Abstract
Background:
Low-income adults in the US have historically had limited access to dental coverage and poor dental health outcomes.
Objective:
We examined the effects of the Affordable Care Act Medicaid expansions on dental visits among low-income adults focusing on the generosity of dental coverage and heterogeneity in effects by dentist supply.
Research Design:
We used data from the 2012, 2014, and 2016 Behavioral Risk Factor Surveillance System surveys. The main analytical sample included nearly 117,000 individuals below 138% FPL. We employed a quasi-experimental difference-in-differences design to identify the impact of the state Medicaid expansions on having a dental visit in the past 12 months by generosity of dental coverage and dentist supply.
Results:
Medicaid expansions were associated with a nearly 6 percentage-point increase in the likelihood of any dental visits in 2016 (over 10% increase from pre-expansion rate) for individuals in Medicaid expanding states with extensive dental benefits. This increase however was concentrated in states with high dentist supply with no evidence of improvement in utilization in states with limited dental coverage or low dentist supply.
Conclusions:
Expanding Medicaid with generous dental coverage improved dental care use only in areas with high dentist supply with no evidence of benefits with low dentist supply or less generous coverage. Improving access to dental care may require both generous coverage and supply-side interventions to increase dentist availability.
Introduction
Low-income adults in the US have historically had worse dental health and less access to dental care than higher income adults. Untreated caries rates are nearly 40% among nonelderly adults below 200% FPL, more than double the rate at higher income.1 Nearly 1 in 4 low-income adults (<200% FPL) have never had a dental visit or not returned for one for more than 5 years, compared to fewer than 1 in 10 higher income adults.2 These inequalities have persisted over the past decade.3
Lack of or limited dental insurance among low-income adults is likely a major barrier to service use. Before the recent Medicaid expansions under the Patient Protection and Affordable Care Act (PPACA), states had very limited Medicaid coverage for poor adults, especially childless adults who were mostly ineligible. Only very poor parents were typically eligible for dental coverage. While the majority of states provided at least some dental coverage in their Medicaid programs for adults, there has been extensive variation in the generosity of that coverage. In 2016, about one third of states provided “extensive” coverage, just over one third provided “limited” coverage, and nearly a quarter provided coverage only for emergency care associated with pain or injury/trauma.1 Therefore, not all adults covered in Medicaid have adequate dental coverage or access to dental services. Despite the limited generosity of dental coverage in many state Medicaid programs for eligible adults, state expansions of Medicaid coverage to adults in 2000–2012 were associated with an increase in dental visits and a decline in untreated dental caries among the newly eligible.4
As of 2016, 31 states and the District of Columbia expanded their Medicaid programs under the PPACA to include all nonelderly adults below 138% FPL, with 26 expanding in 2014.5 Almost all states that had dental coverage for adults prior to the recent expansions extended this coverage to the newly eligible adults after the expansion (Montana and North Dakota the exceptions). Of the expanding states, 28 and DC provide dental coverage to the newly eligible. Of those, 12 have extensive coverage (>100 procedures covered with an annual cap per person ≥ $1,000); 11 states and DC have limited dental coverage (<100 procedures with an annual cap < $1,000); and 5 have only emergency dental coverage.1,6
Several studies have demonstrated that the Medicaid expansions beginning in 2014 have substantially increased Medicaid coverage among low-income adults.7–9 This expansion in Medicaid coverage suggests that the newly eligible low-income adults in expansion states offering dental coverage, especially those offering extensive coverage, would experience an improvement in dental coverage and access to dental services.
Identifying the extent to which increased dental coverage from the recent Medicaid expansions resulted in changes in access and use of dental services is critical for understanding how much dental care use has changed among low-income adults, if at all. However, there has been little work on the effects of the recent Medicaid expansions on dental service use. Nasseh and Vujicic 9 examined the Medicaid expansion effects on any dental visits among adults 21–64 years old with incomes less than 138% FPL. Using the Gallup Wellbeing Index survey from 2010–2016 and a difference-in-differences model, they reported an increase in the likelihood of dental visits of 3–6 percentage-points depending on which comparison states they used (non-expanding states with or without dental benefits or both state groups). Singhal, Damiano, and Sabik 10 provided a descriptive analysis of changes in the likelihood of dental visits in 2014 by state expansion and dental coverage status. They reported a small (1.8 percentage-point) increase in the likelihood of visits among low-income childless adults in expanding states providing coverage for dental services for adults (beyond emergency-only dental services). In contrast, they reported a large decline in the likelihood of visits for parents, a result they suggested might be due to crowd-out of dental services from the newly enrolled childless adults. However, take-up of Medicaid coverage following the recent Medicaid expansions was close between parents and childless adults, raising questions about why crowd-out effects on dental services use (if present) would substantially affect parents but not childless adults. Furthermore, the study’s design did not necessarily rule out time-varying confounders as it did not include Medicaid expanding and non-expanding states in the same regression.
Another unexplored question is the extent to which differences in availability of dentists modify the effects of newly gained Medicaid dental coverage. The premise is that coverage would be more beneficial in areas with greater dentist supply and less beneficial in areas with fewer dentists where access to services is constrained by more limited supply of dentists. The impact of low dentist supply on access of Medicaid beneficiaries is likely exacerbated by the limited participation of dentists in Medicaid, 13,14 increasing the need to explore this question. Recent work has shown that the Medicaid expansions have increased use of cancer screening services only in states with high supply of primary care providers, providing support for this general premise in another context.
This study provides timely evidence on how the PPACA Medicaid expansions have affected use of dental services among low-income non-elderly adults and how these effects vary by the generosity of states in covering dental services. Furthermore, we examine the extent to which these effects change by the availability of dentists in the state. Our hypothesis is that the Medicaid expansions would result in greater access and use of dental services in states with larger dentist supply and smaller returns in states with constrained supply. We also evaluate heterogeneity by demographic factors that are associated with variation in dental services use, unmet dental needs, or differences in Medicaid coverage gains including race/ethnicity, gender, and childless adults versus parents.7,16–18 We generate this evidence for 2016 using quasi-experimental designs.
Study Data and Methods
Data and Sample
We use individual-level data from the Behavior Risk Factors Surveillance System (BRFSS), a nationally representative cross-sectional telephone survey conducted every month in all 50 states and the District of Columbia. BRFSS collects data on individuals’ demographic and socioeconomic characteristics, health behaviors and conditions, and use of preventive services by using random-digit dialing for both landlines and cell phones. BRFSS includes annual core questions and biannual rotating questions. The biannual questionnaires include a question on having dental services, most recently in the 2016 survey. Our outcome measure is a binary indicator for any dental visits in the past 12 months among individuals in the 2012, 2014 and 2016 BRFSS. The BRFSS question inquires about the time since the last visit to a dentist or to a dental clinic regardless of the purpose of the visit, from which we were able to code any visits in the past 12 months. Depending on the month of interview, much of the past 12 months for respondents in 2014 may have occurred in 2013 before Medicaid expansion. Because of this issue in timing of measurement and because changes in coverage and dental services use may take some time before they occur, we expect small effects in 2014 if any. We also use data from 2008 and 2010 for testing model assumptions as noted below. The average BRFSS response rate over the study period was 46.3% with little difference across years.
We restrict the analytical sample to non-elderly adults aged 18 to 64 years with household income below 138% FPL since this is the group affected by the expansions. As household income was reported in categories in BRFSS, we use the midpoints of these categories to calculate household income as a percentage of FPL considering family size and using yearly data on FPL (lagged by one year relative to survey year). Because of the limited income measurement in the survey, we re-estimate the main model for individuals below 200% FPL. Sample descriptive statistics are in Appendix Table 1 online.
Study Design
We employ a quasi-experimental difference-in-differences design to identify the impact of the state Medicaid expansions on dental services use. The model compares pre-post expansion changes in dental service use between Medicaid expanding states (treatment group), and non-expanding states (control group). Treatment states are further separated by generosity of dental coverage. The Medicaid treatment group includes 22 states that had full Medicaid expansions under the PPACA in 2014. We exclude 3 states (Alaska, Montana, and Louisiana) that expanded their Medicaid in late 2015 and 2016 from all analyses as these states would not have experienced the Medicaid expansion effect for the entire post-period (2014-2016). We exclude two other expanding states from the main analysis: Arizona, which did not offer dental coverage to any beneficiaries, and North Dakota, which did not provide any dental coverage to newly eligible adults. The control group includes 18 states that did not expand Medicaid in 2014, and 5 states (Delaware, Maine, Massachusetts, New York and Vermont) plus DC with prior partial or full Medicaid expansions in 2010 but no expansions in 2014. We note Wisconsin expanded Medicaid eligibility up to 100% FPL in 2014, but we assign the state to the controls since the expansion was not part of the PPACA Medicaid expansions. In a sensitivity analysis, we switch Wisconsin to a treatment state because it offers extensive dental coverage. Also, in that additional model, we add Arizona and North Dakota as control states.
The model is specified as follows:
| (1) |
is a binary indicator for having any dental visits in the past 12 months for individual i in state s in year t. is a binary indicator for states that had full Medicaid expansions under the PPACA in 2014 and 2015. The model is estimated separately for expanding states based on their generosity in covering dental services for the newly eligible including: 1) 9 states offering extensive coverage (>100 procedures covered, annual cap per person ≥ $1,000); 2) 8 states offering limited coverage (<100 procedures, annual cap ≤ $1,000); and 3) 5 states offering emergency coverage1. Table 1 lists the treatment states by dental coverage group and control states. and are two binary indicators for year 2014 and 2016. includes age in categories, gender, race/ethnicity, education, employment status, marital status, household income in categories, and two variables considered in BRFSS sampling: homeownership status, and whether respondent was selected as a cellphone or landline user. are state fixed effects capturing time-invariant confounders between states, and includes year fixed effects for capturing national trends between expanding and non-expanding states. is the difference-in-differences parameter representing the Medicaid expansion effect.
Table 1.
Grouping of Treatment and Control States for Medicaid Expansion
| Excluded States | |||
|---|---|---|---|
| Alaska1 Montana1 Indiana1 Arizona2,4 North Dakota3,4 | |||
| Control States | |||
| Alabama Delaware Florida Georgia Idaho Kansas Maine Massachusetts Mississippi Missouri Nebraska New York |
North Carolina Oklahoma South Carolina South Dakota Tennessee Texas Utah Vermont Virginia Washington, DC Wisconsin4 Wyoming |
||
| Treatment States | |||
| Extensive Dental Coverage | Limited Dental Coverage | Emergency Dental Coverage | |
| California Connecticut Iowa New Jersey New Mexico Ohio Oregon Rhode Island Washington |
Arkansas Colorado Illinois Indiana Kentucky Michigan Minnesota Pennsylvania |
Hawaii Maryland Nevada New Hampshire West Virginia |
|
Notes:
indicates states that were excluded in the main estimation of the difference-in-differences model identifying the Medicaid expansion effects because these states expanded in later 2015 and 2016.
Arizona was excluded in the main estimation because it is a Medicaid expanding states but offers no dental coverage.
North Dakota was excluded in the main estimation because it expanded Medicaid in 2014 and provides extensive dental coverage for traditional Medicaid adults, but not for expansion adults.
In a sensitivity analyses, Wisconsin was switched from a control state to treatment state. Arizona and North Dakota were added as control states.
To evaluate heterogeneity in the expansion effects by dentist supply we estimate the model separately by the median proportion of the state population residing in dental health professional shortage areas (HPSAs) in 2013 obtained from Health Resources and Services Administration Data Warehouse.16 For each state, we calculate this proportion by dividing the number of individual’s residing in dental HPSAs by the total population. Next, we calculate the median proportion and separate the states into two groups: 1- above median, representing states with a greater proportion of their populations residing in dental HPSAs and therefore a low supply of dental providers; and 2- below median, representing states with high supply of dental providers. The idea is that states with greater proportions of their populations residing in dental HPSAs have more constrained access to dentists. This is the approach used in another study examining heterogeneity in cancer screening use across primary care provider supply.15
We estimate the regression models using OLS, which enables direct interpretation of the difference-in-differences parameter as the Medicaid expansion effect on the likelihood of any dental visit. Standard errors are clustered at states and all analyses were weighted using the BRFSS individual sampling weights. In order to test the identifying assumption of the difference-in-differences model, we re-estimate the regression by using data from 2008 and 2010 BRFSS. Using an otherwise similar regression specification as shown above but only one period indicator (2010 versus 2008), we test whether the interaction between the period and the Medicaid expansion group (Medicaids) is significant. A significant interaction would suggest differential pre-trends between expanding and non-expanding states and bias in the difference-in-differences estimates. We do not include 2012 in testing pre-trends because of the BRFSS sampling design and weight changes beginning in 2011.
Results
Overall Changes in Dental Visit Rates
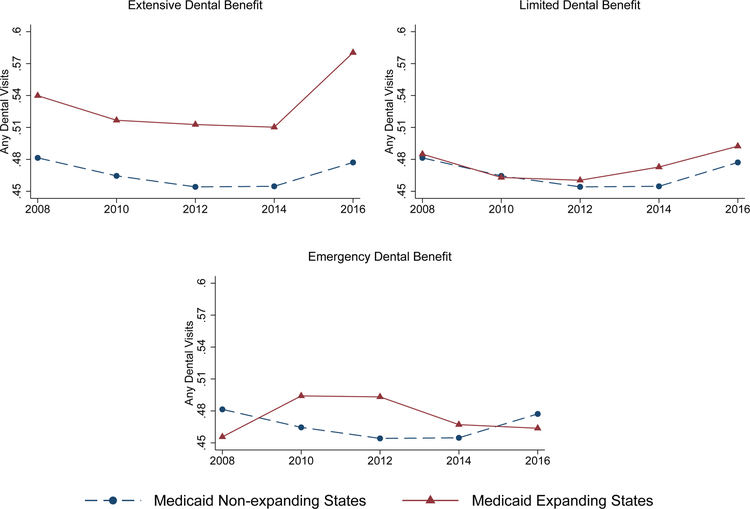
Figure 1 reports dental visit rates between 2008 and 2016 for low-income adults in Medicaid expanding states (by dental coverage generosity) and adults of similar income in non-expanding states. Between 2012 and 2016, individuals in Medicaid expanding states offering extensive dental coverage experienced a 7.5 percentage-point increase in likelihood of dental visits compared to an increase of 2.9 percentage-points for expanding states offering limited dental coverage and 2.2 percentage-points for non-expanding states. There is little evidence of a change in 2014 for these states. The graphs also show overall similar pre-trends between expanding states offering extensive or limited coverage and non-expanding states. In contrast, there is clear evidence of differential pre-trends between Medicaid expanding states covering only emergency dental and non-expanding states.
Figure 1.
Any Dental Visits by Year, Medicaid Expanding Status and State Dental Benefit Generosity
Effects of the Medicaid Expansions on Dental Visits
Table 2 reports the effects of the Medicaid expansions on the likelihood of dental visits by generosity of state dental coverage estimated from the difference-in-differences model for non-elderly adults with income below 138% FPL. Individuals in states expanding Medicaid and offering extensive dental coverage were 5.8 percentage-points more likely to have a dental visit in 2016 compared to 2012. As expected, we find the effect in 2014 to be much smaller and insignificant. Consistent with the descriptive graphic data, we find only a small and insignificant increase (1.1 percentage-points) for individuals in expanding states offering limited dental benefits. In states expanding Medicaid but covering only emergency dental services, the estimates indicate a decline in dental visits, but consistent with the graphical data, we find significant differential pre-trends for this model (pre-trend tests in Appendix Table 2 online), suggesting that these estimates are confounded. For that reason, we only focus on presenting results from the additional models below only for expanding states offering extensive or limited coverage. We observe similar results overall when expanding the sample to include individuals below 200% FPL (Appendix Table 3 online). Results are also similar in the sensitivity analysis switching Wisconsin to a treatment state and adding Arizona and North Dakota as control states (Appendix Table 4 online).
Table 2.
Difference-in-Difference Estimates of Effects of PPACA Medicaid Expansion on the Likelihood of Dental Visits among Non-elderly Adults below 138% FPL by State Generosity of Dental Benefit Coverage
| Dental Benefit Generosity | N | Pre-Mean | Year 2014*Medicaid Expansion | Year 2016*Medicaid Expansion | ||
|---|---|---|---|---|---|---|
| Extensive Dental Benefit | 90308 | 0.491 | 0.004 | (0.017) | 0.058*** | (0.020) |
| Limited Dental Benefit | 88410 | 0.472 | 0.012 | (0.017) | 0.011 | (0.018) |
| Emergency Dental Benefit | 77690 | 0.472 | −0.041**(+) | (0.016) | −0.071**(+) | (0.028) |
Notes: Standard errors are in parentheses and clustered by state. These effects were estimated from the difference-in-differences model and represent the change in likelihood of use of dental services in 2014 and 2016 versus 2012 as a result of the Medicaid expansions. All regressions controlled for age, gender, race/ethnicity, education, employment status, marital status, household income, homeownership status, phone usage and state and year fixed effects, and were weighted by BRFSS sampling weights.
indicates that there are differential pre-trends between expanding states offering only emergency dental coverage and non-expanding states which suggests that the difference-in-difference estimates are confounded and should be viewed with caution.
Significant at 10 percent level;
significant at 5 percent level;
significant at 1 percent level.
Next, we present results from analyses evaluating the heterogeneity in Medicaid expansion effects across demographic factors (Table 3). For expanding states offering extensive dental coverage, the increase in dental visits was larger among non-Whites, females, and parents. The effect on males was small and insignificant. Interestingly, the increase among childless adults was significant but smaller than that among parents, in contrast to other above-mentioned work. For expanding states offering limited coverage, effects were small and insignificant across all subgroups except for a moderate increase for females in 2016 (4.2 percentage-points). For expanding states covering only emergency dental services, we found significant differential pre-trends across multiple subgroups so we do not show those results (available upon request).
Table 3.
Difference-in-Difference Estimates of Effects of PPACA Medicaid Expansion on the Likelihood of Dental Visits among Non-elderly Adults below 138% FPL by State Generosity of Dental Benefit Coverage Stratifying by Age, Race/Ethnicity, Gender and Parental Status
| N | Pre-Mean | Year 2014*Medicaid Expansion | Year 2016*Medicaid Expansion | |||
|---|---|---|---|---|---|---|
| Extensive Dental Benefit | ||||||
| Non-Hispanic Whites | 50813 | 0.472 | −0.016 | (0.022) | 0.042** | (0.019) |
| Non-Whites | 39495 | 0.505 | 0.012 | (0.021) | 0.062** | (0.027) |
| Male | 33553 | 0.452 | −0.026 | (0.025) | 0.021 | (0.026) |
| Female | 56752 | 0.519 | 0.027* | (0.014) | 0.085*** | (0.026) |
| Childless Adults | 44837 | 0.459 | 0.002 | (0.018) | 0.039* | (0.021) |
| Parents | 45471 | 0.515 | 0.007 | (0.023) | 0.072*** | (0.023) |
| Limited Dental Benefit | ||||||
| Non-Hispanic Whites | 53637 | 0.459 | 0.013 | (0.017) | 0.017 | (0.021) |
| Non-Whites | 34773 | 0.486 | 0.014 | (0.030) | 0.011 | (0.025) |
| Male | 32608 | 0.427 | −0.001 | (0.027) | −0.028 | (0.028) |
| Female | 55799 | 0.505 | 0.023 | (0.017) | 0.042** | (0.020) |
| Childless Adults | 44587 | 0.430 | 0.027 | (0.021) | 0.024 | (0.023) |
| Parents | 43823 | 0.506 | −0.002 | (0.028) | −0.001 | (0.026) |
Notes: Standard errors are in parentheses and clustered by state. These effects were estimated from the difference-in-differences model and represent the change in likelihood of use of dental services in 2014 and 2016 versus 2012 as a result of the Medicaid expansions. All regressions controlled for age, gender, race/ethnicity, education, employment status, marital status, household income, homeownership status, phone usage and state and year fixed effects, and were weighted by BRFSS sampling weights.
Significant at 10 percent level;
significant at 5 percent level;
significant at 1 percent level.
Heterogeneity in Expansion Effects by Dentist Supply
As noted above, we separate states based on the median proportion of the state population residing in dental HPSAs and re-estimate the difference-in-differences models for separately for expanding states providing extensive dental coverage and expanding states providing limited coverage. In Appendix Table 5, we show the average proportion of the state’s population in dental HPSAs by dentist supply, Medicaid expansion status, and generosity of dental coverage in expanding states, and the number of states in each group. States designated to have low dentist supply had between 18–27% of their population residing in dental HPSAs compared to 5–9% in states with high dentist supply. Expanding and non-expanding states were relatively close on proportion residing in dental HPSAs.
In Table 4, we report the results from the difference-in-differences models stratified by dentist supply; pre-trend tests in Appendix Table 7 online indicate no significant differential pre-trends for expanding states with extensive or limited coverage but significant pre-trends for only emergency coverage so we focus on extensive or limited coverage. Medicaid expansion with extensive dental coverage increases the likelihood of dental visits only in states with high dentist supply while the effects are noticeably smaller and insignificant from the null in states with low dentist supply. The likelihood of dental visits increases by 6.7 percentage-points in states below median proportion residing in dental HPSAs. We find no significant effects of Medicaid expansion with limited dental coverage in low or high dentist supply.
Table 4.
Difference-in-Difference Estimates of Effects of PPACA Medicaid Expansion on Dental Visit among Non-elderly Adults with Household Income Less than 138% FPL by State Generosity of Dental Benefits and Dental Provider Supply
| N | Pre-Mean | Year 2014*Medicaid Expansion | Year 2016*Medicaid Expansion | |||
|---|---|---|---|---|---|---|
| States with High Provider Supply | ||||||
| Extensive Dental Benefit | 45011 | 0.516 | 0.003 | (0.025) | 0.067** | (0.023) |
| Limited Dental Benefit | 44533 | 0.497 | 0.014 | (0.028) | 0.036 | (0.026) |
| States with Low Provider Supply | ||||||
| Extensive Dental Benefit | 45297 | 0.431 | 0.007 | (0.015) | 0.020 | (0.020) |
| Limited Dental Benefit | 43877 | 0.440 | 0.007 | (0.015) | −0.015 | (0.016) |
Notes: Standard errors are in parentheses and clustered by state. These effects were estimated from the difference-in-differences model and represent the change in likelihood of use of dental services in 2014 and 2016 versus 2012 as a result of the Medicaid expansions. All regressions controlled for age, gender, race/ethnicity, education, employment status, marital status, household income, homeownership status, phone usage and state and year fixed effects, and were weighted by BRFSS sampling weights.
Significant at 10 percent level;
significant at 5 percent level;
significant at 1 percent level.
Discussion
We provide timely evidence using the most recent nationally representative data from the BRFSS on the effects of Medicaid expansion on dental visits by generosity of dental services coverage. Our difference-in-differences model exploiting quasi-experimental variation between expanding and non-expanding states suggests that expanding Medicaid with extensive coverage of dental services has increased the likelihood of dental visits among low-income nonelderly adults by nearly 6 percentage-points in 2016 (compared to 2012), corresponding to over 10% increase from the nearly 50% pre-expansion rate of any dental visits in this population. However, we find no evidence that expanding Medicaid with limited dental services coverage meaningfully changes dental visits in this population. We also find some differences in effects of extensive dental coverage across race/ethnicity and gender. Specifically, we find no evidence of improved dental visits for non-Hispanic Blacks or for males. We do, however, find significant increases in dental visits following Medicaid expansion with extensive coverage for both childless adults and parents, in contrast to a prior study using 2014 data. We find little evidence of changes in 2014, which is expected since use is measured over past 12 months from the interview which may include time before the expansion happened.
Perhaps more importantly, we find evidence of heterogeneity in the Medicaid expansion effects by dentist supply. We find that the only increase in dental visits after expanding Medicaid and offering extensive dental coverage occurred in states with high dentist supply. This finding is intuitive since individuals who gain dental coverage but live in areas with limited availability of dentists are unlikely to benefit much from that coverage. In contrast, gaining coverage in areas with greater availability of dentists translates into a meaningful change in access and use of services. This evidence indicates that in order to meaningfully improve access to dental care for low-income adults, both demand-side interventions such as providing extensive coverage, and supply-side interventions that increase dentists in shortage areas are needed. This finding is similar to recent evidence showing increased use of cancer screening services following the Medicaid expansions only in areas with high primary care provider supply. In contrast, expanding Medicaid with limited dental coverage has overall no effects on dental visits irrespective of dentist supply. This finding is also intuitive since limited coverage may still imply high and unaffordable out-of-pocket cost for many low-income adults.
The study has some limitations but also implications for future research. We cannot separate dental visits into checkups and treatments in this data. However, we expect both to increase with coverage as checkups are typically the starting point to identify treatment needs. Our results and approach provide the basis for future work examining effects separately for preventive services and treatments. We also note that between 2012 and 2016 period, one expanding state (Pennsylvania) and six non-expanding states had changes in the proportion of their populations residing in dental HPSAs that would change their assignment into low or high dentist supply groups. However, excluding these states has no impact on the results (Appendix Table 7 online). Also, in a sensitivity analysis, we control for the number of dentists per capita at the state level and find similar results (Appendix Table 8 online). It is also worth noting that even though the measure of generosity of dental coverage we employ captures both the number of covered procedures and caps on spending,6 there may still be differences in generosity between states in the same group. Future work evaluating such differences is useful for furthering our understanding of the effects of dental coverage generosity on utilization. It is also important to note that 3 states (California, New Jersey, and Washington) increased their dental benefits to extensive coverage along with the ACA Medicaid expansions. Therefore, the increase in dental visits we observe for expanding states with extensive coverage represents an average effect from expanding coverage to more individuals but also expanding dental benefits for Medicaid beneficiaries in some states. Separating these effects and examining potential effect heterogeneity across states in future work are useful for understanding the range of effects from the Medicaid expansions across states. Finally, we are unable to provide evidence on expanding Medicaid but covering only emergency dental services due to significant differential pre-trends between expanding and non-expanding states. Evidence from the Oregon Medicaid expansion experiment indicates increased use of emergency dental visits and medications with emergency only coverage but no changes in use of uncovered dental services. That finding is broadly consistent with our evidence on increased dental visits with extensive dental coverage. Future work considering alternative designs can help identify the effects of expanding Medicaid with emergency only coverage for the five states that did so.
Supplementary Material
Acknowledgments
Funding Source: National Institute of Dental and Craniofacial Research, Grant 1R03 DE02804101
Footnotes
Disclosures: The authors have no conflicts of interest to disclose.
References
- 1.Hinton E, Paradise J. Access to dental care in Medicaid: Spotlight on nonelderly adults Menlo Park, CA: The Henry J Kaiser Family Foundation; 2016. [Google Scholar]
- 2.Licata R, Paradise J. Oral health and low-income nonelderly adults: a review of coverage and access 2012:7798–7702.
- 3.Nasseh K, Vujicic M. Dental care utilization steady among working-age adults and children, up slightly among the elderly. Health Policy Institute Research Brief American Dental Association October 2016.
- 4.Decker SL, Lipton BJ. Do Medicaid benefit expansions have teeth? The effect of Medicaid adult dental coverage on the use of dental services and oral health. Journal of health economics 2015;44:212–225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.The Henry J. Kaiser Family Foundation. Status of State Action on the Medicaid Expansion Decision. State Health Facts 2018; https://www.kff.org/health-reform/state-indicator/state-activity-around-expanding-medicaid-under-the-affordable-care-act/. Accessed Dec. 1st, 2018.
- 6.Nasseh K, Vujicic M, O’Dell A. Affordable Care Act Expands Dental Benefits for Children But Does Not Address Critical Access to Dental Care Issues Health Policy Resources Center Research Brief 2013; https://www.ada.org/en/~/media/ADA/Science%20and%20Research/Files/HPRCBrief_0413_3. Accessed April 18, 2019.
- 7.Wehby GL, Lyu W. The Impact of the ACA Medicaid Expansions on Health Insurance Coverage through 2015 and Coverage Disparities by Age, Race/Ethnicity, and Gender. Health Services Research 2017. [DOI] [PMC free article] [PubMed]
- 8.Courtemanche C, Marton J, Ukert B, Yelowitz A, Zapata D. Impacts of the Affordable Care Act on Health Insurance Coverage in Medicaid Expansion and Non-Expansion States. National Bureau of Economic Research Working Paper Series 2016;No. 22182. [Google Scholar]
- 9.Kaestner R, Garrett B, Chen J, Gangopadhyaya A, Fleming C. Effects of ACA Medicaid expansions on health insurance coverage and labor supply. Journal of Policy Analysis and Management 2017;36(3):608–642. [DOI] [PubMed] [Google Scholar]
- 10.Nasseh K, Vujicic M. The impact of the affordable care act’s Medicaid expansion on dental care use through 2016. Journal of Public Health Dentistry 2017;77(4):290–294. [DOI] [PubMed] [Google Scholar]
- 11.Singhal A, Damiano P, Sabik L. Medicaid Adult Dental Benefits Increase Use Of Dental Care, But Impact Of Expansion On Dental Services Use Was Mixed. Health Affairs 2017;36(4):723–732. [DOI] [PubMed] [Google Scholar]
- 12.Courtemanche C, Marton J, Ukert B, Yelowitz A, Zapata D. Early impacts of the Affordable Care Act on health insurance coverage in Medicaid expansion and non‐expansion states. Journal of Policy Analysis and Management 2017;36(1):178–210. [DOI] [PubMed] [Google Scholar]
- 13.Logan HL, Catalanotto F, Guo Y, Marks J, Dharamsi S. Barriers to Medicaid participation among Florida dentists. Journal of health care for the poor and underserved 2015;26(1):154–167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mofidi M, Rozier RG, King RS. Problems with access to dental care for Medicaid-insured children: what caregivers think. American Journal of Public Health 2002;92(1):53–58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Lyu W, Wehby GL. The Impacts of the ACA Medicaid Expansions on Cancer Screening Use by Primary Care Provider Supply Medical Care Forthcoming 2018. [DOI] [PubMed]
- 16.Doty HE, Weech-Maldonado R. Racial/ethnic disparities in adult preventive dental care use. Journal of health care for the poor and underserved 2003;14(4):516–534. [DOI] [PubMed] [Google Scholar]
- 17.Vaidya V, Partha G, Karmakar M. Gender differences in utilization of preventive care services in the United States. Journal of women’s health 2012;21(2):140–145. [DOI] [PubMed] [Google Scholar]
- 18.Dye BA, Thornton-Evans G, Li X, Iafolla T. Dental caries and tooth loss in adults in the United States, 2011–2012 US Department of Health and Human Services, Centers for Disease Control and …; 2015. [Google Scholar]
- 19.HRSA Data Warehouse. Designated health professional shortage areas statistics. Bureau of Clinician Recruitment and Service, Health Resources and Services Administration (HRSA), US Department of Health & Human Services, as of January 2014 2014.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.