Abstract
A 78-year-old female presented with dislocation of a dual mobility hip prosthesis. On standard radiographs after closed reduction, the hip prosthesis appeared to be properly reduced, but clinically the hip was unstable. A Computed Tomography showed a round foreign body, that was in fact a dislocation of the intra-prosthetic implant. This was confirmed intra-operatively during revision surgery. Intra-prosthetic dislocation is a specific complication of dual mobility system. Classically, it’s a late complication, linked to the wear of retention area of the polyethylene insert. In this case report we describe an unusual reason of intra-prosthetic dislocation caused by a reduction maneuver of a dislocated dual mobility total hip prosthesis, which to our knowledge has never been documented with Computed Tomography imagery and intra operative pictures. The aim of this article is to analyse the advantages and complications of this implant and to establish recommendations. Dealing with an intra-prosthetic dislocation of a dual mobility hip prosthesis, we recommend attempting a reduction under general anesthesia to avoid mechanical complications. In case of persistent instability after reduction, we recommend performing a Computed Tomography scan.
Keywords: hip, instability, dislocation, dual mobility, intra-prosthetic dislocation
CASE REPORT
A 78-year-old female with a left total hip arthroplasty (cemented stem and press-fit cup), performed 6 years earlier, was admitted to our emergency room following a fall on her left hip. The radio-clinical evaluation revealed a transverse peri-prosthetic fracture of the left acetabulum, for which open reduction and osteosynthesis was performed through a posterior approach (Figure 1,2). During the surgery, the acetabular implant was revised by the implantation of a Ganz reinforcement ring fixed by 2 screws and a strapping, as well as a double mobility cup (head 28 mm) cemented in this ring (Figure 3,4).
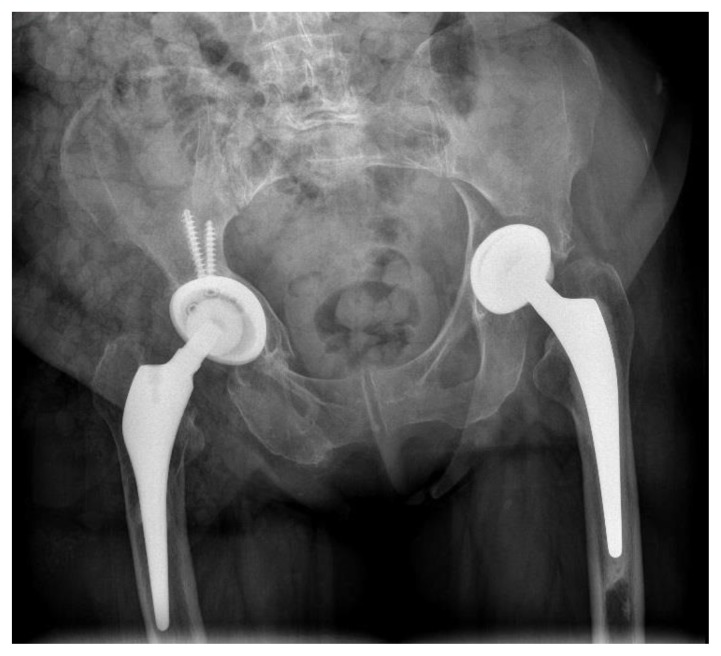
Figure 1.
78-year-old female showing a transverse peri-prosthetic fracture of the left acetabulum.
Technique: plain anteroposterior pelvis radiograph.
Findings: a transverse peri-prosthetic fracture of the left acetabulum. The cup of the left hip prosthesis implant is pushed in the acetabulum. Right hip prosthesis implant properly positioned.
Figure 2.
78-year-old female showing a transverse peri-prosthetic fracture of the left acetabulum.
Technique: plain axial hip radiograph.
Findings: a transverse peri-prosthetic fracture of the left acetabulum. The cup of the left hip prosthesis implant is pushed and turned in the acetabulum.
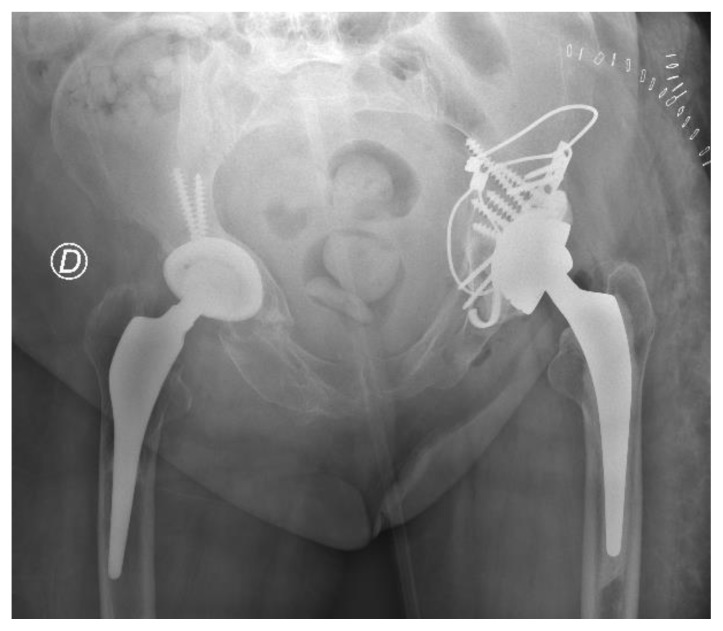
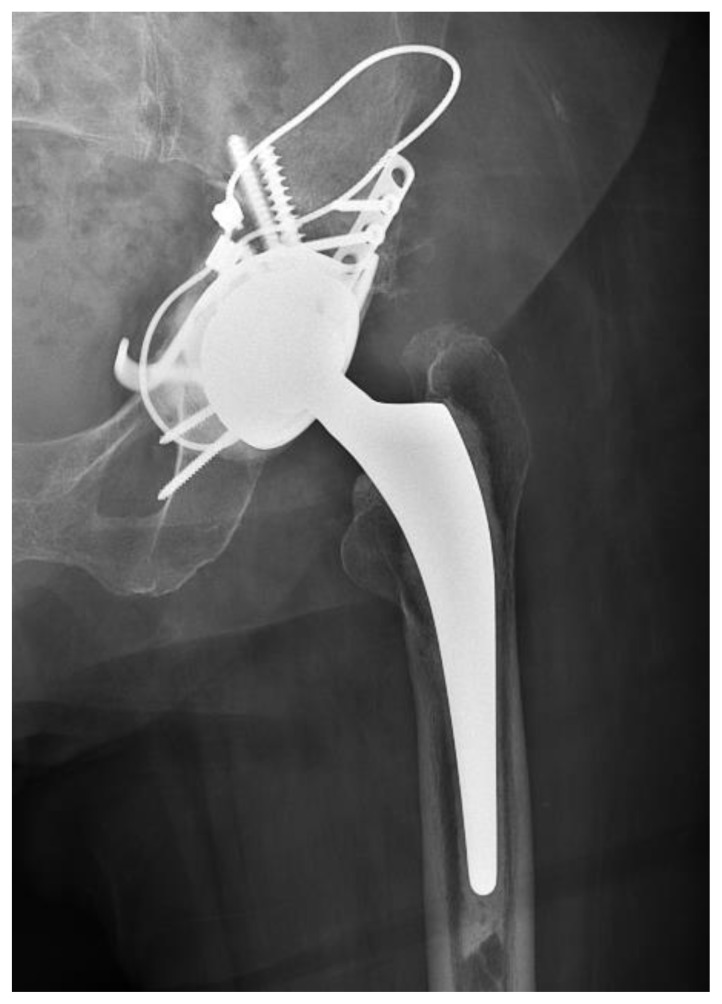
Figure 3.
78-year-old female showing revision surgery on left hip prosthesis.
Technique: plain anteroposterior pelvis radiograph.
Findings: left revision surgery with osteosynthesis of the acetabulum with cerclage, plate, screws and Ganz revision ring, with cemented hip stem and dual mobility cup. Right hip prosthesis implant properly positioned.
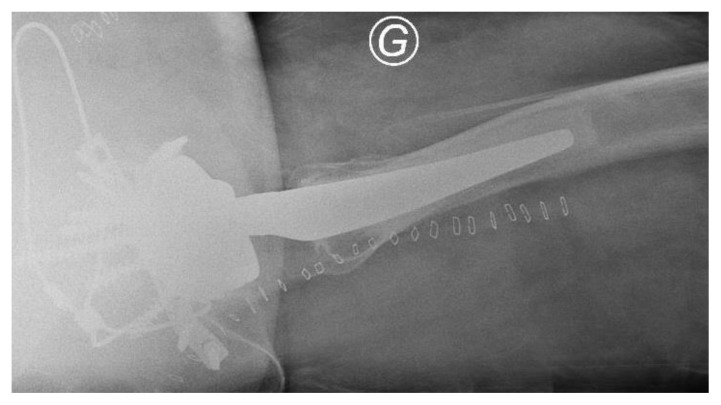
Figure 4.
78-year-old female showing revision surgery on left hip prosthesis.
Technique: plain axial hip radiograph.
Findings: left revision surgery with osteosynthesis of the acetabulum with cerclage, plate, screws and Ganz revision ring, with cemented hip stem and dual mobility cup.
The patient presented a first dislocation of her left hip six days after surgery (Figure 5,6), followed by another episode suggesting a new dislocation 48 hours later. After each closed reduction attempt, the hip appeared clinically unstable. Standard AP x-rays after reduction were nevertheless considered satisfactory with a head appearing centered in the cup (Figure 7). A pelvis CT was thereby performed to investigate the clinical sensation of instability. The CT showed a foreign body corresponding to the mobile polyethylene insert in the gluteal muscle mass and the metal head was in direct contact with the metal cup (Figure 8, 9, 10), which corresponds to an intra-prosthetic dislocation (IPD). A revision was decided which confirmed the presence of the mobile polyethylene in the gluteal muscle masses intraoperatively (Figure 11).
Figure 5.
78-year-old female showing dislocation of the left hip prosthesis.
Technique: plain anteroposterior pelvis radiograph.
Findings: a dislocation of the left hip prosthesis with dual mobility cup. Left revision surgery with osteosynthesis of the acetabulum with cerclage, plate, screws, Ganz revision ring with dual mobility cup, and cemented hip stem. Right hip prosthesis implant properly positioned.
Figure 6.
78-year-old female showing dislocation of the left hip prosthesis.
Technique: plain axial hip radiograph.
Findings: a dislocation of the left hip prosthesis with dual mobility cup. Hip prosthesis is posteriorly positioned. Left revision surgery with osteosynthesis of the acetabulum with cerclage, plate, screws, Ganz revision ring with dual mobility cup, and cemented hip stem.
Figure 7.
78-year-old female after closed reduction on left hip prosthesis.
Technique: plain anteroposterior hip radiograph.
Findings: left hip prosthesis that seems in good place after closed reduction.
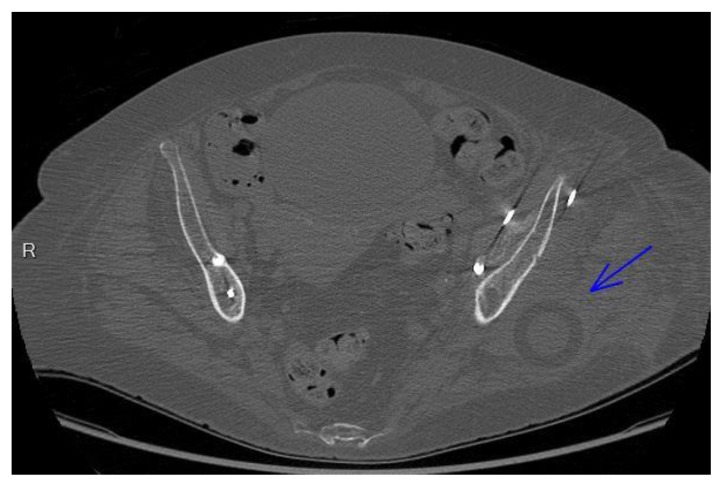
Figure 8.
78-year-old female with intra-prosthetic dislocation.
Findings: this picture shows a foreign body which is the mobile polyethylene insert (blue arrow) in the gluteal muscle mass corresponding to posteriorly dislocated prosthetic implant on axial view
Technique: Computed Tomography on axial view (Toshiba Aquilion 64) without contrast, 150 mA, 120 kV, 2.00 mm slice thickness, Matrix 512*512, FOV 300, artefact reduction
Figure 9.
78-year-old female with intra-prosthetic dislocation.
Findings: this picture shows a foreign body which is the mobile polyethylene insert (blue arrow) in the gluteal muscle mass corresponding to posteriorly dislocated prosthetic implant on sagittal view
Technique: Computed Tomography on sagittal view (Toshiba Aquilion 64) ) without contrast, 150 mA, 120 kV, 2.00 mm slice thickness, Matrix 512*512, FOV 300, artefact reduction
Figure 10.
78-year-old female with intra-prosthetic dislocation.
Findings: this picture shows a foreign body which is the mobile polyethylene insert (blue arrow) in the gluteal muscle mass corresponding to posteriorly dislocated prosthetic implant on coronal view
Technique: Computed Tomography on coronal view (Toshiba Aquilion 64) without contrast, 150 mA, 120 kV, 2.00 mm slice thickness, Matrix 512*512, FOV 300, artefact reduction
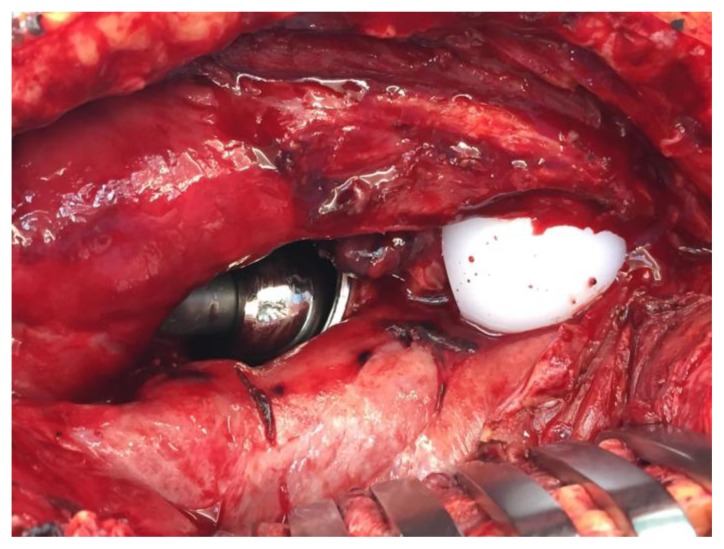
Figure 11.
78-year-old female during revision surgery for intra-prosthetic dislocation.
Findings: this picture shows an intra-prosthetic dislocation. The white part (on the right) is the polyethylene head stuck in the gluteus maximus. On the left we see the metal head articulating directly in the cup.
The surgical revision involved changing and reorienting the acetabular component with a new dual mobility cup (Figure 12, 13). The 3-year follow-up was satisfactory with resumption of the walk in complete load without technical assistance, without new episode of dislocation and with a Harris score of 82 out of 100.
Figure 12.
78-year-old female after revision surgery for intra-prosthetic dislocation.
Technique: plain anteroposterior hip radiograph.
Findings: post-operative picture showing implant in good place with revision cup implant of the hip prosthesis with reorientation of a new acetabular cup with good outcome.
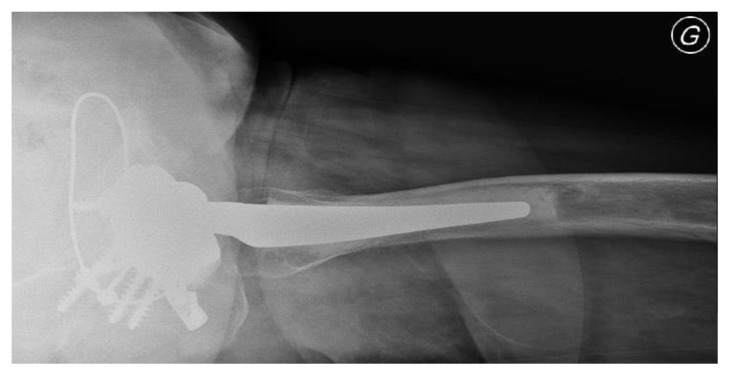
Figure 13.
78-year-old female after revision surgery for intra-prosthetic dislocation.
Technique: plain axial hip radiograph.
Findings: post-operative picture showing implant in good place with revision cup implant of the hip prosthesis with reorientation of a new acetabular cup with good outcome.
DISCUSSION
Etiology & Demographics
Dislocation is known to be one of the complications after total hip replacement (THA). The rates found in the literature are ranging from 0.2% to 7% after total primary hip replacement and up to more than 10% after revision arthroplasty [1–3]. The placement of a dual mobility hip prosthesis is an effective option for preventing or treating instability [4,5]. Classical indications for dual mobility implant are revision surgery, neuromuscular defect, obesity and alcoholism [4,5].
The concept of dual mobility consists of the interposition of a mobile polyethylene insert between the prosthetic head and the external metal cup (Figure 14) in order to increase the effective diameter of the prosthetic head. In comparison, in standard hip prosthesis, the polyethylene insert is fixed in the metal cup. Dislocation is still possible between the mobile insert and the metal cup, especially in case of abductor deficiency [4,5]. During a dislocation of dual mobility prosthesis, an attempt to reduce the dislocation by external maneuver is justified. The large volume of the insert can make this maneuver difficult and justifies a reduction under anesthesia.
Figure 14.
(A) The various components of dual mobility implant (from left to right: stem - head - mobile polyethylene insert- cup)
(B) The implant assembled.
A specific complication of dual mobility implants is the IPD [6–8]. The metal head comes out of the polyethylene head due to the wear of the retention cavity. The head is then housed in the metal cup, which is a late and rare complication. Literature series have reported long-term dislocations rates of 2% to 3% over 15 years with the first generations of dual mobility implants [4,9]. With modern dual mobility implants, IPD is significantly lower with rates of 0% over 7 years follow-up [6] and of 0.3% over 10 years [7]. Several causal mechanisms of wear of the components leading to an IPD have been described by Philippot [10]: the first is wear of dual mobility whose function is normal; another mechanism is wear associated with acetabular loosening, and finally the wear of dual mobility was associated with the blocking of the second joint.
Clinical & Imaging findings
The aim of this article is to demonstrate that IPD can also occur in other circumstances, especially during a reduction episode of closed hip prosthesis. In fact, it can occur as a “bottle opener” effect related to the reduction maneuver by forcing the mobile polyethylene insert “hooked” on the rim of the cup. De Martino and al described in a systematic review that 15 cases of early IPD are mentioned in the literature [11]. None of these cases described this type of dislocation with radiological images, CT scan and intraoperative images.
When an IPD occurs, the diagnosis can be clinically or even radiologically difficult to make. Typically, there is radiological eccentricity of the head in the cup, with direct contact between the two pieces. In our situation, this eccentricity did not appear obvious on post-reduction radiography. Additionally, the clinical diagnosis is made difficult by the fact that the patient is able to walk with direct support of the head into the cup, which can cause damage to the articular surface of the cup. In this present case, the articulation of the head in the metal cup left a sensation of instability while mobilizing the hip. This sensation justified the realization of a CT to investigate the situation. The diagnosis of IPD was made using the CT. In such a situation, revision surgery is necessary, and it is recommended to change the metal cup in case of damage of the articular surface.
Treatment & Prognosis
In case of dislocation of a dual mobility hip implant, as for a standard THA, we recommend attempting a reduction with anesthesia to prevent the risk of mechanical complication during the external maneuver. In addition, we recommend performing a CT if there is any doubt of a persistent sensation of instability after reduction.
If IPD occurs on dual mobility hip prosthesis, the system of dual mobility has failed and the only one treatment is revision surgery with replacement of the dual mobility cup. With this treatment, the prognosis is good with resolution of the problem.
Differential Diagnoses
Hip Prosthetic dislocation (with standard implant)
Clinically, there isn’t any difference with IPD (with dual mobility implant and with standard implant), which makes the diagnosis difficult.
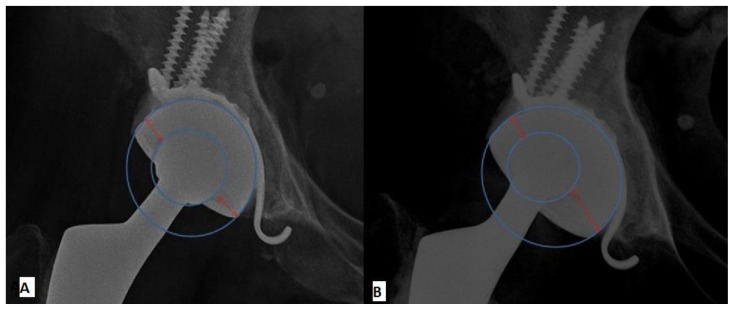
On X-ray, after reduction maneuver, the head is in the center of acetabulum. At the opposite, with IPD after reduction maneuver, there is radiological eccentricity of the head in the cup, with direct contact between the two pieces (Figure 15).
Figure 15.
(A) The various components of dual mobility implant on x-ray in good place. The head is in good place, on the center of the cup
(B) Dual mobility implant on x-ray with intra-prosthetic dislocation after reduction maneuver, there is radiological eccentricity of the head in the cup, with direct contact between the two pieces because mobile polyethylene insert hooked on the rim of the cup.
On CT, after reduction maneuver, the head of the implant is on the center of acetabulum and there is no mobile insert in the gluteal muscle. With IPD after reduction maneuver the CT can show a foreign body corresponding to the mobile insert in the gluteal muscle corresponding to an IPD with a direct contact of the head in the metal cup.
TEACHING POINT
Intra-prosthetic dislocation can happen during a reduction maneuver of a dislocated dual mobility implant. This is an unusual complication, which must be thought of in case of persistent sensation of instability after reduction, and whose diagnosis can be made by performing a computed tomography. Anesthesia is recommended during total hip arthroplasty reduction maneuvers (standard, but also with dual mobility) in order to limit the risk of mechanical complication but remains nevertheless possible.
Table 1.
Summary table of key aspects of Intra-prosthetic hip dislocation.
| Etiology | Intra-prosthetic dislocation is a specific complication of dual mobility hip implants. The head comes out of the polyethylene by wear of the retention cavity or by a reduction maneuver |
| Incidence | 0.3% over 10 years |
| Gender ratio | No determinant |
| Age predilection | Unknown |
| Risk factor |
|
| Treatment | Revision surgery with replacement of the dual mobility cup |
| Prognosis | Resolution of the problem after revision surgery |
| Findings on imaging | A computed tomography can be made to investigate the clinical sensation of instability. The computed tomography can demonstrate an intra-prosthetic dislocation with a direct contact of the head in the metal cup, with the polyethylene insert dislocated. |
Table 2.
Differential diagnosis table for intra-prosthetic dislocation.
| Entity | X-Ray | Computed tomography |
|---|---|---|
| Intra-prosthetic dislocation (with dual mobility implant) | Typically, after reduction maneuver, there is radiological eccentricity of the head in the cup, with direct contact between head and cup. | Computed tomography can show the mobile insert (normally between the head and cup) in the gluteal muscle corresponding to an intra-prosthetic dislocation with a direct contact of the head in the metal cup. |
| Hip Prosthetic dislocation (with standard implant) | After reduction maneuver, the head appears in the center of the cup. | After reduction maneuver, the head of the implant is in the center of the cup. There is no mobile insert in the gluteal muscle. |
ABBREVIATIONS
- CT
Computed Tomography
- IPD
Intra-Prosthetic Dislocation
- THA
Total Hip Arthroplasty
REFERENCES
- 1.Patel PD, Potts A, Froimson MI. The dislocating hip arthroplasty: prevention and treatment. J Arthroplasty. 2007 Jun;22:86–90. doi: 10.1016/j.arth.2006.12.111. [DOI] [PubMed] [Google Scholar]
- 2.Malchau H, Herberts P, Ahnfelt L. Prognosis of total hip replacement in Sweden. Follow-up of 92,675 operations performed 1978–1990. Acta Orthop Scand. 1993 Oct;64(5):497–506. doi: 10.3109/17453679308993679. [DOI] [PubMed] [Google Scholar]
- 3.Joshi A, Lee CM, Markovic L, Vlatis G, Murphy J. Prognosis of dislocation after total hip arthroplasty. J Arthroplasty. 1998;13:17–21. doi: 10.1016/s0883-5403(98)90070-5. [DOI] [PubMed] [Google Scholar]
- 4.Philippot R, Camilleri JP, Boyer B, Adam P, Farizon F. The use of a dual-articulation acetabular cup system to prevent dislocation after primary total hip arthroplasty: analysis of 384 cases at a mean follow-up of 15 years. Int Orthop. 2009;3(4):927–932. doi: 10.1007/s00264-008-0589-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Leclercq S, el Blidi S, Aubriot JH. Bousquet’s device in the treatment of recurrent dislocation of a total hip prosthesis. A propos of 13cases. Rev Chir Orthop Reparatrice Appar Mot. 1995;81(3):89–94. [PubMed] [Google Scholar]
- 6.Vermersch T, Viste A, Desmarchelier R, Fessy MH. Prospective longitudinal study of one hundred patients with total hip arthroplasty using a second-generation cementless dual-mobility cup. Int Orthop. 2015 Nov;39(11):2097–2101. doi: 10.1007/s00264-015-2985-2. [DOI] [PubMed] [Google Scholar]
- 7.Boyer B, Neri T, Geringer J, Philippot R, Farizon F. La luxation intra-prothétique - fossile de l’historique de la double mobilité ? Réponse des explants. Orthop Traumatol Surg Res. 2015;101(Suppl 7):S186–187. [Google Scholar]
- 8.Lecuire F, Benareau I, Rubini J, Basso M. [Intra-prosthetic dislocation of the Bousquet dual mobility socket [in French]]. Rev Chir Orthop Reparatrice Appar Mot. 2004 May;90:249–255. doi: 10.1016/s0035-1040(04)70101-4. [DOI] [PubMed] [Google Scholar]
- 9.Philippot R, Farizon F, Camilleri JP, Boyer B, Derhi G, Bonnan J, Fessy MH, Lecuire F. Survival of dual mobility socket with a mean 17 years follow-up [in French] Rev Chir Orthop Reparatrice Appar Mot. 2008;94:43–48. doi: 10.1016/j.rco.2007.10.011. [DOI] [PubMed] [Google Scholar]
- 10.Philippot R, Bertrand B, Farizon F. Intraprosthetic Dislocation: A specific complication of the dual-mobility system. Clinical Orthopaedic Related, Research. 2013;471:965–970. doi: 10.1007/s11999-012-2639-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.De Martino I, D’Apolito R, Waddell BS, McLawhorn AS, Sculco PK, Sculco TP. Early intraprosthetic dislocation in dual-mobility implants: a systematic review. Arthroplast Today. 2017;3(3):197–202. doi: 10.1016/j.artd.2016.12.002. [DOI] [PMC free article] [PubMed] [Google Scholar]