Abstract
Background:
The incidence of adolescent suicide is rising in the U.S., yet we have limited information regarding short-term prediction of suicide attempts. Our aim was to identify predictors of suicide attempts within 3-months of an emergency department (ED) visit.
Methods:
Adolescents, ages 12 – 17, seeking health care at 13 pediatric EDs (Pediatric Emergency Care Applied Research Network) and one Indian Health Service Hospital in the U.S. were consecutively recruited. Among approached patients, 6,654 (62%) completed a suicide risk survey. A subset of participants (n = 2,902) was assigned to a 3-month telephone follow-up, and 2,104 participants completed this follow-up (72% retention). Our primary outcome was a suicide attempt between the ED visit and 3-month follow-up.
Results:
One hundred four adolescents (4.9%) made a suicide attempt between enrollment and 3-month follow-up. A large number of baseline predictors of suicide attempt were identified in bivariate analyses. The final multivariable model for the full sample included the presence of suicidal ideation during the past week, lifetime severity of suicidal ideation, lifetime history of suicidal behavior, and school connectedness. For the subgroup of adolescents who did not report recent suicidal ideation at baseline, the final model included only lifetime severity of suicidal ideation and social connectedness. Among males, the final model included only lifetime severity of suicidal ideation and past week suicidal ideation. For females, the final model included past week suicidal ideation, lifetime severity of suicidal ideation, number of past-year nonsuicidal self-injury (NSSI) incidents, and social connectedness.
Conclusions:
Results indicate that the key risk factors for adolescent suicide attempts differ for subgroups of adolescents defined by sex and whether or not they report recent suicidal thoughts. Results also point to the importance of school and social connectedness as protective factors against suicide attempts.
Keywords: Suicide risk, adolescence, suicide attempt, social connectedness, emergency department
Introduction
Suicide rates among adolescents in the United States continue to rise (Centers for Disease Control and Prevention, 2019), despite a downturn in the incidence worldwide (World Health Organization, 2017). Moreover, 5.1% of male and 9.3% of female high school students in the U.S. report a suicide attempt (SA) in the past year (Kann et al., 2018).
Risk factors for adolescent SAs span demographic, clinical, and social domains, meaning that the risk profiles for suicidal adolescents are multidimensional and heterogeneous. Female adolescents and adolescents who self-identify as LGBTQ are at increased risk (Kann et al., 2018; O’Brien, Putney, Hebert, Falk, & Aguinaldo, 2016). Previous history of SA and suicidal ideation (SI) (Nock et al., 2013), presence, persistence, and severity of SI (Czyz & King, 2015), and nonsuicidal self-inijury (NSSI) (e.g., Asarnow et al., 2011) have all been reported to be predictors of suicide attempts. Similarly, psychiatric symptom, such as depression and hopelessness, are consistent correlates and predictors of SA (King, Ewell Foster, & Rogalski, 2013), and symptoms of distress (e.g., anxiety and agitation) and impulse control (e.g., aggression, substance abuse) have emerged as the strongest predictors of attempts among adolescents who report ideation (Nock et al., 2013). Sleep disturbance has been reported as an imminent risk factor for SA and death by suicide (e.g., Koyawala, Stevens, McBee-Strayer, Cannon, & Bridge, 2015).
Interpersonal factors such as low social connectedness also have been related to the likelihood of suicidal ideation and behavior (Czyz, Liu, & King, 2012; Gunn, Goldstein, & Gager, 2018). Bully victims and perpetrators have reported an increased incidence of SAs (Borowsky, Taliaferro, & McMorris, 2013), and physical and sexual abuse have been prospectively associated with SAs (Castellví et al., 2017). Interpersonal conflicts and losses, and legal/disciplinary problems are acute stressors associated with SAs and suicide (e.g., Gould, Fisher, Parides, Flory, & Shaffer, 1996).
Given this heterogeneity of suicide risk factors, it is challenging for healthcare providers to assess level of risk and for intervention and prevention specialists to identify potent and potentially modifiable targets for risk reduction. Moreover, extant research has focused on single risk factors (Franklin et al., 2017), despite the growing recognition of the multidimensional nature of suicidal risk and current clinical practice, which attempts to to integrate available information about multiple risk factors. Consequently, further research that takes into account multiple risk factors is sorely needed.
The challenge of suicide risk assessment and identification of potent prevention targets is exacerbated for males and for adolescents who conceal or deny their suicidal thoughts. Adolescent females are more likely than males to report SI and behavior (Kann et al., 2018) and to obtain mental health services (Rhodes et al., 2012); yet the rate of suicide is much higher among adolescent males than females (Centers for Disease Control and Prevention, 2019). An improved understanding of the short-term risk factors for SAs among males may enable us to improve risk recognition and prevention. Similarly, although many of the most commonly used screening tools assess SI (e.g., Horowitz et al., 2012), recent SI is not a significant predictor of SAs for all subgroups of adolescents (e.g., King, Jiang, Czyz, & Kerr, 2014).
Our objective was to examine predictors of SAs during the 3-months following adolescents’ ED visits in the Study One dataset of the Emergency Department Screening for Teens at Risk for Suicide (ED-STARS) Study. This large-scale study was implemented in collaboration with the Pediatric Emergency Care Applied Research Network (PECARN). Its primary aim was to develop the Computerized Adaptive Screen for Suicidal Youth (CASSY), a relatively brief suicide risk screen with the potential for widespread implementation in emergency departments (King et al., under review). Because our baseline assessment included a broad array of previously identified risk factors for SAs, this study also enabled us to examine predictors of SAs following ED visits using multi-variable models.
We examined predictors in the total follow-up sample and in subsamples defined by sex and the presence of recent SI. We hypothesized that predictors of SAs would include indicators of SI and behavior (e.g., past week suicidal ideation, lifetime history of suicidal behavior) and, reflecting a different domain, one or more interpersonal risk factors (e.g., peer victimization, low social or school connectedness). We expect interpersonal factors to be important in light of longitudinal studies (e.g., Gunn et al., 2018) and theoretical formulations about the salience of interpersonal processes to suicidal risk (e.g., Durkheim, 1897; Joiner, 2005).
Methods
Participants
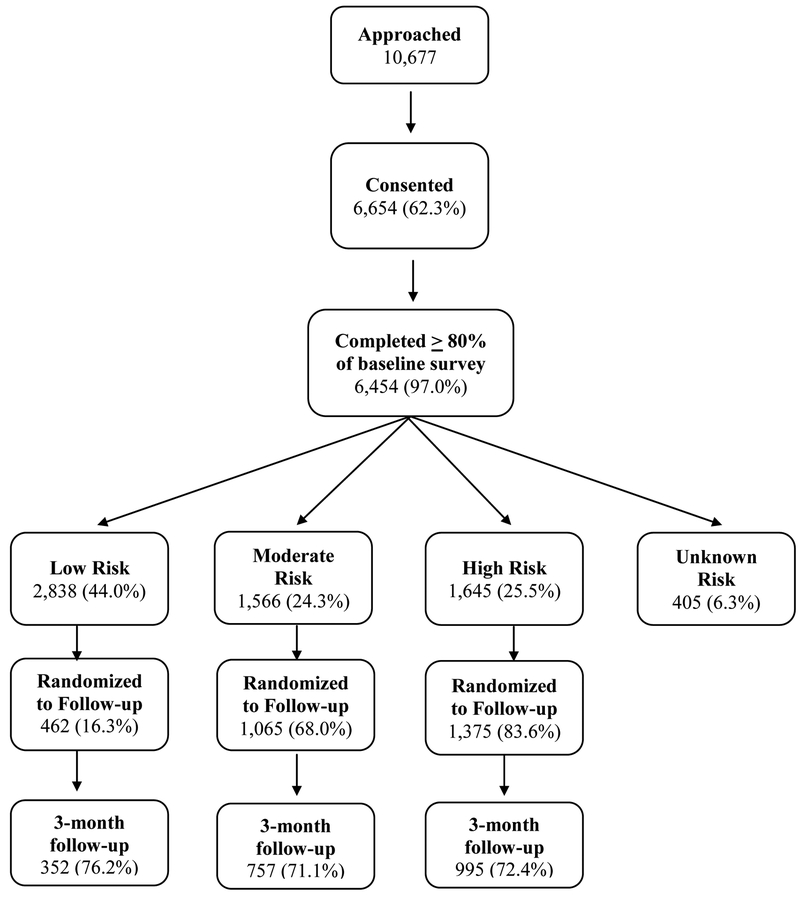
Adolescents (ages 12–17) were recruited from 13 EDs in PECARN (June 2015-July 2016) and the Whiteriver Indian Health Service (IHS) Hospital, which serves the White Mountain Apache Tribe (November 2015–April 2017). Among 10,677 approached adolescents, 6,654 (62%) completed a suicide risk survey. A subset of patients (n=2,902, 45%) enriched for suicide risk (Figure 1 and Appendix S1 in the Supporting Information) was randomly assigned to a 3-month telephone follow-up; 2,104 participants completed this follow-up (72% retention). The sample included 1,327 females (63.1%) and 777 males (36.9%) with a mean age of 15.1 years (SD=1.6). Additonal demographic information is in Appendix S2.
Figure 1.
Participant flow
Note. High risk = suicidal ideation with intent/plan, history of suicide attempt, NSSI 5 or more times in past year, or homicidal ideation with intent/plan; Moderate risk = suicidal ideation, homicidal ideation (without plan/intent), or two or more other suicide risk factors (see Supplement for details). Low risk = does not meet criteria for High or Moderate risk.
Procedure
At PECARN sites, adolescents were recruited during screening shifts that were randomly selected for each site from time periods when research coordinators were on site (primarily afternoons and evenings due to higher volume of adolescent patients). At the IHS Hospital, recruitment was ED-linked with a daily admission review and IRB permission to contact at home for recruitment. Exclusion criteria were: previous study enrollment, ward of State, non-English speaking adolescents (non-English speaking parents enrolled), medically unstable, and severe cognitive impairment.
Adolescents completed a self-report survey assessing demographics and suicide risk factors in the ED (except for IHS site). Participants were included if adolescent and parent (n=1,799, 85.5%), adolescent only (n=183, 8.7%) or parent only (n=122, 5.8%) follow-up interviews were conducted. Follow-up informant (parent or youth versus both) was unrelated to participants’ lifetime histories of suicidal ideation and behavior, and to the suicide attempt outcome. Participants with only youth or only parent follow-up interviews were, however, older than those with both interviews. (p <.001, Kruskal-Wallis test.). Written informed parent/guardian consent and adolescent assent were obtained, in addition to IRB approval from all sites. Adolescents who turned 18 prior to follow-up were reconsented.
Measures
This study incorporated adolescent data from the baseline self-report survey (92 primary, 27 follow-up questions; details in Appendix S3). Due to ED space and time constraints, a concern for respondent burden, and a need to assess a wide range of risk factors to develop CASSY algorithms, brief, adapted versions of standardized scales were used for many risk factors, all of which had been previously associated with adolescent SAs.
An adapted Columbia-Suicide Severity Rating Scale (CSSRS; Posner et al., 2008) was used to assess history of SAs at baseline and SAs between baseline and 3-month follow-up. SA was defined as a positive response to either of two questions: “In the past 3 months, have you made a suicide attempt?” “In the past 3 months, have you tried to harm yourself because you were at least partly trying to end your life?” Past week SI was assessed with question #3 from the Ask Suicide-Screening Questions (ASQ; Horowitz et al., 2012): “In the past week, have you been having thoughts about killing yourself?” In defining subgroups of adolescents who did and did not report recent SI, we removed participants who selected “unknown” or did not respond to the question.
Additional suicide risk factors assessed at baseline included lifetime severity of SI and suicidal behavior, suicidal rumination, NSSI, depression, hopelessness, homicidal ideation, anxiety, agitation, sleep disturbance, adaptive functioning, alcohol and drug use, impulsivity, aggression, connectedness (family, school, social), peer victimization, physical and sexual abuse, negative life events, and identification as a sexual or gender minority.
Statistical analysis
Univariable associations between baseline demographic and clinical risk factors and SAs at 3-months were determined, and predictors with significant associations (p<0.1) were candidates for inclusion in multivariable logistic regression models (Hosmer, Lemeshow, & Sturdivant, 2013). In stage one, demographics and variables pertaining to suicidal thoughts, suicidal behaviors, and NSSI were added to the model in a stepwise fashion; the model with the lowest Akaike Information Criterion (AIC) was carried forward. Remaining candidates, including all other clinical risk factors examined (see Table 1), were considered using forward stepwise selection. In the final stage, variables were dropped using backward selection (p>0.05), such that all variables were statistically significant in the final model.
Table 1.
Univariable relations between baseline variables and suicide attempt/death
| Suicide Attempt/Death | |||||
|---|---|---|---|---|---|
| Yes (N = 104) |
No (N = 2000) |
p value2 |
Unadjusted, weighted3 Odds Ratio | ||
| Demographics | |||||
| Gender: Female | 84 (80.8%) | 1243 (62.2%) | <.001 | 3.4 (1.8, 6.6) | |
| Race | 0.710 | ||||
| American Indian or Alaska Native | 2 (1.9%) | 55 (2.8%) | 0.7 (0.1, 4.0) | ||
| Asian/Native Hawaiian/Pacific Islander | 2 (1.9%) | 30 (1.5%) | 1.0 (0.2, 6.9) | ||
| Black or African American | 22 (21.2%) | 464 (23.2%) | 0.8 (0.4, 1.6) | ||
| White | 64 (61.5%) | 1058 (52.9%) | |||
| Multi-racial | 6 (5.8%) | 126 (6.3%) | 0.9 (0.3, 2.7) | ||
| Unknown/unavailable | 8 (7.7%) | 267 (13.4%) | 0.4 (0.2, 1.2) | ||
| Ethnicity | 0.256 | ||||
| Latinx | 18 (17.3%) | 439 (22.0%) | 0.7 (0.3, 1.4) | ||
| Not Latinx | 70 (67.3%) | 1329 (66.5%) | |||
| Unknown/unavailable | 16 (15.4%) | 232 (11.6%) | 1.5 (0.7, 3.0) | ||
| Childs grade in school | 0.939 | ||||
| 5th - 8th grade | 37 (36.6%) | 673 (34.9%) | |||
| 9th - High School graduate | 64 (63.4%) | 1247 (64.6%) | 1.1 (0.6, 1.9) | ||
| Child does not attend school | 0 (0.0%) | 9 (0.5%) | N/A | ||
| Mother/Stepmother education | 0.695 | ||||
| High school graduate or less | 27 (26.7%) | 559 (29.0%) | |||
| Some college/technical training | 28 (27.7%) | 553 (28.7%) | 1.1 (0.5, 2.2) | ||
| College graduate/professional | 41 (40.6%) | 769 (39.9%) | 1.1 (0.6, 2.1) | ||
| Don’t know/Not applicable | 5 (5.0%) | 47 (2.4%) | 2.2 (0.6, 8.1) | ||
| Father/Stepfather education | 0.374 | ||||
| High school graduate or less | 32 (32.0%) | 761 (39.6%) | |||
| Some college/technical training | 29 (29.0%) | 376 (19.6%) | 1.7 (0.9, 3.4) | ||
| College graduate/professional training | 27 (27.0%) | 599 (31.2%) | 1.1 (0.5, 2.1) | ||
| Don’t know/Not applicable | 12 (12.0%) | 184 (9.6%) | 1.5 (0.6, 3.7) | ||
| Family public assistance | 51 (51.0%) | 859 (44.8%) | 0.389 | 1.3 (0.7, 2.1) | |
| Suicidal Ideation/Behavior/NSSI | |||||
| Suicidal ideation – past week: ASQ #3 | <.001 | ||||
| Yes | 69 (66.3%) | 348 (17.4%) | 22.0 (12.0, 40.2) | ||
| No | 27 (26.0%) | 1503 (75.3%) | |||
| No Response | 8 (7.7%) | 145 (7.3%) | 5.9 (2.1, 17.0) | ||
| Suicide ideation severity - lifetime: C-SSRS; mean (sd) | 4.1 (1.28) | 1.9 (1.98) | <.001 | 2.2 (1.8, 2.6) | |
| NSSI # methods (YRBS); mean (sd) | 2.4 (2.34) | 0.8 (1.50) | <.001 | 1.6 (1.5, 1.8) | |
| NSSI # incidents (YRBS) | <.001 | ||||
| 0 times | 24 (23.1%) | 1354 (67.9%) | |||
| 1–2 times | 27 (26.0%) | 312 (15.6%) | 9.7 (4.6, 20.2) | ||
| 3–4 times | 14 (13.5%) | 107 (5.4%) | 15.2 (6.1, 37.9) | ||
| 5 or more times | 39 (37.5%) | 222 (11.1%) | 21.1 (10.5, 42.3) | ||
| Suicide attempts/behavior - lifetime | <.001 | ||||
| None | 13 (13.0%) | 1243 (63.1%) | |||
| Aborted/Interrupted attempt only | 12 (12.0%) | 199 (10.1%) | 11.8 (4.2, 33.4) | ||
| 1 Previous suicide attempt | 12 (12.0%) | 152 (7.7%) | 15.5 (5.5, 43.9) | ||
| Multiple previous attempts | 63 (63.0%) | 377 (19.1%) | 32.8 (15.1, 71.1) | ||
| Self-Harm Thoughts (PHQ, #9) | <.001 | ||||
| Not at all | 26 (25.0%) | 1447 (72.7%) | |||
| Several days | 20 (19.2%) | 275 (13.8%) | 8.0 (3.6, 17.5) | ||
| More than half the days | 20 (19.2%) | 113 (5.7%) | 20.0 (9.0, 44.8) | ||
| Nearly every day | 38 (36.5%) | 156 (7.8%) | 27.0 (13.5, 54.0) | ||
| Suicidal thoughts – duration: C-SSRS | <.001 | ||||
| Never had suicidal thoughts | 4 (3.9%) | 876 (44.3%) | |||
| A few seconds or minutes | 6 (5.8%) | 362 (18.3%) | 8.2 (1.6, 41.8) | ||
| Less than 1 hour / some of the time | 19 (18.4%) | 330 (16.7%) | 29.5 (7.4, 117.7) | ||
| 1–4 hours / a lot of time | 32 (31.1%) | 205 (10.4%) | 83.3 (22.0, 316.0) | ||
| 4–8 hours / most of day | 19 (18.4%) | 100 (5.1%) | 103.0 (25.4, 417.3) | ||
| More than 8 hours / continuous | 23 (22.3%) | 105 (5.3%) | 118.6 (30.0, 469.4) | ||
| How likely…act on suicidal thoughts? | <.001 | ||||
| No suicidal thoughts/not at all likely | 22 (21.4%) | 1411 (70.9%) | |||
| Slightly possible | 29 (28.2%) | 345 (17.3%) | 10.9 (5.2, 22.9) | ||
| Somewhat likely | 23 (22.3%) | 158 (7.9%) | 19.3 (8.7, 42.9) | ||
| Almost for sure will act on them | 29 (28.2%) | 77 (3.9%) | 49.5 (22.5, 108.9) | ||
| Suicidal Rumination: mean (sd) | 7.2 (2.66) | 2.9 (3.20) | <.001 | 1.6 (1.4, 1.7) | |
| Other Risk Factors | |||||
| Hopelessness item: MFQ | <.001 | ||||
| Not true | 18 (17.3%) | 1178 (58.9%) | |||
| Sometimes | 49 (47.1%) | 613 (30.7%) | 9.2 (4.5, 19.0) | ||
| True | 37 (35.6%) | 209 (10.5%) | 24.2 (11.3, 52.0) | ||
| Depression: PHQ-9; mean (sd) | 15.5 (7.34) | 8.5 (7.04) | <.001 | 1.2 (1.1, 1.2) | |
| Alcohol use: AUDIT-C score; mean (sd) | 0.5 (1.53) | 0.3 (1.12) | 0.047 | 1.2 (1.0, 1.4) | |
| Cannabis use: DUS (adapted) | 20 (19.2%) | 187 (9.4%) | <.001 | 3.5 (1.8, 6.8) | |
| Homicidal thoughts | 15 (14.6%) | 140 (7.0%) | <.001 | 3.9 (1.8, 8.4) | |
| Agitation: BAM; mean (sd) | 13.9 (5.23) | 9.3 (5.72) | <.001 | 1.2 (1.1, 1.3) | |
| Anxiety: SCARED-C; mean (sd) | 4.5 (2.18) | 3.0 (2.37) | <.001 | 1.4 (1.3, 1.5) | |
| Sleep Disturbance: PROMIS; mean (sd) | 13.5 (3.89) | 11.6 (4.18) | <.001 | 1.2 (1.1, 1.3) | |
| Physical abuse -family | 24 (23.3%) | 296 (14.9%) | 0.001 | 2.8 (1.5, 5.3) | |
| Sexual abuse | 36 (36.0%) | 310 (15.7%) | <.001 | 5.2 (3.0, 9.1) | |
| Gender minority | 13 (12.5%) | 125 (6.3%) | 0.009 | 2.9 (1.3, 6.5) | |
| Sexual minority | 61 (58.7%) | 580 (29.0%) | <.001 | 6.1 (3.6, 10.3) | |
| Functional Impairment (PHQ, #10) | 82 (79.6%) | 1016 (50.9%) | <.001 | 7.1 (3.7, 13.5) | |
| Family Connectedness; mean (sd) | 6.5 (1.71) | 7.6 (1.84) | <.001 | 0.6 (0.6, 0.7) | |
| Social connectedness scale: mean (sd) | 6.4 (2.45) | 7.7 (2.10) | <.001 | 0.7 (0.6, 0.8) | |
| School connectedness scale: mean (sd) | 5.2 (2.04) | 6.8 (2.09) | <.001 | 0.6 (0.6, 0.7) | |
| Impulsive aggression screen: mean(sd) | 0.7 (0.93) | 0.4 (0.81) | <.001 | 1.7 (1.3, 2.2) | |
| Impulsivity: UPPS Subscale; mean(sd) | 2.9 (0.72) | 2.5 (0.88) | <.001 | 2.4 (1.8, 3.3) | |
| Peer victimization; mean (sd) | 4.1 (2.41) | 3.2 (1.80) | <.001 | 1.3 (1.2, 1.5) | |
| Peer bullying perpetration; mean (sd) | 2.6 (1.49) | 2.3 (0.97) | 0.002 | 1.3 (1.1, 1.6) | |
| Physical fighting: YRBS | 0.016 | ||||
| 0 times | 68 (66.0%) | 1391 (69.6%) | |||
| 1 time | 11 (10.7%) | 279 (14.0%) | 1.1 (0.5, 2.5) | ||
| 2 or 3 times | 11 (10.7%) | 208 (10.4%) | 1.4 (0.6, 3.4) | ||
| 4 or more times | 13 (12.6%) | 121 (6.1%) | 3.8 (1.7, 8.6) | ||
| Negative life events: mean (sd) | 0.6 (0.72) | 0.4 (0.60) | <.001 | 2.3 (1.6, 3.2) | |
Missing participant data varies across measures from low (PROMIS, n = 1; YRBS fighting and negative life events, n = 2; PHQ-9, n = 3; past week suicidal ideation, n = 4; C-SSRS Severity Score, n = 5) to high (father education, n = 84; public assistance, n = 86).
All p-values come from Wald Chi-squared tests.
To account for the oversampling of higher risk groups for follow-up, a weight equal to the inverse of the sampling probability of each of the three risk groups was applied in analyses.
To account for the oversampling of higher risk groups for follow-up, a weight equal to the inverse of the sampling probability of each of the three risk groups was applied in analyses. For categorical variables, the reference level was ‘No’, ‘None’, or equivalent, when possible. White and non-Hispanic were used as reference populations. When model separation became an issue due to low counts, categories of predictor variables were combined. For each final model, we calculated the predictive performance of the model as the Area Under the Curve (AUC), with a 95% confidence interval (CI). As a sensitivity analysis, we conducted a10-fold cross-validation of the final model for the full sample. Statistical analyses were performed using SAS software version 9.4 (SAS Institute Inc, 2013).
Results
Retention
Retention was greater for males than females (76.0% versus 70.6%; p=.002) and varied by race (p < .001) and ethnicity (p < .001), with higher retention rates for Whites (75.0%) and multi-racial youth (79.5%) than other races (range from 60.4–72.5%), and for non-Latinx than Latinx ethnicity (75.5% vs. 65.8%). Higher parental education was also associated with greater retention (p’s <.001). The rentention rates for mothers and fathers, respectively, were: high school or less (67.9%, 68.0%), some college/technical (73.6%, 73.0%), college graduate (77.4%, 81.6%), unknown/not applicable (65.0%, 70.0%).
Descriptive statistics: suicidal thoughts, suicide attempts, and NSSI
At baseline, 1,090 adolescents (51.9%) reported a lifetime history of SI and 827 adolescents (39.7%) reported a lifetime history of suicidal behavior, including actual, aborted, and interrupted attempts. The mean number of lifetime SAs reported was 1.25 (SD=6.29; Median=0). Regarding number of past-year NSSI incidents, 1378 adolescents (65.7%) reported none, 339 adolescents (16.2%) reported 1–2, 121 (5.8%) reported 3–4, and 261 (12.4%) reported 5 or more (data missing, n=5). A SA between ED visit and 3-month follow-up, was reported for 104 adolescents (4.9%; 84 females, 6.3%; 20 males, 2.6%). There was one suicide death, which was included as a SA in analyses.
Spearman correlations among risk factors are reported in Tables S1, S2, S3, and S4. As examples of the strength of correlations, lifetime severity of SI was highly positively correlated with lifetime history of suicidal behavior (.70, p < .001) and moderately positively correlated with number of NSSI incidents during the past 12 months (.53, p < .001). Social and school connectedness were moderately positively correlated (.47, p < .001).
Site differences were identified in suicide risk predictors and outcomes. This information is provided in Tables S5, S6, S7, S8, and S9.
Predictors of suicide attempt during 3 months following ED visit
Univariable associations with suicide attempts (See Table 1). Sex, sexual and gender minority status, and all of the examined psychosocial and clinical characteristics predicted SAs at 3-month follow-up.
Multivariable regression models. The final multivariable model for the total sample included past week SI (yes/no), lifetime severity of SI, history of suicidal behavior, and school connectedness (AUC=0.86, 95% CI: 0.82–0.89; Table 2). In the sensitivity analysis, the ORs, (CIs), and AUCs fitted from each of the 10 subsamples (each approximately 90% of full cohort) were similar, with a median AUC of 0.87 and IQR 0.84–0.90.
Table 2.
Multivariable models for prediction of suicide attempt in total sample
| Suicide Attempt/Death over 3-month follow-up |
||||
|---|---|---|---|---|
| Baseline Characteristic | Yes N = 98 (%) | No N = 1964 (%) | OR (95% CI) | p |
| Suicidal Ideation – Past Week (ASQ Item #3) | 0.005 | |||
| No | 27 (27.6) | 1489 (75.8) | ||
| Yes | 64 (65.3) | 335 (17.1) | 3.25 (1.56, 6.77) | |
| No Response | 7 (7.1%) | 140 (7.1) | 1.37 (0.42, 4.46) | |
| Suicide ideation severity - lifetime: C-SSRS: q1, median, q3 | 3,5,5 | 0,1,4 | 1.35 (1.03, 1.76) | 0.031 |
| Lifetime History of Suicidal Behavior | 0.033 | |||
| None | 13 (13.3) | 1241 (63.2) | ||
| Aborted or Interrupted Attempt Only | 11 (11.2) | 198 (10.1) | 2.59 (0.75, 8.97) | |
| One Suicide Attempt | 11 (11.2) | 152 (7.7) | 2.48 (0.66, 9.36) | |
| Multiple Attempts | 63 (64.3) | 373 (19.0) | 4.69 (1.56, 14.07) | |
| School Connectedness: q1, median, q3 | 3,5,7 | 6, 7, 8 | 0.84 (0.73, 0.96) | 0.011 |
Note. Lower levels of school connectedness indicate worse school connectedness.
To examine replicability of this model across sites, we examined a model including site and the interaction between site and the final model risk score (fitted logit values for each patient). The interaction was non-significant (p=0.55), suggesting that the relationship between the predicted risk and SA outcome does not differ by site. Site was also unrelated to SA risk (p=0.70) after taking into account risk factors.
For adolescents without past week SI at baseline, the final model included lifetime SI severity and social connectedness (AUC =0.84, 95% CI: 0.78–0.90; Table 3). For adolescents with recent SI at baseline, the final model included family public assistance, suicidal rumination (repetitive thoughts) and social connectedness (AUC=0.69, 95% CI: 0.62–0.76; Table 3).
Table 3.
Multivariable model for prediction of suicide attempts among adolescents who did and did not report recent suicidal ideation in emergency department
| Suicide Attempt/Death over 3-month Follow-Up |
||||
|---|---|---|---|---|
| Yes (%) | No (%) | OR (95% CI) | p | |
| Adolescents without Recent Suicidal Ideation | N= 27 | N = 1496 | ||
| Lifetime Suicide Ideation Severity: q1 median q3 | 2,4,5 | 0,0,2 | 2.02 (1.51, 2.69) | <.001 |
| Social Connectedness q1, median, q3 | 5,7,9 | 7,8,10 | 0.76 (0.60, 0.96) | 0.019 |
| Adolescents with Recent Suicidal Ideation | N = 67 | N = 329 | ||
| Family Public Assistance | 0.002 | |||
| No | 28 (41.8) | 204 (62.0) | ||
| Yes | 39 (58.2) | 125 (38.0) | 2.39 (1.38, 4.13) | |
| Suicidal Rumination: q1, median, q3 | 7,9,10 | 6,7,9 | 1.22 (1.06, 1.39) | 0.004 |
| Social Connectedness: q1, median, q3 | 4,6,9 | 5,8,9 | 0.88 (0.79, 0.98) | 0.023 |
Note. Lower connectedness scores indicate worse connectedness.
For male adolescents, the final model included past week SI and lifetime SI severity (AUC=0.89, 95% CI: 0.85–0.94; Table 4). For female adolescents, the model included past week SI, number of NSSI incidents during the past 12 months, and social connectedness (AUC=0.84, 95% CI: 0.81–0.87).
Table 4.
Multivariable models for prediction of suicide attempts among male and female adolescents
| Suicide Attempt/Death over 3-month Follow-Up |
||||
|---|---|---|---|---|
| Yes (%) | No (%) | OR (95% CI) | p | |
| Males | N = 20 | N = 754 | ||
| Suicidal Ideation – Past Week (ASQ Item #3) | 0.020 | |||
| No | 5 (25.0) | 660 (87.5) | ||
| Yes | 15 (75.0) | 94 (12.5) | 9.33 (1.42, 61.57) | |
| Lifetime Suicidal Ideation Severity Score: q1,median, q3 |
3,4,5 | 0,0,3 | 1.69 (1.04, 2.74) | 0.034 |
| Females | N = 84 | N = 1234 | ||
| Suicidal Ideation – Past Week (ASQ Item #3) | 0.010 | |||
| No | 30 (35.7) | 982 (79.6) | ||
| Yes | 54 (64.3) | 252 (20.4) | 2.48 (1.24, 4.96) | |
| NSSI Past 12 Months | 0.025 | |||
| 0 times | 15 (17.9) | 770 (62.4) | ||
| 1–2 times | 25 (29.8) | 202 (16.4) | 3.93 (1.61, 9.58) | |
| 3–4 times | 10 (11.9) | 81 (6.6) | 2.10 (0.66, 6.64) | |
| 5 or more times | 34 (40.5) | 181 (14.7) | 2.80 (1.11, 7.11) | |
| Lifetime Suicidal Ideation Severity Score: q1,median, q3 |
4,5,5 | 0,2,4 | 1.53 (1.20, 1.95) | <.001 |
| ocial Connectedness: n (q1 median q3) | 4, 6, 8 | 6, 8, 10 | 0.83 (0.73, 0.93) | 0.001 |
Note. Lower connectedness scores indicate worse connectedness.
Discussion
In this prospective study of adolescent ED patients, we identified baseline predictors of SAs across a 3-month period of follow-up using multivariable models for the entire sample, and for subsamples defined by sex and the presence or absence of recent suicidal thoughts. These subgroups included two particularly vulnerable groups: adolescent males who receive fewer mental health services (Rhodes et al., 2012) and have a much higher rate of suicide than adolescent females (Centers for Disease Control and Prevention, 2019), and adolescents who do not report recent suicidal thoughts, which challenges risk recognition.
Study results replicate the importance of previously identified suicide risk factors. Every clinical risk factor included in our baseline suicide risk survey was associated significantly with the likelihood of a SA between the baseline ED visit and 3-month follow-up. Concordant with hypotheses, past week SI, lifetime severity of SI, lifetime history of suicidal behavior, and an interpersonal factor, school connectedness, emerged as the key predictors of attempts for the total sample. Moreover, emphasizing the importance of connectedness to our understanding of risk, either school or social connectedness emerged as a key predictor for three of the four subgroups of adolescents studied. Contrary to hypotheses, however, the model for males included only two factors: recent SI and lifetime severity of SI.
Lifetime severity of SI was found to be a key predictor for the overall sample and three of the four subgroups of adolescents examined. This finding is consistent with previous studies indicating that adolescents who develop a suicide plan are more likely to make an attempt than ideators without a plan (Nock et al., 2013), that intensity of SI predicts SAs (Peters, Mereish, Solomon, Spirito, & Yen, 2018), and that “worst ever” SI is as strong a predictor of suicide risk as current ideation (Beck, Brown, Steer, Dahlsgaard, & Grisham, 1999). Similarly, the importance of lifetime history of suicidal behavior is consistent with studies showing that increased risk for subsequent self-harm and death by suicide persists for years after initially seeking health care for self-harm (Finkelstein et al., 2015).
School or social connectedness emerged as a key predictor for several subgroups of adolescents, which is consistent with a growing body of research (Gunn et al., 2018) indicating that higher levels of school connectedness were associated with less suicidal behavior in general school samples, high risk adolescents, and sexual minority adolescents (Marraccini & Brier, 2017). Social connections may have long-term consequences for mortality as well as morbidity. A 14-year follow-up of adolescent hospitalized for SI and behavior found that those assigned to an intervention to mobilize social support from adults had reduced self-injury mortality (King et al., 2019). Therefore, social and school connectness is likely to be an important target for risk assessment and preventive intervention.
Adolescents who do not report recent SI, who comprised nearly one-third of the youth who made SAs in this study, can be challenging to identify in EDs and other settings where the focus is on current risk. In this subgroup, lifetime severity of SI and social connectedness were the primary risk indicators. The accuracy of prediction in this “hidden” subgroup provides particularly strong support for the need for suicide risk screening in the pediatric ED. Surprisingly, the accuracy of prediction for this subgroup (AUC = 0.84) was higher than the accuracy of prediction for the subgroup of adolescents who reported recent suicidal ideation (AUC = 0.69). This may be due to the inconsistency of adolescents’ reports of SI across study measures, which will be the focus of a future study.
NSSI only emerged as a primary risk factor for females. It is unknown whether or not this relates to the different types of NSSI reported by females (Sornberger, Heath, Toste, & McLouth, 2012), social influences and interpersonal challenges associated with engagement in NSSI (Victor & Klonsky, 2018), or females’ higher likelihood of experiencing suicidal thoughts and engaging in suicidal behavior (Kann et al., 2018). The more limited statistical power for adolescent males, due to fewer SA outcomes, may also be important as NSSI was a predictor of SAs among males in univariable analyses.
The prediction model AUCs for the full sample, the sample of adolescents who did not report recent SI at baseline, and the subsamples of males and females each ranged between 0.84 and 0.89, which can be considered excellent classification accuracy (Hosmer et al., 2013), and contrasts with the disappointing performance of previous single risk factor approaches to suicide risk prediction (Franklin et al., 2017). Although the heterogeneity of suicide risk factors and the low base rates of SAs and suicide are challenges to risk stratification (Belsher et al., 2019), findings suggest that a multivariable prediction model can be useful for the short-term prediction of adolescent SAs. However, of equal or greater importance, these models identify potentially important targets for clinical risk evaluation and prevention. Screening tools for risk recognition can be developed using prediction algorithms developed from large data sources (Belsher et al., 2019). We used this strategy in developing the CASSY, is being vavlidated in a new sample.
Results should be considered within the context of study limitations. We used brief and adapted scales to assess most suicide risk factors to reduce respondent burden and facilitate patient flow in EDs. Although each of the baseline clinical risk factors we assessed was found to be a significant univariable predictor of SAs, the use of brief scales may have reduced the reliability of measurement and our ability to fully capture each construct. Furthermore, this study was conducted primarily in pediatric EDs of academic health systems, which are not representative of the range of EDs in the U.S. In addition, we had lower levels of retention for adolescents from racial and ethnic minority groups, females, and adolescents whose parents had less education. Although we considered weighting the sample for non-response, we chose to prioritize adjusting for the oversampling of higher risk groups because we had specific information pertinent to the oversampling and did not want to apply multiple weights to relatively small subgroups. Moreover, for the most part, these variables were not predictive of SA, and therefore our predictive models are most likely not biased due to non-response. Finally, despite the relatively large size of this study, the relatively low number of youth with SAs limited our statistical power for identifying multiple predictors, especially within critical subgroups such as males ,for whom the number of attempts was smaller than for females. While in this study, our focus was on identifying key risk factors, in future reports we will describe how we also used study data to develop and validate an adaptive screening tool.
In summary, in this short-term prospective study of predictors of SAs in a large and diverse sample of adolescents recruited from pediatrics EDs, we found that past week SI, lifetime severity of SI, lifetime history of suicidal behavior, and connectedness were critical risk and protective factors. We also documented variation in key risk factors across important subgroups, including adolescent males and adolescents who did not report recent SI. The risk and protective factors identified may be important to assess in clinical risk evaluations and can serve as important targets for intervention and prevention strategies.
Supplementary Material
Appendix S1. Baseline criteria for assignment to low, moderate, and high-risk groups.
Appendix S2. Study participants - additional demographic information.
Appendix S3. Study measures.
Table S1. Spearman correlations among categorical suicide risk variables.
Table S2. Spearman correlations among categorical suicide risk variables and social variables.
Table S3. Spearman correlations among categorical suicide risk factors and other clinical risk variables.
Table S4. Spearman correlations among clinical risk variables and social variables.
Table S5. Baseline suicidal ideation and 3-month suicide attempt outcomes by site.
Table S6. Baseline history of suicidal ideation & suicidal behavior by site.
Table S7. Baseline school and social connectedness by site.
Table S8. Baseline Non-Suicidal Self-Injury (NSSI) by site.
Table S9. Public assistance (i.e., food stamps, Medicaid) by site.
Key points
What is known:
A wide range of single demographic, psychiatric, and social risk factors for adolescent suicide attempts during a 6 month period or longer have been identified.
What is new:
This multi-site, prospective study of 2,104 adolescent emergency department patients examined predictors of short-term (3-month) risk for suicide attempts. Using multivariable models, we identified predictors in the total sample and in critically important subgroups. Study findings highlight the importance of adolescents’ social and school connectedness and provide new information regarding predictors of attempts for subgroups of males, females, and adolescents who do not report suicidal thoughts.
What is clinically relevant:
Results regarding predictors of suicide attempts can inform the recognition of adolescents at risk and possible targets for prevention and intervention.
Acknowledgements
This study was supported by a grant from the National Institute of Mental Health (NIMH), “Emergency Department Screen for Teens at Risk for Suicide” (ED-STARS, U01 MH104311). It was also supported in part by the Health Resources and Services Administration (HRSA), Maternal and Child Health Bureau (MCHB), Emergency Medical Services for Children (EMSC) Network Development Demonstration Program under cooperative agreements U03MC00008, U03MC00001, U03MC00003, U03MC00006, U03MC00007, U03MC22684, U03MC28845, H3MC26201 and U03MC22685. The information or content and conclusions in this manuscript are those of the authors and should not be construed as the official position or policy of, nor should any endorsements be inferred by, NIMH, HRSA, HHS or the U.S. Government. The funder had no role in the design and conduct of the study; collection, management, analysis and interpretation of the data; preparation, review, or approval of the manuscript; and the decision to submit the manuscript for publication. The authors thank the following individuals from the PECARN network: Joel Fein from the Violence Prevention Initiative and Division of Emergency Medicine at the University of Pennsylvania, Shilpa Patel from the Departments of Emergency Medicine and Trauma Services at the Children’s National Health System, Susan Duffy from the Departments of Emergency Medicine and Pediatrics at the Alpert Medical School at Brown University, Marlene Melzer-Lange from the Department of Emergency Medicine at the Medical College of Wisconsin, Daniel Cohen from the Department of Emergency Medicine at Nationwide Children’s Hospital, and Robert Hickey from the Department of Pediatrics at the University of Pittsburgh. The authors also thank several NIMH-affiliated individuals for their research collaboration and study facilitation: Lisa Colpe, member of ED-STARS Steering Committee; Galia Siegel, Clinical Trials Program Coordinator; Joel Sherrill, Division of Services and Intervention Research; and members of the NIMH DSMB. The authors appreciate the study and data management assistance of Marie Kay, Michelle Robinson, and Casey Evans from the PECARN Data Coordinating Center at the University of Utah; Esther Ullman, Lisa Carn, and Maureen O’Brien from Survey Research Operations at the University of Michigan; and Rebecca Lindsay and Taylor McGuire from the Department of Psychiatry at the University of Michigan. The authors also thank Novalene Goklish (Whiteriver site) from the Department of International Health at the Johns Hopkins Bloomberg School of Public Health, the PECARN research coordinators at study sites, the telephone follow-up interview team at the University of Michigan, and study research assistants. The authors have declared that they have no competing or potential conflicts of interest.
Conflict of interest statement: No conflicts declared.
Supporting information
Additional supporting information may be found online in the Supporting Information section at the end of this article.
References
- Asarnow JR, Porta G, Spirito A, Emslie G, Clarke G, Wagner KD,…Brent DA (2011). Suicide attempts and nonsuicidal self-injury in the treatment of resistant depression in adolescents: Findings from the TORDIA study. Journal of the American Academy of Child and Adolescent Psychiatry, 50(8), 772–781. doi: 10.1016/j.jaac.2011.04.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beck AT, Brown GK, Steer RA, Dahlsgaard KK, & Grisham JR (1999). Suicide ideation at its worst point: A predictor of eventual suicide in psychiatric outpatients. Suicide and Life-Threatening Behavior, 29(1), 1–9. [PubMed] [Google Scholar]
- Belsher BE, Smolenski DJ, Pruitt LD, Bush NE, Beech EH, Workman DE, … Skopp NA (2019). Prediction models for suicide attempts and deaths: A systematic review and simulation. JAMA Psychiatry. doi: 10.1001/jamapsychiatry.2019.0174 [DOI] [PubMed] [Google Scholar]
- Borowsky IW, Taliaferro LA, & McMorris BJ (2013). Suicidal thinking and behavior among youth involved in verbal and social bullying: Risk and protective factors. Journal of Adolescent Health, 53(1 Suppl), S4–S12. doi: 10.1016/j.jadohealth.2012.10.280 [DOI] [PubMed] [Google Scholar]
- Castellví P, Miranda-Mendizábal A, Parés-Badell O, Almenara J, Alonso I, Blasco MJ, … Alonso J (2017). Exposure to violence, a risk for suicide in youths and young adults. A meta-analysis of longitudinal studies. Acta Psychiatrica Scandinavica, 135(3), 195–211. doi: 10.1111/acps.12679 [DOI] [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. (2019). Web-based Injury Statistics Query and Reporting System (WISQARS). Retrieved from https://webappa.cdc.gov/sasweb/ncipc/leadcause.html
- Czyz EK, & King CA (2015). Longitudinal trajectories of suicidal ideation and subsequent suicide attempts among adolescent inpatients. Journal of Clinical Child and Adolescent Psychology, 44(1), 181–193. doi: 10.1080/15374416.2013.836454 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Czyz EK, Liu Z, & King CA (2012). Social connectedness and one-year trajectories among suicidal adolescents following psychiatric hospitalization. Journal of Clinical Child and Adolescent Psychology, 41(2), 214–226. doi: 10.1080/15374416.2012.651998 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Durkheim E (1897). Suicide. New York: Free Press. [Google Scholar]
- Finkelstein Y, Macdonald EM, Hollands S, Sivilotti MLA, Hutson JR, Mamdani MM, … for the Canadian Drug Safety Effectiveness Research Network (CDSERN). (2015). Risk of suicide following deliberate self-poisoning. JAMA Psychiatry, 72(6), 570–575. doi: 10.1001/jamapsychiatry.2014.3188 [DOI] [PubMed] [Google Scholar]
- Franklin JC, Ribeiro JD, Fox KR, Bentley KH, Kleiman EM, Huang X, … Nock MK (2017). Risk factors for suicidal thoughts and behaviors: A meta-analysis of 50 years of research. Psychological Bulletin, 143(2), 187–232. doi: 10.1037/bul0000084 [DOI] [PubMed] [Google Scholar]
- Gould MS, Fisher P, Parides M, Flory M, & Shaffer D (1996). Psychosocial risk factors of child and adolescent completed suicide. Archives of General Psychiatry, 53(12), 1155–1162. [DOI] [PubMed] [Google Scholar]
- Gunn JF, Goldstein SE, & Gager CT (2018). A longitudinal examination of social connectedness and suicidal thoughts and behaviors among adolescents. Child and Adolescent Mental Health, 23(4), 341–350. doi: 10.1111/camh.12281 [DOI] [PubMed] [Google Scholar]
- Horowitz LM, Bridge JA, Teach SJ, Ballard E, Klima J, Rosenstein DL, … Pao M (2012). Ask Suicide-Screening Questions (ASQ): A brief instrument for the pediatric emergency department. Archives of Pediatrics and Adolescent Medicine, 166(12), 1170–1176. doi: 10.1001/archpediatrics.2012.1276 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hosmer DW, Lemeshow S, & Sturdivant RX (2013). Applied logistic regression (Third ed Vol. 398). Hoboken, NJ: John Wiley & Sons. [Google Scholar]
- Joiner TE (2005). Why people die by suicide. Cambridge, MA: Harvard University Press. [Google Scholar]
- Kann L, McManus T, Harris WA, Shanklin SL, Flint KH, Queen B, … Thornton J (2018). Youth risk behavior surveillance—United States, 2017. MMWR Surveillance Summaries, 67(8), 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- King CA, Arango A, Kramer A, Busby DR, Czyz EC, Ewell Foster CJ, & Gillespie BW (2019). Association of the Youth-Nominated Support Team Intervention for Suicidal Adolescents with 11-to 14-year mortality outcomes. Secondary analysis of a randomized clinical trial. JAMA Psychiatry. doi: 10.1001/jamapsychiatry.2018.4358 [DOI] [PMC free article] [PubMed] [Google Scholar]
- King CA, Brent D, Grupp-Phelan J, Casper T, Dean J, Chernick L, … Pediatric Emergency Care Applied Research Network (PECARN). (under review) A Computerized Adaptive Screen for Suicidal Youth (CASSY): Development in the ED-STARS national sample. [Google Scholar]
- King CA, Ewell Foster C, & Rogalski KM (2013). Teen suicide risk: A practitioner guide to screening, assessment, and management New York, NY: Guilford Press. [Google Scholar]
- King CA, Jiang Q, Czyz EK, & Kerr DC (2014). Suicidal ideation of psychiatrically hospitalized adolescents has one-year predictive validity for suicide attempts in girls only. Journal of Abnormal Child Psychology, 42(3), 467–477. doi: 10.1007/s10802-013-9794-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koyawala N, Stevens J, McBee-Strayer SM, Cannon EA, & Bridge JA (2015). Sleep problems and suicide attempts among adolescents: a case-control study. Behavioral sleep medicine, 13(4), 285–295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marraccini ME, & Brier ZM (2017). School connectedness and suicidal thoughts and behaviors: A systematic meta-analysis. School Psychology Quarterly, 32(1), 5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nock MK, Green JG, Hwang I, McLaughlin KA, Sampson NA, Zaslavsky AM, & Kessler RC (2013). Prevalence, correlates, and treatment of lifetime suicidal behavior among adolescents: Results from the National Comorbidity Survey Replication Adolescent Supplement. JAMA Psychiatry, 70(3), 300–310. doi: 10.1001/2013.jamapsychiatry.55 [DOI] [PMC free article] [PubMed] [Google Scholar]
- O’Brien KHM, Putney JM, Hebert NW, Falk AM, & Aguinaldo LD (2016). Sexual and gender minority youth suicide: understanding subgroup differences to inform interventions. LGBT health, 3(4), 248–251. [DOI] [PubMed] [Google Scholar]
- Peters JR, Mereish EH, Solomon JB, Spirito AS, & Yen S (2018). Suicide ideation in adolescents following inpatient hospitalization: examination of intensity and lability over 6 months Suicide and Life-Threatening Behavior. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Posner K, Brent D, Lucas C, Gould MS, Stanley B, Brown GK, … Mann JJ (2008). Columbia-Suicide Severity Rating Scale (C-SSRS). manuscript. New York State Psychiatric Institute. New York. [Google Scholar]
- Qin P, & Nordentoft M (2005). Suicide risk in relation to psychiatric hospitalization. Archives of General Psychiatry, 62(4), 427–432. doi: 10.1001/archpsyc.62.4.427 [DOI] [PubMed] [Google Scholar]
- Rhodes AE, Khan S, Boyle MH, Wekerle C, Goodman D, Tonmyr L, … Manion I (2012). Sex differences in suicides among children and youth: The potential impact of misclassification. Canadian Journal of Public Health, 103(3), 213–217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- SAS Institute Inc. (2013). SAS Software (Version 9.4). Cary, NC: SAS Institute Inc. [Google Scholar]
- Sornberger MJ, Heath NL, Toste JR, & McLouth R (2012). Nonsuicidal self-injury and gender: Patterns of prevalence, methods, and locations among adolescents. Suicide and Life-Threatening Behavior, 42(3), 266–278. [DOI] [PubMed] [Google Scholar]
- Victor SE, & Klonsky ED (2018). Understanding the social context of adolescent nonsuicidal self-injury. Journal of Clinical Psychology. doi: 10.1002/jclp.22657 [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization. (2017). More than 1.2 million adolescents die every year, nearly all preventable. Retrieved from http://www.who.int/mediacentre/news/releases/2017/yearly-adolescent-deaths/en/
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix S1. Baseline criteria for assignment to low, moderate, and high-risk groups.
Appendix S2. Study participants - additional demographic information.
Appendix S3. Study measures.
Table S1. Spearman correlations among categorical suicide risk variables.
Table S2. Spearman correlations among categorical suicide risk variables and social variables.
Table S3. Spearman correlations among categorical suicide risk factors and other clinical risk variables.
Table S4. Spearman correlations among clinical risk variables and social variables.
Table S5. Baseline suicidal ideation and 3-month suicide attempt outcomes by site.
Table S6. Baseline history of suicidal ideation & suicidal behavior by site.
Table S7. Baseline school and social connectedness by site.
Table S8. Baseline Non-Suicidal Self-Injury (NSSI) by site.
Table S9. Public assistance (i.e., food stamps, Medicaid) by site.