Abstract
Introduction
Low- and middle-income countries (LMICs) are continuing to experience a “triple burden” of disease - traumatic injury, non-communicable diseases (NCDs), and communicable disease with maternal and neonatal conditions (CD&Ms). The epidemiology of this triad is not well characterised and poses significant challenges to resource allocations, administration, and education of emergency care providers. The data collected in this study provide a comprehensive description of the emergency centre at Kenya's largest public tertiary care hospital.
Methods
This study is a retrospective chart review conducted at Kenyatta National Hospital of all patient encounters over a four-month period. Data were collected from financial and emergency centre triage records along with admission and mortality logbooks. Chief complaints and discharge diagnoses collected by specially trained research assistants were manually converted to standardised diagnoses using International Classification of Disease 10 (ICD-10) codes. ICD-10 codes were categorised into groups based on the ICD-10 classification system for presentation.
Results
A total of 23,941 patients presented to the emergency centre during the study period for an estimated annual census of 71,823. The majority of patients were aged 18-64 years (58%) with 50% of patients being male and only 3% of unknown sex. The majority of patients (61%) were treated in the emergency centre, observed, and discharged home. Admission was the next most common disposition (33%) followed by death (6%). Head injury was the overall most common diagnosis (11%) associated with admission.
Conclusions
Trends toward NCDs and traumatic diseases have been described by this study and merit further investigation in both the urban and rural setting. Specifically, the significance of head injury on healthcare cost, utilisation, and patient death and disability points to the growing need of additional resources at Kenyatta National Hospital for acute care. It further demonstrates the mounting impact of trauma in Kenya and throughout the developing world.
Keywords: Kenya, Head injury, Trauma, Triple burden of disease, Emergency medicine, Kenyatta National Hospital
African Relevance
-
•
This is a comprehensive description of the emergency centre at Kenya's largest public tertiary hospital
-
•
It adds to descriptions of trends of non-communicable and traumatic diseases in low- and middle-income countries
-
•
It describes epidemiology in Kenya, one of Africa's largest countries
Introduction
There have been major shifts in the disease patterns of low- and middle-income countries (LMICs) due to industrialisation and economic growth [1]. These countries are now experiencing a well described “triple burden” of disease: traumatic injury, non-communicable diseases (NCDs), and communicable disease with maternal and neonatal conditions (CD&Ms). This has led to major shifts in disease patterns where urbanisation is occurring at a higher rate than in other comparable regions, especially in East Africa [1,2]. However, the epidemiology of this triad of disease remains poorly characterised and poses significant challenges to resource allocation, administration, and education of health care providers. Historically, funds have been more weighted towards research and health system development in communicable diseases (e.g., HIV, tuberculosis and malaria), but that trend must now be re-evaluated [3,4]. Subsequently, these health systems are now tasked with caring for traumatically ill patients at a steadily increasing rate as the incidence of trauma, accidents, and injury rises [1,5]. Only upon acknowledgement of the significant burden of trauma and acute presentations of NCDs can resource allocation be accurately tailored to the true burden of disease and the development of emergency care systems be appropriately prioritised [6,7].
This study provides a comprehensive description of the acute care burden of disease in the emergency centre (EC) at Kenya's largest public tertiary hospital. This information can subsequently be used to drive the development of emergency care systems, redirect the focus of funding, and highlight areas in need of further research in acute care.
Methods
This is a single site study conducted at Kenyatta National Hospital (KNH). KNH is the largest public tertiary referral centre in Kenya. At the time of this study, there were three areas where emergency services were delivered at KNH: the emergency centre, the Paediatric Emergency Unit (PEU), and the Outpatient Unit for lower acuity patients. The emergency centre cares for those with medical or surgical emergencies over the age of twelve. The emergency centre also cares for children with burns or traumatic injuries age twelve or younger. The PEU provides medical care to children aged 0-12 years. As of 2017, the outpatient clinic was disbanded and these lower acuity patients are now either evaluated in the emergency centre or triaged to outpatient specialty clinics. The annual patient census of these combined areas in 2014 was 163,426, with 69,294 patients treated in the EC [8]. Medical care is provided by a combination of full-time and part-time medical officers and nurses along with nursing and emergency medical technician (EMT) students. A medical officer is a physician who has completed medical school and a one-year medical internship. These physicians do not have specialised emergency medicine training; rather, they have varying levels of experience and postgraduate training. Advanced Cardiac Life Support (ACLS), Advanced Trauma Life Support (ATLS), and a variable degree of disaster training has been completed by selected staff. Further, many nurses have completed a one-year emergency nursing certification course that is unique to KNH.
This study is a retrospective chart review of all patient encounters over a four-month period from 01 October 2014 to 31 January 2015. Data were collected from financial and EC triage records along with admission and mortality logbooks. Data collection was completed by trained research assistants (RAs) over a six-week period. Recorded parameters included medical record number, patient demographics (age, sex), presenting vital signs, and chief complaint on arrival, as well as admitting diagnosis or cause of death when applicable. Data were entered via electronic tablets into REDCap [9], a secure, online database, supported by the University of Minnesota [10]. Chief complaints and discharge diagnoses collected by specially trained RAs were manually converted to a standardised diagnosis using International Classification of Disease 10 (ICD-10) codes, as utilised in similar research settings [11,12]. Consensus classifications for both common and rare diagnoses were reached by group discussion under the oversight of the principal investigator.
All data are presented as “n” and a percentage by logbook (triage, admission and mortality). Data are presented by age groups (all, 0-4 years, 5-17 years, 18-64 years and ≥65 years). ICD-10 codes were categorised into groups based on the ICD-10 classification system for presentation. For comparison to previous literature, the subset of patients presenting with head injury and the incidence of each triple burden of disease [13] were described. STATA 15 (StataCorp., College Station, TX) was used for all analyses.
Results
A total of 23,941 patients presented to the EC during the four-month study period for an estimated annual census of 71,823. Triage records were available for 20,359 patients or 85% of all encounters. The majority of patients were aged 18-64 years (n=13,182; 58%) with 50% (n=10,075) of patients being male and only 3% (n = 684) of unknown sex. Table 1 outlines the demographics of all patients presenting to the EC.
Table 1.
Demographic characteristics of patients treated at Kenyatta National Hospital and included in the triage/observation, admission and mortality logbooks presented as n (%).
| All | Age groups (years) |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| 0-4 | 5-17 | 18-64 | ≥65 | |||||||
| Triage/observation | n=20,359 | n=949 | n=1,310 | n=13,802 | n=1,594 | |||||
| Male | 10,075 | (50) | 524 | (57) | 772 | (59) | 6,644 | (48) | 867 | (54) |
| Female | 9,567 | (47) | 375 | (40) | 521 | (40) | 7,022 | (51) | 704 | (44) |
| Missing | 684 | (3) | 28 | (3) | 17 | (1) | 133 | (1) | 23 | (1) |
| Admission | n=7,939 | n=577 | n=666 | n=5,382 | n=778 | |||||
| Sex | n | (%) | n | (%) | n | (%) | n | (%) | n | (%) |
| Male | 4830 | (61) | 364 | (63) | 426 | (64) | 3,226 | (60) | 454 | (58) |
| Female | 3076 | (39) | 205 | (36) | 240 | (36) | 2,145 | (40) | 321 | (41) |
| Missing | 33 | (0) | 8 | (1) | 0 | (0) | 11 | (0) | 3 | (0) |
| Mortality | n=1,340 | n=80 | n=67 | n=823 | n=163 | |||||
| Sex | n | (%) | n | (%) | n | (%) | n | (%) | n | (%) |
| Male | 918 | (69) | 34 | (43) | 46 | (69) | 571 | (69) | 98 | (60) |
| Female | 407 | (31) | 37 | (46) | 20 | (30) | 252 | (31) | 65 | (40) |
| Missing | 7 | (1) | 9 | (11) | 1 | (1) | 0 | (0) | 0 | (0) |
The majority of patients (61%) were presumed to be treated in the EC, observed, and discharged home. This percentage is derived by omission from the other data sets and therefore slightly subject to error. Admission was the next most common disposition (33%) followed by death in the EC (6%). The percentage of patients admitted varied across age groups (range 40-60%). Patients who were dead on arrival to the EC and underwent attempted resuscitation were included in this study (n=191).
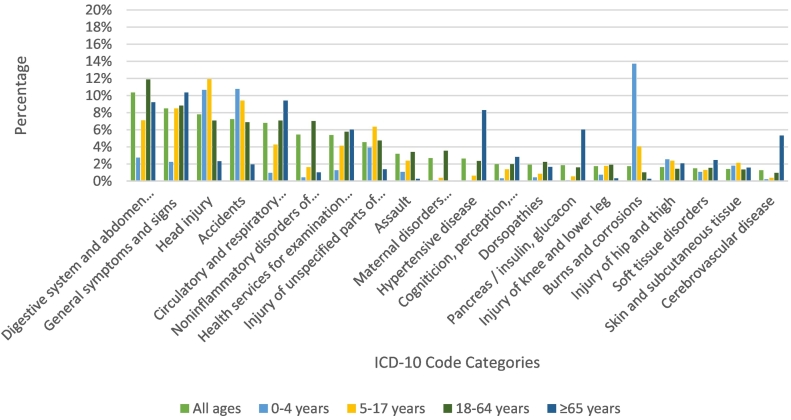
The top 20 ICD-10 diagnoses for the available triage data are listed by percentage for patients presenting to triage/observation (n=20,359) in Fig. 1. These are further divided by the top 20 diagnoses for each age group. The most common overall presenting diagnosis was “digestive system and abdominal complaints” (10%). Head injury (8%) and general signs and symptoms (8%) make up the second most common chief complaints. Accidents (7%), circulatory and respiratory symptoms (7%), non-inflammatory disorders of the female genital tract (5%), encounters for health services evaluation (5%), injury to unspecified part of the body (5%), assault (3%), and other maternal disorders (3%) make up the top ten presenting diagnoses and 61% of all presenting complaints.
Fig. 1.
Top 20 ICD-10 diagnosis categories by age for patients included in the triage/observation logbook
Note: ICD-10, International Classification of Disease 10
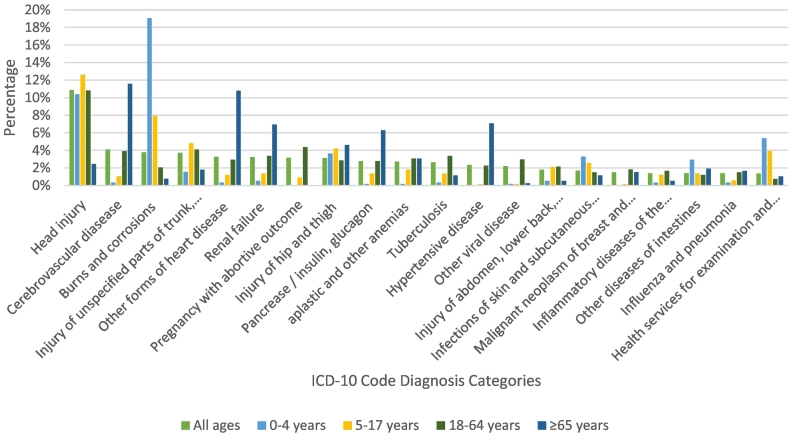
A total of 7,939 patients required admission during our study time period with an estimated annual admission rate of 33% (Fig. 2). Head injury was the overall most common diagnosis (11%) associated with admission and was the leading admission diagnosis in both the 5-17 and 18-64-year age groups. Among patients aged 0-4 years (n=577), burns and corrosions (19%) were the most common diagnoses associated with admission. Patients 65 years and older (n=778) were most commonly admitted due to non-communicable illnesses: cerebrovascular disease (12%), heart disease (11%), hypertensive disease (7%), renal failure (7%), and endocrine disorders (6%).
Fig. 2.
Top 20 ICD-10 diagnosis categories by age for patients included in the admission logbook
Note: ICD-10, International Classification of Disease 10
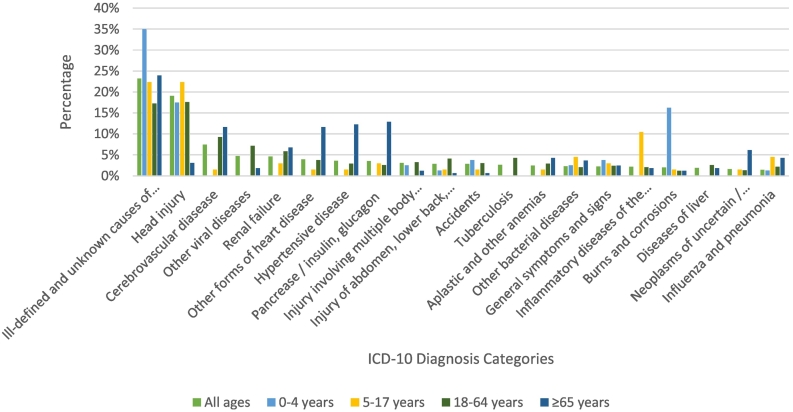
Mortality logbook information is described in Fig. 3. A total of 1,340 patients died while in the EC during our study period. Of these patients, 191 were dead on arrival to the EC and underwent attempted resuscitation. With the exclusion of patients who died from an ill-defined or unknown aetiology (23%), head injury was the most common diagnosis associated with death (19%). This held true for all age categories except patients aged 65 or older where NCDs made up the majority of diagnoses associated with death in the EC.
Fig. 3.
Top 20 ICD-10 diagnosis categories by age for patients included in the mortality logbook
Note: ICD-10, International Classification of Disease 10
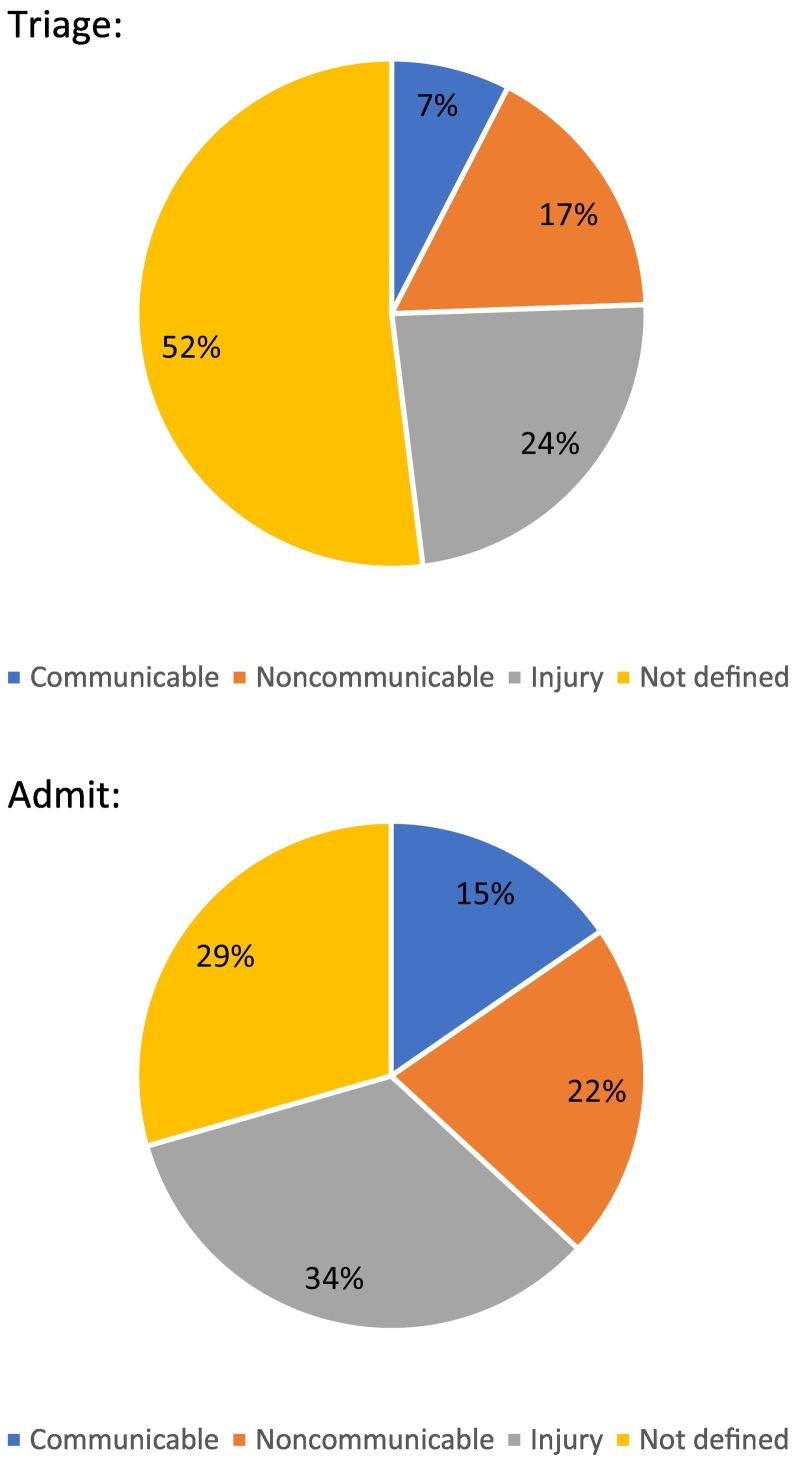
Fig. 4 shows the ICD-10 diagnoses by category (CD&Ms, NCDs, injury, and undefined) for both the triage and admitted populations. The most common category for both groups was traumatic injury (24% and 34%, respectively). This was followed by NCDs (17% and 21%, respectively), and CD&Ms (15% and 8%, respectively). Of note, these data sets have a significant proportion of undefined diagnoses (52% and 29%, respectively).
Fig. 4.
Type of disease: communicable, non-communicable, injury and not defined/seen in triage/observation and admission logbooks (n=%)
Head injury diagnoses are further described regarding mode of injury, sex of the presenting patient, and age of the patient in Table 2. A total of 1,587 patients presented to observation/triage during the study period and were diagnosed with head injury. Eighty percent (n=1,263) of these patients were male with only 3% (n=44) of unknown sex. Among patients with a known mechanism of injury, the most commonly seen was motorised vehicle accidents (n=287; 18%), followed by assault (n=228; 14%), and fall (n=98; 6%). Of the patients requiring admission, 11% carried the primary diagnosis of head injury (n=864). Of those presenting with head injury 16% (n=256) died in the EC.
Table 2.
Gender and trauma type of patients diagnosed with head injury after evaluation at Kenyatta National Hospital and included in the triage/observation, admission and mortality logbooks presented as n (%).
| All | Age groups (years) |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| 0-4 | 5-17 | 18-64 | ≥65 | |||||||
| Triage/observation | n=1,587 | n=101 | n=156 | n=973 | n=47 | |||||
| Sex | n | (%) | n | (%) | n | (%) | n | (%) | n | (%) |
| Male | 1,263 | (80) | 60 | (59) | 109 | (70) | 821 | (84) | 23 | (62) |
| Female | 280 | (18) | 39 | (39) | 45 | (29) | 144 | (15) | 13 | (35) |
| Missing | 44 | (3) | 2 | (2) | 2 | (1) | 8 | (1) | 1 | (3) |
| Trauma mechanism | n | (%) | n | (%) | n | (%) | n | (%) | n | (%) |
| Motorised vehicle | 287 | (18) | 6 | (6) | 23 | (15) | 176 | (18) | 4 | (11) |
| Assault | 228 | (14) | 5 | (5) | 14 | (9) | 149 | (15) | 3 | (8) |
| Fall | 98 | (6) | 28 | (28) | 24 | (15) | 30 | (3) | 4 | (11) |
| Firearm | 7 | (0) | 0 | (0) | 0 | (0) | 4 | (0) | 0 | (0) |
| Shock or burn | 1 | (0) | 0 | (0) | 0 | (0) | 1 | (0) | 0 | (0) |
| Admission | n=864 | n=60 | n=84 | n=582 | n=19 | |||||
| Sex | n | (%) | n | (%) | n | (%) | n | (%) | n | (%) |
| Male | 730 | (84) | 37 | (62) | 58 | (69) | 519 | (89) | 14 | (74) |
| Female | 131 | (15) | 23 | (38) | 26 | (31) | 62 | (11) | 5 | (26) |
| Missing | 3 | (0) | 0 | (0) | 0 | (0) | 1 | (0) | 0 | (0) |
| Mortality | n=256 | n=14 | n=15 | n=145 | n=5 | |||||
| Sex | n | (%) | n | (%) | n | (%) | n | (%) | n | (%) |
| Male | 237 | (93) | 7 | (50) | 14 | (93) | 139 | (96) | 5 | (100) |
| Female | 19 | (7) | 7 | (50) | 1 | (7) | 6 | (4) | 0 | (0) |
| Missing | 0 | (0) | 0 | (0) | 0 | (0) | 0 | (0) | 0 | (0) |
Discussion
This study aimed to describe the acute care burden of disease at the EC of Kenya's largest public hospital. It revealed that traumatic injuries, NCDs, and CD&Ms are all prominent reasons for acute care presentation and admission. This is in contrast to prior data regarding disease patterns in the population at large. Furthermore, it shows high patient volumes, high levels of patient acuity, and high rates of admission at KNH. Of particular interest is the prominent role of head injuries among patients seeking care, those that died in the EC, and those being admitted. This is an important epidemiological finding that merits both current consideration and further evaluation.
Historically, funds have been more heavily weighted towards research and health system development in CD&Ms (e.g., HIV, tuberculosis and malaria) [4,5]. This “vertical approach” of prioritising important diseases over broader health system initiatives has neglected emergency care systems in developing countries. While CD&Ms may still represent the most common cause of death, premature death, and disability in Kenya, this study and other recently published data show that the majority of hospital presentations were related to NCDs and traumatic injuries [13,21]. The difference in this identified burden of acute care relative to broader disease patterns could be due to the urban and tertiary care setting rather than the majority rural setting of Kenya. Data from the same time period seem to confirm the predominance of infectious disease in the acute care rural setting in Kenya [22]. The development of a national acute care data set is crucial to addressing this discrepancy and to understanding disease patterns and prevalence, access to care, and treatment. PROJECT 47, a nation-wide Kenyan public-private partnership, is assessing capacity and access to emergency care in the 47 counties in Kenya with the goal of reaching a universal emergency care coverage system and addressing the longstanding deficit created by the historical focus on CD&Ms. Additionally, the project has the potential to fill information gaps and provide a complete data set on emergency epidemiology of disease [23].
The development of PROJECT 47 and the increased interest in acute care delivery in Kenya could not be timelier. The EC at KNH sees a large number of patients with an estimated annual census of 71,823 patients. The high level of acuity is reflected by an admission rate of 33% and a mortality rate of 6%. However, different patient populations presenting to the EC demonstrate different patterns of illness and injury. Among patients over the age of 65, the most common presentations were for NCDs, such as heart disease or diabetes. These presenting diagnoses accounted for all of the top ten diagnoses seen in the triage cohort in this age group. Further, NCDs accounted for eight of the top diagnoses associated with admission. NCDs are projected to become an increasing cause of disease burden as the number of NCD-related deaths has risen worldwide in all regions since 2000 [24]. Options for treatment and prevention of NCDs are poorly accessible to Kenyans especially in rural areas due to the cost of screening and treatment as well as limited access to care [25]. This trend in rising NCDs provides a framework for both further investigation and targeted intervention.
A different pattern is seen among children under five years old whose most common triage diagnosis was burns and corrosions (14%). Burns in this age category are most commonly related to flame burns or scalds with hot fluids [26,27]. Further, low level of education, use of kerosene for cooking, and lack of knowledge of burn injury prevention and fire safety are studied risk factors related to burn injuries at KNH [26]. Of note, patients under the age of five were incompletely evaluated in this cohort due to being evaluated in the Paediatric Emergency Unit (PEU). Paediatric patients under this age with medical complaints are triaged directly in the PEU and are missing from the data set.
Traumatic injury accounted for three of the top four diagnoses related to admission and 34% (n=2536) of patients requiring admission at KNH. Notably, head injury is the leading diagnosis associated with admission and second leading diagnosis associated with death in patients presenting to the EC. This finding highlights the rising need for tertiary care centres with acute care capabilities and a target ripe for primary, secondary and tertiary public health interventions. The continued urbanisation occurring across LMICs along with the patterns of disease described above foreshadows the inevitable increase in traumatic illness and underscores the importance of emergency medicine research, education, public health interventions and systems development [1,2].
This study shows that the true burden of disease seen at KNH is not limited to CD&Ms but has a much broader base that includes NCDs and traumatic injury. Recognising this fact will allow for the redirection of attention and funding needed for improvement in patient care and outcomes.
Head injury was found to be the leading diagnosis related to admission. The significance of this on healthcare utilisation and subsequently on cost is tremendous. The Healthcare Cost and Utilization Project found that admissions related to traumatic brain injury (TBI) were both longer and more costly in comparison to non-TBI injuries [28]. Although we do not know the level of care required for those admitted for head injury in our cohort, other studies have been done to examine this. A recent study in South Africa found that 20% of patients admitted for head injury were classified as moderate (10%) to severe (10%). All patients categorised as severe met criteria for advanced airway placement and intensive care unit (ICU) admission, however, only 33% of those patients were admitted to the ICU due to limited availability of equipment and resources [29]. They also found the mortality risk to be significantly higher in those patients admitted to the general ward as compared to the ICU. The study highlights the deficit of adequate critical care resources to care for this burden of disease in LMICs [29,30].
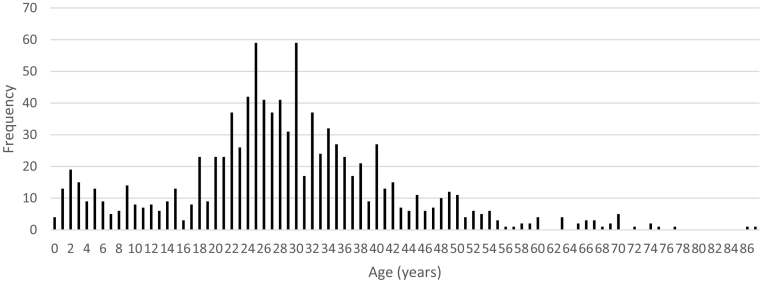
Head injury is a disease largely of the male, working aged population [29,31., 32., 33.]. Our data showed that 80% of all patients presenting to the EC with head injury were male. Of these men, 65% (n=821) were between the age of 18-64 years (Fig. 5). Further, 58% (n=731) of these men were between the age of 18-45 years. Male risk of TBI is nearly fourfold that of female [31]. This is in contrast to the ratios in the United States of 2.2:1 and in China of 2.5:1 [34,35]. From the available data, motor vehicle accidents, assaults, and falls made up nearly 40% of injury mechanisms related to TBI. Of note, a portion of data regarding mechanism of injury was missing from logbooks, rendering this data incomplete. A recent Ethiopian study found very similar results regarding the epidemiology of head injured patients with a predominance of males (87%) and the mechanism of injury of motor vehicle accidents (41%) [33].
Fig. 5.
Frequency of head trauma among males included in the triage/observation logbook by age (in years)
Identifying head injury as the leading cause of morbidity and mortality reveals its potential impact on Kenyan culture, economy, and society. Of patients who survive such injuries, the sequelae of TBI can be life changing. A diagnosis of TBI carries a 2.5-time increased risk of death along with a six-year reduction in life expectancy when compared to the general population in high income countries [32]. These risks have not been calculated or well estimated in LMICs and could potentially be higher. Patients suffering a TBI have also been shown to have a higher risk of developing psychiatric symptoms and illness; most commonly hostility, depression, and anxiety. Low social functioning, low vocational functioning, and lack of independence are all correlated to psychiatric sequelae from head injury [36]. Head injury trends in this specific age population of men could have detrimental effects on Kenyan society, the work force, and the economy in the future.
Thus far, policy initiatives directed towards the prevention of TBIs have manifested as road traffic laws and regulations. For example, speed, helmet, seat-belt, and drink-driving laws have been implemented. The exponential increase in use of motorcycles in LMICs for transportation has been accompanied by a similar rise in motorcycle related deaths [37]. Helmet use is widely known to reduce the risk of head injury in motorcycle related motor vehicle accidents, however, despite this fact, compliance with helmet laws are dismal. Less than 40% of motorcyclists wear a helmet while traveling and there has not been a significant increase in helmet use following implementation of stricter regulations [38]. Issues with compliance and access to both helmets and seat-belts are limiting the impact of these regulations on improved safety.
In addition to preventive efforts, improvement of TBI care from pre-hospital, through EC care, hospitalisation to discharge, and rehabilitation should be addressed. Standardisation of pre-hospital provider training is on the horizon in Kenya and will greatly improve care delivered in the pre-hospital setting [39]. Pre-hospital transportation and equipment needs along with gaps in hospital staffing and equipment are all areas that require further research to improve TBI care. Information is also needed to appreciate outcomes and needs of TBI patients after discharge from facilities such as KNH. As of this time, the burden of post-hospital care is left to families and communities because there are no brain injury rehabilitation centres available to patients following discharge from KNH. This is also true for patients following discharge from private sector hospitals [40].
This study included patients presenting to a tertiary referral centre in the metropolitan hub of Nairobi, Kenya. KNH is a government owned and staffed facility and cares for a mix of patients, the majority of whom are in a lower socioeconomic group [14]. The surrounding private for-profit hospitals in Nairobi see patients from a higher socioeconomic group who could be suffering from different disease patterns [15,16]. For a broader view of the epidemiology of illness and injury, future studies should include data from surrounding hospitals in Nairobi as well as the larger number of rural care centres in Kenya [2,17].
A significant amount of data are missing from record books regarding mechanism of injury which is a known limitation of any retrospective study. Despite the incomplete data, our results align with similar studies reported in the literature. Two recent prospective studies performed in Kenya looking at the epidemiology of injury both found a male majority in patients presenting with injury, as well as road traffic injury as the most common mechanism of injury [18,19]. Another preliminary study points to a high volume of trauma in a rural setting in Kenya as well. [20] Although these studies are from more recent data sets, their results are consistent with our findings, suggesting consistency in data trends over this short time gap. The delay in presentation of our data is largely secondary to the lengthy time required for re-coding and electronic conversion of data.
This study shows that the acute care burden of disease in the EC at KNH is not limited to CD&Ms, which have historically been the target of healthcare investments. Rather, there is a large burden of NCDs, particularly among the elderly, and a large burden of traumatic injury, particularly among the male, working-age population. An especially noteworthy finding of this study is the prominence of patients with head injury, which has broader public health and policy implications. Additional research on the national acute care burden of disease, including rural areas, is needed to better understand both population-level trends in disease epidemiology as well as the epidemiology of acute care. This in turn can lead to improved resource allocation, provider training, and targeted public health initiatives.
Dissemination of results
Information from this study was shared with staff at Kenyatta National Hospital via the Monthly Disaster and Emergency Care Bulletin. Further, the results have been shared with the KNH research office per their protocol. An abstract from this study was also presented at the International Conference of Emergency Medicine in South Africa in 2016.
Author Contribution
Authors contributed as follow to the conception or design of the work; the acquisition, analysis, or interpretation of data for the work; and drafting the work or revising it critically for important intellectual content: JGM contributed 25%; JS contributed 10%; KE and KH contributed 7.5% each; AW, PW, SZ, DB, WD, JS, YA and OO each contributed 5%; and IBKM, SD, VM and AM each contributed 2.5%. All authors approved the version to be published and agreed to be accountable for all aspects of the work.
Declaration of Competing Interest
The authors declare no conflicts of interest.
References
- 1.World Health Organization . 2015. Injuries and violence [Internet]. Health in 2015: From MDGs to SDGs; pp. 171–188.http://www.who.int/gho/publications/mdgs-sdgs/en/ Available from: [Google Scholar]
- 2.Assamala . World Heal Organ; 2014. African Regional Health Report 2014; p. 187.http://www.who.int/intellectualproperty/documents/thereport/ENPublicHealthReport.pdf [Internet]. Available from: [Google Scholar]
- 3.Nell V., Brown D.S.O. Epidemiology of traumatic brain injury in Johannesburg-II. Morbidity, mortality and etiology. Soc Sci Med. 1991;33(3):289–296. doi: 10.1016/0277-9536(91)90363-h. [DOI] [PubMed] [Google Scholar]
- 4.Isaakidis P., Swingler G.H., Pienaar E., Volmink J., Ioannidis J.P. Relation between burden of disease and randomised evidence in sub- Saharan Africa: survey of research. BMJ. 2002;324(7339):702. doi: 10.1136/bmj.324.7339.702. http://www.ncbi.nlm.nih.gov/pubmed/11909786 [Internet]. Available from. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gosselin R.A. The increasing burden of injuries in developing countries: Direct and indirect consequences. Techniques in Orthopaedics. 2009;24:230–232. [Google Scholar]
- 6.Laxminarayan R., Mills A.J., Breman J.G., Measham A.R., Alleyne S., Claeson M. Advancement of global health: key messages from the Disease Control Priorities Project. Lancet. 2006;367(9517):1193–1208. doi: 10.1016/S0140-6736(06)68440-7. https://www.scopus.com/inward/record.uri?eid=2-s2.0-33645966537&partnerID=40&md5=f57b006f2401ad95cd003a5412eb3e76 [Internet]. Available from. [DOI] [PubMed] [Google Scholar]
- 7.MacKenzie E.J., Rivara F.P., Jurkovich G.J., Nathens A.B., Frey K.P., Egleston B.L. A National Evaluation of the Effect of Trauma-Center Care on Mortality. N Engl J Med. 2006;354(4):366–378. doi: 10.1056/NEJMsa052049. http://www.nejm.org/doi/abs/10.1056/NEJMsa052049 Internet. Available from. [DOI] [PubMed] [Google Scholar]
- 8.Maina R. 2015. Health Information Department-Kenyatta National Hospital. Personal Communication. [Google Scholar]
- 9.Harris P.a., Taylor R., Thielke R., Payne J., Gonzalez N., Conde J.G. Research Electronic Data Capture (REDCap) - A metadata driven methodology and workflow process for providing translational research informatict support. J Biomed Inform. 2009;42(2):377–381. doi: 10.1016/j.jbi.2008.08.010. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2700030/ [Internet]. Available from. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.University of Minnesota. Clinical and Translational Science Institute. 2016.
- 11.House D.R., Nyabera S.L., Yusi K., Rusyniak D.E. Descriptive study of an emergency centre in Western Kenya: Challenges and opportunities. African J Emerg Med. 2014;4(1):19–24. [Google Scholar]
- 12.World Health Organisation . International Statistical Classification of Diseases and Related Health Problems 10th Revision (ICD-10)-2015-WHO Version for 2015. 2015. ICD-10 Version: 2015.http://apps.who.int/classifications/icd10/browse/2015/en#/H54 [Internet]. p. Chapter VII. Available from: [Google Scholar]
- 13.Myers JG, Hunold KM, Ekernas K, Wangara A, Maingi A, Mutiso V, et al. Patient characteristics of the Accident and Emergency Department of Kenyatta National Hospital, Nairobi, Kenya: a cross-sectional, prospective analysis. BMJ Open [Internet]. 2017;7(10):e014974. Available from: http://bmjopen.bmj.com/lookup/doi/10.1136/bmjopen-2016-014974 [DOI] [PMC free article] [PubMed]
- 14.Services M., Health P., Macro I.C.F. Kenya Service Provision Assessment Survey 2010 [SPA17] Public Health. 2010 Chapter 2 and 3, pg 13-35. [Google Scholar]
- 15.Chuma J., Maina T., Ataguba J. Does the distribution of health care benefits in Kenya meet the principles of universal coverage? BMC Public Health. 2012;12(1) doi: 10.1186/1471-2458-12-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Munge K., Briggs A.H. The progressivity of health-care financing in Kenya. Health Policy Plan. 2014;29(7):912–920. doi: 10.1093/heapol/czt073. [DOI] [PubMed] [Google Scholar]
- 17.Kobusingye O. Injury patterns in rural and urban Uganda. Inj Prev. 2001;7(1):46–50. doi: 10.1136/ip.7.1.46. http://ip.bmj.com/cgi/doi/10.1136/ip.7.1.46 Internet. Available from. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Botchey I.M.J., Hung Y.W., Bachani A.M., Saidi H., Paruk F., Hyder A.A. Understanding patterns of injury in Kenya: Analysis of a trauma registry data from a National Referral Hospital. Surgery. 2017;162(6S):S54–S62. doi: 10.1016/j.surg.2017.02.016. [DOI] [PubMed] [Google Scholar]
- 19.Botchey I.M., Hung Y.W., Bachani A.M., Paruk F., Mehmood A., Saidi H. Epidemiology and outcomes of injuries in Kenya: A multisite surveillance study. Surg (United States) 2017;162(6):S45–S53. doi: 10.1016/j.surg.2017.01.030. [DOI] [PubMed] [Google Scholar]
- 20.Hart D., Myers J.G., Kilonzo S., Wachira B., Hunold K., Davis W. An Epidemiologic Analysis of Nanyuki District Teaching and Referral Hospital, Laikipia, Kenya. Acad Emerg Med. 2018;25:8–284. Conference Abstract. [Google Scholar]
- 21.Hyder A.A., Wunderlich C.A., Puvanachandra P., Gururaj G., Kobusingye O.C. The impact of traumatic brain injuries: A global perspective. NeuroRehabilitation. 2007;22(5):341–353. http://search.ebscohost.com/login.aspx?direct=true&db=cin20&AN=2009753392&lang=es&site=ehost-live [Internet]. Available from. [PubMed] [Google Scholar]
- 22.Burke T.F., Hines R., Ahn R., Walters M., Young D., Anderson R.E. Emergency and urgent care capacity in a resource-limited setting: An assessment of health facilities in western Kenya. BMJ Open. 2014;4(9) doi: 10.1136/bmjopen-2014-006132. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Emergency Medicine Kenya Foundation. Project 47: Emergency Departments in 47 Counties.
- 24.WHO . World Health; 2014. Global status report on noncommunicable diseases 2014; p. 176. [Google Scholar]
- 25.Subramanian S., Gakunga R., Kibachio J., Gathecha G., Edwards P., Ogola E. Cost and affordability of non-communicable disease screening, diagnosis and treatment in Kenya: Patient payments in the private and public sectors. PLoS One. 2018;13(1) doi: 10.1371/journal.pone.0190113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.W J.K., K. M. Risk factors for burn injuries and fire safety awareness among patients hospitalized at a public hospital in Nairobi, Kenya: A case control study. Burns. 2018;44(4):962–968. doi: 10.1016/j.burns.2017.11.007. http://www.elsevier.com/locate/burns%0Ahttp://ovidsp.ovid.com/ovidweb.cgi?T=JS&PAGE=reference&D=emexb&NEWS=N&AN=620407734 [Internet]. Available from: [DOI] [PubMed] [Google Scholar]
- 27.Dale E.L., Mueller M.A., Wang L., Fogerty M.D., Guy J.S., Nthumba P.M. Epidemiology of operative burns at Kijabe Hospital from 2006 to 2010: Pilot study of a web-based tool for creation of the Kenya Burn Repository. Burns. 2013;39(4):788–795. doi: 10.1016/j.burns.2012.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Russo C.A., Steiner C. Healthcare Cost and Utilization Project (HCUP) Statistical Briefs. 2006. Hospital admissions for traumatic brain injuries, 2004: Statistical Brief #27.http://www.ncbi.nlm.nih.gov/pubmed/21938856 [Internet]. Available from: [PubMed] [Google Scholar]
- 29.Jerome E., Laing G.L., Bruce J.L., Sartorius B., Brysiewicz P., Clarke D.L. An audit of traumatic brain injury (TBI) in a busy developing-world trauma service exposes a significant deficit in resources available to manage severe TBI. South African Med J. 2017;107(7):621–625. doi: 10.7196/SAMJ.2017.v107i7.10562. [DOI] [PubMed] [Google Scholar]
- 30.Kwizera A., Dünser M., Nakibuuka J. National intensive care unit bed capacity and ICU patient characteristics in a low income country. BMC Res Notes. 2012;5 doi: 10.1186/1756-0500-5-475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Emejulu J.K.C., Isiguzo C.M., Agbasoga C.E.O.C. Traumatic brain injury in the accident and emergency department of a tertiary hospital in Nigeria. East Cent African J Surg. 2010;15(2):28–38. http://www.bioline.org.br/request?js10031 [Internet]. Available from: [Google Scholar]
- 32.Ventura T., Harrison-Felix C., Carlson N., DiGuiseppi C., Gabella B., Brown A. Mortality After Discharge From Acute Care Hospitalization With Traumatic Brain Injury: A Population-Based Study. Arch Phys Med Rehabil. 2010;91(1):20–29. doi: 10.1016/j.apmr.2009.08.151. [DOI] [PubMed] [Google Scholar]
- 33.Landes M., Venugopal R., Berman S., Heffernan S., Maskalyk J., Azazh A. Epidemiology, clinical characteristics and outcomes of head injured patients in an Ethiopian emergency centre. African J Emerg Med. 2017;7(3):130–134. doi: 10.1016/j.afjem.2017.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Frost R.B., Farrer T.J., Primosch M., Hedges D.W. Prevalence of traumatic brain injury in the general adult population: A meta-analysis. Neuroepidemiology. 2013;40:154–159. doi: 10.1159/000343275. [DOI] [PubMed] [Google Scholar]
- 35.Zhao Y. Du, Wang W. Neurosurgical trauma in People's Republic of China. World Journal of Surgery. 2001;25:1202–1204. doi: 10.1007/s00268-001-0082-8. [DOI] [PubMed] [Google Scholar]
- 36.Hoofien D., Gilboa A., Vakil E., Donovick P.J., Hoofien D., Gilboa A. Traumatic brain injury (TBI) 10 - 20 years later: a comprehensive outcome study of psychiatric symptomatology, cognitive abilities and psychosocial functioning. Brain Inj. 2009;9052:189–209. doi: 10.1080/026990501300005659. https://www.researchgate.net/profile/Eli_Vakil/publication/12071540_Traumatic_brain_injury_TBI_10-20_years_later_A_comprehensive_outcome_study_of_psychiatric_symptomatology_cognitive_abilities_and_psychosocial_functioning/links/0fcfd50be5638c5a84000000.pd [Internet]. (November 2016). Available from: [DOI] [PubMed] [Google Scholar]
- 37.World Health Organization Motorcycle-related road traffic crashes in Kenya Facts & figures [Internet]. violence_Injury_ prevention. 2011. http://www.who.int/violence_injury_prevention/road_traffic/countrywork/factsheet_kenya.pdf Available from:
- 38.Bachani A.M., Hung Y.W., Mogere S., Akunga D., Nyamari J., Hyder A.A. Helmet wearing in Kenya: prevalence, knowledge, attitude, practice and implications. Public Health. 2017;144:S23–S31. doi: 10.1016/j.puhe.2016.12.005. [DOI] [PubMed] [Google Scholar]
- 39.Nicholson B., McCollough C., Wachira B., Mould-Millman N.K. Emergency medical services (EMS) training in Kenya: Findings and recommendations from an educational assessment. African J Emerg Med. 2017;7(4):157–159. doi: 10.1016/j.afjem.2017.06.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Kinyanjui B. Traumatic Brain Injury in Kenya. SAGE Open [Internet]. 2016;6(1):215824401663839. Available from: http://journals.sagepub.com/doi/10.1177/2158244016638392