Abstract
Objective
Depression is a serious mental health disorder, and untangling its causal agents is a major public health priority in the United States. This study examines the relationship between participating in welfare programs during childhood and experiencing depression during young adulthood.
Method
This study used wave I and IV data from the Add Health (N = 15,701). Multiple imputation is used to deal with missing data. Propensity score matching is used to reduce the selection bias, and then multiple regressions were used to examine the welfare participation and depression relationships.
Results
Overall, young adults from welfare-recipient families reported significantly higher depression scores, rather than the clinical diagnosis of depression. Subgroup analyses showed only the poor group had significantly higher depression scores, whereas only the near-poor group had a significantly diagnosed depression outcome. Additionally, significantly higher depression scores were found for female youth from welfare-recipient families. However, no significant differences were found between the gender groups regarding diagnosed depression.
Discussion
Using welfare participation as an economic marker, the subgroup analyses help to identify target populations for future intervention. Implications of this study will be of interest to policy makers and have value for informing policy decisions.
Keywords: Welfare participation, Child poverty, Depression, CESD, Social determinate of health, Add Health
1. Introduction
The series of New Deal programs proposed by President Franklin Roosevelt and enacted by the U.S. Congress during the 1930s began a transformation of the U.S. from a society of winners and losers to a society that is a unique melding of democracy, welfare, and capitalism (Marshall, 1950; Moffitt, 2015). The New Deal aimed to create a safety net of programs to improve the lives of those suffering the effects of the Great Depression such as high rates of unemployment (about 25%), food insecurity and hunger, inability to afford medical care, and poor housing and homelessness. Specifically, the Social Security Act of 1935 (Public Law 74–271) was enacted to provide general welfare to needy populations (e.g., the elderly, the blind, and dependent children). In the decades that followed, this Act and its subsequent amendments served as a catalyst for the expansion of welfare coverage and eligibility (e.g., the Medicare program of 1965 that provides medical insurance to adults 65 years and older).
Title IV of the 1935 Social Security Act created the federal assistance or “welfare” program known as Aid to Families with Dependent Children (AFDC). AFDC was administered through the U.S. Department of Health and Human Services (U.S. DHHS), and was designed as an unconditional means-tested welfare program to provide cash welfare payments to children who did not have parental support due to the parents’ absence from the home, death, disability, or unemployment (U.S. DHHS, 2009). Over time, eligibility restrictions were relaxed, which led to increases in the number of welfare recipients. Without time limits, AFDC became a long-term, primary income source for some families (Maynard et al., 1998). AFDC operated until 1996, when President Bill Clinton signed the Personal Responsibility and Work Opportunity Reconciliation Act (PRWORA; Public Law 104–193), shifting the U.S. social welfare policy from “welfare” to “workfare”; that is, a shift from a program of unconditional means-tested cash assistance to a program requiring work participation or participation in job training programs. AFDC was replaced by the Temporary Assistance for Needy Families (TANF) program (Besley and Coate, 1992), and introduced other reforms such as lifetime participation limits. The reforms that came with PRWORA rested on the assumption that workforce participation would, overtime, produce families, particularly mothers, that were more self-confident and satisfied with their lives because they were contributing through work to the support of their children. In turn, the children of these mothers would develop better work habits and healthier lifestyles that would help them as they moved into adulthood (Shonkoff et al., 2012). Yet, even though the PRWORA reforms were implemented more than 20 years ago, little is known about the relationship between welfare participation in childhood and mental health. Young adulthood is a developmental period in which young people are making critical choices about work, education, life partners, and forming health habits that have far reaching consequences – positive or negative. Mental health problems, such as depression, impact young peoples’ ability to progress in these important life areas. Because we know poverty is linked to mental health problems, it is important to know if poverty alleviation programs such as TANF make a difference. However, such research has been largely neglected. This study examines the association between participating in welfare programs during childhood (birth to 18 years) and depression during young adulthood (24–32 years). By creating a better understanding of the relationship between welfare participation and depression, this study has potential to inform the development of new programs and interventions at the intersection of poverty alleviation and health care.
1.1. Poverty rates and welfare participation in the United States
Among developed countries, the United States has the world’s highest poverty rate (Organisation for Economic Co-operation and Development, 2017). In 2015 13.5% of the population lived at or below the federal poverty level defined as having income less than $48,072 (200% of the federal poverty level [FPL]; U.S. Census Bureau, 2016). Similarly, the child poverty rate in the United States is among the highest in a developed country (United Nations International Children’s Emergency Fund, 2012, 2014). In 2014, 43% of the U.S. child population, or 31 million children were living in poverty in the U.S. (Jiang et al., 2016).
Living in low-income households exposes adults and children to elevated risk and greater likelihood of experiencing adverse conditions such as homelessness, unsafe neighborhoods, food insecurity, and inadequate health care (Coleman-Jensen et al., 2014; McBride Murry et al., 2011; Smith et al., 2000). In turn, these adverse conditions contribute to negative child outcomes such as poor academic achievement and school drop out as well as short- and long-term problems in the areas of behavioral, psychosocial, physical, and mental health (Casey et al., 2004; Smith et al., 2000).
In response to high poverty rates, the United States federal government has implemented policies and programs aimed at reducing poverty by assisting the low-income population with meeting basic needs. These programs, often referred to as the social safety net, include the Supplemental Nutrition Assistance Program (SNAP; formerly known as the Food Stamp program); Housing Choice Voucher program (i.e., Section 8 housing assistance); Supplemental Security Income; TANF; the Women, Infants, and Children program; and Medicaid. In 2016, about 67.9 million Americans were receiving some form of governmental poverty alleviation benefits. In addition, about 70.5 million people were enrolled in Medicaid (Statistic Brain Research Institute, 2016). By January 2018, 33 States had expanded Medicaid. The Federal government fully covered the Medicaid expansion costs until 2017, and 90% of the costs through 2020 (FamiliesUSA, 2018). Medicaid expansion covers people with income under 138% FPL with severe and persistent mental illness. However, 18 States (35%) from the middle and southeast United States have not yet expanded Medicaid (FamiliesUSA, 2018), meaning low income people from more than one third of the country have limited healthcare access and coverage, especially for mental illness.
Although these safety net programs were instituted to increase child well-being, participation in welfare programs is associated with long-term negative health outcomes. Women who received welfare benefits (e.g., TANF) had a higher risk of developing mental health problems such as depression, compare with those who did not receive welfare benefits (Coiro, 2001). Childhood poverty predicts problem health behavior during adulthood. Children from welfare recipient families faced elevated risk in adulthood for substance use (Wu et al., 2016) and smoking (Zerden et al., accepted). Children participating in TANF had lower cognitive development scores (measured using the Peabody Picture Vocabulary Test) than their counterparts living in households that did not receive benefits (Heflin and Acevedo, 2011). Despite these critical associations between welfare participation and well-being, few studies address problem onset. We do not know whether findings differ for those children in families who are poor and qualify for TANF versus those who do not qualify yet are regularly unable to pay for basic needs. To address this knowledge gap, this study used national representative data to investigate the association between welfare participation in childhood and depression in young adulthood, and whether such relationships differ between families in similar income brackets, some of whom receive benefits and some not.
1.2. Prevalence of depression among U.S. Youth
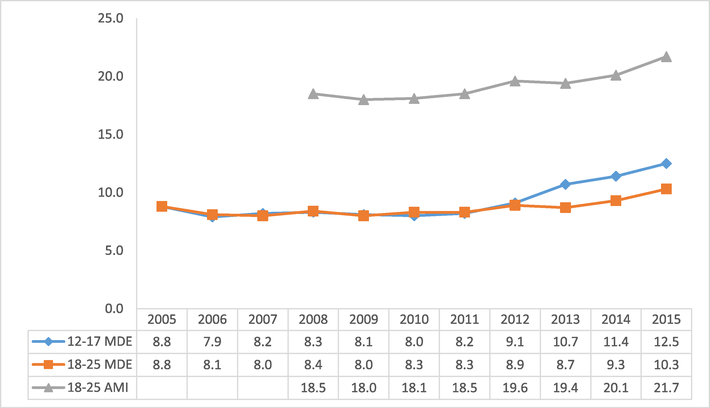
Depression is a common mental disorder among adolescents in the United States (ages 12–17 years; Center for Behavioral Health Statistics and Quality [CBHSQ], 2016). Results from the National Survey on Drug Use and Health (NSDUH) indicate an increasing trend in the number of U.S. adolescents affected by depression (CBHSQ, 2016). As shown in Fig. 1, data from 2005 show about 8.8% of adolescents were diagnosed as having a major depressive episode (MDE) that met the criteria of the Diagnostic and Statistical Manual of Mental Disorders (4th edition; DSM-IV; American Psychiatric Association, 1994). This percentage increased to 9.1% in 2012, 10.7% in 2013, and 11.4% in 2014. In 2015, the percentage of youth with a diagnosed MDE reached a high point of 12.5%, which translates to approximately 3 million adolescents (CBHSQ, 2016).
Fig. 1.
Prevalence of major depressive episodes (MDE) and all other forms of mental illness (AMI) by age group. Figure reproduced from Center for Behavioral Health Statistics and Quality, 2016.
Similarly, in 2015, nearly 10.3% of U.S. young adults (ages 18–25 years), or about 3.6 million, had a past-year MDE meeting DSM-IV criteria (CBHSQ, 2016). Although this percentage is lower than the prevalence among adolescents, the young adult group also had a high prevalence of other types of mental disorders (See Fig. 1). Since 2008, more than 18% of young adults have received a clinical diagnosis for at least one type of mental illness or disorder meeting DSM-IV criteria. In 2015, 21.7% of young adults (about 7.8 million individuals) were reported to have had some type of mental disorder, which means that more than 1 in 5 young American adults suffered from a mental illness (CBHSQ, 2016).
The high prevalence of mental illness among U.S. adolescents and young adults is evidence of a serious public health issue. Urgent attention to this public health crisis is warranted because mental illness at an early age affects not only a person’s physical and psychosocial developmental trajectory but also the person’s ability to live independently and lead a self-sufficient, productive life (Brown et al., 2009; Elovainio et al., 2015; Stewart et al., 2003). Yet, in 2015, among the 3 million youth with a past-year MDE, about 60.7% (1.8 million) did not receive treatment for depression (CBHSQ, 2016). Similarly, more than half (53.2%) of young adults (18–25 years) with a past-year MDE did not receive treatment for depression (CBHSQ, 2016).
Depression is associated with socioeconomic status (SES), with the prevalence of depression unevenly distributed across the different SES strata (Gilman et al., 2002). SES is commonly assessed using the federal poverty level (FPL). The FPL is updated annually to calculate the minimum income needed to sustain households of different family size, composition, and location (e.g., the FPL is higher in Alaska and Hawaii than on the U.S. mainland). SES is often described as having income of a certain percentage above or below the FPL. Mental health researchers have shown statistically significant negative relationships between SES and the presence of mental illness, such that people from lower SES levels have higher risk of mental illness (Gilman et al., 2002; Hudson, 2005; Wu et al., 2018). Given the evidence supporting the links between gender, SES, and mental health (e.g., Aneshensel and Sucoff, 1996; Belle, 1990; Jackson and Williams, 2006), this paper expands the examination of the relationship between childhood welfare participation and depression in young adulthood to include the investigation of whether these relationships differ by household income levels and by respondents’ gender.
1.3. Theoretical framework: wider determinants of health model
Although the Social Determinants of Health Framework has come into widespread use in recent years (Evans et al., 2017; Garg et al., 2015; Marmot, Friel, Bell, Houweling, Taylor, & Commission on Social Determinants of Health, 2008; Viner et al., 2012), The Wider Determinants of Health model (Dahlgren and Whitehead, 1991) posits many, if not all of the same relationships. Both frameworks suggest that good health is produced by the complex interrelationships of genetic make-up, age, gender, behavioral factors (e.g., lifestyle choices of physical activity and dietary habits), social determinants (e.g., work environment, transportation, education, health and social care services, unemployment, and welfare), and other physical and social environmental factors. An increasing number of studies have demonstrated a significant impact of the social determinants of health (SDH) on individual health status. Among other factors, the SDH include quality of housing, suitability of work, and access to health care and social welfare services (Bambra et al., 2010; Marmot et al., 2008; Viner et al., 2012). Poverty becomes a SDH because it inhibits the ability to create a healthy life-style. Specifically, fresh fruits, vegetables, and meats are more expensive than less healthy food choices. Further, access to health care, safe housing, safe neighborhoods, and quality education are all threatened in impoverished conditions. These resource gaps contribute to poor health (Elovainio et al., 2015). However, more research is needed to better understand the relationship between welfare policies and mental health outcomes (Bambra et al., 2010). The current study aims to fill this research gap by using data from a national longitudinal survey to examine the following three research questions:
Compared with young adults from non-welfare recipient families, do young adults from welfare-recipient families during childhood have different depression outcomes?
Does the relationship of depression and welfare participation differ by household income level?
Does the relationship of depression and welfare participation differ by young adults’ gender?
2. Method
2.1. Data and sample
This study used survey data from the National Longitudinal Study of Adolescent to Adult Health (Add Health). Add Health is a longitudinal survey of a nationally representative cohort of students in Grades 7 to 12. Beginning in the 1994–95 academic year, participants have been followed into young adulthood (ages 24–34 years at Wave IV) with four waves of in-home interviews (Wave I, 1995; N = 20,745; Wave IV, 2008–09, N = 15,701). The Add Health study details participants’ social, economic, psychological and physical from childhood to adulthood well-being as well as other health-related measures (See Harris, 2013, for detailed information on the Add Health survey design).
The study sample for this paper consisted of 15,701 respondents with complete data for the Wave I and IV Add Health surveys. In addition, study data included the respondents’ family background and parental information to allow for the examination of the relationship between welfare participation as a child and depression as a young adult. Considering the large amount of missing data for certain variables included in the analytic model (see Table 1), this study used multiple imputation to handle the missing data.
Table 1.
Missingness of variables.
| Variables | Before Multiple Imputation | After Multiple Imputation (N = 15,701)1 | |||||
|---|---|---|---|---|---|---|---|
| n | # Missing | % Missing | M | SD | M | SE | |
| Dependent Variables (Wave IV) | |||||||
| Diagnosed depression | 15,698 | 3 | 0.02 | 0.10 | 0.30 | 0.10 | 0.00 |
| Depression scores | 15,701 | 0 | 0 | 5.29 | 4.13 | 5.29 | 0.03 |
| Independent variable | |||||||
| Childhood welfare receipt | 15,533 | 168 | 1.07 | 0.19 | 0.40 | 0.20 | 0.00 |
| Covariates (Wave I) | |||||||
| Young adult level | |||||||
| Gender (male = 1) | 15,701 | 0 | 0 | 0.47 | 0.50 | 0.47 | 0.00 |
| Age | 15,701 | 0 | 0 | 15.10 | 1.75 | 15.10 | 0.01 |
| Race | 15,688 | 13 | 0.08 | 3.54 | 1.65 | 3.54 | 0.01 |
| General health | 15,689 | 12 | 0.08 | 2.12 | 0.91 | 2.12 | 0.01 |
| Parental level | |||||||
| Health status | 13,560 | 2,141 | 13.64 | 1.17 | 0.45 | 1.18 | 0.00 |
| Education level | 13,497 | 2,204 | 14.04 | 5.48 | 2.37 | 5.46 | 0.02 |
| Employment status | 13,332 | 2,369 | 15.09 | 3.11 | 1.21 | 3.11 | 0.01 |
| Health insurance type | 13,480 | 2,221 | 14.15 | 2.60 | 1.12 | 2.61 | 0.01 |
| Household level | |||||||
| Family structure | 15,701 | 0 | 0 | 2.05 | 1.07 | 2.05 | 0.01 |
| Household income | 11917 | 3,784 | 24.1 | 46.39 | 50.47 | 45.63 | 0.51 |
| Household size | 15,673 | 28 | 0.18 | 3.63 | 1.65 | 3.63 | 0.01 |
| Neighborhood safety | 15,626 | 75 | 0.48 | 0.89 | 0.31 | 0.89 | 0.00 |
| Survey weight | 14,800 | 901 | 5.74 | 1484 | 1435 | 1483 | 12 |
Note.
The M(mean) and SE(standard error) for each variable were aggregated based on the 20 imputed files.
2.2. Measures
Dependent variables
The dependent variables were defined as two dimensions of depression among young adults in Wave IV: Self-report depression scores and diagnosed depression.
Self-report depression scores
Self-reports of depression were measured at Wave IV using the Center for Epidemiologic Studies-Depression Scale (CES-D; Radloff, 1977). The CES-D scale is composed of 20 items that ask respondents to rate the extent to which they agree with statements describing behavior in the past week. The Add Health survey contained 18 of 20 CES-D items for Wave I and Wave II, and included nine items for Wave III and Wave IV. Responses to the items were captured using a 4-point (0–3), with higher scores indicating greater agreement with the statement. Responses for the nine items included in the Wave III and Wave IV surveys were summed, with higher values indicating a greater severity of depression. The CES-D has concurrent validity with other self-report depression scales (Radloff, 1977). The CES-D also has acceptable internal consistency based on Add Health Wave IV data, with an overall Cronbach’s alpha of 0.81.
Diagnosed depression
The variable indicating the respondent had received a clinical diagnosis of depression from a doctor, nurse, or other health care provider after the age of 18 was a dichotomous variable (yes = 1, otherwise = 0).
Variable of interest
Childhood welfare participation was measured by asking participants, “Before you were 18 years old, did anyone in your household ever receive public assistance, welfare payments, or Food Stamps?” Responses to the questions were based on data from Wave III; for participants missing Wave III data (18%), responses were based on the same question from Wave IV data. About 20% of participants reported that their family that received some form of public assistance.
Covariates
This study controlled for demographic and socioeconomic variables at the young adult, parental, and household levels. At the young adult level from Wave I, control variables included gender (1 = female; 0 = male), age (continuous variable), and race/ethnicity. Race/ethnicity was recoded as three dummy variables (reference group = White): Black, Hispanic, Others (e.g., Asian, Native American and mixed). Childhood general health status at Wave I was also controlled by asking participants to rate their general health. Responses were recoded as a dummy variable (1 = excellent/very good/good; 0 = fair/poor).
At the parental level (usually the resident mother), the analysis controlled for parental health status, education levels, employment status and health insurance type using Wave I data. Parental health status was recoded as two dummy variables: fair and poor (reference group = good). Parental education was measured by the highest education level for either of the parents using nine categories that ranged from Grade 8 or less (coded as 1) to professional training beyond a 4-year college or university degree (coded as 9). Employment status was coded as three dummy variables (reference group = full-time employed): unemployed and not looking for a job; unemployed and looking for a job, and part-time employed. Health insurance type was coded as four dummy variables (reference group = uninsured): Medicare or Medicaid, private insurance (e.g., Blue Cross/Blue Shield or Cigna), prepaid health plan (e.g., a health maintenance organization [HMO]), other insurance types.
At the household level, this study controlled for family structure, which was measured as three dummy variables (reference group = two biological parents): two parents but only one biological parent; single parent; and other (e.g., foster parents). Household income was measured by asking parents to report the total before-tax income all persons in the family received in 1994, including income from welfare benefits, dividends, and all other sources (range: $0 to $999,000). Household size (number of persons living in the household), and self-perceived safety in their neighborhood (1/0) from Wave I were also controlled in the analytic models.
2.3. Analytic strategies: a four-fold analysis strategy
Missing data analysis
Because some of the variables had more than 5% missing values (see Table 1), multiple imputation was used to estimate those values for each variable using Stata 13.0 (i.e., estimates computed using “mi” syntax to impute missing values by chained equations). We included the dependent variable in the imputation process (Allison, 2001). Twenty imputed files were generated for further analysis.
Propensity score greedy matching
Because this study used secondary data, the two groups (i.e., those with and those without childhood welfare participation) were not composed of randomly assigned participants. Therefore, the analysis used propensity score matching (PSM) methods to reduce possible selection bias; specifically, the analysis used propensity score greedy matching with the nearest neighbor within caliper. For each “treated” subject (in this case, a welfare recipient), a “control” subject with the closest propensity score within a predetermined common-support region (also called caliper) was selected (Guo et al., 2006; Guo and Fraser, 2015). Following Rosenbaum and Rubin (1985) suggestion, 0.01 was used as the caliper.
A three-step PSM process was used following the approach recommended by Guo and Fraser (2015). In Step 1, logistic regression based on all the co-variates was used to estimate separate propensity scores for each participant indicating the propensity of having been a welfare-recipient during childhood. Step 2 used the estimated propensity score obtained for each participant to determine whether the scores had a common-support region, which would permit one-to-one nearest-neighbor matching and the use of 0.01, as the matching caliper. In Step 3, ordinary least squares (OLS) regression was used with the matched sample to examine the relationship between welfare participation and depression scores. Logistic regression was used for the diagnosed depression outcome variable.
PSM was performed on each imputed file. Following the PSM procedures, post-matching analyses (i.e., OLS regression for depression score and logistic regression for diagnosed depression) were conducted based on the aggregation of matched samples of the 20 imputed files. In addition, the results of the analyses of three data sets are reported to allow comparison of differences across the three data sets: (a) the original data, with no imputation and no PSM; (b) the imputed data, but no PSM; and (c) the imputed data plus propensity score greedy matching.
Propensity score radius matching
Given that the greedy matching process had already reduced the sample size, radius matching was conducted because this method can help retain as many as cases as possible in the analyses. To run radius matching, all the controls with propensity scores within the 0.01 radius were included in the final model. Stata generated a “weight” for each control case. Because Add Health data have survey weights, and using propensity score radius matching also produces weights, this study followed Ridgeway and colleagues’ recommendation to use sampling weights in the estimation of propensity scores and then to use sampling weights multiplied by propensity weights in the outcome regression models (Ridgeway et al., 2015).
Finally, this study used a four-fold analysis strategy to triangulate the results by presenting the regression results based on four permutations of data: (a) the raw data, (b) the imputed data, (c) the imputed data with greedy matching, and (d) the imputed data with radius matching. Because the greedy matching model yielded the closest propensity scores between welfare and non-welfare recipients, we tend to favor the results from greedy matching, and we consider the other three approaches as robustness tests of the greedy matching results.
Subgroup analyses
To answer Research Questions 2 and 3 (i.e., whether the relationship between welfare receipt and depression differs by household income levels or by respondents’ gender), the whole sample was divided into five subsamples, with three subsamples based on Wave I household income levels and two subsamples based on gender. The income levels were defined using 1994 data and the 1994 federal poverty threshold (FPT):
poor, total household annual income less than 100% FPT (n = 1,670; 14%);
near poor, household income between 100% and 200% FPT (n = 2,634; 22%); and
non-poor, household income above 200% FPT; (n = 7,932; 65%);
In addition, the sample was divided into two gender groups: males (n = 8,352, 53%) and females (n = 7,349, 47%). Then, the same multiple imputation, PSM, and post-matching analyses were conducted separately on these five subgroups.
3. Results
Table 2 shows the aggregated descriptive statistics for all variables of 20 imputed data files. On average, participants had an average self-reported depression score of 5.29 (out of 27), and about 10% of young adults had received a clinical diagnosis of depression after the age 18 years. About one fifth (20%) of the sample had received some form of welfare benefits during childhood (i.e., before age 18 years). The sample had slightly more females (54%) than males. At Wave I (1994), the average age of participants was 15 years old. About half of the participants identified as White (53%), 22% identified as Black, 16% identified as Hispanic, 6% identified as American Indians or as other race, and 3% identified as Asian. The majority of the participants (93%) reported their general health as excellent, very good or good.
Table 2.
Weighted descriptive statistics1.
| Measures | M | 95% CI | |
|---|---|---|---|
| Dependent Variables | |||
| Depression score | Sum of CES-D 9-item | 5.29 | [5.23, 5.36] |
| Diagnosed depression | 1 = yes; 0 = no | 0.10 | [0.10, 0.11] |
| Variable of interest | |||
| Childhood welfare participation | 1 = yes; 0 = no | 0.20 | [0.19, 0.20] |
| Covariates | |||
| Individual Level | |||
| Male | 1 = yes; 0 = no | 0.47 | [0.46, 0.48] |
| Age | year | 15.10 | [15.08, 16.13] |
| Race | |||
| White | 1 = yes; 0 = no | 0.53 | [0.52, 0.54] |
| Black | 1 = yes; 0 = no | 0.22 | [0.22, 0.23] |
| Hispanic | 1 = yes; 0 = no | 0.16 | [0.15, 0.17] |
| Other | 1 = yes; 0 = no | 0.09 | [0.08, 0.09] |
| Good general health | (1 = Excellent/very good/good; 0 = Fair/poor) | 0.93 | [0.92, 0.93] |
| Parental Level | |||
| Health status | |||
| Good | 1 = yes; 0 = no | 0.85 | [0.85, 0.86] |
| Fair | 1 = yes; 0 = no | 0.11 | [0.11, 0.12] |
| Poor | 1 = yes; 0 = no | 0.03 | [0.03, 0.03] |
| Parental education leve | Range: Grade 8 or less (=1) to Professional training beyond 4-year college/university (= 9) | 5.46 | [5.42, 5.51] |
| Employment status | |||
| Not working not looking for a job | 1 = yes; 0 = no | 0.21 | [0.20, 0.22] |
| Not working, looking for a job | 1 = yes; 0 = no | 0.06 | [0.05, 0.06] |
| Employed part time | 1 = yes; 0 = no | 0.15 | [0.14, 0.15] |
| Employed full-time | 1 = yes; 0 = no | 0.58 | [0.58, 0.59] |
| Health insurance type | |||
| Medicare or Medicaid | 1 = yes; 0 = no | 0.10 | [0.10, 0.11] |
| Individual or group private coverage | 1 = yes; 0 = no | 0.48 | [0.48, 0.49] |
| Prepaid health plan | 1 = yes; 0 = no | 0.25 | [0.24, 0.25] |
| Others | 1 = yes; 0 = no | 0.05 | [0.04, 0.05] |
| None insurance | 1 = yes; 0 = no | 0.13 | [0.12, 0.13] |
| Household Level | |||
| Family structure | |||
| Single parent | 1 = yes; 0 = no | 0.29 | [0.29, 0.30] |
| Two parents one biological | 1 = yes; 0 = no | 0.11 | [0.10, 0.11] |
| Two biological parents | 1 = yes; 0 = no | 0.52 | [0.51, 0.52] |
| Other | 1 = yes; 0 = no | 0.08 | [0.08, 0.09] |
| Household size | Number of people | 3.63 | [3.60, 3.65] |
| Household income | Total 1994 household income before taxes (by thousands) | 45.63 | [44.61, 46.65] |
| Neighborhood safety | 1 = yes; 0 = no | 0.89 | [0.88, 0.89] |
Note.
Based on the aggregation of 20 imputed files; M = mean; CI= Confident Interval.
In terms of parental and household characteristics at Wave I, the average educational level fell between the post-high school completed vocational/technical training and some college. More than half (58%) of the parents were employed full time, 15% were employed part time, 21% were unemployed and not looking for work, and 6% were unemployed and looking for a job. The majority of parents identified their health status as good (85%). About 10% of parents used Medicare or Medicaid as their health insurance, about half (48%) had private insurance, about one-quarter of parents used a prepaid health plan, and 13% of parents did not have health insurance at Wave I. More than half (52%) of the youth participants lived in a household with two biological parents at Wave I. The average household size at Wave I was 3.63 persons. Only 11% of young adults felt unsafe in their neighborhoods.
3.1. Testing the relationship between childhood welfare receipt and young adult depression
This study used four different approaches to test the relationship between childhood welfare participation and young adult depression: (a) using the original data with missing values; (b) using imputed data; (c) using data based on multiple imputation and greedy matching; and (d) using data based on multiple imputation and radius matching. The first column in Table 3 shows results from list-wise deletion of missing data in the original dataset (n = 12,004), and controlling for all other variables. Shown in Table 3, column a, as compared with non-welfare recipient counterparts, young adults whose families received welfare during their childhood (before age 18 years) had significantly higher depression scores by 0.594 (p < .01). In addition, as compared with young adults from non-welfare recipient families, young adults with welfare benefits had higher probability of being diagnosed with depression by 21.9%, yet it was not statistically significant at the 95% level.
Table 3.
Regression results using different datasets.
| (a) Not Imputed | (b) Imputed | (c)Imputed with greedy matching | (d) Imputed with radius matching | |
|---|---|---|---|---|
| Depression Score (β) | 0.594**[.25 – .94] | 0.474** [.19 – .77] | 0.450* [.05, .85] | 0.486** [.14, .84] |
| Observations | 12,004 | 15,701 | 5,200 | 14,541 |
| Diagnosed Depression (OR) | 1.219 [1.00–1.66] | 1.257* [1.04–1.51] | 1.232 [.95, 1.60] | 1.326** [1.08, 1.63] |
| Observations | 12,004 | 15,701 | 5,200 | 14,541 |
Note. Regressions controlled for all covariates listed in Table 2; 95% confidence intervals are shown in brackets; Number of imputed files = 20.
p < .001
p < .01
p < .05, two-tailed.
However, slightly different estimates were obtained with the imputed data files (m = 20; and each file has 15,701 observations; See Table 3 column b). When using the imputed data files for the depression score, the magnitude of regression coefficient was reduced to 0.474, whereas the significance level remained at the 99% level, which was the same as the original data. For diagnosed depression, the magnitude of the odds ratio increased to 25.7% and was statistically significant at the 95% level.
Using imputed data with propensity score greedy matching reduced the sample size to 5,200 (See Table 3 column c). When controlling for all the covariates, results showed young adults from welfare recipient families reported significantly higher depression scores than non-welfare recipients (higher by 0.450; p < .05). In addition, young adults from welfare recipient families had a 23.2% higher probability than their non-welfare counterparts of being diagnosed with depression after age 18 years; however, this value was not statistically significant at the 95% level.
When using imputed data with propensity score radius matching, the larger sample size (n = 14,541; See Table 3 column d) yielded an increased probability of a significant association between childhood welfare participation and both young adulthood depression scores (by 0.486, p < .01) and rates of diagnosed depression (by 32.6%, p < .01).
3.2. Testing the Welfare–Depression relationship by household income levels
To obtain a better understanding of the relationship between childhood welfare participation and young adult depression, this study also tested whether the relationships differed by household income levels and by respondents’ gender. Table 4 presents the results of subgroup analyses using imputed data with greedy matching, and shows the subgroup results by household income level (i.e., non-poor, near poor, and poor groups) and by gender (i.e., male and female subsample). Overall, young adults from welfare-recipient families had significantly higher depression scores. However, the subgroup analyses showed a statistically significant higher depression score (0.934; p < .05) only among the subsample of young adults from poor households (household annual income < 100% FPT in 1994) that received welfare during their childhood.
Table 4.
Regression results based on imputed data with propensity score greedy matching.
| (A) Full sample | (B) By income level (Wave I) | (C) By gender (full sample) | ||||
|---|---|---|---|---|---|---|
| > 200% FPT (Non-poor) | 100–200% FPT (Near Poor) | < 100% FPT (Poor) | Female | Male | ||
| Depression Score (β) | 0.450* [.05, .85] | 0.381 [−.29, 1.05] | 0.287 [−.41, .98] | 0.934* [.06, 1.81] | 0.494 [−.09, 1.06] | 0.442 [−.08, .96] |
| Diagnosed Depression (OR) | 1.232 [.95, 1.60] | 1.094 [.70, 1.72] | 1.889* [1.07, 3.35] | 1.269 [.77, 2.10] | 1.342 [.96, 1.87] | 1.181 [.68, 2.04] |
| Observations | 5,200 | 1,968 | 1,446 | 1,418 | 2,792 | 2,238 |
Note. FPT = federal poverty threshold; Regression analyses controlled for all covariates listed in Table 2; 95% confidence intervals are shown in brackets
p < .001
p < .01
p < .05, two-tailed.
Overall, the results showed no statistically significant group differences on the diagnosed depression outcome. However, a statistically significant higher probability (89%; p < .01) of being diagnosed with depression was found among the near-poor group from welfare-recipient families. Interestingly, young adults from welfare-recipient families had higher depression scores, but this difference was significant only among the poor household subsample, and was not significant for the near-poor subsample. Young adults from welfare-recipient families had higher probability of being diagnosed with depression, but this difference was statistically significant only among the near-poor families group and not the poor families group (See Table 4, Column B). Results based on imputed data with propensity score radius matching yielded similar trends as found using greedy matching (See Table 5, Column B).
Table 5.
Regression results based on imputed data with propensity score radius matching.
| (A) Full sample | (B) By income level (Wave I) | (C) By gender (full sample) | ||||
|---|---|---|---|---|---|---|
| >200% FPT (Non-poor) | 100–200% FPT (Near Poor) | <100% FPT (Poor) | Female | Male | ||
| Depression Score (β) | 0.486** [.14, .84] | 0.351 [−.15, .85] | 0.291 [−.36, .94] | 0.865* [.16, 1.57] | 0.489* [.00, .98] | 0.454 [−.02, .93] |
| Diagnosed Depression (OR) | 1.326** [1.08, 1.63] | 1.006 [.68, 1.48] | 1.935** [1.24, 3.03] | 1.339 [.84, 2.15] | 1.381* [1.05, 1.81] | 1.150 [.68, 1.94] |
| Observations | 14,541 | 9,661 | 2,921 | 2,175 | 7,512 | 6,588 |
Note. FPT = federal poverty threshold; Regression analyses controlled for all covariates listed in Table 2. 95% confidence intervals are shown in brackets
p < .001
p < .01
p < .05, two-tailed.
3.3. Testing the Welfare–Depression relationship by gender groups
In terms of gender differences on the relationship between welfare participation in childhood and depression in young adulthood, results from propensity score greedy matching (see Table 4, Column C) showed that, for both female and male subgroups, as compared with young adults from non-welfare recipient families, these who came from welfare-recipient families had higher depression scores and an associated higher probability of being diagnosed with depression, however, these values were not statistically significant at the 95% level.
Results from propensity score radius matching (see Table 5, Column C) showed similar trends for the gender differences, with the exception of female welfare recipients had statistically significant higher depression scores (0.489; p < .05) and a 38.1% higher probability of being diagnosed with depression (p < .05). Given (c) approach yield the closest propensity scores between the welfare and non-welfare recipients, we suggest results based on the imputed data and greedy matching as our main findings, and the other three approaches are robustness tests.
4. Discussion
The four-fold results suggest that young adults whose childhoods included living in families that participated in welfare programs had significantly higher depression scores across the four analytical samples, as compared with young adults whose families did not receive any form of public assistance. In addition, some findings suggest that young adults from welfare-recipient families had a higher chance of depression diagnosis, although the significance level varied based on imputation and the matching technique used. Non-significant (p > .1) relationships were found based on OLS regression with raw data (n = 12,004), and on imputed data with greedy matching (n = 5,200), whereas a statistically significant (p < .05) relationship was observed based on radius matching (n = 14,541) with imputation and OLS with imputation (n = 15,701). Therefore, using different sample sizes (based on the analytic method used) produced differences in statistical significance values based on the level of estimations. As noted, when greedy matching was used, the sample size was substantially smaller, and the results of the greedy matching analysis did not reach statistical significance. In contrast, when radius matching was used, which preserved a larger sample, the analysis produced significant outcomes. This difference in significance may be related to power and serves as a cautionary note, especially for those working with large datasets. In general, caution is warranted when drawing conclusions based on large datasets because large sample sizes have an inherent risk of producing significant results for trivially small differences.
Further, diagnosis is a considerably higher standard than a self-reported depression score because receiving a diagnosis depends on accessing care, specifically specialty mental health care. Therefore, we can be confident that there is important finding related to the experience of depression and welfare participation, even though the findings on receiving a formal diagnosis are mixed.
Subgroup analyses suggest that the welfare-depression relationships differed by household income level. Specifically, higher depression scores occur principally among the group of young adults raised in poor welfare-recipient families. No statistically significant group differences were found when the whole sample was considered, whereas the subgroup analyses indicated only the near-poor group had a statistically significant higher probability of being diagnosed with depression. Yet for females in welfare participant families, self-report and diagnosis appeared to go together, perhaps because young women in the target age group are seeing and have access to health care providers for regular reproductive health care, such as family planning. In addition, when using propensity score radius matching, a significant gender difference was observed (See Table 5, column C), indicating that females who came from welfare-recipient families had both significant higher depression scores and a higher probability of being diagnosed with depression. Consistent with previous studies on the subject (e.g., Dooley and Prause, 2002; Kalil et al., 2001; Knab et al., 2006; Pande, 2014), this study found that females from welfare families reported higher incidences of depression compared to non-recipient females. Although low income young women appear to be receiving diagnoses of depression, the current analysis does not describe whether or not they are receiving adequate treatment. If these young women are being diagnosed because they are in regular contact with family planning providers, integrating mental health care into primary care settings would allow these diagnosed young women to receive multi-faceted care including medication management and evidence-based psychotherapy approaches.
The subgroup analyses of this study offer rich opportunities for further investigation of the between-group differences among the three income level groups and the two gender groups. The subgroup analyses yielded very interesting findings regarding the association of welfare receipt during childhood and young adult depression relative to household income and participant gender. The nuanced understanding afforded by the subgroup analyses would have been lost if the study design had not included splitting the sample into subgroups. Such findings have important implications for policy makers. To make best use of limited resources, policy makers must ensure that anti-poverty policies target the correct segment of the population for the desired outcome.
This study also has implications for future research that might use welfare participation as a “marker” in subgroup analyses. The results of this study demonstrate the utility of using welfare participation as a marker in subgroup analyses to identify a target population for future interventions. Young adults who grow up in a household with income under 200% FPT, or females from welfare-recipient families appear to be more vulnerable for depression. Therefore, when developing anti-poverty policies or interventions, these subgroups warrant greater attention.
The subgroup analyses produced conflicting findings on two outcomes, one related to the poor group (significant on depression scores rather than diagnosed depression) and one related to the near-poor group (significant on diagnosed depression rather than depression scores). Possible explanations draw on the SDH perspective. The seeming conundrum of higher depression scores and lower rates of depression diagnoses within the poor group may reflect differential access. That is, although young adults in the poor group were experiencing depression, they did not have access to clinics or could not afford depression screening and diagnostic services. Health policies and reforms, especially in the area of behavioral health, must focus on improving access to mental health screening and treatment for welfare recipients. Coverage for mental health screening and treatment through Medicaid and the integration of physical and behavioral health services have the potential to improve health outcomes. Current Medicaid policy limits mental health services, including treatment of depression.
The current study contributes to the literature on the impact of welfare participation on young adult depression, and it supports the wider determinates of health model and the SDH framework currently used in the Healthy People 2020 roadmap (Koh, 2010). Our analysis advances this framework by considering more about what types of social determinants are important for whom. Our analysis suggests that young men are left out when it comes to the diagnosis and treatment of depression. Young women in similar circumstances appear more likely to be diagnosed. This suggests new avenues to diagnosis and treatment are needed for young men.
Poverty has long been identified as a social determinant of health. This study contributes to the literature by examining the longitudinal risk associated with childhood welfare participation. This contributes to a growing empirical and theoretical rationale for strengthening prevention programs within the income-support programs of the United States.
The study has several limitations. First, the Add Health dataset lacks information on participation in specific welfare programs. Without this information, it is impossible to know if one form of public assistance has a stronger relationship with mental health outcomes of welfare recipients; thus, the study findings have limited policy implications for specific welfare programs. Given this limitation, the findings of this study should be considered as suggested relationships that have implications at only the general welfare policy level. Second, this study has potential threat to internal validity because the comparison groups of welfare participants were not randomly assigned, and this study uses a PSM approach to reduce the selection bias. However, PSM mimics the randomization process only based on the selected control variables and can be biased by missing indicators that may affect the welfare-depression relationship. Last, although propensity score analysis controls selection bias for the effects of household welfare participation based on the observed variables, this analytic approach is vulnerable to unobserved heterogeneity.
Despite the limitations, this study has several strengths that contribute to the literature on the long-term impact of welfare policies on individual mental health, using the indicator of depression experienced in young adulthood, and focusing on vulnerable populations, using the indicator of welfare participation during childhood. First, using the Add Health nationally representative longitudinal dataset allows broad generalization of the findings as well as the exploration of the long-term effects of welfare participation. Second, this study used Multiple Imputation to mitigate against the potential risk of increasing Type I errors posed by the reduction in sample size due to missing data. Third, this study used two propensity score matching methods (greedy and radius matching) to reduce sample selection bias, yielding more robust results. The paper presents a comparison of four estimation approaches using (a) raw data; (b) imputed data; (c) imputed data with greedy matching; and (d) imputed data with radius matching, which showed more nuanced results based on the different sample size. Last, this study included a subgroup analysis, which allows further exploration of whether the relationship between childhood welfare participation and young adult depression differs by income levels and gender.
Our findings reinforce the importance of considering the SDH framework when providing healthcare to impoverished families and children. When young adults are seen by their primary care providers, physicians and others should focus on all aspects of health and consider integrative approaches to providing mental health care. Perhaps policy makers will use the SDH framework to understand that risks to well-being are deeply inter-related as suggested by the SDH framework. Poverty alleviation must be about more than income support. By examining relationships between welfare participation and health outcomes, our work moves this conversation forward and calls on policy makers to look broadly at the needs of low income children and families.
Acknowledgement
This research uses data from Add Health, a program project directed by Kathleen Mullan Harris and designed by J. Richard Udry, Peter S. Bearman, and Kathleen Mullan Harris at the University of North Carolina at Chapel Hill, and funded by Grant P01-HD31921 from the Eunice Kennedy Shriver National Institute of Child Health and Human Development, with cooperative funding from 23 other federal agencies and foundations. Information on how to obtain Add Health data is available on the Add Health website (http://www.cpc.unc.edu/addhealth). The authors particularly thank Kathleen Mullan Harris and Mark W. Fraser for assistance with the access of restricted data and original design. No direct support was received from Grant No. P01-HD31921for this analysis.
Footnotes
Appendix A. Supplementary data
Supplementary data related to this article can be found at https://doi.org/10.1016/j.ssresearch.2018.08.009.
References
- Allison PD, 2001. Missing Data. Sage, Thousand Oaks, CA. [Google Scholar]
- American Psychiatric Association, 1994. Diagnostic and Statistical Manual of Mental Disorders, fourth ed. Author, Washington, DC. [Google Scholar]
- Aneshensel CS, Sucoff CA, 1996. The neighborhood context of adolescent mental health. J. Health Soc. Behav. 293–310. 10.2307/2137258. [DOI] [PubMed] [Google Scholar]
- Bambra C, Gibson M, Amanda S, Wright K, Whitehead M, Petticrew M, 2010. Tackling the wider social determinants of health and health inequalities: evidence from systematic reviews. J. Epidemiol. Community Health 64, 284–291. 10.1136/jech.2008.082743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Belle D, 1990. Poverty and women’s mental health. Am. Psychol 45, 385–389. 10.1037/0003-066X.45.3.385. [DOI] [Google Scholar]
- Besley T, Coate S, 1992. Workfare versus welfare: incentive arguments for work requirements in poverty-alleviation programs. Am. Econ. Rev 82, 249–261. [Google Scholar]
- Brown J, Hanlon P, Turok I, Webster D, Arnott J, Macdonald EB, 2009. Mental health as a reason for claiming incapacity benefit. A comparison of national and local trends. J. Public Health 31, 74–80. 10.1093/pubmed/fdn098. [DOI] [PubMed] [Google Scholar]
- Casey P, Goolsby S, Berkowitz C, Frank D, Cook J, Cutts D, et al. , 2004. Maternal depression, changing public assistance, food security, and child health status. Pediatrics 113, 298–304. 10.1542/peds.113.2.298. [DOI] [PubMed] [Google Scholar]
- CBHSQ, 2016. Key Substance Use and Mental Health Indicators in the United States: Results from the 2015 National Survey on Drug Use and Health (HHS Publication No. SMA 16–4984, NSDUH Series H-51). Retrieved from. https://www.samhsa.gov/data/sites/default/files/NSDUH-FFR1-2015/NSDUH-FFR1-2015/NSDUH-FFR1-2015.pdf.
- Coiro MJ, 2001. Depressive symptoms among women receiving welfare. Women Health 32 (1–2), 1–23. 10.1300/J013v32n01_01. [DOI] [PubMed] [Google Scholar]
- Coleman-Jensen A, Gregory C, Singh A, 2014. Household Food Security in the United States in 2013 (USDA-ERS Economic Research Report Number 173). Retrieved from. https://papers.ssrn.com/sol3/papers.cfm?abstract_id=2504067.
- Dahlgren G, Whitehead M, 1991. Policies and Strategies to Promote Social Equity in Health. Institute for Future Studies, Stockholm, Sweden. [Google Scholar]
- Dooley D, Prause J, 2002. Mental health and welfare transitions: depression and alcohol abuse in AFDC women. Am. J. Community Psychol 30, 787–813. 10.1023/A:1020253002468. [DOI] [PubMed] [Google Scholar]
- Elovainio M, Pulkki-Raback L, Hakulinen C, Ferrie JE, Jokela M, Hintsanen M, et al. , 2015. Childhood and adolesence risk factors and development of depressive symptoms: the 32-year prospective young Finns follow-up study. J. Epidemiol. Community Health 69, 1109–1117. 10.1136/jech-. [DOI] [PubMed] [Google Scholar]
- Evans R, Barer M, Marmor T (Eds.), 2017. Why Are Some People Healthy and Others Not? the Determinants of Health Populations. Routledge, New York, NY. [Google Scholar]
- FamiliesUSA, 2018. A 50-state Look at Medicaid Expansion: 2017. Retrieved from. http://familiesusa.org/product/50-state-look-medicaid-expansion. [Google Scholar]
- Garg A, Toy S, Tripodis Y, Silverstein M, Freeman E, 2015. Addressing social determinants of health at well child care visits: a cluster RCT. Pediatrics 135 (2), e296–e304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gilman SE, Kawachi I, Fitzmaurice GM, Buka SL, 2002. Socioeconomic status in childhood and the lifetime risk of major depression. Int. J. Epidemiol 31, 359–367. 10.1093/intjepid/31.2.359. [DOI] [PubMed] [Google Scholar]
- Guo S, Fraser M, 2015. Propensity Score Analyses: Statistical Methods and Applications, second ed. Sage, Thousand Oaks. CA. [Google Scholar]
- Guo S, Barth RP, Gibbons C, 2006. Propensity score matching strategies for evaluating substance abuse services for child welfare clients. Child. Youth Serv. Rev 28, 357–383. 10.1016/j.childyouth. [DOI] [Google Scholar]
- Harris KM, 2013. The Add Health Study: Design and Accomplishments. Chapel Hill: Carolina Population Center, University of North Carolina; Retrieved from. http://www.cpc.unc.edu/projects/addhealth/documentation/guides/DesignPaperWIIV.pdf. [Google Scholar]
- Heflin CM, Acevedo SK, 2011. Non-income effects of welfare receipt on early childhood cognitive scores. Child. Youth Serv. Rev. 33, 634–643. 10.1016/j.childyouth.2010.11.006. [DOI] [Google Scholar]
- Hudson CG, 2005. Socioeconomic status and mental illness: tests of the social causation and selection hypotheses. Am. J. Orthopsychiatry 75, 3–18. 10.1037/0002-9432.75.1.3. [DOI] [PubMed] [Google Scholar]
- Jackson PB, Williams DR, 2006. The intersection of race, gender, and SES: health paradoxes In: Shulz A, Mullings L (Eds.), Gender, Race, Class and Health. Jossey-Bass, San Francisco, CA. [Google Scholar]
- Jiang Y, Ekono MM, Skinner C, 2016. Basic Facts about Low-income Children: Children under 18 Years, 2014 National Center for Children in Poverty, Mailman School of Public Health, Columbia University, New York, NY. [Google Scholar]
- Kalil A, Born CE, Kunz J, Caudill PJ, 2001. Life stressors, social support, and depressive symptoms among first-time welfare recipients. Am. J. Community Psychol 29, 355–369. 10.1023/A:1010351302196. [DOI] [PubMed] [Google Scholar]
- Knab JMT, Garfinkel I, McLanahan SS, 2006. The Effects of Welfare and Child Support Policies on Maternal Health (Working Paper #2006–04-FF). Center for Research on Child Wellbeing. Princeton University; Retrieved from. http://crcw.princeton.edu/workingpapers/WP06-04-FF.pdf. [Google Scholar]
- Koh HK, 2010. A 2020 vision for healthy people. N. Engl. J. Med 362 (18), 1653–1656. 10.1056/NEJMp1001601. [DOI] [PubMed] [Google Scholar]
- Marmot M, Friel S, Bell R, Houweling TA, Taylor S, Commission on Social Determinants of Health, 2008. Closing the gap in a generation: health equity through action on the social determinants of health. Lancet 372, 1661–1669. 10.1016/S0140-6736(08)61690-6. [DOI] [PubMed] [Google Scholar]
- Marshall TH, 1950. Citizenship and Social Class: and Other Essays. Cambridge University Press, London, UK: Retrieved from. http://www.jura.uni-bielefeld.de/lehrstuehle/davy/wustldata/1950_Marshall_Citzenship_and_Social_Class_OCR.pdf. [Google Scholar]
- Maynard R, Boehnen E, Corbett T, Sandefur G, Mosley J, 1998. Changing family formation behavior through welfare reform In: Moffitt RA (Ed.), Welfare, the Family, and Reproductive Behavior: Research Perspectives. National Academies Press, Washington, DC, pp. 134–176. 10.17226/6133. [DOI] [Google Scholar]
- McBride Murry V, Berkel C, Gaylord-Harden NK, Copeland-Linder N, Nation M, 2011. Neighborhood poverty and adolescent development. J. Res. Adolesc 21, 114–128. 10.1111/j.1532-7795.2010.00718.x. [DOI] [Google Scholar]
- Moffitt RA, 2015. The deserving poor, the family, and the US welfare system. Demography 52, 729–749. 10.1007/s13524-015-0395-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Organisation for Economic Co-operation and Development, 2017. Poverty Rate. 10.1787/0fe1315d-en. [DOI]
- Pande N, 2014. Impact of Mothers’ Welfare Program on Child Outcomes. Retrieved from the Social Science Research Network (SSRN) website at: https://papers.ssrn.com/sol3/papers.cfm?abstract_id=2283828. [Google Scholar]
- Personal Responsibility and Work Opportunity Reconciliation Act of 1996, Pub. L. No. 104–193 (1996).
- Radloff LS, 1977. The CES-D scale: a self-report depression scale for research in the general population. Appl. Psychol. Meas 1, 385–401. 10.1177/014662167700100306. [DOI] [Google Scholar]
- Ridgeway G, Kovalchik SA, Griffin BA, Kabeto MU, 2015. Propensity score analysis with survey weighted data. J. Causal Inference 3, 237–249. 10.1515/jci-2014-0039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosenbaum PR, Rubin DB, 1985. Constructing a control group using multivariate matched sampling methods that incorporate the propensity score. Am. Statistician 39 (1), 33–38. 10.1080/00031305.1985.10479383. [DOI] [Google Scholar]
- Shonkoff JP, Garner AS, Siegel BS, Dobbins MI, Earls MF, McGuinn L, et al. , 2012. The lifelong effects of early childhood adversity and toxic stress. Pediatrics 129 (1), e232–e246. [DOI] [PubMed] [Google Scholar]
- Smith LA, Wise PH, Chavkin W, Romero D, Zuckerman B, 2000. Implications of welfare reform for child health: emerging challenges for clinical practice and policy. Pediatrics 106, 1117–1125. 10.1542/peds.106.5.1117. [DOI] [PubMed] [Google Scholar]
- Social Security Act of 1935, vol. 42 U.S.C. ch. 7 (1935). [Google Scholar]
- Statistic Brain Research Institute, 2016. Welfare Statistics. Retrieved from. http://www.statisticbrain.com/welfare-statistics/.
- Stewart WF, Ricci JA, Chee E, Hahn SR, Morganstein D, 2003. Cost of lost productive work time among U.S. workers with depression. J. Am. Med. Assoc 289, 3135–3144. 10.1001/jama.289.23.3135. [DOI] [PubMed] [Google Scholar]
- U.S. Census Bureau, 2016. 21.3 Percent of U.S. Population Participates in Government Assistance Programs Each Month (CB15–97) [Press Release]. Retrieved from. https://www.census.gov/newsroom/press-releases/2015/cb15-97.html.
- U.S. Department of Health and Human Services, Office of Family Assistance, 2014. Characteristics and Financial Circumstances of TANF Recipients, Fiscal Year 2012. Retrieved from. http://www.acf.hhs.gov/programs/ofa/resource/characteristics-and-financial-circumstances-appendix-fy2012.
- United Nations International Children’s Emergency Fund, Innocenti Research Centre, 2012. Measuring Child poverty: New League Tables of Child Poverty in the World’s Rich Countries (Report Card 10). Author, Florence, Italy: Retrieved from. https://www.unicef-irc.org/publications/pdf/rc10_eng.pdf. [Google Scholar]
- United Nations International Children’s Emergency Fund, Office of Research, 2014. Children of the Recession: the Impact of the Economic Crisis on Child Well-being in Rich Countries (Report Card 12). Author, Florence, Italy: Retrieved from. https://www.unicef.org/publications/index_76438.html. [Google Scholar]
- Viner RM, Ozer EM, Denny S, Marmot M, Resnick M, Fatusi A, Currie C, 2012. Adolescence and the social determinants of health. Lancet 379, 1641–1652. 10.1016/S0140-6736(12)60149-4. [DOI] [PubMed] [Google Scholar]
- Wu S, Zerden de SL, Wu Q, 2016. The influence of childhood welfare participation on adulthood substance use: evidence from the National Longitudinal Study of Adolescent to Adult Health. Am. J. Drug Alcohol Abuse 42, 657–670,. 10.1080/00952990.2016.1176176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu S, Wang X, Wu Q, Harris KM, 2018. Household financial assets inequity and health disparities among young adults: evidence from the national longitudinal study of adolescent to adult health. J. Health Dispar. Res. Pract. 11, 122–135 Spring. [PMC free article] [PubMed] [Google Scholar]
- Zerden de SL, Wu S, Wu Q and Fraser MW, Welfare participation in childhood as a predictor of cigarette use in adulthood in the United States. J. Soc. Social Work Res. accepted. [DOI] [PMC free article] [PubMed] [Google Scholar]