Abstract
Background:
Former combustible cigarette smokers who vape e-cigarettes after quitting smoking may experience health benefits if post-quit vaping prevents smoking relapse.
Methods:
Former combustible cigarette smokers aged >18 that were recent (quit ≤ 12 months) or long-term (quit > 12 months) quitters at baseline were re-surveyed at 1-year follow-up in the Population Assessment of Tobacco and Health (PATH) U.S. nationally-representative longitudinal study. Associations of baseline e-cigarette vaping status (never use, prior use, current occasional use, and current regular use) and smoking relapse (vs. abstinence) at follow-up were estimated.
Results:
Among recent quitters (N = 884), the prevalence of follow-up smoking relapse was 31.6%, 39.0%, 51.6%, and 31.9% among never (N = 233), prior (N = 399), current occasional (N = 56), and current regular (N = 196) baseline e-cigarette users, respectively. Baseline e-cigarette use was not associated with smoking relapse at follow-up after covariate adjustment. In long-term quitters (n = 3210), follow-up smoking relapse was 1.8%, 10.4%, 9.6%, and 15.0% among never (N = 2479), prior (N = 588), current occasional (N = 45), and current regular (N = 98) baseline e-cigarette users, respectively. Both prior use (AOR = 2.00, CI [1.25–3.20]) and current regular use of e-cigarettes (AOR = 3.77, CI [1.48–9.65]) had higher odds of subsequent smoking relapse as compared to never e-cigarette users after covariate adjustment. Among relapsers, baseline e-cigarette vaping was not associated with smoking frequency or intensity at follow-up.
Conclusions:
Vaping more than one year after quitting smoking was associated with smoking relapse at 12-month follow-up in a nationally-representative sample. Further studies are needed to evaluate whether this association is causal.
Keywords: E-Cigarettes, Smoking, Smoking relapse, Quit smoking, PATH study, Adults
1. Introduction
Smoking cessation rates in the U.S. remain low (Babb et al., 2017) with 7.4% of smokers reported successfully quitting smoking in 2015 due in part to underutilization of existing evidence-based smoking cessation treatments (Shiffman, 2010). Electronic cigarettes (e-cigarettes) may appeal to some smokers wishing to quit cigarettes who may not be attracted to other cessation aids. Similar to combustible cigarettes and dissimilar to most FDA-approved nicotine replacement therapies, e-cigarettes can rapidly deliver nicotine boluses to the bloodstream and offer a user experience of inhaling aerosols with pleasant tastes and other sensory effects (Breland et al., 2017). Research of e-cigarettes as a cessation tool has predominately examined whether smokers who concurrently use e-cigarettes are differentially likely to achieve abstinence from combustible cigarettes than smokers who do not use e-cigarettes. The results have yielded inconclusive evidence on the effectiveness of e-cigarettes (El Dib et al., 2017).
A separate question is whether e-cigarette use in former smokers prevents, precipitates, or has no effect on risk of protracted relapse back to combustible cigarette smoking. An estimated 2.4 million U.S. adults in 2015 who had previously quit smoking were current e-cigarette users (Phillips et al., 2017), which represent a mix of individuals who started vaping either prior to, shortly after, or long after quitting smoking. Because evidence suggests that e-cigarette aerosol is substantially less toxic than combustible cigarette smoking (National Academies of Sciences Engineering Medicine, 2018), switching from smoking to indefinite use of e-cigarettes may provide significant health benefits (Levy et al., 2018), particularly if post-quit e-cigarette vaping reduces odds of protracted smoking relapse by continuously satiating a long-standing desire to self-administer nicotine. Alternatively, persistent nicotine exposure in post-quit e-cigarette use could perpetuate vulnerability to smoking relapse that would otherwise be mitigated by ceasing use of tobacco products altogether and disrupting a cycle of nicotine addiction.
In this study, nationally-representative longitudinal data were analyzed to investigate whether e-cigarette use in former smokers was associated with lower, higher, or no difference in odds of relapse back to combustible cigarette smoking one year later. As prior evidence suggests that 12-months is an important threshold in determining future odds of relapse (Gilpin et al., 1997), associations were estimated separately for recent (≤12 months) and long-term (>12 months) quitters of combustible cigarettes at baseline to investigate odds of smoking relapse attributable to early and protracted post-quit e-cigarette use, respectively. Secondary outcomes addressed whether e-cigarette vaping differentiated the frequency or intensity of smoking in re-lapsers.
2. Methods
2.1. Data source
Data were obtained from the first two waves of the PATH study, a longitudinal cohort study of tobacco product use in U.S. civilian, noninstitutionalized individuals (United States Department of Health and Human Services, 2017) A four-stage, stratified probability sample design was used. A stratified sample of 156 geographical primary sampling units (PSUs) constituting a county or group of counties were first selected. Smaller geographical segments were then formed and sampled within each selected PSU at the second stage. The third stage sampled residential addresses within these segments. The fourth stage selected residents from the sampled households of these addresses, intentionally oversampling adult tobacco users, young adults, and African Americans. The weighted response rate for the Wave 1 household screener was 54.0%, of whom the weighted response rate for the baseline interview (September 2013 - December 2014) was 74.0% (N = 32,320 adults), and the weighted retention rate for resurveying at 12-month follow-up was 83.1% (October 2014 - October 2015; N = 28,362) (United States Department of Health and Human Services, 2017). Other details regarding the PATH study methods are presented elsewhere. This report used the public-use data files of participants aged >18 years. The study was conducted by Westat and approved by Westat’s Institutional Review Board.
2.2. Measures
At both waves, participants were asked about lifetime and current tobacco product use and other factors using a standardized in-person interview (United States Department of Health and Human Services, 2017).
2.1.1. Combustible cigarette use
Baseline former smoker status. Those who reported having ever smoked >100 combustible cigarettes and responded ‘not at all’ to the question ‘Do you now smoke cigarettes?’ at baseline were classified as former combustible cigarette smokers. Based on their response to ‘About how long has it been since you completely quit smoking cigarettes?’ baseline former smokers were classified as ‘recent quitters’ (smoked within the past 12 months) or ‘long-term quitters’ (last smoked >12 months ago), as in prior PATH study classifications (Coleman et al., 2017).
Follow-up outcomes. At follow-up, participants were asked, ‘Do you now smoke cigarettes?’ Those who responded ‘every day’ or ‘some days’ were classified positive (relapsers) and those responding ‘not at all’ were classified negative (abstainers) for the primary cigarette smoking relapse outcome. Among relapsers, frequency (number of days smoked in past 30 days) and intensity (average number of cigarettes smoked per day on days smoked in past 30 days) of current smoking at follow-up were secondary outcomes.
2.2.2. Baseline E-cigarette vaping
All participants were shown a brief description and pictures of e-cigarettes followed by a question, “Have you seen or heard of e-cigarettes before this study?” and those who responded “yes” were asked “Have you ever used an e-cigarette, even 1 or 2 times?” Those who responded “Yes” were asked “Have you ever used e-cigarettes fair regularly” and “Do you now use e-cigarettes?” We classified participants as never e-cigarette users (those who have never seen or heard or never used e-cigarettes), prior e-cigarette users (those who reported having ever used e-cigarettes and currently not using them at all), current occasional e-cigarette users (those who reported having ever used an e-cigarette, having never used fairly regularly, and using every day or some days), and current regular e-cigarette users (those who reported having ever used an e-cigarette, having used fairly regularly, and using some days or every day).
Since the publicly-accessible PATH study data omits e-cigarette use onset time and duration variables, we did not analyze the time interval between quitting smoking and starting vaping for each respondent.
2.2.3. Covariates
Baseline variables potentially associated with e-cigarette and smoking relapse liability were a priori as covariates based on the literature (Hartmann-Boyce et al., 2016).
Sociodemographics. Sociodemographic covariates included age (18–24, 25–34, 35–44, 45–54, 55–64, or 65 + ), sex (male/female), race/ethnicity (non-Hispanic white, Non-Hispanic black, Hispanic, or other Non-Hispanic classifications), education (less than high school, high school graduate, some college, or Bachelor’s degree or above), poverty level (self-reported income < 100%, 100–199%, ≥200%, or unknown in reference to the federal poverty level), region (Northeast, South, Midwest, West), and health insurance (yes/no).
Tobacco product use characteristics. Smoking chronicity based on lifetime years of smoking (excluding temporary periods of abstinence), typical number of combustible cigarettes smoked per day during the period of regular smoking, and length of time since quit smoking (months for recent quitters; years for long-term quitters) were covariates characterizing smoking history. Current regular use of other tobacco products was classified (yes/no). Non-e-cigarette tobacco product dependence was measured (in recent quitters only) by the Wisconsin Inventory of Smoking Dependence Motives (WISDM) Primary Dependence Motives scale (Piper et al., 2004; Smith et al., 2010), which collects agreement level (1–5 scale) ratings to self-statements indicative of habitual and heavy tobacco product use, loss of control over use, and craving. As in prior work (Strong et al., 2017), a dependence severity score was calculated as the mean response to the 8 items.
Responses to questions (administered to recent quitters only) regarding past-year use of cessation aids, were operationalized as three variables (pharmacotherapy [yes/no]; Support of friends/family [yes/ no]; Tobacco cessation counseling [yes/no]).
2.3. Data analysis
Descriptive analyses involved reporting study accrual and comparing those included vs. excluded from the analytic sample by baseline e-cigarette use status using Rao-Scott Chi-square tests. Also reported were descriptive statistics and comparisons of covariates amongst shortterm and long-term quitters with Rao-Scott X2 and ANOVA tests for categorical and continuous variables, respectively. Further descriptive results between e-cigarette use groups within recent and long-term quitters were reported using the same strategy.
For the main analysis, logistic regression was used to estimate the association of baseline e-cigarette use status (Never, Prior, Current Occasional, and Current Regular) and covariates with smoking relapse (relapser vs. abstainer) at follow-up. Odds ratios (ORs) in the univariate analysis and adjusted odds ratios (AORs) in the multivariable analysis were reported along with 95% confidence intervals (CIs). For secondary outcomes, linear regression models were tested in subsamples of re-lapsers to obtain regression coefficients (b values) and 95% CIs for associations of the baseline e-cigarette use with frequency and intensity of cigarette smoking at follow-up. For each model, separate analyses were performed in the subsamples of baseline recent and long-term quitters and both univariable (unadjusted) and multivariable (adjusted) regression models that included all available covariates as simultaneous regressors were tested.
Statistical analyses were performed with SAS 9.4 (Cary, NC) using replicate weights and the balanced repeated replication method with Fay’s adjustment = 0.3 to account for the PATH study’s complex design (Judkins, 1990; McCarthy, 1969). Per recommendations, sampling weights from the follow-up were used to weight results to the 2010 U.S. Census population profile. The analytic sample included only former smokers with baseline vaping and follow-up smoking relapse data. Missing covariate data was addressed in the multivariable models using multiple imputation (Rubin, 2004). Missing data observations ranged from 1(0.11%) to 15(1.70%) and 1(0.03%) to 17(0.53%) across covariates for short-term and long-term quitters, respectively. Tests were two-sided.
Since e-cigarette devices, reasons for e-cigarette use, e-cigarette use frequency, and the duration of smoking abstinence could be additional factors related to smoking relapse cessation (Glasser et al., 2017; Herd et al., 2009), we conducted sensitivity analysis in the supplemental document.
3. Results
3.1. Descriptive analyses
Fig. 1 summarizes the sample size and selection criteria in the final analysis. Baseline former smokers without follow-up smoking relapse data (n = 820) and the combined analytic sample of long-term and short-term quitters (n = 4094) did not differ on baseline e-cigarette use (p = .17), years of regular smoking (p = .71), cigarettes smoked per day while smoking (p = .28), tobacco nicotine dependence (p = .63), and months since quit smoking p = .07).
Fig. 1.
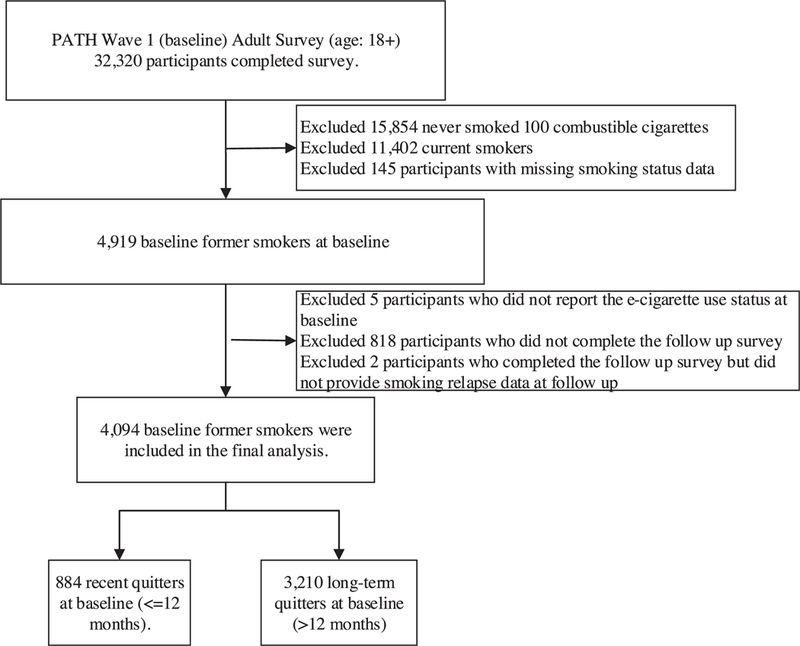
Flowchart for participants included in the final analytic sample.
Illustrated in Table 1, recent (vs. long-term) quitters had higher proportions of baseline prior (34.7% vs. 7.3%), current occasional (5.0% vs. 0.5%), and current regular (17.6% vs. 1.2%) e-cigarette use (X2 = 1337.0, p < .001). Recent (vs. long-term) quitters had higher proportions of respondents who were younger, female, with incomes below the national poverty line, of non-white race/ethnicity, did not attain Bachelor’s degree or above, and did not have health insurance. Recent (vs. long-term) quitters had a higher prevalence of current regular use of other (non-e-cigarette) tobacco products and reported fewer cigarettes smoked per day when smoking.
Table 1.
Baseline e-cigarette vaping status and sample characteristics, by duration of baseline smoking abstinencea.
| Quit smoking within the prior 12 months (n = 884) |
Quit smoking longer than 12 months ago (n = 3210) |
P-Value | |||
|---|---|---|---|---|---|
| n | Weighted % (95% CI)b or Median (IQR) | n | Weighted % (95% CI)b or Median (IQR) | ||
| E-Cigarette Vaping Status, % (95% CI) | |||||
| Never Use | 233 | 42.7 (38.0 to 47.7) | 2,479 | 91.0 (90.0 to 92.0) | < .001c |
| Prior Use | 399 | 34.7 (30.8 to 38.8) | 588 | 7.3 (6.4 to 8.2) | |
| Current Occasional Use | 56 | 5.0 (3.8 to 6.7) | 45 | 0.5 (0.3 to 0.8) | |
| Current Regular Use | 196 | 17.6 (14.9 to 20.6) | 98 | 1.2 (0.9 to 1.6) | |
| Sociodemographics, % (95% CI) | |||||
| Age | |||||
| 18–24 | 246 | 16.5 (13.9 to 19.4) | 163 | 1.5 (1.1 to 1.9) | < .001c |
| 25–34 | 246 | 27.1 (23.2 to 31.6) | 516 | 9.5 (8.3 to 10.7) | |
| 35–44 | 150 | 17.0 (14.2 to 20.4) | 519 | 12.9 (11.6 to 14.2) | |
| 45–54 | 111 | 16.3 (13.1 to 19.9) | 564 | 17.5 (15.9 to 19.3) | |
| 55–64 | 86 | 14.4 (10.4 to 19.6) | 666 | 23.6 (21.7 to 25.6) | |
| 65 + | 45 | 8.6 (5.8 to 12.7) | 782 | 35.1 (32.9 to 37.3) | |
| Sex | |||||
| Male | 413 | 46.9 (42.7 to 51.0) | 1,829 | 54.1 (52.3 to 55.9) | .003c |
| Female | 471 | 53.1 (49.0 to 57.3) | 1,381 | 45.9 (44.1 to 47.7) | |
| Race/ethnicity | |||||
| Non-Hispanic White | 621 | 73.9 (69.9 to 77.6) | 2,445 | 80.8 (79.2 to 82.3) | .004c |
| Non-Hispanic Black | 76 | 7.8 (5.9 to 10.4) | 236 | 5.9 (5.0 to 6.9) | |
| Hispanic | 116 | 11.9 (9.1 to 15.3) | 315 | 8.3 (7.4 to 9.4) | |
| Other | 71 | 6.4 (4.8 to 8.4) | 214 | 5.0 (4.1 to 6.1) | |
| Education | |||||
| Less than high school | 84 | 11.1 (8.3 to 14.5) | 248 | 8.1 (7.0 to 9.5) | < .001c |
| High school graduate | 263 | 33.7 (29.1 to 38.6) | 690 | 28.8 (27.0 to 30.6) | |
| Some College | 387 | 37.2 (33.1 to 41.6) | 1,189 | 32.1 (30.5 to 33.8) | |
| Bachelor’s degree or above | 150 | 18.0 (14.7 to 21.9) | 1,072 | 31.0 (29.3 to 32.7) | |
| Household income | |||||
| Below poverty line | 241 | 24.6 (20.7 to 28.9) | 429 | 11.2 (10.0 to 12.5) | < .001c |
| 100%−200% poverty line | 196 | 20.9 (18.1 to 24.1) | 662 | 20.3 (18.4 to 22.2) | |
| > 200% poverty line | 369 | 44.1 (39.9 to 48.4) | 1,851 | 57.5 (55.4 to 59.7) | |
| Unknown | 78 | 10.4 (8.1 to 13.3) | 268 | 11.0 (9.6 to 12.5) | |
| Health insurance | 710 | 81.9 (78.1 to 85.2) | 2,886 | 93.2 (92.1 to 94.1) | < .001c |
| Region of residence | |||||
| Northeast | 118 | 16.2 (12.6 to 20.6) | 524 | 19.1 (17.5 to 21.0) | .18c |
| South | 243 | 24.9 (21.8 to 28.2) | 799 | 22.6 (20.4 to 24.9) | |
| Midwest | 329 | 37.7 (32.9 to 42.7) | 1,067 | 34.1 (31.9 to 36.3) | |
| West | 194 | 21.2 (17.4 to 25.7) | 820 | 24.2 (21.8 to 26.8) | |
| Current regular use of other tobacco productse | 120 | 9.9 (8.0 to 12.1) | 507 | 6.6 (5.8 to 7.5) | .001c |
| Smoking characteristics, Median (IQR) | |||||
| Time since quit smoking (months/years)f | 5.5 (2.0 to 11.8) | 18.7 (8.0 to 29.9) | < .001d | ||
| Years of regular smoking | 11.0 (3.3 to 25.9) | 10.9 (3.9 to 24.0) | .17d | ||
| Cigarettes smoked per day while smoking | 11.9 (5.3 to 19.2) | 15.0 (5.4 to 19.8) | < .001d | ||
| WISDM tobacco dependence scoreg | 1.2 (1.0 to 1.9) | – | – | ||
| Relapse at follow-up, % (95% CI) | 335 | 35.2 (31.2 to 39.4) | 157 | 2.6 (2.1 to 3.2) | < .001c |
Abbreviations: WISDM, Wisconsin Inventory of Smoking Dependence Motives; –, not available in long-term quitters in PATH survey.
Estimates weighted to reflect the sociodemographic population in the 2010 Census.
From Rao-Scott Chi-square test comparing variable status between recent and long-term quitters.
From ANOVA test comparing variable level between recent and long-term quitters.
Current regular use of traditional cigars, cigarillos, filtered cigars, pipe, hookah, smokeless tobacco, snus, and dissolvable tobacco.
Expressed in months for recent quitters and years in long-term quitters.
Based on an average of 8 items indicating automaticity, craving, loss of control, and tolerance tobacco dependence symptoms experienced for non-e-cigarette tobacco products. Each item is scored from 1 to 5 with higher score indicating more severe tobacco dependence.
There were several differences in sociodemographics and tobacco product use by e-cigarette use among recent and long-term quitters at baseline (Supplementary Tables 1–3). Of note, e-cigarette use was associated shorter duration since quit, younger age, current other tobacco product use, and other factors.
3.2. Association of baseline E-cigarette use with smoking relapse at follow-up
3.2.1. Respondents that quit smoking within the 12 months prior to baseline
Among recent quitters at baseline, smoking relapse prevalence at follow-up was 31.6%, 39.0%, 51.6%, and 31.9% among never, prior, current occasional, and current regular baseline e-cigarette users, respectively. Prior (AOR, 1.34 [95% Cl, 0.78–2.29]), current occasional (AOR, 1.92 [Cl, 0.84–4.40]), and current regular use (AOR, 1.00 [Cl, 0.57–1.75]) of e-cigarettes at baseline were not associated with smoking relapse at follow-up after covariate adjustments.
Associations of covariates with smoking relapse are reported in Table 2 and Supplementary Table 4. Smoking relapse at follow-up was associated with younger age, less time of time since quitting, and higher tobacco dependence severity but was not associated with use of other smoking cessation aids.
Table 2.
Association of baseline e-cigarette vaping and covariates with current smoking relapse at follow-up, by baseline duration of smoking abstinencea.
| Baseline regressor | Relapse at follow-up in those who quit smoking within the prior 12 months at baseline (n=884) |
Relapse at follow-up in those who quit smoking longer than 12 months ago at baseline (n=3210) |
||||
|---|---|---|---|---|---|---|
| Prevalence % (95% CI)b |
Unadjusted OR (95% CI)c |
Adjusted OR (95% CI)d |
Prevalence % (95% CI)b |
Unadjusted OR (95% CI)c |
Adjusted OR (95% CI)d |
|
| E-cigarette vaping | ||||||
| Never Use | 31.6 (23.9 to 40.5) | Reference | Reference | 1.8 (1.3 to 2.4) | Reference | Reference |
| Prior Use | 39.0 (33.8 to 44.4) | 1.38 (0.83 to 2.30) | 1.34 (0.78 to 2.29) | 10.4 (8.2 to 13.2) | 6.36 (4.49 to 9.00) | 2.00 (1.25 to 3.20) |
| Current Occasional Use | 51.6 (36.2 to 66.7) | 2.31 (1.17 to 4.54) | 1.92 (0.84 to 4.40) | 9.6 (3.5 to 23.5) | 5.79 (1.50 to 22.33) | 1.56 (0.34 to 7.14) |
| Current Regular Use | 31.9 (25.8 to 38.7) | 1.02 (0.66 to 1.57) | 1.00 (0.57 to 1.75) | 15.0 (8.8 to 24.6) | 9.68 (4.74 to 19.75) | 3.77 (1.48 to 9.65) |
| Categorical covariates | ||||||
| Use quit smoking pharmacotherapye | ||||||
| No | 35.4 (31.2 to 39.8) | Reference | Reference | – | – | – |
| Yes | 33.6 (25.6 to 42.7) | 0.93 (0.60 to 1.43) | 0.87 (0.54 to 1.40) | – | – | – |
| Obtained social support to assist quittingf | ||||||
| No | 34.9 (30.0 to 40.1) | Reference | Reference | – | – | – |
| Yes | 36.5 (30.0 to 43.5) | 1.07 (0.73 to 1.58) | 0.96 (0.63 to 1.47) | – | – | – |
| Tobacco cessation counselingg | ||||||
| No | 35.1 (31.1 to 39.4) | Reference | Reference | – | – | – |
| Yes | 37.9 (20.8 to 58.8) | 1.13 (0.44 to 2.92) | 1.46 (0.62 to 3.41) | – | – | – |
| Current regular use of other tobacco productsh | ||||||
| No | 34.0 (29.8 to 38.6) | Reference | Reference | 2.2 (1.7 to 2.8) | Reference | Reference |
| Yes | 46.2 (36.9 to 55.8) | 1.66 (1.07 to 2.59) | 1.44 (0.90 to 2.31) | 8.3 (6.2 to 11.0) | 4.00 (2.75 to 5.82) | 2.44 (1.51 to 3.95) |
| Continuous covariates | ||||||
| Time since quit smoking (months/years)i | 0.88 (0.84 to 0.92) | 0.88 (0.84 to 0.92) | 0.89 (0.86 to 0.92) | 0.91 (0.87 to 0.96) | ||
| Years of regular smoking | 0.99 (0.98 to 1.00) | 1.00 (0.97 to 1.02) | 0.98 (0.97 to 1.00) | 0.98 (0.96 to 1.01) | ||
| Cigarettes smoked per day while smoking | 0.99 (0.98 to 1.00) | 0.99 (0.98 to 1.01) | 1.00 (0.99 to 1.02) | 1.01 (1.00 to 1.01) | ||
| WISDM tobacco dependence scorej | 1.29 (1.09 to 1.51) | 1.23 (1.02 to 1.47) | – | – | ||
| Demographic covariates | ||||||
| Age: | ||||||
| 18–24 | 45.2 (39.1 to 51.5) | Reference | Reference | 15.7 (10.2 to 23.4) | Reference | Reference |
| 25–34 | 32.5 (27.0 to 38.6) | 0.58 (0.42 to 0.82) | 0.59 (0.38 to 0.92) | 8.3 (5.7 to 11.9) | 0.48 (0.25 to 0.95) | 0.75 (0.38 to 1.49) |
| 35–44 | 38.6 (29.5 to 48.7) | 0.76 (0.46 to 1.25) | 0.92 (0.49 to 1.72) | 4.6 (3.0 to 7.1) | 0.26 (0.13 to 0.52) | 0.67 (0.33 to 1.38) |
| 45–54 | 30.9 (19.6 to 45.3) | 0.55 (0.27 to 1.11) | 0.68 (0.26 to 1.80) | 1.7 (0.9 to 3.2) | 0.09 (0.04 to 0.22) | 0.39 (0.14 to 1.09) |
| 55–64 | 21.5 (12.8 to 33.7) | 0.33 (0.16 to 0.68) | 0.36 (0.13 to 1.01) | 2.0 (1.1 to 3.3) | 0.11 (0.05 to 0.24) | 0.71 (0.26 to 1.95) |
| 65 + | 48.6 (31.2 to 66.3) | 1.15 (0.49 to 2.66) | 1.40 (0.34 to 5.81) | 0.7 (0.3 to 1.6) | 0.04 (0.02 to 0.10) | 0.44 (0.09 to 2.06) |
| Sex: | ||||||
| Male | 33.8 (28.4 to 39.6) | Reference | Reference | 2.8 (2.2 to 3.7) | Reference | Reference |
| Female | 36.4 (30.2 to 43.2) | 1.13 (0.75 to 1.69) | 1.30 (0.84 to 2.02) | 2.4 (1.7 to 3.3) | 0.84 (0.52 to 1.36) | 0.96 (0.58 to 1.60) |
| Race/ethnicity | ||||||
| Non-Hispanic White | 34.3 (29.3 to 39.6) | Reference | Reference | 2.1 (1.6 to 2.8) | Reference | Reference |
| Non-Hispanic Black | 41.7 (29.2 to 55.4) | 1.37 (0.74 to 2.56) | 1.10 (0.52 to 2.31) | 6.2 (3.4 to 11.2) | 3.01 (1.47 to 6.18) | 2.65 (1.21 to 5.8.0) |
| Hispanic | 36.9 (26.4 to 48.8) | 1.12 (0.63 to 1.99) | 0.91 (0.48 to 1.72) | 4.8 (2.6 to 8.7) | 2.32 (1.15 to 4.68) | 1.66 (0.68 to 4.03) |
| Other | 34.9 (21.5 to 51.2) | 1.03 (0.47 to 2.23) | 1.12 (0.47 to 2.71) | 2.3 (1.0 to 5.4) | 1.09 (0.53 to 2.25) | 0.68 (0.30 to 1.57) |
| Education | ||||||
| Less than high school | 47.0 (33.0 to 61.5) | Reference | Reference | 3.1 (1.5 to 6.0) | Reference | Reference |
| High school graduate | 34.8 (27.0 to 43.4) | 0.59 (0.28 to 1.27) | 0.65 (0.30 to 1.43) | 2.4 (1.5 to 3.8) | 0.77 (0.33 to 1.78) | 0.82 (0.31 to 2.19) |
| Some College | 32.2 (26.5 to 38.5) | 0.53 (0.26 to 1.06) | 0.57 (0.27 to 1.22) | 3.0 (2.1 to 4.3) | 0.99 (0.43 to 2.29) | 0.81 (0.28 to 2.32) |
| Bachelor’s degree or above | 35.0 (25.3 to 46.1) | 0.60 (0.26 to 1.40) | 0.84 (0.32 to 2.19) | 2.3 (1.6 to 3.4) | 0.76 (0.34 to 1.67) | 0.90 (0.29 to 2.77) |
| Household income | ||||||
| Below poverty line | 37.3 (29.8 to 45.5) | Reference | Reference | 3.8 (2.3 to 6.0) | Reference | Reference |
| 100%−200% poverty line | 40.3 (31.5 to 49.7) | 1.13 (0.66 to 1.94) | 1.43 (0.83 to 2.46) | 3.4 (2.2 to 5.1) | 0.89 (0.49 to 1.61) | 1.22 (0.63 to 2.34) |
| > 200% poverty line | 31.1 (24.6 to 38.3) | 0.76 (0.47 to 1.21) | 0.90 (0.54 to 1.47) | 2.3 (1.7 to 3.1) | 0.61 (0.37 to 1.00) | 1.00 (0.46 to 2.20) |
| Unknown | 37.6 (24.7 to 52.5) | 1.03 (0.50 to 2.10) | 1.00 (0.47 to 2.12) | 1.7 (0.7 to 4.0) | 0.43 (0.19 to 0.96) | 0.87 (0.35 to 2.20) |
| Health insurance: | ||||||
| Yes | 33.7 (29.1 to 38.6) | Reference | Reference | 2.5 (2.0 to 3.2) | Reference | Reference |
| No | 39.9 (29.8 to 50.9) | 1.30 (0.77 to 2.22) | 1.33 (0.74 to 2.40) | 4.1 (2.3 to 7.0) | 1.63 (0.91 to 2.93) | 0.63 (0.31 to 1.28) |
| Region of residence | ||||||
| Northeast | 32.2 (20.3 to 47.1) | Reference | Reference | 2.4 (1.4 to 4.3) | Reference | Reference |
| South | 32.6 (27.1 to 38.8) | 1.03 (0.50 to 2.10) | 1.05 (0.47 to 2.33) | 2.5 (1.6 to 3.8) | 1.01 (0.46 to 2.19) | 0.89 (0.40 to 1.97) |
| Midwest | 39.4 (33.1 to 46.2) | 1.37 (0.67 to 2.81) | 1.45 (0.67 to 3.14) | 3.0 (2.1 to 4.2) | 1.22 (0.62 to 2.38) | 0.93 (0.44 to 2.00) |
| West | 32.9 (25.3 to 41.6) | 1.03 (0.49 to 2.20) | 0.99 (0.43 to 2.26) | 2.4 (1.6 to 3.7) | 1.00 (0.46 to 2.15) | 0.76 (0.33 to 1.78) |
Abbreviations: WISDM, Wisconsin Inventory of Smoking Dependence Motives; –, not available in long-term quitters in PATH survey. Statistically significant confidence intervals of OR and AOR are in bold.
Estimates weighted to reflect the sociodemographic population in the 2010 Census.
Estimate of association in univariable logistic regression model.
Estimate of association in multivariable logistic regression model involving each variable listed in the table as simultaneous regressors as well as adjustment for sociodemographic covariates, including age, sex, race/ethnicity, education, household income, health insurance, and region (estimates for sociodemographic covariates can be found in Supplementary Table 4).
Used a nicotine patch, gum, inhaler, nasal spray, lozenge, or other pharmacotherapy when last tried to quit smoking/using tobacco product(s) in past 12 months.
Relied on support of friends and family to help when last tried to quit smoking /using tobacco product(s) in past 12 months.
Used counseling, telephone help line, books, pamphlets, videos, quit tobacco clinic, class, support group or web-based program to help when last tried to quit smoking/using tobacco product(s) in past 12 months.
Current regular use of traditional cigars, cigarillos, filtered cigars, pipe, hookah, smokeless tobacco, snus, or dissolvable tobacco.
Expressed in months for recent quitters and years for long-term quitters.
WISDM primary dependence score, rescaled (M = 0, SD = 1) and standardized to the analytic subsample of recent-quitters. Based on sum of responses to 8 items of automaticity, craving, loss of control, and tolerance-related expressions of tobacco dependence.
3.2.2. Respondents that quit smoking longer than 12 months before baseline
Among long-term quitters at baseline, the prevalence of smoking relapse at follow-up was 1.8%, 10.4%, 9.6% and 15.0% among never, prior, current occasional, and current regular baseline e-cigarette users, respectively. Smoking relapse at follow-up was significantly higher in baseline current regular (vs. never) e-cigarette users (AOR, 2.00 [CI, 1.25–3.20]; difference in prevalence, 13.2% [CI, 5.2%–21.3%]) and prior (vs. never) e-cigarette users (AOR, 3.77 [CI, 1.48–9.65]; difference in prevalence, 8.6%[CI, 7.0%−10.2%]); Relapse at follow-up was significantly higher in baseline current occasional vs. never e-cigarette users before (OR, 5.79 [CI, 1.50–22.33]), but not after, covariate adjustment (AOR, 1.56 [CI, 0.34–7.14]) (Table 2).
Other tobacco product use, non-Hispanic black (vs. white) race/ ethnicity, and less time since quitting covariates were associated with smoking relapse (Table 2). Other than non-Hispanic black race/ethnicity, each of these covariates was associated with e-cigarette use and may account for the reduction in the e-cigarette use OR estimate after covariate adjustment.
3.3. Association of baseline E-cigarette vaping with combustible cigarette smoking frequency and intensity among relapsers at follow-up
Among baseline recent quitters who relapsed at follow-up (N = 335), mean (CI) number of days smoked within the past month (frequency) and cigarettes per day on smoking day (intensity) at follow-up did not significantly differ across baseline never (frequency, 21.3 [CI, 18.1–24.4]; intensity: 7.1 [CI 5.0–9.2], prior (20.5 [18.9–22.2]; 7.7 [6.3–9.1]), current occasional (20.1 [15.2–25.0]; 6.2 [4.2–8.2]), and current regular (22.1 [18.9–25.2]; 8.8 [7.1–10.4]) e-cigarette users with and without covariate adjustment (Table 3). Analyses of baseline long-term quitters who relapsed at follow-up (N = 157) also found no differences in smoking frequency or intensity by baseline e-cigarette use status (Table 3).
Table 3.
Association of baseline e-cigarette use with current combustible smoking frequency and intensity at follow-up in relapsers, by baseline duration of smoking abstinence.
| E-cigarette Use at Baseline | Number of days smoked cigarettes in past 30 days at follow-up (smoking frequency) |
Number of cigarettes smoked per day on smoking day in past 30 days at follow-up (smoking intensity) |
||||
|---|---|---|---|---|---|---|
| Mean (95%CI)a | Unadjusted Coefficient (95% CI)b | Adjusted Coefficient (95% CI)c | Mean (95%CI)a | Unadjusted Coefficient (95% CI)b | Adjusted Coefficient (95% CI)c | |
| In those quit smoking within the prior 12 months at baseline (n = 335) | ||||||
| Never use (n = 85) | 21.3(18.1 to 24.4) | Reference | Reference | 7.1(5.0 to 9.2) | Reference | Reference |
| Prior use (n = 156) | 20.5(18.9 to 22.2) | −0.73 (−4.27 to 2.82) | −0.68 (−3.83 to 2.47)d | 7.7(6.3 to 9.1) | 0.56 (−1.81 to 2.93) | −1.47 (−3.49 to 0.55)d |
| Current occasional use (n = 30) | 20.1(15.2 to 25.0) | −1.15 (−7.22 to 4.92) | −1.79 (−7.79 to 4.20)d | 6.2(4.2 to 8.2) | −0.95 (−3.80 to 1.90) | −1.76 (−3.89 to 0.37)d |
| Current regular use (n = 64) | 22.1(18.9 to 25.2) | 0.79 (−3.57 to 5.16) | −0.52 (−4.06 to 3.02)d | 8.8(7.1 to 10.4) | 1.62 (−1.02 to 4.27) | −0.78 (−3.02 to 1.45)d |
| In those who quit smoking longer than 12 months ago at baseline (n = 157) | ||||||
| Never use (n = 99) | 12.7(9.5 to 16.0) | Reference | Reference | 5.8(3.7 to 7.8) | Reference | Reference |
| Prior use (n = 84) | 14.7(11.2 to 18.2) | 1.97 (−2.94 to 6.89) | 1.28 (−4.09 to 6.65) | 5.8(3.5 to 8.1) | 0.01 (−3.36 to 3.37) | −1.60 (−4.96 to 1.75) |
| Current use (n = 26)e | 12.6(6.2 to 18.9) | −0.17 (−7.09 to 6.75) | 0.48 (−6.65 to 7.60) | 6.1(3.0 to 9.3) | 0.38 (−3.13 to 3.89) | −0.30 (−4.30 to 3.69) |
Estimates weighted to reflect the sociodemographic population in the 2010 Census.
Estimate of association in univariable linear regression model.
Estimate of association in multivariable linear regression model adjusting for baseline age, sex, race/ethnicity, education, poverty, health insurance, region, years of regular smoking, cigarettes smoked per day when smoking, and time since quit smoking as covariates (estimates for covariates not shown).
Additionally adjusted for covariates available in recent quitters only, including use of pharmacotherapy, counseling, or social support as a cessation aid, and Wisconsin Inventory of Smoking Dependence Motives tobacco dependence score (estimates for covariates not presented).
Current use (occasional and regular use collapsed into singe groups due to low frequencies).
3.4. Sensitivity analyses
Sensitivity analyses found no evidence that associations between baseline e-cigarette vaping and smoking relapse at follow-up were influenced by variation in e-cigarette device characteristics and nicotine concentration used, whether respondents reported using e-cigarette for the purpose of quitting smoking, the application of more granular distinctions of daily vs. non-daily e-cigarette use frequency or length of time since quit smoking at baseline, and respondent age (results detailed in the sensitivity analysis in the Online Supplement).
4. Discussion
This analysis of nationally-representative data provides new evidence that e-cigarette vaping more than a year after stopping smoking is associated with increased risk of future smoking relapse. The association followed a gradient—smoking relapse likelihood at one-year follow-up was lowest in baseline never-vapers, moderate in baseline prior or current occasional vapers, and highest in baseline current regular vapers. In baseline former smokers who quit within the prior year, e-cigarette vaping status was not associated with subsequent smoking relapse. Results of secondary smoking frequency and intensity outcomes did not find that post-quit e-cigarette use was associated with different patterns of combustible cigarette smoking in relapsers.
The difference in associations of e-cigarette use predicting subsequent smoking relapse in recent quitters and long-term quitters may be due to several factors. Current e-cigarette vaping was fairly common within the first 12-months after quitting while vaping was far less common in long-term former smokers. E-cigarette use among recent quitters may reflect individuals who started vaping before or shortly after quitting smoking. Since the rate of smoking relapse is typically high among this group (Herd et al., 2009), e-cigarette use might not be a risk factor for smoking relapse. It is also noteworthy that current occasional vapers at baseline had the highest prevalence of relapse at follow up among recent quitters though the association was not significant after covariate adjustment. Additional analyses (see Supplementary Table 3) show that this group had the highest nicotine dependence and the shortest months since quit smoking at baseline, which could explain the increased risk of relapse among current occasional vapers. Alternatively, e-cigarette users among long-term quitters could include some individuals with no intention of using nicotine prior to the arrival of e-cigarettes to the marketplace. The distribution of years since quitting smoking at baseline (see Supplementary Table 3) suggest that many long-term former smokers who used e-cigarettes had quit smoking years before e-cigarettes sales in the U.S. started picking up in 2009 (Regan et al., 2013). Thus, e-cigarette use might simply be a marker of nicotine intake among long-term quitters and increases the risk of smoking relapse.
Additional analyses (see Supplement Table 4) show that former smokers who used rechargeable e-cigarette devices had a lower prevalence of relapse than those who did not though the associations attenuated to be insignificant. Given the differences in device type to deliver nicotine and assist in smoking cessation (Glasser et al., 2017), more research is needed to assess whether e-cigarette devices could impact the relapse risk.
The failure to find evidence that vaping reduced smoking relapse risk in this study may have several explanations. Former smokers with the highest relapse risk may have the most chronic and recent histories of smoking or have other fundamental characteristics that differ from those with low relapse risk (Herd et al., 2009). Such factors may be indicative of a willingness to use any product to keep from smoking or a particularly strong drive for nicotine intake. We attempted to address these confounds by statistically adjusting for tobacco product use history, use of other cessation aids, and various sociodemographic factors. While the association estimate remained significant among long-term quitters, it was substantially reduced after covariate adjustment. Time since quit smoking markedly differed by e-cigarette use and was associated with relapse (Table 2), prompting sensitivity analyses which found no significant interaction between the duration of smoking abstinence and e-cigarette use level. These results suggest that the vaping-relapse association did not significantly vary by months since quitting. Thus, it is possible that the association between vaping and subsequent relapse may generalize across those who quit decades ago and those who may have quit within the past several years. Still, it is possible that unmeasured (and possibly unknown) confounds might affect post-quit vaping, smoking relapse, and their association.
Another explanation may be that e-cigarette vaping reduces relapse risk, but the effect was obscured here for reasons similar to the discordance in cessation outcomes observed for FDA-approved pharmacotherapies in controlled trials versus observational studies (Leas et al., 2017). Incidentally, we found no associations between the use of traditional cessation aids covariates and smoking relapse. Like evidence-based cessation treatments, a sufficient level of dosing may be necessary to derive clinical benefit from e-cigarettes. Prior research of e-cigarette use among current smokers (i.e., concurrent dual product use) tends to find more favorable combustible cigarette cessation outcomes in those who vape more frequently, use e-cigarettes with the expressed purpose of quitting smoking, and use e-cigarettes products that deliver more nicotine (Glasser et al., 2017). In contrast with extant findings in concurrent dual users, this study of former smokers found no evidence that e-cigarette product variation or reasons for e-cigarette use were associated with reduced odds of relapse. We further found that more frequent vaping was associated with poorer relapse outcomes in long-term former smokers. Whether any cessation-sustaining benefit derived from e-cigarettes may degrade or perhaps reverse when vaping occurs following extended smoking abstinence warrants future inquiry.
It is also plausible that post-quit vaping may perpetuate a vulnerability to smoking relapse that typically absolves after extended abstinence. Like combustible cigarettes, modern vaping products can produce pleasurable sensory effects and deliver rapid boluses of nicotine to the bloodstream (National Academies of Sciences Engineering Medicine, 2018). Vaping long after quitting smoking may rouse or propagate a compulsive urge to self-administer inhaled nicotine that originated from smoking, which could, in turn, increase the risk of relapse. Because this is an observational study, and one of the first to address smoking relapse in extended post-quit vaping, causal inferences cannot be made.
Even if future research demonstrates that extended post-quit vaping may play a causal role in heightening smoking relapse risk, the availability of e-cigarettes could still increase population quit rates pending the following circumstances. First, vaping remains uncommon in long-term former smokers (as observed here). Second, as suggested in a recent population trend analysis (Zhu et al., 2017), vaping encourages more smokers to make quit attempts, including smokers who otherwise may not have tried to quit if e-cigarettes were not available, even if their relapse rates are not improved by vaping.
This study had limitations. First, vaping and smoking relapse were not biochemically verified and subject to reporting and recall errors. Second, the PATH study methodology omitted assessment of some covariates in long-term former smokers and the onset date and duration of vaping from publicly assessable data. Third, attrition between PATH baseline and follow-up surveys may introduce biases. Fourth, small sample sizes for certain subgroups and for analyses of secondary smoking frequency and intensity outcomes in relapses produced wide CIs for some estimates.
5. Conclusions
In conclusion, e-cigarette vaping more than one year after having quit smoking was associated with increased odds of smoking relapse at 12-month follow-up in U.S. adults. Further research determining the causality of this association is warranted to inform whether extended post-quit vaping in long-term former smokers should be encouraged or potentially discouraged due to smoking relapse concerns.
Supplementary Material
Acknowledgments
Role of funding source
Research reported in this publication was supported by the National Cancer Institute and the FDA Center for Tobacco Products (CTP) under Award Number R03CA228909 (Dai) and Award Number U54CA180905 (Leventhal). The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH or the Food and Drug Administration.
Footnotes
Appendix A. Supplementary data
Supplementary material related to this article can be found, in the online version, at doi:https://doi.org/10.1016/j.drugalcdep.2019.01.043.
Conflict of interests
No conflict declared.
References
- Babb S, Malarcher A, Schauer G, Asman K, Jamal A, 2017. Quitting smoking among adults—United States, 2000–2015. MMWR Morb. Mortal. Wkly. Rep. 65, 1457–1464. [DOI] [PubMed] [Google Scholar]
- Breland A, Soule E, Lopez A, Ramoa C, El-Hellani A, Eissenberg T, 2017. Electronic cigarettes: what are they and what do they do? Ann. N. Y. Acad. Sci. 1394, 5–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coleman BN, Rostron B, Johnson SE, Ambrose BK, Pearson J, Stanton CA, Wang B, Delnevo C, Bansal-Travers M, Kimmel HL, Goniewicz ML, Niaura R, Abrams D, Conway KP, Borek N, Compton WM, Hyland A, 2017. Electronic cigarette use among US adults in the Population Assessment of Tobacco and Health (PATH) study, 2013–2014. Tob. Control 26, e117–e126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- El Dib R, Suzumura EA, Akl EA, Gomaa H, Agarwal A, Chang Y, Prasad M, Ashoorion V, Heels-Ansdell D, Maziak W, Guyatt G, 2017. Electronic nicotine delivery systems and/or electronic non-nicotine delivery systems for tobacco smoking cessation or reduction: a systematic review and meta-analysis. BMJ Open 7, e012680. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gilpin EA, Pierce JP, Farkas AJ, 1997. Duration of smoking abstinence and success in quitting. J. Natl. Cancer Inst. 89, 572–576. [DOI] [PubMed] [Google Scholar]
- Glasser AM, Collins L, Pearson JL, Abudayyeh H, Niaura RS, Abrams DB, Villanti AC, 2017. Overview of electronic nicotine delivery systems: a systematic review. Am. J. Prev. Med. 52, e33–e66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hartmann-Boyce J, McRobbie H, Bullen C, Begh R, Stead LF, Hajek P, 2016. Electronic cigarettes for smoking cessation. Cochrane Database Syst. Rev. 9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Herd N, Borland R, Hyland A, 2009. Predictors of smoking relapse by duration of abstinence: findings from the International Tobacco Control (ITC) four country survey. Addiction 104, 2088–2099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Judkins DR, 1990. Fay’s method for variance estimation. J. Off. Stat. 6, 223–239. [Google Scholar]
- Leas EC, Pierce JP, Benmarhnia T, White MM, Noble ML, Trinidad DR, Strong DR, 2017. Effectiveness of pharmaceutical smoking cessation aids in a nationally representative cohort of American smokers. J. Natl. Cancer Inst. 110, 1141. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levy DT, Borland R, Lindblom EN, Goniewicz ML, Meza R, Holford TR, Yuan Z, Luo Y, O’Connor RJ, Niaura R, 2018. Potential deaths averted in USA by replacing cigarettes with e-cigarettes. Tob. Control 27, 18–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCarthy PJ, 1969. Pseudoreplication: further evaluation and application of the balanced half-sample technique. Vital Health Stat. 2, 1–24. [PubMed] [Google Scholar]
- National Academies of Sciences, Engineering, and Medicine, Health and Medicine Division, 2018. Board on population health and public health practice, committee on the review of the health effects of electronic nicotine delivery systems In: Eaton DL, Kwan LY, Stratton K (Eds.), Public Health Consequences of E-Cigarettes. National Academies Press (US), Washington, DC: https://www.ncbi.nlm.nih.gov/books/NBK507171/. [PubMed] [Google Scholar]
- Phillips E, Wang TW, Husten CG, Corey CG, Apelberg BJ, Jamal A, Homa DM, King BA, 2017. Tobacco product use among adults - United States, 2015. MMWR Morb. Mortal. Wkly. Rep. 66, 1209–1215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Piper ME, Piasecki TM, Federman EB, Bolt DM, Smith SS, Fiore MC, Baker TB, 2004. A multiple motives approach to tobacco dependence: the Wisconsin Inventory of Smoking Dependence Motives (WISDM-68). J. Consult. Clin. Psychol. 72, 139–154. [DOI] [PubMed] [Google Scholar]
- Regan AK, Promoff G, Dube SR, Arrazola R, 2013. Electronic nicotine delivery systems: adult use and awareness of the ‘e-cigarette’ in the USA. Tob. Control 22, 19–23. [DOI] [PubMed] [Google Scholar]
- Rubin DB, 2004. Multiple Imputation for Nonresponse in Surveys. John Wiley and Sons. [Google Scholar]
- Shiffman S, 2010. Smoking-cessation treatment utilization: the need for a consumer perspective. Am. J. Prev. Med. 38, S382–384. 10.1016/j.amepre.2009.12.004. [DOI] [PubMed] [Google Scholar]
- Smith SS, Piper ME, Bolt DM, Fiore MC, Wetter DW, Cinciripini PM, Baker TB, 2010. Development of the brief Wisconsin inventory of smoking dependence motives. Nicotine Tob. Res. 12, 489–499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Strong DR, Pearson J, Ehlke S, Kirchner T, Abrams D, Taylor K, Compton WM, Conway KP, Lambert E, Green VR, Hull LC, Evans SE, Cummings KM, Goniewicz M, Hyland A, Niaura R, 2017. Indicators of dependence for different types of tobacco product users: descriptive findings from wave 1 (2013–2014) of the Population Assessment of Tobacco and Health(PATH) study. Drug Alcohol Depend. 178, 257–266. [DOI] [PubMed] [Google Scholar]
- United States Department of Health and Human Services, National Institutes of Health, National Institute on Drug Abuse and United States Department Of Health and Human Services, Food And Drug Administration, Center For Tobacco Products, 2017. Population Assessment of Tobacco and Health (PATH) Study [United States] Public-Use Files. Inter-University Consortium for Political and Social Research, Ann Arbor, MI: 10.3886/icpsr36498.V6. [DOI] [Google Scholar]
- Zhu SH, Zhuang YL, Wong S, Cummins SE, Tedeschi GJ, 2017. E-Cigarette use and associated changes in population smoking cessation: evidence from us current population surveys. BMJ 358, j3262. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


