Abstract
Urinary tract infections (UTIs) are among the most common microbial infections in humans and represent a substantial burden on the health care system. UTIs can be uncomplicated, as when affecting healthy individuals, or complicated, when affecting individuals with compromised urodynamics and/or host defenses, such as those with a urinary catheter. There are clear differences between uncomplicated UTI and catheter-associated UTI (CAUTI) in clinical manifestations, causative organisms, and pathophysiology. Therefore, uncomplicated UTI and CAUTI cannot be approached similarly, or the risk of complications and treatment failure may increase. It is imperative to understand the key aspects of each condition to develop successful treatment options and improve patient outcomes. Here, we will review the epidemiology, pathogen prevalence, differential mechanisms used by uropathogens, and treatment and prevention of uncomplicated UTI and CAUTI.
Keywords: CAUTI, prevalence, susceptibility, uncomplicated UTI, uropathogens
Urinary tract infections (UTIs), despite many efforts to manage them, still affect almost 11 million people in the United States1 and almost 150 million worldwide2 annually, placing UTIs among the most common microbial infections. UTIs cause serious sequelae, including frequent recurrences, pyelonephritis with sepsis, renal damage, and complications caused by constant or repetitive antimicrobial use, including multi-class antibiotic resistance and Clostridium difficile colitis.3 These consequences further emphasize the continued need to understand UTI pathophysiology and to develop new, efficient, and antibiotic-sparing therapies.
UTIs may be classified as uncomplicated or complicated.3 Uncomplicated UTIs, typically representing community-onset cystitis, are more frequent in outpatient settings4 and occur in otherwise healthy individuals without structural or neurologic abnormalities of the urinary tract. Uncomplicated UTIs occur predominantly in females of all ages but also in subsets of the male population (infant boys and older adult men).1,5 On the other hand, complicated UTIs are associated with patient-level factors that compromise urodynamics or host defenses, such as indwelling or intermittent urinary catheterization, urinary obstruction (e.g., by stones) or retention, immunosuppression, renal failure, renal transplantation, and pregnancy.6,7 Indwelling urinary catheterization is the most common risk factor for complicated UTI; such catheter-associated UTI (CAUTI) accounts for 40% of all nosocomial infections worldwide5,8 and often leads to secondary bloodstream infections.5,9–11 Though recognition of this risk has led to reductions in insertion or duration of use of indwelling urinary catheters, a sizable number of hospitalized patients still undergo urinary catheterization during their stay. In the United States, the 30 million Foley catheters used annually confer substantial risk for CAUTI.12–16
As there are notable differences in clinical manifestations, causative organisms, and pathologic mechanisms between uncomplicated UTI and CAUTI, it is critical to dissect key aspects of each one to better assess specific treatment options and reduce the risks of complications and treatment failure. Here we will review and contrast the epidemiology, pathogen prevalence, differential mechanisms used by uropathogens, and treatment and prevention during uncomplicated UTI and CAUTI.
Host Factors in Uncomplicated UTI and CAUTI
Uncomplicated UTI occurs significantly more often in women than in men1,3,17; a nationwide US outpatient study showed that 84% of patients suffering UTI were women,18 and an earlier administrative data study of more than 10 million US emergency department UTI patients showed identically that 84% were female.19 These and other studies indicate that the female-to-male ratio in UTI is between 5:1 and 8:1.18–20 It is estimated that 50% of women will experience at least one episode of UTI during their lifespan, and 25% of those women will experience recurrent UTIs (rUTIs).1,17 The majority of female UTIs manifest primarily in the lower urinary tract (community-onset cystitis); however, ascension of bacteria from the bladder can lead to kidney infection (pyelonephritis). Beyond female sex, other risk factors associated with cystitis include prior UTI, sexual activity, pregnancy, vaginal infection, diabetes, obesity, and genetic susceptibility.1,3,21
The higher incidence of community-onset UTI in women is historically attributed to anatomic factors that enable transit of uropathogenic bacteria from a gastrointestinal tract reservoir to the urinary tract. Specifically, women have a shorter distance from anus to urethral opening and shorter urethral length than men and a vaginal/perineal microenvironment that may facilitate colonization of the urethra (and thus an indwelling catheter) by uropathogens. Among men, UTI incidence is higher in the elderly (where prostatic hypertrophy impairs urodynamics and promotes urinary retention) and in infants (where UTI incidence under 6 months of age is higher in boys than in girls).22–25 In comparison, gender disparity in CAUTI is comparatively narrow; epidemiologic studies show that 30% to 43% of CAUTI patients are male, yielding a female-to-male ratio of only about 2:1.3,26,27 Men who develop complicated UTI exhibit increased morbidity and mortality compared to women,28–31 and morbidity from upper-tract UTI increases risk for hypertension and end-stage renal disease later in life.32
Beyond anatomy, other sex differences that influence UTI susceptibility and severity are beginning to be identified, enabled by recent advances in laboratory models of UTI. Historically, mouse modeling of UTI has been limited to females, as reliable access to the male mouse bladder via catheter insertion is technically challenging. Studies using a mini-surgical bladder inoculation method in both male and female mice show that once anatomic protections were bypassed in this way, male mice suffered more severe UTI, with strikingly higher incidences of chronic cystitis, severe pyelonephritis, and renal abscess formation.33,34 This increased morbidity of uropathogenic Escherichia coli (UPEC) UTI was shown to be driven by androgens: In C3H/HeN mice (a strain susceptible to cystitis and pyelonephritis), castrated males exhibited low bacterial loads and no abscess formation (equivalent to females), whereas treatment of castrated males with testosterone or 5α-dihydrotestosterone (DHT; a non-hydrolyzable testosterone derivative) restored susceptibility to severe UTI phenotypes.33,35 In related studies, female C3H/HeN or C57BL/6 mice (a strain resistant to cystitis and pyelonephritis) treated with DHT exhibited higher bacterial loads and more frequent severe UTI outcomes (including abscesses) than placebo-treated females, whereas treatment of these androgenized females with enzalutamide, a second-generation androgen receptor antagonist, enabled them to clear UPEC effectively and avoid complications.35 Though identification of androgens as drivers of a female-predominant disease may seem counterintuitive, epidemiologic data in specific, relevant populations do support a role for androgens in UTI susceptibility. First, infant males exhibit a postnatal burst of testosterone that returns to a prepubertal baseline by 6 months of age, matching the increased incidence of UTI in boys compared with girls in that interval.36 Further, women with polycystic ovary syndrome, a common hyperandrogenic condition, may have an increased rate of UTI compared with their peers.37,38 Thus far, updated mouse models have identified altered cytokine responses as a possible mechanism underlying sex differences in UTI pathogenesis33,39; however, other androgen-responsive mechanisms and pathways are actively being investigated.
In CAUTI, duration of catheterization is the most important determinant of bacteriuria, and CAUTI risk increases by 3% to 7% each day after placement of an indwelling urinary catheter.40 Even short-term urinary catheterization increases the risk of developing CAUTI and other complications up to 80%, and prolonged catheterization can increase the risk to nearly 100%.14–16 Furthermore, patients with catheter-associated bacteriuria have a 3% risk of developing bacteremia.41 Clinical studies have shown that the mechanical stress induced by urinary catheterization elicits histological and immunological changes in the bladder, resulting in a robust inflammatory response, exfoliation, edema, and mucosal lesions of the bladder epithelium and even affecting the kidneys.42–44 Furthermore, prolonged urinary catheterization results in ongoing epithelial irritation and persistent inflammation and has been linked with development of proliferative pathologies including squamous carcinoma, keratinizing squamous carcinoma, or cystitis granularis (which can progress to adenocarcinoma).45 It is important to note that urinary catheterization not only induces ongoing inflammation but also interferes with normal micturition (voiding)1 and mechanically impairs host defenses in the bladder, enabling microbial colonization, multiplication, and dissemination within the urinary tract.9,46,47 Additionally, inflammation elicited by the catheter can expose cryptic epithelial receptors that can be recognized and leveraged for colonization by the pathogen.48 Recent studies in both mice and humans show that urinary catheterization-induced inflammation elicits fibrinogen release into the bladder to heal damaged tissue and prevent bleeding. Due to constant mechanical damage caused by the urinary catheter, fibrinogen accumulates in the bladder and deposits onto the catheter, at concentrations that increase with extended time of catheterization.49–51 Some uropathogens, such as E. faecalis, Staphylococcus aureus, and Candida albicans, use fibrinogen to establish colonization (discussed below).49–53 Therefore, the presence of a urinary catheter and associated inflammation modify the bladder environment, offering a window of opportunity for microbial colonization and disease causation.
Pathogen Prevalence in Uncomplicated UTI and CAUTI
UPEC is the major causative agent of both uncomplicated UTI and CAUTI.54–56 In uncomplicated UTI, UPEC accounts for 75% to 85% of cases,3,54,55 followed by Klebsiella pneumoniae (~6%), Staphylococcus saprophyticus (~6%), and the remaining fraction comprising Enterococcus spp, group B streptococcus (GBS), Proteus spp, and Pseudomonas aeruginosa. In contrast, causative pathogens in CAUTI are more diverse than in uncomplicated UTI (Figure 1). A National Healthcare Safety Network (NHSN) review showed that UPEC accounts for just 23.9% of cases of CAUTI, followed by Candida spp (17.8%), Enterococcus spp (13.8%), P. aeruginosa (10.3%), Klebsiella spp (10.1%), Proteus spp (4%), Enterobacter spp (3.7%), coagulase-negative staphylococci (2.4%), S. aureus (1.6%), and even Bacteroides spp (<0.1%).56 Notably, the catheterized bladder environment lowers the threshold for uropathogens that might not be successful otherwise and provides a platform for other opportunistic microbes to infect.
Figure 1.
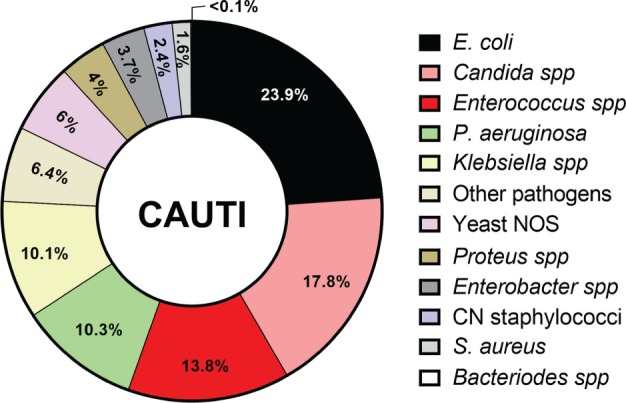
Catheter-associated urinary tract infection (CAUTI) uropathogen prevalence. CN = coagulase-negative; NOS = not otherwise specified.
Virulence Mechanisms in Uncomplicated UTI
UPEC and K. pneumoniae are the most common uncomplicated UTI pathogens. Distinct from other uropathogens, UPEC and K. pneumoniae have dedicated mechanisms for (a) recognition, adherence, and invasion of urothelial cells; (b) replication inside the cell to form intracellular bacterial communities; and (c) bacterial dispersion and host cell re-invasion.1,13,17
Recognition, Adherence, and Invasion of Urothelial Cells
After periurethral contamination by the gastrointestinal flora, UPEC cystitis isolate UTI89 and K. pneumoniae cystitis isolate TOP52 can colonize the urethra and ascend to the bladder; this migration may be enabled by the use of appendages such as flagella and pili.1,3,17 Once in the bladder lumen, UPEC and K. pneumoniae utilize the type 1 pilus, specifically its tip adhesin FimH, to bind superficial umbrella cells of the uroepithelium.57,58 FimH recognizes mannose decorating the uroplakin protein UPIa, a major component of the apical surfaces of umbrella cells.59 Expression of type 1 pili is critical for colonization, invasion, and establishment of cystitis.1 In fact, K. pneumoniae (on the basis of encoding the “extra” type 1 pilus regulator fimK) appears programmed for reduced expression of type 1 pili, which may explain why it is a less prevalent agent of UTI than UPEC.58 After adherence, some of the attached bacteria are internalized inside the umbrella cells with the purpose of replicating while subverting certain host defenses.57,60 The bacterial internalization cascade starts when Rho GTPases are activated, inducing actin rearrangement and internalizing surface-bound bacteria by plasma membrane engulfment.61 However, umbrella cells can also reverse this critical pathogenic step by expelling internalized UPEC. The expulsion mechanism relies on the recognition of Gram-negative lipopolysaccharide (LPS) by Toll-like receptor 4 (TLR4) expressed on umbrella cells; this interaction leads to an increase in intracellular cyclic AMP, which prompts expulsion of UPEC-containing vesicles.3,62,63
Replication Within Umbrella Cells Forming Intracellular Bacterial Communities
To evade expulsion, UPEC and K. pneumoniae escape the endocytic compartment and gain access to the umbrella cell cytoplasm by an undefined mechanism. The pathogen then rapidly multiplies forming type 1 pilus-dependent, biofilm-like intracellular bacterial communities (IBCs).64 IBCs are initially loose collections of rod-shaped bacteria that subsequently mature into tightly packed, coccoid organisms.65,66 IBC formation is critical for acute cystitis, since bacteria in the IBC are inaccessible to the phagocytic action of arriving neutrophils.65,66 An important host response to bacterial invasion is to exfoliate IBC-containing umbrella cells, liberating IBCs into the urine.67
Bacterial Dispersion and Host Cell Re-invasion
In a mature IBC, the bacteria in the periphery of the biofilm either adopt a filamentous phenotype or detach from the community; following bacterial fluxing from the umbrella cell, bacteria disperse with the purpose of invading naïve umbrella cells. This filamentous phenotype allows the bacteria to resist phagocytosis by neutrophils. To accomplish this phenotype, the bacterium requires the expression of the cell division inhibitor SulA, which enables elongation without septation.65,66,68 Once in the lumen of the bladder, the bacteria can either re-enter the IBC cycle or infect immature bladder cells exposed by exfoliation, consequently establishing quiescent intracellular reservoirs (QIRs). Distinct from IBCs, QIRs are composed of 4 to 10 nonreplicating bacteria that remain viable for months and are re-activated to seed recurrent UTIs. QIRs resist immune clearance and are not eradicated by antibiotic treatment.65,69,70
Furthermore, survival in the urinary tract is essential for colonization, persistence, and dissemination. The bladder is an iron-limited environment; therefore, UPEC and K. pneumoniae utilize a variety of virulence factors to obtain nutrients, including several iron acquisition systems called siderophores.1,3,71,72
Virulence Mechanisms in CAUTI
UPEC and K. pneumoniae cause UTIs regardless of the presence of a urinary catheter, due to these specialized mechanisms for bladder cell colonization and invasion.57,58,61,64–67,69,73 This section will focus on other prevalent CAUTI pathogens such as Enterococcus spp, S. aureus, Candida spp, P. aeruginosa, and P. mirabilis. The importance of the catheter in enabling pathogenesis by these organisms is exemplified by E. faecalis oral isolate OG1RF (model organism for CAUTI) and S. aureus isolate MRSA-1369, which are cleared from mouse bladders within a few days in the absence of a catheter but are able to establish persistent colonization during CAUTI.53,74 In the following sections, we will discuss the strategies that each pathogen uses to successfully cause CAUTI.
Enterococci
Enterococci have become the second most common bacteria recovered in CAUTI.3,9,40 E. faecalis uses endocarditis- and biofilm-associated (Ebp) pili for catheter adherence, colonization, and persistence during CAUTI.52,75–78 Initial in vitro characterization of E. faecalis OG1RF growth and biofilm in urine showed that E. faecalis was neither able to grow nor bind to the catheter material under these conditions.49 This contradiction was explained by the finding that urinary catheterization-induced inflammation response results in the release of the host protein fibrinogen, which accumulates in the bladder and on the catheter. Fibrinogen is normally found in the bloodstream, is a marker of vascular rupture, and is responsible for coagulation, fibrosis, protection from infections, and other functions.79 In CAUTI, the released fibrinogen is used by E. faecalis as a nutrient and a scaffold to form biofilms in the urinary catheter.49 During growth in urine, E. faecalis induces the expression of two major secreted proteases, SprE and GelE, which degrade fibrinogen for nutrient acquisition. Host proteases also enable enterococci to utilize fibrinogen and play a major role in promoting inflammation and dissemination.80 Furthermore, E. faecalis uses additional virulence factors to exploit fibrinogen-coated catheters and form biofilms during mouse and human CAUTI.49,50 E. faecalis expresses the Ebp pilus, tipped by the adhesin EbpA, which binds directly to fibrinogen via its N-terminal domain (EbpANTD); this interaction is critical for the formation of catheter-associated biofilms and persistence.49,50
Acquisition of nutrients, such as manganese (Mn), is essential for E. faecalis survival in the catheterized bladder. Mn is an essential micronutrient for bacterial pathogens during infection. In fact, one of the host mechanisms of defense is to reduce Mn availability to invading bacteria. To overcome this limitation, E. faecalis OG1RF contains three Mn transporters: one ABC-type (EfaCBA) and two Nramp-type transporters (MntH1 and MntH2). Deletion of all three Mn transporters from E. faecalis limits its ability to grow in Mn-minimal media or urine, and this mutant is defective in causing CAUTI. Single and double deletions showed that MntH2 is the primary player in Mn acquisition during CAUTI.81
Staphylococcus aureus
Despite the fact that S. aureus accounts for only approximately 1.5% of all CAUTI,56 S. aureus CAUTIs are frequently associated with severe sequelae, leading to increased rates of morbidity and mortality.53 Like E. faecalis, methicillin-resistant S. aureus (MRSA) takes advantage of urinary catheterization-induced inflammation, using the released fibrinogen to facilitate catheter colonization during mouse and human CAUTI.74 S. aureus strains are equipped with at least 20 fibrinogen-binding proteins.82 Interactions between MRSA and host fibrinogen are known to contribute to pathogenesis in other models of disease, such as central line infections and endocarditis.83–85 During CAUTI, S. aureus binds to fibrinogen via clumping factor B (ClfB).53 However, distinct from E. faecalis, MRSA-1369 and other S. aureus strains are able to grow in urine conditions without the need to use fibrinogen as a protein source.53
Proteus mirabilis
P. mirabilis forms biofilms on catheters86 and accounts for 5% of CAUTI.56 P. mirabilis is more prevalent in long-term catheterization patients and has become a common pathogen in nursing home residents.87 P. mirabilis urinary isolate H14320 uses an arsenal of virulence factors including mannose-resistant Proteus-like (MR/P) fimbria, ureases, flagella, a variety of toxins and proteases, numerous secretion systems (types I, III, IV, V, and VI), and iron transporters.86,88 P. mirabilis uses MR/P fimbria to attach to urothelial cells or the catheter, facilitating biofilm formation.89–92 During cystitis, P. mirabilis forms large communities on the luminal surfaces of bladder cells, in contrast to the IBC mechanism employed by UPEC and K. pneumoniae.64,69,86 During CAUTI, P. mirabilis produces ureases that hydrolyze urea to carbon dioxide and ammonia. The resulting increase in urinary pH induces precipitation of calcium crystals and magnesium ammonium phosphate, which then are incorporated into P. mirabilis polysaccharide capsules, creating crystalline biofilms on the catheter. Crystalline biofilms provide protection for P. mirabilis against immune components, particularly neutrophils.86 In the health care setting, 50% of patients with long-term catheterization (>28 days) experience catheter blockage by crystalline deposits,86 which affects urine flow and may promote reflux of infected urine to the kidneys. Moreover, P. mirabilis flagella contribute to ascending UTI and confer motility on hard surfaces such as a urinary catheter.93 To survive and grow in the urinary tract, P. mirabilis uses a variety of factors to obtain nutrients such as cytotoxin (hemolysin), proteases (ZapA and Pta), and iron acquisition systems (proteobactin, Nrp, and α-keto acids).86
Pseudomonas aeruginosa
P. aeruginosa is responsible for about 10% of CAUTI,81 using a variety of factors to exploit the catheterized bladder. Biofilm formation of P. aeruginosa isolate PA01 (also a CAUTI model organism) is enabled by production of extracellular DNA (eDNA), rhamnolipids, lectins, elastases, and toxins.94 Quorum sensing and exopolysaccharides are important for P. aeruginosa biofilm development in other environments but are not required for biofilm formation during CAUTI.95,96 Furthermore, bis-(3′-5′) cyclic dimeric GMP (c-di-GMP) concentration levels influence P. aeruginosa-mediated biofilms during CAUTI.97 Initially, P. aeruginosa promotes microcolony formation by using rhamnolipids, which modify the hydrophobicity of the bacterial cell surface. In later biofilm stages, rhamnolipids are responsible for migration initiation, enabling P. aeruginosa ascension in the urinary tract.94,98 P. aeruginosa expresses two siderophores, pyoverdin and pyochelin, that are dedicated to scavenging iron. Additionally, P. aeruginosa produces elastases, exoenzyme S, and hemolytic phospholipase C that destroy host cells, releasing nutrients.99,100
Candida spp
Candida is increasing as a causative agent of CAUTI, accounting for 17.8% of cases56; however, its pathogenic mechanisms during CAUTI are not well described.3,56,101 Candida species have been found associated with latex and silicone urinary catheters, with preference for latex material.101 Candida biofilms are readily detected on indwelling catheters by scanning electron microscopy.102 C. albicans adheres poorly to the bladder mucosa, and risk for Candida UTI increases sharply in the presence of an indwelling catheter.103,104 A recent ex vivo study showed that a C. albicans CAUTI isolate binds to urinary catheters via fibrinogen.50 C. albicans encodes a fibrinogen-binding protein, Mp58, which is expressed during candidiasis.105,106 In total, the wide distribution of diverse fibrinogen-binding adhesins among common uropathogens suggests that fibrinogen binding is a common theme in CAUTI pathogenesis.50
Prevention and Treatment of CAUTI
Urinary catheters are the most commonly used devices in hospitals; it is estimated that up to 25% of hospitalized patients undergo catheterization for different reasons such as urinary retention, surgical procedures, and prolonged immobilization.9,107,108 As our population ages, the use of urinary catheters becomes more frequent due to increased incidence of chronic and lifestyle-related diseases. Up to 13% of men and 12% of women have an indwelling urinary catheter on admission to nursing homes.109 Hospitalizations resulting from catheter-related complications are increasing.110 In 2008, the Centers for Medicare and Medicaid Services ceased reimbursement for the increased costs of care resulting from hospital-acquired CAUTI.111 In response, hospitals have developed strategies to reduce costs incurred and improve patient outcomes.112
Reducing Usage of Urinary Catheters and Minimizing Dwell Time
The Centers for Disease Control and Prevention (CDC) recommends minimizing urinary catheter use and duration, particularly in those at higher risk for CAUTI or mortality from catheterization such as women, the elderly, and patients with impaired immunity. CDC recommendations include the following: (a) avoid urinary catheterization to manage incontinence in patients and nursing home residents; (b) use urinary catheters in operative patients only as necessary, rather than routinely; and (c) in operative patients who have an indication for an indwelling catheter, remove the catheter as soon as possible postoperatively, preferably within 24 hours.108 Furthermore, recent bundles of interventions in clinical settings have shown success in reducing the incidence of CAUTI.113–115 These bundles focus on strategies to (a) reduce unnecessary placement of indwelling urinary catheters and encourage prompt removal and (b) ensure proper adherence to general infection control principles such as hand hygiene, surveillance/feedback of catheter use, aseptic insertions, proper maintenance, and education of clinical personnel.115 These interventions appear to be low cost, low risk, effective, and sustainable.115
Prophylactic Antibiotic Treatments
Control of CAUTIs has become a major challenge due to the development and dissemination of antibiotic resistance among the bacteria that cause health care–associated infections (HAI).9,116–118 Prophylactic antibiotics have been shown to promote the development of resistant organisms.8 Therefore, antibiotic stewardship initiatives have been developed to reduce the unnecessary use of antibiotics to curb development of resistant pathogens.119 Current CDC guidelines on management of CAUTI do not recommend the use of routine prophylaxis with systemic antibiotics for prevention of CAUTI in patients requiring short- or long-term urinary catheterization, unless clinical indications exist (e.g., in patients with bacteriuria upon catheter removal post urologic surgery).108 Additionally, there is no recommendation for use of antimicrobial prophylaxis at the time of catheter removal.120 Moreover, the CDC does not recommend the routine irrigation of the bladder with antimicrobial agents.108 Therefore, best practice is to reduce unnecessary catheterization and minimize dwell time.
Antimicrobial-Coated Urinary Catheters
Microbial biofilm formation on the surface of the urinary catheters is the most common underlying cause of bacteriuria.121 Biofilm formation is a microbial strategy to protect against antibiotic action and host immune defenses.122 Current CDC guidelines recommend the use of silicone catheters over other materials, because silicone catheters reduce the risk of encrustation in long-term catheterized patients who have frequent obstruction.108 Therefore, efforts to prevent biofilm formation have been focused on developing antimicrobial/antiseptic-impregnated, silicone-based urinary catheters.123,124 Tested in vitro, these new catheters efficiently killed bacteria and prevented biofilm formation. However, in clinical settings they have proven unsuccessful in controlling CAUTI or have yielded mixed results.110,123,125,126 For example, a large multicenter randomized controlled trial of silver-alloy and nitrofurazone-releasing catheters showed no significant reduction in symptomatic CAUTI.127
Treatment of CAUTI
Systemic antibiotic treatment is recommended for patients suffering CAUTI.110,128 A definite diagnosis of CAUTI requires bacteriuria between ≥103 and ≤105 CFU/mL with a positive urinalysis (defined by a positive dipstick, pyuria, or microorganisms seen on Gram stain).129 After CAUTI is diagnosed, the catheter should be removed (if possible) or replaced by a new catheter before starting antimicrobial therapy. Empiric antibiotic therapy can be broad spectrum but later should be optimized according to culture and susceptibility results.110 Inappropriate management of CAUTI has been linked with development of bacteremia, which is more worrisome with multidrug-resistant uropathogens.130 Therefore, appropriate management of CAUTI is important to reduce poor outcomes and mortality.110,130
Future Therapies: Vaccine and Immunotherapies
Antibiotic treatment, the standard of care for CAUTI, is becoming increasingly challenging as multidrug resistance expands among uropathogens. In addition, antibiotic treatment exerts collateral effects such as intestinal dysbiosis that can create niches for colonization by multidrug-resistant pathogens, which can ultimately dominate the gut microflora.131–133 Thus, understanding the molecular basis of host–pathogen interactions in CAUTI is crucial for development of efficient antibiotic-sparing intervention strategies and for preventing the further evolution of multidrug-resistant uropathogens.
A vaccine strategy targeting enterococcal interactions with fibrinogen may hold considerable promise, since EbpA is highly conserved among the enterococci and is critical for catheter colonization. In a mouse model of CAUTI, active immunization with EbpANTD protected mice against infection.49 Similarly, passive immunotherapy using anti-EbpANTD antibodies protected mice against E. faecalis CAUTI prophylactically and therapeutically. Notably, these antibodies disrupted established biofilms in vivo, which are well known to be difficult to eradicate in clinical settings. Furthermore, this immunotherapy was effective in treating CAUTI caused by a diverse collection of enterococcal clinical isolates from the urinary tract, bloodstream, and gastrointestinal tract, including representatives of E. faecalis, E. faecium, E. gallinarum, and vancomycin-resistant enterococci, as well as several unclassified enterococcal isolates.51 Thus, development of adhesin-based vaccines and monoclonal immunotherapies represent a promising avenue for novel therapeutics against selected uropathogens.
Outlook
Infection prevention and control represent a paramount achievement of modern medicine. Though urinary catheters are often necessary in managing complicated patients, these devices make patients susceptible to infections. CAUTIs impose a substantial threat to public health, and their treatment and control is becoming challenging due to the rise of antibiotic-resistant uropathogens. Recent discoveries of the adverse health effects of gut microbiota disruption provide additional impetus to reduce antibiotic use. Current research into understanding host-uropathogen interactions is moving the field toward new antibiotic-sparing approaches to CAUTI, with promising results.
REFERENCES
- 1.O'Brien VP, Hannan TJ, Nielsen HV, Hultgren SJ. Drug and vaccine development for the treatment and prevention of urinary tract infections. Microbiol Spectr. 2016;4(1) doi: 10.1128/microbiolspec.UTI-0013-2012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Stamm WE, Norrby SR. Urinary tract infections: Disease panorama and challenges. J Infect Dis. 2001;183(Suppl 1):S1–4. doi: 10.1086/318850. [DOI] [PubMed] [Google Scholar]
- 3.Flores-Mireles AL, Walker JN, Caparon M, Hultgren SJ. Urinary tract infections: Epidemiology, mechanisms of infection and treatment options. Nat Rev Microbiol. 2015;13(5):269–284. doi: 10.1038/nrmicro3432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Nimri L, Sulaiman M, Hani OB. Community-acquired urinary tract infections caused by Burkholderiacepacia complex in patients with no underlying risk factor. JMM Case Rep. 2017;4(1) doi: 10.1099/jmmcr.0.005081. e005081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Tambyah PA, Maki DG. Catheter-associated urinary tract infection is rarely symptomatic: A prospective study of 1,497 catheterized patients. Arch Intern Med. 2000;160(5):678–682. doi: 10.1001/archinte.160.5.678. [DOI] [PubMed] [Google Scholar]
- 6.Levison ME, Kaye D. Treatment of complicated urinary tract infections with an emphasis on drug-resistant gram-negative uropathogens. Curr Infect Dis Rep. 2013;15(2):109–115. doi: 10.1007/s11908-013-0315-7. [DOI] [PubMed] [Google Scholar]
- 7.Lichtenberger P, Hooton TM. Complicated urinary tract infections. Curr Infect Dis Rep. 2008;10(6):499–504. doi: 10.1007/s11908-008-0081-0. [DOI] [PubMed] [Google Scholar]
- 8.Hooton TM, Bradley SF, Cardenas DD et al. Diagnosis, prevention, and treatment of catheter-associated urinary tract infection in adults: 2009 International Clinical Practice Guidelines from the Infectious Diseases Society of America. Curr Infect Dis. 2010;50(5):625–663. doi: 10.1086/650482. [DOI] [PubMed] [Google Scholar]
- 9.Warren JW. Catheter-associated urinary tract infections. Infect Dis Clin N Am. 1997;11(3):609–622. doi: 10.1016/s0891-5520(05)70376-7. [DOI] [PubMed] [Google Scholar]
- 10.Trautner BW, Darouiche RO. Catheter-associated infections: Pathogenesis affects prevention. Arch Intern Med. 2004 Apr 26;164(8):842–850. doi: 10.1001/archinte.164.8.842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Melzer M, Welch C. Outcomes in UK patients with hospital-acquired bacteraemia and the risk of catheter-associated urinary tract infections. Postgrad Med J. 2013;89(1052):329–334. doi: 10.1136/postgradmedj-2012-131393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Saint S, Wiese J, Amory JK et al. Are physicians aware of which of their patients have indwelling urinary catheters? Am J Med. 2000;109(6):476–480. doi: 10.1016/s0002-9343(00)00531-3. [DOI] [PubMed] [Google Scholar]
- 13.Jain P, Parada JP, David A, Smith LG. Overuse of the indwelling urinary tract catheter in hospitalized medical patients. Arch Intern Med. J1995;155(13):1425–1429. [PubMed] [Google Scholar]
- 14.Parker D, Callan L, Harwood J, Thompson DL, Wilde M, Gray M. Nursing interventions to reduce the risk of catheter-associated urinary tract infection. Part 1: Catheter selection. J Wound Ostomy Continence Nurs. 2009;36(1):23–34. doi: 10.1097/01.WON.0000345173.05376.3e. [DOI] [PubMed] [Google Scholar]
- 15.Maki DG, Tambyah PA. Engineering out the risk for infection with urinary catheters. Emerg Infect Dis. 2001;7(2):342–347. doi: 10.3201/eid0702.010240. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Willson M, Wilde M, Webb ML et al. Nursing interventions to reduce the risk of catheter-associated urinary tract infection: part 2: Staff education, monitoring, and care techniques. J Wound Ostomy Continence Nurs. 2009;36(2):137–154. doi: 10.1097/01.WON.0000347655.56851.04. [DOI] [PubMed] [Google Scholar]
- 17.McLellan LK, Hunstad DA. Urinary tract infection: Pathogenesis and outlook. Trends Molec Med. 2016;22(11):946–957. doi: 10.1016/j.molmed.2016.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Schappert SM, Rechtsteiner EA. Ambulatory medical care utilization estimates for 2007. Vital Health Statistics 13. 2011;Apr(169):1–38. [PubMed] [Google Scholar]
- 19.Sammon JD, Sharma P, Rahbar H et al. Predictors of admission in patients presenting to the emergency department with urinary tract infection. World J Urol. 2014;32(3):813–819. doi: 10.1007/s00345-013-1167-3. [DOI] [PubMed] [Google Scholar]
- 20.Al-Badr A, Al-Shaikh G. Recurrent urinary tract infections management in women: A review. Sultan Qaboos University Med J. 2013;13(3):359–367. doi: 10.12816/0003256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hannan TJ, Hunstad DA. A murine model for Escherichia coli urinary tract infection. Methods Molec Biol. 2016;1333:159–175. doi: 10.1007/978-1-4939-2854-5_14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Foxman B. Epidemiology of urinary tract infections: Incidence, morbidity, and economic costs. Am J Med. 2002;133(Suppl 1A):5S–13S. doi: 10.1016/s0002-9343(02)01054-9. [DOI] [PubMed] [Google Scholar]
- 23.Ruben FL, Dearwater SR, Norden CW et al. Clinical infections in the noninstitutionalized geriatric age group: Methods utilized and incidence of infections. The Pittsburgh Good Health Study. Am J Epidemiol. 1995;141(2):145–157. doi: 10.1093/oxfordjournals.aje.a117402. [DOI] [PubMed] [Google Scholar]
- 24.Shaikh N, Morone NE, Bost JE, Farrell MH. Prevalence of urinary tract infection in childhood: A meta-analysis. Pediatr Infect Dis J. 2008;27(4):302–308. doi: 10.1097/INF.0b013e31815e4122. [DOI] [PubMed] [Google Scholar]
- 25.Wettergren B, Jodal U, Jonasson G. Epidemiology of bacteriuria during the first year of life. Acta Paediatrica Scand. 1985;74(6):925–933. doi: 10.1111/j.1651-2227.1985.tb10059.x. [DOI] [PubMed] [Google Scholar]
- 26.Kakaria BA, Ashish K, Tushar R. Study of incidence and risk factors of urinary tract infection in catheterised patients admitted at tertiary care. Int J Res Med Sci. 2018;6(5) [Google Scholar]
- 27.Daniels KR, Lee GC, Frei CR. Trends in catheter-associated urinary tract infections among a national cohort of hospitalized adults, 2001–2010. Am J Infect Control. 2014;42(1):17–22. doi: 10.1016/j.ajic.2013.06.026. [DOI] [PubMed] [Google Scholar]
- 28.Foxman B, Klemstine KL, Brown PD. Acute pyelonephritis in US hospitals in 1997: Hospitalization and in-hospital mortality. Ann Epidemiol. 2003;13(2):144–150. doi: 10.1016/s1047-2797(02)00272-7. [DOI] [PubMed] [Google Scholar]
- 29.Efstathiou SP, Pefanis AV, Tsioulos DI et al. Acute pyelonephritis in adults: Prediction of mortality and failure of treatment. Arch Intern Med. 2003;163(10):1206–1212. doi: 10.1001/archinte.163.10.1206. [DOI] [PubMed] [Google Scholar]
- 30.Nicolle LE, Friesen D, Harding GK, Roos LL. Hospitalization for acute pyelonephritis in Manitoba, Canada, during the period from 1989 to 1992; impact of diabetes, pregnancy, and aboriginal origin. Clin Infect Dis. 1996;22(6):1051–1056. doi: 10.1093/clinids/22.6.1051. [DOI] [PubMed] [Google Scholar]
- 31.Ki M, Park T, Choi B, Foxman B. The epidemiology of acute pyelonephritis in South Korea, 1997–1999. Am J Epidemiol. 2004;160(10):985–993. doi: 10.1093/aje/kwh308. [DOI] [PubMed] [Google Scholar]
- 32.Calderon-Margalit R, Golan E, Twig G et al. History of childhood kidney disease and risk of adult end-stage renal disease. New Engl J Med. 2018;378(5):428–438. doi: 10.1056/NEJMoa1700993. [DOI] [PubMed] [Google Scholar]
- 33.Olson PD, Hruska KA, Hunstad DA. Androgens enhance male urinary tract infection severity in a new model. J Am Soc Nephrol. 2016;27(6):1625–1634. doi: 10.1681/ASN.2015030327. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Olson PD, McLellan LK, Liu A et al. Correction: Renal scar formation and kidney function following antibiotic-treated murine pyelonephritis. Dis Model Mech. 2018;11(9) doi: 10.1242/dmm.036798. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Olson PD, McLellan LK, Hreha TN et al. Androgen exposure potentiates formation of intratubular communities and renal abscesses by Escherichia coli. Kidney Int. 2018;94(3):502–513. doi: 10.1016/j.kint.2018.04.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Lamminmaki A, Hines M, Kuiri-Hanninen T, Kilpelainen L, Dunkel L, Sankilampi U. Testosterone measured in infancy predicts subsequent sex-typed behavior in boys and in girls. Horm Behav. 2012;61(4):611–616. doi: 10.1016/j.yhbeh.2012.02.013. [DOI] [PubMed] [Google Scholar]
- 37.Risma KA, Clay CM, Nett TM, Wagner T, Yun J, Nilson JH. Targeted overexpression of luteinizing hormone in transgenic mice leads to infertility, polycystic ovaries, and ovarian tumors. Proc Natl Acad Sci USA. 1995;92(5):1322–1326. doi: 10.1073/pnas.92.5.1322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Idrizi A, Barbullushi M, Koroshi A et al. Urinary tract infections in polycystic kidney disease. Med Arhiv. 2011;65(4):213–215. doi: 10.5455/medarh.2011.65.213-215. [DOI] [PubMed] [Google Scholar]
- 39.Zychlinsky Sharff A, Rousseau M, Lacerna Mariano L et al. Sex differences in IL-17 determine chronicity in male versus female urinary tract infections. JCI Insight. 2019 doi: 10.1172/jci.insight.122998. doi: 10.1172/jci.insight.122998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Nicolle LE. Catheter-associated urinary tract infections. Antimicrob Resist Infect Control. 2014;3:23. doi: 10.1186/2047-2994-3-23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Saint S. Clinical and economic consequences of nosocomial catheter-related bacteriuria. Am J Infect Control. 2000;28(1):68–75. doi: 10.1016/s0196-6553(00)90015-4. [DOI] [PubMed] [Google Scholar]
- 42.Goble NM, Clarke T, Hammonds JC. Histological changes in the urinary bladder secondary to urethral catheterisation. Brit J Urol. 1989;63(4):354–357. doi: 10.1111/j.1464-410x.1989.tb05216.x. [DOI] [PubMed] [Google Scholar]
- 43.Glahn BE, Braendstrup O, Olesen HP. Influence of drainage conditions on mucosal bladder damage by indwelling catheters. II. Histological study. Scand J Urol Nephrol. 1988;22(2):93–99. doi: 10.1080/00365599.1988.11690392. [DOI] [PubMed] [Google Scholar]
- 44.Peychl L, Zalud R. [Changes in the urinary bladder caused by short-term permanent catheter insertion] Casopis Lekaru Ceskych. 2008;147(6):325–329. [PubMed] [Google Scholar]
- 45.Delnay KM, Stonehill WH, Goldman H, Jukkola AF, Dmochowski RR. Bladder histological changes associated with chronic indwelling urinary catheter. J Urol. 1999;161(4):1106–1108. discussion 1108–1109. [PubMed] [Google Scholar]
- 46.Garibaldi RA, Burke JP, Dickman ML, Smith CB. Factors predisposing to bacteriuria during indwelling urethral catheterization. New Engl J Med. 1974;291(5):215–219. doi: 10.1056/NEJM197408012910501. [DOI] [PubMed] [Google Scholar]
- 47.Norden CW, Green GM, Kass EH. Antibacterial mechanisms of the urinary bladder. J Clin Invest. 1968;47(12):2689–2700. doi: 10.1172/JCI105952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Parsons CL. Pathogenesis of urinary tract infections. Bacterial adherence, bladder defense mechanisms. Urol Clin N Am. 1986;13(4):563–568. [PubMed] [Google Scholar]
- 49.Flores-Mireles AL, Pinkner JS, Caparon MG, Hultgren SJ. EbpA vaccine antibodies block binding of Enterococcus faecalis to fibrinogen to prevent catheter-associated bladder infection in mice. Sci Transl Med. 2014;6(254) doi: 10.1126/scitranslmed.3009384. 254ra127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Flores-Mireles AL, Walker JN, Bauman TM et al. Fibrinogen release and deposition on urinary catheters placed during urological procedures. J Urol. 2016;196(2):416–421. doi: 10.1016/j.juro.2016.01.100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Flores-Mireles AL, Walker JN, Potretzke A et al. Antibody-based therapy for enterococcal catheter-associated urinary tract infections. mBio. 2016;7(5) doi: 10.1128/mBio.01653-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Nielsen HV, Flores-Mireles AL, Kau AL et al. Pilin and sortase residues critical for endocarditis- and biofilm-associated pilus biogenesis in Enterococcus faecalis. J Bacteriol. 2013;195(19):4484–4495. doi: 10.1128/JB.00451-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Walker JN, Flores-Mireles AL, Pinkner CL et al. Catheterization alters bladder ecology to potentiate Staphylococcus aureus infection of the urinary tract. Proc Natl Acad Sci USA. 2017;114(41):E8721–E8730. doi: 10.1073/pnas.1707572114. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Foxman B. The epidemiology of urinary tract infection. Nat Rev Urol. 2010;7(12):653–660. doi: 10.1038/nrurol.2010.190. [DOI] [PubMed] [Google Scholar]
- 55.Foxman B. Urinary tract infection syndromes: Occurrence, recurrence, bacteriology, risk factors, and disease burden. Infect Dis Clin N Am. 2014;28(1):1–13. doi: 10.1016/j.idc.2013.09.003. [DOI] [PubMed] [Google Scholar]
- 56.Weiner LM, Webb AK, Limbago B et al. Antimicrobial-resistant pathogens associated with healthcare-associated infections: Summary of data reported to the national healthcare safety network at the Centers for Disease Control and Prevention, 2011–2014. Infect Control Hosp Epidemiol. 2016;37(11):1288–1301. doi: 10.1017/ice.2016.174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Martinez JJ, Mulvey MA, Schilling JD, Pinkner JS, Hultgren SJ. Type 1 pilus-mediated bacterial invasion of bladder epithelial cells. EMBO J. 2000;19(12):2803–2812. doi: 10.1093/emboj/19.12.2803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Rosen DA, Pinkner JS, Walker JN, Elam JS, Jones JM, Hultgren SJ. Molecular variations in Klebsiella pneumoniae and Escherichia coli FimH affect function and pathogenesis in the urinary tract. Infect Immun. 2008;76(7):3346–3356. doi: 10.1128/IAI.00340-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Zhou G, Mo WJ, Sebbel P et al. Uroplakin Ia is the urothelial receptor for uropathogenic Escherichia coli Evidence from in vitro FimH binding. J Cell Sci. 2001;114(Pt 22):4095–4103. doi: 10.1242/jcs.114.22.4095. [DOI] [PubMed] [Google Scholar]
- 60.Schwartz DJ, Chen SL, Hultgren SJ, Seed PC. Population dynamics and niche distribution of uropathogenic Escherichia coli during acute and chronic urinary tract infection. Infect Immun. 2011;79(10):4250–4259. doi: 10.1128/IAI.05339-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Martinez JJ, Hultgren SJ. Requirement of Rho-family GTPases in the invasion of type 1-piliated uropathogenic Escherichia coli. Cell Microbiol. 2002;4(1):19–28. doi: 10.1046/j.1462-5822.2002.00166.x. [DOI] [PubMed] [Google Scholar]
- 62.Song J, Bishop BL, Li G, Grady R, Stapleton A, Abraham SN. TLR4-mediated expulsion of bacteria from infected bladder epithelial cells. Proc Natl Acad Sci USA. 2009;106(35):14966–14971. doi: 10.1073/pnas.0900527106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Miao Y, Bist P, Wu J et al. Collaboration between distinct Rab small GTPase trafficking circuits mediates bacterial clearance from the bladder epithelium. Cell Host Microbe. 2017;22(3):330–342. e334. doi: 10.1016/j.chom.2017.08.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Wright KJ, Seed PC, Hultgren SJ. Development of intracellular bacterial communities of uropathogenic Escherichia coli depends on type 1 pili. Cell Microbiol. 2007;9(9):2230–2241. doi: 10.1111/j.1462-5822.2007.00952.x. [DOI] [PubMed] [Google Scholar]
- 65.Justice SS, Hung C, Theriot JA et al. Differentiation and developmental pathways of uropathogenic Escherichia coli in urinary tract pathogenesis. Proc Natl Acad Sci USA. 2004;101(5):1333–1338. doi: 10.1073/pnas.0308125100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Justice SS, Hunstad DA, Seed PC, Hultgren SJ. Filamentation by Escherichia coli subverts innate defenses during urinary tract infection. Proc Natl Acad Sci USA. 2006;103(52):19884–19889. doi: 10.1073/pnas.0606329104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Mulvey MA, Lopez-Boado YS, Wilson CL et al. Induction and evasion of host defenses by type 1-piliated uropathogenic Escherichia coli. Science. 1998;282(5393):1494–1497. doi: 10.1126/science.282.5393.1494. [DOI] [PubMed] [Google Scholar]
- 68.Olson PD, Hunstad DA. Subversion of host innate immunity by uropathogenic Escherichia coli. Pathogens. 2016;5(1) doi: 10.3390/pathogens5010002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Rosen DA, Pinkner JS, Jones JM, Walker JN, Clegg S, Hultgren SJ. Utilization of an intracellular bacterial community pathway in Klebsiella pneumoniae urinary tract infection and the effects of FimK on type 1 pilus expression. Infect Immun. 2008;76(7):3337–3345. doi: 10.1128/IAI.00090-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Mysorekar IU, Hultgren SJ. Mechanisms of uropathogenic Escherichia coli persistence and eradication from the urinary tract. Proc Natl Acad Sci USA. 2006;103(38):14170–14175. doi: 10.1073/pnas.0602136103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Robinson AE, Heffernan JR, Henderson JP. The iron hand of uropathogenic Escherichia coli The role of transition metal control in virulence. Future Microbiol. 2018;13:745–756. doi: 10.2217/fmb-2017-0295. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Su Q, Guan T, He Y, Lv H. Siderophore biosynthesis governs the virulence of uropathogenic Escherichia coli by coordinately modulating the differential metabolism. J Proteome Res. 2016;15(4):1323–1332. doi: 10.1021/acs.jproteome.6b00061. [DOI] [PubMed] [Google Scholar]
- 73.Justice SS, Harrison A, Becknell B, Mason KM. Bacterial differentiation, development, and disease: Mechanisms for survival. FEMS Microbiol Lett. 2014;360(1):1–8. doi: 10.1111/1574-6968.12602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Guiton PS, Hannan TJ, Ford B, Caparon MG, Hultgren SJ. Enterococcus faecalis overcomes foreign body-mediated inflammation to establish urinary tract infections. Infect Immun. 2013;81(1):329–339. doi: 10.1128/IAI.00856-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Nielsen HV, Guiton PS, Kline KA et al. The metal ion-dependent adhesion site motif of the Enterococcus faecalis EbpA pilin mediates pilus function in catheter-associated urinary tract infection. mBio. 2012;3(4):e00177–00112. doi: 10.1128/mBio.00177-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Singh KV, Nallapareddy SR, Murray BE. Importance of the ebp (endocarditis- and biofilm-associated pilus) locus in the pathogenesis of Enterococcus faecalis ascending urinary tract infection. J Infect Dis. 2007;195(11):1671–1677. doi: 10.1086/517524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Nallapareddy SR, Singh KV, Sillanpaa J et al. Endocarditis and biofilm-associated pili of Enterococcus faecalis. J Clin Invest. 2006;116(10):2799–2807. doi: 10.1172/JCI29021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Nallapareddy SR, Singh KV, Sillanpaa J, Zhao M, Murray BE. Relative contributions of Ebp Pili and the collagen adhesin ace to host extracellular matrix protein adherence and experimental urinary tract infection by Enterococcus faecalis OG1RF. Infect Immun. 2011;79(7):2901–2910. doi: 10.1128/IAI.00038-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Jennewein C, Tran N, Paulus P, Ellinghaus P, Eble JA, Zacharowski K. Novel aspects of fibrin(ogen) fragments during inflammation. Molec Med. 2011;17(5–6):568–573. doi: 10.2119/molmed.2010.00146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Xu W, Flores-Mireles AL, Cusumano ZT, Takagi E, Hultgren SJ, Caparon MG. Host and bacterial proteases influence biofilm formation and virulence in a murine model of enterococcal catheter-associated urinary tract infection. NPJ Biofilms Microbiomes. 2017;3:28. doi: 10.1038/s41522-017-0036-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Colomer-Winter C, Flores-Mireles AL, Baker SP et al. Manganese acquisition is essential for virulence of Enterococcus faecalis. PLoS Pathog. 2018;14(9) doi: 10.1371/journal.ppat.1007102. e1007102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Crosby HA, Kwiecinski J, Horswill AR. Staphylococcus aureus aggregation and coagulation mechanisms, and their function in host-pathogen interactions. Adv Appl Microbiol. 2016;96:1–41. doi: 10.1016/bs.aambs.2016.07.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Rivera J, Vannakambadi G, Hook M, Speziale P. Fibrinogen-binding proteins of Gram-positive bacteria. Thrombosis Haemostasis. 2007;98(3):503–511. [PubMed] [Google Scholar]
- 84.Arciola CR, Visai L, Testoni F et al. Concise survey of Staphylococcus aureus virulence factors that promote adhesion and damage to peri-implant tissues. Intern J Artificial Organs. 2011;34(9):771–780. doi: 10.5301/ijao.5000046. [DOI] [PubMed] [Google Scholar]
- 85.Foster TJ, Hook M. Surface protein adhesins of Staphylococcus aureus. Trends Microbiol. 1998;6(12):484–488. doi: 10.1016/s0966-842x(98)01400-0. [DOI] [PubMed] [Google Scholar]
- 86.Armbruster CE, Mobley HLT, Pearson MM. Pathogenesis of Proteus mirabilis infection. EcoSal Plus. 2018;8(1) doi: 10.1128/ecosalplus.esp-0009-2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Armbruster CE, Prenovost K, Mobley HL, Mody L. How often do clinically diagnosed catheter-associated urinary tract infections in nursing homes meet standardized criteria? J Am Geriatr Soc. 2017;65(2):395–401. doi: 10.1111/jgs.14533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Armbruster CE, Forsyth-DeOrnellas V, Johnson AO et al. Genome-wide transposon mutagenesis of Proteus mirabilis Essential genes, fitness factors for catheter-associated urinary tract infection, and the impact of polymicrobial infection on fitness requirements. PLoS Pathog. 2017;13(6) doi: 10.1371/journal.ppat.1006434. e1006434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Nielubowicz GR, Mobley HL. Host-pathogen interactions in urinary tract infection. Nat Rev Urol. 2010;7(8):430–441. doi: 10.1038/nrurol.2010.101. [DOI] [PubMed] [Google Scholar]
- 90.Jacobsen SM, Stickler DJ, Mobley HL, Shirtliff ME. Complicated catheter-associated urinary tract infections due to Escherichia coli and Proteus mirabilis. Clin Microbiol Rev. 2008;21(1):26–59. doi: 10.1128/CMR.00019-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Jacobsen SM, Shirtliff ME. Proteus mirabilis biofilms and catheter-associated urinary tract infections. Virulence. 2011;2(5):460–465. doi: 10.4161/viru.2.5.17783. [DOI] [PubMed] [Google Scholar]
- 92.Armbruster CE, Mobley HL. Merging mythology and morphology: The multifaceted lifestyle of Proteus mirabilis. Nat Rev Microbiol. 2012;10(11):743–754. doi: 10.1038/nrmicro2890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Mobley HL, Belas R, Lockatell V et al. Construction of a flagellum-negative mutant of Proteus mirabilis Effect on internalization by human renal epithelial cells and virulence in a mouse model of ascending urinary tract infection. Infect Immun. 1996;64(12):5332–5340. doi: 10.1128/iai.64.12.5332-5340.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Newman JW, Floyd RV, Fothergill JL. The contribution of Pseudomonas aeruginosa virulence factors and host factors in the establishment of urinary tract infections. FEMS Microbiol Lett. 2017;364(15) doi: 10.1093/femsle/fnx124. [DOI] [PubMed] [Google Scholar]
- 95.Cole SJ, Records AR, Orr MW, Linden SB, Lee VT. Catheter-associated urinary tract infection by Pseudomonas aeruginosa is mediated by exopolysaccharide-independent biofilms. Infect Immun. 2014;82(5):2048–2058. doi: 10.1128/IAI.01652-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Cole SJ, Hall CL, Schniederberend M et al. Host suppression of quorum sensing during catheter-associated urinary tract infections. Nat Commun. 2018;9(1):4436. doi: 10.1038/s41467-018-06882-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Cole SJ, Lee VT. Cyclic Di-GMP Signaling contributes to Pseudomonas aeruginosamediated catheter-associated urinary tract infection. J Bacteriol. 2016;198(1):91–97. doi: 10.1128/JB.00410-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Pamp SJ, Tolker-Nielsen T. Multiple roles of biosurfactants in structural biofilm development by Pseudomonas aeruginosa. J Bacteriol. 2007;189(6):2531–2539. doi: 10.1128/JB.01515-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Mittal R, Khandwaha RK, Gupta V, Mittal PK, Harjai K. Phenotypic characters of urinary isolates of Pseudomonas aeruginosa and their association with mouse renal colonization. Indian J Med Res. 2006;123(1):67–72. [PubMed] [Google Scholar]
- 100.Mittal R, Sharma S, Chhibber S, Harjai K. Iron dictates the virulence of Pseudomonas aeruginosa in urinary tract infections. J Biomed Sci. 2008;15(6):731–741. doi: 10.1007/s11373-008-9274-7. [DOI] [PubMed] [Google Scholar]
- 101.Tamura NK, Gasparetto A, Svidzinski TI. Evaluation of the adherence of Candida species to urinary catheters. Mycopathologia. 2003;156(4):269–272. doi: 10.1023/b:myco.0000003559.59676.f7. [DOI] [PubMed] [Google Scholar]
- 102.Azmy M, Nawar N, Mohiedden M, Warille L. Electron microscopic assay of bacterial biofilm formed on indwelling urethral catheters. J Egyptian Soc Parasitol. 2016;46(3):475–484. [PubMed] [Google Scholar]
- 103.Jain M, Dogra V, Mishra B, Thakur A, Loomba PS, Bhargava A. Candiduria in catheterized intensive care unit patients: Emerging microbiological trends. Indian J Pathol Microbiol. 2011;54(3):552–555. doi: 10.4103/0377-4929.85091. [DOI] [PubMed] [Google Scholar]
- 104.Y R, S M P, B U A, R R, A K B. Candiduria: Prevalence and trends in antifungal susceptibility in a tertiary care hospital of mangalore. J Clin Diagn Res. 2013;7(11):2459–2461. doi: 10.7860/JCDR/2013/6298.3578. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Casanova M, Lopez-Ribot JL, Monteagudo C, Llombart-Bosch A, Sentandreu R, Martinez JP. Identification of a 58-kilodalton cell surface fibrinogen-binding mannoprotein from Candida albicans. Infect Immun. 1992;60(10):4221–4229. doi: 10.1128/iai.60.10.4221-4229.1992. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Sepulveda P, Lopez-Ribot JL, Murgui A, Canton E, Navarro D, Martinez JP. Candida albicans fibrinogen binding mannoprotein: Expression in clinical strains and immunogenicity in patients with candidiasis. Intern Microbiol. 1998;1(3):209–216. [PubMed] [Google Scholar]
- 107.Haley RW, Hooton TM, Culver DH et al. Nosocomial infections in U.S. hospitals, 1975–1976: Estimated frequency by selected characteristics of patients. Am J Med. 1981;70(4):947–959. doi: 10.1016/0002-9343(81)90561-1. [DOI] [PubMed] [Google Scholar]
- 108.Gould C, Umscheid CA, Agarwal PK, Kuntz G, Pegues DA, Healthcare Infection Control Practices Advisory Committee Centers for Disease Control and Prevention; 2017 updated. Guideline for Prevention of Catheter-Associated Urinary Tract Infections 2009; pp. 1–61. https://www.cdc.gov/infectioncontrol/guidelines/cauti/index.html. [DOI] [PubMed] [Google Scholar]
- 109.Mody L, Greene MT, Meddings J et al. A national implementation project to prevent catheter-associated urinary tract infection in nursing home residents. JAMA Intern Med. 2017;177(8):1154–1162. doi: 10.1001/jamainternmed.2017.1689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Tenke P, Koves B, Johansen TE. An update on prevention and treatment of catheter-associated urinary tract infections. Curr Opin Infect Dis. 2014;27(1):102–107. doi: 10.1097/QCO.0000000000000031. [DOI] [PubMed] [Google Scholar]
- 111.Saint S, Greene MT, Kowalski CP, Watson SR, Hofer TP, Krein SL. Preventing catheter-associated urinary tract infection in the United States: A national comparative study. JAMA Intern Med. 2013;173(10):874–879. doi: 10.1001/jamainternmed.2013.101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Durant DJ. Nurse-driven protocols and the prevention of catheter-associated urinary tract infections: A systematic review. Am J Infect Control. 2017;45(12):1331–1341. doi: 10.1016/j.ajic.2017.07.020. [DOI] [PubMed] [Google Scholar]
- 113.Parker V, Giles M, Graham L et al. Avoiding inappropriate urinary catheter use and catheter-associated urinary tract infection (CAUTI): A pre-post control intervention study. BMC Health Services Res. 2017;17(1):314. doi: 10.1186/s12913-017-2268-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Ternavasio-de la Vega HG, Barbosa Ventura A, Castano-Romero F et al. Assessment of a multimodal intervention for the prevention of catheter-associated urinary tract infections. J Hosp Infect. 2016;94(2):175–181. doi: 10.1016/j.jhin.2016.07.011. [DOI] [PubMed] [Google Scholar]
- 115.Meddings J, Rogers MA, Krein SL, Fakih MG, Olmsted RN, Saint S. Reducing unnecessary urinary catheter use and other strategies to prevent catheter-associated urinary tract infection: An integrative review. BMJ Qual Safety. 2014;23(4):277–289. doi: 10.1136/bmjqs-2012-001774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Tambyah PA, Oon J. Catheter-associated urinary tract infection. Curr Opin Infect Dis. 2012;25(4):365–370. doi: 10.1097/QCO.0b013e32835565cc. [DOI] [PubMed] [Google Scholar]
- 117.Greene MT, Chang R, Kuhn L et al. Predictors of hospital-acquired urinary tract-related bloodstream infection. Infect Control Hosp Epidemiol. 2012;33(10):1001–1007. doi: 10.1086/667731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Johnson JR, Kuskowski MA, Wilt TJ. Systematic review: Antimicrobial urinary catheters to prevent catheter-associated urinary tract infection in hospitalized patients. Ann Intern Med. 2006;144(2):116–126. doi: 10.7326/0003-4819-144-2-200601170-00009. [DOI] [PubMed] [Google Scholar]
- 119.Trautner BW, Prasad P, Grigoryan L et al. Protocol to disseminate a hospital-site controlled intervention using audit and feedback to implement guidelines concerning inappropriate treatment of asymptomatic bacteriuria. Implementation Sci. 2018;13(1):16. doi: 10.1186/s13012-018-0709-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Marschall J, Carpenter CR, Fowler S, Trautner BW, Program CDCPE Antibiotic prophylaxis for urinary tract infections after removal of urinary catheter: Meta-analysis. Br Med J. 2013;346 doi: 10.1136/bmj.f3147. f3147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Stickler DJ. Bacterial biofilms in patients with indwelling urinary catheters. Nat Clin Pract Urol. 2008;5(11):598–608. doi: 10.1038/ncpuro1231. [DOI] [PubMed] [Google Scholar]
- 122.Thomas WE, Nilsson LM, Forero M, Sokurenko EV, Vogel V. Shear-dependent “stick-and-roll” adhesion of type 1 fimbriated Escherichia coli. Mol Microbiol. 2004;53(5):1545–1557. doi: 10.1111/j.1365-2958.2004.04226.x. [DOI] [PubMed] [Google Scholar]
- 123.Ha US, Cho YH. Catheter-associated urinary tract infections: New aspects of novel urinary catheters. Int J Antimicrob Agents. 2006;28(6):485–490. doi: 10.1016/j.ijantimicag.2006.08.020. [DOI] [PubMed] [Google Scholar]
- 124.Singha P, Locklin J, Handa H. A review of the recent advances in antimicrobial coatings for urinary catheters. Acta Biomaterialia. 2017;50:20–40. doi: 10.1016/j.actbio.2016.11.070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Pickard R, Lam T, Maclennan G et al. Types of urethral catheter for reducing symptomatic urinary tract infections in hospitalised adults requiring short-term catheterisation: Multicentre randomised controlled trial and economic evaluation of antimicrobial- and antiseptic-impregnated urethral catheters (the CATHETER trial) Health Technol Assessment. 2012;16(47):1–197. doi: 10.3310/hta16470. [DOI] [PubMed] [Google Scholar]
- 126.Tenke P, Koves B, Nagy K et al. Update on biofilm infections in the urinary tract. World J Urol. 2012;30(1):51–57. doi: 10.1007/s00345-011-0689-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Pickard R, Lam T, MacLennan G et al. Antimicrobial catheters for reduction of symptomatic urinary tract infection in adults requiring short-term catheterisation in hospital: A multicentre randomised controlled trial. Lancet. 2012;380(9857):1927–1935. doi: 10.1016/S0140-6736(12)61380-4. [DOI] [PubMed] [Google Scholar]
- 128.Niel-Weise BS, van den Broek PJ, da Silva EM, Silva LA. Urinary catheter policies for long-term bladder drainage. Cochrane Datab System Rev. 2012;(8) CD004201. [Google Scholar]
- 129.Trautner BW. Management of catheter-associated urinary tract infection. Curr Opinion Infect Dis. 2010;23(1):76–82. doi: 10.1097/QCO.0b013e328334dda8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Ortega M, Marco F, Soriano A et al. Epidemiology and prognostic determinants of bacteraemic catheter-acquired urinary tract infection in a single institution from 1991 to 2010. J Infect. 2013;67(4):282–287. doi: 10.1016/j.jinf.2013.06.003. [DOI] [PubMed] [Google Scholar]
- 131.Van Tyne D, Gilmore MS. Friend turned foe: Evolution of enterococcal virulence and antibiotic resistance. Ann Rev Microbiol. 2014;68:337–356. doi: 10.1146/annurev-micro-091213-113003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Cardoso T, Ribeiro O, Aragao IC, Costa-Pereira A, Sarmento AE. Additional risk factors for infection by multidrug-resistant pathogens in healthcare-associated infection: A large cohort study. BMC Infect Dis. 2012;12:375. doi: 10.1186/1471-2334-12-375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Miller WR, Munita JM, Arias CA. Mechanisms of antibiotic resistance in enterococci. Expert Rev Anti-infect Ther. 2014;12(10):1221–1236. doi: 10.1586/14787210.2014.956092. [DOI] [PMC free article] [PubMed] [Google Scholar]


