Abstract
Serious side effects of vaccinations are not common, though rare complications can occur. We present a case of one such uncommon side effect, influenza vaccine-related subacromial/subdeltoid bursitis. A 72-year-old female presented with severe shoulder pain following influenza vaccination. The pain persisted for up to two months despite conservative measures, and MRI demonstrated moderate subacromial/subdeltoid bursitis. Vaccine-related shoulder dysfunction includes a range of pathology, from osteonecrosis to bursitis, which will be reviewed in this report. Recognition of infrequent vaccine-related musculoskeletal pathology is important to prevent delay of diagnosis.
Keywords: Influenza, vaccine, bursitis, myositis, vaccine-related bursitis, autoimmune/inflammatory syndrome induced by adjuvants, shoulder injury related to vaccine administration, vaccine-related shoulder dysfunction
CASE REPORT
A 72-year-old female presented to an outpatient internal medicine clinic, two weeks following administration of the influenza vaccination. The patient reported right upper arm pain extending from the injection site to the mid upper arm. No erythema, edema, or neuropathic symptoms (motor weakness or sensory changes) were reported. The patient’s only relevant past medical history included hypertension. The patient did not have a known history of diabetes, rheumatoid arthritis or gout. The patient did not have a history of known trauma. Her physical activities included walking, yoga, and Pilates. Her occupation is as an office worker. The pain started following the injection and persisted up to the patient’s presentation to internal medicine clinic. On physical exam, the patient displayed mild to moderate tenderness to palpation at the site of vaccine injection. No visible wound, erythema, or edema was noted at the injection site. The patient was instructed to take non-steroidal anti-inflammatory drugs, as needed, as well as to apply heat or ice packs to the region for pain relief.
The patient returned to clinic two weeks after the initial appointment, with increasing right shoulder pain that had affected her range of motion, activities of daily living, and sleep. Given the worsening symptoms, the patient was referred to orthopedic surgery and was ultimately evaluated in the orthopedic clinic four weeks following vaccine administration. At that time, the patient complained of persistent shoulder pain, which worsened with overhead movements and now affected her ability to sleep. Physical examination demonstrated skin erythema overlying the right acromioclavicular joint and superior aspect of the deltoid muscle. Labs obtained at the time of the orthopedic surgery appointment, including a white blood cell count (WBC) of 9.1 K/uL (normal range is 3.8–10.8 K/uL) and erythrocyte sedimentation rate (ESR) of 6 mm/h (normal range is < or = 15 mm/h), were normal.
Imaging Findings
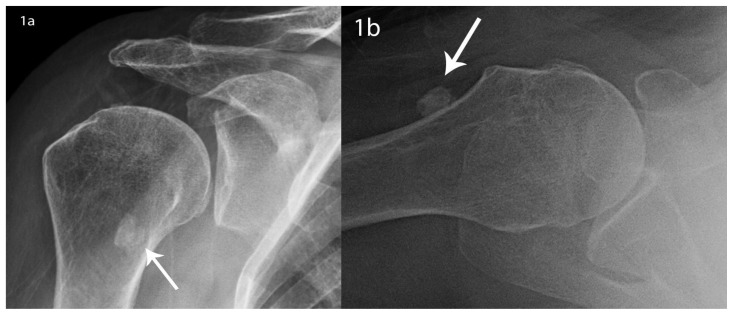
Radiographs of the right shoulder obtained at the time of presentation to the orthopedic clinic showed no acute fracture or dislocation. There was a 9 mm ossification noted at the anterior aspect of the joint, which was interpreted as an ossified chondral body within the bicipital groove (Figure 1). The acromioclavicular and glenohumeral joint spaces were maintained. Given the patient’s persistent symptoms at follow-up appointments, an MRI of the right shoulder was subsequently obtained.
Figure 1.
72 year-old female with right shoulder pain following influenza vaccination, secondary to vaccine-related subacromial/subdeltoid bursitis.
FINDINGS: Initial imaging included a) AP and b) axillary view radiographs. Radiographs showed no acute fracture or dislocation. There was a 9 mm ossification (arrow) noted at the anterior aspect of the joint, which was interpreted as an ossified chondral body within the bicipital groove. The acromioclavicular and glenohumeral joint spaces were maintained.
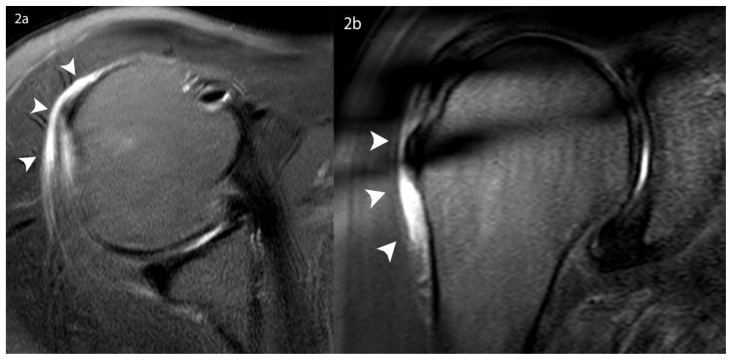
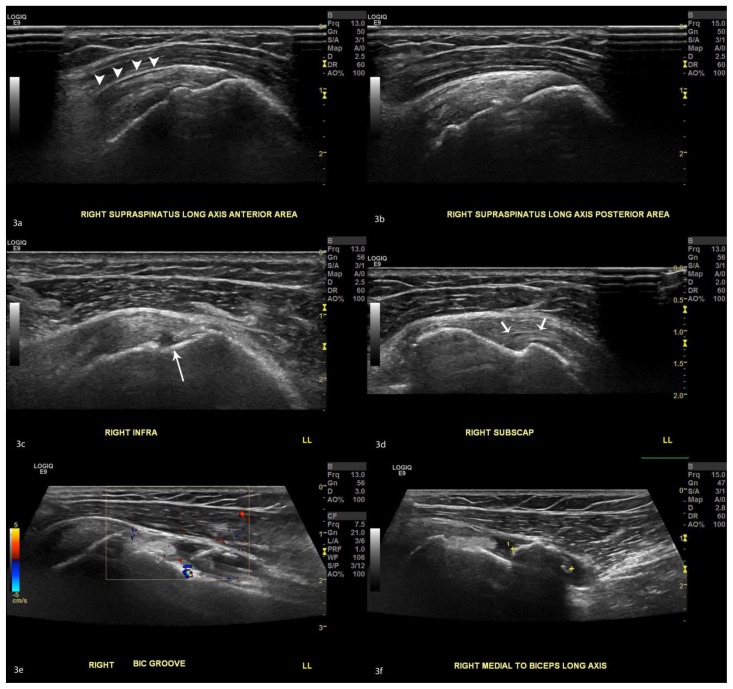
MRI of the right shoulder was performed without intravenous contrast four weeks after the influenza vaccine administration. The patient continued to have severe pain at that time, which affected her ability to limit motion during the MRI acquisition. Limited fluid sensitive sequences were obtained, including axial and coronal T2 fat saturation sequences (Figure 2). These sequences showed moderate T2 hyperintense signal abnormality within the subacromial/subdeltoid bursa, reflecting inflammation of the bursa. Fluid was also noted within the bicipital groove, which was attributed to tenosynovitis. No glenohumeral joint effusion was noted. No other fluid collections or areas of T2 hyperintense signal abnormality were noted, whether in the muscles or bones. Follow-up diagnostic shoulder ultrasound was obtained approximately two weeks after the MRI (Figure 3). The exam showed small amount of residual fluid in the subacromial/subdeltoid bursa. The ossific body in the bicipital groove and fluid within the bicipital groove were redemonstrated. A very small partial thickness, intra-substance tear was noted within the subscapularis tendon. A small partial thickness, articular sided tear in the infraspinatus tendon was noted at the footprint. No full thickness rotator cuff tear was noted.
Figure 2.
72 year-old female with right shoulder pain following influenza vaccine, secondary to vaccine-related subacromial/subdeltoid bursitis.
FINDINGS: 3 Tesla MRI without contrast show images that are somewhat limited by motion artifact and the patient’s request for early termination of the exam. However, fluid distention of the subacromial/subdeltoid bursa is distinctly visualized on the available sequences. A) Axial and b) coronal T2 FS sequence shows subacromial/subdeltoid bursal fluid (arrowheads).
Technique: 3T Axial T2 with fat saturation (TR 5145, TE 80); 3T Coronal T2 with fat saturation (TR 4662, TE 80).
Figure 3.
72 year-old female with right shoulder pain following influenza vaccine, secondary to vaccine-related subacromial/subdeltoid burisits.
FINDINGS: Sonographic evaluation of the right shoulder (a–f) with a linear GE ML6-15 transducer set at 11 to 15 MHz shows a) small amount of residual fluid in the subacromial/subdeltoid bursa (arrowheads). B) Intact supraspinatus tendon at the footprint. C) Small partial thickness, articular sided tear in the infraspinatus tendon at the footprint (long arrow). D) A very small partial thickness intra-substance tear is noted within the subscapularis tendon (short arrows). No full thickness rotator cuff tear is noted. E–F) Redemonstrated ossific body in the bicipital groove. Small amount of fluid and hyperemia around the bicipital groove.
Management
The patient continued to have pain for 2 months following the vaccine administration and was therefore referred for ultrasound-guided injection of the subacromial/subdeltoid bursa. Under ultrasound-guidance, 2 cc of 1% lidocaine and 1 cc of 40 mg/mL depomedrol were injected into the subacromial/subdeltoid bursa. The patient’s pain decreased from 5/10 to 1/10 following injection. At a follow-up appointment one month after the steroid injection, the patient noted significant improvement in her pain and range of motion. Baseline shoulder pain was reported to be 3/10 and the patient had resumed almost all activities of daily living that had been limited by the pain.
DISCUSSION
Etiology & Demographics
In the United States, annual influenza vaccination is recommended in all people unless contraindicated, and compliance with this recommendation is common. For the 2015 – 2016 flu season, approximately 45.6% of all people over the age of 6 months were covered by the flu vaccination [1]. Mild musculoskeletal symptoms are common after influenza vaccination. An estimated 60–80% of people who receive the injectable influenza vaccine report site tenderness, swelling, and pain [2]. Serious complications of vaccination are uncommon and vary according to the type of vaccination. The incidence of developing a complication after intramuscular injection ranges from 0.4 – 19.4% [3,4]. The influenza vaccine has been associated with Guillain-Barre syndrome or severe allergic reaction, though both are rare [2]. Although transient shoulder pain is common, persistent pain is rare. Persistent pain following vaccine injection has been referred to as vaccine-related shoulder dysfunction. In these cases, prolonged shoulder pain and dysfunction may be due to uncommon underlying injuries related to vaccination administration, including myositis, bursitis, osteitis, intramuscular sterile abscess formation, rotator cuff tears, tendonitis, adhesive capsulitis, and osteonecrosis [5,6,7,8,9]. Proposed hypotheses for potential causes include vaccine over-penetration/poor injection technique, inappropriate needle length, the patient’s physical characteristics, and a robust local immune-mediated inflammatory reaction if vaccine antigen is injected into synovial tissues under the deltoid muscle [7,10]. Post-vaccine complications are more frequently seen in females with a male/female ratio ranging from 0.31 – 0.41, which may be explained by women’s smaller muscle mass [10]. Children and adults are both affected, however the majority of the literature reports a mean age of approximately 50 years old. Female gender, smaller muscle mass, pre-existing asymptomatic shoulder injuries which might be aggravated as a result of an inflammatory reaction related to vaccination, or possibly injection of a vaccine antigen to which a person has previously been sensitized as a result of previous naturally occurring infection or past vaccination are thought to be risk factors for vaccine related musculoskeletal injury [5,11].
Clinical and Imaging Findings
Patients with vaccine-related shoulder dysfunction present with persistent shoulder pain following vaccination. The reported length of time from vaccination to onset of symptoms ranges from immediately following the injection to three days post-injection. The time the patient presents for clinical evaluation varies from immediately following injection to a few months later [5,6,7,9,11,12]. Symptoms include shoulder pain, limited range of motion, altered sensation, and weakness. Systemic symptoms, such as fever, have been described in some cases, including within the pediatric population [7,11]. In most cases, laboratory results, including white blood cell count, C-reactive protein, and erythrocyte sedimentation rate, are normal. Exceptions include more severe cases such as post vaccine related myositis and myocarditis, in which cases laboratory findings demonstrate rhabdomyolysis and acute kidney injury [13].
Vaccine-related shoulder dysfunction is a diagnosis of exclusion. Clinical history and timing related to vaccination are the most important findings. Lack of other laboratory findings, including normal white blood cell count (WBC), can help confirm clinical suspicion. The role of imaging is to further characterize the source of the pain, whether osseous, bursal, or muscle-related.
Imaging findings in shoulder dysfunction related to vaccine administration vary depending on the source of shoulder pain. Radiographs are nonspecific and may not provide useful diagnostic information. MRI and ultrasound may demonstrate increased fluid +/− debris within the subacromial/subdeltoid bursa, intramuscular edema, rotator cuff tendinopathy or tear, or cortical irregularity. Vaccine-related myositis will present as focal or diffuse edema within the muscle at the site of the injection, most commonly the deltoid [14]. Fluid with or without synovitis in the subacromial/subdeltoid bursa is suggestive of bursitis. Osseous changes include focal marrow edema, typically at the lateral aspect of the proximal humerus. When present, this marrow edema is typically described as osteitis. At least one case of osteonecrosis has been described, which presented with typical imaging findings of osteonecrosis including hyperemia, bone marrow edema, and incongruity of the humeral head contour compatible with bone collapse [15].
Treatment & Prognosis
The imaging findings of myositis, osteitis, bursitis, or osteonecrosis are not specific to a particular etiology. If radiologists are not aware that these findings can be associated with vaccine-related injury, then they may incorrectly attribute the findings to another diagnosis or may recommend unnecessary further imaging evaluation or diagnostic procedures. When needed, treatment is mostly supportive, including non-steroidal anti-inflammatory drugs (NSAIDs), corticosteroid injections, physical therapy, and rarely surgery [10]. While severity and duration may vary depending upon the underlying injury, a review of several case series found that more than half of patients required at least one steroid injection. All patients had symptoms for at least 6 months, and less than one third eventually achieved complete recovery [11].
Differential Diagnosis
The differential diagnosis for vaccine-related bursitis includes other etiologies of bursitis, such as infection or trauma. Inflammatory bursitis, including secondary to rheumatoid arthritis, dermatomyositis, and polymyositis, may be considered in the appropriate clinical setting.
Distinguishing infectious versus vaccine-related bursitis is particularly difficult on imaging alone. While radiographs of the shoulder are most likely normal in appearance, cortical irregularity may be present. On CT, the inflamed bursa appears hypodense with an enhancing wall. On MRI, the fluid-filled bursa will appear T2 hyperintense. On ultrasound, the bursa will appear as a fluid filled anechoic structure lined by a hyperechoic wall. Ultimately, the clinical history and laboratory findings are the most helpful factor in distinguishing these etiologies.
In contrast to vaccine-related myositis, and as the name implies, rotator cuff injury-related bursitis is always associated with rotator cuff tear. Radiographs may be normal or demonstrate decreased acromiohumeral interval. CT again shows an inflamed hypodense bursa with a hyperenhancing wall. In the case of full-thickness tears of the rotator cuff, MRI will demonstrate T2 hyperintense/T1 hypointense fluid from within the glenohumeral joint which tracks through the tear into the bursa. Communication with the joint is abnormal in this location. Ultrasound will show a fluid-filled anechoic structure both on longitudinal and transverse planes corresponding to bursal fluid. Again, many of these imaging features are nonspecific, and therefore, the key to differentiating vaccine-related pathology from rotator cuff injury is the additional presence of a full-thickness rotator cuff tear.
Inflammatory bursitis has some overlapping imaging findings as well, however will have additional features of the underlying inflammatory arthropathy to help distinguish it from other etiologies. For example, in the case of rheumatoid arthritis, cortical irregularity, joint effusion, erosions of the distal clavicle, or marginal erosions of the humeral head may be present as well. On CT, the inflamed bursa will again appear hypodense with an enhancing wall, however there may be an associated joint effusion and cortical erosions. In addition to nonspecific high T2 signal within the bursa, juxta-articular T2 hyperintense pre-erosions, T1/T2 hypointense rice bodies, and thickened, hyperemic synovium with contrast enhancement may be present in cases of rheumatoid-related inflammatory bursitis. Ultrasound may demonstrate heterogeneity of the usual smooth hypoechoic cartilage, nodular proliferation of the synovium, and hypervascularity on power Doppler.
TEACHING POINT
Vaccine-related shoulder dysfunction is a known but uncommon complication of vaccination. Radiologists should be aware of this complication to help guide recommendations for imaging of a patient with persistent post-vaccination shoulder pain. An MRI or ultrasound may be considered to evaluate for the following: osteonecrosis, osteitis, bursitis, or myositis. Bursitis is a nonspecific finding and other etiologies, including infectious, inflammatory, or traumatic, may be considered depending on the clinical setting. Given the prevalence of yearly vaccination, vaccine-related bursitis should be considered when no other etiology is evident.
Table 1.
Summary table for flu-shot related orthopedic findings.
| Etiology | Prolonged shoulder pain and dysfunction from uncommon underlying injuries related to vaccination administration, including myositis, intramuscular sterile abscess formation, bursitis, rotator cuff tears, tendonitis, adhesive capsulitis, and osteonecrosis. Proposed hypotheses for potential causes include vaccine over-penetration/poor injection technique, inappropriate needle length, the patient’s physical characteristics, and a robust local immune-mediated inflammatory reaction if vaccine antigen is injected into synovial tissues under the deltoid muscle. |
| Incidence | The incidence of developing a complication after intramuscular injection ranges from 0.4 – 19.4%. |
| Gender Ratio | Post-vaccine complications are more frequently seen in females with a male/female ratio ranging from 0.31 – 0.41, which may be explained by women’s smaller muscle mass. |
| Age Predilection | Children and adults are both affected, however the majority of papers report a mean age of approximately 50 years old. |
| Risk Factors | Female gender, smaller muscle mass, pre-existing asymptomatic shoulder injuries which might be aggravated as a result of an inflammatory reaction related to vaccination, or possibly injection of a vaccine antigen to which a person has previously been sensitized as a result of previous naturally occurring infection or past vaccination. |
| Treatment | NSAIDs, corticosteroid injections, physical therapy, and rarely surgery |
| Prognosis | While severity and duration may vary depending upon the underlying injury, a review of several case series found that more than half of patients required at least one steroid injection. All patients had symptoms for at least 6 months, and less than one third eventually achieved complete recovery. |
| Findings on Imaging | Varies depending upon the underlying vaccine-related injury. Radiographs are nonspecific and may not provide useful diagnostic information. MRI and ultrasound may demonstrate increased fluid +/− debris within the subacromial/subdeltoid bursa, intramuscular edema, rotator cuff tendinopathy or tear, or cortical irregularity. |
Table 2.
Differential diagnosis table for subacromial/subdeltoid bursitis.
| Radiography | Computed Tomography (CT) | MRI | Ultrasound (US) | |
|---|---|---|---|---|
| Infectious Bursitis |
|
|
|
|
| Rotator Cuff injury-related bursal fluid |
|
|
|
|
| Inflammatory Bursitis (i.e. secondary to Rheumatoid Arthritis) |
|
|
|
|
| Flu-shot related bursitis |
|
|
|
|
ABBREVIATIONS
- CT
computed tomography
- MRI
magnetic resonance imaging
- NSAIDs
non-steroidal anti-inflammatory drugs
- US
ultrasound
- WBC
white blood cell
REFERENCES
- 1.Centers for Disease Control and Prevention. Flu Vaccination Coverage, United States 2015-16 Influenza Season. [Accessed December 15, 2017]. Retrieved from https://www.cdc.gov/flu/fluvaxview/coverage-1516estimates.htm.
- 2.Influenza Vaccine. STN BL 125254. Jul, 2017. Seqirus Package Insert. [Google Scholar]
- 3.Greenblatt DJ, Allen MD. Intramuscular injection-site complications. JAMA. 1978;240:542–544. [PubMed] [Google Scholar]
- 4.Treadwell T. Intramuscular injection site injuries masquerading as pressure ulcers. Wounds. 2003;15:302–312. [Google Scholar]
- 5.Barnes MG, Ledford C, Hogan K.A “needling” problem: shoulder injury related to vaccine administration J Am Board Fam Med 2012.Nov-Dec 256919–22. 10.3122/jabfm.2012.06.110334 [DOI] [PubMed] [Google Scholar]
- 6.Martin Arias LH, Sanz Fadrique R, Sainz Gil M, Salgueiro-Vazquez ME. Risk of bursitis and other injuries and dysfunctions of the shoulder following vaccinations. Vaccine. 2017;35(37):4870–4876. doi: 10.1016/j.vaccine.2017.07.055. [DOI] [PubMed] [Google Scholar]
- 7.Katz, Lee D. Vaccination-induced myositis with intramuscular sterile abscess formation. Skeletal Radiology. 2011;40:1099–1101. doi: 10.1007/s00256-011-1158-7. [DOI] [PubMed] [Google Scholar]
- 8.Cook IF. Subdeltoid/subacromial bursitis associated with influenza vaccination. Hum Vaccin Immunother. 2014;10(3):605–606. doi: 10.4161/hv.27232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bodor M, Montalvo E. Vaccination-related shoulder dysfunction. Vaccine. 2007 Jan 8;25(4):585–7. doi: 10.1016/j.vaccine.2006.08.034. Epub 2006 Sep 8. [DOI] [PubMed] [Google Scholar]
- 10.Cross GB, Moghaddas J, Buttery J, Ayoub S, Korman TM. Don’t aim too high: avoiding shoulder injury related to vaccine administration. Aust Fam Physician. 2016;45(5):303–306. [PubMed] [Google Scholar]
- 11.Atanasoff S, Ryan T, Lightfoot R, Johann-Liang R. Shoulder injury related to vaccine administration (SIRVA) Vaccine. 2010 Nov;28(51):8049–52. doi: 10.1016/j.vaccine.2010.10.005. [DOI] [PubMed] [Google Scholar]
- 12.Polat AV, Bekci T, Dabak N, Ulu EM, Selcuk MB. Vaccine-induced myositis with intramuscular sterile abscess formation: MRI and ultrasound findings. Skeletal Radiol. 2015 Dec;44(12):1849–52. doi: 10.1007/s00256-015-2242-1. Epub 2015 Aug 26. [DOI] [PubMed] [Google Scholar]
- 13.Cheng MP, Kozoriz MG, Ahmadi AA, Kelsall J, Paquette K, Onrot JM. Post-vaccination myositis and myocarditis in a previously healthy male. Allergy Asthma Clin Immunol. 2016 Feb 11;12:6. doi: 10.1186/s13223-016-0114-4. eCollection 2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Okur G, Chaney KA, Lomasney LM. Magnetic resonance imaging of abnormal shoulder pain following influenza vaccination. Skeletal Radiol. 2014 Sep;43(9):1325–31. doi: 10.1007/s00256-014-1875-9. Epub 2014 Apr 11. [DOI] [PubMed] [Google Scholar]
- 15.Kuether G, Dietrich B, Smith T, Peter C, Gruessner S. Atraumatic osteonecrosis of the humeral head after influenza A-(H1N1) v-2009 vaccination. Vaccine. 2011 Sep 16;29(40):6830–3. doi: 10.1016/j.vaccine.2011.07.052. [DOI] [PubMed] [Google Scholar]