Abstract
目的
探讨急性下消化道大出血患者进行急诊肠镜的必要性及最佳肠道准备方式。
方法
收集近年南方医院188例急性下消化道大出血病例结肠镜检查相关资料,根据检查时机将患者分为急诊组与择期组,通过单因素分析不同肠镜检查时机对急性下消化道大出血诊断率的影响,在此基础上纳入肠道清洁度进行多因素分层分析,分析不同肠道清洁度对急诊肠镜诊断率的影响。
结果
急诊组118例,择期组70例,两组的诊断率无统计学差异(P=0.724),但急诊组确定性出血灶的诊断率显著高于择期组(P=0.041),口服泻药的比例则显著低于择期组(P < 0.001)。肠道清洁度“优”、“良”、“差”在口服泻药及清洁灌肠的患者中的比例依次为63.6% vs 13.5%、28.6% vs 24.3%、7.8% vs 62.2%(P < 0.001)。单因素Logistic分析结果示,清洁度“优”较“差”显著提高肠镜诊断率(P=0.012),多因素logistic模型中,分组与清洁度的交互效应分析结果显示清洁度“优”时急诊组诊断率显著高于择期组(P=0.030);亚组分析结果显示,急诊组清洁度“优”时诊断率显著高于清洁度“差”(P=0.015)。
结论
当肠道清洁度为“优”时,急诊肠镜对急性下消化道大出血的诊断率优于择期肠镜,但通过清洁灌肠准备肠道时肠道清洁度差,从而降低了其诊断优势,因此在患者血流动力学稳定的前提下,急诊肠镜肠道准备应尽量选用口服泻药。
Keywords: 急性下消化道大出血, 急诊肠镜, 择期肠镜, 肠道准备方式, 肠道清洁度
Abstract
Objective
To investigate the value of urgent colonoscopy in the diagnosis of severe acute lower gastrointestinal bleeding and the optimal bowel preparation before examination.
Methods
The clinical data were collected from 188 patients undergoing wither urgent or elective colonoscopy for severe acute lower gastrointestinal bleeding in Nanfang Hospital. Univariate analysis was used to assess the effect of the timing of colonoscopy on the diagnostic rate of hemorrhage, and a multivariate model which stratified bowel cleanliness was used to analyze the impact of bowel cleanliness on the diagnostic rate of urgent colonoscopy.
Results
Of the 188 patients, 118 underwent urgent colonoscopy and 70 underwent elective colonoscopy examinations. The diagnostic rates were comparable between the two groups (44.1% vs 41.4%, P=0.724), but urgent colonoscopy resulted in a significantly higher diagnostic rate for identifying the bleeding source (32.2% vs 18.6%, P= 0.041). The proportion of the patients taking oral laxatives was significantly lower in urgent colonoscopy group (P < 0.001). Oral laxatives versus enema resulted in good, moderate, and poor bowel cleanliness in 63.6% vs 13.5%, 28.6% vs 24.3%, and 7.8% vs 62.2% of the patients (P < 0.001). Univariate analysis indicated that good bowel cleanliness was associated with a significantly higher diagnostic rate of colonoscopy than poor bowel cleanliness (P=0.012). Multivariate analysis showed that with good bowel cleanliness, urgent colonoscopy yielded a significantly higher diagnostic rate than elective colonoscopy (P=0.030); subgroup analyses suggested that good bowel cleanliness improved the diagnostic rate of urgent colonoscopy as compared with poor bowel cleanliness (P=0.015).
Conclusion
In patients with good bowel cleanliness, urgent colonoscopy yields a higher diagnostic rate than elective colonoscopy for severe acute lower gastrointestinal bleeding. Poor bowel cleanliness resulting from bowel preparation by enema significantly lowers the diagnostic performance of urgent colonoscopy. Oral laxatives are recommended over enemas for bowel preparation before urgent colonoscopy when the patients have stable hemodynamics.
Keywords: severe acute lower gastrointestinal bleeding, urgent colonoscopy, elective colonoscopy, bowel preparation, bowel cleanliness
下消化道出血是消化科常见的急症之一,其发病率逐年上升[1],其中大出血约占15%~22% [2]。肠镜下的直观表现及治疗优势使得肠镜成为下消化道出血的首选诊治方式[3-5]。
对急性下消化道大出血的患者,目前肠镜执行的时机尚存在争议[6-9]。早期的研究表明在入院24 h内实施的肠镜相比择期肠镜可以提供更为早期、准确的诊断,缩短低风险出血人群的住院时间[10-13];然而,有些研究却认为对于急性下消化道出血,急诊肠镜在诊断上并无显著优势[14-15],且尚无明确证据表明急诊肠镜相比择期肠镜更能提高临床预后[15-16]。
一般情况下,急诊肠镜的实施需要快速的肠道准备,常用的肠道准备方式包括口服泻药及清洁灌肠[17-20]。临床实践中,因口服泻药做肠道准备需4 h甚至更多时间,常难以普及,而清洁灌肠则相对简便快捷,常用于行急诊肠镜前的肠道准备[21]。临床中我们观察到通过灌肠后行急诊肠镜时往往因肠道清洁度较差难以完成全结肠检查,常需二次肠镜。目前,对于急性下消化道大出血患者的肠镜检查,肠道清洁度对不同时机的肠镜检查,尤其是急诊肠镜的诊治效果影响的研究较少[22]。
因此,本研究通过分析不同肠镜时机对急性下消化道大出血诊断率的影响以明确急诊肠镜与择期肠镜的诊断价值,在此基础上,分析不同肠道清洁度对急诊肠镜诊断率的影响,旨在进一步明确急诊肠镜前的最佳肠道准备方式;此外,对进行急诊与择期肠镜患者在住院时间及住院费用等方面是否存在差异也进行了比较分析。
1. 资料和方法
1.1. 研究对象及纳入、排除标准
选取2004年6月~2015年3月因急性下消化道大出血就诊于南方医院且行肠镜检查的患者。记录指标:性别、年龄、血压、心率、血红蛋白(HB)、血小板计数(PLT)、红细胞压积(HCT)、国际标准化比值(INR)、肠镜时机、肠道准备方式、肠镜检查相关结果、输血相关指标、是否二次肠镜或手术、住院时间及住院费用。
纳入标准:患者新发便血(3 d内红色或者暗红色大便)或既往有便血病史但在一周以内便血加重入院,且伴有大量血液丢失的临床或者实验室证据,这些证据包括:(a)输血超过2个单位的浓缩红细胞;(b)大量失血需收入重症监护病房;(c)红细胞压积12 h内下降超过5%;(d)血流动力学不稳定征象:心绞痛,晕厥或者晕厥前症状;(e)收缩压 < 100 mmHg,或者静息时脉搏≥100次/min。
排除标准:(1)胃镜提示为明确的上消化出血来源;(2)年龄小于18岁;(3)起病前10 d曾行腹部外科手术;(4)半月内曾行肠道息肉切除术;(5)已行血管造影或放射性核素显像明确病变部位者。
1.2. 分组及变量定义
分组:依肠镜执行时机将研究对象分为急诊组和择期组,急诊组包括在入院24 h之内实施肠镜或在住院期间因病情需要由临床医生紧急实施急诊肠镜的患者,择期组即为入院后超过24h行肠镜检查的患者。
肠道准备方式包括口服泻药、清洁灌肠。常用的泻药包括聚乙二醇,甘露醇和磷酸钠盐口服液。
肠道准备质量的分级:优-肠道粘膜无粪渣、血液及血凝块覆盖者;良-仅少量( < 25%的黏膜表面)粪便、血液或凝块,可通过内镜下下冲洗抽吸不影响观察者;差-肠腔中有大量血凝块或成形大便,甚至肠镜难以通过者。由研究组中两组成员通过查阅每位患者在行肠镜检查过程中记录的所有图片进行统一评判,意见一致即确定为分级结果,有异议者则全组成员讨论决定(图 1)。
1.
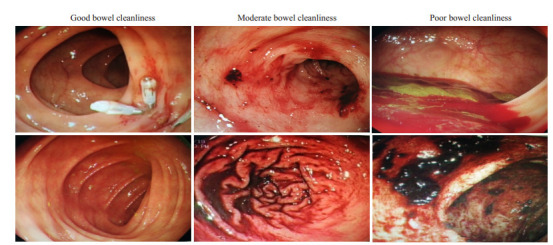
肠道清洁度分级标准
Grading criteria of bowel cleanliness.
本研究将内镜下出血的病变分为“确定性出血灶”和“可疑出血灶”。确定性出血灶:肠腔内有新鲜血液从病变处活动性渗出或病变部位有新鲜血痂附着。可疑出血灶:病变表面发红并在其周围有新鲜血液,同时肠腔内又未观察到其他明确出血点者或虽无上述表现,但被临床医生高度怀疑为出血来源并将此病变作为出院诊断者。肠镜诊断率是指行肠镜检查发现确定性出血灶或可疑出血灶的患者占行肠镜检查的患者的比例。
二次肠镜的时机包括以下几种情况:部分首次肠镜未发现出血来源或病变,但仍高度怀疑结肠出血者、首次肠镜未完成者、首次肠镜治疗后有继续出血表现(便血、黑便、贫血、HGB下降等)者。
1.3. 统计学分析
通过使用IBM SPSS statistics 22来分析所获取的数据,所有的因素都进行了描述性统计,连续性正态分布的变量以均数±标准差的形式表示,采用t检验或秩和检验分析;分类变量通过频数或者率的形式表示,采用卡方检验。多因素分析分组对诊断率影响时采用logistic模型中纳入分组与清洁度的交互效应分析及根据清洁度做分层分析,其较正变量有:性别、年龄、血压(≥100, < 100 mmHg)、心率(≥100, < 100次/min)、察尔森评分(0,1,≥2)、高血压病史、HB(31-60/61-90/ 91-120/>120 g/L)、入院前输血史。Cox回归模型用于分析影响住院时间的因素,采用逐步纳入的方法,选取上述相关变量及手术、二次肠镜以及入院后是否输血。检验水准设为0.05。
2. 结果
2.1. 患者特点
研究共纳入188人,女性63人,男性125人,年龄18~88岁(表 1)。急诊组与择期组在年龄、性别、收缩压、心率、HB、HCT、PLT、INR、察尔森评分以及高血压病史等方面分布上均无统计学差异,而在入院前输血人数比例方面有显著差异(37.3% vs 21.4%,P=0.023)。在肠道准备方式上,急诊组口服泻药比例显著低于择期组(19.5% vs 77.1%,P < 0.001)。
1.
急诊组与择期组患者基线资料对比
Baseline characteristics of the patients in urgent group and elective group
| Characteristics | All patients* | P** | |
| Urgent colonoscopy ( < 24 h) (n=118) | Elective colonoscopy (≥24 h) (n=70) | ||
| *Values are expressed as Mean±SD or the number of patients (%). **Student's t-tests were used for continuous variables, and Pearson's χ test for categorical factors. | |||
| Age (year) | 52.8±17.5 | 52.3±18.4 | 0.855 |
| Gender | 0.884 | ||
| Female | 40 (33.9%) | 23 (32.9%) | |
| Male | 78 (66.1%) | 47 (67.1%) | |
| Charlson comorbidity index | 0.900 | ||
| 0 | 74 (62.7%) | 42 (60.0%) | |
| 1 | 19 (16.1%) | 13 (18.6%) | |
| ≥2 | 25 (21.2%) | 15(21.4%) | |
| SBP (mmHg) | 118.0±24.0 | 119.4± 19.0 | 0.636 |
| < 100 | 10 (8.5%) | 4 (5.7%) | 0.576 |
| Pulse (bpm) | 88.0±17.5 | 91.6±18.5 | 0.185 |
| ≥100 | 31 (26.3%) | 25 (35.7%) | 0.171 |
| HB (g/L) | 0.884 | ||
| > 120 | 13 (11.0%) | 8(11.4%) | |
| 90-120 | 35 (29.7%) | 17 (24.3%) | |
| 61-90 | 52 (44.1%) | 33 (47.1%) | |
| 31-60 | 18 (15.3%) | 12 (17.1%) | |
| HCT (%) | 0.259±0.075 | 0.261±0.075 | 0.879 |
| PLT (G/L) | 210.9±84.0 | 218.6±114.3 | 0.600 |
| PT-INR | 1.17±0.22 | 1.19±0.35 | 0.592 |
| History of hypertension | 0.171 | ||
| Yes | 38 (32.2%) | 16 (22.9%) | |
| No | 80 (67.8%) | 54 (77.1%) | |
| Transfusion requirement before admission | 0.023 | ||
| Yes | 44 (37.3%) | 15(21.4%) | |
| No | 74 (62.7%) | 55 (78.6%) | |
| Bowel preparation | < 0.001 | ||
| Oral laxatives | 23 (19.5%) | 54 (77.1%) | |
| Enemas | 95 (80.5%) | 16 (22.9%) | |
2.2. 急诊组与择期组的肠镜相关结果比较
急诊组与择期组在诊断率方面无统计学差异(44.1% vs 41.4%,P=0.724),急诊组对确定性出血灶的诊断率显著高于择期组(32.2% vs 18.6%,P=0.041),其中镜下发现活动性出血的人数占各组的比例分别是14.4%和10.0%(P=0.381);而急诊组回盲部完成率较低(66.9% vs 78.6%,P=0.089),二次肠镜率较高(30.5% vs 14.3%,P=0.012,表 2)。
2.
急诊组与择期组的镜下检查、治疗结果比较
Comparison of endoscopic outcomes between urgent group and elective group
| Outcome | Urgent colonoscopy | Elective colonoscopy | P* |
| *Pearson's χ test was used to evaluate P value. | |||
| Diagnostic rate | 44.1% | 41.4% | 0.724 |
| Ileocecal intubation | 66.9% | 78.6% | 0.089 |
| State of lesion | 0.041 | ||
| Probable bleeding | 11.9% | 22.9% | |
| Definite bleeding | 32.2% | 18.6% | |
| Repeated colonoscopy | 30.5% | 14.3% | 0.012 |
| Endoscopic therapy | 16.1% | 11.4% | 0.377 |
| Success rate of therapy | 68.4% | 62.5% | 1.000 |
2.3. 不同肠道准备方式对肠道清洁度的影响
肠道清洁度“优”、“良”、“差”在口服泻药及清洁灌肠患者中的比例依次为63.6% vs 13.5%、28.6% vs 24.3%、7.8% vs 62.2%(整体检验组间P < 0.001,图 2)。口服泻药较清洁灌肠时清洁度“优”的比例显著提高(63.6% vs 13.5%,Bonferroni校正后P < 0.001)、清洁度“差”的比例显著降低(7.8% vs 62.2%,Bonferroni校正后P < 0.001),清洁度“良”的比例则无显著差异(28.6% vs 24.3%,Bonferroni校正后P=1.000)。
2.
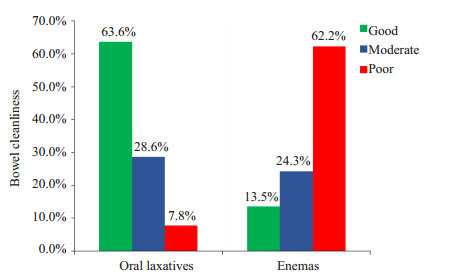
不同肠道准备方式后肠道清洁度比较
Bowel cleanliness after different bowel preparations.
2.4. 多因素Logistic分析镜下诊断率
单因素Logistic分析,结果示清洁度“优”较“差”显著提高肠镜诊断率(OR=2.689,95%CI:1.241-5.827,P= 0.012),但清洁度“优”与“良”时肠镜诊断率无统计学差异(OR=2.041,95%CI:0.871-4.785,P=0.100)。Logistic模型中纳入分组与清洁度交互效应的多因素分析及根据清洁度分层分析的结果显示:清洁度“优”时急诊组诊断率显著高于择期组(P=0.030),清洁度“良”或“差”时,急诊组与择期组对出血灶的诊断率差异无统计学意义;且亚组分析结果显示,急诊组中,清洁度“优”时的肠镜诊断率显著高于清洁度“差”(表 3)。
3.
多因素Logistic分析及亚组分析结果
Multivariate Logistic analysis and subgroup analysis
| Group | Total data analysis* | Stratified analysis** | P | |||
| RR | 95% CI | RR | 95% CI | |||
| *Although the interaction result was not significantly different(P=0.305)in total data analysis, the advantage of urgent group in diagnosis is more obvious than elective group with the improvement of cleanliness. **We considered that the interaction was underpowered to detect a difference. | ||||||
| Urgent vs. Elective | ||||||
| Cleanliness-good | 3.195 | 1.047-9.750 | 4.597 | 1.158-18.254 | 0.030 | |
| Cleanliness-moderate | 1.133 | 0.325-3.945 | 1.967 | 0.406-9.536 | 0.401 | |
| Cleanliness-poor | 0.986 | 0.280-3.475 | 1.536 | 0.366-6.450 | 0.556 | |
| Good vs. poor | ||||||
| Urgent group | 4.350 | 1.576-12.001 | 3.491 | 1.274-9.569 | 0.015 | |
| Elective group | 1.342 | 0.360-4.996 | 1.248 | 0.235-6.629 | 0.795 | |
| Moderate vs. poor | ||||||
| Urgent group | 1.291 | 0.474-3.520 | 1.144 | 0.412-3.177 | 0.797 | |
| Elective group | 1.123 | 0.271-4.651 | 1.095 | 0.211-5.680 | 0.914 | |
| Good vs. moderate | ||||||
| Urgent group | 3.369 | 1.039-10.914 | 3.053 | 0.992-10.112 | 0.068 | |
| Elective group | 1.194 | 0.360-4.996 | 1.140 | 0.219-5.922 | 0.876 | |
2.5. 急诊组与择期组转归比较
两组共47人行外科手术治疗(表 4),急诊组人数显著多于择期组(33.1% vs 11.4%,P=0.001),其中因内科保守治疗效果差而行外科手术的急诊组有34人、择期组6人,其余7人因发现肠道恶性肿瘤行外科治疗。急诊组住院费用显著高于择期组(P=0.003),住院时间较择期组长,但差异无统计学意义(P=0.574)。
4.
急诊组与择期组的临床效果比较
Comparison of clinical outcomes between urgent group and elective group
| Item | Frequency (%)/Median (quartiles) | P* | |
| Urgent colonoscopy | Elective colonoscopy | ||
| *Mann-Whitney U was used for continuous variables, and Pearson's χ test for categorical factors. | |||
| Surgery | 39 (33.1%) | 8 (11.4%) | 0.001 |
| Transfusion requirement | 81 (68.6%) | 47 (67.1%) | 0.831 |
| Transfusion volume (U) | 4 (0, 10) | 3.75 (0, 6) | 0.227 |
| lengths ofstay (d) | 10(6, 15) | 9 (6, 15) | 0.574 |
| Cost (¥) | 28511.0 (14243.5, 58083.5) | 17803.0 (10132.5, 33690.7) | 0.003 |
COX回归分析显示与住院时间延长显著相关的因素有手术治疗(P < 0.001)、二次肠镜(P < 0.001)、入院后输血(P=0.003)。
3. 讨论
目前肠镜已成为急性下消化道大出血患者的首选检查方法,但该检查的最佳时机尚未达成共识。本研究通过单因素分析发现急诊肠镜的诊断率相对择期肠镜并无明显优势,但对确定性出血灶的诊断率高于择期肠镜,由于肠道清洁度较差造成回盲部完成率低于择期组,同时行二次肠镜的比例也明显高于择期组。据文献报道,肠镜对下消化道出血的诊断率达48%~90% [23-25],本研究中首次肠镜诊断率较低,尤其对可疑出血灶的诊断率低于文献报道,主要原因可能是研究对象为急性下消化道大出血,有时肠镜下发现引起大出血可能性小的病变,如表面光滑的结肠憩室、息肉或者痔疮等,未被认定为可疑出血灶,而相同的病变在其他文献中多被定义为可疑出血灶[15, 26]。单因素分析结果示肠道清洁度“优”时肠镜诊断率显著高于“差”时,考虑到清洁度的差异对分析肠镜检查的时机也有影响,故进一步采用纳入分组与清洁度交互效应的多因素分析及亚组分析,结果显示清洁度“优”时,急诊肠镜诊断率显著高于择期肠镜,且行急诊肠镜时,清洁度“优”较“差”显著提高诊断率。因此,我们认为急诊肠镜较择期肠镜的确具有更高的诊断率,但在临床实践中,肠道清洁度不佳的影响使得急诊肠镜的诊断优势并不明显。
本研究中行急诊肠镜的患者口服泻药所占的比例为19.5%,对比Lim,D.S.的研究中35.6% [18],急诊肠镜中使用口服泻药的比例均较低。早期报道若出血量过多,血液可起到部分导泻的作用从而清除大肠中的粪便,所以即使没有充分的肠道准备,内镜下也可有很高的诊断率[20]。最近一项小样本前瞻性研究同样显示:不使用口服泻药,带自冲洗装置的肠镜联合灌肠也是安全有效的。但本研究的结果显示,对比清洁灌肠,口服泻药可以明显提高肠道清洁度,进而提高肠镜诊断率。肠道清洁度为“优”时急诊组的诊断率明显高于择期组,而清洁度“差”时两组并无明显差异。因此若要更好地发挥急诊肠镜的诊断优势,应尽量使用口服泻药提高肠道清洁度。
Lim [18]及Angtuaco等[22]提出对急性下消化道大出血进行肠镜检查应该推迟到患者血流动力学稳定时,并且应该有充分的肠道准备,这样可以提高诊断率并避免对患者造成不必要的风险。本研究中多数患者血流动力学尚稳定,但部分临床医生在患者没有明确口服泻药禁忌的情况下使用清洁灌肠,结果常因肠道清洁度差需行二次肠镜检查。因此,为了提高诊断率,避免不必要的二次肠镜检查,应该加强对肠道准备质量的重视,在患者血流动力学稳定时,尽量选用口服泻药作充分的肠道准备。
本研究中急诊组患者入院时的一般状况及实验室检查结果与择期组相比并无显著差异,但入院前急诊组输血人数要明显多于择期组,这可能是由于急诊组患者病情较择期组更重,院外治疗使入院时两组患者生命体征及化验结果差异并不明显,这也提示了对于病情严重者临床医生更倾向于行急诊肠镜[16]。同时急诊组外科手术人数比例、住院费用均明显高于择期组,这可能也与急诊组病情相对严重有关。此外,本研究结果显示急诊肠镜的执行并不能明显缩短住院时间,住院时间的延长跟手术、二次肠镜及入院后输血均有关。因此我们认为通过提高首次肠镜诊断率,减少不必要的二次肠镜对缩短住院时间更有效。
综上所述,当肠道清洁度为“优”时,急诊肠镜对急性下消化道大出血的诊断率优于择期肠镜,但通过清洁灌肠准备肠道时肠道清洁度差,从而降低了其诊断优势,因此在患者血流动力学稳定的前提下,急诊肠镜肠道准备应尽量选用口服泻药。
Biography
李璟,在读硕士研究生,E-mail: 15622143848@163.com
Funding Statement
广州市科技计划项目(2012J4300091)
Contributor Information
李 璟 (Jing LI), Email: 15622143848@163.com.
何 美蓉 (Meirong HE), Email: hemr@263.net.
References
- 1.Lanas A, García-Rodríguez LA, Polo-Tomás M, et al. Time trends and impact of upper and lower gastrointestinal bleeding and perforation in clinical practice. Am J Gastroenterol. 2009;104(7):1633–41. doi: 10.1038/ajg.2009.164. [Lanas A, García-Rodríguez LA, Polo-Tomás M, et al. Time trends and impact of upper and lower gastrointestinal bleeding and perforation in clinical practice[J]. Am J Gastroenterol, 2009, 104 (7): 1633-41.] [DOI] [PubMed] [Google Scholar]
- 2.García Sánchez M, González Galilea A, López Vallejos P, et al. Role of early colonoscopy in severe acute lower gastrointestinal bleeding. Gastroenterol Hepatol. 2001;24(7):327–32. doi: 10.1016/S0210-5705(01)70187-2. [García Sánchez M, González Galilea A, López Vallejos P, et al. Role of early colonoscopy in severe acute lower gastrointestinal bleeding [J]. Gastroenterol Hepatol, 2001, 24(7): 327-32.] [DOI] [PubMed] [Google Scholar]
- 3.Lhewa DY, Strate LL. Pros and cons of colonoscopy in management of acute lower gastrointestinal bleeding. World J Gastroenterol. 2012;18(11):1185–90. doi: 10.3748/wjg.v18.i11.1185. [Lhewa DY, Strate LL. Pros and cons of colonoscopy in management of acute lower gastrointestinal bleeding[J]. World J Gastroenterol, 2012, 18(11): 1185-90.] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Strate LL, Naumann CR. The role of colonoscopy and radiological procedures in the management of acute lower intestinal bleeding. Clin Gastroenterol Hepatol. 2010;8(4):333–43. doi: 10.1016/j.cgh.2009.12.017. [Strate LL, Naumann CR. The role of colonoscopy and radiological procedures in the management of acute lower intestinal bleeding[J]. Clin Gastroenterol Hepatol, 2010, 8(4): 333-43; quiz e44.] [DOI] [PubMed] [Google Scholar]
- 5.Machicado GA, Jensen DM. Endoscopic diagnosis and treatment of severe lower gastrointestinal bleeding. https://www.researchgate.net/profile/Dennis_Jensen2/publication/6648853_Endoscopic_diagnosis_and_treatment_of_severe_lower_gastrointestinal_bleeding/links/00b4951814172d681d000000.pdf?inViewer=true&disableCoverPage=true&origin=publication_detail. Indian J Gastroenterol. 2006;25(Suppl 1):S43–51. [Machicado GA, Jensen DM. Endoscopic diagnosis and treatment of severe lower gastrointestinal bleeding[J]. Indian J Gastroenterol, 2006, 25(Suppl 1): S43-51.] [PubMed] [Google Scholar]
- 6.Jang BI. Lower gastrointestinal bleeding: is urgent colonoscopy necessary for all hematochezia? Clin Endosc. 2013;46(5):476–9. doi: 10.5946/ce.2013.46.5.476. [Jang BI. Lower gastrointestinal bleeding: is urgent colonoscopy necessary for all hematochezia[J]? Clin Endosc, 2013, 46(5): 476-9.] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.李 承恩, 欧 希龙, 贺 永军, et al. 下消化道出血结肠镜检查方法探讨及结果分析. http://www.cnki.com.cn/Article/CJFDTOTAL-TDYX201105005.htm. 现代医学. 2011;39(5):520–3. [李承恩, 欧希龙, 贺永军, 等.下消化道出血结肠镜检查方法探讨及结果分析[J].现代医学, 2011, 39(5): 520-3.] [Google Scholar]
- 8.Strate LL. Editorial: urgent colonoscopy in lower GI bleeding: not so fast. Am J Gastroenterol. 2010;105(12):2643–5. doi: 10.1038/ajg.2010.401. [Strate LL. Editorial: urgent colonoscopy in lower GI bleeding: not so fast[J]. Am J Gastroenterol, 2010, 105(12): 2643-5.] [DOI] [PubMed] [Google Scholar]
- 9.Green BT, Rockey DC, Portwood G, et al. Urgent colonoscopy for evaluation and management of acute lower gastrointestinal hemorrhage: a randomized controlled trial. Am J Gastroenterol. 2005;100(11):2395–402. doi: 10.1111/ajg.2005.100.issue-11. [Green BT, Rockey DC, Portwood G, et al. Urgent colonoscopy for evaluation and management of acute lower gastrointestinal hemorrhage: a randomized controlled trial[J]. Am J Gastroenterol, 2005, 100(11): 2395-402.] [DOI] [PubMed] [Google Scholar]
- 10.Schmulewitz N, Fisher DA, Rockey DC. Early colonoscopy for acute lower GI bleeding predicts shorter hospital stay: a retrospective study of experience in a single center. Gastrointest Endosc. 2003;58(6):841–6. doi: 10.1016/S0016-5107(03)02304-6. [Schmulewitz N, Fisher DA, Rockey DC. Early colonoscopy for acute lower GI bleeding predicts shorter hospital stay: a retrospective study of experience in a single center[J]. Gastrointest Endosc, 2003, 58(6): 841-6.] [DOI] [PubMed] [Google Scholar]
- 11.Nagata N, Niikura R, Sakurai T, et al. Safety and effectiveness of early colonoscopy in management of acute lower gastrointestinal bleeding on the basis of propensity score matching analysis. Clin Gastroenterol Hepatol. 2016;14(4):558–64. doi: 10.1016/j.cgh.2015.10.011. [Nagata N, Niikura R, Sakurai T, et al. Safety and effectiveness of early colonoscopy in management of acute lower gastrointestinal bleeding on the basis of propensity score matching analysis[J]. Clin Gastroenterol Hepatol, 2016, 14(4): 558-64.] [DOI] [PubMed] [Google Scholar]
- 12.Navaneethan U, Njei B, Venkatesh PG, et al. Timing of colonoscopy and outcomes in patients with lower GI bleeding: a nationwide population-based study. Gastrointest Endosc. 2014;79(2):297–306.e12. doi: 10.1016/j.gie.2013.08.001. [Navaneethan U, Njei B, Venkatesh PG, et al. Timing of colonoscopy and outcomes in patients with lower GI bleeding: a nationwide population-based study[J]. Gastrointest Endosc, 2014, 79(2): 297-306.e12.] [DOI] [PubMed] [Google Scholar]
- 13.赵 晓军, 李 娜, 王 海红, et al. 急诊结肠镜在急性下消化道出血诊断及治疗中的应用价值. http://www.cnki.com.cn/Article/CJFDTOTAL-WCBX201208015.htm. 胃肠病学和肝病学杂志. 2012;21(8):730–2. [赵晓军, 李娜, 王海红, 等.急诊结肠镜在急性下消化道出血诊断及治疗中的应用价值[J].胃肠病学和肝病学杂志, 2012, 21(8): 730-2.] [Google Scholar]
- 14.Smoot RL, Gostout CJ, Rajan E, et al. Is early colonoscopy after admission for acute diverticular bleeding needed? Am J Gastroenterol. 2003;98(9):1996–9. doi: 10.1111/j.1572-0241.2003.07635.x. [Smoot RL, Gostout CJ, Rajan E, et al. Is early colonoscopy after admission for acute diverticular bleeding needed[J]? Am J Gastroenterol, 2003, 98(9): 1996-9.] [DOI] [PubMed] [Google Scholar]
- 15.Laine L, Shah A. Randomized trial of urgent vs. elective colonoscopy in patients hospitalized with lower GI bleeding. Am J Gastroenterol. 2010;105(12):2636–41; quiz 2642. doi: 10.1038/ajg.2010.277. [Laine L, Shah A. Randomized trial of urgent vs. elective colonoscopy in patients hospitalized with lower GI bleeding[J]. Am J Gastroenterol, 2010, 105(12): 2636-41; quiz 2642.] [DOI] [PubMed] [Google Scholar]
- 16.Albeldawi M, Ha D, Mehta P, et al. Utility of urgent colonoscopy in acute lower gastro-intestinal bleeding: a single-center experience. Gastroenterol Rep (Oxf) 2014;2(4):300–5. doi: 10.1093/gastro/gou030. [Albeldawi M, Ha D, Mehta P, et al. Utility of urgent colonoscopy in acute lower gastro-intestinal bleeding: a single-center experience [J]. Gastroenterol Rep (Oxf), 2014, 2(4): 300-5.] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Saito K, Inamori M, Sekino Y, et al. Management of acute lower intestinal bleeding: what bowel preparation should be required for urgent colonoscopy? Hepatogastroenterology. 2009;56(94/95):1331–4. [Saito K, Inamori M, Sekino Y, et al. Management of acute lower intestinal bleeding: what bowel preparation should be required for urgent colonoscopy[J]? Hepatogastroenterology, 2009, 56(94/95): 1331-4.] [PubMed] [Google Scholar]
- 18.Lim DS, Kim HG, Jeon SR, et al. Comparison of clinical effectiveness of the emergent colonoscopy in patients with hematochezia according to the type of bowel preparation. J Gastroenterol Hepatol. 2013;28(11):1733–7. doi: 10.1111/jgh.2013.28.issue-11. [Lim DS, Kim HG, Jeon SR, et al. Comparison of clinical effectiveness of the emergent colonoscopy in patients with hematochezia according to the type of bowel preparation[J]. J Gastroenterol Hepatol, 2013, 28(11): 1733-7.] [DOI] [PubMed] [Google Scholar]
- 19.Repaka A, Atkinson MR, Faulx AL, et al. Immediate unprepared hydroflush colonoscopy for severe lower GI bleeding: a feasibility study. Gastrointest Endosc. 2012;76(2):367–73. doi: 10.1016/j.gie.2012.03.1391. [Repaka A, Atkinson MR, Faulx AL, et al. Immediate unprepared hydroflush colonoscopy for severe lower GI bleeding: a feasibility study[J]. Gastrointest Endosc, 2012, 76(2): 367-73.] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Chaudhry V, Hyser MJ, Gracias VH, et al. Colonoscopy: the initial test for acute lower gastrointestinal bleeding. https://www.researchgate.net/publication/13587170_Colonoscopy_The_initial_test_for_acute_lower_gastrointestinal_bleeding. Am Surg. 1998;64(8):723–8. [Chaudhry V, Hyser MJ, Gracias VH, et al. Colonoscopy: the initial test for acute lower gastrointestinal bleeding[J]. Am Surg, 1998, 64 (8): 723-8.] [PubMed] [Google Scholar]
- 21.刘 涵, 陈 磊, 徐 世伟, et al. 急诊结肠镜检查在急性下消化道出血诊治中的价值. http://www.cnki.com.cn/Article/CJFDTOTAL-ZZLC201608016.htm. 临床急诊杂志. 2016;17(8):628–30. [刘涵, 陈磊, 徐世伟, 等.急诊结肠镜检查在急性下消化道出血诊治中的价值[J].临床急诊杂志, 2016, 17(8): 628-30.] [Google Scholar]
- 22.Angtuaco TL, Reddy SK, Drapkin S, et al. The utility of urgent colonoscopy in the evaluation of acute lower gastrointestinal tract bleeding: a 2-year experience from a single center. Am J Gastroenterol. 2001;96(6):1782–5. doi: 10.1111/j.1572-0241.2001.03871.x. [Angtuaco TL, Reddy SK, Drapkin S, et al. The utility of urgent colonoscopy in the evaluation of acute lower gastrointestinal tract bleeding: a 2-year experience from a single center[J]. Am J Gastroenterol, 2001, 96(6): 1782-5.] [DOI] [PubMed] [Google Scholar]
- 23.Ohyama T, Sakurai Y, Ito M, et al. Analysis of urgent colonoscopy for lower gastrointestinal tract bleeding. Digestion. 2000;61(3):189–92. doi: 10.1159/000007756. [Ohyama T, Sakurai Y, Ito M, et al. Analysis of urgent colonoscopy for lower gastrointestinal tract bleeding[J]. Digestion, 2000, 61(3): 189-92.] [DOI] [PubMed] [Google Scholar]
- 24.Davila RE, Rajan E, Adler DG, et al. ASGE guideline: the role of endoscopy in the patient with lower-GI bleeding. Gastrointest Endosc. 2005;62(5):656–60. doi: 10.1016/j.gie.2005.07.032. [Davila RE, Rajan E, Adler DG, et al. ASGE guideline: the role of endoscopy in the patient with lower-GI bleeding[J]. Gastrointest Endosc, 2005, 62(5): 656-60.] [DOI] [PubMed] [Google Scholar]
- 25.Strate LL, Syngal S. Timing of colonoscopy: impact on length of hospital stay in patients with acute lower intestinal bleeding. http://www.nature.com/ajg/journal/v98/n2/fig_tab/ajg200383t2.html?message=remove. Am J Gastroenterol. 2003;98(2):317–22. doi: 10.1111/j.1572-0241.2003.07232.x. [Strate LL, Syngal S. Timing of colonoscopy: impact on length of hospital stay in patients with acute lower intestinal bleeding[J]. Am J Gastroenterol, 2003, 98(2): 317-22.] [DOI] [PubMed] [Google Scholar]
- 26.Elta GH. Urgent colonoscopy for acute lower-GI bleeding. Gastrointest Endosc. 2004;59(3):402–8. doi: 10.1016/S0016-5107(03)02721-4. [Elta GH. Urgent colonoscopy for acute lower-GI bleeding[J]. Gastrointest Endosc, 2004, 59(3): 402-8.] [DOI] [PubMed] [Google Scholar]


