Abstract
Background:
Before penicillin, the syphilis case-fatality rate was 10% within 40 years. Late complications, such as cardiovascular syphilis, were still common in the 1950s but now seem quite rare even though some infections likely go undetected. We studied trends in syphilis mortality as an indicator of trends in severe complications of syphilis.
Methods:
We assessed underlying cause of death from U.S. death certificates for 1968—2015. We examined death trends by type of syphilis (cardiovascular, neuro, congenital, other). We compared trends in deaths to trends in primary and secondary syphilis from national STD surveillance data.
Results:
During 1968—2015 there were 6,498 deaths attributed to syphilis; 4,149 males and 2,349 females. Annual syphilis deaths decreased from 586 in 1968 to 94 in 1984, then leveled off to between 24—46 since 1998. Between 1968 and 2015, the decrease in annual cardiovascular syphilis deaths (from 338 to 3) exceeded the decrease in annual neurosyphilis deaths (from 191 to 33). Congenital syphilis deaths (which do not include stillbirths) generally decreased from 28 to 2 per year. An increase in primary and secondary syphilis among women in the late 1980s was accompanied by a 4-fold increase in congenital syphilis deaths (from 9 in 1986 to 35 in 1990) but there was no subsequent increase in syphilis deaths among women.
Conclusion:
Adults now rarely die from syphilis. Increases in infections in the late 1980s did not lead to an increase in adult syphilis deaths. Congenital syphilis deaths still increase when syphilis increases among women.
Keywords: syphilis, congenital syphilis, cardiovascular syphilis, neurosyphilis, mortality
Brief Summary:
Adult syphilis deaths decreased greatly since 1968, and did not increase after infections increased in the late 1980s. Congenital syphilis deaths still increase when infections among women increase.
Background
In the pre-penicillin era, infection with Treponema pallidum was common and syphilis was a major cause of disability and death. The annual incidence of infection was 1.8% in US Army soldiers stationed in the US in 1914. [1] Over 575,000 cases (of all stages) were reported in the United States in 1943. [2] Long term complications from syphilis occurred in 28% of the Oslo cohort of patients with untreated syphilis diagnosed in 1891—1910. [3] Cardiovascular syphilis was diagnosed in 10.4% of patients and 6.5% developed neurosyphilis. [3] The case fatality rate was 10.8% (15.1% in males, 8.3% in females) with deaths occurring up to 40 years after infection. [3] Syphilis was the 10th leading cause of death in the United States in 1923—1925, averaging 17,515 deaths per year. [4]
When penicillin became available in the 1940s there were major decreases in incidence of syphilis. Reported cases of primary and secondary syphilis fell from 94,957 in 1946 to 6,454 in 1955. [2] Serious complications of syphilis also decreased. Between 1927 and 1937, 6.9% (1,040) of the 15,000 autopsies at Philadelphia General Hospital had evidence of cardiovascular syphilis. [5] By 1950—1960, the prevalence of syphilitic aortitis had fallen to 0.8% (100) of 13,082 autopsies at Kings County Hospital in Brooklyn, NY. [6] Since then case series of cardiovascular syphilis have been reported, [7] but it is difficult to say what the rates of disease due to cardiovascular syphilis have been. Similarly, syphilis was responsible for 8.6% of admissions to the Boston Psychopathic Hospital between 1912 and 1934. [8] However, by 2001, syphilis was so rarely associated with dementia that the American Academy of Neurology dropped syphilis testing from the routine workup. [9]
Increases in syphilis in the late 1980s, [2] high prevalence of coinfection with HIV, [2] and increased recognition of ocular syphilis [10] have raised concerns about potential increases in syphilis-related morbidity among persons whose infections have remained undiagnosed. Syphilis surveillance focuses on infection and does not monitor complications of syphilis. Trends in tertiary syphilis are not available. [11] However, death certificates offer an opportunity to search for trends in severe complications of syphilis. [12] We studied trends in syphilis as an underlying cause of death as a surrogate for trends in severe complications of syphilis, and to help assess the frequency of severe complications.
Methods
We used CDC Wonder [13] to access US mortality data which were available from 1968—2015. Three different ICD codes were used during this time, ICD8 (1968–1978), ICD9 (1980–1998), and ICD10 (1999—2015). Categories for classifying syphilis changed minimally with these different code sets. The main diagnostic categories for syphilis were consistent over time: congenital, early, cardiovascular, neuro, and late unspecified. ICD9 contained a few more subcategories for early, cardiovascular, and neurosyphilis than ICD8 or ICD10. For example, ICD8 cases of “other cardiovascular syphilis” could be specified as “syphilitic aortitis”, “syphilitic endocarditis”, or “other specified cardiovascular syphilis” in ICD9.
We searched for mortality records with the reported underlying cause of death attributed to syphilis (ICD codes 090—097). Deaths from subcategories were collapsed and counted according to the main diagnostic categories: congenital, early, cardiovascular, neuro, and late unspecified. Numbers of deaths were examined after stratifying by age, race, and sex.
Reported cases of primary and secondary syphilis, by gender, were obtained from the National Electronic Telecommunications System for Surveillance (NETSS), the system through which CDC receives notifiable STD data from all 50 states and the District of Columbia. Trends in syphilis deaths were plotted to compare to trends in primary and secondary syphilis among men and women. Trends in congenital syphilis deaths were compared to trends in primary and secondary syphilis among women.
Results
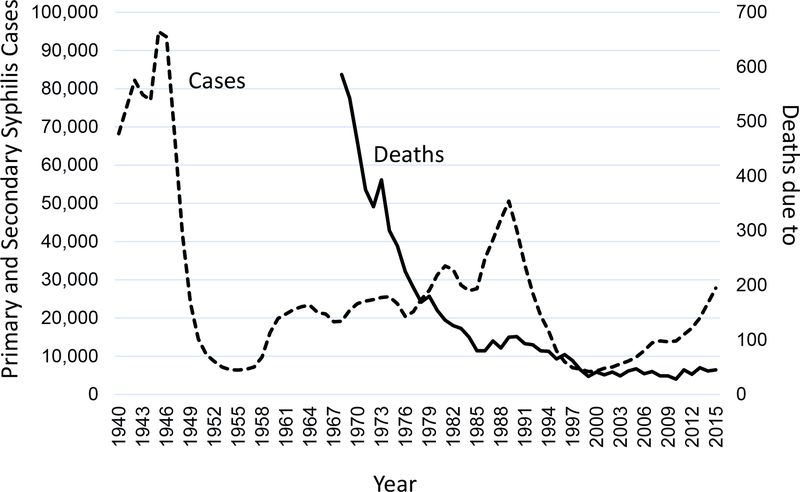
During 1968—2015, syphilis was listed as the underlying cause for 6,498 deaths. The annual number of deaths decreased rapidly from 586 in 1968 to 80 in 1985. Since 1998 deaths due to syphilis have fluctuated between 28 and 47 per year. (Figure 1). Yearly reports of primary and secondary syphilis declined rapidly from 93,545 in 1947 to 10,449 in 1952, increased to over 20,000 in the 1960’s and then peaked at 50,578 in 1990. (Figure 1) There was no clear increase in deaths due to syphilis among adults following the increase in syphilis cases in the late 1980’s.
Figure 1.
Primary and secondary syphilis 1940—2015 and syphilis deaths, 1968—2015, United States.
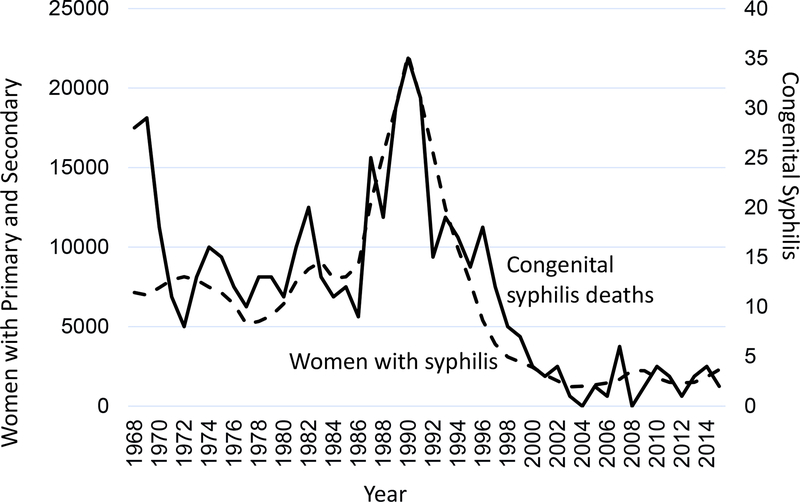
Congenital syphilis was the underlying cause for 568 of the 6,498 syphilis deaths from 1968 through 2015 (this does not include stillbirths). The number of deaths decreased from 28 in 1968 to 9 in 1972, then remained relatively stable until they increased from 9 in 1986 to 35 in 1990. (Figure 2) Deaths due to congenital syphilis tracked closely with reported cases of primary and secondary syphilis among women which increased 4-fold between 1978 and 1990.
Figure 2.
Women with primary and secondary syphilis and deaths due to congenital syphilis, United States, 1968—2015
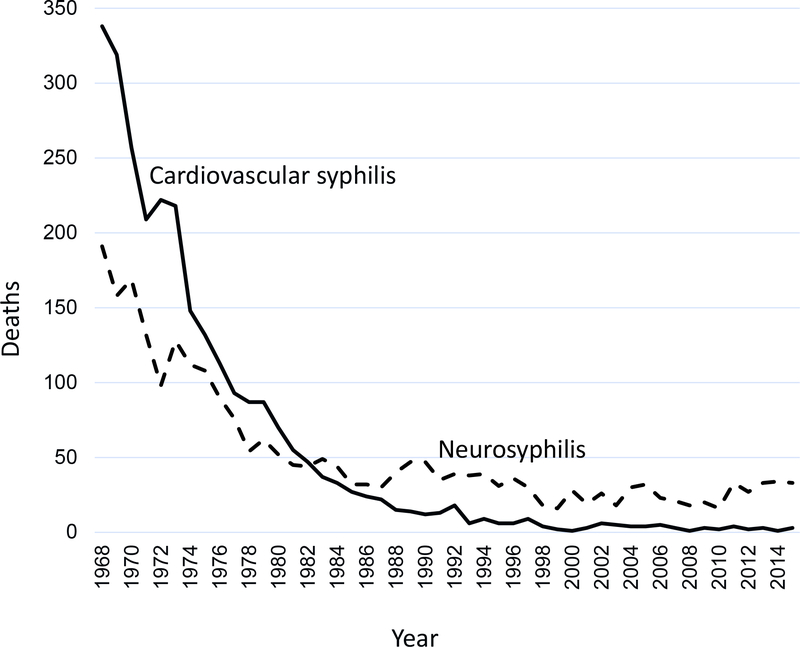
The total number of deaths for the major categories were: congenital 568, cardiovascular syphilis 2,702, neurosyphilis 2,533, late unspecified syphilis 668, and early syphilis 27. All categories of syphilis deaths decreased over time, however, cardiovascular syphilis deaths decreased more than neurosyphilis deaths (Figure 3). Cardiovascular syphilis accounted for 338 deaths in 1968 but only between 1—6 per year since 1998. Neurosyphilis accounted for 191 deaths in 1968 and between 16—34 per year since 1998.
Figure 3.
Deaths due to cardiovascular syphilis and neurosyphilis, United States, 1968—2015.
Over-all, 63.6% of syphilis deaths were in persons aged 65 years or older. The age at death increased slightly over time. The most common age group was 65 to 74 during 1968—1978 and 75 to 84 during 1979—2015. By race, there were more deaths among whites (151 per year) than blacks (111 per year) during 1968—1985; thereafter, numbers of deaths were similar (28 per year for each).
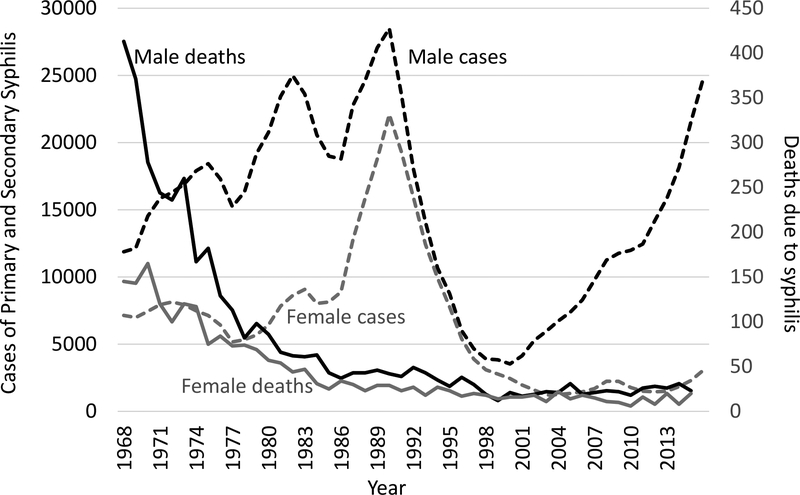
More deaths due to syphilis occurred among males (4,149) than females (2,349). There were 2.2 times more male deaths than female deaths during 1968—1975. (Figure 4) Since that time, the male:female ratio of deaths has fluctuated, but remained at about 1.6. There was a 4-fold increase in reported primary and secondary syphilis among women between 1978 (5,331 cases) and 1990 (22,088 cases). The number of syphilis deaths among females (excluding congenital cases) did not increase after this epidemic; it has continued to fall from an average of 23.6 per year (1991—1995) to 14.4 per year (2011—2015). (Figure 4). Similarly, deaths among males have not increased despite increases in reported cases from 1968—1990.
Figure 4.
Cases of primary and secondary syphilis, and deaths due to syphilis, by sex, United States, 1968—2015.
Discussion
Death certificates are a crude approach to tracking severity of disease over time, [14, 15] but for syphilis there are few alternatives. The trends in deaths due to syphilis showed little year-to-year variation, suggesting that they might be valid reflections of trends in disease. The rapid decline in syphilis deaths among adults that occurred through 1980 likely reflects the dramatic decreases in incidence that occurred 30–40 years earlier and the ability of penicillin to prevent progression of prevalent infections to tertiary disease. For adults, deaths due to untreated syphilis can occur 10–40 years after infection. [3] This broad interval blurs the correlation between infection and death. In contrast, deaths due to congenital syphilis usually occur within a year of birth, so trends in congenital syphilis deaths would be expected to mirror trends in congenital syphilis and syphilis among pregnant women. Indeed, the increase in deaths due to congenital syphilis in the late 1980s very closely matches the increases in syphilis that occurred among women at that time.
The absence of any increase in adult deaths 25 years after the major increases in syphilis in the late 1980s suggests that the attack rate for late manifestations of syphilis is much lower than it was in the past. This finding is consistent with observations in the 1970s that a predicted rise in neurosyphilis due to untreated infections acquired during World War II never materialized. [16] Perhaps deaths have decreased because nearly all infections are detected and treated before late complications can occur. Alternatively, many infections may be inadvertently cured when antibiotics are taken for other reasons. [16] It is also possible that the organism has evolved to be less pathogenic. [17] Even in the 1930s, before penicillin, it was noted that “an often fatal infection has evolved into one of exquisite chronicity”. [1]
In contrast to the decrease in likelihood of progression to tertiary syphilis in adults, the likelihood of progression to serious disease following congenital infection has not changed; 66.5% of women with untreated syphilis will have an adverse outcome of pregnancy, including 25.6% who will have fetal loss or a stillbirth. [18] This change for adults but not for babies may be due to differences in pathogenesis, or to the differences in opportunities for treatment (including inadvertent treatment). The time between infection and serious complications is often measured in decades for adults, but can be a matter of weeks for the developing fetus.
Our findings raise a few questions about complications of syphilis. Why did cardiovascular syphilis deaths decrease faster than neurosyphilis deaths? This trend appears to be consistent with changes in non-fatal tertiary syphilis, though data are sparse. [19, 20] These changes could be influenced by changes in clinical suspicion, ability to diagnose and treat complications, or changes in autopsy rates. It is possible that the blood brain barrier limits the impact of antibiotics taken for other reasons, so inadvertent treatment reduces cardiovascular syphilis more than neurosyphilis. [21, 22] Maybe the pathogenesis of neurosyphilis begins earlier in the course of infection or is less likely to be stopped by treatment [22] than cardiovascular syphilis, [21] providing a shorter opportunity for cure.
Why are men more likely to develop complications and die from syphilis than women? [3, 5, 6, 18, 23] Men have been more likely to acquire infection than women, [2] and there may also be differences in how often infections are detected and treated. However, difference in complication rates were consistently seen before penicillin, even when confining analyses to infected persons. [3, 23] In the Oslo cohort of untreated syphilis, infected men were more likely than infected women to develop neurosyphilis (9.2% vs 5.1%), cardiovascular syphilis (14.9% vs 8.0%), or to die from syphilis (15.1% vs 8.3%). [3] Previous hypotheses to explain these differences include the possibility that physical exertion increased the risk of cardiovascular syphilis. [24] Differences in immune systems are now thought to contribute to gender differences in response to many other infections. [25] Advances in understanding of physiology and new laboratory techniques may someday solve this mystery.
These changes in disease caused by syphilis have implications for prevention. Reduction in adverse effects of syphilis among adults means that there is less urgency to find and cure adults with syphilis than in the past. Continuing high risk for complications from congenital syphilis means congenital syphilis should be considered a higher priority. In 2016, deaths from congenital syphilis (including stillbirths) exceeded deaths from syphilis among adults even though adult cases exceeded congenital cases by a factor of 100. [2] Most congenital infections can be prevented by screening and rescreening pregnant women. [26] However, preventing all congenital infections requires preventing syphilis among women. Low rates of infection among women and recent successes in stopping outbreaks among heterosexuals suggest this is possible. [27]
Our study has important limitations. We measured deaths, not nonfatal outcomes which can also be serious. Deaths were determined by a wide variety of providers and coders which likely leads to inconsistency among observers and could cause trends over time. We did not examine medical records to validate the cause of death. We had little information on each death beyond basic demographics. We did not have information on sexual orientation so we could not look specifically at trends among men who have sex with men. We compared trends in deaths to trends in reported cases. Trends in deaths are more likely related to changes in the number of untreated infections, which are not known.
In conclusion, the reduction in deaths due to syphilis is miraculous and continues despite the inability to prevent infection among adults. Some characteristics of syphilis remain medical mysteries, including the greater decreases in cardiovascular syphilis compared to neurosyphilis, and the higher case-fatality rate for males compared to females. Changes in prognosis following an infection call for changes in priorities to prevent serious disease with an emphasis on preventing syphilis among women in order to prevent congenital syphilis.
Acknowledgments
The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention. No outside funding was obtained for this work. The authors have no conflicts of interest.
References
- 1.Moore JE. An Evaluation of public-health measures for the control of syphilis: an epidemiological study. Lancet 1951;1(6657):699–711. [DOI] [PubMed] [Google Scholar]
- 2.Centers for Disease Control and Prevention. Sexually Transmitted Disease Surveillance 2016. Atlanta: U.S. Department of Health and Human Services; 2017. [Google Scholar]
- 3.Gjestland T. The Oslo study of untreated syphilis: an epidemiologic investigation of the natural course of the syphilitic infection based upon a re-study of the Boeck-Bruusgaard Material. Acta Dermato-Venereologica 1955;35 Supp 34:364. [DOI] [PubMed] [Google Scholar]
- 4.Leading causes of death, 1900–1998. https://www.cdc.gov/nchs/data/dvs/lead1900_98.pdf
- 5.Welty JW. A necropsy survey of cardiovascular syphilis with particular reference to its decreasing incidence. Am J Med Sci 1939;197:782–793. [Google Scholar]
- 6.Heggtveit HA. Syphilitic Aortitis: a clinicopathologic autopsy study of 100 cases, 1950—1960. Circulation 1964;29:346–355. [DOI] [PubMed] [Google Scholar]
- 7.Roberts WC, Barbin CM, Weissenborn MR, Ko JM, Henry AC. Syphilis as a cause of thoracic aortic aneurysm. Am J Cardiol 2015;116:1298–1303. [DOI] [PubMed] [Google Scholar]
- 8.Moore M, Merritt HH. Role of syphilis of the nervous system in the production of mental disease. JAMA;1936;107:1292–1293 [Google Scholar]
- 9.Knopman DS, DeKosky ST, Cummings JL, et al. Practice parameter: diagnosis of dementia (an evidence-based review). Neurology 2001;56:1143–1153. [DOI] [PubMed] [Google Scholar]
- 10.Oliver SE, Cope AB, Rinsky JL, et al. Increases in ocular syphilis—North Carolina, 2014–2015. Clin Infect Dis. In Press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Tuddenham S, Ghanem KG. Neurosyphilis: knowledge gaps and controversies. Sex Transm Dis 2018;45:147–151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Barragan NC, Moschetti K, Smith LV, et al. Differential declines in syphilis-related mortality in the United States, 2000–2014. Am J Infect Control 2017;45:417–420. [DOI] [PubMed] [Google Scholar]
- 13.Underlying cause of death. https://wonder.cdc.gov/mortSQL.html.
- 14.Johansson LA, Westerling R, Rosenberg HM. Methodology of studies evaluating death certificate accuracy were flawed. J Clin Epidemiol 2006;59:125–131. [DOI] [PubMed] [Google Scholar]
- 15.McGivern L, Shulman L, Carney JK, Shapiro S, Bundock E. Death certification errors and the effect on mortality statistics. Pub Health Rep 2017;132:669–675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Catterall RD. Neurosyphilis. Br J Hosp Med 1977;17:585–604. [PubMed] [Google Scholar]
- 17.Smajs D, Norris SJ, Weinstock GM. Genetic diversity in Treopnema pallidum: implications for pathogenesis, evolution and molecular diagnostics of syphilis and yaws. Infect Genet Evol 2012;12:191–202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Gomez GB, Kamb ML, Newman LM, Mark J, Broutet N, Hawkes SJ. Untreated maternal syphilis and adverse outcomes of pregnancy: a systematic review and meta-analysis. Bull World Health Organ 2013;91:217–226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sparling PF, Swartz MN, Musher DM, et al. Clinical Manifestations of Syphilis Chapter 37 in Holmes KK, Sparling PF, Stamm WE et al. Eds. Sexually Transmitted Diseases Fourth Edition. 2008. McGraw-Hill, New York. [Google Scholar]
- 20.Hook EW 3rd. Syphilis. Lancet 2017;389:1550–1557. [DOI] [PubMed] [Google Scholar]
- 21.Thompson WP, Comeau WJ, White PD. The role of the treatment of syphilis in the prevention of cardiovascular involvement. Am Heart J 1939;17:286–293. [Google Scholar]
- 22.Drago F, Javor S, Parodi A. Neurosyphilis: from infection to autoinflammation? (letter) Int J STD & AIDS 2016;27:327–328. [DOI] [PubMed] [Google Scholar]
- 23.Singh AAE, Romanowski B. Syphilis: review with emphasis on clinical, epidemiologic, and some biologic features. Clin Micro Rev 1999;12:187–209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Nicol CS. Cardiovascular syphilis. Br J Vener Dis 1950;26:109–125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Giefing-Kröll C, Berger P, Lepperdinger G, Grubeck-Loebenstein B. How sex and age affect immune responses, susceptibility to infections, and response to vaccination. Aging Cell 2015:14:309–321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Matthias JM, Rahman MM, Newman DR, Peterman TA. Effectiveness of prenatal screening and treatment to prevent congenital syphilis, Louisiana and Florida, 2013–2014. Sex Transm Dis. 2017;44:498–502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Peterman TA, Su J, Bernstein KT, Weinstock H. Syphilis in the United States: On the rise? Expert Rev Anti-infective Therapy. 2015:13:161–168. [DOI] [PMC free article] [PubMed] [Google Scholar]