Abstract
Background:
Whether readmission rates vary by primary care physician (PCP) is unknown, although federal policy holds PCPs accountable for reducing readmissions.
Objective:
To determine whether 30-day readmission rates vary by PCP.
Design:
Retrospective cohort study using marginal models and multilevel logistic regression with 100% of data on Texas Medicare claims from 2008 to 2015.
Setting:
Texas.
Participants:
Patients discharged alive between 1 January 2008 and 30 November 2015 who had a PCP in the prior year and whose PCP had at least 50 admissions in the study period.
Measurements:
Readmission within 30 days of discharge. Follow-up visits with a PCP within 7 days of discharge were also measured.
Results:
Between 2012 and 2015, the mean risk-standardized rate of 30-day readmissions was 12.9%. Of 4230 PCPs, 1 had a readmission rate that was significantly higher than the mean and none had a significantly lower rate. The 10th and 90th percentiles of PCP readmission rates were 12.4% and 13.4%, respectively, each only 0.5 percentage point different from the mean. The 99th percentile of PCP readmission rates was 14.0%, 1.1 percentage points higher than the mean. Detecting a 1.1–percentage point difference from the mean adjusted readmission rate would require more than 3500 admissions per PCP per year.
Limitations:
Only fee-for-service Medicare patients in a single state were included. The authors could not account for confounders not included in Medicare databases or classify read-missions as avoidable.
Conclusion:
Variation in readmission rates among PCPs is very low. Programs holding PCPs accountable for readmissions may prove ineffective.
Primary Funding Source:
National Institutes of Health.
Readmissions for Medicare beneficiaries are costly, and some may represent poor quality of care (1, 2). Prompted by the high cost, poor quality, and hospital variation associated with readmissions (3), the Centers for Medicare & Medicaid Services (CMS) launched the Hospital Readmissions Reduction Program, a pay-for-performance program that encourages hospitals to reduce readmissions by decreasing payments to hospitals with excess readmissions (4). Evidence suggests that the program may have succeeded in reducing re-admissions (5). Nevertheless, rates remain high, and further improvements will require a better understanding of other factors that may influence readmissions.
Risk for readmission might be influenced by the physicians providing care. This includes care during the initial hospitalization by the inpatient physician, follow-up care after discharge by the primary care physician (PCP), and emergency care after discharge by the emergency department (ED) physician. Readmission rates are higher in patients receiving inpatient care from hospitalists than in those receiving it from their PCP (6). However, risk for readmission does not vary by individual hospitalist (7). Early follow-up after hospital discharge is sometimes associated with lower readmission rates (8, 9). We previously reported that risk for readmission varies moderately but significantly by ED physician, identifying an opportunity for improvement (10). However, whether PCP care influences readmissions is uncertain, although CMS has implemented a policy incentivizing PCPs to reduce readmissions (11).
We undertook this study to determine whether risk for readmission varies by PCP. We also assessed variation among PCPs in the rate at which they see patients in outpatient follow-up within a week of discharge.
METHODS
Data Source
We used 100% of data from Texas Medicare claims for 1 January 2007 through 31 December 2015. These include the Medicare denominator file for demographic and enrollment information, the carrier file for physician claims, the outpatient statistical analysis file for outpatient claims, and the Medicare Provider Analysis and Review (MedPAR) file for inpatient claims.
Cohort Selection
The study used 2 different cohorts, 1 to study 30-day readmission rates and the other to study whether patients were seen by their PCP within 7 days of hospital discharge.
To develop the readmission cohort, we started with all hospitalized patients who were discharged between 1 January 2012 and 30 November 2015 (Appendix Table 1, available at Annals.org). For beneficiaries with multiple hospitalizations in the same year, the first hospitalization was kept. We then identified patients who were discharged alive and not transferred to other acute care hospitals. We included only hospitalizations for beneficiaries aged 66 years or older with continuous coverage from Medicare Parts A and B and no HMO in the 12 months before and 1 month after hospitalization. We excluded those who died without a re-admission within 30 days after hospital discharge. We selected beneficiaries who had an identifiable PCP in the year before hospitalization and excluded those whose PCPs had fewer than 50 hospital admissions in the data. We defined a PCP as a generalist (general practitioner, family physician, internist, or geriatrician) who saw a given patient on 2 or more occasions in an outpatient setting in the year before the hospitalization of interest (12). We used CPT (Current Procedural Terminology) codes 99201 to 99205 (new patient encounters), 99211 to 99215 (established patient encounters), and G0463 to identify outpatient visits from carrier files. The generalist with the most visits was assigned as the PCP. When 2 generalists had an equal number of visits, the most recently visited provider was assigned.
The follow-up cohort differed from the readmission cohort in that it included only patients discharged directly to the community and did not exclude those who died in the 30 days after discharge (Appendix Table 2, available at Annals.org).
Measurements
Patient age, sex, ethnicity, and Medicaid eligibility were obtained from Medicare beneficiary summary files. We used the Medicaid eligibility indicator as a proxy for low socioeconomic status. Admission type (emergency vs. nonemergency and weekday vs. weekend) and diagnosis-related group (DRG) codes were obtained from MedPAR files. We determined residence in a nursing facility in the 3 months before the hospitalization of interest using the MedPAR files and evaluation and management codes 99304 to 99318 (nursing facility services) from carrier files (13). Total numbers of hospitalizations and outpatient visits in the prior year were identified from MedPAR files and carrier files, respectively. Education level at the ZIP code of residence was obtained from the 2011 American Community Survey estimates from the U.S. Census Bureau. Elixhauser comorbidity indicators were identified using claims from the MedPAR, carrier, and outpatient statistical analysis files in the year before the hospitalization of interest (14).
Study Outcomes
The primary outcome was any readmission within 30 days of discharge. A secondary outcome was whether patients were evaluated in an outpatient setting by their PCP within 7 days of hospital discharge.
Overview of Analytic Approach
Our aim was to describe the degree of variation in readmission rates that is attributable to PCPs. We explored many analytic approaches, which yielded near identical results. Our main results were generated from a marginal logistic model. We repeated the analyses using a multilevel logistic regression model and a conditional model. To plot risk-standardized rates of 30-day readmissions for each PCP, we used bootstrapping with the multilevel regression model to estimate the 95% CI for each PCP.
We estimated the stability of the PCP-adjusted read-mission rates by comparing the results based on admissions from 2012 to 2015 with those based on data from 2008 to 2011 for the 3408 PCPs with data in both time periods. Finally, we calculated the 95% CIs for different postulated rates of readmission for a PCP at different sample sizes (numbers of admissions) to explore the feasibility of generating robust information on PCP performance using the readmission rates of their patients.
Statistical Analysis
Descriptive analyses were used to summarize the association between patient characteristics and read-mission rates within 30 days of hospital discharge. We used generalized estimating equations (population average or marginal) models in the GENMOD package in SAS to obtain predicted 30-day readmission rates and population-averaged odds ratios associated with patient characteristics. We obtained the predicted 30-day readmission rate and 95% CI for each patient characteristic from a multilevel logistic model and a generalized estimating equations model using the margins command after running a logistic regression in Stata (15). For continuous variables, the predicted readmission rates were calculated at the median point. The model was adjusted for patient age, ethnicity, sex, Medicaid eligibility, education, emergency admission, weekend admission, DRG weight, major DRG diagnostic class, nursing home residence in the 90 days before admission, the 31 Elixhauser comorbid conditions entered separately, number of acute hospitalizations in the 12 months before the admission, and number of outpatient visits in the prior year. As an alternative, we implemented a multilevel logistic regression model (patient and PCP) using the same covariates. The model was implemented using the GLIMMIX package in SAS, and the QUAD method allowed variables to be estimated by quadrature (16, 17).
We estimated the risk-standardized rate of 30-day readmissions for each PCP with the method used by CMS (18). Risk-standardized rates were calculated as the ratio of the predicted to expected number of read-missions, multiplied by the national unadjusted rate of readmission. For each PCP, the numerator of the ratio is the number of readmissions predicted within 30 days based on the PCP’s observed case mix. The denominator is the number of readmissions expected based on the nation’s performance with that PCP’s case mix. The model was repeated 1000 times, and the means and 95% CIs were calculated on the basis of these 1000 values for each PCP. We then plotted the adjusted rate and 95% CI for each PCP and ranked them from low to high. We considered a PCP’s readmission rate to be statistically significantly higher or lower than the mean if the 95% CI excluded the mean risk-standardized rate of readmission for all PCPs.
We evaluated the stability of the PCP-level profiling by comparing the risk-standardized rate of 30-day re-admissions generated from the bootstrapping method in 2 time periods (1 January 2008 to 30 November 2011 and 1 January 2012 to 30 November 2015) for the 3408 PCPs with at least 50 admissions in each time period. For each time period, we categorized each PCP as having adjusted rates that were significantly higher than the mean, significantly lower than the mean, or not significantly different from the mean; we then compared the categories in a 2 × 3 table.
To explore the robustness of the estimates of PCP readmission rates, we calculated the 95% CIs for different postulated readmission rates at different postulated sample sizes using the following formula:
We set the expected readmission rate at 13% and calculated the minimum sample sizes that could be used to detect different postulated observed rates (starting at 14.0% and increasing by 0.25–percentage point intervals) that would be significantly different from the expected rate (that is, their 95% CIs excluded 13%).
The analyses of rates of follow-up visits with the PCP were similar to those of readmission rates and had the same covariates. We used SAS, version 9.4 (SAS Institute), and Stata, version 15.1 (StataCorp), for the statistical analyses. The research was reviewed and approved by the University of Texas Medical Branch Institutional Review Board.
Role of the Funding Source
This research was supported by grants from the National Institutes of Health, which had no role in the design, conduct, or analysis of the study or in the decision to submit the manuscript for publication.
RESULTS
The cohorts for investigating readmission included 565 579 hospital admissions in 2012 to 2015 and 4230 PCPs. Each PCP had at least 50 admissions; the median was 108 (interquartile range, 74 to 168 admissions). The Table presents the results of a marginal or population-averaged model examining the association of patient characteristics with the odds of a patient being readmitted within 30 days and with adjusted 30-day readmission rates. Higher adjusted readmission rates were associated with increasing age, male sex, Medicaid eligibility, emergency or weekend admission, nursing home residence, higher DRG weight (indicating greater illness severity), and more episodes of inpatient or ambulatory care in the prior year, but most associations were of small magnitude. Lower rates were associated with Hispanic ethnicity and residence in areas where a higher proportion of residents had a high school education. These results were nearly identical to those from a multilevel logistic regression model that was used to generate risk-standardized rates of 30-day readmissions for PCPs (Appendix Table 3, available at Annals.org).
Table.
Adjusted 30-Day Readmission Rates, by Patient Characteristics, in Medicare Enrollees With a PCP Who Were Discharged Between 1 January 2012 and 30 November 2015, Estimated From a Marginal Logistic Regression Model (PROC GENMOD) (n = 565 579)*
| Patient Characteristic | Patients, n (%) | Odds Ratio (95% CI)† | Adjusted 30-Day Readmission Rate (95% CI), %† | |
|---|---|---|---|---|
| Age | ||||
| 66–70 y | 110 806 (19.6) | 1.00 (reference) | 11.0 (10.8–11.3) | |
| 71–75 y | 120 348 (21.3) | 1.02 (0.99–1.05) | 11.2 (11.0–11.4) | |
| 76–80 y | 117 894 (20.8) | 1.10 (1.06–1.13) | 12.0 (11.7–12.2) | |
| 81–85 y | 105 702 (18.7) | 1.14 (1.11–1.18) | 12.4 (12.2–12.7) | |
| ≥86 y | 110 829 (19.6) | 1.22 (1.18–1.26) | 13.1 (12.9–13.4) | |
| Race | ||||
| Non-Hispanic white | 426 316 (75.4) | 1.00 (reference) | 12.0 (11.9–12.2) | |
| Black | 38 878 (6.9) | 0.99 (0.96–1.04) | 12.0 (11.6–12.4) | |
| Hispanic | 91 731 (16.2) | 0.94 (0.91–0.97) | 11.4 (11.1–11.6) | |
| Other | 10 654 (1.9) | 0.95 (0.89–1.01) | 11.5 (10.8–12.1) | |
| Sex | ||||
| Female | 339 944 (60.1) | 1.00 (reference) | 11.7 (11.5–11.9) | |
| Male | 225 635 (39.9) | 1.05 (1.03–1.07) | 12.2 (12.0–12.4) | |
| Medicaid-eligible | ||||
| No | 466 580 (82.5) | 1.00 (reference) | 11.7 (11.6–11.9) | |
| Yes | 98 999 (17.5) | 1.09 (1.06–1.12) | 12.7 (12.4–13.0) | |
| Percentage of persons aged ≥25 y with high school education or higher in the ZIP code of residence | ||||
| 1st quartile | 142 745 (25.2) | 1.00 (reference) | 11.9 (11.7–12.1) | |
| 2nd quartile | 140 365 (24.8) | 1.03 (1.01–1.06) | 12.2 (12.0–12.5) | |
| 3rd quartile | 142 798 (25.2) | 0.99 (0.97–1.02) | 11.9 (11.6–12.1) | |
| 4th quartile | 139 671 (24.7) | 0.97 (0.94–0.99) | 11.6 (11.4–11.9) | |
| Emergency admission | ||||
| No | 236 106 (41.7) | 1.00 (reference) | 11.3 (11.1–11.4) | |
| Yes | 329 473 (58.3) | 1.12 (1.09–1.14) | 12.4 (12.2–12.6) | |
| Weekend admission | ||||
| No | 432 890 (76.5) | 1.00 (reference) | 11.9 (11.7–12.0) | |
| Yes | 132 689 (23.5) | 1.02 (1.01–1.04) | 12.1 (11.9–12.3) | |
| Nursing home residence | ||||
| No | 541 869 (95.8) | 1.00 (reference) | 11.9 (11.7–12.0) | |
| Yes | 23 710 (4.2) | 1.07 (1.03–1.11) | 12.6 (12.2–13.1) | |
| Mean (SD) | Median (IQR) | Odds Ratio (95% CI)†‡ | Adjusted 30-Day Readmission Rate (95% CI), %†§ | |
| DRG weight | 1.6 (1.3) | 1.1 (0.8–2.0) | 1.06 (1.05–1.07) | 11.6 (11.5–11.8) |
| Hospitalizations in the prior year | 0.4 (0.9) | 0 (0–0) | 1.10 (1.09–1.11) | 11.5 (11.4–11.6) |
| Physician visits in the prior year | 13.4 (8.6) | 11 (7–17) | 1.07 (1.05–1.08) | 11.8 (11.6–11.9) |
DRG = diagnosis-related group; IQR = interquartile range; PCP = primary care physician.
Odds ratios generated from the same model are also presented. Percentages may not sum to 100 due to rounding.
Estimated from a multilevel model with patient characteristics presented in the table, plus major diagnostic category and 31 Elixhauser comorbidity indicators entered individually.
Per 1 DRG unit, 1 hospitalization, or 10 physician visits.
Calculated at the median point for continuous variables.
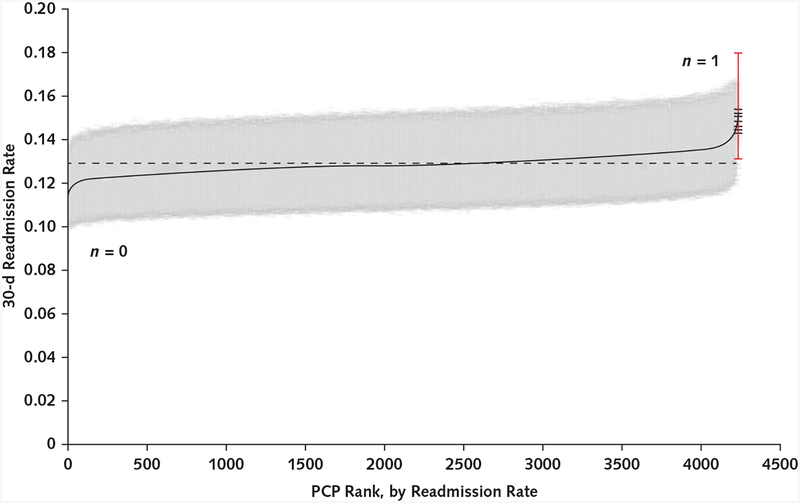
Figure 1 shows the variation among PCPs in the risk-standardized 30-day readmission rates of their patients, adjusted for all of the variables in the Table and generated using the CMS method with bootstrapping. It shows the mean value and 95% CI of the rates for each physician. The average risk-standardized readmission rate for the 4230 PCPs was 12.9%. There was little variation in readmission rates. The minimum value was 11.2% and the maximum 15.3%. The 10th and 90th percentiles for the rates were 12.4% and 13.4%, respectively; each differed from the mean rate by 0.5 percentage point. Only 1 PCP had a rate that was statistically significantly higher than the average, and none had a significantly lower rate.
Figure 1.
Variation among 4230 PCPs in 30-day risk-standardized readmission rates.
Readmission rate estimates were generated with a method used by the Centers for Medicare & Medicaid Services, which generates the ratio of the predicted to expected number of readmissions, multiplied by the national unadjusted rate, with bootstrapping (18). The readmission rates (adjusted means and 95% CIs) for each PCP are ranked from lowest to highest. The adjusted mean rate was 12.9% (dashed line). The minimum and maximum adjusted rates were 11.2% and 15.3%, respectively. The 10th percentile was 12.4% and the 90th was 13.4%, each only 0.5 percentage point from the mean. The 99th percentile rate was 14.0%, 1.1 percentage points above the mean. Only 1 PCP had a significantly higher readmission rate, indicated in red, and no PCP had a significantly lower rate. PCP = primary care physician.
We examined the stability of the readmission rates between the 2 time periods (2008 to 2011 vs. 2012 to 2015) for the 3408 PCPs who had at least 50 admissions in each. In 2008 to 2011, 2 PCPs had risk-adjusted readmission rates that were significantly higher than the mean and 1 had a rate that was lower than the mean. In 2012 to 2015, rates for these 3 PCPs did not differ from the mean.
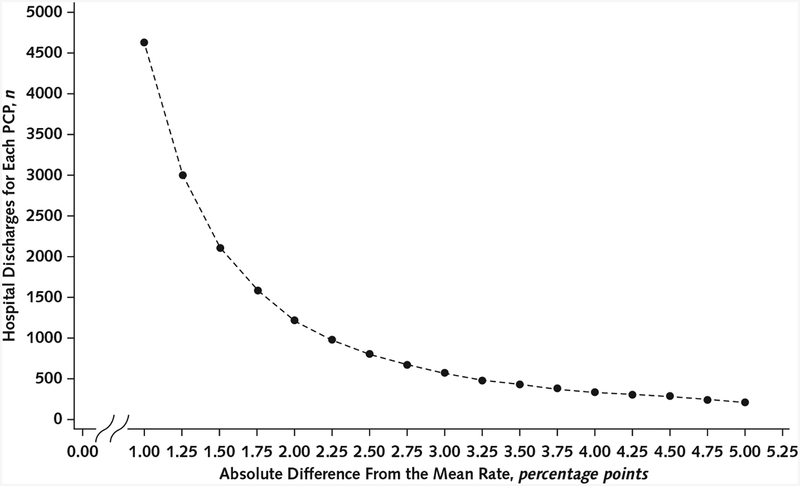
We estimated the minimum number of admissions attributable to a PCP that would result in a readmission rate significantly different from the average adjusted rate. Figure 2 shows the absolute difference from the mean rate for postulated readmission rates versus the minimum number of admissions whereby the 95% CI for that rate would exclude the average rate for all PCPs. The 99th percentile of PCP readmission rates was 14.0%, a difference of 1.1 percentage points from the mean rate of 12.9%. A sample size of more than 3500 admissions would be required for the 95% CI of that rate to exclude the mean rate.
Figure 2.
The number of admissions for each PCP (or group practice) that would result in 95% CIs that exclude a mean readmission rate of 13%, at different absolute differences from the mean rate.
Differences ≤1 percentage point would require >4500 hospital discharges. PCP = primary care physician.
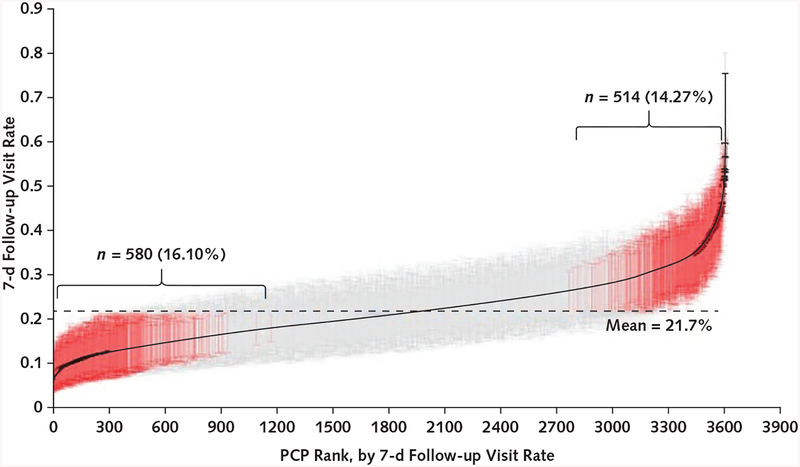
As a comparison with readmission rates, we also calculated rates at which individual PCPs saw their patients within 7 days of hospital discharge to the community (Appendix Table 4, available at Annals.org). The overall rate for the 413 527 beneficiaries followed by 3603 PCPs was 20.4%. Patients were more likely to be seen if they were older, of Hispanic ethnicity, or male; had an emergency admission; had had more physician visits in the prior year; or resided in an area where a higher proportion of adults had a high school education. Patients were less likely to be seen if they were black, had a higher DRG weight, or had been hospitalized more often in the prior year. Figure 3 shows the variation among the 3603 PCPs in rates of seeing their patients within 7 days. The analysis was similar to that used to produce Figure 1. Approximately 14% of PCPs had adjusted follow-up rates that were significantly above average, and approximately 16% of PCPs had significantly lower rates.
Figure 3.
Variation among 3603 PCPs in the risk-standardized rates of follow-up of their hospitalized patients within 7 days of discharge.
Estimates were derived by a method similar to that used by the Centers for Medicare & Medicaid Services to measure readmission rates. We generated the ratio of the predicted to expected number of patients with follow-up for each PCP, multiplied by national rates, with bootstrapping (18). Adjusted rates of follow-up are ranked from lowest to highest. Rates and 95% CIs that significantly differ from the adjusted mean rate of 21.7% (dashed line) are shown in red. Of 3603 PCPs, 514 (14.3%) had 7-d follow-up rates significantly higher than the mean and 580 (16.1%) had rates significantly lower than the mean. The 10th percentile for the rates was 13.0%, and the 90th percentile was 31.2%. PCP = primary care physician.
DISCUSSION
We found almost no significant variation in read-mission rates by PCP. The adjusted readmission rate at the 99th percentile and the mean rate for the 4230 PCPs differed by only 1.1 percentage points. The number of admissions per PCP that would be required for reasonable power to detect the differences in readmission rates among PCPs is far larger than the number of admissions actually generated by individual PCPs. Of note, the data on PCP admissions in our analyses were obtained over 47 months. Any evaluations based on yearly data would have only about a quarter as many cases. Also, we included only PCPs with at least 50 hospital admissions. This excluded 65% of the PCPs in the Texas Medicare data (Appendix Table 1).
This research has important implications for health care policy. In 2015, CMS launched the Merit-based Incentive Payment System, a pay-for-performance program (11). In this program, performance on readmissions is a mandatory and important measure for groups with 16 or more physicians who collectively have more than 200 admissions per year. An assumption underlying this requirement is that readmission rates vary by PCP independently of patient characteristics; therefore, applying penalties and incentives will incentivize PCPs to change their practice patterns to reduce readmissions. Our finding of minimal variation in risk for readmission among PCPs calls into question any pay-for-performance program that aims to reduce readmissions and assumes variation by PCP. Furthermore, our analysis indicates that the threshold used in the Merit-based Incentive Payment System of 200 or more readmissions per year is far too low to distinguish real-world differences among PCPs or group practices.
Tang and colleagues (19) described substantial variation in readmission rates among primary care clinics within a single tertiary care center. This variation may be explained by the clinical diversity of patients between clinics (for example, HIV vs. geriatric clinics) and lack of adjustment for individual patient characteristics. We are not aware of any other studies that have examined variation in readmission rates among individual PCPs.
We show low rates of and substantial variation in early postdischarge follow-up by PCP. These results mirror the findings noted at the hospital level in previous research (9, 20). Our research points to a continued opportunity to increase rates of and standardize decision making about postdischarge follow-up, as recommended by professional societies (21) and encouraged by federal policy (22).
Our finding of minimal variation in readmission rates by PCP should be taken in the context of our previous research that showed significant variation in risk for readmission by ED physician (10). At the hospital level, overall admission rates are a major determinant of hospital readmission rates (23). The lack of variation in readmission rates by PCP coupled with significant variation among ED physicians suggests that admission and readmission decisions for many patients are made by the ED physician rather than the PCP (24). This may be especially true for recently discharged patients because PCPs may feel less equipped to address their care owing to increasing discontinuity because of increasing use of hospitalists (25). This discontinuity is amplified by poor handoffs of care to the PCP at discharge (26, 27), and most PCPs are unaware of the worsening condition that leads to their patient’s readmission (28).
This study has limitations. We studied patients with fee-for-service Medicare over a 4-year period. We could not control for patient characteristics that are not captured in Medicare databases. Our findings may not be generalizable to younger patient populations or other time periods. We could not classify our readmissions as avoidable versus unavoidable. The readmission rates in our study are lower than those reported for Medicare beneficiaries nationally (1), perhaps because we selected only patients who had a PCP and selected only 1 hospitalization per patient per year. Our study was limited to Texas and may not be generalizable to other areas, although the readmission rates in Texas are similar to nationwide rates (29). Our finding of lack of variation in readmission rates by PCP does not necessarily mean that incentivizing and penalizing PCPs to reduce readmissions will not influence readmission rates. An alternate but less likely interpretation of our findings is that PCP practice patterns influencing read-mission rates are uniformly poor, with room for improvement among all PCPs.
In summary, this study shows negligible variation in readmission rates among PCPs when patient characteristics are controlled for. Primary care physicians do not generate sufficient admissions to expect reasonable power to detect differences by PCPs or by most group practices. Therefore, pay-for-performance programs to reduce readmissions on the basis of variation in read-mission rates among PCPs may not be effective.
Grant Support:
By grants AG033134, K05CA134923, P30AG024832, and UL1TR001439 from the National Institutes of Health.
Appendix
Appendix Table 1.
Steps in Cohort Selection for Analyzing Readmission Within 30 Days After Discharge
| Step | 2012 | 2013 | 2014 | 2015* |
|---|---|---|---|---|
| Step 1: Select short-stay hospitalizations of TX beneficiaries from TX physicians | 854 399 | 834 217 | 848 694 | 789 283 |
| Step 2: Select first hospitalization for patients with >1 hospitalization in that year | 540 889 | 535 530 | 544 301 | 516 297 |
| Step 3: Include only patients discharged alive and not to other acute care hospitals | 509 401 | 505 134 | 513 343 | 486 902 |
| Step 4: Select patients aged ≥66 y at admission | 395 056 | 392 642 | 400 962 | 381 860 |
| Step 5: Exclude those who died without readmission ≤30 d after hospital discharge | 380 546 | 377 474 | 385 188 | 366 388 |
| Step 6: Include only those patients with complete enrollment in the prior year before admission and ≥30 d after hospital discharge | 277 851 | 258 097 | 255 277 | 234 310 |
| Step 7: Select patients who had a PCP in the prioryear | 184 069 (8584 PCPs) | 169 031 (8596 PCPs) | 164 778 (8659 PCPs) | 150 274 (8542 PCPs) |
| Step 8: Exclude those without DRG or education information | 184 069 (8584 PCPs) | 169 031 (8596 PCPs) | 164 764 (8659 PCPs) | 150 257 (8542 PCPs) |
| Step 9: Combine 4 y of data | - | - | - | 664 092 (11 958 PCPs) |
| Step 10: Keep enrollees who had PCPs with ≥50 admissions | - | - | - | 565 579 (4230 PCPs) |
DRG = diagnosis-related group; PCP = primary care physician; TX = Texas.
Discharges on or before 1 December 2015, to allow for 30 d of follow-up.
Appendix Table 2.
Steps in Cohort Selection for Analyzing 7-Day Follow-up Visit*
| Step | 2012 | 2013 | 2014 | 2015† |
|---|---|---|---|---|
| Step 1: Select short-stay hospitalizations of TX beneficiaries from TX physicians | 854 399 | 834217 | 848 694 | 789 283 |
| Step 2: Select all patients discharged home after hospitalization | 564 944 | 546 783 | 550 458 | 510 520 |
| Step 3: Select first hospitalization for patients with >1 hospitalization in that year | 398 925 | 390 824 | 394 593 | 372 607 |
| Step 4: Select patients aged ≥66 y at admission | 298 227 | 292 280 | 296 517 | 281 461 |
| Step 5: Include only those patients with complete enrollment in the prioryear before admission and ≥30 d after hospital discharge | 213 500 | 195 083 | 190 896 | 174 599 |
| Step 6: Select patients who had a PCP in the prior year | 146 363 (8358 PCPs) | 132 407 (8321 PCPs) | 127 926 (8358 PCPs) | 116 042 (8265 PCPs) |
| Step 7: Exclude those without DRG or education information | 145 575 (8354 PCPs) | 131 613 (8313 PCPs) | 127 199 (8351 PCPs) | 115 474 (8263 PCPs) |
| Step 8: Combine 4 y of data | - | - | - | 519 861 (11 412 PCPs) |
| Step 9: Keep enrollees with PCPs who had ≥50 admissions | - | - | - | 413 527 (3603 PCPs) |
DRG = diagnosis-related group; PCP = primary care physician; TX = Texas.
Selection of the cohort for calculating rate of follow-up visits within 7 d of discharge differs from that of the readmission cohort in that the follow-up visit cohort includes only patients discharged to the community and includes enrollees who died within 30 d of discharge.
Discharges on or before 1 December 2015, to allow for 30 d of follow-up.
Appendix Table 3.
Adjusted 30-Day Readmission Rates, by Patient Characteristics, in Medicare Enrollees With a PCP Who Were Discharged Between 1 January 2012 and 30 November 2015, Estimated From a Multilevel Logistic Regression Model (PROC GLIMMIX) Adjusted by Patient Characteristics (n = 565 579)*
| Patient Characteristic | Patients, n (%) | Odds Ratio (95% CI)† | Adjusted 30-Day Readmission Rate (95% CI), %† | |
|---|---|---|---|---|
| Age | ||||
| 66–70 y | 110 806 (19.6) | 1.00 (reference) | 11.0 (10.8–11.3) | |
| 71–75 y | 120 348 (21.3) | 1.02 (0.99–1.05) | 11.2 (11.0–11.4) | |
| 76–80 y | 117 894 (20.8) | 1.10 (1.06–1.13) | 12.0 (11.7–12.2) | |
| 81–85 y | 105 702 (18.7) | 1.14 (1.11–1.18) | 12.4 (12.2–12.7) | |
| ≥86 y | 110 829 (19.6) | 1.22 (1.18–1.26) | 13.1 (12.9–13.4) | |
| Race | ||||
| Non-Hispanic white | 426 316 (75.4) | 1.00 (reference) | 12.0 (11.9–12.2) | |
| Black | 38 878 (6.9) | 0.99 (0.96–1.04) | 12.0 (11.6–12.4) | |
| Hispanic | 91 731 (16.2) | 0.94 (0.91–0.97) | 11.4 (11.1–11.6) | |
| Other | 10 654 (1.9) | 0.95 (0.89–1.01) | 11.5 (10.8–12.1) | |
| Sex | ||||
| Female | 339 944 (60.1) | 1.00 (reference) | 11.7 (11.5–11.9) | |
| Male | 225 635 (39.9) | 1.05 (1.03–1.07) | 12.2 (12.0–12.4) | |
| Medicaid-eligible | ||||
| No | 466 580 (82.5) | 1.00 (reference) | 11.7 (11.6–11.9) | |
| Yes | 98 999 (17.5) | 1.09 (1.06–1.12) | 12.7 (12.4–13.0) | |
| Percentage of persons aged ≥25 y with high school education or higher in the ZIP code of residence | ||||
| 1st quartile | 142 745 (25.2) | 1.00 (reference) | 11.9 (11.7–12.1) | |
| 2nd quartile | 140 365 (24.8) | 1.03 (1.01–1.06) | 12.2 (12.0–12.5) | |
| 3rd quartile | 142 798 (25.2) | 0.99 (0.97–1.02) | 11.9 (11.6–12.1) | |
| 4th quartile | 139 671 (24.7) | 0.97 (0.94–0.99) | 11.6 (11.4–11.8) | |
| Emergency admission | ||||
| No | 236 106 (41.7) | 1.00 (reference) | 11.3 (11.1–11.4) | |
| Yes | 329 473 (58.3) | 1.12 (1.09–1.14) | 12.4 (12.2–12.6) | |
| Weekend admission | ||||
| No | 432 890 (76.5) | 1.00 (reference) | 11.9 (11.7–12.0) | |
| Yes | 132 689 (23.5) | 1.02 (1.01–1.04) | 12.1 (11.8–12.3) | |
| Nursing home residence | ||||
| No | 541 869 (95.8) | 1.00 (reference) | 11.9 (11.7–12.0) | |
| Yes | 23 710 (4.2) | 1.07 (1.03–1.11) | 12.6 (12.2–13.1) | |
| Mean (SD) | Median (IQR) | Odds Ratio (95% CI)†‡ | Adjusted 30-Day Readmission Rate (95% CI), %†§ | |
| DRG weight | 1.6 (1.3) | 1.1 (0.8–2.0) | 1.06 (1.05–1.07) | 11.6 (11.5–11.8) |
| Hospitalizations in the prior year | 0.4 (0.9) | 0 (0–0) | 1.10 (1.09–1.11) | 11.5 (11.3–11.6) |
| Physician visits in the prior year | 13.4 (8.6) | 11 (7–17) | 1.07 (1.05–1.08) | 11.8 (11.6–11.9) |
DRG = diagnosis-related group; IQR = interquartile range; PCP = primary care physician.
Odds ratios generated from the same model are also presented. Percentages may not sum to 100 due to rounding.
Estimated from a multilevel model with patient characteristics presented in the table, plus major diagnostic category and 31 Elixhauser comorbidity indicators entered individually.
Per 1 DRG unit, 1 hospitalization, or 10 physician visits.
Calculated at the median point for continuous variables.
Appendix Table 4.
Adjusted Rates of Medicare Enrollees Seeing Their PCP Within 7 Days of Hospital Discharge, by Patient Characteristics, for Enrollees With an Identifiable PCP, 1 January 2012 to 30 November 2015 (n = 413 527)*
| Patient Characteristic | Patients, n (%) | Odds Ratio (95% CI)† | Adjusted 7-Day Follow-up Visit Rate (95% CI), %† | |
|---|---|---|---|---|
| Age | ||||
| 66–70 y | 90 044 (19.8) | 1.00 (reference) | 17.5 (17.1–17.9) | |
| 71–75 y | 94 841 (21.5) | 1.06 (1.03–1.09) | 18.4 (18.0–18.8) | |
| 76–80 y | 87 945 (21.5) | 1.10 (1.07–1.13) | 19.0 (18.5–19.4) | |
| 81–85 y | 73 033 (17.7) | 1.14 (1.10–1.17) | 19.5 (19.0–19.9) | |
| ≥86 y | 67 664 (16.4) | 1.11 (1.07–1.14) | 19.0 (18.5–19.4) | |
| Race | ||||
| Non-Hispanic white | 308 324 (74.6) | 1.00 (reference) | 18.5 (18.1–18.9) | |
| Black | 27 045 (6.5) | 0.96 (0.92–0.99) | 17.9 (17.3–18.5) | |
| Hispanic | 70 646 (17.1) | 1.05 (1.02–1.09) | 19.3 (18.8–19.8) | |
| Other | 7512 (1.8) | 1.04 (0.97–1.11) | 19.1 (18.1–20.1) | |
| Sex | ||||
| Female | 239 580 (57.9) | 1.00 (reference) | 18.3 (18.0–18.7) | |
| Male | 173 947 (42.1) | 1.04 (1.02–1.06) | 19.0 (18.5–19.3) | |
| Medicaid-eligible | ||||
| No | 341 815 (82.7) | 1.00 (reference) | 18.7 (18.3–19.0) | |
| Yes | 71 712 (17.3) | 0.98 (0.95–1.01) | 18.3 (17.8–18.8) | |
| Percentage of persons aged ≥25 y with high school education or higher in the ZIP code of residence | ||||
| 1st quartile | 103 760 (25.1) | 1.00 (reference) | 19.2 (18.8–19.7) | |
| 2nd quartile | 104 189 (25.6) | 0.96 (0.92–0.98) | 18.5 (18.1–18.9) | |
| 3rd quartile | 103 346 (25.0) | 0.97 (0.93–0.99) | 18.7 (18.2–19.1) | |
| 4th quartile | 102 232 (24.7) | 0.92 (0.89–0.95) | 18.0 (17.5–18.4) | |
| Emergency admission | ||||
| No | 176 688 (42.7) | 1.00 (reference) | 16.3 (15.9–16.7) | |
| Yes | 236 839 (57.3) | 1.32 (1.28–1.35) | 20.4 (20.0–20.8) | |
| Weekend admission | ||||
| No | 316 313 (76.5) | 1.00 (reference) | 18.6 (18.2–19.0) | |
| Yes | 97 214 (23.5) | 0.99 (0.97–1.02) | 186. (18.1–19.0) | |
| Nursing home residence | ||||
| No | 395 983 (95.8) | 1.00 (reference) | 18.7 (18.3–19.0) | |
| Yes | 17 544 (4.2) | 0.89 (0.84–0.93) | 16.9 (16.2–17.6) | |
| Mean (SD) | Median (IQR) | Odds Ratio (95% CI)†‡ | Adjusted 7-Day Follow-up Visit Rate (95% CI), %†§ | |
| DRG weight | 1.4 (1.1) | 1.1 (0.8–1.8) | 0.85 (0.84–0.87) | 19.6 (19.0–19.9) |
| Hospitalizations in the prioryear | 0.5 (1.0) | 0 (0–1.0) | 0.89 (0.88–0.90) | 19.4 (19.0–19.8) |
| Physician visits in the prioryear | 13.6 (8.7) | 12 (7–18) | 1.17 (1.15–1.18) | 18.2 (17.8–18.6) |
DRG = diagnosis-related group; IQR = interquartile range; PCP = primary care physician.
The rates are estimated from a marginal logistic regression model (PROC GENMOD). Odds ratios generated from the same model are also presented. Percentages may not sum to 100 due to rounding.
Estimated from a multilevel model with patient characteristics presented in the table, plus major diagnostic category and 31 Elixhauser comorbidity indicators entered individually.
Per 1 DRG unit, 1 hospitalization, or 10 physician visits.
Calculated at the median point for continuous variables.
Footnotes
Disclosures: Dr. Singh reports personal fees from AstraZeneca outside the submitted work. Dr. Goodwin reports grants from the National Institutes of Health during the conduct of the study. Dr. Nattinger reports grants from the National Institutes of Health during the conduct of the study. Authors not named here have disclosed no conflicts of interest. Disclosures can also be viewed at www.acponline.org/authors/icmje/ConflictOfInterestForms.do?msNum=M18–2526.
Reproducible Research Statement: Study protocol and statistical code: Available from Dr. Zhou (jiezhou@utmb.edu). Data set: The analytic data set is restricted by a data use agreement with CMS that precludes sharing.
References
- 1.Jencks SF, Williams MV, Coleman EA. Rehospitalizations among patients in the Medicare fee-for-service program. N Engl J Med. 2009;360:1418–28. doi: 10.1056/NEJMsa0803563 [DOI] [PubMed] [Google Scholar]
- 2.Halfon P, Eggli Y, Prêtre-Rohrbach I, Meylan D, Marazzi A, Burnand B. Validation of the potentially avoidable hospital readmission rate as a routine indicator of the quality of hospital care. Med Care. 2006;44:972–81. [DOI] [PubMed] [Google Scholar]
- 3.Medicare Payment Advisory Commission. Report to the Congress: Promoting Greater Efficiency in Medicare. Washington, DC: Medicare Payment Advisory Commission; 2007. [Google Scholar]
- 4.Centers for Medicare & Medicaid Services. Hospital Readmissions Reduction Program (HRRP). Accessed at www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/AcuteInpatientPPS/Readmissions-Reduction-Program.html on 31 August 2018.
- 5.McIlvennan CK, Eapen ZJ, Allen LA. Hospital Readmissions Reduction Program. Circulation 2015;131:1796–803. doi: 10.1161/CIRCULATIONAHA.114.010270 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kuo YF, Goodwin JS. Association of hospitalist care with medical utilization after discharge: evidence of cost shift from a cohort study. Ann Intern Med. 2011;155:152–9. doi: 10.7326/0003-4819-155-3-201108020-00005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Goodwin JS, Lin YL, Singh S, Kuo YF. Variation in length of stay and outcomes among hospitalized patients attributable to hospitals and hospitalists. J Gen Intern Med. 2013;28:370–6. doi: 10.1007/s11606-012-2255-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Sharma G, Kuo YF, Freeman JL, Zhang DD, Goodwin JS. Outpatient follow-up visit and 30-day emergency department visit and re-admission in patients hospitalized for chronic obstructive pulmonary disease. Arch Intern Med. 2010;170:1664–70. doi: 10.1001/archinternmed.2010.345 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Hernandez AF, Greiner MA, Fonarow GC, Hammill BG, Heiden reich PA, Yancy CW, et al. Relationship between early physician follow-up and 30-day readmission among Medicare beneficiaries hospitalized for heart failure. JAMA. 2010;303:1716–22. doi: 10.1001/jama.2010.533 [DOI] [PubMed] [Google Scholar]
- 10.Singh S, Lin YL, Nattinger AB, Kuo YF, Goodwin JS. Variation in readmission rates by emergency departments and emergency department providers caring for patients after discharge. J Hosp Med. 2015;10:705–10. doi: 10.1002/jhm.2407 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Centers for Medicare & Medicaid Services . MIPS overview. Accessed at https://qpp.cms.gov/mips/overview on 31 August 2018.
- 12.Shah BR, Hux JE, Laupacis A, Zinman B, Cauch-Dudek K, Booth GL. Administrative data algorithms can describe ambulatory physician utilization. Health Serv Res. 2007;42:1783–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Goodwin JS, Li S, Zhou J, Graham JE, Karmarkar A, Ottenbacher K. Comparison of methods to identify long term care nursing home residence with administrative data. BMC Health Serv Res. 2017;17: 376. doi: 10.1186/s12913-017-2318-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Quan H, Sundararajan V, Halfon P, Fong A, Burnand B, Luthi JC, et al. Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Med Care. 2005;43:1130–9. [DOI] [PubMed] [Google Scholar]
- 15.Rabe-Hesketh S, Skrondal A. Multilevel and Longitudinal Modeling Using STATA. 2nd ed. College Station, TX: Stata Pr; 2008. [Google Scholar]
- 16.Zhu M Analyzing multilevel models with the GLIMMIX procedure. Cary, NC: SAS Institute; 2014. Accessed at https://support.sas.com/resources/papers/proceedings14/SAS026-2014.pdf on 31 August 2018. [Google Scholar]
- 17.Leyland AH, Goldstein H. Multilevel Modelling of Health Statistics. New York: Wiley; 2001. [Google Scholar]
- 18.Horwitz L, Partovian C, Lin Z, Herrin J, Grady J, Conover M, et al. Hospital-Wide All-Cause Risk-Standardized Readmission Measure: Measure Methodology Report Prepared for the Centers for Medicare & Medicaid Services. New Haven, CT: Yale New Haven Health Services Corporation/Center for Outcomes Research & Evaluation; 2011. [Google Scholar]
- 19.Tang N, Maselli JH, Gonzales R. Variations in 30-day hospital readmission rates across primary care clinics within a tertiary referral center. J Hosp Med. 2014;9:688–94. doi: 10.1002/jhm.2243 [DOI] [PubMed] [Google Scholar]
- 20.Hess CN, Shah BR, Peng SA, Thomas L, Roe MT, Peterson ED. Association of early physician follow-up and 30-day readmission after non-ST-segment-elevation myocardial infarction among older patients. Circulation. 2013;128:1206–13. doi: 10.1161/CIRCULATIONAHA.113.004569 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Albert NM, Barnason S, Deswal A, Hernandez A, Kociol R, Lee E, et al. ; American Heart Association Complex Cardiovascular Patient and Family Care Committee of the Council on Cardiovascular and Stroke Nursing, Council on Clinical Cardiology, and Council on Quality of Care and Outcomes Research. Transitions of care in heart failure: a scientific statement from the American Heart Association. Circ Heart Fail. 2015;8:384–409. doi: 10.1161/HHF.0000000000000006 [DOI] [PubMed] [Google Scholar]
- 22.Bloink J, Adler KG. Transitional care management services: new codes, new requirements. Fam Pract Manag. 2013;20:12–7. [PubMed] [Google Scholar]
- 23.Epstein AM, Jha AK, Orav EJ. The relationship between hospital admission rates and rehospitalizations. N Engl J Med. 2011;365: 2287–95. doi: 10.1056/NEJMsa1101942 [DOI] [PubMed] [Google Scholar]
- 24.Morganti KG, Bauhoff S, Blanchard JC, Abir M, Smith A, Vesely J, et al. The evolving roles of emergency departments. Santa Monica, CA: RAND Corporation; 2013. Accessed at www.rand.org/pubs/research_briefs/RB9715.html on 31 August 2018. [PMC free article] [PubMed] [Google Scholar]
- 25.Kuo YF, Sharma G, Freeman JL, Goodwin JS. Growth in the care of older patients by hospitalists in the United States. N Engl J Med. 2009;360:1102–12. doi: 10.1056/NEJMsa0802381 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.van Walraven C, Seth R, Austin PC, Laupacis A. Effect of discharge summary availability during post-discharge visits on hospital readmission. J Gen Intern Med. 2002;17:186–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kripalani S, LeFevre F, Phillips CO, Williams MV, Basaviah P, Baker DW. Deficits in communication and information transfer between hospital-based and primary care physicians: implications for patient safety and continuity of care. JAMA. 2007;297:831–41. [DOI] [PubMed] [Google Scholar]
- 28.Feigenbaum P, Neuwirth E, Trowbridge L, Teplitsky S, Barnes CA, Fireman E, et al. Factors contributing to all-cause 30-day readmissions: a structured case series across 18 hospitals. Med Care. 2012;50:599–605. doi: 10.1097/MLR.0b013e318249ce72 [DOI] [PubMed] [Google Scholar]
- 29.United Health Foundation. Trend: hospital readmissions, Texas, United States. Accessed at www.americashealthrankings.org/explore/senior/measure/hospital_readmissions_sr/state/TX?edition-year=2016 on 31 August 2018.