furthermore, classical monocytes express higher amounts of CD62L and CD49b as compared to their non-classical counterparts (table 1) [15]. Thus, one may speculate that these molecules primarily contribute to the accumulation of classical rather than non-classical monocytes. Monocytes express both α4- as well as β2-integrins interacting with endothelial VCAM-1 and ICAM-1, respectively. Absence of either ICAM-1 or β2-integrins or both led to reduction in aortic root lesion sizes [49]. Similarly, VCAM-1-dependent mechanisms were found to be crucial in early stages of atherosclerosis [50]. Hence, inhibition of α4-integrin and ICAM-1 markedly attenuates lesional macrophage accumulation in atherosclerotic plaques in Apoe−/− mice [51]. The junctional adhesion molecule (JAM)-C is known to be a counter receptor for CD11b/CD18, thereby promoting leukocyte adhesion. JAM-C is highly expressed in atherosclerotic vessels [52]. Exposure of endothelial cell monolayers to oxidized low-density lipoprotein induces reorganization from interendothelial junctions towards the luminal side of the endothelium, thus promoting leukocyte adhesion [52]. In line, blockade of JAM-C reduces monocyte adhesion in vivo [53]. Similarly, JAM-A binds to CD11b/CD18 [54] and promotes monocyte adhesion under atherosclerotic conditions [55]. Interfering with chemokine-dependent activation has been widely described to protect from atherosclerosis [56, 57]. CCL5 for example, as well as other chemokines, have been shown to be deposited onto inflamed endothelium, thereby triggering the arrest of rolling monocytes [58, 59]. In general, leukocyte integrin affinity can be modulated in a chemokine and G-protein-coupled receptor-dependent manner [60, 61]. Besides a possible role of chemokine receptors in cell endurance [4], inflammatory monocytes were depicted to emigrate into atherosclerotic lesions by utilizing CX3CR1, CCR2 and CCR5 [62]. However, by dissecting chemokine-related effects on myeloid cell hemostasis from direct impact on recruitment, we recently demonstrated that adhesion and recruitment of classical monocytes to atherosclerotic lesions relies on CCR1 and CCR5 but is not dependent on CX3CR1 or CCR2 [28].
Fig. 1.
Recruitment of classical monocytes in atherosclerosis. a Rolling of classical monocytes along atherosclerotic endothelium is primarily mediated by selectins and PSGL-1 but also by the interaction of α4- and β2-integrins with ICAM-1 and VCAM-1. Integrins on the cell surface of classical monocytes are further activated by binding of chemokines such as CCL5 to its receptors CCR1 and CCR5, thereby promoting firm adhesion of cells. Once emigrated, classical monocytes become macrophages and provide a cytokine milieu favoring M1-like macrophage polarization and, after uptake of oxidized low-density lipoprotein (oxLDL), transform into foam cells. b Platelets and classical monocytes can form aggregates (PLAs), thereby promoting tethering and slow rolling along the endothelium. Activated platelets secret several chemokines which are either deposited onto the endothelium or can directly activate classical monocytes via their respective receptors. c By releasing azurocidin (LL37/CRAMP), neutrophils mediate adhesion of classical monocytes to atherosclerotic endothelium via FPRs (FPR1/2). Another proposed mechanism is the shedding of IL-6Rα from neutrophils which forms complexes with IL-6 released from either macrophages or endothelial cells, thus inducing release of CCL2 and upregulation of VCAM-1 on endothelial cells.
Monocyte-Platelet Interplay in Atherosclerosis
In addition to their well-appreciated role in coagulation, the importance of activated platelets in the initiation of atherosclerotic lesion formation evolved over the last decade and is now widely accepted [63, 64]. The importance of platelets was further proven in a study where repeated injection of activated platelets led to exacerbated atherosclerosis in hyperlipidemic mice [59]. Two principal mechanisms have been proposed by which platelets might trigger monocyte recruitment during atherosclerosis development. First, activated platelets have been described to form aggregates with leukocytes (platelet-leukocyte aggregate, PLA), especially monocytes, thereby triggering inflammatory reactions of the arterial wall and endothelial cells [64, 65, 66]. The clinical relevance of those aggregates was evidenced in acute coronary syndrome [67]. Through P-selectin, platelets bind to PSGL-1 and thereby form multicellular aggregates, which can promote the release of chemokines CCL2 and CCL5 and cytokines such as IL-1β to further activate leukocytes [59, 64]. Additionally, physical interaction of platelets and leukocytes induces tethering and rolling of PLAs on endothelial cells with higher avidity compared to non-aggregated leukocytes enhancing endothelial activation and leukocyte transmigration [65, 68] (fig. 1).
A second mechanism of platelet-mediated monocyte recruitment involves the release of a multitude of preformed proteins from platelet α-granules. Secreted proteins include chemokines such as CXCL4 (PF4), CCL5 (RANTES), CXCL7 (CTAP-III) and CXCL12 (SDF1) [64] that can easily be deposited on activated endothelium, thereby triggering monocyte adhesion [58]. Deposition of CCL5 requires platelet activation through P-selectin [69, 70]. Hence, blockade of P-selectin or depletion of platelets in hyperlipidemic mice markedly reduced CCL5 deposition on arterial endothelium, thereby reducing adhesion of monocytes and neutrophils [69, 70]. CCL5 acts through CCR1 and CCR5, both of which have been identified to be crucially involved in classical monocyte recruitment to sites of atherosclerosis [28, 62]. Of note, heteromers of platelet-derived CXCL4 and CCL5 have been demonstrated to further amplify monocyte adhesion to endothelial cells under flow conditions [71]. In line, blockade of heteromerization by a peptide inhibitor resulted in attenuated monocyte recruitment and reduced atherosclerosis in vivo [72].
Neutrophils Pave the Way for Classical Monocytes in Atherosclerosis
Neutrophil depletion during early stages of atherosclerosis leads to significantly reduced numbers of inflammatory monocytes as well as macrophages within the arterial wall [70]. Hence, a partnership between these two leukocyte subsets especially during onset of atherosclerosis appears likely. Once adhering to the vessel wall, neutrophils release soluble components such as azurocidin, which is cationic in nature and therefore favors immobilization on the endothelium, where it is presented to rolling monocytes and promotes their firm adhesion [73]. This is complemented by the capacity of azurocidin to increase expression of adhesion molecules [74, 75]. Other neutrophil-borne antimicrobial peptides described to possess monocyte-attracting activity are cathepsin G [76], cathelicidins (LL37 in humans, CRAMP in mice) and defensins [77], all of which can be found in plaques [15, 78]. Cathepsin G and cathelicidins have been described to induce chemotactic activity by engagement of formyl peptide receptors (FPRs) [79, 80, 81] which are present on classical monocytes, whereas human neutrophil peptides seem to trigger endothelial and platelet activation, thereby promoting monocyte adhesion and accumulation [82]. However, until recently, a conclusive mechanism linking neutrophil secretion products and monocyte recruitment in atherosclerosis remained elusive. Then it became evident that neutrophil-derived CRAMP is responsible for classical monocyte adhesion to atherosclerotic endothelium during early stages of lesion formation. Hyperlipidemic Apoe−/− mice rendered neutropenic as well as Apoe−/− mice deficient in CRAMP not only displayed markedly reduced endothelial and intraplaque deposition of CRAMP but were accordingly characterized by decreased luminal adhesion of classical monocytes [83]. CRAMP-mediated adhesion of classical monocytes was found to be FPR dependent [84]. These data clearly indicate a direct link between neutrophil-derived CRAMP and monocyte recruitment in atherosclerosis.
In addition to the direct monocyte-attracting activity of neutrophil secretion products, granule proteins such as proteinase 3 can directly activate cells, e.g., endothelial cells, to secrete chemokines, thereby promoting recruitment of classical, inflammatory monocytes [74]. Proteinase 3 for example was shown to induce production of CCL2 from endothelial cells [85]. Additionally, CCL6, CCL9, CCL15 and CCL23, all of which are macrophage-derived chemokines, have been described to act as weak ligands for CCR1 [74]. Interestingly, their ability to activate CCR1 on inflammatory monocytes was shown to be increased by up to 1,000-fold following exposure to neutrophil-derived serine protease [86], thus providing an alternative mechanism of neutrophil-driven monocyte recruitment.
Yet another mechanism of neutrophil-triggered monocyte recruitment is known as IL-6 trans-signaling. In this regard, activated or apoptotic neutrophils cause the shedding of IL-6Rα; sIL-6Rα then binds to IL-6 released by macrophages and endothelial cells and via ligation of endothelial gp130 triggers upregulation of CCL2 and VCAM-1 in endothelial cells leading to increased recruitment of monocytes in conditions of acute inflammation [87, 88, 89]. The importance of this mechanism in arterial macrophage accumulation was shown in recent studies [90, 91, 92]. Therein, the authors could show that treatment with a fusion protein of the natural IL-6 trans-signaling inhibitor soluble gp130 dramatically reduced atherosclerosis in hypercholesterolemic mice without affecting serum lipid levels. In addition, VCAM-1, a downstream effector of the IL-6 trans-signaling pathway is known to be critical in arterial monocyte recruitment as mice deficient in VCAM-1 display lowered monocyte influx accompanied by reduced lesion sizes [50].
Summary
Continuous influx of classical monocytes is indispensable in the initiation and progression of atherosclerotic plaque development, and blocking recruitment may be a promising target to induce plaque regression and enhance plaque stability, also during late stages of atherosclerosis [3]. Thus, identification of molecular cues specifically guiding classical monocytes into atherosclerotic lesions is a primary interest in ongoing and future atherosclerosis research. Besides adhesion molecules being involved in the traditionally established leukocyte adhesion cascade, chemotactic molecules released from activated neutrophils and platelets may serve as promising targets for future research.
Disclosure Statement
None declared.
Acknowledgements
This study was supported by the Deutsche Forschungsgemeinschaft (SFB914 TP B08, SO876/3-1, FOR809), the German-Israeli Foundation, the Else Kröner-Fresenius Stiftung, Medical Faculty LMU Munich (FöFoLe 773) and the NWO (VIDI 91712303).
References
- 1.Weber C, Zernecke A, Libby P. The multifaceted contributions of leukocyte subsets to atherosclerosis: lessons from mouse models. Nat Rev Immunol. 2008;8:802–815. doi: 10.1038/nri2415. [DOI] [PubMed] [Google Scholar]
- 2.Swirski FK, Pittet MJ, Kircher MF, Aikawa E, Jaffer FA, Libby P, Weissleder R. Monocyte accumulation in mouse atherogenesis is progressive and proportional to extent of disease. Proc Natl Acad Sci USA. 2006;103:10340–10345. doi: 10.1073/pnas.0604260103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Potteaux S, Gautier EL, Hutchison SB, van Rooijen N, Rader DJ, Thomas MJ, Sorci-Thomas MG, Randolph GJ. Suppressed monocyte recruitment drives macrophage removal from atherosclerotic plaques of Apoe−/− mice during disease regression. J Clin Invest. 2011;121:2025–2036. doi: 10.1172/JCI43802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Landsman L, Bar-On L, Zernecke A, Kim KW, Krauthgamer R, Shagdarsuren E, Lira SA, Weissman IL, Weber C, Jung S. CX3CR1 is required for monocyte homeostasis and atherogenesis by promoting cell survival. Blood. 2009;113:963–972. doi: 10.1182/blood-2008-07-170787. [DOI] [PubMed] [Google Scholar]
- 5.Llodra J, Angeli V, Liu J, Trogan E, Fisher EA, Randolph GJ. Emigration of monocyte-derived cells from atherosclerotic lesions characterizes regressive, but not progressive, plaques. Proc Natl Acad Sci USA. 2004;101:11779–11784. doi: 10.1073/pnas.0403259101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Watanabe T, Hirata M, Yoshikawa Y, Nagafuchi Y, Toyoshima H. Role of macrophages in atherosclerosis. Sequential observations of cholesterol-induced rabbit aortic lesion by the immunoperoxidase technique using monoclonal antimacrophage antibody. Lab Invest. 1985;53:80–90. [PubMed] [Google Scholar]
- 7.Gown AM, Tsukada T, Ross R. Human atherosclerosis. 2. Immunocytochemical analysis of the cellular composition of human atherosclerotic lesions. Am J Pathol. 1986;125:191–207. [PMC free article] [PubMed] [Google Scholar]
- 8.Ylitalo R, Oksala O, Yla-Herttuala S, Ylitalo P. Effects of clodronate (dichloromethylene bisphosphonate) on the development of experimental atherosclerosis in rabbits. J Lab Clin Med. 1994;123:769–776. [PubMed] [Google Scholar]
- 9.Stoneman V, Braganza D, Figg N, Mercer J, Lang R, Goddard M, Bennett M. Monocyte/macrophage suppression in CD11b diphtheria toxin receptor transgenic mice differentially affects atherogenesis and established plaques. Circ Res. 2007;100:884–893. doi: 10.1161/01.RES.0000260802.75766.00. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Tabas I. Macrophage death and defective inflammation resolution in atherosclerosis. Nat Rev Immunol. 2010;10:36–46. doi: 10.1038/nri2675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ziegler-Heitbrock L, Ancuta P, Crowe S, Dalod M, Grau V, Hart DN, Leenen PJ, Liu YJ, MacPherson G, Randolph GJ, Scherberich J, Schmitz J, Shortman K, Sozzani S, Strobl H, Zembala M, Austyn JM, Lutz MB. Nomenclature of monocytes and dendritic cells in blood. Blood. 2010;116:e74–e80. doi: 10.1182/blood-2010-02-258558. [DOI] [PubMed] [Google Scholar]
- 12.Geissmann F, Jung S, Littman DR. Blood monocytes consist of two principal subsets with distinct migratory properties. Immunity. 2003;19:71–82. doi: 10.1016/s1074-7613(03)00174-2. [DOI] [PubMed] [Google Scholar]
- 13.Strauss-Ayali D, Conrad SM, Mosser DM. Monocyte subpopulations and their differentiation patterns during infection. J Leukoc Biol. 2007;82:244–252. doi: 10.1189/jlb.0307191. [DOI] [PubMed] [Google Scholar]
- 14.Gordon S, Taylor PR. Monocyte and macrophage heterogeneity. Nat Rev Immunol. 2005;5:953–964. doi: 10.1038/nri1733. [DOI] [PubMed] [Google Scholar]
- 15.Soehnlein O, Weber C. Myeloid cells in atherosclerosis: initiators and decision shapers. Semin Immunopathol. 2009;31:35–47. doi: 10.1007/s00281-009-0141-z. [DOI] [PubMed] [Google Scholar]
- 16.Ingersoll MA, Spanbroek R, Lottaz C, Gautier EL, Frankenberger M, Hoffmann R, Lang R, Haniffa M, Collin M, Tacke F, Habenicht A, JR, Ziegler-Heitbrock L, Randolph GJ. Comparison of gene expression profiles between human and mouse monocyte subsets. Blood. 2010;115:E10–E19. doi: 10.1182/blood-2009-07-235028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Woollard KJ, Geissmann F. Monocytes in atherosclerosis: subsets and functions. Nat Rev Cardiol. 2010;7:77–86. doi: 10.1038/nrcardio.2009.228. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Serbina NV, Jia T, Hohl TM, Pamer EG. Monocyte-mediated defense against microbial pathogens. Annu Rev Immunol. 2008;26:421–452. doi: 10.1146/annurev.immunol.26.021607.090326. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Swirski FK, Libby P, Aikawa E, Alcaide P, Luscinskas FW, Weissleder R, Pittet MJ. Ly-6Chi monocytes dominate hypercholesterolemia-associated monocytosis and give rise to macrophages in atheromata. J Clin Invest. 2007;117:195–205. doi: 10.1172/JCI29950. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Yvan-Charvet L, Pagler T, Gautier EL, Avagyan S, Siry RL, Han S, Welch CL, Wang N, Randolph GJ, Snoeck HW, Tall AR. ATP-binding cassette transporters and HDL suppress hematopoietic stem cell proliferation. Science. 2010;328:1689–1693. doi: 10.1126/science.1189731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Murphy AJ, Akhtari M, Tolani S, Pagler T, Bijl N, Kuo CL, Wang M, Sanson M, Abramowicz S, Welch C, Bochem AE, Kuivenhoven JA, Yvan-Charvet L, Tall AR. ApoE regulates hematopoietic stem cell proliferation, monocytosis, and monocyte accumulation in atherosclerotic lesions in mice. J Clin Invest. 2011;121:4138–4149. doi: 10.1172/JCI57559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Soehnlein O, Swirski FK. Hypercholesterolemia links hematopoiesis with atherosclerosis. Trends Endocrinol Metab. 2012 doi: 10.1016/j.tem.2012.10.008. DOI: 10.1016/j.tem.2012.10.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Westerterp M, Gourion-Arsiquaud S, Murphy AJ, Shih A, Cremers S, Levine RL, Tall AR, Yvan-Charvet L. Regulation of hematopoietic stem and progenitor cell mobilization by cholesterol efflux pathways. Cell Stem Cell. 2012;11:195–206. doi: 10.1016/j.stem.2012.04.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Swirski FK, Nahrendorf M, Etzrodt M, Wildgruber M, Cortez-Retamozo V, Panizzi P, Figueiredo JL, Kohler RH, Chudnovskiy A, Waterman P, Aikawa E, Mempel TR, Libby P, Weissleder R, Pittet MJ. Identification of splenic reservoir monocytes and their deployment to inflammatory sites. Science. 2009;325:612–616. doi: 10.1126/science.1175202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Robbins CS, Chudnovskiy A, Rauch PJ, Figueiredo JL, Iwamoto Y, Gorbatov R, Etzrodt M, Weber GF, Ueno T, van Rooijen N, Mulligan-Kehoe MJ, Libby P, Nahrendorf M, Pittet MJ, Weissleder R, Swirski FK. Extramedullary hematopoiesis generates Ly-6C(high) monocytes that infiltrate atherosclerotic lesions. Circulation. 2012;125:364–374. doi: 10.1161/CIRCULATIONAHA.111.061986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Leuschner F, Rauch PJ, Ueno T, Gorbatov R, Marinelli B, Lee WW, Dutta P, Wei Y, Robbins C, Iwamoto Y, Sena B, Chudnovskiy A, Panizzi P, Keliher E, Higgins JM, Libby P, Moskowitz MA, Pittet MJ, Swirski FK, Weissleder R, Nahrendorf M. Rapid monocyte kinetics in acute myocardial infarction are sustained by extramedullary monocytopoiesis. J Exp Med. 2012;209:123–137. doi: 10.1084/jem.20111009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Combadiere C, Potteaux S, Rodero M, Simon T, Pezard A, Esposito B, Merval R, Proudfoot A, Tedgui A, Mallat Z. Combined inhibition of CCL2, CX3CR1, and CCR5 abrogates Ly6C(hi) and Ly6C(lo) monocytosis and almost abolishes atherosclerosis in hypercholesterolemic mice. Circulation. 2008;117:1649–1657. doi: 10.1161/CIRCULATIONAHA.107.745091. [DOI] [PubMed] [Google Scholar]
- 28.Soehnlein O, Drechsler M, Döring Y, Lievens D, Hartwig H, Kemmerich K, Ortega-Gómez A, Mandl M, Vijayan S, Projahn D, Garlichs CD, Koenen RR, Hristov M, Lutgens E, Zernecke A, Weber C. Distinct function of chemokine receptor axes in the atherogenic mobilization and recruitment of classical monocytes. EMBO Mol Med. 2013;5:471–481. doi: 10.1002/emmm.201201717. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Jia T, Serbina NV, Brandl K, Zhong MX, Leiner IM, Charo IF, Pamer EG. Additive roles for MCP-1 and MCP-3 in CCR2-mediated recruitment of inflammatory monocytes during Listeria monocytogenes infection. J Immunol. 2008;180:6846–6853. doi: 10.4049/jimmunol.180.10.6846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Serbina NV, Pamer EG. Monocyte emigration from bone marrow during bacterial infection requires signals mediated by chemokine receptor CCR2. Nat Immunol. 2006;7:311–317. doi: 10.1038/ni1309. [DOI] [PubMed] [Google Scholar]
- 31.Berg KE, Ljungcrantz I, Andersson L, Bryngelsson C, Hedblad B, Fredrikson GN, Nilsson J, Bjorkbacka H. Elevated cd14++cd16- monocytes predict cardiovascular events. Circ Cardiovasc Genet. 2012;5:122–131. doi: 10.1161/CIRCGENETICS.111.960385. [DOI] [PubMed] [Google Scholar]
- 32.Rogacev KS, Cremers B, Zawada AM, Seiler S, Binder N, Ege P, Grosse-Dunker G, Heisel I, Hornof F, Jeken J, Rebling NM, Ulrich C, Scheller B, Bohm M, Fliser D, Heine GH. Cd14++cd16+ monocytes independently predict cardiovascular events: A cohort study of 951 patients referred for elective coronary angiography. J Am Coll Cardiol. 2012;60:1512–1520. doi: 10.1016/j.jacc.2012.07.019. [DOI] [PubMed] [Google Scholar]
- 33.Auffray C, Sieweke MH, Geissmann F. Blood monocytes: development, heterogeneity, and relationship with dendritic cells. Annu Rev Immunol. 2009;27:669–692. doi: 10.1146/annurev.immunol.021908.132557. [DOI] [PubMed] [Google Scholar]
- 34.Martinez FO, Gordon S, Locati M, Mantovani A. Transcriptional profiling of the human monocyte-to-macrophage differentiation and polarization: new molecules and patterns of gene expression. J Immunol. 2006;177:7303–7311. doi: 10.4049/jimmunol.177.10.7303. [DOI] [PubMed] [Google Scholar]
- 35.Stein M, Keshav S, Harris N, Gordon S. Interleukin 4 potently enhances murine macrophage mannose receptor activity: a marker of alternative immunologic macrophage activation. J Exp Med. 1992;176:287–292. doi: 10.1084/jem.176.1.287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Khallou-Laschet J, Varthaman A, Fornasa G, Compain C, Gas‑ton AT, Clement M, Dussiot M, Levillain O, Graff-Dubois S, Nicoletti A, Caligiuri G. Macrophage plasticity in experimental atherosclerosis. PLoS One. 2010;5:e8852. doi: 10.1371/journal.pone.0008852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Bouhlel MA, Derudas B, Rigamonti E, Dievart R, Brozek J, Haulon S, Zawadzki C, Jude B, Torpier G, Marx N, Staels B, Chinetti-Gbaguidi G. PPARgamma activation primes human monocytes into alternative M2 macrophages with anti-inflammatory properties. Cell Metab. 2007;6:137–143. doi: 10.1016/j.cmet.2007.06.010. [DOI] [PubMed] [Google Scholar]
- 38.Stoger JL, Goossens P, de Winther MP. Macrophage heterogeneity: relevance and functional implications in atherosclerosis. Curr Vasc Pharmacol. 2010;8:233–248. doi: 10.2174/157016110790886983. [DOI] [PubMed] [Google Scholar]
- 39.Wolfs IM, Donners MM, de Winther MP. Differentiation factors and cytokines in the atherosclerotic plaque micro-environment as a trigger for macrophage polarisation. Thromb Haemost. 2011;106:763–771. doi: 10.1160/TH11-05-0320. [DOI] [PubMed] [Google Scholar]
- 40.Cardilo-Reis L, Gruber S, Schreier SM, Drechsler M, Papac-Milicevic N, Weber C, Wagner O, Stangl H, Soehnlein O, Binder CJ. Interleukin-13 protects from atherosclerosis and modulates plaque composition by skewing the macrophage phenotype. EMBO Mol Med. 2012;4:1072–1086. doi: 10.1002/emmm.201201374. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Ross R. Atherosclerosis-an inflammatory disease. The New England journal of medicine. 1999;340:115–126. doi: 10.1056/NEJM199901143400207. [DOI] [PubMed] [Google Scholar]
- 42.Papaspyridonos M, Smith A, Burnand KG, Taylor P, Padayachee S, Suckling KE, James CH, Greaves DR, Patel L. Novel candidate genes in unstable areas of human atherosclerotic plaques. Arteriosclerosis, thrombosis, and vascular biology. 2006;26:1837–1844. doi: 10.1161/01.ATV.0000229695.68416.76. [DOI] [PubMed] [Google Scholar]
- 43.Stoger JL, Gijbels MJ, van der Velden S, Manca M, van der Loos CM, Biessen EA, Daemen MJ, Lutgens E, de Winther MP. Distribution of macrophage polarization markers in human atherosclerosis. Atherosclerosis. 2012;225:461–468. doi: 10.1016/j.atherosclerosis.2012.09.013. [DOI] [PubMed] [Google Scholar]
- 44.Ley K, Laudanna C, Cybulsky MI, Nourshargh S. Getting to the site of inflammation: the leukocyte adhesion cascade updated. Nat Rev Immunol. 2007;7:678–689. doi: 10.1038/nri2156. [DOI] [PubMed] [Google Scholar]
- 45.Johnson-Tidey RR, McGregor JL, Taylor PR, Poston RN. Increase in the adhesion molecule P-selectin in endothelium overlying atherosclerotic plaques. Coexpression with intercellular adhesion molecule-1. Am J Pathol. 1994;144:952–961. [PMC free article] [PubMed] [Google Scholar]
- 46.Johnson RC, Chapman SM, Dong ZM, Ordovas JM, Mayadas TN, Herz J, Hynes RO, Schaefer EJ, Wagner DD. Absence of P-selectin delays fatty streak formation in mice. J Clin Invest. 1997;99:1037–1043. doi: 10.1172/JCI119231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Collins RG, Velji R, Guevara NV, Hicks MJ, Chan L, Beaudet AL. P-selectin or intercellular adhesion molecule (ICAM)-1 deficiency substantially protects against atherosclerosis in apolipoprotein E-deficient mice. J Exp Med. 2000;191:189–194. doi: 10.1084/jem.191.1.189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.An G, Wang H, Tang R, Yago T, McDaniel JM, McGee S, Huo Y, Xia L. P-selectin glycoprotein ligand-1 is highly expressed on Ly-6Chi monocytes and a major determinant for Ly-6Chi monocyte recruitment to sites of atherosclerosis in mice. Circulation. 2008;117:3227–3237. doi: 10.1161/CIRCULATIONAHA.108.771048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Nageh MF, Sandberg ET, Marotti KR, Lin AH, Melchior EP, Bullard DC, Beaudet AL. Deficiency of inflammatory cell adhesion molecules protects against atherosclerosis in mice. Arterioscler Thromb Vasc Biol. 1997;17:1517–1520. doi: 10.1161/01.atv.17.8.1517. [DOI] [PubMed] [Google Scholar]
- 50.Cybulsky MI, Iiyama K, Li H, Zhu S, Chen M, Iiyama M, Davis V, Gutierrez-Ramos JC, Connelly PW, Milstone DS. A major role for VCAM-1, but not ICAM-1, in early atherosclerosis. J Clin Invest. 2001;107:1255–1262. doi: 10.1172/JCI11871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Patel SS, Thiagarajan R, Willerson JT, Yeh ET. Inhibition of alpha4 integrin and ICAM-1 markedly attenuate macrophage homing to atherosclerotic plaques in ApoE-deficient mice. Circulation. 1998;97:75–81. doi: 10.1161/01.cir.97.1.75. [DOI] [PubMed] [Google Scholar]
- 52.Keiper T, Al-Fakhri N, Chavakis E, Athanasopoulos AN, Isermann B, Herzog S, Saffrich R, Hersemeyer K, Bohle RM, Haendeler J, Preissner KT, Santoso S, Chavakis T. The role of junctional adhesion molecule-C (JAM-C) in oxidized LDL-mediated leukocyte recruitment. FASEB J. 2005;19:2078–2080. doi: 10.1096/fj.05-4196fje. [DOI] [PubMed] [Google Scholar]
- 53.Shagdarsuren E, Djalali-Talab Y, Aurrand-Lions M, Bidzhekov K, Liehn EA, Imhof BA, Weber C, Zernecke A. Importance of junctional adhesion molecule-C for neointimal hyperplasia and monocyte recruitment in atherosclerosis-prone mice - brief report. Arterioscler Thromb Vasc Biol. 2009;29:1161–1163. doi: 10.1161/ATVBAHA.109.187898. [DOI] [PubMed] [Google Scholar]
- 54.Ostermann G, Weber KS, Zernecke A, Schroder A, Weber C. JAM-1 is a ligand of the beta(2) integrin LFA-1 involved in transendothelial migration of leukocytes. Nat Immunol. 2002;3:151–158. doi: 10.1038/ni755. [DOI] [PubMed] [Google Scholar]
- 55.Zernecke A, Liehn EA, Fraemohs L, von Hundelshausen P, Koenen RR, Corada M, Dejana E, Weber C. Importance of junctional adhesion molecule-A for neointimal lesion formation and infiltration in atherosclerosis-prone mice. Arterioscler Thromb Vasc Biol. 2006;26:e10–e13. doi: 10.1161/01.ATV.0000197852.24529.4f. [DOI] [PubMed] [Google Scholar]
- 56.Weber C, Schober A, Zernecke A. Chemokines: Key regulators of mononuclear cell recruitment in atherosclerotic vascular disease. Arterioscler Thromb Vasc Biol. 2004;24:1997–2008. doi: 10.1161/01.ATV.0000142812.03840.6f. [DOI] [PubMed] [Google Scholar]
- 57.Zernecke A, Weber C. Chemokines in the vascular inflammatory response of atherosclerosis. Cardiovasc Res. 2010;86:192–201. doi: 10.1093/cvr/cvp391. [DOI] [PubMed] [Google Scholar]
- 58.von Hundelshausen P, Weber KS, Huo Y, Proudfoot AE, Nelson PJ, Ley K, Weber C. RANTES deposition by platelets triggers monocyte arrest on inflamed and atherosclerotic endothelium. Circulation. 2001;103:1772–1777. doi: 10.1161/01.cir.103.13.1772. [DOI] [PubMed] [Google Scholar]
- 59.Huo Y, Schober A, Forlow SB, Smith DF, Hyman MC, Jung S, Littman DR, Weber C, Ley K. Circulating activated platelets exacerbate atherosclerosis in mice deficient in apolipoprotein E. Nat Med. 2003;9:61–67. doi: 10.1038/nm810. [DOI] [PubMed] [Google Scholar]
- 60.Giagulli C, Scarpini E, Ottoboni L, Narumiya S, Butcher EC, Constantin G, Laudanna C. RhoA and zeta PKC control distinct modalities of LFA-1 activation by chemokines: critical role of LFA-1 affinity triggering in lymphocyte in vivo homing. Immunity. 2004;20:25–35. doi: 10.1016/s1074-7613(03)00350-9. [DOI] [PubMed] [Google Scholar]
- 61.Chan JR, Hyduk SJ, Cybulsky MI. Chemoattractants induce a rapid and transient upregulation of monocyte alpha4 integrin affinity for vascular cell adhesion molecule 1 which mediates arrest: an early step in the process of emigration. J Exp Med. 2001;193:1149–1158. doi: 10.1084/jem.193.10.1149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Tacke F, Alvarez D, Kaplan TJ, Jakubzick C, Spanbroek R, Llodra J, Garin A, Liu J, Mack M, van Rooijen N, Lira SA, Habenicht AJ, Randolph GJ. Monocyte subsets differentially employ CCR2, CCR5, and CX3CR1 to accumulate within atherosclerotic plaques. J Clin Invest. 2007;117:185–194. doi: 10.1172/JCI28549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Massberg S, Brand K, Gruner S, Page S, Muller E, Muller I, Bergmeier W, Richter T, Lorenz M, Konrad I, Nieswandt B, Gawaz M. A critical role of platelet adhesion in the initiation of atherosclerotic lesion formation. J Exp Med. 2002;196:887–896. doi: 10.1084/jem.20012044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Lievens D, von Hundelshausen., P Platelets in atherosclerosis. Thromb Haemost. 2011;106:827–838. doi: 10.1160/TH11-08-0592. [DOI] [PubMed] [Google Scholar]
- 65.van Gils JM, Zwaginga JJ, Hordijk PL. Molecular and functional interactions among monocytes, platelets, and endothelial cells and their relevance for cardiovascular diseases. J Leukoc Biol. 2009;85:195–204. doi: 10.1189/jlb.0708400. [DOI] [PubMed] [Google Scholar]
- 66.Totani L, Evangelista V. Platelet-leukocyte interactions in cardiovascular disease and beyond. Arterioscler Thromb Vasc Biol. 2010;30:2357–2361. doi: 10.1161/ATVBAHA.110.207480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Sarma J, Laan CA, Alam S, Jha A, Fox KA, Dransfield I. Increased platelet binding to circulating monocytes in acute coronary syndromes. Circulation. 2002;105:2166–2171. doi: 10.1161/01.cir.0000015700.27754.6f. [DOI] [PubMed] [Google Scholar]
- 68.da Costa Martins PA, van Gils JM, Mol A, Hordijk PL, Zwaginga JJ. Platelet binding to monocytes increases the adhesive properties of monocytes by up-regulating the expression and functionality of beta1 and beta2 integrins. J Leukoc Biol. 2006;79:499–507. doi: 10.1189/jlb.0605318. [DOI] [PubMed] [Google Scholar]
- 69.Schober A, Manka D, von Hundelshausen P, Huo Y, Hanrath P, Sarembock IJ, Ley K, Weber C. Deposition of platelet RANTES triggering monocyte recruitment requires P-selectin and is involved in neointima formation after arterial injury. Circulation. 2002;106:1523–1529. doi: 10.1161/01.cir.0000028590.02477.6f. [DOI] [PubMed] [Google Scholar]
- 70.Drechsler M, Megens RTA, van Zandvoort M, Weber C, Soehnlein O. Hyperlipidemia-triggered neutrophilia promotes early atherosclerosis. Circulation. 2010;122:1837–1845. doi: 10.1161/CIRCULATIONAHA.110.961714. [DOI] [PubMed] [Google Scholar]
- 71.von Hundelshausen P, Koenen RR, Sack M, Mause SF, Adriaens W, Proudfoot AEI, Hackeng TM, Weber C. Heterophilic interactions of platelet factor 4 and RANTES promote monocyte arrest on endothelium. Blood. 2005;105:924–930. doi: 10.1182/blood-2004-06-2475. [DOI] [PubMed] [Google Scholar]
- 72.Koenen RR, von Hundelshausen P, Nesmelova IV, Zernecke A, Liehn EA, Sarabi A, Kramp BK, Piccinini AM, Paludan SR, Kowalska MA, Kungl AJ, Hackeng TM, Mayo KH, Weber C. Disrupting functional interactions between platelet chemokines inhibits atherosclerosis in hyperlipidemic mice. Nat Med. 2009;15:97–103. doi: 10.1038/nm.1898. [DOI] [PubMed] [Google Scholar]
- 73.Soehnlein O, Xie X, Ulbrich H, Kenne E, Rotzius P, Flodgaard H, Eriksson EE, Lindbom L. Neutrophil-derived heparin-binding protein (HBP/CAP37) deposited on endothelium enhances monocyte arrest under flow conditions. J Immunol. 2005;174:6399–6405. doi: 10.4049/jimmunol.174.10.6399. [DOI] [PubMed] [Google Scholar]
- 74.Soehnlein O, Lindbom L. Phagocyte partnership during the onset and resolution of inflammation. Nat Rev Immunol. 2010;10:427–439. doi: 10.1038/nri2779. [DOI] [PubMed] [Google Scholar]
- 75.Lee TD, Gonzalez ML, Kumar P, Chary-Reddy S, Grammas P, Pereira HA. CAP37, a novel inflammatory mediator: its expression in endothelial cells and localization to atherosclerotic lesions. Am J Pathol. 2002;160:841–848. doi: 10.1016/S0002-9440(10)64907-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Chertov O, Ueda H, Xu LL, Tani K, Murphy WJ, Wang JM, Howard OM, Sayers TJ, Oppenheim JJ. Identification of human neutrophil-derived cathepsin G and azurocidin/CAP37 as chemoattractants for mononuclear cells and neutrophils. J Exp Med. 1997;186:739–747. doi: 10.1084/jem.186.5.739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Territo MC, Ganz T, Selsted ME, Lehrer R. Monocyte-chemotactic activity of defensins from human neutrophils. J Clin Invest. 1989;84:2017–2020. doi: 10.1172/JCI114394. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Barnathan ES, Raghunath PN, Tomaszewski JE, Ganz T, Cines DB, Higazi AAR. Immunohistochemical localization of defensin in human coronary vessels. Am J Pathol. 1997;150:1009–1020. [PMC free article] [PubMed] [Google Scholar]
- 79.Soehnlein O, Zernecke A, Eriksson EE, Rothfuchs AG, Pham CT, Herwald H, Bidzhekov K, Rottenberg ME, Weber C, Lindbom L. Neutrophil secretion products pave the way for inflammatory monocytes. Blood. 2008;112:1461–1471. doi: 10.1182/blood-2008-02-139634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Soehnlein O, Lindbom L, Weber C. Mechanisms underlying neutrophil-mediated monocyte recruitment. Blood. 2009;114:4613–4623. doi: 10.1182/blood-2009-06-221630. [DOI] [PubMed] [Google Scholar]
- 81.Sun R, Iribarren P, Zhang N, Zhou Y, Gong W, Cho EH, Lockett S, Chertov O, Bednar F, Rogers TJ, Oppenheim JJ, Wang JM. Identification of neutrophil granule protein cathepsin G as a novel chemotactic agonist for the G protein-coupled formyl peptide receptor. J Immunol. 2004;173:428–436. doi: 10.4049/jimmunol.173.1.428. [DOI] [PubMed] [Google Scholar]
- 82.Quinn KL, Henriques M, Tabuchi A, Han B, Yang H, Cheng WE, Tole S, Yu H, Luo A, Charbonney E, Tullis E, Lazarus A, Robinson LA, Ni H, Peterson BR, Kuebler WM, Slutsky AS, Zhang H. Human neutrophil peptides mediate endothelial-monocyte interaction, foam cell formation, and platelet activation. Arterioscler Thromb Vasc Biol. 2011;31:2070–2079. doi: 10.1161/ATVBAHA.111.227116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Doring Y, Drechsler M, Wantha S, Kemmerich K, Lievens D, Vijayan S, Gallo RL, Weber C, Soehnlein O. Lack of neutrophil-derived CRAMP reduces atherosclerosis in mice. Circ Res. 2012;110:1052–1056. doi: 10.1161/CIRCRESAHA.112.265868. [DOI] [PubMed] [Google Scholar]
- 84.Wantha S, Alard JE, Megens RT, van der Does AM, Döring Y, Drechsler M, Pham CT, Wang MW, Wang JM, Gallo RL, von Hundelshausen P, Lindbom L, Hackeng T, Weber C, Soehnlein O. Neutrophil-derived cathelicidin promotes adhesion of classical monocytes. Circ Res. 2013;112:792–801. doi: 10.1161/CIRCRESAHA.112.300666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Taekema-Roelvink ME, Kooten C, Kooij SV, Heemskerk E, Daha MR. Proteinase 3 enhances endothelial monocyte chemoattractant protein-1 production and induces increased adhesion of neutrophils to endothelial cells by upregulating intercellular cell adhesion molecule-1. J Am Soc Nephrol. 2001;12:932–940. doi: 10.1681/ASN.V125932. [DOI] [PubMed] [Google Scholar]
- 86.Berahovich RD, Miao Z, Wang Y, Premack B, Howard MC, Schall TJ. Proteolytic activation of alternative CCR1 ligands in inflammation. J Immunol. 2005;174:7341–7351. doi: 10.4049/jimmunol.174.11.7341. [DOI] [PubMed] [Google Scholar]
- 87.Chalaris A, Rabe B, Paliga K, Lange H, Laskay T, Fielding CA, Jones SA, Rose-John S, Scheller J. Apoptosis is a natural stimulus of IL6R shedding and contributes to the proinflammatory trans-signaling function of neutrophils. Blood. 2007;110:1748–1755. doi: 10.1182/blood-2007-01-067918. [DOI] [PubMed] [Google Scholar]
- 88.Romano M, Sironi M, Toniatti C, Polentarutti N, Fruscella P, Ghezzi P, Faggioni R, Luini W, van Hinsbergh V, Sozzani S, Bussolino F, Poli V, Ciliberto G, Mantovani A. Role of IL-6 and its soluble receptor in induction of chemokines and leukocyte recruitment. Immunity. 1997;6:315–325. doi: 10.1016/s1074-7613(00)80334-9. [DOI] [PubMed] [Google Scholar]
- 89.Hurst SM, Wilkinson TS, McLoughlin RM, Jones S, Horiuchi S, Yamamoto N, Rose-John S, Fuller GM, Topley N, Jones SA. IL-6 and its soluble receptor orchestrate a temporal switch in the pattern of leukocyte recruitment seen during acute inflammation. Immunity. 2001;14:705–714. doi: 10.1016/s1074-7613(01)00151-0. [DOI] [PubMed] [Google Scholar]
- 90.Scheller J, Rose-John S. The interleukin 6 pathway and atherosclerosis. Lancet. 2012;380:338. doi: 10.1016/S0140-6736(12)61246-X. [DOI] [PubMed] [Google Scholar]
- 91.Luchtefeld M, Schunkert H, Stoll M, Selle T, Lorier R, Grote K, Sagebiel C, Jagavelu K, Tietge UJ, Assmus U, Streetz K, Hengstenberg C, Fischer M, Mayer B, Maresso K, El Mokhtari NE, Schreiber S, Muller W, Bavendiek U, Grothusen C, Drexler H, Trautwein C, Broeckel U, Schieffer B. Signal transducer of inflammation gp130 modulates atherosclerosis in mice and man. J Exp Med. 2007;204:1935–1944. doi: 10.1084/jem.20070120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Schuett H, Oestreich R, Waetzig GH, Annema W, Luchtefeld M, Hillmer A, Bavendiek U, von Felden J, Divchev D, Kempf T, Wollert KC, Seegert D, Rose-John S, Tietge UJ, Schieffer B, Grote K. Transsignaling of interleukin-6 crucially contributes to atherosclerosis in mice. Arterioscler Thromb Vasc Biol. 2012;32:281–290. doi: 10.1161/ATVBAHA.111.229435. [DOI] [PubMed] [Google Scholar]