Abstract
Introduction:
Rotator cuff tears are one of the most common injuries worldwide, yet it is difficult to predict which patients will have poor outcomes after arthroscopic rotator cuff repair (RCR). The purpose of this study was to identify an association between preoperative vitamin D (25D) levels and postoperative complications in arthroscopic RCR.
Methods:
From a national claims database, patients undergoing arthroscopic RCR with preoperative 25D levels were reviewed. Patients were stratified into 25D-sufficient (≥20 ng/dL) or 25D-deficient (<20 ng/dL) categories and examined for development of postoperative complications. Multivariate logistic regression was performed using age, sex, and Charlson Comorbidity Index (CCI) as covariates. From this, risk-adjusted odds ratios (ORs) were calculated comparing complications between the two groups.
Results:
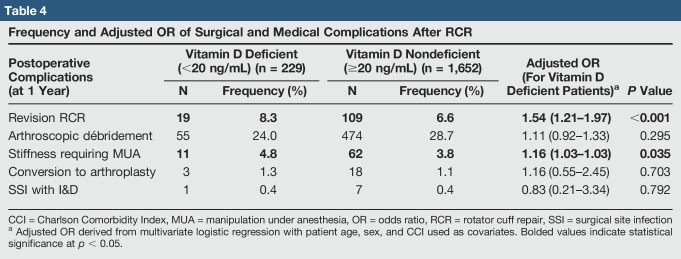
One thousand eight hundred eighty-one patients with measured preoperative 25D levels were identified; 229 patients were 25D deficient (12.2%). After adjusting for age, sex, and Charlson Comorbidity Index, 25D-deficient patients had increased odds of revision RCR (OR 1.54, 95% confidence interval 1.21 to 1.97, P < 0.001) and stiffness requiring manipulation under anesthesia (OR 1.16, 95% confidence interval 1.03 to 2.03, P = 0.035).
Conclusions:
Vitamin D deficiency is associated with a greater risk of postoperative surgical complications after arthroscopic RCR and may be a modifiable risk factor. Further investigation on preoperative vitamin D repletion is warranted.
Rotator cuff tears are one of the most common and costly injuries worldwide. Some studies estimate a prevalence of 20% to 34% in the asymptomatic general population with incidence increasing to 64% in patients with shoulder pain.1,2,3 As of 2002, these injuries accounted for over 4 million hospital visits and $560 million dollars in surgical expenses.4,5 Shoulder arthroscopy likely accounts for a notable portion of these expenses and remains the technique of choice for rotator cuff repair (RCR) given favorable, although variable, patient-reported and functional outcomes. Despite these positive results, studies have found a number of preoperative risk factors for arthroscopic RCR failure, ultimately drawing into question which patients are surgically optimal candidates.6
Recently, 25-hydroxyvitamin D (25D) has become a popular topic of investigation because its benefits to musculoskeletal health are believed to extend beyond bone mineralization. Studies have found that 25D deficiency may be associated with decreased bone and soft-tissue healing, as well as dysregulation of inflammatory biomarkers.7,8 Some studies have also found that 25D may have a role in preventing postoperative surgical site infection (SSI) because it is believed to have a role in upregulating wound closure and the innate immune system.8 Specifically, 25D interfaces with the vitamin D receptor to transcriptionally upregulate epidermal stem cells, phagocytosis, and other antimicrobial peptides.8,9 Together, this may effectively the minimize risk of SSI and supports the notion that repletion of 25D may be a modifiable perioperative risk factor to minimize adverse outcomes in surgery.8,9 Interestingly, a previous study by Hegde et al10 in 2016 supports this hypothesis because they noted that 25D deficiency was associated with an increased risk of adverse postoperative complications after total knee arthroplasty. However, to date, no studies have examined what role perioperative 25D levels have on outcomes in arthroscopic RCR.
The purpose of this study was to further explore the benefits of 25D in arthroscopic RCR by using a large administrative claims patient registry to examine the relationship between preoperative 25D levels and subsequent surgical complications. Given recent literature regarding the utility of 25D, it was hypothesized that low preoperative 25D levels would be associated with higher incidence of adverse outcomes after arthroscopic cuff repair.
Methods
The authors performed a retrospective study of administrative claims through the PearlDiver Patient Record Database (PearlDiver) to identify patients who underwent arthroscopic RCR. This commercially available database consists of roughly 20 million patient records from the nationwide health insurance provider, Humana. Diagnoses and procedures were queried using defined billing codes classified by the International Classification of Diseases, Ninth Revision (ICD-9), Current Procedural Terminology (CPT), and Logical Observation Identifiers Names and Codes.
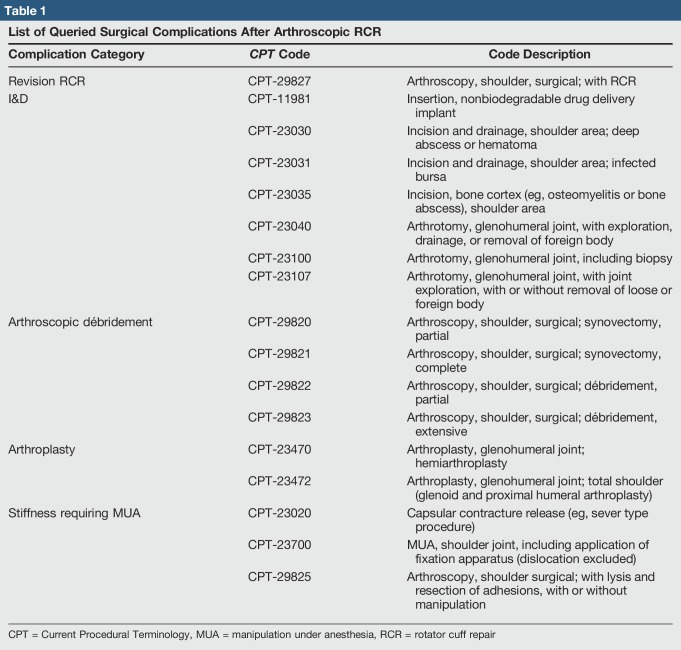
Patients who underwent arthroscopic RCR between 2007 and 2016 were identified using CPT-29827 (arthroscopy, shoulder, surgical; with RCR), with identification of preoperative plasma 25D levels (Logical Observation Identifiers Names and Codes-1989-3) within the 90 days preceding the procedure. Those who were 25D sufficient (≥20 ng/mL) were compared with those who were 25D deficient (<20 ng/mL) against a series of postoperative surgical complications using corresponding CPT codes (Table 1). 25D cutoffs were based on definitions established by the Institute of Medicine as criteria for diagnosis and treatment with repletion.11 Surgical complications included revision RCR, SSI requiring incision and drainage, arthroscopic débridement, revision to arthroplasty, and stiffness requiring manipulation under anesthesia (MUA). Patient demographics such as age (reported in 5-year groups), sex, geographic region, other medical comorbidities (using ICD-9 codes), and Charlson Comorbidity Index (CCI) were also collected (Table 2). The CCI is a well-validated metric for 1-year mortality using 22 medical conditions.12
Table 1.
List of Queried Surgical Complications After Arthroscopic RCR
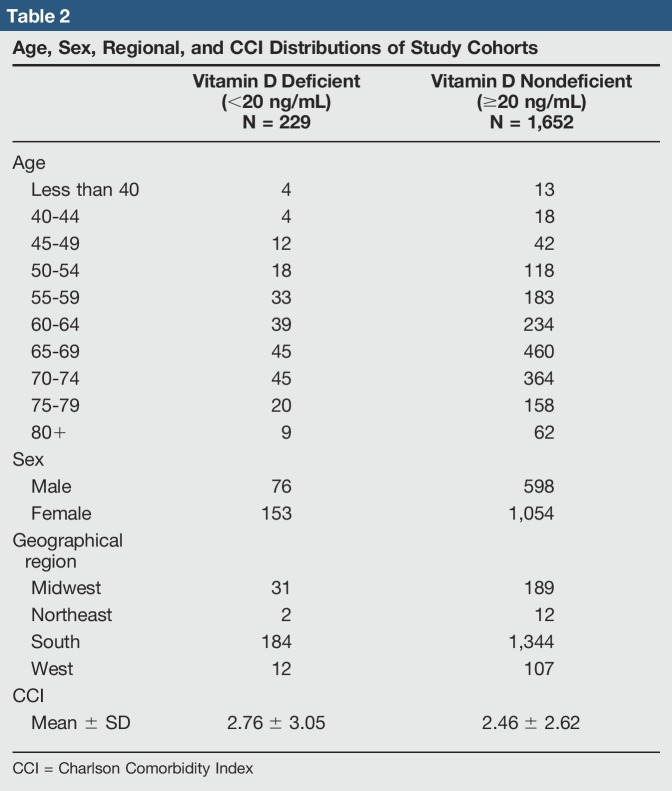
Table 2.
Age, Sex, Regional, and CCI Distributions of Study Cohorts
Inferential statistics comparing the baseline age, sex, regional, and comorbidity distributions of the two 25D-stratified cohorts was performed using chi-square analysis. A two-sided Student t-test was used to assess CCI between the two cohorts. Statistical significance was defined as P < 0.05. PearlDiver's statistics package was used to fit a multivariate logistic regression using age, sex, and CCI as covariates, and to calculate the adjusted odds ratios (ORs), 95% confidence intervals (CIs), and associated P-values for each surgical complication with 25D-deficient patients defined as the exposed group. All additional analysis was performed using SPSS version 21 software (IBM Corp).
Results
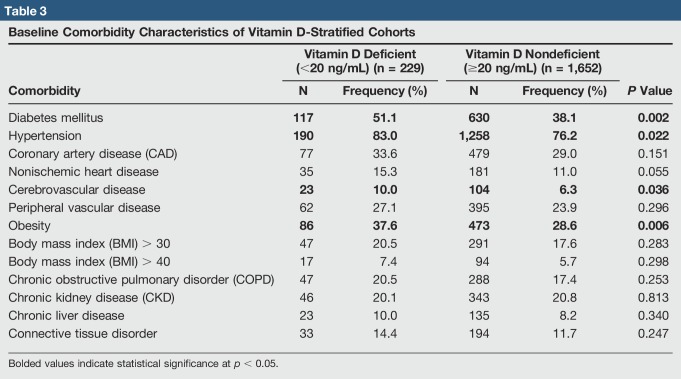
Between 2007 and 2016, 1,881 patients undergoing arthroscopic RCR had measured preoperative 25D levels in the Humana database (Table 2). Of these, 229 (229/1,881 = 12.2%) were found to be 25D deficient (<20 mg/dL). Both 25D-deficient and -sufficient groups were similar in distribution and had a median and mode age in the 65 to 69 years group (P = 0.237) (Table 2). In addition, sex distribution was equivalent between the two groups, as females comprised 66.8% and 63.8% of the 25D-deficient and -sufficient cohorts, respectively (P = 0.373). Most cases were reported in the South geographic region (25D-deficient 80.3%; 25D-sufficient 81.4%). The 25D-deficient cohort had a higher comorbid rates of diabetes mellitus (P = 0.002), hypertension (P = 0.022), obesity (P = 0.006), and cerebrovascular disease (P = 0.036) (Table 3).
Table 3.
Baseline Comorbidity Characteristics of Vitamin D-Stratified Cohorts
The most common complication after arthroscopic RCR was arthroscopic débridement (25D-deficient 24.0%; 25D-sufficient 28.7%), followed by revision RCR (25D-deficient 8.3%; 25D-sufficient 6.6%) and stiffness, requiring MUA (25D-deficient 4.8%; 25D-sufficient 3.8%) (Table 4). After adjusting for age, sex, and comorbidities using multivariate logistic regression, 25D-deficient patients undergoing arthroscopic RCR were more likely to undergo future revision RCR (OR 1.54, 95% CI 1.21 to 1.97, P < 0.001) and MUA for postoperative stiffness (OR 1.16, 95% CI 1.03 to 2.03, P = 0.035). Risks of postoperative SSI, arthroscopic débridement, and conversion to arthroplasty were not statistically significantly different between the two cohorts (Table 4).
Table 4.
Frequency and Adjusted OR of Surgical and Medical Complications After RCR
Discussion
As shown, vitamin D deficiency is associated with increased postoperative complications in arthroscopic RCR. This finding comes in light of other studies highlighting the significance of 25D as a potential modifiable risk factor to limit muscle strains, improve fracture outcomes, promote articular cartilage health, and decrease postoperative complications in arthroplasty.10,13,14,15,16 Although mechanistically it is unclear how normalizing 25D can lead to improved outcomes in arthroscopy, addressing deficiency preoperatively is, in principle, a simple task and has the potential to improve clinical results at a relatively low cost. Further study is warranted to investigate what role preoperative normalization of 25D may have on decreasing rates of revision RCR and stiffness requiring MUA.
The role of 25D in human biology is constantly evolving, though with ample evidence to support bone, muscle, and calcium and phosphoregulatory mechanisms. Conversely, 25D's role in tendon-to-bone healing is poorly understood. Rotator cuff surgery heavily relies on this healing mechanism, and failure is often attributed to ineffective tendon-to-bone repair. Some studies report as high as a 22% to 36% rate of recurrent tears after arthroscopic RCR.6,17,18 In turn, this has stimulated the need for augmentation of the procedure, with recent developments including dermal allografts and scaffolding to create more stable biomechanical constructs.19,20 Similarly, the role of supplementing 25D in these repairs is under consideration because it has been shown to mitigate the inflammatory milieu, with reports of improved healing in animal models.21 Theoretically, this implies that a lack of 25D could promote an environment hostile to adequate repair and predispose the patient to increased postoperative complications. Irrespective, a deeper understanding of the biochemical role of 25D in facilitation of tendon-to-bone healing is required to validate these conclusions and should be a target of future study.
As predicted, vitamin D deficiency was associated with a greater average CCI and associated medical comorbidities. Within the 25D-deficient cohort, there were higher rates of obesity (P = 0.006), diabetes mellitus (P = 0.002), hypertension (P = 0.022), and cerebrovascular disease (P = 0.036) than in the 25D-sufficient group. In the current literature, 25D deficiency has been associated with each of these conditions, although its role in pathogenesis is still an active topic of debate. In the obese, 25D deficiency is thought to be diluted by body mass because some data have shown obese individuals have identical serum concentrations to nonobese after controlling for body size.22 This deficiency, whether dilutional or not, is thought to allow inflammatory processes in the metabolic syndrome, leading to damage of β-cells in the pancreas and cardiovascular dysfunction. This subsequently leads to an increase in insulin resistance and coronary, cerebral, and peripheral vascular diseases.23 Notably, these comorbidities suggest that the 25D-deficient cohort inherently comprises a sicker population, and may confound why this group had more complications overall.
However, after controlling for these comorbidities, low levels of 25D were markedly associated with an increased need for RCR revisions. Re-tear or incomplete healing of the rotator cuff is common after RCR, although it may be of questionable clinical significance. Some studies note that the structural integrity of a RCR does not correlate with clinically notable differences in strength or pain, and patients will often report functional improvement despite failure to heal.24,25,26,27,28 As such, revision is often reserved for patients with persistent functional deficits or intolerable levels of residual pain.4,26,29 These outcomes, although likely multifactorial, could theoretically be affected by 25D deficiency. However, further investigation is required to determine how 25D is associated with the development of postoperative complications.
This study also found postoperative stiffness requiring MUA to be associated with 25D deficiency after controlling for age, sex, and comorbidities. Stiffness in the shoulder can be a direct result of postoperative inflammation because the upregulation of cytokines in an inflammatory response is thought to lead to myofibroblast-induced capsular hyperplasia and fibrosis. This subsequently decreases capsular volume and limits shoulder range of motion.30 Although speculative, 25D may have a role in this pathogenesis secondary to its role in inflammatory regulation. Some studies have highlighted 25D's ability to inhibit myofibroblast activity, and it is thought that supplementation of this nutrient may have a role in preventing fibrosis and scarring.31,32 As such, the increased incidence of stiffness in the 25D-deficient cohort may be explained by uninhibited myofibroblast proliferation, leading to increased scarring and decreased mobility at the glenohumeral joint. Of note, previous studies estimate the prevalence of comorbid adhesive capsulitis in the diabetic population to be around 10% to 30%.33 Given the large incidence of diabetes in the study population, it is possible that this condition explains part of the increased incidence of postoperative shoulder stiffness as well. Although no clear etiology exists regarding the development of shoulder stiffness in diabetics, it is believed to also be related to chronic inflammation and increased fibroblast activity.34 Theoretically, by acting through similar mechanisms, this implies that diabetes and 25D deficiency might synergistically increase the risk of developing postoperative shoulder stiffness. Future study should aim to identify the role of 25D in this pathogenesis and determine whether supplementation can decrease the risk of this outcome.
Limitations
First, the PearlDiver database is less amenable to the study of patients on an individual level, and instead allows efficient analysis of larger groups. As such, ability to interpret and analyze patient-specific outcomes is likely inferior to that of chart review. Furthermore, data within PearlDiver is entirely driven by billing codes. As a result, entries may be subject to clerical error, miscategorization, or inconsistencies due to subjective interpretation of respective CPT or ICD codes. Similarly, given that the queried CPT and ICD codes were limited in detailing the specifics of a particular diagnosis or procedure, comparisons between severity of rotator cuff tear and different techniques for repair could not be accounted for in analysis. Next, some degree of selection bias was likely also present because not all patients had preoperative 25D levels drawn. This likely means providers ordered this laboratory test in a cohort at greater risk for 25D deficiency, which may have skewed the observed results. This could imply that a large portion of the 25D-sufficient cohort may represent a population receiving adequate repletion, thus strengthening the argument that supplementation may mitigate the outcomes observed in the deficient group. Last, although beyond the scope of this study, these results do not comment on postoperative function or other subjective, patient-reported outcomes.
Conclusions
Among the patients scheduled for an arthroscopic RCR between 2007 and 2016, 12.2% were found to be deficient in 25D in the 90 days preceding surgery. This was associated with a greater risk of postoperative stiffness requiring MUA and need for future RCR revision. Although the role of 25D in the development of postoperative complications is unclear at this time, this study suggests the possibility that preoperative repletion could have a role in mitigating adverse outcomes. Further study should aim to investigate what role 25D supplementation may have on markedly reducing postoperative complications after arthroscopic RCR.
Footnotes
None of the following authors or any immediate family member has received anything of value from or has stock or stock options held in a commercial company or institution related directly or indirectly to the subject of this article: Mr. Harada, Dr. Arshi, Dr. Fretes, Mr. Formanek, Dr. Gamradt, Dr. McAllister, and Dr. Petrigliano.
References
- Levels of evidence are described in the table of contents. In this article, references 3, 7, 12, 13, 14, and 27 are level II studies. References 1, 6, 10, 22, 23, and 29 are level III studies. References 4, 5, 11, 15, 17, 18, 20, 24, 25, 26, 28, 30, and 33 are level IV studies. References 2, 8, 9, 16, 19, 21, 31, 32, and 34 are level V studies.
- 1.Yamamoto A, Takagishi K, Osawa T: Prevalence and risk factors of a rotator cuff tear in the general population. J Shoulder Elb Surg 2010;19:116-120. [DOI] [PubMed] [Google Scholar]
- 2.Sambandam SN, Khanna V, Gul A, Mounasamy V: Rotator cuff tears: An evidence based approach. World J Orthop 2015;6:902-918. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Milgrom C, Schaffler M, Gilbert S, Holsbeeck M: Rotator-cuff changes in asymptomatic adults. J Bone Joint Surg 1995;77:296-298. [PubMed] [Google Scholar]
- 4.Oh LS, Wolf BR, Hall MP, Levy BA, Marx RG: Indications for rotator cuff repair: A systematic review. Clin Orthop Relat Res 2007;455:52-63. [DOI] [PubMed] [Google Scholar]
- 5.Sher J, Uribe J, Posada A, Murphy B, Zlatkin M: Abnormal findings on magnetic resonance images of asymptomatic shoulders. J Bone Joint Surg 1995;77:10-15. [DOI] [PubMed] [Google Scholar]
- 6.Chung SW, Oh JH, Gong HS: Factors affecting rotator cuff healing after arthroscopic repair osteoporosis as one of the independent risk factors. Am J Sports Med 2008;39:2099-2107. [DOI] [PubMed] [Google Scholar]
- 7.Sprague S, Petrisor B, Scott T, et al. : What is the role of vitamin D supplementation in acute fracture patients? A systematic review and meta-analysis of the prevalence of hypovitaminosis D and supplementation efficacy. J Orthop Trauma 2015;30:1. [DOI] [PubMed] [Google Scholar]
- 8.Watkins RR, Lemonovich TL, Salata RA: An update on the association of vitamin D deficiency with common infectious diseases. Can J Physiol Pharmacol 2015;93:363-368. [DOI] [PubMed] [Google Scholar]
- 9.Oda Y, Tu C, Menendez A, Nguyen T, Bikle DD: Vitamin D and calcium regulation of epidermal wound healing. J Steroid Biochem Mol Biol 2017;1:379-385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hegde V, Arshi A, Wang C, et al. : Associated with higher postoperative complication rates in total knee arthroplasty. Orthopedics 2018;201:1-7. [DOI] [PubMed] [Google Scholar]
- 11.Hatfield DP, Sweeney KP, Lau J, Lichtenstein AH: Critical assessment of high-circulation print newspaper coverage of the Institute of Medicine report dietary reference intakes for calcium and vitamin D. Public Health Nutr 2014;17:1868-1876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Charlson ME, Pompei P, Ales KL, Mackenzie CR: A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis 1987;40:373-383. [DOI] [PubMed] [Google Scholar]
- 13.Nurmi-Luthje I, Luthje P, Kataja M: Positive effects of a sufficient pre-fracture serum vitamin D level on the long-term survival of hip fracture patients in Finland: A minimum 11-year follow-up. Drugs Aging 2015;32:477-486. [DOI] [PubMed] [Google Scholar]
- 14.Maier GS, Horas K, Seeger JB, Roth KE: Is there an association between periprosthetic joint infection and low vitamin D levels? Int Orthop 2014;38:1499-504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Rebolledo B, Bernard J, Rodeo S: Extremity muscle strains and core muscle injuries at the national football league combine. J Arthrosc Relat Surg 2018;34:1280-1285. [DOI] [PubMed] [Google Scholar]
- 16.Pascual-garrido C, Angeline ME, Ma R, et al. : Low levels of vitamin D have a deleterious effect on the articular cartilage in a rat model. HSS J 2016;12:150-157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Diebold G, Lam P, Walton J, Murrell GAC: Relationship between age and rotator cuff retear. J Bone Joint Surg 2017;99-A:1198-1205. [DOI] [PubMed] [Google Scholar]
- 18.Galatz LM, Ball CM, Yamaguchi K: The outcome and repair integrity of completely arthroscopically repaired large and massive rotator cuff tears. J Bone Joint Surg 2004;86-A:219-224. [DOI] [PubMed] [Google Scholar]
- 19.Lipner J, Shen H, Cavinatto L, et al. : In vivo evaluation of adipose-derived stromal cells delivered with a nanofiber scaffold for tendon-to-bone repair. Tissue Eng 2015;21:2766-2774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Gupta AK, Hug K, Berkoff DJ, et al. : Dermal tissue allograft for the repair of massive irreparable rotator cuff tears. Am J Sports Med 2012;40:141-147. [DOI] [PubMed] [Google Scholar]
- 21.Angeline ME, Ma R, Pascual-Garrido C, et al. : Effect of diet-induced vitamin D deficiency on rotator cuff healing in a rat model. Am J Sports Med 2014;42:27-34. [DOI] [PubMed] [Google Scholar]
- 22.Drincic AT, Armas LAG, Van Diest EE, Heaney RP: Volumetric dilution, rather than sequestration best explains the low vitamin D status of obesity. Obesity 2012;20:1444-1448. [DOI] [PubMed] [Google Scholar]
- 23.Anderson JL, May HT, Horne BD, et al. : Relation of vitamin D deficiency to cardiovascular risk factors, disease status, and incident events in a general healthcare population. Am J Cardiol 2010;106:963-968. [DOI] [PubMed] [Google Scholar]
- 24.Jost BYB, Pfirrmann CWA, Gerber C: Clinical outcome after structural failure of rotator cuff repairs. J Bone Joint Surg 2000;82-A:304-314. [DOI] [PubMed] [Google Scholar]
- 25.Jost B, Zumstein M, Pfirrmann CWA, Gerber C: Long-term outcome after structural failure of rotator cuff repairs. J Bone Joint Surg 2006;88-A:472-479. [DOI] [PubMed] [Google Scholar]
- 26.Lädermann A, Denard PJ, Burkhart SS: Management of failed rotator cuff repair: A systematic review. Br J Sports Med 2016;16:1-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Russell RD, Knight JR, Mulligan E, Khazzam MS: Not correlate with patient function and pain. J Bone Joint Surg 2014;96:265-271. [DOI] [PubMed] [Google Scholar]
- 28.Lafosse BL, Jost B, Reiland Y: Structural integrity and clinical outcomes after arthroscopic repair of isolated subscapularis tears. J Bone Joint Surg 2007;89:1184-1193. [DOI] [PubMed] [Google Scholar]
- 29.Namdari S, Donegan RP, Chamberlain AM, Galatz LM, Yamaguchi K, Keener JD: Factors affecting outcome after structural failure of repaired rotator cuff tears. J Bone Joint Surg 2014;96:99-105. [DOI] [PubMed] [Google Scholar]
- 30.Uppal HS: Frozen shoulder: A systematic review of therapeutic options. World J Orthop 2015;6:263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Zerr P, Vollath S, Palumbo-Zerr K, et al. : Vitamin D receptor regulates TGF-β signalling in systemic sclerosis. Ann Rheum Dis 2015;74:1-8. [DOI] [PubMed] [Google Scholar]
- 32.Lee SA, Yang HW, Um JY, Shin JM, Park IH, Lee HM: Vitamin D attenuates myofibroblast differentiation and extracellular matrix accumulation in nasal polyp-derived fibroblasts through smad2/3 signaling pathway. Sci Rep 2017;7:1-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Zreik NH, Malik RA, Charalambous CP: Adhesive capsulitis of the shoulder and diabetes: A meta-analysis of prevalence. Muscles Ligaments Tendons J 2016;6:26-34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Pons-Villanueva J, Escalada San Martín J: The stiff shoulder in diabetic patients. Int J Rheum Dis 2016;19:1226-1236. [DOI] [PubMed] [Google Scholar]