Abstract
Background: Depression is associated with weight change outside of pregnancy. We assessed associations of prepregnancy or early pregnancy onset depression with gestational weight gain (GWG) rate overall and according to Institute of Medicine (IOM) recommendations.
Materials and Methods: Depression from 6 months prepregnancy through 20 weeks gestation was identified in a health care system in northern California with perinatal depression screening (2011–2016; n = 87,600). GWG rate (lbs/week) was calculated using weight at delivery and at diagnosis or depression screening ≤20 weeks.
Results: Compared to women without prepregnancy or early pregnancy depression, women with prepregnancy onset depression had 11% greater risk of GWG rate <IOM recommendations (95% confidence intervals [CI]: 1.07–1.15) and 3% greater risk of GWG rate >IOM recommendations (95% CI: 1.01–1.05), with a stronger association for >IOM in normal weight women. Early pregnancy onset depression was associated with 0.04 lbs/week greater GWG rate (95% CI: 0.02–0.07) and 4% greater risk of GWG rate >IOM recommendations (95% CI: 1.02–1.07) compared to no prepregnancy or early pregnancy depression, with stronger associations in obese women.
Conclusions: Women with prepregnancy onset depression may be at higher risk for GWG both below and above recommendations. Women with early onset prenatal depression may be at slightly higher risk for GWG rate above recommendations. Our results suggest that the relationship between depression and GWG may vary based on timing of depression onset, prepregnancy body mass index category, and antidepressant use. Additional research should identify factors that predict how a woman's lifestyle behaviors and weight change after depression diagnosis.
Keywords: pregnancy, depression, gestational weight gain, perinatal depression
Introduction
Both inadequate and excessive gestational weight gain (GWG) are associated with adverse maternal and newborn outcomes. The Institute of Medicine (IOM) recommends prepregnancy body mass index (BMI)-specific ranges for total GWG across pregnancy and weekly GWG rate across the second and third trimesters that balance the risks for adverse maternal outcomes, such as cesarean delivery, and adverse newborn outcomes, such as small- and large-for-gestational age birth weight and preterm birth.1,2 GWG within the IOM recommendations is associated with reduced risk of preterm birth and small-for-gestational age compared to GWG below the recommendations.3 GWG within the IOM recommendations is also associated with reduced risk of cesarean delivery and large-for-gestational age compared to GWG above the recommendations.3
Reproductive-age women are at high risk of depression.4 In the United States, depression affects 14% of nonpregnant reproductive-age women and between 7% and 12% of pregnant women.5–7 Women with depressive symptoms before and during pregnancy may be at especially high risk for GWG outside the IOM recommendations, given associations of depression with both weight loss and weight gain outside of pregnancy.8–11 Individuals with depression may experience either increased or decreased appetite,12 decreased dietary quality,13,14 and reduced physical activity,15–17 which may contribute to weight changes. Previous studies have found inconsistent associations of prenatal depression with total GWG, calculated from the beginning of pregnancy, and were unable to look at the prospective association between depression and subsequent GWG.18–20 The objective of this study was to determine whether pre- or early pregnancy depression was prospectively associated with GWG rate or risk of GWG rate outside the IOM recommendations after depression screening.
Materials and Methods
Study setting and study population
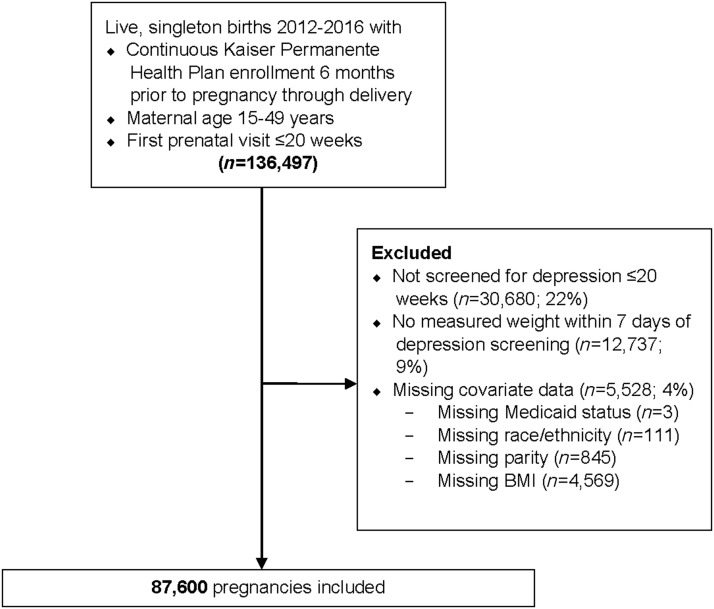
This study was conducted within Kaiser Permanente Northern California (KPNC), an integrated health care delivery system that provides medical care for about one third of the population in the San Francisco Bay Area. KPNC members are representative of the underlying population of this region.21 KPNC members with pregnancies from 2011 to 2016 that ended in a live singleton birth were identified from the KPNC electronic health record database. Inclusion and exclusion criteria are described in Figure 1. The final analytic sample consisted of 87,600 pregnancies among 79,506 women.
FIG. 1.
Inclusion and exclusion criteria.
Data collection
Data were collected during routine primary and prenatal care visits and entered into the electronic health record database. Prepregnancy BMI was calculated using the prepregnancy (within 12 months before pregnancy) weight measured closest to the start of pregnancy (88% of analytic sample). If a measured weight within 12 months before pregnancy was not available, the first measured weight in the first 10 weeks of pregnancy was used (12%). In women 15–19 years of age, prepregnancy BMI was categorized using the Centers for Disease Control and Prevention 2000 BMI-for-age Growth Charts: underweight: <5th percentile, normal weight: 5th–84.9th percentile, overweight: 85th–94.9th percentile, and obese: ≥95th percentile.22 In women 20 years of age and older, prepregnancy BMI was categorized using standard adult cutoff points: underweight: <18.5 kg/m2, normal weight: 18.5–24.9 kg/m2, overweight: 25–29.9 kg/m2, and obese: ≥30 kg/m2.23 This study was approved by the KPNC institutional review board.
Pre- and early pregnancy depressive symptoms
Prepregnancy onset depression was identified using depression diagnosis codes and antidepressant medication dispensing. Women were considered to have prepregnancy onset depression if they had at least one International Classification of Diseases, 9th Revision diagnosis code for depression (296.20–296.25, 296.30–296.35, 296.82, 298.0, 300.4, 309.0, 309.1, 309.28, 311, or 648.41–648.44), at least one International Classification of Diseases, 10th Revision diagnosis code for depression (F32.0-F32.4, F32.89, F32.9, F33.0-F33.3, F33.41, F33.9, F34.1, F43.21, F43.23, 099.341, 099.342, or 099.343), at least one Kaiser Permanente combination code for depression (501223 or 5027004), or at least one antidepressant medication dispensing (selective serotonin reuptake inhibitor, serotonin and norepinephrine reuptake inhibitors, tricyclic antidepressants, serotonin antagonist and reuptake inhibitor, norepinephrine dopamine reuptake inhibitor, monoamine oxidase inhibitor, serotonin partial agonist-reuptake inhibitor, selective norepinephrine reuptake inhibitor, noradrenergic and specific serotonergic antidepressant; Supplementary Table S1) in the 6 months before pregnancy. Used together, depression diagnosis codes and antidepressant medication dispensing information in the electronic health record is a valid measure of depression (sensitivity = 85%, specificity = 73%, area under the curve = 0.79).24
In women with no prepregnancy onset depression, early onset prenatal depression was identified using depression diagnosis codes or PHQ-9 screening scores. The PHQ-9 is a reliable and valid self-administered questionnaire, which assesses each of the nine criteria upon which depression diagnosis is based.25 The PHQ-9 has high sensitivity (>88%) and specificity (>88%) in obstetric patients for scores ≥10.25–29 It has been adopted by clinicians and researchers for screening in populations, including pregnant and postpartum women,30–34 and is considered the dimensional depression measure in the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-V) classification manual.35 Each of the nine items is scored from 0 (not at all) to 3 (nearly every day) for a total score ranging from 0 to 27. Scores of 5, 10, and 15 are considered the lower cutoff points for mild, moderate, and moderately severe to severe depression, respectively.25 Women were considered to have early onset prenatal depression if they had at least one depression code (listed above) or a positive depression screening (PHQ-9 score ≥10) within the first 20 weeks of pregnancy. For women with early onset prenatal depression, severity of depressive symptoms was categorized as mild (PHQ-9 < 10), moderate (PHQ-9 10–14), or severe (PHQ-9 ≥ 15).
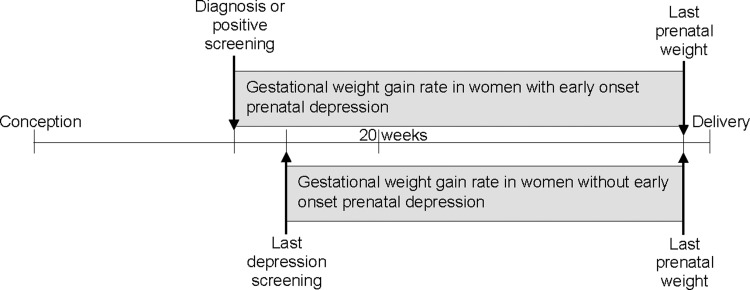
GWG rate
Among women with early onset prenatal depression, rate of GWG (lbs/week) was calculated using weight at depression screening (weight measured within 7 days of early pregnancy depression diagnosis or positive depression screening) and last prenatal weight before delivery divided by the difference in gestational weeks between the two measurements (Fig. 2). Among women without early onset prenatal depression, GWG rate was calculated using weight at last depression screening before 20 weeks gestation and last prenatal weight before delivery divided by the difference in gestational weeks between the two measurements. Rate of GWG was categorized based on the recommended ranges for rate of GWG according to the IOM (below, within, above; Supplementary Table S2).1
FIG. 2.
Gestational weight gain rate in women with and without early onset prenatal depression.
Statistical analyses
Descriptive statistics were calculated in the overall analytic population and stratified by categories based on prepregnancy onset depression and early onset prenatal depression. Mean and standard deviation were used to describe the distribution of continuous variables. Frequency and percent were used to describe categorical variables.
Multiple linear regression was used to estimate mean differences and 95% confidence intervals (CI) in GWG rate associated with prepregnancy onset depression and early onset prenatal depression. Modified Poisson regression36 was used to estimate relative risks (RR) and 95% CIs for GWG rate category associated with prepregnancy onset depression and early onset prenatal depression. Depression categories were treated as a three-level exposure (prepregnancy onset depression, early pregnancy onset depression, and no pre- or early pregnancy onset depression). Separate Poisson regression models were run comparing below versus within IOM recommendations and above versus within IOM recommendations. Regression parameter estimates were obtained using generalized estimating equations to account for the nonindependence of pregnancies for women with multiple pregnancies during the study period. The model was adjusted for a priori selected covariates associated with perinatal depression and GWG37,38: maternal age (years), race/ethnicity (non-Hispanic white, non-Hispanic black, Hispanic, Asian/Pacific Islander, Native American/multiracial, other/unknown), nulliparity (Y/N), Medicaid (Y/N), smoking in the first 20 weeks of pregnancy (Y/N), alcohol use in the first 20 weeks of pregnancy (Y/N), and prepregnancy BMI category (underweight, normal weight, overweight, and obese). In additional analyses, models were stratified by prepregnancy BMI category, early pregnancy depression severity (mild, moderate, and severe), and race/ethnicity. Exposure groups taking antidepressant treatment during pregnancy into account were also created (prepregnancy onset depression treated with antidepressants in early pregnancy, prepregnancy onset depression not treated with antidepressants in early pregnancy, early pregnancy onset depression treated with antidepressants, and early pregnancy onset depression not treated with antidepressants).
We conducted sensitivity analyses using GWG rate calculated using weight at the first depression screening through 20 weeks gestation, as opposed to weight at the last depression screening through 20 weeks gestation, among women without early onset prenatal depression. This was done to account for potential differences in timing of depression screening between women with early onset prenatal depression and women without early onset prenatal depression. We also conducted sensitivity analyses excluding women without a measured prepregnancy weight in the 12 months before pregnancy and sensitivity analyses in nulliparous women with last measured weight ≥37 weeks. A two-sided alpha level of 0.05 was used for statistical significance in all analyses. Analyses were performed using SAS 9.3 (SAS Institute, Inc., Cary NC) and R 3.4.1.39
Results
In our study population, women had prepregnancy onset depression in 9% of pregnancies and early onset prenatal depression in 8% of pregnancies (Table 1). Women with prepregnancy onset depression were more likely to be non-Hispanic white and prepregnancy obese than women with early onset prenatal depression or no pre- or early pregnancy onset depression. Women with early onset prenatal depression were more likely to be non-Hispanic black or Hispanic compared to women with prepregnancy onset depression or no pre- or early pregnancy depression. Women with pregnancies with either pre- or early pregnancy onset depression were more likely to receive Medicaid and smoke during early pregnancy than women with pregnancies without pre- or early pregnancy onset depression. Most women with prepregnancy onset depression were treated with medication, with or without counseling. Most women with early onset prenatal depression were treated with counseling only or did not receive any treatment.
Table 1.
Characteristics of Pregnancies by Prepregnancy Depression and Early Onset Prenatal Depression, Kaiser Permanente Northern California 2011–2016
| Total (N = 87,600) | Prepregnancy onset depression (N = 7696) | Early pregnancy onset depression (N = 7337) | No pre- or early pregnancy depression (N = 72,567) | |
|---|---|---|---|---|
| Sociodemographic characteristics | ||||
| Age (years), mean (SD) | 30.2 (5.4) | 30.1 (5.8) | 29.3 (6.0) | 30.3 (5.3) |
| Race/ethnicity, n (%) | ||||
| Non-Hispanic white | 35,991 (41) | 4238 (55) | 1963 (27) | 29,790 (41) |
| Non-Hispanic black | 5011 (6) | 535 (7) | 807 (11) | 3669 (5) |
| Hispanic | 21,733 (25) | 1878 (24) | 2223 (30) | 17,632 (24) |
| Asian/Pacific Islander | 20,994 (24) | 639 (8) | 1987 (27) | 18,368 (25) |
| Native American/multiracial | 3117 (4) | 352 (5) | 281 (4) | 2484 (3) |
| Other/unknown | 754 (1) | 54 (1) | 76 (1) | 624 (1) |
| Prepregnancy BMI category, n (%) | ||||
| Underweight | 2390 (3) | 174 (2) | 223 (3) | 1893 (3) |
| Normal weight | 42,304 (48) | 3072 (40) | 3430 (47) | 35,802 (49) |
| Overweight | 23,605 (27) | 2085 (27) | 1994 (27) | 19,526 (27) |
| Obese | 19,401 (22) | 2365 (31) | 1690 (23) | 15,346 (21) |
| Timing of measured weight used for prepregnancy BMI, n (%) | ||||
| Within 12 months before pregnancy | 76,713 (88) | 7357 (96) | 6549 (89) | 62,807 (87) |
| Within first 10 weeks of pregnancy | 10,887 (12) | 339 (4) | 788 (11) | 9760 (13) |
| Medicaid, n (%) | 5688 (6) | 984 (13) | 771 (11) | 3933 (5) |
| Pregnancy characteristics | ||||
| Nulliparous, n (%) | 31,545 (36) | 2674 (37) | 2742 (37) | 26,129 (36) |
| Smoking during early pregnancy, n (%) | 3591 (4) | 717 (9) | 567 (8) | 2307 (3) |
| Alcohol use during early pregnancy, n (%) | 31,411 (36) | 3096 (40) | 2424 (33) | 25,891 (36) |
| Gestational age at first prenatal visit (weeks), mean (SD) | 6.3 (2.2) | 5.9 (2.2) | 6.2 (2.2) | 6.3 (2.2) |
| Gestational age at diagnosis or last PHQ-9 before 20 weeks gestation (weeks), mean (SD) | 9.2 (2.6) | 8.9 (3.3) | 9.3 (3.3) | 9.2 (2.4) |
| Gestational age at last weight before delivery (weeks), mean (SD) | 38.6 (1.9) | 38.4 (2.1) | 38.5 (2.0) | 38.6 (1.9) |
| GWG rate (lbs/week), mean (SD) | 0.92 (0.42) | 0.92 (0.49) | 0.94 (0.48) | 0.92 (0.41) |
| IOM GWG rate category, n (%) | ||||
| Below guidelines | 20,582 (24) | 1877 (24) | 1721 (23) | 16,984 (23) |
| Meets guidelines | 18,534 (21) | 1373 (18) | 1448 (20) | 15,713 (22) |
| Exceeds guidelines | 48,484 (55) | 4446 (58) | 4168 (57) | 39,870 (55) |
| Depression severity and treatment | ||||
| Depression treatment in prepregnancy, n (%) | ||||
| Medication and counseling | 2174 (28) | |||
| Medication only | 3502 (46) | |||
| Counseling only | 1146 (15) | |||
| No treatment | 874 (11) | |||
| Early pregnancy depressive symptom severity, n (%) | ||||
| Very mild (PHQ-9 0–4) | 3893 (51) | 584 (8) | ||
| Mild (PHQ-9 5–9) | 2299 (30) | 480 (7) | ||
| Moderate (PHQ-9 10–14) | 912 (12) | 4699 (64) | ||
| Severe (PHQ-9 ≥ 15) | 592 (27) | 1574 (21) | ||
| Depression treatment in early pregnancy, n (%) | ||||
| Medication and counseling | 1354 (18) | 221 (3) | 95 (0) | |
| Medication only | 788 (10) | 66 (1) | 94 (0) | |
| Counseling only | 2656 (35) | 3042 (41) | 17,859 (25) | |
| No treatment | 2898 (38) | 4008 (55) | 54,519 (75) | |
| Later pregnancy depressive symptoms (after 20 weeks), n (%) | ||||
| Yes | 10,922 (12) | 3754 (49) | 2230 (30) | 4938 (7) |
| No | 49,614 (57) | 2568 (33) | 3190 (43) | 43,856 (60) |
| No PHQ-9 after 20 weeks | 27,064 (31) | 1374 (18) | 1917 (26) | 23,773 (33) |
SD, standard deviation; IOM, Institute of Medicine; GWG, gestational weight gain; BMI, body mass index.
Prepregnancy onset depression was not associated with GWG rate (mean difference = 0.00; 95% CI: −0.01 to 0.01; Table 2). Adjustment for depression treatment in early pregnancy did not change the results. Early onset prenatal depression was associated with 0.04 lbs/week greater GWG rate (95% CI: 0.02–0.07) compared to no pre- or early pregnancy onset depression.
Table 2.
Associations of Prepregnancy and Early Pregnancy Onset Depression with Gestational Weight Gain Rate Starting at Depression Screening or Diagnosis (lbs/Week)
| N | Mean differencea (95% CI) | |
|---|---|---|
| No pre- or early pregnancy depression | 72,567 | Reference |
| Prepregnancy onset depression | 7696 | 0.00 (−0.01 to 0.01) |
| Early pregnancy onset depression | 7337 | 0.04 (0.02 to 0.07) |
Model is adjusted for maternal age, race/ethnicity (non-Hispanic white, non-Hispanic black, Hispanic, Asian/Pacific Islander, Native American/multiracial, other/unknown), nulliparity (Y/N), Medicaid (Y/N), smoking in first 20 weeks of pregnancy (Y/N), alcohol use in first 20 weeks of pregnancy (Y/N), prepregnancy BMI category (underweight, normal weight, overweight, obese), and severity of early pregnancy depressive symptoms (mild, moderate, severe).
CI, confidence intervals.
Prepregnancy onset depression was associated with 11% greater risk of GWG rate below the IOM recommendations and 3% greater risk of GWG rate above the IOM recommendations (95% CI: 1.07–1.15 and 1.01–1.05, respectively; Table 3). Early onset prenatal depression was associated with 4% greater risk of GWG rate above the IOM recommendations (95% CI: 1.02–1.07).
Table 3.
Associations of Prepregnancy and Early Pregnancy Onset Depression with Gestational Weight Gain Rate Category
| N | RRa (95% CI) | |
|---|---|---|
| GWG rate below the IOM recommendations | ||
| No pre- or early pregnancy depression | 16,970 | Reference |
| Prepregnancy onset depression | 1880 | 1.11 (1.07, 1.15) |
| Early pregnancy onset depression | 1716 | 1.03 (0.97, 1.10) |
| GWG rate above the IOM recommendations | ||
| No pre- or early pregnancy depression | 39,908 | Reference |
| Prepregnancy onset depression | 4451 | 1.03 (1.01, 1.05) |
| Early pregnancy onset depression | 4176 | 1.04 (1.02, 1.07) |
Model is adjusted for maternal age, race/ethnicity (non-Hispanic white, non-Hispanic black, Hispanic, Asian/Pacific Islander, Native American/multiracial, other/unknown), nulliparity (Y/N), Medicaid (Y/N), smoking in first 20 weeks of pregnancy (Y/N), alcohol use in first 20 weeks of pregnancy (Y/N), prepregnancy BMI category (underweight, normal weight, overweight, obese), and severity of early pregnancy depressive symptoms (mild, moderate, severe).
RR, relative risks.
Associations of prepregnancy onset depression or early pregnancy onset depression with GWG rate did not differ by prepregnancy BMI category (P for interaction = 0.17; Table 4). Associations of prepregnancy onset depression with greater risk of GWG rate below IOM recommendations were similar in normal weight, overweight, and obese women (P for interaction = 0.20). Associations of prepregnancy onset depression with greater risk of GWG rate above IOM recommendations were stronger among normal weight women than overweight and obese women (RR = 1.06 in normal weight women, RR = 1.01 in overweight and obese women). Associations of early pregnancy onset depression with GWG rate or GWG rate categories did not differ by early pregnancy depression severity (Supplementary Table S3). Associations may differ by race/ethnicity (P for interaction = 0.04 for continuous GWG rate, 0.001 for GWG below IOM, 0.001 for GWG above IOM) (Supplementary Table S4). Differences in associations of prepregnancy onset depression or early pregnancy onset depression with GWG by race/ethnicity need further exploration.
Table 4.
Associations of Pre- and Early Pregnancy Onset Depression with Gestational Weight Gain Rate Starting at Depression Screening or Diagnosis (lbs/Week) Stratified by Prepregnancy Body Mass Index Category
| N | Mean differencea (95% CI) | N | RRa (95% CI) for GWG rate below the IOM recommendations | N | RRa (95% CI) for GWG rate above the IOM recommendations | |
|---|---|---|---|---|---|---|
| Underweight | ||||||
| No pre- or early pregnancy depression | 1962 | Reference | 1096 | Reference | 258 | Reference |
| Prepregnancy onset depression | 244 | 0.02 (−0.04 to 0.08) | 93 | 0.96 (0.82 to 1.11) | 35 | Did not converge |
| Early pregnancy onset depression | 188 | 0.02 (−0.07 to 0.11) | 122 | 0.97 (0.76 to 1.22) | 49 | |
| Normal weight | ||||||
| No pre- or early pregnancy depression | 35,593 | Reference | 9421 | Reference | 16,604 | Reference |
| Prepregnancy onset depression | 3383 | 0.01 (−0.01 to 0.02) | 806 | 1.14 (1.08 to 1.20) | 1574 | 1.06 (1.03 to 1.10) |
| Early pregnancy onset depression | 3044 | 0.03 (−0.01 to 0.07) | 854 | 0.97 (0.88 to 1.08) | 1694 | 1.03 (0.98 to 1.08) |
| Overweight | ||||||
| No pre- or early pregnancy depression | 19,632 | Reference | 2649 | Reference | 14,004 | Reference |
| Prepregnancy onset depression | 2011 | 0.01 (−0.01 to 0.03) | 315 | 1.15 (1.05 to 1.25) | 1499 | 1.01 (0.99 to 1.03) |
| Early pregnancy onset depression | 2097 | 0.04 (0.00 to 0.08) | 309 | 1.13 (0.98 to 1.31) | 1416 | 1.02 (0.98 to 1.07) |
| Obese | ||||||
| No pre- or early pregnancy depression | 15,380 | Reference | 3804 | Reference | 9042 | Reference |
| Prepregnancy onset depression | 1699 | −0.01 (−0.04 to 0.02) | 666 | 1.08 (1.02 to 1.14) | 1343 | 1.01 (0.98 to 1.04) |
| Early pregnancy onset depression | 2367 | 0.06 (0.01 to 0.11) | 431 | 1.06 (0.97 to 1.17) | 1017 | 1.07 (1.02 to 1.12) |
Model is adjusted for maternal age, race/ethnicity (non-Hispanic white, non-Hispanic black, Hispanic, Asian/Pacific Islander, Native American/multiracial, other/unknown), nulliparity (Y/N), Medicaid (Y/N), smoking in first 20 weeks of pregnancy (Y/N), alcohol use in first 20 weeks of pregnancy (Y/N), and severity of early pregnancy depressive symptoms (mild, moderate, severe).
P for interaction = 0.17 for mean difference, 0.20 for GWG below IOM, <0.0001 for GWG above IOM (excluding underweight).
In analyses considering antidepressant treatment in early pregnancy, associations of prepregnancy onset depression with GWG rate and GWG rate categories were similar in women with and without antidepressant use during early pregnancy (Table 5). There was an association of early pregnancy onset depression with greater risk of GWG rate below IOM recommendations in women with antidepressant use in early pregnancy (RR = 1.44; 95% CI: 1.07–1.93), which was not present in women without antidepressant use in early pregnancy (RR = 1.02; 95% CI: 0.96–1.09). Associations of early pregnancy onset depression with GWG rate above IOM recommendations were similar in women with and without antidepressant use during early pregnancy.
Table 5.
Associations of Pre- and Early Pregnancy Onset Depression and Early Pregnancy Antidepressant Treatment with Gestational Weight Gain Rate Starting at Depression Screening or Diagnosis (lbs/Week)
| N | Mean differencea (95% CI) | N | RRa (95% CI) for GWG rate below the IOM recommendations | N | RRa (95% CI) for GWG rate above the IOM recommendations | |
|---|---|---|---|---|---|---|
| No pre- or early pregnancy depressive symptoms | 72,567 | Reference | 16,970 | Reference | 39,908 | Reference |
| Prepregnancy onset depression treated with antidepressants in early pregnancy | 2142 | −0.04 (−0.10 to 0.02) | 532 | 1.34 (1.04 to 1.72) | 1256 | 1.10 (0.99 to 1.22) |
| Prepregnancy onset depression not treated with antidepressants in early pregnancy | 5554 | 0.01 (0.00 to 0.02) | 1348 | 1.09 (1.05 to 1.13) | 3195 | 1.02 (1.00 to 1.04) |
| Early pregnancy onset depression treated with antidepressants | 287 | −0.03 (−0.12 to 0.05) | 77 | 1.44 (1.07 to 1.93) | 164 | 1.12 (0.98 to 1.27) |
| Early pregnancy onset depression not treated with antidepressants | 7050 | 0.05 (0.02 to 0.08) | 1639 | 1.02 (0.96 to 1.09) | 4012 | 1.05 (1.01 to 1.08) |
Model is adjusted for maternal age, race/ethnicity (non-Hispanic white, non-Hispanic black, Hispanic, Asian/Pacific Islander, Native American/multiracial, other/unknown), nulliparity (Y/N), Medicaid (Y/N), smoking in first 20 weeks of pregnancy (Y/N), alcohol use in first 20 weeks of pregnancy (Y/N), and severity of early pregnancy depressive symptoms (mild, moderate, severe).
Results of sensitivity analyses using GWG rate calculated using weight at the first depression screening through 20 weeks gestation among women without early pregnancy depressive symptoms (Supplementary Table S5), excluding women without a measured prepregnancy weight in the 12 months before pregnancy (Supplementary Table S6), and in nulliparous women with last measured weight at term (Supplementary Table S7) were similar to main results.
Discussion
We observed associations of prepregnancy onset depression with greater risk of GWG rate below and above the IOM recommendations, with stronger associations with GWG rate above the IOM recommendations observed in normal weight women. Early pregnancy onset depression was associated with a greater rate of GWG after identification of depression and slightly greater risk of GWG rate above the IOM recommendations, with stronger associations in obese women. Women with early pregnancy onset depression who are treated with antidepressants may also be at greater risk of GWG rate below the IOM recommendations.
Our study was the first to assess associations of prepregnancy onset depression and early pregnancy onset depression with rate of GWG after diagnosis. Previous studies of prenatal depression and GWG have evaluated total GWG from the beginning of pregnancy and have not separated new onset depression in early pregnancy from prepregnancy onset depression. In contrast to our findings, these studies have reported associations of prenatal depression with lower GWG,18 lower likelihood of GWG above the IOM recommendations,19 or no associations of prenatal depression with GWG.20 To determine the correct temporal sequence of the association between depression during pregnancy and GWG, it is important to examine GWG starting after the diagnosis of depression. Lifestyle behaviors, such as nutrition, which may contribute to weight change after depression diagnosis may also influence depression risk.40 In addition, some previous studies have adjusted for health behaviors, such as diet and physical activity at the time of depression assessment.19,20 Diet and physical activity changes are likely mechanisms through which depression influences GWG. Adjusting for these lifestyle behaviors at or after depression diagnosis may “adjust away,” or mask, the true association between depression and GWG, possibly explaining null results in previous studies.
The association between prenatal depression and GWG is complicated. Our study found that prepregnancy onset depression and early pregnancy onset depression were both associated with a greater rate of GWG after depression screening and slightly higher risk of GWG rate above the IOM recommendations with stronger associations for prepregnancy onset depression in normal weight women and stronger associations for early pregnancy onset depression in obese women. Some studies in nonpregnant adult populations have also reported associations of depression with greater risk of weight gain8,11 and developing obesity,9,10 particularly among women.9 Some studies have found associations of depression with unhealthy lifestyle behaviors, including poor diet quality,13,14 emotional eating (eating in response to negative emotions),41 low levels of physical activity,17 and greater sedentariness,16 which contribute to weight gain. Depression before and during early pregnancy may result in similar unhealthy diet and physical activity changes, which may contribute to greater GWG rate. Perinatal depression and GWG below and above the IOM recommendations are risk factors for pregnancy complications.2,42,43 Increasing the number of high risk women with GWG within the IOM recommendations, even by modest amounts, may be beneficial for preventing pregnancy complications.
Our study also found that prepregnancy onset depression, regardless of early pregnancy antidepressant use, and early onset prenatal depression in women with antidepressant use were associated with greater risk of GWG rate below the IOM recommendations. Some previous studies in nonpregnant adult populations have similarly reported associations of depression with both weight loss and weight gain.8,11 Identifying which individuals with depression are at risk of weight gain and which are at risk of weight loss is challenging. In a previous study, younger age, lower weight, fewer chronic disease comorbidities, and comorbid anxiety disorder at depression assessment were associated with weight gain, and being a former smoker was associated with weight loss.8 In our study, women with prepregnancy onset depression who were normal weight before pregnancy, parous, or receiving counseling but not antidepressant medications were more likely to have a GWG rate below the IOM recommendations (Supplementary Table S8). Unlike the previous study in nonpregnant adults, maternal age and smoking were not associated with less weight gain. We did not assess comorbid anxiety disorders in our study. There may be differences in how depression and antidepressant medications influence weight change during pregnancy and outside of pregnancy.
Strengths of our study include perinatal depression screening in our study population, consideration of GWG starting after early pregnancy depression screening to establish temporality of associations, consideration of prepregnancy onset and early onset prenatal depression separately, and adjustment for depression severity. We were not able to assess severity or duration of prepregnancy depression, or history of depression before 6 months before pregnancy, which may play a role in subsequent weight change. We did not have information about chronic medical conditions and lifestyle behaviors during pregnancy, such as diet and physical activity, which may help clarify which women with chronic depression are at risk for GWG below (vs. above) recommendations. We were not able to determine the reason for counseling. It is possible that women had counseling for reasons other than depression, which may have introduced misclassification in our assessment of depression treatment. About 25% of women eligible for our study were not screened for perinatal depression in early pregnancy. Women who were pregnant at the end of the perinatal depression screening rollout (201244)and women who reported alcohol use during pregnancy were more likely to be included in our analytic cohort (Supplementary Table S9). Women excluded from our cohort may have been receiving care at a medical center in which perinatal depression screening may not yet have been implemented (missing at random) or may have had low risk behaviors during pregnancy. Although we adjusted for high risk behaviors in our analyses, our analytic population may include some women at higher risk than the general population of pregnant women, especially for the earlier years of the study.
Conclusions
Women with prepregnancy onset depression may be at greater risk of GWG either below or above the IOM recommendations. Women with early onset prenatal depression may be at slightly greater risk of GWG rate above the IOM recommendations. Our findings suggest that the relationship between prepregnancy and early pregnancy onset depression and GWG rate is complex and may vary based on timing of depression onset, prepregnancy BMI category, and antidepressant use in early pregnancy. Women with depression during early pregnancy may benefit from lifestyle-related counseling for healthy GWG. Further research is needed to clarify the association between depression and GWG and identify factors that predict how a woman's lifestyle behaviors and weight change after depression diagnosis.
Supplementary Material
Acknowledgments
Funding: Participation by Lyndsay Avalos on this study was funded by K01MH103444 awarded by the National Institute of Mental Health (NIMH). Participation by Sylvia Badon on this study was funded by T32DK11668401 awarded by the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK).
Author Disclosure Statement
No competing financial interests exist.
Supplementary Material
References
- 1. ACOG Committee opinion no. 548: Weight gain during pregnancy. Obstet Gynecol 2013;121:210–212 [DOI] [PubMed] [Google Scholar]
- 2. Committee on Obstetric Practice. Weight gain during pregnancy: reexamining the guidelines. Washington, DC: National Academies Press, 2009 [PubMed] [Google Scholar]
- 3. Goldstein RF, Abell SK, Ranasinha S, et al. . Association of gestational weight gain with maternal and infant outcomes: A systematic review and meta-analysis. JAMA 2017;317:2207–2225 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Burt VK, Stein K. Epidemiology of depression throughout the female life cycle. J Clin Psychiatry 2002;63 Suppl 7:9–15 [PubMed] [Google Scholar]
- 5. Farr SL, Bitsko RH, Hayes DK, Dietz PM. Mental health and access to services among US women of reproductive age. Am J Obstet Gynecol 2010;203:542.e541–e549 [DOI] [PubMed] [Google Scholar]
- 6. Avalos LA, Raine-Bennett T, Chen H, Adams AS, Flanagan T. Improved perinatal depression screening, treatment, and outcomes with a universal obstetric program. Obstet Gynecol 2016;127:917–925 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Bennett HA, Einarson A, Taddio A, Koren G, Einarson TR. Prevalence of depression during pregnancy: Systematic review. Obstet Gynecol 2004;103:698–709 [DOI] [PubMed] [Google Scholar]
- 8. Gibson-Smith D, Bot M, Milaneschi Y, et al. . Major depressive disorder, antidepressant use, and subsequent 2-year weight change patterns in the Netherlands Study of Depression and Anxiety. J Clin Psychiatry 2016;77:e144–e151 [DOI] [PubMed] [Google Scholar]
- 9. Luppino FS, de Wit LM, Bouvy PF, et al. . Overweight, obesity, and depression: A systematic review and meta-analysis of longitudinal studies. Arch Gen Psychiatry 2010;67:220–229 [DOI] [PubMed] [Google Scholar]
- 10. Blaine B. Does depression cause obesity?: A meta-analysis of longitudinal studies of depression and weight control. J Health Psychol 2008;13:1190–1197 [DOI] [PubMed] [Google Scholar]
- 11. Haukkala A, Uutala A, Salomaa V. Depressive symptoms, cynical hostility, and weight change: A 3-year follow-up among middle-aged men and women. Int J Behav Med 2001;8:116–133 [Google Scholar]
- 12. Maxwell MA, Cole DA. Weight change and appetite disturbance as symptoms of adolescent depression: Toward an integrative biopsychosocial model. Clin Psychol Rev 2009;29:260–273 [DOI] [PubMed] [Google Scholar]
- 13. Beydoun MA, Kuczmarski MT, Mason MA, Ling SM, Evans MK, Zonderman AB. Role of depressive symptoms in explaining socioeconomic status disparities in dietary quality and central adiposity among US adults: A structural equation modeling approach. Am J Clin Nutr 2009;90:1084–1095 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Pagoto SL, Ma Y, Bodenlos JS, et al. . Association of depressive symptoms and lifestyle behaviors among Latinos at risk of type 2 diabetes. J Am Diet Assoc 2009;109:1246–1250 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Wielopolski J, Reich K, Clepce M, et al. . Physical activity and energy expenditure during depressive episodes of major depression. J Affect Disord 2015;174:310–316 [DOI] [PubMed] [Google Scholar]
- 16. Helgadottir B, Forsell Y, Ekblom O. Physical activity patterns of people affected by depressive and anxiety disorders as measured by accelerometers: A cross-sectional study. PLoS One 2015;10:e0115894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Bonnet F, Irving K, Terra JL, Nony P, Berthezene F, Moulin P. Anxiety and depression are associated with unhealthy lifestyle in patients at risk of cardiovascular disease. Atherosclerosis 2005;178:339–344 [DOI] [PubMed] [Google Scholar]
- 18. Shieh C, Wu J. Depressive symptoms and obesity/weight gain factors among Black and Hispanic pregnant women. J Community Health Nurs 2014;31:8–19 [DOI] [PubMed] [Google Scholar]
- 19. Heery E, Kelleher CC, Wall PG, McAuliffe FM. Prediction of gestational weight gain—A biopsychosocial model. Public Health Nutr 2015;18:1488–1498 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Molyneaux E, Poston L, Khondoker M, Howard LM. Obesity, antenatal depression, diet and gestational weight gain in a population cohort study. Arch Womens Mental Health 2016;19:899–907 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Gordon N. Similarity of the adult kaiser permanente membership in northern california to the insured and general population in Northern California: statistics from the 2009 California health interview survey. Oakland, CA: Kaiser Permanente Division of Research, 2012 [Google Scholar]
- 22. Kuczmarski RJ, Ogden CL, Guo SS, et al. . 2000 CDC Growth Charts for the United States: Methods and development, Hyattsville, Maryland. Vital and Health Statistics. Series 11, Data from the national health survey, 2002:1–190 [PubMed] [Google Scholar]
- 23. Obesity: Preventing and managing the global epidemic. Report of a WHO consultation, Geneva. World Health Organization Technical Report Series 2000;894:i–xii, 1–253 [PubMed] [Google Scholar]
- 24. Trinh NH, Youn SJ, Sousa J, et al. . Using electronic medical records to determine the diagnosis of clinical depression. Int J Med Inform 2011;80:533–540 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Kroenke K, Spitzer RL, Williams JB. The PHQ-9: Validity of a brief depression severity measure. J Gen Intern Med 2001;16:606–613 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Spitzer RL, Kroenke K, Williams JB. Validation and utility of a self-report version of PRIME-MD: The PHQ primary care study. Primary care evaluation of mental disorders. Patient Health Questionnaire. JAMA 1999;282:1737–1744 [DOI] [PubMed] [Google Scholar]
- 27. Spitzer RL, Williams JB, Kroenke K, Hornyak R, McMurray J. Validity and utility of the PRIME-MD patient health questionnaire in assessment of 3000 obstetric-gynecologic patients: The PRIME-MD Patient Health Questionnaire Obstetrics-Gynecology Study. Am J Obstet Gynecol 2000;183:759–769 [DOI] [PubMed] [Google Scholar]
- 28. Gilbody S, Richards D, Brealey S, Hewitt C. Screening for depression in medical settings with the Patient Health Questionnaire (PHQ): A diagnostic meta-analysis. J Gen Intern Med 2007;22:1596–1602 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Wittkampf KA, Naeije L, Schene AH, Huyser J, van Weert HC. Diagnostic accuracy of the mood module of the Patient Health Questionnaire: A systematic review. Gen Hosp Psychiatry 2007;29:388–395 [DOI] [PubMed] [Google Scholar]
- 30. Desai MM, Rosenheck RA, Craig TJ. Case-finding for depression among medical outpatients in the Veterans Health Administration. Med Care 2006;44:175–181 [DOI] [PubMed] [Google Scholar]
- 31. Engel CC, Oxman T, Yamamoto C, et al. . RESPECT-Mil: Feasibility of a systems-level collaborative care approach to depression and post-traumatic stress disorder in military primary care. Mil Med 2008;173:935–940 [DOI] [PubMed] [Google Scholar]
- 32. Arnow BA, Hunkeler EM, Blasey CM, et al. . Comorbid depression, chronic pain, and disability in primary care. Psychosom Med 2006;68:262–268 [DOI] [PubMed] [Google Scholar]
- 33. Katzelnick DJ, Von Korff M, Chung H, Provost LP, Wagner EH. Applying depression-specific change concepts in a collaborative breakthrough series. Jt Comm J Qual Patient Saf 2005;31:386–397 [DOI] [PubMed] [Google Scholar]
- 34. Sederer LI, Silver L, McVeigh KH, Levy J. Integrating care for medical and mental illnesses. Prev Chronic Dis 2006;3:A33. [PMC free article] [PubMed] [Google Scholar]
- 35. Andrews G, Anderson TM, Slade T, Sunderland M. Classification of anxiety and depressive disorders: Problems and solutions. Depress Anxiety 2008;25:274–281 [DOI] [PubMed] [Google Scholar]
- 36. Zou G. A modified poisson regression approach to prospective studies with binary data. Am J Epidemiol 2004;159:702–706 [DOI] [PubMed] [Google Scholar]
- 37. Lancaster CA, Gold KJ, Flynn HA, Yoo H, Marcus SM, Davis MM. Risk factors for depressive symptoms during pregnancy: A systematic review. Am J Obstet Gynecol 2010;202:5–14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Rasmussen KM, Abrams B, Bodnar LM, et al. . Determinants of gestational weight gain. In: Rasmussen KM, Yaktine AL, eds. Weight gain during pregnancy. Reexamining the GUIDELINES. Washington, DC: The National Academies Press, 2009:111–172 [PubMed] [Google Scholar]
- 39. R Core Team. R: A language and environment for statistical computing. Vienna, Austria: R Foundation for Statistical Computing, 2017 [Google Scholar]
- 40. Leung BM, Kaplan BJ. Perinatal depression: Prevalence, risks, and the nutrition link—A review of the literature. J Am Diet Assoc 2009;109:1566–1575 [DOI] [PubMed] [Google Scholar]
- 41. Ouwens MA, van Strien T, van Leeuwe JF. Possible pathways between depression, emotional and external eating. A structural equation model. Appetite 2009;53:245–248 [DOI] [PubMed] [Google Scholar]
- 42. Li D, Liu L, Odouli R. Presence of depressive symptoms during early pregnancy and the risk of preterm delivery: A prospective cohort study. Hum Reprod 2009;24:146–153 [DOI] [PubMed] [Google Scholar]
- 43. Grigoriadis S, VonderPorten EH, Mamisashvili L, et al. . The impact of maternal depression during pregnancy on perinatal outcomes: A systematic review and meta-analysis. J Clin Psychiatry 2013;74:e321–e341 [DOI] [PubMed] [Google Scholar]
- 44. Flanagan T, Avalos LA. Perinatal obstetric office depression screening and treatment: Implementation in a Health Care System. Obstet Gynecol 2016;127:911–915 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.