Abstract
OBJECTIVE:
To describe recent syphilis trends among pregnant women and to evaluate the prevalence of reported high-risk behaviors in this population.
METHODS:
We analyzed U.S. national case report data for 2012–2016 to assess trends among pregnant women with all stages of syphilis. Risk behavior data collected through case interviews during routine local health department investigation of syphilis cases were used to evaluate the number of pregnant women with syphilis reporting these behaviors.
RESULTS:
During 2012–2016, the number of syphilis cases among pregnant women increased 61%, from 1,561 to 2,508, and this increase was observed across all races and ethnicities, all women aged 15–45 years, and all U.S. regions. Of 15 queried risk factors, including high-risk sexual behaviors and drug use, 49% of pregnant women with syphilis did not report any in the past year. The most commonly reported risk behaviors were a history of a sexually transmitted disease (43%) and more than one sex partner in the past year (30%).
CONCLUSION:
Syphilis cases among pregnant women increased from 2012 to 2016, and in half, no traditional behavioral risk factors were reported. Efforts to reduce syphilis among pregnant women should involve increasing health care provider awareness of the Centers for Disease Control and Prevention and the American College of Obstetricians and Gynecologists’ recommendations, which include screening all pregnant women for syphilis at the first prenatal visit and rescreening high-risk women during the third trimester and at delivery. Health care providers should also consider local syphilis prevalence in addition to individual reported risk factors when deciding whether to repeat screening.
Syphilis is a sexually transmitted infection caused by the spirochete Treponema pallidum. Syphilis can also be spread through mother-to-child transmission and results in congenital syphilis if untreated in up to 80% of cases.1 Mother-to-child transmission of syphilis can occur during any trimester of pregnancy and at any stage of syphilis with the highest risk of transmission during early syphilis (primary, secondary, or early latent stages).1 The sequelae of congenital syphilis affect multiple organ systems and can cause prematurity, stillbirth, and neonatal and infant death.2,3 However, congenital syphilis is preventable with adequate and timely screening, diagnosis, and benzathine penicillin G treatment of maternal syphilis.4,5
In the United States, syphilis rates among women and infants have increased dramatically in recent years. Between 2012 and 2016 the rate of reported primary and secondary syphilis among women more than doubled (111.1% increase; 0.9–1.9 cases/100,000 women) and the congenital syphilis rate increased 86.9% (8.4–15.7 cases/100,000 live births).6 Given the preventable nature of congenital syphilis, several studies have examined possible missed opportunities and highlighted the importance of early and adequate prenatal care, timely identification of pregnant women with syphilis, and, if infected, timely receipt of a stage-appropriate penicillin regimen at least 30 days before delivery (Introcaso CE, Bradley H, Gruber D, Markowitz LE. Missed opportunities for preventing congenital syphilis infection [letter]. Sex Transm Dis 2013;40:431.).7–12
The timely identification of pregnant women with syphilis requires universal screening at the first prenatal care appointment and possible repeat screening in the third trimester for certain populations. For the latter, the Centers for Disease Control and Prevention and the American College of Obstetricians and Gynecologists recommend repeat syphilis screening in the third trimester and at delivery for pregnant women who are at high risk for syphilis or who live in areas with high syphilis morbidity.5
Many studies have demonstrated increased rates of sexually transmitted diseases (STDs) in those who have a partner in a high-risk sexual network or who themselves have a history of incarceration or substance abuse.13–16 However, it is unclear what proportion of pregnant women with syphilis report risk factors and which risk factors are most common among pregnant women with syphilis. To better understand pregnant women with syphilis, we analyzed national case report data to describe recent trends in syphilis among pregnant women and evaluated the prevalence and trends of reported risk behaviors in this population.
METHODS
Data on all reported female syphilis cases (any stage) were extracted from the National Notifiable Diseases Surveillance System, which provides the CDC with data about notifiable sexually transmitted infections from all 50 states and the District of Columbia. The syphilis case reports are received as deidentified, line-listed data that include demographic information, stage of syphilis (primary, secondary, early latent, or late latent cases), and other variables such as pregnancy status if ascertained. Additional data on demographics, self-reported risk behaviors and information about sexual partners in the past 12 months, and self-reported lifetime history of previous STDs are collected by local health department staff and included in this system. Data on prenatal care, treatment, and pregnancy outcomes are not included in these reports.
In this study, we analyzed the case reports for all pregnant women with any stage of syphilis, from all 50 states and the District of Columbia, from 2012 to 2016 by maternal characteristics, including age, race and Hispanic ethnicity, and census region. Race and Hispanic ethnicity were defined using National Center for Health Statistics bridged-race categories (Asian or Pacific Islander, non-Hispanic black, Hispanic, Native American or Alaska Native, and non-Hispanic white), and U.S. regions were defined using the U.S. Census geographic regions (Midwest, North, South, or West).6,17 In addition to demographic data, information about risk behaviors is collected for cases that are interviewed or investigated by the local public health department. To evaluate the prevalence of reported risk factors among pregnant women with syphilis, we focused on high-risk sexual behaviors (prior STD; greater than one sex partner; sex while intoxicated; anonymous sex partner; sex for drugs or money; sex with persons known to inject drugs; sex with gay, bisexual, or other men who have sex with men), drug-related risk factors, history of incarceration, and human immunodeficiency virus (HIV) infection. The timing of each of these risk factors referred to the 12 months before the diagnosis of syphilis except for evaluation of prior STD, which asked about one’s lifetime risk and HIV status, documented through test result, record search, or self-reported at the time of syphilis diagnosis.
Most risk factor variables were collected and reported with values of “yes,” “no,” “missing,” or “unknown.” However, in some jurisdictions, variables on specific drug use (ie, crack, cocaine, heroin, methamphetamine, “other drug use,” and “no drug use”) were collected in a “check all that apply” format, where the absence of a “yes” response indicates a “no” response, but were reported to the CDC as “yes,” “no,” “missing,” or “unknown.” Thus, a reported value of “missing” or “unknown” could indicate either a “no” response for each of the specific drugs listed or be truly missing or unknown. To account for the “check all apply” format for these specific variables, if a case was reported without data for the specific drug (eg, crack) and also responded “yes” to either the variable “no drug use” or one of the other specific drug variables (eg, methamphetamine), this case was counted as a “no” response for the specific drug (crack). The proportion of cases reporting each risk factor was calculated using a denominator made up of those with a yes or no response for that risk factor. When calculating the proportion of pregnant women with syphilis reporting any risk factor, the total number of pregnant women with syphilis from 2012 to 2016 was used as the denominator.
We also applied this same method to focus specifically on pregnant females with early syphilis, because this group is at higher risk for congenital syphilis and may represent a higher risk population. When calculating the proportion of pregnant women with early syphilis reporting any risk factor, the total number of pregnant women with primary and secondary or early latent syphilis from 2012 to 2016 was used as the denominator.
Trends in the proportion of cases reporting each risk factor were assessed using the Cochran-Armitage trend test; a two-sided P value <.05 was considered statistically significant. All data were analyzed using SAS 9.4. This study used data that are routinely collected as a part of public health surveillance for the purpose of guiding public health disease control efforts and was therefore not subject to institutional review board approval for human subjects’ protection.
RESULTS
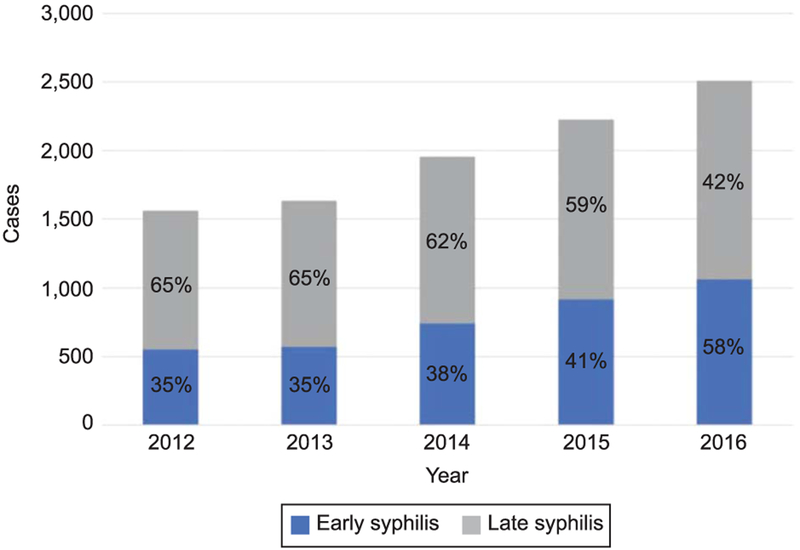
During 2012–2016, the number of reported cases of syphilis among females increased 55%, from 9,551 to 14,838, and the number of cases among pregnant women increased 61%, from 1,561 to 2,508 (Fig. 1). The percentage of reported female syphilis cases known to be pregnant was relatively stable during this time period, ranging from 16% to 18% of all reported female syphilis cases. The percentage of female syphilis cases with “missing” or “unknown” pregnancy status decreased from 27% in 2012 to 20% in 2016.
Fig. 1.
Reported cases of early and late latent syphilis among pregnant women. The increase in the proportion of cases that were early syphilis cases was statistically significant (P<.001).
During 2012–2016, the increase in early syphilis cases (primary, secondary, or early latent syphilis) among pregnant women exceeded the increase in late latent syphilis cases so that the proportion of pregnant syphilis cases that were late latent decreased from 65% to 42% over the same time period (P<.001) (Fig. 1). Early syphilis cases among pregnant women increased 52% from 553 cases in 2012 to 1,065 cases in 2016. Late latent syphilis cases among pregnant women increased 43%, from 1,008 to 1,443 cases.
Overall, most (59%) pregnant women with syphilis were in their 20s and the greatest number of cases was consistently among non-Hispanic blacks, averaging 49% of reported syphilis cases among pregnant women per year. Most (56%) pregnant women with syphilis were from the South (Table 1). Reported cases of syphilis among pregnant women increased in those aged 15–45 years, in every race and ethnicity group, and in every region during 2012–2016. By age, the greatest increase in cases was seen in women aged 30–34 years (90%). By race and ethnicity, the greatest increase in cases was among Native Americans or Alaskan Natives (420%). By region, the greatest increase was seen in the West (292%) followed by the North (44%), the Midwest (35%), and the South (29%).
Table 1.
Demographic Characteristics of Pregnant Women With Reported Syphilis Cases (All Stages), 2012–2016*
| Demographic | 2012 (n = 1,561) | 2013 (n = 1,633) | 2014 (n = 1,955) | 2015 (n = 2,226) | 2016 (n = 2,508) | 2012–2016* (n = 9,883) |
|---|---|---|---|---|---|---|
| Age (y) | ||||||
| Younger than 15 | 1 (0.1) | 5 (0.3) | 6 (0.3) | 3 (0.1) | 1 (0.04) | 16 (0.2) |
| 15–19 | 227 (14.5) | 212 (13.0) | 253 (12.9) | 235 (10.6) | 307 (12.2) | 1,234 (12.5) |
| 20–24 | 522 (33.4) | 560 (34.3) | 626 (32.0) | 748 (33.6) | 772 (30.8) | 3,228 (32.7) |
| 25–29 | 378 (24.2) | 375 (23.0) | 524 (26.8) | 594 (26.7) | 689 (27.5) | 2,560 (25.9) |
| 30–34 | 238 (15.3) | 268 (16.4) | 326 (16.7) | 396 (17.8) | 451 (18.0) | 1,679 (17.0) |
| 35–39 | 140 (9.0) | 166 (10.2) | 165 (8.4) | 188 (8.5) | 212 (8.5) | 871 (8.8) |
| 40–44 | 44 (2.8) | 43 (2.6) | 53 (2.7) | 54 (2.4) | 66 (2.6) | 260 (2.6) |
| Older than 45 | 11 (0.7) | 3 (0.2) | 2 (0.1) | 8 (0.4) | 9 (0.4) | 33 (0.3) |
| Race and Hispanic ethnicity | ||||||
| Native American or Alaskan Native | 5 (0.3) | 12 (0.8) | 15 (0.8) | 15 (0.7) | 26 (1.1) | 73 (0.7) |
| Asian or Pacific Islander | 47 (3.2) | 59 (3.8) | 63 (3.5) | 93 (4.5) | 78 (3.3) | 340 (3.4) |
| Hispanic | 394 (26.4) | 460 (29.7) | 555 (30.4) | 625 (30.0) | 755 (31.8) | 2,789 (28.2) |
| Non-Hispanic black | 833 (55.8) | 781 (50.5) | 876 (48.0) | 946 (45.4) | 1,070 (45.0) | 4,506 (45.6) |
| Non-Hispanic white | 215 (14.4) | 236 (15.3) | 316 (17.3) | 405 (19.4) | 448 (18.9) | 1,620 (16.4) |
| Region | ||||||
| Midwest | 235 (15.1) | 203 (12.4) | 234 (12.0) | 294 (13.2) | 316 (12.6) | 1,282 (13.0) |
| Northeast | 187 (12.0) | 195 (11.9) | 234 (12.0) | 228 (10.2) | 270 (10.8) | 1,114 (11.3) |
| South | 965 (61.8) | 969 (59.3) | 1,132 (57.9) | 1,212 (54.5) | 1,240 (49.4) | 5,518 (55.8) |
| West | 174 (11.2) | 266 (16.3) | 355 (18.2) | 492 (22.1) | 682 (27.2) | 1,969 (19.9) |
Data are n (%).
Column totals may not add up to total number of cases or 100% because of cases reported with missing or unknown data.
Combining data from 2012 to 2016, the overall prevalence of any reported risk factor was 51% (4,997/9,883) (Table 2). Stated differently, 49% of pregnant women with syphilis did not report having any high-risk behaviors. The most commonly reported risk behaviors, in pregnant women with any stage of syphilis, were prior STD (43%) and more than one sex partner in the past 12 months (30%). When the analysis was restricted to pregnant women with early syphilis, representing women with a recent infection, the overall prevalence of any reported risk factor was slightly higher at 63% (2,434/3,850) (Table 3). These women reported the same risk behaviors most commonly, but again in higher proportions, with 50% reporting a prior STD and 38% reporting more than one sex partner. Of the specific drugs surveyed, the highest overall prevalence was for methamphetamine use in pregnant women with all stages (4.5%) and in pregnant women with early syphilis (6.3%).
Table 2.
Reported Risk Factors Among Pregnant Women With Syphilis (All Stages), 2012–2016
| Reported Risk Factor* | 2012 (n=1,561) | 2013 (n=1,633) | 2014 (n=1,955) | 2015 (n=2,226) | 2016 (n=2,508) | 2012–2016*† (n=9,883) |
|---|---|---|---|---|---|---|
| Prior STDठ| 452/1,135 (39.8) | 512/1,196 (42.8) | 581/1,410 (41.2) | 673/1,544 (43.6) | 831/1,740 (47.8) | 3,049/7,025 (43.4) |
| More than 1 sex partner | 387/1,258 (30.8) | 421/1,301 (32.4) | 457/1,570 (29.1) | 495/1,784 (27.8) | 656/2,063 (31.8) | 2,416/7,976 (30.3) |
| Sex while intoxicated | 177/1,165 (15.2) | 178/1,200 (14.8) | 212/1,455 (14.6) | 272/1,629 (16.7) | 301/1,873 (16.1) | 1,140/7,322 (15.6) |
| Anonymous sex partner | 98/1,152 (8.5) | 94/1,187 (7.9) | 117/1,466 (8.0) | 157/1,622 (9.7) | 177/1,873 (9.5) | 643/7,300 (8.7) |
| Incarceration | 87/1,157 (7.5) | 86/1,198 (7.2) | 104/1,463 (7.1) | 114/1,627 (7.0) | 171/1,865 (9.2) | 562/7,310 (7.7) |
| Sex for drugs or money | 49/1,173 (4.2) | 48/1,213 (4.0) | 52/1,460 (3.6) | 62/1,651 (3.8) | 61/1,907 (3.2) | 272/7,404 (3.7) |
| Sex with persons known to inject drugs§ | 21/1,122 (1.9) | 32/1,149 (2.8) | 35/1,394 (2.5) | 65/1,575 (4.1) | 79/1,771 (4.5) | 232/7,011 (3.3) |
| HIV-positive‡ | 13/1,071 (1.2) | 18/1,080 (1.7) | 13/1,330 (1.0) | 26/1,420 (1.8) | 31/1,877 (1.7) | 101/6,788 (1.5) |
| Sex with MSM∥ | 11/1,106 (1.0) | 11/1,121 (1.0) | 11/1,344 (0.8) | 19/1,539 (1.2) | 35/1,727 (2.0) | 87/6,837 (1.3) |
| Methamphetamine use∥ | 24/1,081 (2.2) | 22/1,147 (1.9) | 47/1,411 (3.3) | 94/1,523 (6.2) | 129/1,827 (7.1) | 316/6,986 (4.5) |
| Cocaine use | 30/1,083 (2.8) | 22/1,147 (1.9) | 41/1,409 (2.9) | 37/1,524 (2.4) | 43/1,812 (2.4) | 173/6,975 (2.5) |
| Crack use | 25/1,083 (2.3) | 14/1,146 (1.2) | 21/1,408 (1.5) | 18/1,522 (1.2) | 25/1,809 (1.4) | 103/6,968 (1.5) |
| Heroin use | 17/1,082 (1.6) | 18/1,146 (1.6) | 18/1,407 (1.3) | 30/1,524 (2.0) | 26/1,816 (1.4) | 109/6,975 (1.6) |
| Injection drug use | 24/1,136 (2.1) | 29/1,155 (2.5) | 27/1,434 (1.9) | 51/1,567 (3.3) | 50/1,733 (2.9) | 181/7,025 (2.6) |
| Nitrates or poppers use | 2/1,066 (0.2) | 1/1,144 (0.1) | 4/1,406 (0.3) | 6/1,519 (0.4) | 7/1,772 (0.4) | 20/6,907 (0.3) |
| Other drug use | 115/1,080 (10.7) | 138/1,146 (12.0) | 198/1,407 (14.1) | 198/1,531 (12.9) | 226/1,826 (12.4) | 875/6,990 (12.5) |
| Any risk factor§∥ | 747/1,561 (47.9) | 828/1,633 (50.7) | 987/1,955 (50.5) | 1,095/2,226 (49.2) | 1,340/2,508 (53.4) | 4,997/9,883 (50.6) |
STD, sexually transmitted disease; HIV, human immunodeficiency virus; MSM, men who have sex with men.
Data are n/N (%).
Timing of risk factors referred to the last 12 months before diagnosis of syphilis except: prior STD (lifetime risk); HIV-positive (documented or self-reported at the time of syphilis diagnosis).
Values are a sum of data from 2012 to 2016. Denominators vary because number missing or unknown (excluded) varies by risk factor.
Timing of risk factors referred to the last 12 months before diagnosis of syphilis except: prior STD (lifetime risk); HIV-positive (documented or self-reported at the time of syphilis diagnosis).
Change in proportion was statistically significant (P<.05).
Combines all risk factors.
Table 3.
Reported Risk Factors Among Pregnant Women With Early Syphilis, 2012–2016 (n=3,850)
| Reported Risk Factor* | n/N*† (%) |
|---|---|
| Prior STD‡ | 1,524/3,021 (50.4) |
| Greater than 1 sex partner | 1,317/3,436 (38.3) |
| Sex while intoxicated | 628/3,215 (19.5) |
| Anonymous sex partner | 337/3,193 (10.6) |
| Incarceration | 304/3,212 (9.5) |
| Sex for drugs or money | 154/3,245 (4.7) |
| Sex with persons known to inject drugs | 132/3,047 (4.3) |
| HIV-positive‡ | 53/2,863 (1.9) |
| Sex with MSM | 61/2,933 (2.1) |
| Methamphetamine use | 192/3,052 (6.3) |
| Cocaine use | 81/3,043 (2.7) |
| Crack use | 47/3,038 (1.5) |
| Heroin use | 63/3,044 (2.1) |
| Injection drug use | 101/3,050 (3.3) |
| Nitrates or poppers use | 13/3,010 (0.4) |
| Other drug use | 481/3,053 (15.8) |
| Any risk factor§ | 2,434/3,850 (63.2) |
STD, sexually transmitted disease; HIV, human immunodeficiency virus; MSM, men who have sex with men.
Timing of risk factors referred to the last 12 months before diagnosis of syphilis except: prior STD (lifetime risk); HIV-positive (documented or self-reported at the time of syphilis diagnosis).
Values are a sum of data from 2012 to 2016. Denominators vary because number missing or unknown (excluded) varies by risk factor.
Timing of risk factors referred to the last 12 months before diagnosis of syphilis except: prior STD (lifetime risk); HIV-positive (documented or self-reported at the time of syphilis diagnosis).
Combines all risk factors.
For trends in reported risk behaviors over time, the proportion of pregnant women, with any stage of syphilis, reporting a prior STD increased (P<.001) as did the proportion of women reporting having sex with a known injection drug user (P<.001) and the proportion reporting having sex with a partner known to be a man who has sex with men (P=.0076) (Table 2). The proportion of pregnant women with syphilis reporting crack, cocaine, or heroin use in the past 12 months decreased or remained stable over time as did the proportion reporting having sex in exchange for drugs or money. The proportion reporting injection drug use was stable. Of the drugs surveyed, the largest increase was in methamphetamine use reported by pregnant women with syphilis. From 2012 to 2016, the proportion reporting methamphetamine use more than doubled from 2.2% to 7.1% (P<.001).
DISCUSSION
Syphilis cases among pregnant women increased among all demographic groups from 2012 to 2016. Of these cases, the proportion that was early syphilis also rose, which is concerning because these represent more recent infections with higher titers and a greater risk of mother-to-child transmission. Our data demonstrate that screening relying solely on behavioral risk factors would miss approximately half of pregnant women with any stage of syphilis and approximately one third of pregnant women with recently acquired syphilis.
These findings support current recommendations for universal syphilis screening at the first prenatal visit and indicate that it may be necessary to include population context when determining whether to implement repeat screening during pregnancy. The CDC and the American College of Obstetricians and Gynecologists both recommend repeat screening between 28 0/7 weeks and 32 0/7 weeks of estimated gestation and again at delivery for pregnant women in communities and populations with a high prevalence of syphilis.5 Health departments, particularly in areas with a high burden of female syphilis, should ensure that health care providers are aware of local syphilis prevalence and regulations for prenatal syphilis screening.
Although identification of risk behaviors may only detect less than half of the pregnant women with syphilis, women who do report risk factors, particularly drug use, likely require special attention and additional efforts to prevent congenital syphilis. Socioeconomic factors and risk behaviors such as drug use are intimately related and both have been shown to affect the uptake of prenatal care, which in turn affects timely syphilis screening and treatment.18,19 Moreover, even when these women are adequately screened and offered treatment, they likely remain at a higher risk for being lost to follow-up, for not receiving adequate treatment, and for having reinfection after treatment.
These data and this analysis have limitations. As a result of the lack of current data on the number of pregnancies in the United States, we were unable to calculate syphilis rates per 100,000 pregnant women. Therefore, trend data or comparisons between demographic groups might be affected by changes in the pregnancy rates over time or differences in pregnancy rates in different demographic groups. We considered using the number of live births per year to calculate a ratio of pregnant women with syphilis per 1,000 live births. However, given that pregnancies complicated by maternal syphilis can result in miscarriage or stillbirth, these cases would not have been included in the denominator of live births. The sample we described included any pregnant woman with syphilis, regardless of pregnancy outcome. Moreover, the number of live births from 2012 to 2016 was relatively stable and did not fluctuate more than 1.5% over this time period.20 In addition, STD surveillance data have inherent limitations. Case-based surveillance data likely underestimate the true number of syphilitic infections among pregnant women in the country as a result of underascertainment and underreporting of syphilitic infections and pregnancy status. For instance, if all women with syphilis with unknown pregnancy status were pregnant, the estimated number of pregnant women with syphilis in 2016 would be more than double our estimate (from 2,508 to 5,523); however, it is unlikely that all or most women with unknown pregnancy status were truly pregnant. It is possible that women with unknown pregnancy status are more likely to have risk factors, so exclusion from our analysis could underestimate prevalence of reported risk factors among pregnant women. Analysis of reported behavioral risk data is also limited given these data are collected in an interview format and the completion of the report form is performed at the interpretation and discretion of a local health officer. Moreover, the personal nature of some of the behavioral questions, along with a fear of legal repercussions including the possible loss of custody of children, may also contribute to underreporting of risk factors. Finally, our data did not include information about pregnancy outcome, and we were unable to link pregnant syphilis cases to reported congenital syphilis cases. Thus, we were not able to examine whether certain risk behaviors were associated with congenital syphilis or adverse pregnancy outcomes.
Despite these limitations, this study adds to the limited information on national trends in demographic data and reported behavioral risk factor data among pregnant women with syphilis. Through an increased awareness of the rising syphilis cases among pregnant women as well as these trend data, health care providers can be better informed to ensure they are following national guidelines and state policies for syphilis screening in pregnancy. Lastly, we hope that these data and the continued collection of surveillance data, including risk factors, may help guide the evolution of future public health interventions so they are tailored to the socioeconomic factors and behaviors of this population.
Footnotes
Financial Disclosure
The authors did not report any potential conflicts of interest.
Presented as a poster at the American College of Obstetricians and Gynecologists’ Annual Clinical and Scientific Meeting, Austin, Texas, April 27–30, 2018.
The findings and conclusions in this manuscript are those of the authors and do not necessarily represent the views of the Centers for Disease Control and Prevention.
REFERENCES
- 1.Ingraham NR Jr. The value of penicillin alone in the prevention and treatment of congenital syphilis. Acta Derm Venereol Suppl (Stockh) 1950;31(suppl 24):60–87. [PubMed] [Google Scholar]
- 2.Gomez GB, Kamb ML, Newman LM, Mark J, Broutet N, Hawkes SJ. Untreated maternal syphilis and adverse outcomes of pregnancy: a systematic review and meta-analysis. Bull World Health Organ 2013;91:217–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cooper JM, Sánchez PJ. Congenital syphilis. Semin Perinatol 2018;42:176–84. [DOI] [PubMed] [Google Scholar]
- 4.Alexander JM, Sheffield JS, Sanchez PJ, Mayfield J, Wendel GD Jr. Efficacy of treatment for syphilis in pregnancy. Obstet Gynecol 1999;93:5–8. [DOI] [PubMed] [Google Scholar]
- 5.Workowski KA, Bolan GA; Centers for Disease Control and Prevention. Sexually transmitted diseases treatment guidelines, 2015. MMWR Recomm Rep 2015;64:1–137. [PMC free article] [PubMed] [Google Scholar]
- 6.Centers for Disease Control and Prevention. Sexually transmitted disease surveillance 2016. Atlanta (GA): U.S. Department of Health and Human Services; 2017. [Google Scholar]
- 7.Biswas HH, Chew Ng RA, Murray EL, Chow JM, Stoltey JE, Watt JP, et al. Characteristics associated with delivery of an infant with congenital syphilis and missed opportunities for prevention—California, 2012–2014. Sex Transm Dis 2018; 45:435–41. [DOI] [PubMed] [Google Scholar]
- 8.Matthias JM, Rahman MM, Newman DR, Peterman TA. Effectiveness of prenatal screening and treatment to prevent congenital syphilis, Louisiana and Florida, 2013–2014. Sex Transm Dis 2017;44:498–502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kidd S, Bowen VB, Torrone EA, Bolan G. Use of national syphilis surveillance data to develop a congenital syphilis prevention cascade and estimate the number of potential congenital syphilis cases averted. Sex Transm Dis 2018;45(suppl 1):S23–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Patel SJ, Klinger EJ, O’Toole D, Schillinger JA. Missed opportunities for preventing congenital syphilis infection in New York City. Obstet Gynecol 2012;120:882–8. [DOI] [PubMed] [Google Scholar]
- 11.Taylor MM, Mickey T, Browne K, Kenney K, England B, Blasini-Alcivar L. Opportunities for the prevention of congenital syphilis in Maricopa County, Arizona. Sex Transm Dis 2008;35:341–3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Warner L, Rochat RW, Fichtner RR, Stoll BJ, Nathan L, Toomey KE. Missed opportunities for congenital syphilis prevention in an urban southeastern hospital. Sex Transm Dis 2001; 28:92–8. [DOI] [PubMed] [Google Scholar]
- 13.Healthy People 2020. Sexually transmitted diseases—social, economic, and behavioral factors. Available at: https://www.healthypeople.gov/2020/topics-objectives/topic/sexually-transmitted-diseases. Retrieved May 15, 2018.
- 14.Marx R, Aral SO, Rolfs RT, Sterk CE, Kahn JG. Crack, sex, and STD. Sex Transm Dis 1991;18:92–101. [DOI] [PubMed] [Google Scholar]
- 15.Eng TR, Butler WT, editors. The hidden epidemic: confronting sexually transmitted diseases: summary. Washington, DC: National Academies Press; 1997. [PubMed] [Google Scholar]
- 16.Kirkcaldy RD, Su JR, Taylor MM, Koumans E, Mickey T, Winscott M, et al. Epidemiology of syphilis among Hispanic women and associations with congenital syphilis, Maricopa County, Arizona. Sex Transm Dis 2011;38:598–602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.National Vital Statistics System. United States census 2000 population with bridged race categories In: Centers for Disease Control and Prevention National Center for Health Statistics. Hyattsville (MD): U.S. Department of Health and Human Services; 2003. [Google Scholar]
- 18.Funkhouser AW, Butz AM, Feng TI, McCaul ME, Rosenstein BJ. Prenatal care and drug use in pregnant women. Drug Alcohol Depend 1993;33:1–9. [DOI] [PubMed] [Google Scholar]
- 19.Maupin R Jr, Lyman R, Fatsis J, Prystowiski E, Nguyen A, Wright C, et al. Characteristics of women who deliver with no prenatal care. J Matern Fetal Neonatal Med 2004;16:45–50. [DOI] [PubMed] [Google Scholar]
- 20.Martin JA, Hamilton BE, Osterman MJK, Driscoll AK, Drake P. Births: final data for 2016. Natl Vital Stat Rep 2018;67:1–55. [PubMed] [Google Scholar]