Abstract
Both epiploic appendagitis and femoral herniae are rare diagnoses individually. No radiological cases of a patient having epiploic appendagitis within a femoral hernia have been documented in the literature. We present a case of a 65-year-old patient who underwent clinical work-up for a tender left groin lump. When undergoing a CT scan for investigating possible lymphadenopathy, she was found to have epiploic appendagitis contained within an incarcerated left sided femoral hernia. In this case report, we review the relevant anatomy, aetiology, patient demographics, as well as clinical and imaging findings and management.
Keywords: Epiploic appendagitis, appendagitis epiploica, femoral hernia, incarcerated hernia
CASE REPORT
A 65-year-old female presented acutely to the surgical receiving unit with a short history of a tender left groin lump. She reported no nausea or vomiting, no alteration of bowel habit, weight loss or anorexia. There was no significant medical, surgical or medication history. On examination she had a tender, erythematous non-reducible mass in the left groin. Observations were stable and she was afebrile. Routine blood tests including inflammatory markers were normal. Erect chest x-ray was unremarkable with no evidence of free subdiaphragmatic gas and abdominal x-ray showed no bowel obstruction or radio-opacities.
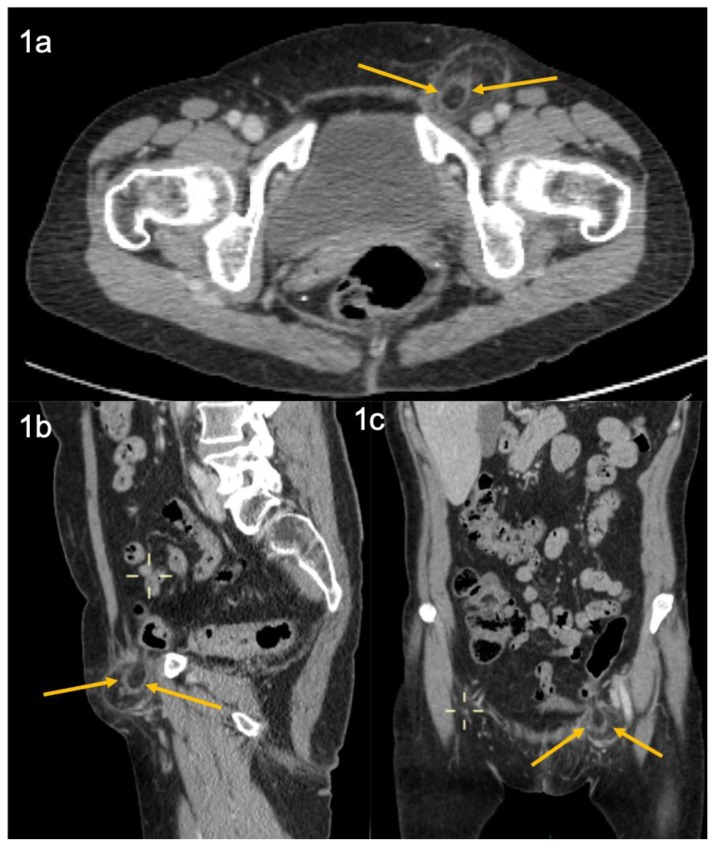
Given the concern for the possibility of lymphadenopathy, she underwent contrast enhanced CT (GE Optima CT660) of the abdomen and pelvis (Figure 1). This demonstrated a left sided incarcerated femoral hernia containing an inflamed appendix epiploica.
Figure 1.
65-year-old female with epiploic appendagitis within a left sided femoral hernia
FINDINGS: Fat density ovoid appendage surrounded by a high attenuation rim (arrows) and inflammatory stranding within a groin hernia with a ‘funnel shaped’ neck, protruding through the femoral ring, a) axial; b) sagittal; c) coronal. On the sagittal and coronal images the attachment of the fat density structure to sigmoid colon is evident with the thrombosed central vein seen as a high density line on the coronal view.
TECHNIQUE: Portal Venous phase IV contrast enhanced (100 ml Omnipaque) volume acquisition 128 detector CT (GE Optima CT660) of the abdomen and pelvis acquired at 1 mm slice thickness, 120 kVp 120, 50–200 mAs.
Operative intervention was discussed and appropriate consent obtained. The patient proceeded to the operating theatre and underwent a high suprainguinal extraperitoneal (McEvedy) procedure and the incarcerated hernial sac was reduced. The sac was opened and an infarcted appendix epiploica was excised. Wounds were closed in the standard fashion and she made an uneventful post-operative recovery.
DISCUSSION
Anatomy, Aetiology & Demographics
Both femoral hernia and epiploic appendagitis are individually relatively rare entities.
Abdominal herniae have an incidence of around 5%, with approximately 5% of these being femoral herniae [1]. These occur when there is weakness in the femoral canal and arise inferior to the inguinal ligament, protruding through the femoral ring. They lie medial to the femoral nerve and vessels, often indenting or compressing the femoral vein, and lateral to the lacunar ligament and inferior aspect of the inguinal canal [2]. Increased prevalence is noted in females and they are more commonly right sided [3]. Such a hernia can contain preperitoneal fat, omentum, peritoneum and bowel content. Very rarely they can contain an inflamed vermiform appendix (deGarengeot hernia) [4], bladder, ectopic testis or fallopian tube.
Appendices epiploica are peduncles containing fat, covered in serosa, lying on the antimesenteric border of the colon [5] attached by a vascular pedicle and arising anywhere between the caecum and rectosigmoid junction, sparing the rectum. They are most commonly located in the large bowel, particularly at the rectosigmoid junction (57%). When arising from around the sigmoid colon, they tend to be larger in size and more numerous. The appendages are distributed longitudinally in rows of two: one lateral to the tenia omentalis, and the other medial to the tenia libera [6]. Appendices epiploica are supplied by two arteries and drained by a single tortuous vein.
Epiploic appendagitis is very uncommon, with an incidence of 8.8 per million patients [7]. It predominantly occurs as a primary event due to torsion of the appendix epiploica with venous outflow obstruction and resulting ischaemia and infarction. Incarceration within a hernial sac can also result in venous obstruction [8]. Patients of any age group may be diagnosed however, the peak incidence occur in patients aged 30 to 50 years old with obesity and excessive exercise being the most common causes [7]. It can affect both genders although is slightly more prevalent in males [9].
Clinical & Imaging Findings
The clinical and CT findings of both epiploic appendagitis and femoral hernias individually are well documented.
Epiploic appendagitis typically presents with localised sharp or stabbing abdominal pain and can mimic other causes of acute abdomen. It is more frequently left sided. The patient is normally afebrile with no leucocytosis.
Appendices epiploica are only really demonstrable on CT when they are inflamed or surrounded by fluid and epiploic appendagitis is characterised by several key features on imaging. The most well-known appearance is a fat density centre adjoined to the colon with surrounding inflammatory changes. The fatty centre measures between 1.5 and 3.5 cm in the majority (86%) of patients [10] and is characteristically surrounded by a high attenuation rim [11]. Within the fatty centre there is frequently, a high density ‘dot’, which is present in around 50% of cases and not necessary for the diagnosis [10]. This occurs due to venous thrombosis.
Epiploic appendagitis has been reported in inguinal [12,13,14], incisional [8] and Spigelian [15] hernias. Occurrence within a femoral hernia is extremely unusual although there is a recently published report of such a case in a patient who proceeded directly to theatre without imaging. [16].
Femoral herniae typically present as a groin lump often tender and non-reducible and may be difficult to differentiate clinically from other groin hernias and lymphadenopathy. On cross sectional imaging they are described as having a ‘funnel shaped’ neck, protruding through the femoral ring, and sometimes compressing the common femoral vein. The coronal plane is often better at assessing the degree of common femoral vein compression and the presence of congestion of the distal veins [17].
Differential Diagnosis
Epiploic appendagitis within an inguinal hernia
The findings of epiploic appendagitis would be seen however the hernial sac is above the inguinal ligament. In an indirect inguinal hernia the sac arises lateral to the inferior epigastric vessels and often compresses the fat in the inguinal canal into a lateral crescent.
Acute appendicitis within a femoral hernia
A blind ending thickened tubular structure with attachment to the caecum representing the inflamed appendix, potentially containing an appendicolith at its base with periappendiceal fat stranding within a femoral hernial sac.
Colonic diverticulitis within a femoral hernia
Gas containing diverticulum with colonic wall thickening and pericolic fat stranding and often adjacent free fluid in a femoral hernial sac.
Treatment & Prognosis
Epiploic appendagitis alone is a self-limiting benign condition and does not generally require any surgical intervention, with effective response to non-steroidal anti-inflammatories being documented [6]. It is important to get the radiological diagnosis correct to prevent operating on a patient unnecessarily.
The management of patients with epiploic appendagitis within a femoral hernia is dependent on whether the femoral hernia is complicated or uncomplicated. If complicated by bowel obstruction or strangulation, femoral hernias are treated urgently due to their higher mortality rate, often needing bowel resection. Strangulation reportedly occurs in 22% of cases by the 3-month period therefore, patients with a new diagnosis even if asymptomatic are preferably operated on electively to minimise this risk [18].
TEACHING POINT
Epiploic appendagitis within a concomitant femoral hernia is rare but a consideration when a patient attends with a painful lump in the groin. CT appearances are diagnostic.
Table 1.
Summary table of Epiploic Appendagitis in a Femoral Hernia.
| Etiology | Torsion or venous thrombosis |
| Incidence | One previous documented case found at surgery |
| Gender ratio | Epiploic appendagitis is more common in males. Femoral herniae more common in females. |
| Age predilection | Fourth and fifth decades of life |
| Risk factors | Obesity and excessive exercise |
| Treatment | Conservative or surgical |
| Prognosis | Emergency surgical repair has higher morbidity and mortality than elective surgical repair |
| Findings on Imaging | High density ‘dot’ in a fat density centre, which is surrounded by a high attenuation rim and inflammatory changes. These changes are within a hernia with a ‘funnel shaped’ neck, protruding through the femoral ring, and sometimes compressing the common femoral vein. |
Table 2.
Differential diagnosis table of Epiploic Appendagitis in a Femoral Hernia.
| Differential Diagnoses | Computed tomography (CT) findings |
|---|---|
| Epiploic appendagitis within a femoral hernia | High density ‘dot’ in a fat density centre, which is surrounded by a high attenuation rim and inflammatory changes. These changes are within a hernia with a ‘funnel shaped’ neck, protruding through the femoral ring, and sometimes compressing the common femoral vein. |
| Epiploic appendagitis within an inguinal hernia | High density ‘dot’ in a fat density centre, which is surrounded by a high attenuation rim and inflammatory changes. These changes are within a ‘lateral crescent’ shape and extend anteromedially and inferiorly to the inferior epigastric vessels. |
| Appendicitis within a femoral hernia | Dilated, inflamed appendix with a thick and enhancing periphery as well as thickening of the caecal apex. These changes are within a right sided hernia with a ‘funnel shaped’ neck, protruding through the femoral ring, and sometimes compressing the common right femoral vein. |
| Colonic diverticulitis within a femoral hernia. | Focal areas of pericolic inflammatory stranding adjacent to bowel diverticula. These changes are within a hernia with a ‘funnel shaped’ neck, protruding through the femoral ring, and sometimes compressing the common femoral vein. |
ABBREVIATIONS
- CT
Computerised Tomography
- GE
General Electric
- NSAID
Non-Steroidal Anti Inflammatory
- IV
Intravenous
REFERENCES
- 1.Burkhardt J, Arshanskiy Y, Munson J, et al. Diagnosis of inguinal region hernias with axial CT: the lateral crescent sign and other key findings. Radiographics. 2011 Mar-Ap;31(2):1–12. doi: 10.1148/rg.312105129. [DOI] [PubMed] [Google Scholar]
- 2.Papanikitas J, Sutcliffe R, Rohatgi A, Atkinson S. Bilateral Retrovascular Femoral Hernia. Ann R Coll Surg Engl. 2008 Jul;90(5):423–424. doi: 10.1308/003588408X301235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Jamadar D, Jacobson J, Morag Y, et al. Sonography of inguinal region hernias. AJR Am J Roentgenol. 2006 Jul;187(1):185–90. doi: 10.2214/AJR.05.1813. [DOI] [PubMed] [Google Scholar]
- 4.Kalles V, Mekras A, Mekras D, et al. De Garengeot’s hernia: a comprehensive review. Hernia. 2013 Apr;17(2):177–82. doi: 10.1007/s10029-012-0993-3. [DOI] [PubMed] [Google Scholar]
- 5.Yang P, Lee Y, Chuang C. Primary Epiploic Appendagitis. West J Emerg Med. 2015 Dec;16(7):1183–4. doi: 10.5811/westjem.2015.8.27997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Singh A, Gervais D, Hahn P, et al. Acute epiploic appendagitis and its mimics. Radiographics. 2005 Nov;25(6):1521–34. doi: 10.1148/rg.256055030. [DOI] [PubMed] [Google Scholar]
- 7.de Brito P, Gomez MA, Besson M, et al. Frequency and epidemiology of primary epiploic appendagitis on CT in adults with abdominal pain. J Radiol. 2008;89:235–243. doi: 10.1016/s0221-0363(08)70399-8. [DOI] [PubMed] [Google Scholar]
- 8.Singh A, Gervais D, et al. Acute epiploic appendagitis in hernia sac: CT appearance. Emerg Radiol. 2005;11:226. doi: 10.1007/s10140-004-0391-y. [DOI] [PubMed] [Google Scholar]
- 9.Jain T, Shah T, Juneja S, Tambi R. Case of the season: primary epiploic appendagitis: radiological diagnosis can avoid surgery. Semin Roentgenol. 2008 Jan;43(1):4–6. doi: 10.1053/j.ro.2007.09.001. [DOI] [PubMed] [Google Scholar]
- 10.Singh A, Gervais D, Hahn P, et al. CT appearance of acute appendagitis. AJR Am J Roentgenol. 2004;183(5):1303–7. doi: 10.2214/ajr.183.5.1831303. [DOI] [PubMed] [Google Scholar]
- 11.Almeida A, Melão L, Viamonte B, et al. Epiploic appendagitis: an entity frequently unknown to clinicians--diagnostic imaging, pitfalls, and look-alikes. AJR Am J Roentgenol. 2009;193(5):1243–51. doi: 10.2214/AJR.08.2071. [DOI] [PubMed] [Google Scholar]
- 12.Özkurt H, Karata? O, Karaarslan E, Ba?ak M. Clinical and CT findings of epiploic appendagitis within an inguinal hernia. Diagnostic and Interventional Radiology. 2007;13(1):23–25. [PubMed] [Google Scholar]
- 13.Kulacoglu H, Tumer H, Aktimur R, Kusdemir A. Epiploic appendicitis in inguinal hernia sac presenting an inguinal mass. Hernia. 2005 Oct;9(3):288–290. doi: 10.1007/s10029-004-0306-6. [DOI] [PubMed] [Google Scholar]
- 14.Ballas K, Kontoulis T, Skouras C, et al. Unusual findings in inguinal hernia surgery: report of 6 rare cases. Hippokratia. 2009 Jul-Sep;13(3):169–171. [PMC free article] [PubMed] [Google Scholar]
- 15.Coulier B, Broze B. Epiploic appendagitis within a Spigelian hernia. Journal of the Belgian Society of Radiology. 2010;93(5):271. doi: 10.5334/jbr-btr.335. [DOI] [PubMed] [Google Scholar]
- 16.Janez J. Epiploic Appendix of the Sigmoid Colon Incarcerated in the Right Femoral Hernia Sac. J Clin Case Rep Rev. 2018;1(1):2. [Google Scholar]
- 17.Cherian P, Parnell A. The diagnosis and classification of inguinal and femoral hernia on multisection spiral CT. Clin Radiol. 2008;63(2):184–92. doi: 10.1016/j.crad.2007.07.018. [DOI] [PubMed] [Google Scholar]
- 18.Gallegos N, Dawson J, Jarvis M, Hobsley M. Risk of strangulation in groin hernias. Br J Surg. 1991 Oct;78(10):1171–1173. doi: 10.1002/bjs.1800781007. [DOI] [PubMed] [Google Scholar]