Key Points
Question
Is obstructive sleep apnea associated with the risk of affective disorder, such as depression and anxiety?
Findings
In this cohort study using a Korean nationwide representative sample of 2004 through 2006 data on 985 individuals, the overall incidence of affective disorder, such as depression and anxiety, during a 9-year follow-up was higher in the obstructive sleep apnea group than in the comparison group. The adjusted hazard ratio for development of depression and anxiety in patients with obstructive sleep apnea appears to be higher in female than in male patients with obstructive sleep apnea.
Meaning
Clinicians may consider taking specific precautions to reduce the risks of development of depressive and anxiety disorders among patients with obstructive sleep apnea.
Abstract
Importance
Obstructive sleep apnea (OSA) is a common subtype of sleep breathing disorder; however, the association between OSA and the psychological health of affected individuals has not been fully evaluated.
Objective
To investigate the association between OSA and development of affective disorders.
Design, Setting, and Participants
This study used a nationwide representative cohort sample from the Korea National Health Insurance Service–National Sample Cohort database comprising data from 1 025 340 patients. The study included 197 patients with OSA diagnosed between January 2004 and December 2006 and 780 individuals without OSA who were matched using propensity score matching. Data were analyzed from September 28, 2018, to March 30, 2019.
Main Outcomes and Measures
Affective disorder events over a 9-year follow-up period. Kaplan-Meier survival curves with log-rank tests and Cox proportional hazards regression models were used to calculate cumulative incidence and hazard ratios (HRs) of affective disorders for each group.
Results
Of the total population of 985 (860 male [87.3%], 540 [54.8%] were aged <45 years), the incidences per 1000 person-years of affective disorders were 49.57 and 27.18 in the OSA and comparison groups, respectively. A total of 1371.7 person-years in the OSA group and 6328.6 person-years in the comparison group were evaluated for affective disorder events. After adjustment for sociodemographic factors (age, residential area, and household income), disability, and comorbidities, the adjusted HRs for patients with OSA developing affective disorders in patients with OSA during the 9-year follow-up period was 2.04 (95% CI, 1.53-2.70). In a subgroup analysis, the adjusted HRs for patients with OSA who developed depressive and anxiety disorders were 2.90 (95% CI, 1.98–4.24) and 1.75 (95% CI, 1.26–2.44), respectively. Moreover, female patients with OSA had a significant likelihood of prospective development of depression and anxiety (adjusted HR for depression, 3.97 [95% CI, 1.54-10.19]; adjusted HR for anxiety, 2.42 [95% CI, 1.17-5.02]) compared with male patients with OSA (adjusted HR for depression, 2.74 [95% CI, 1.80-4.17]; adjusted HR for anxiety, 1.64 [95% CI, 1.13-2.39]).
Conclusions and Relevance
This observational study using nationwide data suggests that OSA is associated with an increased incidence of affective disorder, such as depression and anxiety. Further studies appear to be needed to confirm our findings and, if validated, then studies are needed to explore the nature of the observed association, including potential causality, between OSA and affective symptoms.
This cohort study uses a Korean nationwide database to investigate whether obstructive sleep apnea is associated with the development of depression and anxiety.
Introduction
Obstructive sleep apnea (OSA) is a serious, potentially life-threatening condition characterized by repeated cessation of breathing during sleep associated with complete or partial airway obstruction. Episodes of airway obstruction induce nocturnal hypoxemia, hypercapnia, and sleep fragmentation. Numerous studies have reported that OSA can cause or exacerbate severe major organ disorders, including cardiovascular disease, metabolic syndrome, and neurocognitive deterioration.1,2,3 Obstructive sleep apnea is also associated with asthma exacerbation, open-angle glaucoma, and erectile dysfunction.4,5,6 The most common clinical presentations of OSA are loud snoring; breathing pauses observed by the bed partner; and excessive daytime sleepiness.7,8 Other symptoms include choking or gasping, restless sleep, morning headache, morning sore throat, excessive fatigue, impaired concentration, memory loss, and mood disturbances.9,10,11 For these reasons, OSA may have consequences for daytime functioning and may be associated with increases in crashes by motor vehicle while in traffic and decreases in work productivity.12,13,14 While the physical components of OSA have been extensively investigated, the psychological aspects of OSA, including the presence of affective disorders, such as depressive disorder and anxiety disorder, have not been fully evaluated to date.
Although the underlying factors in OSA associated with affective disorders have not been fully elucidated, these disorders are prevalent among people with OSA.15,16,17,18,19,20,21,22 Recent systematic reviews and meta-analyses have reported an increased OSA prevalence in patients who are diagnosed with depressive and anxiety disorders.16,17,22 In addition, 1 large cohort study showed a higher prevalence of psychiatric comorbidities, such as mood disorders and anxiety, in patients with OSA than in patients without OSA.15 Another cohort study described the prospective association between OSA and subsequent depressive disorders within 1 year of OSA onset.18 Moreover, numerous studies have reported that psychiatric comorbidities in patients with OSA may adversely affect the quality of life of these patients and their adherence to continuous positive airway pressure therapy.19,20,21 However, the association between OSA and affective disorders is not yet fully understood.
Therefore, the present study investigated the association between OSA and the prospective risk of developing affective disorders, such as depressive and anxiety disorders, using a nationwide representative cohort sample of 1 025 340 adults from the National Sample Cohort 2002-2013 of the Korea National Health Insurance Service (KNHIS-NSC) in South Korea. Because this nationwide population-based data set contains information on the use of medical services history of more than 1 million Koreans, we were able to examine the association between OSA and the risk for affective disorder while adjusting for clinical and demographic factors.
Methods
National Sample Cohort
The present study used a nationwide representative sample from the 1 025 340 adults from the KNHIS–NSC in South Korea from 2002-2013 (eAppendix in the Supplement). This data set accounted for approximately 2.2% of the South Korean population in 2002. Stratified random sampling of the 46 million inhabitants of South Korea in 2002 was performed using 1476 strata, including age (18 groups per 5 years old), sex (2 groups), and income level (41 groups: 40 health insurance groups and 1 medical aid beneficiary). Additionally, the KNHIS–NSC contains data on all health services, including hospital visits (inpatient and outpatient), medical procedures, drug prescriptions, hospital diagnoses, and demographic information (including sex, age, household income, and mortality) obtained during the study period. This study was approved by the Institutional Review Board of Hallym Medical University Chuncheon Sacred Hospital (Chuncheon, Korea); the need for written informed consent was waived because the KNHIS-NSC data set consisted of deidentified secondary data for research purposes.
Study Population
We used a nationwide representative cohort sample from the KNHIS–NSC database and established a 2-year washout period (2002-2003). The OSA group included all patients who received inpatient and outpatient care for an initial diagnosis of OSA between January 2004 and December 2006. Patients were considered for inclusion if they were diagnosed with OSA 2 or more times between 2004 and 2006 (first diagnosis, initial clinic visit; second diagnosis, polysomnography; and third diagnosis, follow-up visit after polysomnography). In this study, the definition of the start of the follow-up period was the date of the first occurrence of an OSA diagnostic code for the cases. Patients were excluded if they were (1) diagnosed with depressive or anxiety disorders before the first diagnosis of OSA, (2) deceased as a result of any cause between 2002 and 2006 or as a result of an accident after 2007, (3) diagnosed with OSA before 2004, or (4) less than 20 years of age at the first diagnosis of OSA. The comparison group, which comprised 4 individuals for every 1 patient with OSA, was selected using propensity score matching according to registry year, age, sex, residential area, household income, disability, and comorbidities; 197 eligible patients with OSA and 788 patients in the comparison group were enrolled. We tracked each patient from the first date of OSA diagnosis until 2013, and tabulated the information on patients who were diagnosed with affective disorders based on the criteria outlined by the Korean Classification of Diseases (KCD) (eTable 1 in the Supplement). In addition, only patients diagnosed by psychiatrists as having depressive or anxiety disorders were included in the present study.
Predictor and Outcome Variables
Patient characteristics, including sex, age, residence, household income, disability, and comorbidities, are presented in eTable 2 in the Supplement. The study population was divided into 3 age groups (<45, 45–64, and >64 years), 3 income groups (low: ≤30%, middle: 30.1%-69.9%, and high: ≥70% of the median income), and 3 residential areas (Seoul [the largest metropolitan region in South Korea]; second area [other metropolitan cities in South Korea]; and third area [small cities and rural areas]). Death of the patient or the incidence of an affective disorder was used as the end point of the study. Data from patients who did not experience affective symptoms or those who were alive until December 31, 2013, were censored. The risk of depressive and anxiety disorders for the OSA and comparison groups was determined using person-years at risk, which were defined as either the duration between the date of OSA diagnosis in the OSA group or the respective same date of diagnosis in the matched comparison group and the end point for the respective patient. Disabilities and hypertension, diabetes, and chronic kidney disease, which are known risk factors for affective disorders, were obtained from the KCD. Disabilities and comorbidities were defined as a diagnosis of any of these conditions before to the diagnosis of OSA between 2002 and 2006.
Statistical Analysis
To evaluate the differences of sex, age groups, residence, household income, disability, and comorbidities between the OSA and comparison groups, we conducted descriptive and χ2 analyses. To calculate the effect size, we used the standardized difference of proportions with 95% CIs. We found no difference in variables for the χ2 test when values of effect size were below reference values (small effect size: 0.20). Incidence rates per 1000 person-years for depressive and anxiety disorders were obtained by dividing the number of patients with occurrence of specific diseases by person-years at risk. The cumulative incidence of affective disorders was described using Kaplan-Meier survival curves. To identify associations between OSA and affective disorders, we conducted Cox proportional hazards regression model analyses to adjust for the other predictor variables and calculated hazard ratios (HRs) and 95% CIs. In this study, we used univariate and multiple Cox regression models to analyze the HRs for the development of affective disorders, such as depressive and anxiety disorders, during the 9-year follow-up period. Additionally, we tested the proportionality using Schoenfeld residuals in this study. This verification confirmed that the proportionality assumption was not violated. Data were analyzed from September 28, 2018, to March 30, 2019. All statistical analyses were performed using R version 3.5.0 (R Foundation for Statistical Computing).
Results
The present study comprised 197 patients with OSA and 788 comparison individuals. Patients were matched for sex, age, residential area, household income, disability, and comorbidities; thus, similar distributions of all variables were observed between the 2 groups (eTable 3 in the Supplement). A total of 1371.7 person-years in the OSA group and 6328.6 person-years in the comparison group were evaluated for affective disorder events. A summary of time to event as well as censored data appears in eTable 4 in the Supplement.
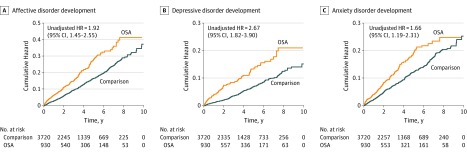
We found that the overall incidence of affective disorders was significantly higher in the OSA group (49.57 per 1000 person-years) than in the comparison group (27.18 per 1000 person-years), with an adjusted HR of 2.04 (95% CI, 1.53-2.70) (Table 1). Additionally, we detected that the overall incidences of depressive and anxiety disorders in the OSA group were 28.35 and 34.61 per 1000 person-years, respectively, and were higher than the incidences observed in the comparison group. After adjusting for sociodemographic factors, including sex, age, residential area, and household income, disability, and comorbidities, the adjusted HRs for the development of a new depressive or anxiety disorder among individuals with OSA during the 9-year follow-up period were 2.90 (95% CI, 1.98-4.24) and 1.75 (95% CI, 1.26-2.44), respectively (Table 2 and Table 3). Moreover, Kaplan-Meier survival curves with log-rank tests for the 9-year follow-up period are presented in the Figure. The log-rank test results indicated that patients with OSA developed affective disorders, such as depressive and anxiety disorders, more frequently than the individuals without OSA (depressive disorder development unadjusted HR, 2.67; 95% CI, 1.82-3.90; anxiety disorder development unadjusted HR, 1.66; 95% CI, 1.19-2.31).
Table 1. Incidence per 1000 Person-Years and Hazard Ratios (HRs) for Affective Disorder Development During a 9-Year Follow-up Period.
| Variable | No. | Cases | Incidence | HR (95% CI) | |
|---|---|---|---|---|---|
| Unadjusted | Adjusted | ||||
| Group | |||||
| Comparison | 788 | 172 | 27.18 | 1 [Reference] | 1 [Reference] |
| OSA | 197 | 68 | 49.57 | 1.92 (1.45-2.55) | 2.04 (1.53-2.70) |
| Sex | |||||
| Male | 860 | 198 | 29.36 | 1 [Reference] | 1 [Reference] |
| Female | 125 | 42 | 43.94 | 1.50 (1.07-2.09) | 1.64 (1.15-2.34) |
| Age, y | |||||
| <45 | 540 | 94 | 21.51 | 1 [Reference] | 1 [Reference] |
| 45-64 | 405 | 131 | 42.87 | 2.01 (1.54-2.62) | 1.62 (1.20-2.20) |
| >64 | 40 | 15 | 54.57 | 2.59 (1.50-4.46) | 1.77 (0.95-3.28) |
| Residencea | |||||
| Seoul | 315 | 62 | 24.50 | 1 [Reference] | 1 [Reference] |
| Second area | 165 | 54 | 42.28 | 1.72 (1.20-2.48) | 2.1 (1.43-3.07) |
| Third area | 505 | 124 | 31.86 | 1.31 (0.96-1.77) | 1.25 (0.92-1.70) |
| Household incomeb | |||||
| Low | 125 | 35 | 35.17 | 1 [Reference] | 1 [Reference] |
| Middle | 300 | 59 | 24.51 | 0.69 (0.45-1.05) | 0.73 (0.47-1.13) |
| High | 560 | 146 | 33.97 | 0.97 (0.67-1.40) | 0.91 (0.63-1.33) |
| Disability | |||||
| No | 960 | 230 | 30.49 | 1 [Reference] | 1 [Reference] |
| Yes | 25 | 10 | 64.06 | 2.15 (1.14-4.04) | 1.07 (0.54-2.12) |
| Comorbidities | |||||
| No | 660 | 119 | 22.13 | 1 [Reference] | 1 [Reference] |
| Yes | 325 | 121 | 52.08 | 2.38 (1.85-3.07) | 1.95 (1.47-2.61) |
Abbreviation: OSA, obstructive sleep apnea.
Seoul indicates the largest metropolitan area; second area, other metropolitan cities; third area, small cities and rural areas.
From 0 to the 30th percentile was defined as low income; percentiles 30.1 to 69.9, middle income; and 70th to 100th percentile, high income.
Table 2. Incidence per 1000 Person-Years and Hazard Ratios (HRs) for Depressive Disorder Development During a 9-Year Follow-up Period.
| Variable | No. | Cases | Incidence | HR (95% CI) | |
|---|---|---|---|---|---|
| Unadjusted | Adjusted | ||||
| Group | |||||
| Comparison | 788 | 75 | 11.20 | 1 [Reference] | 1 [Reference] |
| OSA | 197 | 42 | 28.35 | 2.67 (1.82-3.90) | 2.90 (1.98-4.24) |
| Sex | |||||
| Male | 860 | 98 | 13.73 | 1 [Reference] | 1 [Reference] |
| Female | 125 | 19 | 18.20 | 1.31 (0.80-2.14) | 1.58 (0.94-2.64) |
| Ages, y | |||||
| <45 | 540 | 42 | 9.18 | 1 [Reference] | 1 [Reference] |
| 45-64 | 405 | 65 | 19.58 | 2.13 (1.44-3.14) | 1.53 (0.99-2.39) |
| >64 | 40 | 10 | 35.01 | 3.85 (1.93-7.67) | 2.46 (1.12-5.41) |
| Residencea | |||||
| Seoul | 315 | 31 | 11.75 | 1 [Reference] | 1 [Reference] |
| Second area | 165 | 26 | 18.65 | 1.57 (0.93-2.65) | 2.06 (1.19-3.58) |
| Third area | 505 | 60 | 14.47 | 1.24 (0.80-1.91) | 1.23 (0.79-1.92) |
| Household incomeb | |||||
| Low | 125 | 15 | 14.14 | 1 [Reference] | 1 [Reference] |
| Middle | 300 | 29 | 11.52 | 0.81 (0.44-1.52) | 0.91 (0.48-1.74) |
| High | 560 | 73 | 15.86 | 1.12 (0.65-1.96) | 1.08 (0.62-1.90) |
| Disability | |||||
| No | 960 | 113 | 14.13 | 1 [Reference] | 1 [Reference] |
| Yes | 25 | 4 | 22.30 | 1.59 (0.59-4.32) | 0.67 (0.23-1.92) |
| Comorbidities | |||||
| No | 660 | 48 | 8.51 | 1 [Reference] | 1 [Reference] |
| Yes | 325 | 69 | 27.16 | 3.20 (2.21-4.62) | 2.73 (1.80-4.14) |
Abbreviation: OSA, obstructive sleep apnea.
Seoul indicates the largest metropolitan area; second area, other metropolitan cities; third area, small cities and rural areas.
From 0 to the 30th percentile was defined as low income; percentiles 30.1 to 69.9, middle income; and 70th to 100th percentile, high income.
Table 3. Incidence per 1000 Person-Years and Hazard Ratios (HRs) for Anxiety Disorder Development During a 9-Year Follow-up Period.
| Variable | No. | Cases | Incidence | HR (95% CI) | |
|---|---|---|---|---|---|
| Unadjusted | Adjusted | ||||
| Group | |||||
| Comparison | 804 | 122 | 19.53 | 1 [Reference] | 1 [Reference] |
| OSA | 201 | 50 | 34.61 | 1.66 (1.19-2.31) | 1.75 (1.26-2.44) |
| Sex | |||||
| Male | 870 | 135 | 20.23 | 1 [Reference] | 1 [Reference] |
| Female | 135 | 37 | 36.37 | 1.71 (1.18-2.48) | 1.95 (1.31-2.9) |
| Ages, y | |||||
| <45 | 555 | 68 | 15.36 | 1 [Reference] | 1 [Reference] |
| 45-64 | 402 | 86 | 28.68 | 2.24 (1.64-3.05) | 2.09 (1.47-2.97) |
| >64 | 48 | 18 | 68.05 | 2.61 (1.38-4.94) | 1.95 (0.95-4.03) |
| Residencea | |||||
| Seoul | 333 | 55 | 21.44 | 1 [Reference] | 1 [Reference] |
| Second area | 165 | 30 | 23.02 | 1.74 (1.15-2.65) | 2.24 (1.45-3.47) |
| Third area | 507 | 87 | 22.76 | 1.27 (0.89-1.8) | 1.23 (0.86-1.75) |
| Household incomeb | |||||
| Low | 130 | 23 | 23.40 | 1 [Reference] | 1 [Reference] |
| Middle | 302 | 45 | 19.02 | 0.58 (0.36-0.92) | 0.64 (0.39-1.04) |
| High | 573 | 104 | 23.95 | 0.8 (0.54-1.2) | 0.76 (0.5-1.16) |
| Disability | |||||
| No | 982 | 162 | 21.42 | 1 [Reference] | 1 [Reference] |
| Yes | 23 | 10 | 77.10 | 2.13 (1.05-4.32) | 1.08 (0.5-2.35) |
| Comorbidities | |||||
| No | 665 | 85 | 16.04 | 1 [Reference] | 1 [Reference] |
| Yes | 340 | 87 | 36.37 | 2.17 (1.62-2.9) | 1.65 (1.19-2.29) |
Abbreviation: OSA, obstructive sleep apnea.
Seoul indicates the largest metropolitan area; second area, other metropolitan cities; third area, small cities and rural areas.
From 0 to the 30th percentile was defined as low income; percentiles 30.1 to 69.9, middle income; and 70th to 100th percentile, high income.
Figure. Kaplan-Meier Survival Curves and Log-Rank Tests for Development of OSA.
A, Kaplan-Meier survival curves and log-rank tests for development of affective disorders in the OSA and comparison groups. B, Kaplan-Meier survival curves and log-rank tests for development of depressive disorders in the OSA and comparison groups. C, Kaplan-Meier survival curves and log-rank tests for development of anxiety disorders in the OSA and comparison groups. HR indicates hazard ratio; OSA, obstructive sleep apnea.
Furthermore, we calculated HRs for the development of affective disorders during the 9-year follow-up period according to sex. After adjusting for other factors, we observed that female patients with OSA had a significant likelihood of prospective development of depression and anxiety (adjusted HR for depression, 3.97 [95% CI, 1.54-10.19]; adjusted HR for anxiety, 2.42 [95% CI, 1.17-5.02]) compared with male patients with OSA (adjusted HR for depression, 2.74 [95% CI, 1.80-4.17]; adjusted HR for anxiety, 1.64 [95% CI, 1.13-2.39]) (Table 4).
Table 4. Hazard Ratios (HRs) for Depressive and Anxiety Disorder by Sex.
| Variable | HR (95% CI) | |||
|---|---|---|---|---|
| Male | Female | |||
| Comparison | OSA | Comparison | OSA | |
| Depressive Disorder | ||||
| Unadjusted | 1 [Reference] | 2.54 (1.67-3.85) | 1 [Reference] | 3.37 (1.35-8.42) |
| Adjusted | 1 [Reference] | 2.74 (1.80-4.17) | 1 [Reference] | 3.97 (1.54-10.19) |
| Anxiety Disorder | ||||
| Unadjusted | 1 [Reference] | 1.55 (1.07-2.26) | 1 [Reference] | 2.2 (1.07-4.52) |
| Adjusted | 1 [Reference] | 1.64 (1.13-2.39) | 1 [Reference] | 2.42 (1.17-5.02) |
Abbreviation: OSA, obstructive sleep apnea.
Discussion
We examined the association between OSA and affective disorders among sociodemographically matched individuals who were extracted from a nationwide 9-year longitudinal cohort database of 1 025 340 South Korean patients. To date, numerous studies have been published using these data.23,24,25,26 However, to our knowledge, this study is the first to analyze the risk of developing affective disorders, such as depressive or anxiety disorders, among patients with OSA. In this study, we observed a significant difference in the number of patients who developed an affective disorder among patients with newly diagnosed OSA and individuals without OSA (49.57 vs 27.18 per 1000 person-years). Thus, patients with OSA had a risk of developing affective disorders that was 2.04 times higher than that of individuals without OSA after adjusting for sociodemographic characteristics, disability, and comorbidities.
To date, several studies have reported that patients with OSA exhibit an increased prevalence of psychological symptoms, such as depressive and anxiety disorders, although the exact association between OSA and psychological symptoms remains unknown.15,16,17,18,19,20,21,22 Some studies have stated that oxygen desaturation, which occurs in patients with OSA during sleep, may affect the presentation of psychological symptoms in this group of individuals.27,28 The severity of OSA is usually measured by the apnea/hypopnea index, as defined by the American Academy of Sleep Medicine.29 The apnea/hypopnea index score is based on the number of partial or complete cessations of breathing per hour during sleep. However, associations between OSA severity and psychological symptoms have not been established in previous studies.30,31,32 Therefore, mechanisms other than the number and frequency of hypoxic events may be associated with the development of affective disorders, such as depressive and anxiety disorders, in patients with OSA. Some researchers insist that psychological symptoms are more associated with excessive daytime sleepiness than with hypoxemia.32,33,34 One study described that the presence of sleepiness, irrespective of OSA severity, may be associated with the development of depressive symptoms, whereas reduced sleepiness appears to decrease depressive symptoms.35 Meanwhile, other researchers have reported that the structural or metabolic changes in the brains of patients with OSA may be associated with the elevated rates of depressive and anxiety disorders.36,37 In addition, we further analyzed HRs for depressive and anxiety disorders, which were stratified by sex, because these disorders are reportedly more prevalent in women than in men.38 The adjusted HRs for depressive and anxiety disorders in female patients with OSA were 3.97 and 2.42, respectively, whereas the adjusted HRs in male patients with OSA were significantly increased at 2.74 for depressive disorder and 1.64 for anxiety disorder. Therefore, our findings appear to have described that the incidence of depressive and anxiety disorders was higher in female patients with OSA patients than in male patients with OSA. These findings are consistent with findings from previous studies which showed that the prevalence of depressive and anxiety disorders is higher in female patients with OSA than in male patients.18,32,34 However, confidence intervals were wide on the comparison of HRs for depressive and anxiety disorder according to the age; thus, further studies appear to be needed to confirm these findings.
Strengths and Limitations
This study has several strengths. First, this was a cohort study using a nationwide population-based data set, which allowed us to effectively analyze all events for each affective disorder. Second, our cohort had a relatively long follow-up period (9 years). Third, we improved diagnostic accuracy by only including patients who had 2 or more OSA diagnostic codes and were diagnosed with anxiety or depressive disorders by a psychiatrist. A previous study that used the KNHIS–NSC data reported a similar prevalence of 20 major diseases for each year; thus, the KNHIS–NSC data are considered to have fair to good reliability.39
However, the present study has limitations. We were unable to access other specific health data, including body mass index, lipid profiles, and information regarding behavioral risk factors, such as smoking and alcohol consumption. Therefore, possible confounding factors associated with these variables could not be controlled in this study. Specifically, the unknown information regarding obesity could have been an important confounding factor in the present study. Moreover, this database does not provide information from medical records or data from polysomnography, a criterion standard for diagnosis of OSA. Thus, we could not determine OSA symptom duration, OSA severity, or subjective excessive daytime sleepiness with other measures, such as the Epworth Sleepiness Scale. Furthermore, positive airway pressure or oral appliances used as treatments for OSA are not covered under KNHIS; therefore, this information was unavailable in our claims data set, and we were unable to determine whether patients undergoing these treatments for OSA had a lower incidence of affective disorders.
Conclusions
The findings of this study suggest an association between OSA and the development of affective disorders; specifically, depressive and anxiety disorders over a 9-year follow-up period. Further studies appear to be needed to validate the findings and explore possible underlying mechanisms. Clinicians may consider taking specific precautions to reduce the risks of development of depressive and anxiety disorders among patients with OSA. Studies that investigate the OSA management and the risk of developing affective disorders may yield strategies for effective prevention and intervention practices.
eAppendix. Korea National Health Insurance Service
eTable 1. Korean Classification of Diseases diagnostic practice codes selected from the 2002–2013 Korea National Health Insurance Service–National Sample Cohort
eTable 2. Characteristics of the study subjects
eTable 3. Characteristics of study participants
eTable 4. A summary of events and censoring in this cohort study
References
- 1.Bradley TD, Floras JS. Obstructive sleep apnoea and its cardiovascular consequences. Lancet. 2009;373(9657):82-93. doi: 10.1016/S0140-6736(08)61622-0 [DOI] [PubMed] [Google Scholar]
- 2.Drager LF, Togeiro SM, Polotsky VY, Lorenzi-Filho G. Obstructive sleep apnea: a cardiometabolic risk in obesity and the metabolic syndrome. J Am Coll Cardiol. 2013;62(7):569-576. doi: 10.1016/j.jacc.2013.05.045 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Edwards KM, Kamat R, Tomfohr LM, Ancoli-Israel S, Dimsdale JE. Obstructive sleep apnea and neurocognitive performance: the role of cortisol. Sleep Med. 2014;15(1):27-32. doi: 10.1016/j.sleep.2013.08.789 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Alkhalil M, Schulman E, Getsy J. Obstructive sleep apnea syndrome and asthma: what are the links? J Clin Sleep Med. 2009;5(1):71-78. [PMC free article] [PubMed] [Google Scholar]
- 5.Wu X, Liu H. Obstructive sleep apnea/hypopnea syndrome increases glaucoma risk: evidence from a meta-analysis. Int J Clin Exp Med. 2015;8(1):297-303. [PMC free article] [PubMed] [Google Scholar]
- 6.Kellesarian SV, Malignaggi VR, Feng C, Javed F. Association between obstructive sleep apnea and erectile dysfunction: a systematic review and meta-analysis. Int J Impot Res. 2018;30(3):129-140. doi: 10.1038/s41443-018-0017-7 [DOI] [PubMed] [Google Scholar]
- 7.Sleep-related breathing disorders in adults: recommendations for syndrome definition and measurement techniques in clinical research: the Report of an American Academy of Sleep Medicine Task Force. Sleep. 1999;22(5):667-689. doi: 10.1093/sleep/22.5.667 [DOI] [PubMed] [Google Scholar]
- 8.Seneviratne U, Puvanendran K. Excessive daytime sleepiness in obstructive sleep apnea: prevalence, severity, and predictors. Sleep Med. 2004;5(4):339-343. doi: 10.1016/j.sleep.2004.01.021 [DOI] [PubMed] [Google Scholar]
- 9.Redline S, Strohl KP. Recognition and consequences of obstructive sleep apnea hypopnea syndrome. Clin Chest Med. 1998;19(1):1-19. doi: 10.1016/S0272-5231(05)70428-7 [DOI] [PubMed] [Google Scholar]
- 10.Engleman HM, Douglas NJ. Cognitive effects and daytime sleepiness. Sleep. 1993;16(8)(suppl):S79. [PubMed] [Google Scholar]
- 11.Sánchez AI, Martínez P, Miró E, Bardwell WA, Buela-Casal G. CPAP and behavioral therapies in patients with obstructive sleep apnea: effects on daytime sleepiness, mood, and cognitive function. Sleep Med Rev. 2009;13(3):223-233. doi: 10.1016/j.smrv.2008.07.002 [DOI] [PubMed] [Google Scholar]
- 12.Ward KL, Hillman DR, James A, et al. Excessive daytime sleepiness increases the risk of motor vehicle crash in obstructive sleep apnea. J Clin Sleep Med. 2013;9(10):1013-1021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ulfberg J, Carter N, Talbäck M, Edling C. Excessive daytime sleepiness at work and subjective work performance in the general population and among heavy snorers and patients with obstructive sleep apnea. Chest. 1996;110(3):659-663. doi: 10.1378/chest.110.3.659 [DOI] [PubMed] [Google Scholar]
- 14.Findley L, Smith C, Hooper J, Dineen M, Suratt PM. Treatment with nasal CPAP decreases automobile accidents in patients with sleep apnea. Am J Respir Crit Care Med. 2000;161(3, pt 1):857-859. doi: 10.1164/ajrccm.161.3.9812154 [DOI] [PubMed] [Google Scholar]
- 15.Sharafkhaneh A, Giray N, Richardson P, Young T, Hirshkowitz M. Association of psychiatric disorders and sleep apnea in a large cohort. Sleep. 2005;28(11):1405-1411. doi: 10.1093/sleep/28.11.1405 [DOI] [PubMed] [Google Scholar]
- 16.Gupta MA, Simpson FC. Obstructive sleep apnea and psychiatric disorders: a systematic review. J Clin Sleep Med. 2015;11(2):165-175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Stubbs B, Vancampfort D, Veronese N, et al. The prevalence and predictors of obstructive sleep apnea in major depressive disorder, bipolar disorder and schizophrenia: a systematic review and meta-analysis. J Affect Disord. 2016;197:259-267. doi: 10.1016/j.jad.2016.02.060 [DOI] [PubMed] [Google Scholar]
- 18.Chen YH, Keller JK, Kang JH, Hsieh HJ, Lin HC. Obstructive sleep apnea and the subsequent risk of depressive disorder: a population-based follow-up study. J Clin Sleep Med. 2013;9(5):417-423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Pamidi S, Knutson KL, Ghods F, Mokhlesi B. Depressive symptoms and obesity as predictors of sleepiness and quality of life in patients with REM-related obstructive sleep apnea: cross-sectional analysis of a large clinical population. Sleep Med. 2011;12(9):827-831. doi: 10.1016/j.sleep.2011.08.003 [DOI] [PubMed] [Google Scholar]
- 20.Sampaio R, Pereira MG, Winck JC. Psychological morbidity, illness representations, and quality of life in female and male patients with obstructive sleep apnea syndrome. Psychol Health Med. 2012;17(2):136-149. doi: 10.1080/13548506.2011.579986 [DOI] [PubMed] [Google Scholar]
- 21.Diamanti C, Manali E, Ginieri-Coccossis M, et al. Depression, physical activity, energy consumption, and quality of life in OSA patients before and after CPAP treatment. Sleep Breath. 2013;17(4):1159-1168. doi: 10.1007/s11325-013-0815-6 [DOI] [PubMed] [Google Scholar]
- 22.Garbarino S, Bardwell WA, Guglielmi O, Chiorri C, Bonanni E, Magnavita N. Association of anxiety and depression in obstructive sleep apnea patients: a systematic review and meta-analysis. Behav Sleep Med. 2018;19:1-23. doi: 10.1080/15402002.2018.1545649 [DOI] [PubMed] [Google Scholar]
- 23.Kim JY, Hong JY, Kim DK. Association of sudden sensorineural hearing loss with risk of cardiocerebrovascular disease: a study using data from the Korea National Health Insurance Service. JAMA Otolaryngol Head Neck Surg. 2018;144(2):129-135. doi: 10.1001/jamaoto.2017.2569 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kim JY, Lee JW, Kim M, Kim MJ, Kim DK. Association of idiopathic sudden sensorineural hearing loss with affective disorders. JAMA Otolaryngol Head Neck Surg. 2018;144(7):614-621. doi: 10.1001/jamaoto.2018.0658 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Park SJ, Choi NK, Yang BR, Park KH, Woo SJ. Risk of stroke in retinal vein occlusion. Neurology. 2015;85(18):1578-1584. doi: 10.1212/WNL.0000000000002085 [DOI] [PubMed] [Google Scholar]
- 26.Shin JY, Roughead EE, Park BJ, Pratt NL. Cardiovascular safety of methylphenidate among children and young people with attention-deficit/hyperactivity disorder (ADHD): nationwide self controlled case series study. BMJ. 2016;353:i2550. doi: 10.1136/bmj.i2550 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Bardwell WA, Norman D, Ancoli-Israel S, et al. Effects of 2-week nocturnal oxygen supplementation and continuous positive airway pressure treatment on psychological symptoms in patients with obstructive sleep apnea: a randomized placebo-controlled study. Behav Sleep Med. 2007;5(1):21-38. doi: 10.1207/s15402010bsm0501_2 [DOI] [PubMed] [Google Scholar]
- 28.Schröder CM, O’Hara R. Depression and obstructive sleep apnea (OSA). Ann Gen Psychiatry. 2005;4:13. doi: 10.1186/1744-859X-4-13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Berry RB, Budhiraja R, Gottlieb DJ, et al. ; American Academy of Sleep Medicine; Deliberations of the Sleep Apnea Definitions Task Force of the American Academy of Sleep Medicine . Rules for scoring respiratory events in sleep: update of the 2007 AASM Manual for the Scoring of Sleep and Associated Events. J Clin Sleep Med. 2012;8(5):597-619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.McCall WV, Harding D, O’Donovan C. Correlates of depressive symptoms in patients with obstructive sleep apnea. J Clin Sleep Med. 2006;2(4):424-426. [PubMed] [Google Scholar]
- 31.Kezirian EJ, Harrison SL, Ancoli-Israel S, et al. ; Study of Osteoporotic in Men Research Group . Behavioral correlates of sleep-disordered breathing in older men. Sleep. 2009;32(2):253-261. doi: 10.1093/sleep/32.2.253 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Asghari A, Mohammadi F, Kamrava SK, Tavakoli S, Farhadi M. Severity of depression and anxiety in obstructive sleep apnea syndrome. Eur Arch Otorhinolaryngol. 2012;269(12):2549-2553. doi: 10.1007/s00405-012-1942-6 [DOI] [PubMed] [Google Scholar]
- 33.Ye L, Liang ZA, Weaver TE. Predictors of health-related quality of life in patients with obstructive sleep apnoea. J Adv Nurs. 2008;63(1):54-63. doi: 10.1111/j.1365-2648.2008.04652.x [DOI] [PubMed] [Google Scholar]
- 34.Lee SA, Han SH, Ryu HU. Anxiety and its relationship to quality of life independent of depression in patients with obstructive sleep apnea. J Psychosom Res. 2015;79(1):32-36. doi: 10.1016/j.jpsychores.2015.01.012 [DOI] [PubMed] [Google Scholar]
- 35.Ishman SL, Benke JR, Cohen AP, Stephen MJ, Ishii LE, Gourin CG. Does surgery for obstructive sleep apnea improve depression and sleepiness? Laryngoscope. 2014;124(12):2829-2836. doi: 10.1002/lary.24729 [DOI] [PubMed] [Google Scholar]
- 36.Kumar R, Macey PM, Cross RL, Woo MA, Yan-Go FL, Harper RM. Neural alterations associated with anxiety symptoms in obstructive sleep apnea syndrome. Depress Anxiety. 2009;26(5):480-491. doi: 10.1002/da.20531 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Yadav SK, Kumar R, Macey PM, Woo MA, Yan-Go FL, Harper RM. Insular cortex metabolite changes in obstructive sleep apnea. Sleep. 2014;37(5):951-958. doi: 10.5665/sleep.3668 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Young T, Palta M, Dempsey J, Skatrud J, Weber S, Badr S. The occurrence of sleep-disordered breathing among middle-aged adults. N Engl J Med. 1993;328(17):1230-1235. doi: 10.1056/NEJM199304293281704 [DOI] [PubMed] [Google Scholar]
- 39.Rim TH, Kim DW, Han JS, Chung EJ. Retinal vein occlusion and the risk of stroke development: a 9-year nationwide population-based study. Ophthalmology. 2015;122(6):1187-1194. doi: 10.1016/j.ophtha.2015.01.020 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eAppendix. Korea National Health Insurance Service
eTable 1. Korean Classification of Diseases diagnostic practice codes selected from the 2002–2013 Korea National Health Insurance Service–National Sample Cohort
eTable 2. Characteristics of the study subjects
eTable 3. Characteristics of study participants
eTable 4. A summary of events and censoring in this cohort study