Abstract
Coexistence of Klippel-Feil syndrome with Sprengel deformity and omovertebral bone is a rare complex bone abnormality with unknown incidence and etiology. Herein, we report a case of a 6-year-old girl with coexistence of these congenital abnormalities evaluated by three-dimensional computed tomography. We also make a brief review and discuss in details the role of this imaging modality in the evaluation of such complex cases.
Keywords: Klippel-Feil syndrome, Sprengel deformity, omovertebral bone, computed tomography
CASE REPORT
A 6-year-old girl was referred for three dimensional computed tomography (3D-CT) due to shoulder asymmetry and short neck. Clinically, short neck, low posterior hairline, restricted neck mobility and high left scapula were observed. The shoulder joint was elevated by 4 cm as compared with the contralateral side. The omovertebral bone was palpable. These findings suggested a coexistence of Klippel–Feil Syndrome (KFS) with Sprengel Deformity (SD).
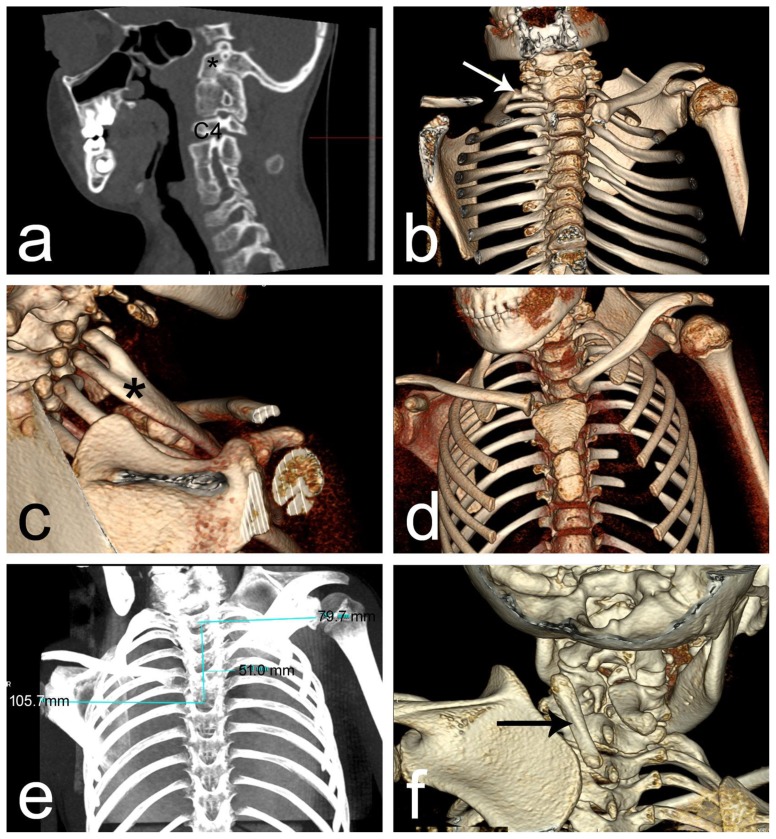
Multidetector CT of the cervical spine and thorax was performed with 320 row Aquillion One, Toshiba. Images were analyzed on dedicated Vitrea software and multiplanar and three-dimensional reconstructions were performed. In the cervical spine an atlantooccipital fusion was found together with diffuse block of vertebrae. Fusion of the vertebrae was noticed both at the level of the bodies and the arches. Only the fourth cervical vertebra was not included in the fusion at the cervical spine (Figure 1a). Incomplete fusion of the dorsal arches was found at the level of C5-C6. At the level of C5 we found a massive growth, with the characteristics of a spinous process of the vertebra, protruding to the right side. On the right side, the first two ribs were fused anteriorly (Figure 1b,c). The thorax had a slight asymmetry. In the thoracic spine the vertebral bodies were normally presented, except for a fusion of the dorsal arches at the level Th 4-Th 5 level.
Figure 1.
6-year-old girl with Klippel-Feil Syndrome with Sprengel Deformity
A: Findings: atlantooccipital fusion (asterisk) and diffuse block of vertebrae, and fusion of the vertebrae at the areas of the bodies and the arches, except forth vertebra (C4);
Technique: Computed tomography, non-contrast scan, bone window, sagittal view
B: Findings: the merged first two ribs on the right side (arrow)
Technique: Computed tomography, three-dimensional reconstruction
C: Findings: merged first two ribs on the right side (asterisk)
Technique: Computed tomography, three-dimensional reconstruction
D: Findings: higher standing left scapula and asymmetry of the two shoulder joints
Technique: Computed tomography, three-dimensional reconstruction
E: Findings: Measurement of the left scapula located 51 mm higher than the right scapula
Technique: Computed tomography, Maximum intensity projection reconstruction
F: Findings: presence of an omovertebral bone (arrow).
Technique: Computed tomography, three-dimensional reconstruction
The 3D-CT revealed a higher standing left scapula and asymmetry of the two shoulder joints (Figure 1d). The left scapula had an abnormal shape. It was located 51 mm higher than the right one, measured by the distance between the two horizontal lines drawn from the middle of the glenoid cavity of each scapula to the median line of the spine over the spinous processes of the vertebras (Figure 1e). The length of the left scapula was 81 mm and the width measured on the level of the glenoid fossa was 80 mm. Corresponding dimensions of the right scapula, were as follows: length – 97mm and width - 70 mm. The left scapula was rotated and had a prominent medial edge with a convex curve. The presence of an omovertebral bone between the superomedial border of the scapula and a course upwards along to the transverse processes of cervical spine C3 to C7 was visualized. The additional bone was 45 mm in length and 9 mm in width (Figure 1f). We did not observe any anomalies of cardiorespiratory, genitourinary, and auditory systems in the presented case.
In our case the patient was referred for simple resection of the omovertebral bone. Postoperative recovery was uneventful.
DISCUSSION
Etiology & Demographics
KFS, also known as synostosis of cervical spine is a rare condition, presented by fusion of the cervical vertebrae due to failure of normal segmentation of the cervical somites during embriological development. KFS is characterized by classical triad found in around 50% of the patients and consisting of a short neck, low posterior hairline and restricted neck mobility. This congenital syndrome, usually sporadic syndrome, affects approximately 1 in 40,000–42,000 live births. KFS is associated with other deformities as congenital high scapula and scoliosis. Cardiorespiratory, genitourinary, and auditory systems could also be impaired [1]. However, in our case such abnormalities were not diagnosed.
SD, also known as congenital high scapula, undescended scapula, or scapula elevata is a rare congenital deformity of the shoulder girdle associated with malposition and dysplasia of the scapula with muscle hypoplasia or atrophy, which causes disfigurement and limitation of movement of the shoulder [2,3].
Clinical & Imaging findings
Herein, we described a rare case of a 6-year-old girl with coexistence of KFS with SD evaluated by 3D-CT, revealing the anatomical abnormalities of this case and discussed in details the role of this imaging modality in the evaluation of such a complex cases.
In KFS, the clinical symptoms could vary from lack of symptoms to neurological complains, ranging from radiculopathy to quadriplegia and also death. The neurological complaints could be due to degenerative disc changes in the neighboring healthy cervical segments, instability of the spine and spinal stenosis [5,6]. In 65 % of patients with this syndrome the symptoms appear before the age of 30 years, while in 20 % the symptoms are present before the age of 5 [7]. In contrast, in the literature there is data of patients who are free of symptoms up to the age of 40 years [8]. In KFS, most commonly the cervical fusion is between C2-C3 vertebras (71.0 %), followed by C5-C6 (67.7 %), C6-C7 (67.6 %), and C3-C4 (29.0 %). An occipitalization of the atlas, hemivertebrae, and basilar impression can also be reported [9]. In our case 3D-CT clearly presents diffuse vertebral block between C1-3 and C5-7 presented by fusion of the bodies and the arches.
SD is commonly found at birth or later in childhood. Children with this deformity have restricted shoulder and cervical spine movements [2,3,10]. CT diagnosis is essential in the evaluation of undescended scapula. 3D-CT could present clearly the characteristics of SD, such as undescended scapula, as well as its hypoplasia, morphological characteristics, medialization and adduction, prominent upper angle, distally rotated and laterally angulated glenoid cavity, different position of the clavicle, anomalies of the vertebrae and ribs, changes of muscles around the shoulder [2,3,10]. In our study 3D-CT revealed an abnormal shape and morphology of the left scapula with a prominent medial edge with a convex curve; the width and length of the scapula were 81 and 80 mm, respectively. In the presented case we also detected an omovertebral bone. Usually, this additional bone is situated between the scapula and the cervical spine and occurs in 25–50% of cases with SD. This bone has a major role in determining the shape and position of the undescended scapula [10]. 3D CT presents in detail the omovertebral bone which, in this is case, was a trapezoid-shaped structure measuring 45 mm long and 9 mm in width.
Multidetector CT is an excellent method for the evaluation of complex bony anatomical abnormalities because of its capacity for high spatial resolution and possibility for 3D visualization. It presents clearly bony margins and visualizes anatomical structures in different planes and thus, helps in the planning of the surgical treatment. With improvements of software, CT can quickly and easily present high quality images and allows obtaining 3D reconstructions without any additional radiation exposure [4,6]. The major disadvantages of 3D-CT apart from the radiation exposure are the high costs for software and the time spend by the radiologist for 3D reconstruction [6].
Treatment & Prognosis
In SD surgery is proposed to patients with moderate to severe disability. Surgery is aimed at improving esthetical appearance and reducing functional disability. Physical therapy might improve neck mobility in KFS. Patients are advised to avoid some activities that can possibly lead to cervical injuries. In our case the patient was referred for simple resection of the omovertebral bone.
Differential diagnosis of Klippel-Feil Syndrome
a) Ankylosing spondylitis
Ankylosing spondylitis is an inflammatory spondyloarthropathy that affects the spine, sacroiliac joints, peripheral joints, and entheses and could cause conjunctivitis and uveitis. It is characteristic for early to mid-adulthood and commonly involves sacroiliac joints. CT could reveal in details the joint erosions, subchondral sclerosis, and bony ankyloses. Moreover, it is useful in patients with unremarkable imaging findings of the sacroiliac joints on plain radiography
b) Chronic discitis
The symptoms of this disease are nonspecific. The laboratory tests, such as elevated erythrocyte sedimentation rate and elevated levels of C-reactive protein could help in diagnosis. CT present the endplate involvement and bone destruction and could reveal paraspinous inflammatory changes. MRI is superior to CT and clearly present the T2 hypointensity in the vertebral bodies with loss of disc space.
c) Surgical fusion
The patient has an anamnestic and clinical history for previous spinal surgery. CT revealed presence of orthopedic implants, fusion of facet joints and spinous processes. bone graft materials and absence of anteroposterior narrowing of the vertebral bodies.
d) Juvenile idiopathic arthritis
Juvenile idiopathic arthritis is an autoimmune, noninfective, inflammatory joint disease and is the most common chronic arthritic disease in children and adolescents. It occurs in children from the ages of 1 to 6, but it may develop as late as 15 years of age. Roentgenography could reveal soft tissue swelling, osteopenia, loss of joint space, erosions, growth disturbances, atlantoaxial subluxation, odontoid erosions and ankyloses.
Differential diagnosis of Sprengel Deformity
a) Malunited and nonunited scapular fractures
The patient with malunited and nonunited scapular fractures should have a previous history of high energy trauma. CT can reveal the fracture presenting with lack of bone continuity across the fracture site and clearly distinguish the presence or absence of bone bridging in different planes.
b) Winged scapula
Winged scapula affects the ability of the person to lift heavy objects and compromise ithe daily activities. Commonly scapular winging is due to serratus anterior muscle palsy. Clinically the winged scapula is presented with pain around the shoulder, appeared spontaneously or after trauma. The patient with Winged scapula should have a motor deficiency of serratus anterior muscle confirmed by electromyography.
c) Osteomalacia
Osteomalacia is caused by impaired bone metabolism primarily due to inadequate levels of available phosphate, calcium, and vitamin D, or because of resorption of calcium. Patients with osteomalacia have laboratory detected phosphate, calcium, and vitamin D deficiency or defects in phosphate metabolism. Radiological study demonstrates osteoporotic-like pattern of the bones.
d) Rickets
This disease is presented by osteomalacia in children before fusion of the growth plate. Patients with rickets have common symptoms as bowed legs, stunted growth, bone pain, large forehead, and trouble sleeping. They present by non-mineralised osteoid resulting in growth plate widening affecting the knee, ulna and anterior rib ends.
TEACHING POINT
The complex anatomical abnormalities in Klippel-Feil Syndrome and Sprengel Deformity are easily demonstrated with multidetector CT with 3D reconstructions which could help in making the diagnosis, as well as in planning surgical treatment. Imaging reveals in most cases in details the typical abnormalities as atlantoocipital fusion, fusion of the cervical spine, together with malposition, rotation and morphology of the undescended scapula and the vertical omovertebral bone.
Table 1.
Summary table of Klippel-Feil syndrome with Sprengel deformity.
| Etiology | Unknown, sporadic, congenital |
| Incidence | (Klippel-Feil syndrome is seen in approximately 1 in 42,400 births and is associated with Sprengel’s deformity between 7%–42% of cases |
| Gender ratio | Slight male predominance (1.5:1) |
| Age predilection | Found at birth, early childhood |
| Risk factors | Not known |
| Treatment | Surgical, physical therapy |
| Prognosis | Usually good, depending on |
| Imaging findings | undescended scapula, hypoplasia of scapula, morphological characteristics of the scapula -medialization and adduction, prominent upper angle, distally rotated and laterally angulated glenoid cavity; different position of the clavicle; anomalies of the vertebrae and ribs; changes of muscles around the shoulder |
Table 2.
Differential diagnosis table for Klippel-Feil syndrome.
| Diagnosis | CT | MR imaging |
|---|---|---|
| Ankylosing spondylitis | - Joint erosions, subchondral sclerosis, bony ankyloses. - cervical spine fracture |
- Inflammatory changes |
| Complications of discitis: chronic | - Endplate involvement, bone destruction, paraspinous inflammatory changes. | - Hypointensity of the vertebral bodies in T1 with loss of disc space |
| Surgical fusion | - Absence of wasp-waist sign and fusion of facet joints and spinous processes. | -Fusion of facet joints and spinous processes |
| Juvenile idiopathic arthritis | - Osteopenia, loss of joint space, erosions, growth disturbances, atlantoaxial subluxation, odontoid erosions and ankyloses. | - Synovial hypertrophy, joint effusions, osseous and cartilaginous erosions. |
Table 3.
Differential diagnosis table for Sprengel deformity.
| Diagnosis | CT | MR imaging |
|---|---|---|
| Malunited and nonunited scapular fractures | - Lack of bone continuity across the fracture site and clearly distinguish the presence or absence of bone bridging in different planes. | - Abnormal marrow sign - Discontinuity across the fracture rim. |
| Winged scapula | - In cases of etiology of bone tumours. | - Denervation changes in the serratus anterior muscle. - Increased signal, consistent with edema, within the serratus anterior muscle. - In chronic stage muscle atrophy and fatty infiltration with increased signal in T1 images |
| Osteomalacia | - Demonstrates osteoporotic-like pattern of the bones. - Coarsened trabeculae - Insufficiency fractures - Articular manifestations - Looser’s fracture |
- Subchondral bone absorption. - Looser’s zones - Bone marrow edema - The insufficiency fractures seen as a hypointense lines or fissures on T1- and T2-weighted images |
| Rickets | - Hypodense appearance of trabeculae and cortex - Looser’s fracture (cortical and trabecular bone destructions). |
- Widening of the growth plate. - Subepiphyseal fracture. Heterogeneously increased T2 signal intensity in the marrow |
ABBREVIATIONS
- CT
Computed tomography
- KFS
Klippel-Feil Syndrome
- SD
Sprengel deformity
REFERENCES
- 1.Stelzer JW, Flores MA, Mohammad W, Esplin N, Mayl JJ, Wasyliw C. Klippel-Feil syndrome with Sprengel deformity and extensive upper extremity deformity: a case report and literature review. Case Rep Orthop. Jan 18;2018 doi: 10.1155/2018/5796730. 5796730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bindoudi A, Kariki EP, Vasiliadis K, Tsitouridis I. The rare sprengel deformity: our experience with three cases. J Clin Imaging Sci. Oct 27;4:55. doi: 10.4103/2156-7514.143407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Kadavkolan AS, Bhatia DN, Dasgupta B, Bhosale PB. Sprengel’s deformity of the shoulder: Current perspectives in management. Int J Shoulder Surg. 2011 Jan;5(1):1–8. doi: 10.4103/0973-6042.80459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Laker SR, Concannon LG. Radiologic evaluation of the neck: a review of radiography, ultrasonography, computed tomography, magnetic resonance imaging, and other imaging modalities for neck pain. Phys Med Rehabil Clin N Am. 2011 Aug;22(3):411–28. doi: 10.1016/j.pmr.2011.03.010. [DOI] [PubMed] [Google Scholar]
- 5.Mears DC. Partial resection of the scapula and a release of the long head of triceps for the management of Sprengel’s deformity. J Pediatr Orthop. 2001 Mar-Apr;21(2):242–5. [PubMed] [Google Scholar]
- 6.Yuksel M, Karabiber H, Yuksel KZ, Parmaksiz G. Diagnostic importance of 3D CT images in Klippel-Feil Syndrome with multiple skeletal anomalies: a case report. Korean J Radiol. 2005 Oct-Dec;6(4):278–81. doi: 10.3348/kjr.2005.6.4.278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gray SW, Romaine CB, Skandalakis JE. Congenital Fusion of the Cervical Vertebrae. Surg Gynecol Obstet. 1964 Feb;118:373–85. [PubMed] [Google Scholar]
- 8.Nagashima H, Morio Y, Teshima R. No neurological involvement for more than 40 years in Klippel-Feil syndrome with severe hypermobility of the upper cervical spine. Arch Orthop Trauma Surg. 2001;121(1–2):99–101. doi: 10.1007/s004020000164. [DOI] [PubMed] [Google Scholar]
- 9.Samartzis DD, Herman J, Lubicky JP, Shen FH. Classification of congenitally fused cervical patterns in Klippel-Feil patients: epidemiology and role in the development of cervical spine-related symptoms. Spine (Phila Pa 1976) 2006 Oct 1;31(21):E798–804. doi: 10.1097/01.brs.0000239222.36505.46. [DOI] [PubMed] [Google Scholar]
- 10.Fullbier L, Tanner P, Henkes H, Hopf NJ. Omovertebral bone associated with Sprengel deformity and Klippel-Feil syndrome leading to cervical myelopathy. J Neurosurg Spine. 2010 Aug;13(2):224–8. doi: 10.3171/2010.3.SPINE09665. [DOI] [PubMed] [Google Scholar]