Abstract
Introduction:
Stress urinary incontinence (SUI), though is more prevalent than many chronic diseases, has remained largely underreported and underdiagnosed condition. We aimed to find the improvement in the quality of life (QoL) of women with SUI after individual interventions, namely mid-urethral sling (MUS), pelvic floor muscle training (PFMT), and no treatment/control group, as primary treatment modalities.
Materials and Methods:
This was a prospective interventional case–control study conducted at a university teaching hospital, over a period of 2 years. Parous women with at least one vaginal delivery, attending the gynecology outpatient department, were encouraged to fill the International Consultation on Incontinence Questionnaire-Urinary Incontinence Short Form. Those with SUI were divided into three arms (MUS, PFMT, and no treatment/control group), according to the informed decision for choice of management. Baseline QoL was documented for all with King's Health Questionnaire. QoL was again recorded after 3 months of the start of treatment and was compared with the baseline.
Results:
In our study cohort, the prevalence of SUI was 15.2%, with a consultation rate of only 30.7%. MUS surgery improves QoL significantly in women with SUI, followed by PFMT. We found 100% symptomatic relief, high rate of improvement in QoL with minimal easy to manage complications, in the surgical intervention arm. PFMT, though has a positive impact on QoL, requires continuous motivation, as 22% discontinued. Without treatment, QoL in SUI patients remained more or less the same.
Conclusion:
The help-seeking behavior (consultation rate) for SUI is poor. MUS (surgical arm) had 100% symptom relief in 3-month follow-up. MUS showed the best results in terms of QoL improvement, followed by PFMT in SUI in our study. It is important not only to educate women about the problem but also to encourage them to seek treatment and indicate that it is a treatable condition.
Keywords: King's Health Questionnaire, pelvic floor muscle training, quality of life, stress urinary incontinence, tension-free vaginal tape
INTRODUCTION
Stress urinary incontinence (SUI), defined as the involuntary leakage of urine on effort or physical exertion or on sneezing or coughing, is the most common subtype of urinary incontinence (UI) in women. While all subtypes of UI represent a significant suffering and burden, SUI needs a special attention as it usually occurs in younger population, so having a greater as well as longer impact in the quality of life (QoL).[1,2,3] SUI, though is more prevalent than many chronic diseases, has remained largely underreported and underdiagnosed condition.
Interestingly, compared to other forms of UI, SUI is most amenable to treatment with available treatment being easy and efficacious. Awareness of SUI as a treatable entity thus becomes more important. Regrettably, many women consider it a part of normal aging and childbirth and silently suffer without seeking medical help.[4]
Based on the questionnaire, we tried to explore the prevalence of SUI in parous women attending the gynecology outpatient department (OPD). This exercise was also an effort to make the affected women aware of the treatment modalities for SUI. Usually the first line treatment of SUI is considered as conservative management. Only when conservative management fails surgical correction is offered. However, this exercise sometimes can be frustrating for a patient and she would like to get cured of her symptoms as soon as possible. Thus, the present study aimed primarily to find the improvement in QoL of women with SUI after individual interventions (mid-urethral sling [MUS], pelvic floor muscle training [PFMT], and no treatment/control group) used as primary treatment modalities.
MATERIALS AND METHODS
This was a prospective interventional case–control study conducted at a university teaching hospital, over a period of 2 years from October 2013 to September 2015. Approval from the Institutional Ethical Committee was obtained on December 13th in 2013 (IEC 563/2013).
Sample size and study population
Anticipating 10% of women to report of SUI, with the relative precision of 25% and with 95% confidence level, 553 women needed to be studied. We surveyed 579 consecutive women attending the OPD of our hospital, who had delivered at least once vaginally.
During the time of recruitment, a detailed history was taken including the demography and symptomatology related to UI. General physical examination was done. Patients were then asked to make the bladder full (by drinking water and other beverages) and hold urine until she starts feeling a sensation of urgency. During this waiting period, the International Consultation on Incontinence Questionnaire-Urinary Incontinence Short Form (ICIQ-UI SF) was filled as a tool to categorize urinary problems. Women identified with pure urge incontinence were excluded from the study. Women identified with SUI (pure SUI or Mixed incontinence) were further subjected to a cough stress test with full bladder, which if positive were included in the study. All women with SUI underwent a urine microscopy and culture sensitivity test to rule out cystitis. These women then were provided with King's Health Questionnaire (KHQ) to assess their baseline QoL.
All women with demonstrable SUI were counseled regarding the nature of problem and available treatment options with the help of a printed subject information sheet. They were provided time and were allowed to discuss their concerns and issues to make an informed decision about the treatment options. They were also told about the complication rates (with reference to whatever is available in the literature) and success versus failure rates.
Thus, women with SUI were divided into three management groups based on their choice of management. The management options were surgical, i.e., the tension-free vaginal tape-obturator (TVT-O), PFMT, and no treatment. All women were allowed to make an informed decision regarding choice of management after one-to-one discussion. All these women were followed up after 3 months and their QoL was reassessed with KHQ, either when they come for follow-up or telephonically.
Interventions: (a) TVT-O: All procedures were performed under spinal anesthesia by a single surgeon by the standard surgical technique using a macroporous polypropylene tape. (b) PFMT: PFMT was taught in the physiotherapy outpatient department. The correct technique of exercises was determined by per-vaginal palpation of the pelvic floor muscles. The exercises were given in the supine position initially and were progressed to other positions such as sitting, standing, walking, and squatting later on. The women were instructed to repeat the exercises, ten sets of contractions for at least three times in a day in the initial phase and later to progress to three sets of thirty contractions three times a day, for a period of 3 months. (c) No intervention arm (control group): No intervention group was the one where the women refused any treatment even after counselling. This happened because of a common myth in our society that SUI is but a part and parcel of childbirth and aging. In this study, we used this group as a control group to compare our results with the intervention groups.
Statistical analysis
Discrete variables such as age, parity, body mass index, hypertension, diabetes mellitus, menopausal status, pelvic relaxation, and past history of hysterectomy were compared using the Chi-square test. Logistic regression analysis was done to correlate the associated risk factors. One-way analysis of variance (ANOVA) was used to compare scores on the ICIQ-UI SF questionnaire. Baseline scores in the KHQ were compared with multivariate ANOVA. Student's t-test/Wilcoxon signed-rank test was done to compare the QoL scores before and after intervention. Statistical analysis was performed using the Statistical Package for the Social Sciences Version 23.0. (SPSS-15, IBM Corp., Armonk, NY) for windows. The result was considered to be statistically significant at 5% level of significance (P < 0.05).
RESULTS
During the recruitment, 600 women who attended gynecological OPD for various complaints were asked to participate in the study. Of these, 579 consented and filled the ICIQ-UI SF questionnaire. With the help of this questionnaire, 120 (20.7%) were identified with urinary complaints. Women with overactive bladder and SUI secondary to cystitis and women in whom cough stress test could not be demonstrated were excluded and 88 women were analyzed further [Figure 1]. Thus, the prevalence of SUI either alone or as a part of mixed incontinence was 15.2%.
Figure 1.
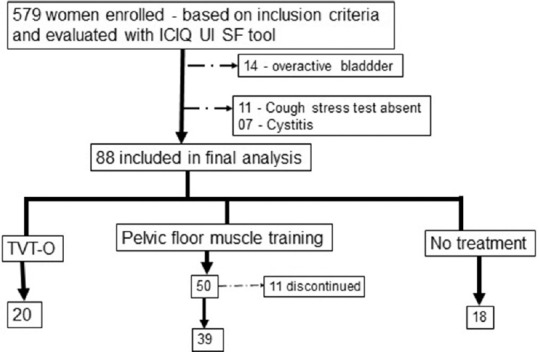
Distribution of the study population
Among this population of women, the consultation rate for SUI was 30.68% which means that out of 88 women with SUI, only 27 presented with a chief complaint of SUI. Rest (55.68%, n = 49) did not complain of the same and presented with some other gynecological complaints but on filling up the ICIQ-UI SF questionnaire were found to have SUI. Twelve women (13.63%) who came for routine health check were also found to have with SUI demonstrable on physical examination [Figure 2].
Figure 2.
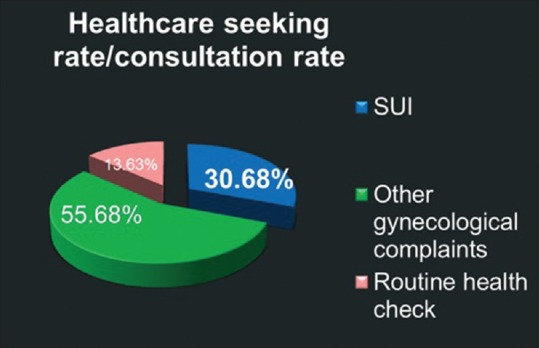
Health-care-seeking rate for urinary incontinence in our cohort
On detailed explanation about the various modes of treatment, maximum (n = 50) choose PFMT. However, 11 of these (22%) discontinued in due course of follow-up. Twenty agreed to undergo TVT-O procedure, whereas 18 refused any treatment for SUI and thus formed the control group to compare our results [Figure 1].
On comparing the scores from the ICIQ-UI SF tool, we found that the higher mean scores, which reflect more symptom severity, were associated with the women who choose to undergo TVT-O (14 ± 3.18), followed by PFMT (10.46 ± 3.37) and no treatment group (9.5 ± 3.69) [Table 1]. This finding may pose a selection bias in the final QoL-related outcome.
Table 1.
Correlation between the International Consultation on Incontinence Questionnaire-Urinary Incontinence Short Form scores and choice of intervention
| n | ICIQ-UI SF scores, mean±SD | P* | |
|---|---|---|---|
| TVT-O | 20 | 14.3±3.18 | 0.001 |
| PFMT | 50 | 10.46±3.37 | |
| No treatment | 18 | 9.5±3.69 |
Values are given as mean±SD, *P value: One-way ANOVA, <0.05 is significant. ICIQ-UI SF: International Consultation on Incontinence Questionnaire-Urinary Incontinence Short Form, SD: Standard deviation, TVT-O: Tension-free vaginal tape-obturator, PFMT: Pelvic floor muscle training, ANOVA: Analysis of variance
Baseline scores: The mean baseline scores in the ten domains of the KHQ are tabulated in Table 2. The mean scores were higher in the TVT-O group (all ten domains) when compared with the PFMT and no treatment group. The mean scores were slightly higher in the PFMT group (except incontinence impact) in comparison to no treatment group.
Table 2.
Baseline scores in the King’s Health Questionnaire before intervention in the three groups (n=77)
| Tool number | Domains | TVT-O group (n=20) | PFMT group (n=39) | Nil intervention group (n=18) | P |
|---|---|---|---|---|---|
| KHQ1 | General health perceptions | 67.5±20.03 | 54.48±18.02 | 44.44±16.66 | <0.001 |
| KHQ2 | Incontinence impact | 74.99±23.88 | 51.27±18.48 | 51.84±24.21 | <0.001 |
| KQH3 | Role limitations | 64.99±24.72 | 48.71±23.99 | 35.18±32.74 | 0.001 |
| KHQ4 | Physical limitations | 67.49±29.85 | 49.14±30.09 | 38.88±33.33 | 0.008 |
| KHQ5 | Social limitations | 63.60±29.25 | 36.74±30.06 | 27.77±34.01 | 0.001 |
| KHQ6 | Personal relationships | 34.41±36.43 | 16.92±32.10 | 11.11±19.80 | 0.051 |
| KHQ7 | Emotions | 63.88±24.94 | 39.59±29.81 | 27.15±25.90 | <0.001 |
| KHQ8 | Sleep/energy | 29.16±26.42 | 15.38±16.83 | 13.88±16.41 | 0.024 |
| KHQ9 | Severity measures | 57.49±25.34 | 44.43±22.07 | 28.69±21.62 | 0.001 |
| KHQ10 | Symptom severity score | 7.95±4.37 | 5.38±3.70 | 4.72±4.32 | 0.030 |
Values are given as mean±SD, P value: Multivariate ANOVA, <0.05 is significant. TVT-O: Tension-free vaginal tape-obturator, PFMT: Pelvic floor muscle training, ANOVA: Analysis of variance, KHQ: King’s Health Questionnaire, SD: Standard deviation
Comparison of scores before and after intervention: QoL scores from the KHQ at baseline before intervention (t0) and 3 months after intervention (t3) were compared. It also shows the change in points from baseline to 3 months postintervention. Higher scores represent worse QoL and lower scores represent good QoL of life.
At 3-month follow-up in the TVT-O group, QoL improved significantly in all the ten domains [Table 3]. The maximum improvement in QoL was seen on incontinence impact, change in points of 74.99 at baseline (t0) to 16.66 after 3 months (t3), i.e., 58.33. These results are followed by role limitations (53.33), sleep/energy (51.67), emotions (51.66), social limitations (49.16), and physical limitations (48.33).
Table 3.
Comparison of various domains of King’s Health Questionnaire before and 3 months after tension-free vaginal tape-obturator (n=20)
| Domains | Before TVT-O (t0) | After TVT-O (t3) | Change in points | P | |
|---|---|---|---|---|---|
| KHQ1 | General health perception | 67.5±20.03 | 27.5±7.69 | 40 | <0.0001 |
| KHQ2 | Incontinence impact | 74.99±23.88 | 16.66±17.09 | 58.33 | <0.0001 |
| KQH3 | Role limitations | 64.99±24.72 | 11.66±15.38 | 53.33 | <0.0001 |
| KHQ4 | Physical limitations | 67.49±29.85 | 19.16±13.5 | 48.33 | <0.0001 |
| KHQ5 | Social limitations | 63.60±29.25 | 14.44±18.05 | 49.16 | <0.0001 |
| KHQ6 | Personal relationships | 34.41±36.43 | 4.99±7.83 | 29.42 | 0.0019 |
| KHQ7 | Emotions | 63.88±24.94 | 12.22±11.34 | 51.66 | <0.0001 |
| KHQ8 | Sleep/energy | 29.16±26.42 | 7.49±10.07 | 51.67 | 0.004 |
| KHQ9 | Severity measures | 57.49±25.34 | 13.74±14.62 | 43.75 | <0.0001 |
| KHQ10 | Symptom severity scale | 7.95±4.37 | 2.35±1.03 | 5.6 | <0.0003 |
Values are given as mean±SD, P value: Paired t-test/Wilcoxon signed-rank test, <0.05 is significant. TVT-O: Tension-free vaginal tape-obturator, KHQ: King’s Health Questionnaire, SD: Standard deviation
As any surgical procedure, TVT-O also carries a risk of complications. We analyzed the rate of complications and found that there were no life-threatening or serious complications in our series. Three women had voiding difficulty in the first 48 h, which was managed with tape adjustment. Two had groin pain requiring hospital visit within the first 3 months, both of them responded well to oral analgesics. One patient came with sinus formation with pus discharge at the groin and required excision of part of the mesh which was exposed and debridement of the surrounding tissue. There were no cases of bladder injury, hematoma, or mesh erosion in our cohort.
Table 4 reflects QoL in women who underwent PFMT, at baseline (t0) and at 3 months after (t3). At 3-month follow-up (t3), the improvement in QoL was significant in all domains except sleep/energy (P = 0.44) and symptom severity scale (P = 0.074). Although the overall QoL improved at t3, the improvement in individual scores was much less compared to the TVT-O group. The maximum improvement in PFMT group was seen in emotional status (change in points – 20.79), followed by general health perceptions (16.02), role limitations (15.38), severity measures (15.17), and incontinence impact (12.82). Women did not report a significant change in QoL in terms of sleep/energy and symptom severity scale after 3 months of PFMT.
Table 4.
Comparison of various domains of King’s Health Questionnaire before and 3 months after pelvic floor muscle training (n=39)
| Domains | Before PFMT (t0) | After PFMT (t3) | Change in points | P | |
|---|---|---|---|---|---|
| KHQ1 | General health perception | 54.48±18.02 | 38.46±12.62 | 16.02 | <0.0001 |
| KHQ2 | Incontinence impact | 51.27±18.48 | 38.45±14.38 | 12.82 | 0.001 |
| KQH3 | Role limitations | 48.71±23.99 | 33.33±0 | 15.38 | 0.001 |
| KHQ4 | Physical limitations | 49.14±30.09 | 42.30±24.13 | 6.84 | 0.006 |
| KHQ5 | Social limitations | 36.74±30.06 | 30.19±19.23 | 6.55 | 0.010 |
| KHQ6 | Personal relationships | 16.92±32.10 | 11.11±21.40 | 5.81 | 0.045 |
| KHQ7 | Emotions | 39.59±29.81 | 18.80±16.93 | 20.79 | 0.0003 |
| KHQ8 | Sleep/energy | 15.38±16.83 | 13.24±13.34 | 2.14 | 0.44 |
| KHQ9 | Severity measures | 44.43±22.07 | 29.26±16.87 | 15.17 | 0.001 |
| KHQ10 | Symptom severity scale | 5.38±3.70 | 4.46±2.90 | 0.92 | 0.074 |
Values are given as mean±SD, P value: Paired t-test/Wilcoxon signed-rank test, <0.05 is significant. KHQ: King’s Health Questionnaire, SD: Standard deviation, PFMT: Pelvic floor muscle training
We also compared QoL women who did not want any treatment for SUI, at baseline (t0) and at 3-month interval (t3). There was an only minimal perceptive improvement in QoL. Personal relationships did not change, and social limitations became worse, probably because these women became aware of their urinary problem, which they thought earlier that it was a normal part of aging or had now developed more awareness of their problem [Table 5].
Table 5.
Comparison of various domains of King’s Health Questionnaire before and 3 months after no treatment (n=18)
| Domains | No treatment (t0) | No treatment (t3) | Change in points | P | |
|---|---|---|---|---|---|
| KHQ1 | General health perception | 41.66±17.14 | 36.11±12.78 | 5.55 | 0.10 |
| KHQ2 | Incontinence impact | 49.99±23.57 | 46.29±23.25 | 3.7 | 0.05 |
| KQH3 | Role limitations | 33.32±29.70 | 27.77±24.25 | 5.55 | 0.36 |
| KHQ4 | Physical limitations | 37.02±28.89 | 36.10±24.42 | 0.92 | 0.655 |
| KHQ5 | Social limitations | 28.70±30.85 | 29.62±29.27 | −0.92 | 0.65 |
| KHQ6 | Personal relationships | 11.11±19.80 | 11.11±16.16 | 0 | 0.6 |
| KHQ7 | Emotions | 27.15±25.90 | 22.22±18.66 | 4.93 | 0.197 |
| KHQ8 | Sleep/energy | 13.88±16.41 | 12.95±13.46 | 0.93 | 0.63 |
| KHQ9 | Severity measures | 28.69±21.62 | 25.92±17.82 | 2.77 | 0.285 |
| KHQ10 | Symptom severity scale | 4.72±4.32 | 3.77±2.42 | 0.95 | 0.052 |
Values are given as mean±SD, P value: Paired t-test/Wilcoxon signed-rank test, <0.05 is significant. KHQ: King’s Health Questionnaire, SD: Standard deviation
Changes in the mean scores of the KHQ at baseline and 3 months later were compared among the three study arms [Table 6]. The maximum improvement in QoL was observed in the TVT-O group, followed by the PFMT group. Bare minimal difference was observed in the QoL scores reported by the women with no treatment after 3 months, indicating that SUI is not a self-limiting or self-resolving condition and it requires intervention to improve QoL.
Table 6.
Comparison between the improvement in quality of life in the study arms (tension-free vaginal tape-obturator, pelvic floor muscle training, and no treatment group)
| Tool number | Domains | TVT-O group (n=20) | PFMT group (n=39) | Nil intervention group (n=18) | P |
|---|---|---|---|---|---|
| KHQ1 | General health perceptions | 40 | 16.02 | 5.55 | <0.001 |
| KHQ2 | Incontinence impact | 58.33 | 12.82 | 3.7 | <0.001 |
| KQH3 | Role limitations | 53.33 | 15.38 | 5.55 | <0.001 |
| KHQ4 | Physical limitations | 48.33 | 6.84 | 0.92 | <0.001 |
| KHQ5 | Social limitations | 49.16 | 6.55 | −0.92 | <0.001 |
| KHQ6 | Personal relationships | 29.42 | 5.81 | 0 | <0.001 |
| KHQ7 | Emotions | 51.66 | 20.79 | 4.93 | <0.001 |
| KHQ8 | Sleep/energy | 51.67 | 2.14 | 0.93 | <0.001 |
| KHQ9 | Severity measures | 43.75 | 15.17 | 2.77 | <0.001 |
| KHQ10 | Symptom severity score | 5.6 | 0.92 | 0.95 | <0.001 |
Values are given as mean±SD, P value: Multivariate ANOVA, <0.05 is significant. KHQ: King’s Health Questionnaire, SD: Standard deviation, PFMT: Pelvic floor muscle training, TVT-O: Tension-free vaginal tape-obturator, ANOVA: Analysis of variance
DISCUSSION
In our study cohort of parous women with at least one vaginal delivery attending the gynecology OPD, the prevalence of SUI was 15.2%. The prevalence of SUI varies according to the geographical area and population studied. It is estimated to be as high as 50% in the literature.[5]
The present study emphasizes the suboptimal health- care-seeking behavior in our society too. By “health-seeking behavior” of “help-seeking behavior,” we meant those women who came to the gynecology OPD with a chief complaint of SUI as compared to those who presented in our OPD with other complaints such as abnormal uterine bleeding and pain abdomen and then on asking directly were found to have SUI. Only around a third (30.68%) of women presented to us with a chief complaint of SUI. SUI with an immense negative impact on QoL is a neglected problem with poor health-care-seeking behavior worldwide.[4,6,7,8]
A study in Sri Lankan women found the health-seeking behavior only in 12.9% of women suffering silently with SUI. They went further ahead to find the reasons for not seeking medical advice. The reasons were as follows: being embarrassed (n = 27, 33.33%), not knowing that it is remediable (n = 23, 28.40%), perceiving SUI to be a normal consequence of childbirth (n = 19, 23.46%), and having to attend to needs of the family (n = 12, 14.81%).[4] Another study from India in a tribal population revealed a similar (14.4%) health-care-seeking behavior with a reason for not complaining of incontinence being either acceptance of it as a normal aging process or associated embarrassed.[9]
SUI has been tried to manage by lifestyle modifications, behavioral therapy, PFMT or the Kegel exercises, pharmacotherapy and surgical interventions, i.e., Burch colposuspension, and MUS surgeries, i.e., TVT and transobturator tape (TVT-O). More recently with the popularization of minimally invasive mid-urethral tapes, more invasive surgical options are being performed infrequently. MUS surgery is demonstrated to have subjective cure rates between 75% and 94% and objective cure rates between 57% and 92%, with minimal complications.[10,11,12] PFMT is generally regarded as the first-line therapy[13] though its long-term effectiveness still needs to be studied.
SUI significantly impacts QoL in women, which has been studied with various instruments and was also noted in our study too. KHQ has been found to be a reliable predictor of improvement or deterioration of women's QoL following interventions.[14,15] We found a significant improvement in all ten domains of QoL studied by KHQ in those women who underwent TVT-O as compared to PFMT or no treatment group. However, even PFMT was quite useful for improving the QoL of women as compared to women who decided not to undergo any form of treatment, mostly because they thought that it was a normal process of aging and were not bothered about it until we had directly asked.
This was a hospital-based rather than a true population-based prevalence study. The limitations of our study are also lack of randomization for different treatment modalities, which possibly created a selection bias, as women with more impaired QoL and severe disease opted for surgical intervention and vice versa. This might have created a bias in the results, as women who are more bothered about their symptoms would have felt more satisfied after the treatment. The data here were solely obtained on verbal response, and hence, the perception of QoL was purely subjective. The other drawback was the limited follow-up period, as studies have shown the early response of PFMT while a doubtful long-term effectiveness.[13] A multicentric randomized trial concluded that MUS should be the first-line treatment for SUI not PFMT in view of higher subjective improvement and objective cure at 1-year follow-up.[16]
There is a definitive need to educate women and make them aware about SUI as a treatable pathological progress with a possibility of its aggravation with age- and menopause-related hormone deficiency. They also need to be made aware about its impact on various domains of their QoL. Last but not the least, these silent sufferers need to be made aware about the availability of effective treatment modalities for SUI.
It has been recommended that health-care professionals should play a more proactive role by directly identifying cases of UI, to guide them appropriately.[16,17]
CONCLUSION
The prevalence of SUI in our study was 15.2%, which reflects that every fifth or sixth parous woman who delivered vaginally, presenting to the gynecology OPD, is likely to have SUI. However, the consultation rate was only 30.7%; hence, the responsibility lies on the primary care physician to ask a leading question regarding urinary complaints as a primary screening tool. MUS surgery improves QoL significantly in women with SUI, followed by PFMT. We found 100% symptomatic relief, high rate of improvement in QoL with minimal easy to manage complications, in the surgical intervention arm. PFMT, though has a positive impact on QoL, requires continuous motivation, as 22% discontinued. Without treatment, QoL in SUI patients remained more or less the same. Awareness of symptom as an aberration from normal health status might have a negative impact on social life. Hence, it is important not only to educate women about the problem but also to encourage them to seek treatment and indicate that it is a preventable as well as treatable condition.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Minassian VA, Stewart WF, Hirsch AG. Why do stress and urge incontinence co-occur much more often than expected? Int Urogynecol J Pelvic Floor Dysfunct. 2008;19:1429–40. doi: 10.1007/s00192-008-0647-2. [DOI] [PubMed] [Google Scholar]
- 2.Komesu YM, Schrader RM, Ketai LH, Rogers RG, Dunivan GC. Epidemiology of mixed, stress, and urgency urinary incontinence in middle-aged/older women: The importance of incontinence history. Int Urogynecol J. 2016;27:763–72. doi: 10.1007/s00192-015-2888-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Reynolds WS, Dmochowski RR, Penson DF. Epidemiology of stress urinary incontinence in women. Curr Urol Rep. 2011;12:370–6. doi: 10.1007/s11934-011-0206-0. [DOI] [PubMed] [Google Scholar]
- 4.Perera J, Kirthinanda DS, Wijeratne S, Wickramarachchi TK. Descriptive cross sectional study on prevalence, perceptions, predisposing factors and health seeking behaviour of women with stress urinary incontinence. BMC Womens Health. 2014;14:78. doi: 10.1186/1472-6874-14-78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cervigni M, Gambacciani M. Female urinary stress incontinence. Climacteric. 2015;18(Suppl 1):30–6. doi: 10.3109/13697137.2015.1090859. [DOI] [PubMed] [Google Scholar]
- 6.Hannestad YS, Rortveit G, Hunskaar S. Help-seeking and associated factors in female urinary incontinence. The Norwegian EPINCONT study. Epidemiology of incontinence in the county of Nord-Trøndelag. Scand J Prim Health Care. 2002;20:102–7. [PubMed] [Google Scholar]
- 7.Koch LH. Help-seeking behaviors of women with urinary incontinence: An integrative literature review. J Midwifery Womens Health. 2006;51:e39–44. doi: 10.1016/j.jmwh.2006.06.004. [DOI] [PubMed] [Google Scholar]
- 8.Wójtowicz U, Płaszewska-Zywko L, Stangel-Wójcikiewicz K, Basta A. Barriers in entering treatment among women with urinary incontinence. Ginekol Pol. 2014;85:342–7. doi: 10.17772/gp/1734. [DOI] [PubMed] [Google Scholar]
- 9.Prabhu SA, Shanbhag SS. Prevalence and risk factors of urinary incontinence in women residing in a tribal area in Maharashtra, India. J Res Health Sci. 2013;13:125–30. [PubMed] [Google Scholar]
- 10.Novara G, Artibani W, Barber MD, Chapple CR, Costantini E, Ficarra V, et al. Updated systematic review and meta-analysis of the comparative data on colposuspensions, pubovaginal slings, and midurethral tapes in the surgical treatment of female stress urinary incontinence. Eur Urol. 2010;58:218–38. doi: 10.1016/j.eururo.2010.04.022. [DOI] [PubMed] [Google Scholar]
- 11.Fusco F, Abdel-Fattah M, Chapple CR, Creta M, La Falce S, Waltregny D, et al. Updated systematic review and meta-analysis of the comparative data on colposuspensions, pubovaginal slings, and midurethral tapes in the surgical treatment of female stress urinary incontinence. Eur Urol. 2017;72:567–91. doi: 10.1016/j.eururo.2017.04.026. [DOI] [PubMed] [Google Scholar]
- 12.Ford AA, Rogerson L, Cody JD, Aluko P, Ogah JA. Mid-urethral sling operations for stress urinary incontinence in women. Cochrane Database Syst Rev. 2017;7:CD006375. doi: 10.1002/14651858.CD006375.pub4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Dumoulin C, Hay-Smith EJC, Mac Habée-Séguin G. Pelvic floor muscle training versus no treatment, or inactive control treatments, for urinary incontinence in women. Cochrane Database of Systematic Reviews. 2014;(5) doi: 10.1002/14651858.CD005654.pub3. Art. No.: CD005654. DOI: 10.1002/14651858.CD005654.pub3. [DOI] [PubMed] [Google Scholar]
- 14.Abdel-fattah M, Hasafa Z, Mostafa A. Correlation of three validated questionnaires for assessment of outcomes following surgical treatment of stress urinary incontinence in women. Eur J Obstet Gynecol Reprod Biol. 2011;157:226–9. doi: 10.1016/j.ejogrb.2011.03.020. [DOI] [PubMed] [Google Scholar]
- 15.Bjelic-Radisic V, Dorfer M, Tamussino K, Frudinger A, Kern P, Winter R, et al. The incontinence outcome questionnaire: An instrument for assessing patient-reported outcomes after surgery for stress urinary incontinence. Int Urogynecol J Pelvic Floor Dysfunct. 2007;18:1139–49. doi: 10.1007/s00192-007-0302-3. [DOI] [PubMed] [Google Scholar]
- 16.Labrie J, Berghmans BL, Fischer K, Milani AL, van der Wijk I, Smalbraak DJ, et al. Surgery versus physiotherapy for stress urinary incontinence. N Engl J Med. 2013;369:1124–33. doi: 10.1056/NEJMoa1210627. [DOI] [PubMed] [Google Scholar]
- 17.Fultz NH, Burgio K, Diokno AC, Kinchen KS, Obenchain R, Bump RC. Burden of stress urinary incontinence for community-dwelling women. Am J Obstet Gynecol. 2003;189:1275–82. doi: 10.1067/s0002-9378(03)00598-2. [DOI] [PubMed] [Google Scholar]


