Abstract
Subperiosteal hematoma of the orbit is an uncommon radiologic finding. Most typically, the hemorrhage is in the superior aspect of the orbit, however, location within the orbit may vary. Subperiosteal hematoma of the orbit may be associated with trauma. Nontraumatic etiology has also been well documented. We present a series of three cases, to illustrate typical and atypical radiologic findings of subperiosteal hematoma of the orbit, both traumatic and nontraumatic. Review of the pertinent radiologic literature and its relation to the cases presented here is also provided.
Keywords: Subperiosteal, orbital, hematoma, traumatic, nontraumatic
CASE SERIES
Case 1
A 45-year-old male complained of sharp pain above his right eye and periorbital swelling, which had begun after a bout of prolonged vomiting and retching. The patient had a history of hepatitis C with cirrhosis. Due to ongoing polysubstance abuse, the patient was currently admitted in the inpatient rehabilitation program at the time of onset of these symptoms. The patient denied any trauma to the eye. On physical examination, there was no loss of vision. There was mild right proptosis and periorbital swelling.
Noncontrast CT imaging demonstrated an extraconal mass, slightly hyperdense to the extraocular muscles (average 76 HU, maximum 94 HU), in the right superior orbit, consistent with a subperiosteal hematoma (Figure 1A). There was mild downward displacement of the right superior muscle complex (Figures 1B, 1C) and right ocular globe. There was no associated fracture or osseous defect of the orbital roof (figure 1D). The patient was managed conservatively for several days while in the rehabilitation program, but subsequently lost to follow-up.
Figure 1.
50-year-old male with nontraumatic subperiosteal orbital hematoma.
Findings: (A) Coronal soft tissue CT image at mid-globe level shows an extraconal mass, slightly hyperdense to the extraocular muscles, in the right superior orbit (arrow), consistent with a subperiosteal hematoma. Region of interest measurement gave an average 76 HU, maximum 94 HU of the hematoma. The hematoma measures approximately 2.3 × 0.6 × 2.9 cm in transverse, craniocaudad and AP dimensions respectively (also see sagittal view in panel C). There is mild downward displacement of the globe. (B) Coronal soft tissue CT image posterior to the globe shows the mass (arrow) inferiorly displacing the superior muscle complex (arrowhead). (C) Sagittal soft tissue CT image shows the hematoma (arrow) inferiorly displacing the superior muscle complex (arrowhead). (D) Sagittal image with bone algorithm shows that the right orbital roof is intact (arrow).
Technique: Coronal and sagittal noncontrast CT, 180 mAs, 120 kV, 2 mm slice thickness
Case 2
A 5-year-old male with a history of hemoglobin SS, and no past ocular history, presented with bilateral periorbital swelling and bilateral eye pain. These orbital symptoms were preceded by abdominal and leg pain typical of previous vaso-occlusive crises. At presentation, the patient was febrile at 40.2C. Abduction of the right eye, as well as up and down gaze bilaterally, were limited. However, fundoscopy was normal.
On contrast enhanced CT, there were bilateral heterogeneous density extraconal masses in the superolateral aspects of the orbits, consistent with subperiosteal hematomas (Figures 2A, 2C). The hematomas were slightly hypodense compared to the enhancing extraocular muscles (average 38 HU, maximum 58 HU), and inferiorly displacing the lacrimal glands. There was also bilateral fullness of the periorbital soft tissues. No osseous abnormality was visible on the CT images (Figure 2B). MRI was ordered to further assess for bone infarction, inflammation of the orbital soft tissues, and possible intracranial complications. The hematomas were isointense to muscle, with thin curvilinear peripheral enhancement (Figures 3A, 3B). MRI also showed abnormal fullness with T2 signal hyperintensity and enhancement of the preseptal soft tissues and temporalis muscles, left more than right (Figures 3B, 3C, 3D). Abnormal signal in the sphenotemporal buttresses, right more than left, was consistent with bone infarcts (Figures 3C, 3D).
Figure 2.
5-year-old male with sickle cell disease, with bilateral subperiosteal orbital hematomas
Findings: (A) Axial soft tissue algorithm contrast enhanced CT image of the head at the level of the orbits shows bilateral extraconal intermediate density masses (black arrows), consistent with subperiosteal hematomas. There is abnormal fullness of the preseptal soft tissues (arrowheads) and temporalis muscles (white arrows), left more than right. The bilateral hematomas measure approximately 2.0 × 2.2 × 2.9 cm in the transverse, craniocaudad and AP dimensions respectively (also see coronal view in panel C). (B) Axial bone algorithm CT image of the head shows a normal appearance of the bilateral sphenotemporal buttresses (arrows). (C) Coronal soft tissue algorithm contrast enhanced CT image of the head at the level of the orbits, just posterior to the ocular globes, shows the hematomas (arrows) inferiorly displacing the lacrimal glands (arrowheads).
Technique: Axial and coronal post contrast CT, 120 mAs, 120 kV, 3 mm slice thickness. Contrast agent: 20 mL Omnipaque 350
Figure 3.
5-year-old male with sickle cell disease, with bilateral subperiosteal orbital hematomas
Findings: (A) Coronal noncontrast T1W image of the orbits shows bilateral extraconal masses (arrows) isointense to skeletal muscle, corresponding to the hematomas shown in figure 2. (B) Axial postcontrast T1W image shows curvilinear peripheral enhancement of the hematomas (asterices). There is abnormal hypointense signal of the sphenotemporal buttresses, more homogeneous on the right (arrows). There is abnormal fullness of the preseptal soft tissues and temporalis muscles (arrowheads). There is marked bilateral proptosis. (C) Axial T2W image at the same level as panel B shows bilateral hematocrit levels in the hematomas (arrows). There is abnormal heterogeneous signal of the sphenotemporal buttresses (arrowheads). (D) Coronal fat saturated T2-weighted image shows abnormal signal consistent with edema in the right sphenotemporal buttress (arrow). There is also fullness and edema of the temporalis muscles (arrowheads).
Technique: 1.5T magnet, Spin Echo precontrast coronal T1-weighted sequence (TR 450 ms, TE 12 ms). Spin Echo post contrast axial T1-weighted sequence (TR 581 ms, TE 12 ms), gadobutrol 3 mL. Spin Echo axial T2-weighted sequence (TR 4360 ms, TE 122 ms). Fat-saturated Spin Echo T2-weighted sequence (TR 4820 ms, TE 126 ms, TI 166 ms).
The patient had resolution of symptoms with conservative management, but returned to the hospital 10 months later with another vaso-occlusive crisis, and underwent MR imaging to evaluate for a possible cerebral infarct. The MR images showed resolution of the previous bilateral subperiosteal orbital hematomas and near resolution of abnormal marrow signal in the lateral orbital walls (Figures 4A, 4B).
Figure 4.
5-year-old male with sickle cell disease, with resolution of subperiosteal orbital hematomas.
Findings: (A) Coronal T1W image acquired 10 months after the images in figures 2 and 3, showing resolution of the previously demonstrated hematomas in the bilateral orbits (white arrows). (B) Axial T2W image from the follow-up examination again shows normal fat planes in the lateral aspects of the bilateral orbits (white arrows). There is also near resolution of the previously seen abnormal signal in the sphenotemporal buttresses (black arrows).
Technique: 1.5T magnet, Spin Echo precontrast coronal T1-weighted sequence (TR 450 ms, TE 12 ms. Spin Echo axial T2-weighted sequence (TR 4360 ms, TE 122 ms)
Case 3
A 76-year-old male with a past medical history of hypertension fell while getting up from a chair. There was no loss of consciousness. Subsequently, the patient had a seizure in the emergency department. On physical examination, there was no visual field deficit or extraocular motor dysfunction. There were bilateral periorbital hematomas.
CT imaging demonstrated a lateral extraconal mass in the left orbit, hyperdense to muscle (average 46 HU, maximum 70 HU), displacing the lateral rectus muscle and causing proptosis, consistent with a subperiosteal hematoma (Figures 5A, 5B). This finding was not present on a prior head CT from approximately one year earlier (Figure 6A). There were additional findings consistent with acute trauma, including a hemorrhagic contusion in the right inferior frontal lobe and a right anterior scalp hematoma (Figures 5B, 5C), suggesting that the left orbital subperiosteal hematoma may have represented a contrecoup injury. There was hyperdense opacification of the right maxillary sinus, suspicious for an nondisplaced fracture (Figure 5B). However, the left lateral orbital wall and sphenotemporal buttress were intact (Figure 5D).
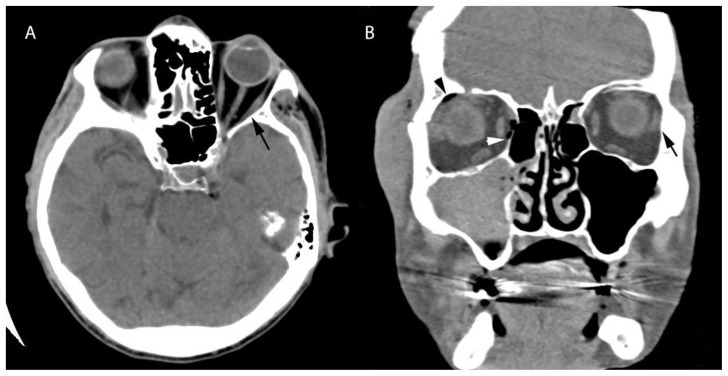
Figure 5.
76-year-old male with traumatic subperiosteal orbital hematoma
Findings: (A) Axial soft tissue algorithm CT image of the head at mid-orbit level shows an extraconal mass (arrow), hyperdense to muscle, consistent with a hematoma. Region of interest measurement gave an average 46 HU, maximum 70 HU of the hematoma. There is displacement of the left lateral rectus muscle (arrowhead) and proptosis. The hematoma measures approximately 1.5 × 2.3 × 2.9 cm in the transverse, craniocaudad and AP dimensions respectively (also see coronal view in panel B). (B) Coronal soft tissue algorithm CT image of the head, posterior to the ocular globes, again demonstrates the hematoma (black arrow), displacing the lateral rectus muscle (arrowhead). There is a contralateral right scalp hematoma (white arrow). There is also hyperdense opacification of the right maxillary sinus (*), suspicious for a right-sided fracture. (C) Axial soft tissue algorithm CT image of the head at the level of the superior orbits shows shows a hemorrhagic contusion in the right inferior frontal lobe (arrow). (D) Axial bone algorithm image from a dedicated CT of the facial bones at mid orbit level shows a miniscule lucency consistent with a normal suture (arrow), but no displaced fracture.
Technique: Axial and coronal CT images, 220 mAs, 120 kV, 1.2 mm slice thickness
Figure 6.
76-year-old male with traumatic subperiosteal orbital hematoma
Findings: (A) Axial noncontrast CT image at mid-orbit level of the same patient in figure 5, from approximately one year earlier. The lateral aspect of the left orbit is normal (arrow). (B) Coronal noncontrast orbital CT image of the same patient approximately 6 months later than the images in figure 5, showing that the left lateral subperiosteal hematoma has resolved (arrow). However, there are new right-sided traumatic injuries, as evidenced by abnormal gas in the right orbit (white and black arrowheads).
Technique: Axial head CT, 220 mAs, 120 kV, 5 mm slice thickness; Coronal orbit CT, 24 mAS, 130 kV, 3 mm slice thickness
The patient was managed conservatively, and was discharged several days later. Approximately 6 months later, the patient returned to the emergency department following another episode of trauma. A CT scan of the facial bones showed new right-sided injuries. However, there had been interval resolution of the previous left-sided subperiosteal hematoma (Figure 6B).
DISCUSSION
Etiology & Demographics
Subperiosteal orbital hematoma (SOH) in adults is uncommon. The majority of cases involve young males with blunt trauma. However, nontraumatic SOH has been described, in relation to sudden increased intracranial or intraorbital venous pressure or venous congestion, or in the setting of various bleeding diatheses. Processes associated with increased thoracic pressure, likely with Valsalva maneuver, have been reported in cases of non-traumatic SOH. For example, SOH in the settings of weight-lifting [1], SCUBA diving [2], and vomiting [3] have been described.
SOH has also been reported in association with abnormal bleeding tendencies, such as hepatic disease [4], and in the setting of paranasal sinusitis [5,6], as well as following an anxiety attack [7]. Rarely, no cause is identifiable, and these cases have been previously labeled “spontaneous” [8,9].
Hemorrhage secondary to increased venous pressure is purported to arise from the bleeding of small veins into the potential subperiosteal space between the osseous orbital roof and the periosteum (periorbita). Attachment sites between the periosteum and the osseous orbital roof are relatively fewer than elsewhere in the orbit, which is likely the reason that the majority of nontraumatic cases of SOH occur in the superior orbit [9,10,11,12,13,14]. There are no named blood vessels crossing the orbital roof, however, there are small diploic vessels that may be the source of hemorrhage [9]. Furthermore, orbital veins are valveless, allowing for transmission of increased intrathoracic pressure [15].
Bone infarction is common in sickle cell disease, although involvement of the orbits is rare [16]. Infarction of the orbital walls is more common in younger patients, who have relatively more marrow space in their orbital bones than adults [17], and is more common in females. In addition to the inflammatory swelling associated with the bone infarction, subperiosteal hematoma may occur in this setting, contributing to orbital compression syndrome [16]. These cases are frequently bilateral [18, 19].
Traumatic SOH may frequently be seen in infants with birth trauma, as the periosteum is only firmly attached to the bone [20] at the suture lines, making the potential space between the periosteum and the bone more susceptible to expansion by hemorrhage. The attachment of the periosteum to the bone develops with age, therefore adults are less likely than young children to sustain SOH [13, 20].
Clinical & Imaging findings
In this series, we present three cases of SOH. In Case 1, the patient reported sharp pain in their left orbit following a bout of prolonged retching, presumably resulting in increased venous pressure. This acute onset of pain likely coincided with the onset of the subperiosteal hematoma. Diplopia may also develop acutely in such cases, but was not present in this patient. Also potentially relevant in this case is the patient’s chronic liver disease, which may be considered as a risk factor for hemorrhage. At CT imaging, there is a hematoma in the most common superior location, causing downward displacement of the ocular globe. The hematoma is recognizable by its morphology, specifically, an extraconal mass forming obtuse angles with the adjacent bone, reminiscent of the lentiform shape of an intracranial epidural hematoma. As with hematomas in other locations, hyperdensity with respect to skeletal muscle is common but variable.
In Case 2, there is bilateral SOH in the setting of sickle cell anemia. Nonenhanced CT is generally sufficient to characterize SOH and its associated mass effect on adjacent structures. In this case, the hematomas are superolateral and are inferiorly displacing the bilateral lacrimal glands. The sickle cell anemia patient in Case 2 underwent contrast enhanced CT and MRI evaluation. As expected, the hematomas do not enhance, and are therefore hypodense relative to the extraocular muscles on the contrast enhanced CT. On MRI, SOH has signal on T1 and T2 that varies with the age of the hematoma. For example, on T1- weighted images, a hyperacute hematoma may have low signal, and high signal in the subacute (3–7 days) phase. Conversely, on T2-weighted images, the hematoma will commonly have high signal in the hyperacute phase, and low signal in the subacute phase [9]. In Case 2 of this series, the patient’s subperiosteal hematomas had visible hematocrit levels on T2WI. In addition, there was thin curvilinear enhancement of the tissue along the periphery of the hematomas.
In Case 3, there is a lateral posttraumatic SOH, which is a rare presentation. However, the hematoma in this case has otherwise typical CT density and morphology, manifesting as an extraconal mass with obtuse angles to the adjacent bone. As with nontraumatic SOH, involvement of the superior orbit is most common in traumatic cases [21]. There has been a prior report of a lateral nontraumatic subperiosteal orbital hemorrhage in a case series [14], however, no images were included for this particular case. Subperiosteal hematoma in the lateral orbit has also been described in prior reports of cases related to sickle cell disease [17, 19]. A Pubmed search conducted during the preparation of this manuscript did not reveal any previous reports of a traumatic subperiosteal hematoma in the lateral orbit. Some traumatic cases may be associated with an acute fracture (21), however, the osseous margins of the involved orbit often appear intact at imaging.
Treatment and Prognosis
Most cases of orbital compression syndrome related to sickle cell disease are successfully managed conservatively, mainly by treating the vaso-occlusive crisis and associated inflammation [19]. Similarly, other nontraumatic cases of SOH are frequently dealt with conservatively, with focus on correction of associated conditions such as coagulopathy or sinusitis [9]. However, large subperiosteal hematomas or those accompanied by optic nerve dysfunction may warrant surgical treatment [16, 22]. As with nontraumatic cases, management of traumatic cases may be conservative, but surgical treatment is warranted when there is visual impairment, either by needle aspiration or exploration and drainage [20]. Needle aspiration is less invasive than exploration and drainage, however, it does not provide an opportunity for clot removal or control of active bleeding. Exploration and drainage may provide these benefits, and also may allow for concurrent fracture repair [23].
Patients with large SOH have been reported to be at risk for developing optic nerve atrophy, strabismus, and permanent choroidal folds. However, in a nontraumatic series described by Atalla et al, only one patient out of nine developed any of these complications, specifically optic nerve atrophy, and this may have been ischemic rather than compressive [9]. In a traumatic series described by Yazici and Gonen, eight out of twenty-three patients had signs of optic neuropathy, and two went on to permanent visual loss despite surgical treatment (21, 13, 24).
Differential diagnosis
The acute onset of signs and symptoms, known trauma, or associated nontraumatic activities which raise orbital pressure, usually allow for distinction of SOH from other etiologies. However, there are several entities that warrant mention.
Retrobulbar hematoma
Retrobulbar hematoma is a posttraumatic finding, and may be dense on CT, similar to SOH. However, retrobulbar hematoma presents on imaging as an intraconal mass, possibly exerting mass effect on the optic nerve at its insertion on the globe.
Intraosseous Meningioma
Intraosseous meningioma of the lateral orbital wall classically appears in the sphenotemporal buttress. There may be components that extend into the middle cranial fossa or the orbit. When present, an orbital component may have morphology similar to SOH; specifically, it may lie along the lateral orbital wall and have obtuse angles with the adjacent bone. However, lateral position is very uncommon for SOH. In addition, meningiomas will typically enhance after administration of intravenous contrast for cross sectional imaging.
Metastasis
Orbital metastases are uncommon, but may occur anywhere in the orbit, and therefore may have an appearance similar to SOH in rare cases. However, metastases will most likely enhance after administration of intravenous contrast for cross-sectional imaging. Abnormality of the adjacent bone, or an abnormal periosteal reaction, may be further clues to the correct diagnosis.
Cavernoma
Orbital cavernous venous malformation, formerly called cavernous hemangioma, presents with slowly progressive painless proptosis. This entity is a well-circumscribed intraconal mass with intermediate density on CT. On MRI, T1 and T2 signal varies, and enhancement may be heterogeneous if the mass is imaged early after injection.
Schwannoma
Orbital schwannoma may be indistinguishable from cavernoma. Schwannoma is also intraconal and well circumscribed, with intermediate CT density. Enhancement on MRI is more homogeneous. It is very uncommon in the orbit, and the symptoms depend on which structures are involved/displaced.
TEACHING POINT
Subperiosteal orbital hematoma is uncommon. However, awareness of this entity, and understanding that it may occur in a variety of non-traumatic settings, will allow the radiologist to make this diagnosis accurately.
Table 1.
Summary table for adenoma - hemangioma adrenal collision tumor.
| Etiology | Traumatic, nontraumatic |
| Prevalence | Rare |
| Gender Ratio | Young males following trauma most common |
| Age predilection | Young males following trauma most common |
| Risk factors | Trauma, increased venous pressure (Valsalva), bleeding tendencies |
| Treatment | Usually conservative, needle aspiration or orbitotomy if optic neuropathy present |
| Prognosis | Most cases resolve on their own |
| Findings on imaging | CT: intermediate density mass, extraconal with obtuse angles to the adjacent bone, most commonly superior MRI: mass with variable signal on T1 and T2, similar morphology as with CT |
Table 2.
Differential diagnosis table for subperiosteal orbital hematoma.
| CT | MRI | |
|---|---|---|
| Subperiosteal hematoma |
|
|
| Retrobulbar hematoma |
|
|
| Cavernous Venous Malformation |
|
|
| Schwannoma |
|
|
| Intraosseous Meningioma |
|
|
| Metastasis |
|
|
ABBREVIATIONS
- CT
Computed Tomography
- MRI
Magnetic Resonance Imaging
- SOH
Subperiosteal orbital hematoma
- TE
Echo Time
- TR
Repetition Time
REFERENCES
- 1.Katz B, Carmody R. Subperiosteal orbital hematoma induced by Valsalva maneuver [letter] Am J Ophthalmol. 1985;100:617–8. doi: 10.1016/0002-9394(85)90696-8. [DOI] [PubMed] [Google Scholar]
- 2.Chen JC, Kucharczyk W. Nontraumatic orbital subperiosteal hematoma in a scuba diver: CT and MR findings. J Comput Assist Tomogr. 1988;12(3):504–506. doi: 10.1097/00004728-198805010-00031. [DOI] [PubMed] [Google Scholar]
- 3.Katz RS, Abrams G. Orbital subperiosteal hematoma (epidural hematoma of the orbit) J Clin Neuroophthalmol. 1981;45:45–52. [PubMed] [Google Scholar]
- 4.Moorthy RS, Yung CW, Nunery WR, et al. Spontaneous orbital subperiosteal hematomas in patients with liver disease [case report] Ophthal Plast Reconstr Surg. 1992;8:150–2. doi: 10.1097/00002341-199206000-00012. [DOI] [PubMed] [Google Scholar]
- 5.Choi S, Lawson W, Urken ML. Subperiosteal orbital hematoma. An unusual complication of sinusitis [case report] Arch Otolaryngol Head Neck Surg. 1988;114:1464–6. doi: 10.1001/archotol.1988.01860240114035. [DOI] [PubMed] [Google Scholar]
- 6.Zalzal GH. Periorbital hematoma secondary to sinusitis in a child [case report] Arch Otolaryngol Head Neck Surg. 1991;117:557–9. doi: 10.1001/archotol.1991.01870170103023. [DOI] [PubMed] [Google Scholar]
- 7.Swanenberg IM, Rizzuti AE, Shinder R. Spontaneous subperiosteal hematoma precipitated by anxiety attack. Orbit. 2013;32(6):402–404. doi: 10.3109/01676830.2013.833255. [DOI] [PubMed] [Google Scholar]
- 8.Carrion LT, Edwards WC, Perry LD. Spontaneous subperiosteal orbital hematoma. Ann Ophthalmol. 1979;11:1754–57. [PubMed] [Google Scholar]
- 9.Atalla ML, McNab AA, Sullivan TJ, et al. Nontraumatic subperiosteal orbital hemorrhage. Ophthalmology. 2001;108(1):183–9. doi: 10.1016/s0161-6420(00)00482-6. [DOI] [PubMed] [Google Scholar]
- 10.McNab AA. Nontraumatic orbital hemorrhage. Surv Ophthalmol. 2014;59(2):166–84. doi: 10.1016/j.survophthal.2013.07.002. [DOI] [PubMed] [Google Scholar]
- 11.Subiras X, Koch KR, Schrittenlocher S, et al. Spontaneous Unilateral Subperiosteal Hematoma in the Orbit due to Self-Induced Asphyxia: Unusual Cause of Unilateral Exophthalmos. Case Rep Ophthalmol. 2017;8(1):232–236. doi: 10.1159/000469701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sakurai K, Morita S, Otsuka H, et al. Non-traumatic bilateral orbital subperiosteal hematoma in a person who attempted suicide by hanging. Tokai J Exp Clin Med. 2014;39(3):103–105. [PubMed] [Google Scholar]
- 13.Wolter JR. Subperiosteal hematomas of the orbit in young males: a serious complication of trauma or surgery in the eye region. J Pediatr Ophthalmol Strabismus. 1979;16(5):291–296. doi: 10.3928/0191-3913-19790901-06. [DOI] [PubMed] [Google Scholar]
- 14.Polito E, Leccisotti A. Diagnosis and treatment of orbital hemorrhagic lesions. Ann Ophthalmol. 1994;26:85–93. [PubMed] [Google Scholar]
- 15.Hakin KN, McNab AA, Sullivan TJ. Spontaneous hemorrhage within the rectus muscle [case report] Ophthalmology. 1994;101:1631–4. doi: 10.1016/s0161-6420(94)31126-2. [DOI] [PubMed] [Google Scholar]
- 16.Sundu C, Dinc E, Sari A, et al. Bilateral subperiosteal hematoma and orbital compression syndrome in sickle cell disease. J Craniofac Surg. 2017;28(8):e775–e776. doi: 10.1097/SCS.0000000000003972. [DOI] [PubMed] [Google Scholar]
- 17.Ganesh A, William RR, Mitra S, et al. Orbital involvement in sickle cell disease: a report of five cases and review literature. Eye. 2001;15(6):774–780. doi: 10.1038/eye.2001.248. [DOI] [PubMed] [Google Scholar]
- 18.Ghafouri RH, Lee I, Freitag SK, et al. Bilateral orbital bone infarction in sickle-cell disease. Ophthalmic Plast Reconstr Surg. 2011;27(2):e26–7. doi: 10.1097/IOP.0b013e3181c70b65. [DOI] [PubMed] [Google Scholar]
- 19.Sokol JA, Baron E, Lantos G, et al. Orbital compression syndrome in sickle cell disease. Ophthalmic Plat Reconstr Surg. 2008;24(3):181–4. doi: 10.1097/IOP.0b013e31816b960e. [DOI] [PubMed] [Google Scholar]
- 20.Ganesan K, Fabbroni G, Loukota R, et al. Traumatic subperiosteal hematomas of the orbit: a report of 2 cases. J Oral Maxillofac Surg. 2008;66:1266–1269. doi: 10.1016/j.joms.2007.06.656. [DOI] [PubMed] [Google Scholar]
- 21.Yazici B, Gonen T. Posttraumatic subperiosteal hematomas of the orbit in children. Ophthal Plast Reconstr Surg. 2011;27:33–37. doi: 10.1097/IOP.0b013e3181eea1e9. [DOI] [PubMed] [Google Scholar]
- 22.Curran EL, Fleming JC, Rice K, et al. Orbital compression syndrome in sickle cell disease. Ophthalmology. 1997;104(10):1610–5. doi: 10.1016/s0161-6420(97)30088-8. [DOI] [PubMed] [Google Scholar]
- 23.Pope-Pegram LD, Hamill MB. Post traumatic subgaleal hematoma with subperiosteal orbital extension. Surv Ophthalmol. 1986;30:258–62. doi: 10.1016/0039-6257(86)90122-0. [DOI] [PubMed] [Google Scholar]
- 24.Kersten RC, Rice CD. Subperiosteal orbital hematoma: visual recovery following delayed drainage. Ophthalmic Surg. 1987;18:423–7. [PubMed] [Google Scholar]