Abstract
Objective
To evaluate the efficacy of ustekinumab by prior treatment exposure and disease duration in tumour necrosis factor inhibitor (TNF)-naïve patients with psoriatic arthritis (PsA) in the PSUMMIT 1 and PSUMMIT 2 studies.
Methods
In the phase 3, randomised, placebo-controlled PSUMMIT 1 and PSUMMIT 2 studies, adults with active PsA for ≥6 months despite conventional synthetic disease-modifying antirheumatic drugs (csDMARDs) and/or non-steroidal anti-inflammatory drugs (NSAIDs) (PSUMMIT 1) or csDMARDs, NSAIDs and/or anti-TNF agents (PSUMMIT 2) were enrolled. Patients were randomised to subcutaneous injections of placebo, ustekinumab 45 mg or ustekinumab 90 mg at weeks 0 and 4 and every 12 weeks. Efficacy was assessed at week 24 using the American College of Rheumatology criteria and 28-joint count disease activity score using C reactive protein (DAS28-CRP); radiographical progression, enthesitis, and dactylitis were also assessed in this post hoc analysis.
Results
A total of 747 patients were included; all 747 were TNF-naïve, of which, 179 were methotrexate-naïve and TNF-naïve, and 146 were all csDMARD-naïve and TNF-naïve. At week 24, greater proportions of ustekinumab-treated patients had ≥20%/50%/70% improvement in American College of Rheumatology criteria (ACR20/ACR50/ACR70) responses, DAS28-CRP response and DAS28-CRP remission versus placebo in all three prior-treatment populations, with similar differences between treatment groups. Greater proportions of ustekinumab-treated patients also had complete resolution of enthesitis and dactylitis at week 24 across the three prior-treatment populations. Mean changes from baseline in total van der Heijde-Sharp Score at week 24 were generally smaller for ustekinumab-treated patients versus placebo but were statistically significant only in the full TNF-naïve population. Response rates for ACR20/ACR50/ACR70 were similar for TNF-naïve patients with PsA durations of <1 year, ≥1 to <3 years, and ≥3 years.
Conclusion
Ustekinumab-treated patients demonstrated greater clinical response at week 24 compared with placebo regardless of prior treatment exposure and PsA disease duration.
Keywords: psoriatic arthritis; ustekinumab; anti-Il-12, anti-Il-23; biologics
Key messages.
What is already known about this subject?
The PSUMMIT 1 and PSUMMIT 2 trials demonstrated the efficacy of ustekinumab in both biologic-naïve and tumour necrosis factor inhibitor (TNF)-experienced adult patients with active PsA.
What does this study add?
Among TNF-naïve patients, ustekinumab is efficacious in patients with PsA irrespective of prior conventional synthetic disease-modifying antirheumatic drug (csDMARD) treatment and duration of disease.
How might this impact on clinical practice?
The patients in this analysis represent the heterogeneity of patients with PsA in real-world clinical practice. These results suggest that ustekinumab could be considered an appropriate treatment option for biologic-naïve patients with PsA irrespective of previous csDMARD therapy and disease duration.
Introduction
Patients with psoriatic arthritis (PsA) are often treated with conventional synthetic disease-modifying antirheumatic drugs (csDMARDs) or non-steroidal anti-inflammatory drugs (NSAIDs) as their initial therapy, followed by biologic therapies for patients who do not have an adequate response to csDMARDs or NSAIDs or are unable to tolerate these therapies.1 2 Current treatment recommendations support a treat-to-target approach, in which patients are closely monitored and treatment modifications are made as needed with the goal of reaching remission or low disease activity.2 3 Additionally, it is also recommended that the treatment approach be made in consideration of the disease domains involved (ie, peripheral arthritis, axial disease, enthesitis, dactylitis, skin and nails).1
The PSUMMIT trials evaluated the safety and efficacy of ustekinumab, a fully human monoclonal antibody to the shared p40 subunit of interleukin (IL)-12 and IL-23 in adults with active PsA. Patients in PSUMMIT 1 had active disease despite prior therapy with NSAIDS or csDMARDs. The patient population in PSUMMIT 2 was similar, with the exception that some patients had undergone prior antitumour necrosis factor (TNF) therapy. In these trials, ustekinumab was shown to be efficacious in reducing the signs and symptoms of PsA,4 5 including inhibition of radiographical progression.6 In this post hoc exploratory analysis, we examined efficacy outcomes in TNF-naïve patients pooled from PSUMMIT 1 and PSUMMIT 2 by prior treatment exposure and disease duration.
Methods
Patients and study design
The patient eligibility criteria and study design for the PSUMMIT 1 and PSUMMIT 2 studies have been previously reported in detail.4 5 Briefly, patients in both studies had active PsA for ≥6 months despite ≥3 months of csDMARD therapy or ≥4 weeks of NSAID therapy or demonstrated intolerance to these therapies. In PSUMMIT 1, patients could not have previously underwent biologic therapy. In PSUMMIT 2, previous treatment with anti-TNF therapies was permitted; patients who had previously underwent anti-TNF therapy had to have undergone therapy for ≥8 weeks with etanercept, adalimumab, golimumab or certolizumab pegol or for ≥14 weeks with infliximab, or had to demonstrate intolerance to these therapies.
In both PSUMMIT 1 and PSUMMIT 2, eligible patients were randomly assigned to receive subcutaneous injections of ustekinumab 45 or 90 mg at weeks 0 and 4 and every 12 weeks thereafter, or placebo at weeks 0, 4 and 16, with crossover to ustekinumab 45 mg at week 24. At week 16, patients with <5% improvement from baseline in both tender and swollen joint counts entered double-blind early escape, and patients in the placebo group received ustekinumab 45 mg, while patients in the ustekinumab 45 mg group received ustekinumab 90 mg. Patients randomised to ustekinumab 90 mg did not have any adjustments to therapy regardless of early escape status.
PSUMMIT 1 and PSUMMIT 2 were conducted in accordance with good clinical practices and the Declaration of Helsinki. The protocol was approved by the institutional review board or the ethics committee at each site, and all patients gave written informed consent before any study-related procedures were performed.
Assessments
Efficacy was assessed using the American College of Rheumatology (ACR) criteria7 and 28-joint count disease activity score using C reactive protein (DAS28-CRP).8 The Maastricht Ankylosing Spondylitis Enthesitis Score Index modified for PsA (inclusion of bilateral plantar fascia),9 resulting in a scale of 0–15, was used to evaluate changes in enthesitis. Dactylitis was assessed in all 20 digits using a scale of 0–3 (0, no dactylitis; 1, mild dactylitis; 2, moderate dactylitis; and 3, severe dactylitis). Radiographical progression was assessed using the van der Heijde-Sharp (vdH-S) Score modified for PsA.10
Statistical analysis
Only TNF-naïve patients from PSUMMIT 1 and PSUMMIT 2 were included in this post hoc analysis, including patients who met the early escape criteria. Clinical efficacy and radiographical progression were summarised using descriptive statistics. The proportions of patients achieving a ≥20%/50%/70% improvement in ACR criteria (ACR20/ACR50/ACR70) response, DAS28-CRP response and DAS28-CRP remission, and complete resolution of enthesitis and dactylitis at week 24 were determined. The mean change from baseline to week 24 in total PsA-modified vdH-S Score was also determined. Three non-mutually exclusive prior-treatment populations were evaluated: TNF-naïve, methotrexate (MTX)-naïve and TNF-naïve (no prior treatment with MTX or anti-TNF therapy, but could have received csDMARDs other than MTX), and csDMARD-naïve and TNF-naïve (no prior treatment with either csDMARDs or anti-TNF therapy). Comparisons between placebo and combined ustekinumab (45 and 90 mg) groups were performed for each prior-treatment population (χ2 test). ACR20/ACR50/ACR70 response rates were also determined for TNF-naïve patients according to the duration of PsA (<1 year, ≥1 to <3 years, and ≥3 years).
Results
Baseline demographic and disease characteristics
A total of 927 patients (PSUMMIT 1, n=615; PSUMMIT 2, n=312) were randomised in the PSUMMIT trials.4 5 Of these, 747 TNF-naïve patients (PSUMMIT 1, n=615; PSUMMIT 2, n=132) were included in this analysis, and of these, 179 were both MTX-naïve and TNF-naïve, and 146 were both all csDMARD-naïve and TNF-naïve. Baseline demographic and disease characteristics of TNF-naïve patients were well balanced among the treatment groups (table 1).
Table 1.
Baseline demographic and disease characteristics
| Placebo | Ustekinumab | Total | ||
| 45 mg | 90 mg | |||
| Patients, n | 248 | 248 | 251 | 747 |
| Male | 128 (51.6) | 131 (52.8) | 143 (57.0) | 402 (53.8) |
| BMI (kg/m2) | 30.6±7.5 | 30.1±6.5 | 30.4±7.1 | 30.4±7.0 |
| Disease duration (years) | ||||
| PsA | 6.8±7.7 | 6.2±7.6 | 6.8±7.7 | 6.6±7.7 |
| <1 year | 61 (24.6) | 47 (19.0) | 40 (15.9) | 148 (19.8) |
| ≥1 to <3 years | 59 (23.8) | 72 (29.0) | 62 (24.7) | 193 (25.8) |
| ≥3 years | 128 (51.6) | 129 (52.0) | 149 (59.4) | 406 (54.4) |
| Psoriasis | 15.6±12.9 | 14.5±12.6 | 15.1±12.6 | 15.1±12.7 |
| Patients with psoriasis involving ≥3% BSA, n | 176 | 181 | 189 | 546 |
| PASI | 12.0±10.2 | 11.9±12.1 | 10.7 (8.7) | 11.5±10.4 |
| DLQI | 11.9±7.6 | 11.2±7.2 | 10.6±7.1 | 11.2±7.3 |
| Swollen joint count (0–66) | 14.7±9.9 | 12.6±7.6 | 12.8±8.6 | 13.4±8.8 |
| Tender joint count (0–68) | 24.4±14.6 | 22.5±14.1 | 22.8±13.8 | 23.2±14.2 |
| CRP (mg/L) | 15.6±18.4 | 18.1±22.1 | 17.4±18.7 | 17.1±19.8 |
| HAQ-DI | 1.24±0.67 | 1.22±0.62 | 1.21±0.62 | 1.22±0.64 |
| DAS28-CRP | 5.2±1.1 | 5.2±1.0 | 5.2±1.0 | 5.2±1.0 |
| Patients with dactylitis in ≥1 digit | 113 (45.6) | 120 (48.4) | 113 (45.0) | 346 (46.3) |
| Dactylitis score | 8.3±10.0 | 7.8±9.7 | 7.9±8.6 | 8.0±9.4 |
| Patients with enthesitis | 176 (71.0) | 167 (67.3) | 184 (73.3) | 527 (70.5) |
| Enthesitis score | 5.2±3.8 | 5.1±3.6 | 5.7±3.9 | 5.3±3.8 |
| SF-36 PCS score | 31.3±8.6 | 31.0±8.4 | 31.4±8.0 | 31.2±8.3 |
| SF-36 MCS score | 42.7±11.2 | 42.7±11.2 | 43.4±11.5 | 42.9±11.3 |
| Concomitant MTX use at baseline | 121 (48.8) | 127 (51.2) | 129 (51.4) | 377 (50.5) |
| MTX-naïve | 56 (22.6) | 58 (23.4) | 65 (25.9) | 179 (24.0) |
| csDMARD-naïve | 45 (18.1) | 48 (19.4) | 53 (21.1) | 146 (19.5) |
Data are presented as n (%) or mean±SD unless otherwise noted.
BMI, body mass index; BSA, body surface area; CRP, C reactive protein; csDMARD, conventional synthetic disease-modifying antirheumatic drug; DAS28-CRP, 28-joint count disease activity score using C reactive protein; DLQI, Dermatology Life Quality Index; HAQ-DI, Health Assessment Questionnaire–Disability Index; MTX, methotrexate; PASI, psoriasis area and severity index; SF-36 PCS/MCS, 36-item Short-Form Health Survey physical/mental component summary; PsA, psoriatic arthritis.
Efficacy
At week 24, greater proportions of ustekinumab-treated patients had an ACR20/ACR50/ACR70 response compared with placebo in all three of the prior-treatment populations, and the differences between treatment groups were similar among the three prior-treatment populations (figure 1A). Greater proportions of ustekinumab-treated patients achieved DAS28-CRP response and DAS28-CRP remission compared with placebo in all three prior-treatment populations (figure 1B).
Figure 1.
Proportions of patients who achieved (A) ACR20/ACR50/ACR70 responses at week 24, (B) DAS28-CRP response and remission at week 24, and (C) mean changes from baseline in total PsA-modified vdH-S score at week 24 among patients who were TNF-naïve, MTX-naïve and TNF-naïve, and csDMARD-naïve and TNF-naïve. ACR20/ACR50/ACR70, ≥20%/50%/70% improvement in American College of Rheumatology criteria; csDMARD, conventional synthetic disease-modifying antirheumatic drug; DAS28-CRP, 28-joint count disease activity score using C reactive protein; MTX, methotrexate; TNF, tumour necrosis factor; vdH-S, van der Heijde-Sharp.
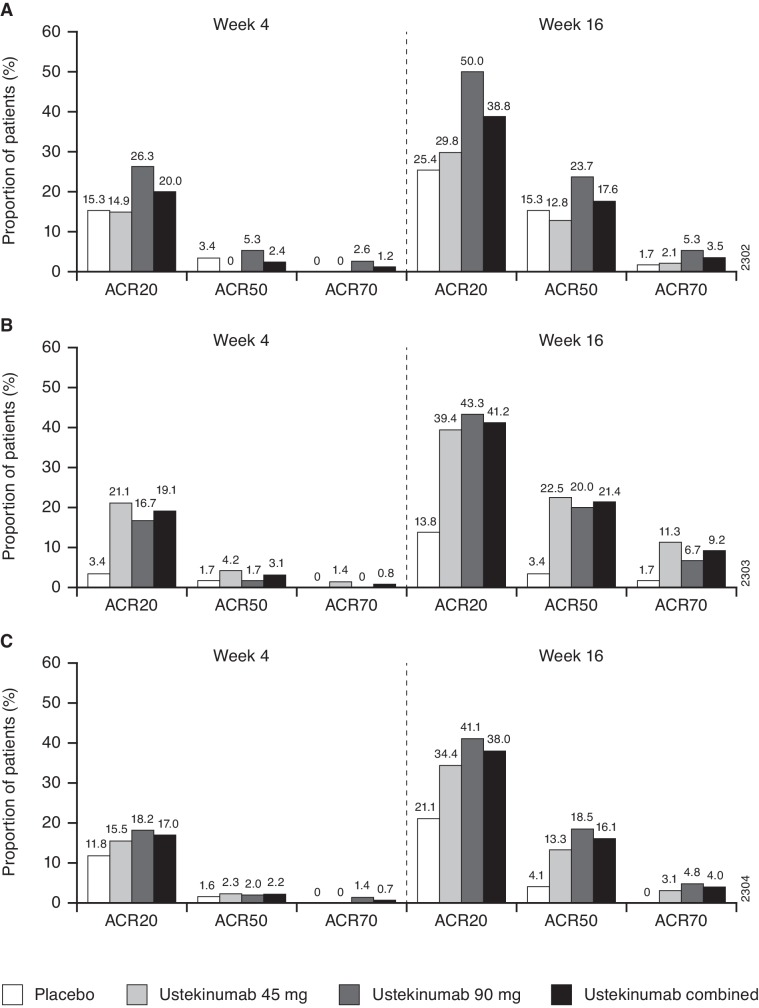
The proportion of patients with complete resolution of enthesitis at week 24 was significantly greater in the combined ustekinumab group than in the placebo group within the TNF-naïve population (36.2% vs 19.9%, p<0.001) (figure 2A). Similar response rates were observed for patients who were MTX-naïve and TNF-naïve and those who were csDMARD-naïve and TNF-naïve; however, these differences did not reach statistical significance (figure 2A). Likewise, within the TNF-naïve population, a significantly greater proportion of ustekinumab-treated patients had complete resolution of dactylitis at week 24 compared with placebo (42.9% vs 25.5%, p=0.003) (figure 2B). Response rates were similar for the MTX-naïve and TNF-naïve and the csDMARD-naïve and TNF-naïve populations; however, the differences between the placebo and combined ustekinumab groups did not reach statistical significance (figure 2B). Among TNF-naïve patients, those in the ustekinumab group had a significantly smaller mean change from baseline in total PsA-modified vdH-S Score at week 24 compared with placebo (0.3 vs 1.1, p<0.001). Mean changes from baseline in total PsA-modified vdH-S Score were numerically lower for ustekinumab-treated patients compared with placebo; similar mean changes from baseline were observed in the MTX-naïve and TNF-naïve and the csDMARD-naïve and TNF-naïve populations, but did not reach statistical significance (figure 1C). The proportions of patients who achieved an ACR20/ACR50/ACR70 response at weeks 4 and 16 were generally similar for patients with PsA disease durations of <1 year, ≥1 to <3 years, and ≥3 years (figure 3).
Figure 2.
Proportions of patients with (A) complete resolution of enthesitis and (B) complete resolution of dactylitis at week 24 among patients who were TNF-naïve, MTX-naïve and TNF-naïve, and csDMARD-naïve and TNF-naïve. csDMARD, conventional synthetic disease-modifying antirheumatic drug; MTX, methotrexate; TNF, tumour necrosis factor.
Figure 3.
Proportions of patients who achieved ACR20/ACR50/ACR70 responses at weeks 4 and 16 among patients with a PsA disease duration of (A) <1 year, (B) ≥1 to <3 years, and (C) ≥3 years among patients who were TNF-naïve. ACR20/ACR50/ACR70, ≥20%/50%/70% improvement in American College of Rheumatology criteria; PsA, psoriatic arthritis; TNF, tumour necrosis factor.
Discussion
In this novel post hoc analysis of biologic-naïve patients with PsA from PSUMMIT 1 and PSUMMIT 2, greater proportions of ustekinumab-treated patients achieved ACR20/50/70 responses and DAS28-CRP response and remission compared with placebo at week 24. Likewise, greater proportions of patients in the ustekinumab group had complete resolution of enthesitis and dactylitis at week 24, and ustekinumab-treated patients had less radiographical progression compared with the placebo group. The treatment effect was generally consistent among the three prior-treatment populations (TNF-naïve, MTX-naïve and TNF-naïve, and csDMARD-naïve and TNF-naïve). In addition, ACR response rates were higher for patients in the ustekinumab group than for patients in the placebo group at earlier time points (weeks 4 and 16), with similar efficacy regardless of PsA disease duration.
These results are consistent with the previous analyses of the overall populations in PSUMMIT 1 and PSUMMIT 2, in which greater proportions of patients in the ustekinumab groups achieved ACR and Psoriasis Area and Severity Index (PASI) responses compared with the placebo group.4 5 In general, ACR and PASI responses were achieved irrespective of MTX use among the overall study populations in both trials, though the response rates were somewhat numerically higher among patients who did not receive concomitant MTX than among those undergoing combination therapy of ustekinumab plus MTX.4–6 A recent analysis of real-world data from a patient registry (BIOPURE) provided findings similar to those from the PSUMMIT trials; biologic-naïve patients tended to have longer treatment persistence and better clinical outcomes than those who previously had an inadequate response to one or more anti-TNF therapies.11 In addition, there was no apparent effect of concomitant MTX use on ustekinumab treatment persistence in this registry.
Although disease duration is not always correlated with disease severity, it should be noted that the patients in the PSUMMIT studies were required to have active PsA for at least 6 months despite treatment with csDMARDs and/or NSAIDs and have moderate to severe disease at baseline. Prior research by Husted et al has shown a relationship between PsA disease duration and changes in Health Assessment Questionnaire–Disability Index (HAQ-DI) scores, with patients having a disease duration of <2 years more likely to experience changes in HAQ-DI score when compared with patients having a disease duration of 2–5 years or >5 years.12 Increasing age was also associated with fewer changes in HAQ-DI over time and more persistent physical impairment.12 Notably, there was patient variability in the course of physical function, including a stable state of impaired physical function throughout the study period, with 28% of the patients experiencing no impairment over the study duration. However, 12% and 6% of patients experienced moderate or severe physical impairment, respectively.12 Additional research by the same authors found that, although disease activity, as measured by the number of active joints, is a strong predictor of HAQ-DI, this influence lessened over time, leading to decreased variability in HAQ-DI with longer disease duration.13 Notably, other manifestations of disease activity in PsA, such as enthesitis, have also been observed to influence functional status as assessed by HAQ-DI. In a separate post hoc analysis also of TNF-naïve patients from PSUMMIT 1 and PSUMMIT 2, patients with improvements in enthesitis had greater improvements in HAQ-DI than did patients with unchanged or worsened enthesitis through week 24; this association was observed for both ACR20 responders and nonresponders.14 Another recent analysis in patients with PsA demonstrated with statistical significance that patients with, versus without, enthesitis had poorer functional status as assessed by HAQ-DI.15 While dactylitis was associated with similar numerical trends, differences versus patients without dactylitis were not statistically significant.15
Dysregulation of the IL-23/IL-17 pathway has been implicated in the pathogenesis of PsA. In a previously published murine model, systemic expression of IL-23 resulted in increased local expression of several cytokines and chemokines, leading to the development of enthesitis in the peripheral joints and in the spine.16 This study was further supported by an exploratory analysis of human entheseal tissue (from individuals with no systemic inflammatory burden), which found significantly increased expression of the IL-23 receptor transcript in innate lymphoid cells isolated from entheseal soft tissue or perientheseal bone.17 Additionally, both the IL-12 p40 subunit18 and IL-23 (both p19 and p40 subunits)19 are overexpressed in psoriatic plaques. Hence, by targeting the shared p40 subunit of IL-12 and IL-23, ustekinumab inhibits the upstream regulatory cytokines that serve as key drivers of the resultant inflammatory cytokine cascade and clinical manifestations observed in patients with PsA.
The current treatment paradigm in PsA encourages a shared decision-making process.1 2 Multiple factors should ideally be assessed when considering appropriate therapy, including the presence of peripheral arthritis, axial disease, enthesitis and dactylitis, skin manifestations and overall disease severity. Treatment selection should be shaped by various factors, including disease activity, structural damage, comorbid conditions and previous therapies. Additionally, from the patient perspective, treatment options should factor in any contraindications for a particular therapy, as well as preference regarding mode and frequency of administration. Results from the PSUMMIT trials previously demonstrated the efficacy of ustekinumab in adults with active PsA. The additional post hoc data reported here show that the treatment effect was similar among TNF-naïve patients regardless of prior csDMARD therapy or disease duration.
Acknowledgments
The authors thank Rebecca Clemente, PhD, of Janssen Scientific Affairs, LLC, for writing support. Portions of these data have been presented at EULAR 2017 and ACR 2017 and were published in the meeting proceedings (Ann Rheum Dis. 2017; 76 (suppl 2): 944 and Arthritis Rheumatol. 2017; 69 (suppl 10), respectively).
Footnotes
Contributors: All authors contributed to the study design, YY conducted the data analysis, and all authors interpreted the data and revised the manuscript.
Funding: This study was funded by Janssen Research & Development, LLC.
Competing interests: IBM has received consulting fees from AbbVie, Celgene, Janssen, Novartis, Pfizer and UCB. AK has received consulting fees and research support from AbbVie, Amgen, Janssen, Lilly, Novartis, Pfizer and UCB. IA is an employee of Janssen Biologics BV. SDC and SK are employees of Janssen Scientific Affairs, LLC, and own stock in Johnson & Johnson, of which Janssen Scientific Affairs, LLC, is a wholly owned subsidiary. ECH and YY are employees of Janssen Research & Development, LLC, and own stock in Johnson & Johnson, of which Janssen Research & Development, LLC, is a wholly owned subsidiary.
Patient consent for publication: Not required.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Coates LC, Kavanaugh A, Mease PJ, et al. Group for Research and Assessment of Psoriasis and Psoriatic Arthritis 2015 treatment recommendations for psoriatic arthritis. Arthritis Rheumatol 2016;68:1060–71. 10.1002/art.39573 [DOI] [PubMed] [Google Scholar]
- 2.Singh JA, Guyatt G, Ogdie A, et al. Special article: 2018 American College of Rheumatology/National Psoriasis Foundation guideline for the treatment of psoriatic arthritis. Arthritis Rheumatol 2019;71:5–32. 10.1002/art.40726 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Smolen JS, Braun J, Dougados M, et al. Treating spondyloarthritis, including ankylosing spondylitis and psoriatic arthritis, to target: recommendations of an international Task force. Ann Rheum Dis 2014;73:6–16. 10.1136/annrheumdis-2013-203419 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.McInnes IB, Kavanaugh A, Gottlieb AB, et al. Efficacy and safety of ustekinumab in patients with active psoriatic arthritis: 1 year results of the phase 3, multicentre, double-blind, placebo-controlled PSUMMIT 1 trial. Lancet 2013;382:780–9. 10.1016/S0140-6736(13)60594-2 [DOI] [PubMed] [Google Scholar]
- 5.Ritchlin C, Rahman P, Kavanaugh A, et al. Efficacy and safety of the anti-IL-12/23 p40 monoclonal antibody, ustekinumab, in patients with active psoriatic arthritis despite conventional non-biological and biological anti-tumour necrosis factor therapy: 6-month and 1-year results of the phase 3, multicentre, double-blind, placebo-controlled, randomised PSUMMIT 2 trial. Ann Rheum Dis 2014;73:990–9. 10.1136/annrheumdis-2013-204655 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kavanaugh A, Puig L, Gottlieb AB, et al. Maintenance of clinical efficacy and radiographic benefit through two years of ustekinumab therapy in patients with active psoriatic arthritis: results from a randomized, placebo-controlled phase III trial. Arthritis Care Res (Hoboken) 2015;67:1739–49. 10.1002/acr.22645 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Felson DT, Anderson JJ, Boers M, et al. American College of Rheumatology. Preliminary definition of improvement in rheumatoid arthritis. Arthritis Rheum 1995;38:727–35. 10.1002/art.1780380602 [DOI] [PubMed] [Google Scholar]
- 8.van Riel P, van Gestel AM, Scott DL. EULAR Handbook of clinical assessments in rheumatoid arthritis. Alphen Aan Den Rijn, The Netherlands: Van Zuiden Communications, BV, 2000. [Google Scholar]
- 9.Heuft-Dorenbosch L, Spoorenberg A, van Tubergen A, et al. Assessment of enthesitis in ankylosing spondylitis. Ann Rheum Dis 2003;62:127–32. 10.1136/ard.62.2.127 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.van der Heijde D, Sharp J, Wassenberg S, et al. Psoriatic arthritis imaging: a review of scoring methods. Ann Rheum Dis 2005;64(Suppl 2):ii61–4. 10.1136/ard.2004.030809 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Iannone F, Santo L, Bucci R, et al. Drug survival and effectiveness of ustekinumab in patients with psoriatic arthritis. real-life data from the biologic Apulian registry (BIOPURE). Clin Rheumatol 2018;37:667–75. 10.1007/s10067-018-3989-2 [DOI] [PubMed] [Google Scholar]
- 12.Husted JA, Tom BD, Farewell VT, et al. Description and prediction of physical functional disability in psoriatic arthritis: a longitudinal analysis using a Markov model approach. Arthritis Rheum 2005;53:404–9. 10.1002/art.21177 [DOI] [PubMed] [Google Scholar]
- 13.Husted JA, Tom BD, Farewell VT, et al. A longitudinal study of the effect of disease activity and clinical damage on physical function over the course of psoriatic arthritis: does the effect change over time? Arthritis Rheum 2007;56:840–9. 10.1002/art.22443 [DOI] [PubMed] [Google Scholar]
- 14.McInnes IB, Puig L, Gottlieb AB, et al. Association between enthesitis and health-related quality of life in psoriatic arthritis in biologic-naive patients from 2 phase III ustekinumab trials. J Rheumatol 2019:jrheum.180792 10.3899/jrheum.180792 [DOI] [PubMed] [Google Scholar]
- 15.Mease PJ, Karki C, Palmer JB, et al. Clinical characteristics, disease activity, and patient-reported outcomes in psoriatic arthritis patients with dactylitis or enthesitis: results from the Corrona psoriatic arthritis/spondyloarthritis registry. Arthritis Care Res (Hoboken) 2017;69:1692–9. 10.1002/acr.23249 [DOI] [PubMed] [Google Scholar]
- 16.Sherlock JP, Joyce-Shaikh B, Turner SP, et al. Il-23 induces spondyloarthropathy by acting on ROR-γt+ CD3+CD4-CD8- entheseal resident T cells. Nat Med 2012;18:1069–76. 10.1038/nm.2817 [DOI] [PubMed] [Google Scholar]
- 17.Cuthbert RJ, Fragkakis EM, Dunsmuir R, et al. Brief report: group 3 innate lymphoid cells in human enthesis. Arthritis Rheumatol 2017;69:1816–22. 10.1002/art.40150 [DOI] [PubMed] [Google Scholar]
- 18.Yawalkar N, Karlen S, Hunger R, et al. Expression of interleukin-12 is increased in psoriatic skin. J Invest Dermatol 1998;111:1053–7. 10.1046/j.1523-1747.1998.00446.x [DOI] [PubMed] [Google Scholar]
- 19.Lee E, Trepicchio WL, Oestreicher JL, et al. Increased expression of interleukin 23 P19 and p40 in lesional skin of patients with psoriasis vulgaris. J Exp Med 2004;199:125–30. 10.1084/jem.20030451 [DOI] [PMC free article] [PubMed] [Google Scholar]