Abstract
The KRAS oncoprotein, a critical driver in 33% of lung adenocarcinoma (LUAD), has remained an elusive clinical target due to its perceived undruggable nature. The identification of dependencies borne through common co-occurring mutations are sought to more effectively target KRAS-mutant lung cancer. Approximately 20% of KRAS-mutant LUAD carry loss-of-function mutations in KEAP1, a negative regulator of the antioxidant response transcription factor NFE2L2/NRF2. We demonstrate that Keap1-deficient KrasG12D lung tumors arise from a bronchiolar cell-of-origin, lacking pro-tumorigenic macrophages observed in tumors originating from alveolar cells. Keap1 loss activates the pentose phosphate pathway, inhibition of which, using 6-AN, abrogated tumor growth. These studies highlight alternative therapeutic approaches to specifically target this unique subset of KRAS-mutant LUAD cancers.
Subject terms: Cancer metabolism, Cancer microenvironment, Cancer models, Non-small-cell lung cancer
Lung adenocarcinomas frequently harbour KRAS mutations, of which a subset are characterized by co-mutation of KEAP1. Here the authors show, in mice, that KrasG12D mutant tumours are metabolically distinct, with a bronchiolar cell-of-origin.
Introduction
The Kirsten Rat Sarcoma viral oncogene homolog (KRAS) oncoprotein is a critical driver in 22% of all cancers1. Constitutive GTPase function is gained through a point mutation, typically at codon 12, 13 or 612, responsible for the hyperactivation of key proliferative and survival pathways. Unlike other key oncoproteins in cancer (i.e., EGFR, HER2, ALK), KRAS has remained an elusive clinical target in cancer due to its perceived undruggable nature3. In lung cancer, KRAS is most frequently mutated in lung adenocarcinoma (LUAD), where it is altered in 33% of patients4.
Genetically engineered mouse models (GEMMs) based on temporal and spatial expression of oncogenic Kras5,6 have proven instrumental in understanding the molecular and cellular events that underpin this genetic subset of tumors. Alveolar type 2 cells appear to be the predominant cell-of-origin of KrasG12D-mutant tumors6,7. However, as seen in other lung cancer subsets, a high level of plasticity likely exists within the lung epithelium with multiple cell populations capable of transformation given an appropriate stimulus8,9. In murine models, co-mutation of critical tumor suppressor genes p53 and Lkb1 accelerate KrasG12D-induced tumorigenesis and in the case of Lkb1 inactivation, alter the tumor spectrum10,11. In line with the model that genetic alterations can drive a distinct immune response12, tumor-bearing lungs from KrasG12D-mutant mice exhibit an increase in alveolar macrophages. This is thought to be driven by an inflammatory response13, though the mechanism is not well understood. Despite this progress, chemotherapy, radiotherapy and/or surgery remain the standard-of-care for patients with KRAS-mutant lung cancer. Indeed, the recent identification of dependencies borne through common co-occurring mutations provide an appealing strategy to target KRAS-mutant lung cancer.
Approximately 20% of KRAS-mutant LUAD carry loss-of-function mutations in Kelch-like ECH-associated protein 1 (KEAP1)14. A key member of the antioxidant response pathway, KEAP1 functions as a negative regulator of the transcription factor nuclear factor erythroid 2-like 2 (NFE2L2/NRF2)15. Loss-of-function mutations in KEAP1 activate the NRF2 pathway, which in turn alters the transcription of over 200 downstream genes, involved in cellular antioxidant, detoxification, and metabolic pathways16. In GEMMs, we have previously described a synergy between the Keap1/Nrf2 and PI3K pathways in LUAD17. However, controversy exists over the capacity of Keap1 to function as a tumor suppressor in the context of KrasG12D-driven lung cancer18–21, where the ability to accelerate tumorigenesis in the absence of additional loss-of-function mutations in p53 or Lkb1 remains unclear18.
Here, we identify dependencies in the KEAP1-mutant LUAD subgroup through the generation of GEMMs based on Cre-inducible expression of oncogenic KrasG12D and combined loss of Keap1. Strikingly, we show that Keap1-deficient KrasG12D tumors arise from a bronchiolar cell-of-origin, without the concomitant induction of pro-tumorigenic alveolar macrophage expansion observed in tumors originating from alveolar cells. Furthermore, Keap1 loss reprogrammed the metabolic wiring of oncogenic KrasG12D tumor cells by hijacking the pentose phosphate pathway (PPP). Treatment with the PPP inhibitor 6-aminonicotinamide (6-AN) abrogated the growth of Keap1-deficient tumor cells, suggesting a potential therapeutic approach to target this subset of KRAS-mutant LUAD cancers.
Results
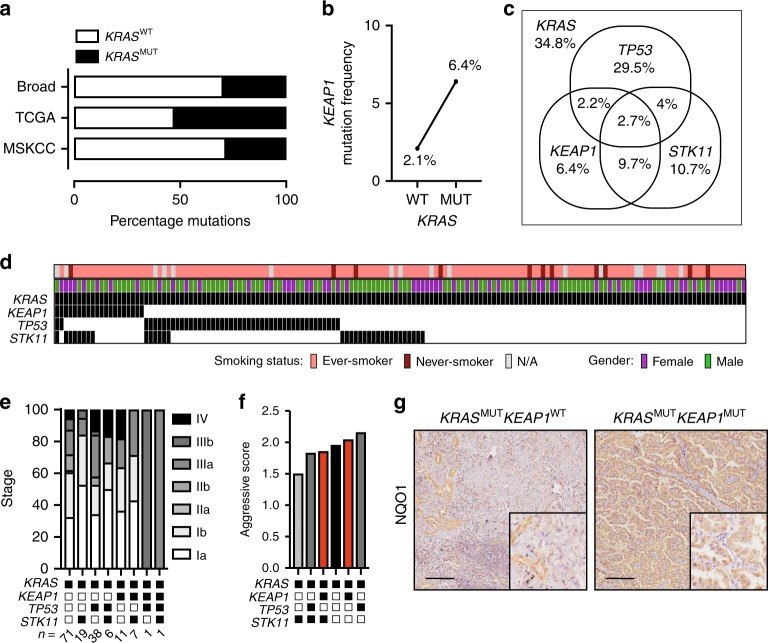
KEAP1 alterations are enriched in KRAS-mutant LUAD
To investigate the key genetic alterations in KRAS-mutant NSCLC, we interrogated large publicly available datasets from the Broad Institute22, the Cancer Genome Atlas4 and the Memorial Sloan Kettering Cancer Center (MSKCC)23 using cBioPortal24,25. KRAS was mutated in 36.9% of cases (Fig. 1a and Supplementary Table 1), with a notable increase in mutation frequency of KEAP1 in KRAS-mutant cases compared to KRAS-WT (Fig. 1b). Top co-mutated genes TP53, KEAP1 and STK11 were interrogated for their mutual exclusivity and co-mutation frequency. In accordance with previous findings14, TP53 and KEAP1 were seldom co-mutated, while co-mutation of KEAP1 and STK11 was more frequent (Fig. 1c and Supplementary Fig. 1 and Supplementary Table 1). Importantly, a significant proportion of KRAS-mutant LUAD were mutant for either KEAP1 or STK11, highlighting that these mutations also occur independently.
Fig. 1.
KEAP1 mutation is enriched in KRAS-mutant lung adenocarcinoma. a Frequency of KRAS mutation in lung adenocarcinoma (LUAD) obtained from the Broad Institute (n = 182), The Cancer Genome Atlas (n = 313) and the Memorial Sloan Kettering Cancer Center (MSKCC) (n = 864). b Frequency of KEAP1 mutation status in KRAS WT (wild type; n = 921) or MUT (mutant; n = 627) LUAD samples. c Venn Diagram of co-mutation/mutual exclusivity of KEAP1, TP53, and STK11 mutations in the subset of KRAS-mutant LUAD (n = 627). d KEAP1, TP53, and STK11 mutation status in KRAS-mutant LUAD patient samples from the Clinical Lung Cancer Genome Project (CLCGP) cohort (n = 155). e Frequency of clinical stage in subsets of KRAS-mutant LUAD from (d). f Aggressive score assessed by clinical stage in each KRAS-mutant subgroup. g NQO1 immunostaining on KRASMUTKEAP1WTTP53MUT and KRASMUTKEAP1MUTTP53WT patient samples. Scale, 200 μm
To verify these findings in an independent LUAD dataset, we mined 161 KRAS-mutant patient samples from the Clinical Lung Cancer Genome Project (CLCGP)26. Patient stratification by co-mutation found a similar frequency of KEAP1-only, KEAP1/STK11, TP53 only, TP53/STK11, and STK11 only samples (Fig. 1d and Supplementary Data 1). Interestingly, KRAS-mutant tumors co-mutated with TP53 or KEAP1 only were associated with increased tumor stage (Fig. 1e, f) suggesting that inactivation of these tumor suppressors drives a more aggressive tumor phenotype. Furthermore, expression of the NRF2 transcriptional target, NAD(P)H:quinone dehydrogenase 1 (NQO1) was elevated in KRAS-mutant LUAD, co-mutant for KEAP1 (Fig. 1g), confirming its potential as a clinical biomarker for this subgroup of patients17,18.
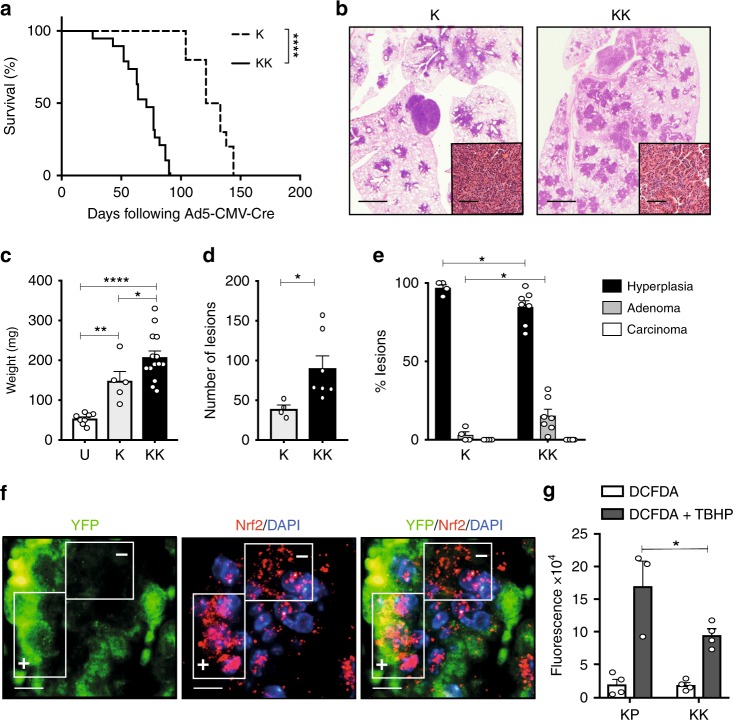
Keap1 loss accelerates KrasG12D-induced lung tumorigenesis
To date, CRISPR/Cas9 technology has been utilized to investigate the functional consequences of Keap1 inactivation concomitant with activation of oncogenic KrasG12D19,20. Discrepancies, however, exist between these studies and the clinical relevance questionable, with models generated reflecting a minor subclass of human tumors18. To overcome this, we crossed loxP-STOP-loxP KrasG12D/+5 (K) with mice carrying the Keap1flox/flox allele27 (KrasG12D/+;Keap1flox/flox; hereafter KK). Consistent with the aggressive nature of KEAP1-mutant LUAD18,28, Ad5-CMV-Cre-infected KK mice exhibited a significantly reduced lifespan compared to K mice, with a median survival of 71 and 127 days, respectively (Fig. 2a; Mantel-Cox test p > 0.0001). At autopsy, moribund mice had significant lung tumor burden (Fig. 2b) and no additional abnormalities or metastases. In line with reduced survival rates, the lungs of KK mice, analyzed 3 months following Ad5-CMV-Cre infection, were significantly heavier (Fig. 2c), and displayed an increased number of lesions (Fig. 2d) compared to the lungs of K mice. Quantification of the tumor spectrum revealed a significant increase in the frequency of adenomas in KK mice compared to K only control mice (Fig. 2e). Consistent with activation of the Nrf2 pathway following loss of Keap1, Nrf2 was concentrated in the nucleus of recombined cells (Fig. 2f) in KK mice expressing a YFP reporter allele29. Moreover, cell lines derived from KK tumors displayed a greater clearance of reactive oxygen species (Fig. 2g), further exemplifying the enhanced function of the Nrf2 pathway in tumors with loss of Keap1. Together, these data indicate that Keap1 is a potent tumor suppressor in KrasG12D-induced lung tumorigenesis.
Fig. 2.
Keap1 inactivation accelerates KrasG12D-induced lung adenocarcinoma. a Survival analysis of K (n = 10) and KK (n = 19) mice following Ad5-CMV-Cre administration. Mantel-Cox test: ****p < 0.0001. b Hematoxylin and eosin (H&E) stained lungs of representative K and KK mice at ethical endpoint. Scale, 1 mm; inset, 100 μm. c Weight of left lung lobe of uninfected littermates (U, n = 8), K (n = 5) and KK (n = 14) mice 3 months following Ad5-CMV-Cre infection. Ordinary one-way ANOVA/Holm-Sidak’s multiple comparisons test: U v K: **p = 0.006; U v KK: ****p < 0.0001; K v KK: *p = 0.0327. Mean ± SEM. d Number of lesions in the lungs of K (n = 4) and KK (n = 7) mice 3 months post Ad5-CMV-Cre. Ordinary one-way ANOVA/Tukey’s multiple comparisons test K v KK *p = 0.0397. Mean ± SEM. e Lesion classification of K (n = 4) and KK (n = 7) lungs 3 months post Ad5-CMV-Cre infection. Two-way ANOVA/Tukey’s multiple comparisons test: alveolar hyperplasia K v KK *p = 0.05, adenoma K v KK *p = 0.05. Mean ± SEM. f Immunofluorescence of EYFP and Nrf2 expression in EYFPT/+;KrasG12D/+;Keap1Δ/Δ three months following Ad5-CMV-Cre infection. Boxes represent EYFP positive and negative regions. Scale, 10 μm. g Quantification of 2,7-dichlorofluorescin diacetate (DCFDA) alone or in combination with 110 μM tert-butyl hydrogen peroxide (TBHP) to stimulate reactive oxygen species (ROS) in primary cell lines (n = 4 KP and KK). Mann–Whitney test DCFDA + TBHP KP v KK *p = 0.0286. Mean ± SEM
While these findings suggest that Keap1 can exert its tumor suppressive function in a p53- and Lkb1-indpendent manner, the co-occurrence of KEAP1 mutations with STK11, and to a lesser extent TP53, in KRAS-mutant tumors may imply that cancer cells gain additional growth advantage. To systematically evaluate this hypothesis, Keap1flox/flox mice were crossed with KrasG12D/+;p53flox/flox mice10 (hereafter KPK) and KrasG12D/+;Lkb1flox/flox mice30 (hereafter KLK). KrasG12D/+;p53flox/flox (KP) and KrasG12D/+;Lkb1flox/flox (KL) mice served as controls. Lung tumor induction was monitored in cohorts of mice following intranasal Ad5-CMV-Cre delivery. Keap1 loss minimally impacted the survival rate of KP (KPK mice; 57 days versus KP mice; 83 days; Mantel-Cox test p = 0.36; Supplementary Fig. 2a) and KL (KLK mice; 49 days versus KL; 43 days) mice (Table 1). No lung tumors were observed in mice carrying bi-allelic inactivation of Keap1 and Lkb1 or Keap1 and p53 (Table 1), indicating the requirement of a collaborative oncogene to drive tumorigenesis. Consistent with activation of the Nrf2 pathway following loss of Keap1, lung tumor pieces from KK, KPK, and KLK GEMMs all displayed enhanced Nqo1 transcriptional activation (Supplementary Fig. 2b), further exemplifying the enhanced function of the Nrf2 pathway in tumors with loss of Keap1. With the exception of KLK mice, all lesions displayed an adenomatous phenotype, with increased Nkx2.1 expression (Supplementary Fig. 2c), while the lungs of KLK mice displayed a mixture of adenomatous and squamous lesions (Supplementary Fig. 2d). Importantly, while Keap1 does not significantly collaborate with p53 or Lkb1 loss to accelerate KrasG12D-induced tumorigenesis, all tumor cells harboring Keap1 inactivation exhibit augmented Nrf2 pathway activation.
Table 1.
Comparison of murine lung cancer model cohorts
| Genotype | # of mice infected | Survival (range)a | Histopathology |
|---|---|---|---|
| Kras G12D/+ | 10 | 127 (104–144) | Adenomatous |
| KrasG12D/+;p53Δ/Δ | 10 | 83 (60–91) | Adenomatous |
| KrasG12D/+;Keap1Δ/Δ | 19 | 71 (26–90) | Adenomatous |
| Keap1 Δ/Δ17 | 26 | >365 | No lesions |
| Keap1Δ/Δ;p53Δ/Δ | 10 | >365 | No lesions |
| KrasG12D/+;Lkb1Δ/Δ | 8 | 43 (37–101) | Mixture of adenomatous and squamous |
| Keap1Δ/Δ;Lkb1Δ/Δ | 10 | >365 | No lesions |
| KrasG12D/+;p53Δ/Δ;Keap1Δ/Δ | 5 | 57 (55–104) | Adenomatous |
| KrasG12D/+;Lkb1Δ/Δ;Keap1Δ/Δ | 9 | 49 (30–64) | Mixture of adenomatous and squamous |
aMedian survival is represented as days following intra-nasal injection of 2 × 108 PFU Ad5-CMV-Cre virus
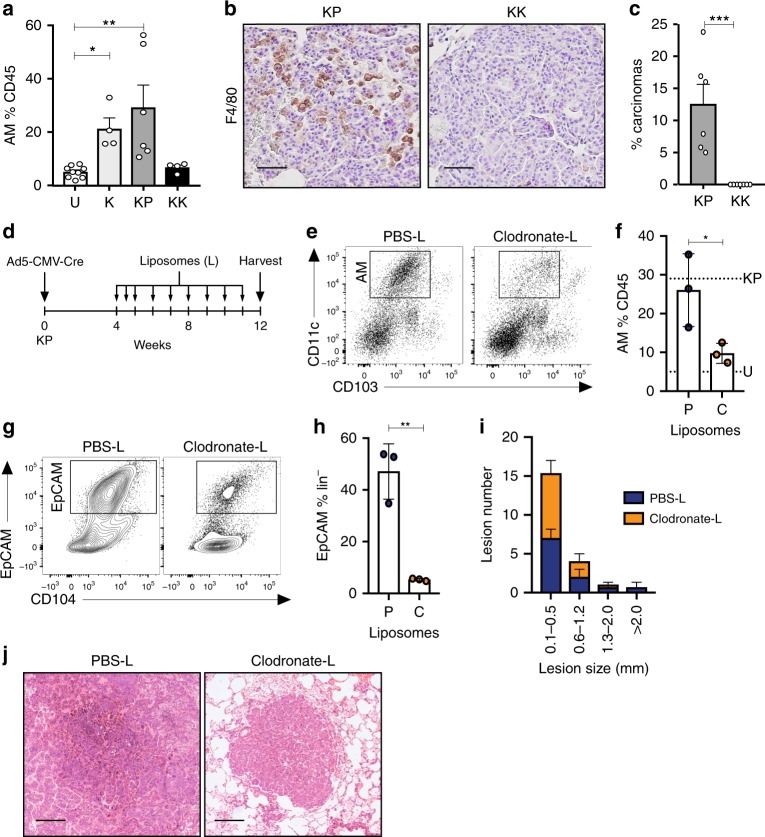
Reduced inflammatory response in Keap1-deficient tumors
Given the emerging evidence linking the inactivation of specific tumor suppressors with unique immune microenvironments of KRAS-mutant LUAD14,31,32, we interrogated the immune cell composition of Keap1-deficient tumors using a multiparametric flow cytometry approach17. KK and KP mice were used for this analysis, due to similarities in tumor phenotype and latency between models (Table 1). The presence of adenomatous and squamous lesions in KLK mice (Supplementary Fig. 2d and Table 1) prohibited the use of this model, as the immune milieu of squamous tumors appears to be distinct to that of LUAD8,33. Consistent with previous findings13, the alveolar macrophage compartment (CD45+CD11c+CD103−) was significantly altered in the lungs of tumor-bearing K and KP mice compared to non-tumor bearing control mice (Fig. 3a and Supplementary Fig. 3a). In stark contrast however, no expansion in alveolar macrophages was observed in the lungs of KK tumor-bearing mice. Critically, macrophage expansion was an early tumorigenic event in KP mice, with infiltration already apparent in atypical adenomatous hyperplastic (AAH) lesions (Supplementary Fig. 3b). Immunohistochemical staining using F4/80, a well-characterized macrophage marker, confirmed these observations in established tumors (Fig. 3b). Interestingly, no differences in the phenotype of infiltrating alveolar macrophages was detected (Supplementary Fig. 3c–e), nor were any significant alterations in the expression of GM-CSF or secretion of IL-6 and TNFα observed in KK and KP tumor cells (Supplementary Fig. 3f–h) that could explain the difference in macrophage recruitment between the KK and KP tumor subgroups. Intriguingly, although the latency of KK and KP mice were similar, there was an increase in carcinomatous lesions in KP mice (Fig. 3c). To investigate whether the increased macrophages were playing a role in tumor development, we reduced alveolar macrophage numbers in KP mice through intranasal administration of Clodronate-loaded liposomes (Fig. 3d). Alveolar macrophages were effectively reduced in KP lungs to levels comparable to that of non-tumor bearing mice (U) 12 weeks following Ad5-CMV-Cre (Fig. 3e, f). Strikingly, the epithelial compartment in clodronate treated KP mice was significantly reduced compared to PBS control-treated mice (Fig. 3g, h). Consistent with this finding, tumor size was reduced in clodronate treated KP mice (Fig. 3i, j and Supplementary Fig. 3i). Taken together, these findings suggest that alveolar macrophages infiltrating the lungs of KP mice are tumor-promoting.
Fig. 3.
Alveolar macrophages contribute to KrasG12D-induced tumorigenesis. a Quantification of alveolar macrophages (CD11c+CD11b−CD103−) in CD45+ immune lung infiltrate in uninfected (U; n = 9) and K (n = 4), KP (n = 6), KK (n = 4) mice 3 months post Ad5-CMV-Cre infection. Kruskal–Wallis test/Dunn’s multiple comparisons test U v K *p = 0.0127; U v KP **p = 0.0042. Mean ± SEM. b F4/80 immunostaining on KP and KK lung tissue 3 months post Ad5-CMV-Cre infection. Scale, 50 μm. c Frequency of carcinomatous lesions in KP (n = 6) and KK (n = 7) lungs 3 months post Ad5-CMV-Cre infection. Unpaired t test ***p = 0.001. Mean ± SEM. d Schematic of treatment plan. Briefly, KP mice were administered weekly PBS-liposomes or Clodronate-liposomes four weeks following Ad5-CMV-Cre infection. Lungs were harvested and analyzed for alveolar macrophages and tumor burden following 8 weeks of liposome treatment. e Representative flow cytometry plot of alveolar macrophage population (CD45+CD11c+CD103−) in the lungs of PBS- or Clodronate-liposome (L) treated mice. f Quantification of alveolar macrophages as a proportion of CD45+ cells in the lungs of KP mice treated with PBS (P; n = 3) or Clodronate (C; n = 3) liposomes. Dotted line represents mean value of alveolar macrophages in KP and U from (a), above. Unpaired t test *p = 0.0443. Mean ± SD. g Representative flow cytometry plot of epithelial cells (EpCAM+) in the lungs of PBS or Clodronate liposome treated mice. h Quantification of EpCAM+ population as a proportion of lineage negative (CD31−CD45−) cells. Unpaired t test **p = 0.0025. Mean ± SD. i Quantification of lesion size in PBS- and Clodronate-liposome (L) treated mice. j Representative H&E of PBS- and Clodronate-liposome (L) treated mice. Scale, 200 μm
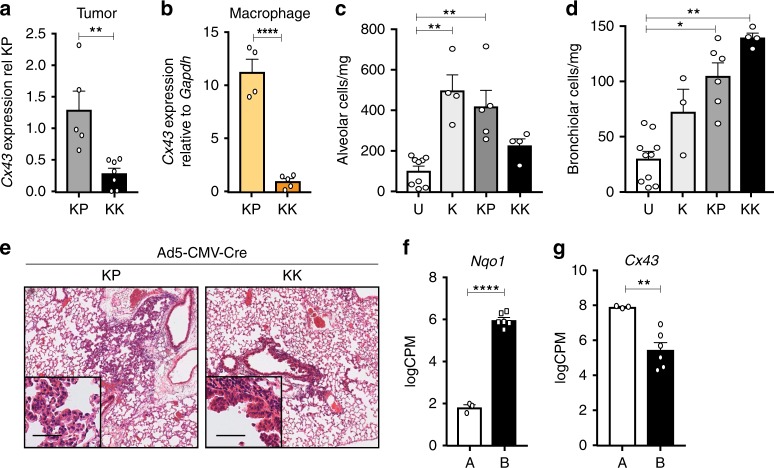
Bronchiolar cells are sensitive to Nrf2 hyperactivation
To investigate the absence of alveolar macrophage infiltration in KK tumor-bearing lungs, we dissected the mechanisms by which alveolar macrophages interact with epithelial cells. Alveolar macrophages are believed to directly interact with alveolar type 2 (AT2) epithelial cells via CD20034,35 and/or the gap junction Connexin-43 (Cx43)36. Whilst no difference in CD200 expression was detected between KP and KK tumors (Supplementary Fig. 4a), significantly lower Cx43 expression was observed in FACS-isolated tumor cells (Fig. 4a) and alveolar macrophages (Fig. 4b) from KK lungs. To evaluate this relationship in patient samples, we curated a consensus NRF2 signature based on published NRF2 signatures (Supplementary Fig. 4b) and stratified KRAS-mutant LUAD samples from the TCGA cohort into low and high NRF2 subgroups based on NRF2 signature expression (Supplementary Fig. 4c). Critically, GJA1/CX43 expression was significantly decreased in KRAS-mutant LUAD with a high NRF2 score (Supplementary Fig. 4d), suggesting that NRF2 pathway activity negatively correlates with Cx43 expression, concordant with the GEMM findings (Fig. 4a). In line with the utilization of NQO1 as a clinical biomarker of NRF2 pathway activity, expression of NQO1 alone stratified the NRF2 signature (Supplementary Fig. 4e) and distribution of KRAS-mutant LUAD samples from the TCGA cohort based on NQO1 expression similarly negatively correlated with GJA1/CX43 expression (Supplementary Fig. 4f). Importantly, these findings further support the use of NQO1 as a single-gene biomarker for NRF2 pathway activity. Next, we sought to functionally assess the importance of Cx43 gap junctions in the interaction between alveolar cells and alveolar macrophages. We exposed the lungs of healthy adult mice to intranasal inhalation of an intracellular inhibitor of Cx43, Gap19 peptide. Extended exposure to Gap19 resulted in the displacement of alveolar macrophages from the lungs (Supplementary Fig. 4g), confirming the importance of Cx43 in mediating epithelial-immune cell interactions. Consistent with the proposed expression of Cx43 in alveolar cells themselves36, the tumor-bearing lungs of KK mice displayed a reduced alveolar compartment (Fig. 4c). Interestingly, and consistent with a bronchiolar trophism observed in previous models of Keap1 loss17, KK tumor-bearing lungs were characterized by elevated levels of EpCAM+CD104+ bronchiolar cells (Fig. 4d) and increased expression of Scgb1a1, a marker of Club cells (Supplementary Fig. 5a). To further evaluate the cell-types that undergo initial transformation upon recombination, lungs of KP and KK mice were analyzed 3-weeks following Ad5-CMV-Cre infection, prior to the onset of overt malignant disease (Supplementary Fig. 5b). AAH was pronounced in the lungs of KP mice (Fig. 4e and Supplementary Fig. 5c), consistent with an alveolar cell-of-origin in KrasG12D induced tumors6,7,37. In contrast, hyperplasia of the bronchiolar epithelium was predominant in the lungs of KK mice at this time, while AAH was not detected (Fig. 4e and Supplementary Fig. 5d). To interrogate why bronchiolar cells are more sensitive to transformation upon enhanced activation of the Nrf2 pathway, we performed KEGG pathway analysis of alveolar and bronchiolar cells purified from normal murine lung epithelium38. Although primary transcript levels of Nrf2 and Keap1 were comparable between the two epithelial compartments (Supplementary Fig. 6a), ubiquitin ligase pathways that mediate Nrf2 post-translational degradation were expressed at significantly higher levels in alveolar cells (Supplementary Fig. 6b; Differential ROAST analysis p = 1.29 × 10−9). In line with these findings, expression of antioxidant genes and glutathione transferases regulated by the Nrf2 pathway were enriched in the bronchiolar compartment (Supplementary Fig. 6c; Differential ROAST analysis p = 5 × 10−4) as was the expression of Nrf2 target gene Nqo1 (Fig. 4f). To further dissect this relationship, we applied the NRF2 consensus signature score (Supplementary Fig. 4b) to differentially expressed genes in the alveolar and bronchiolar compartments. Interestingly, a significant correlation was observed between the NRF2 signature and the bronchiolar compartment (Supplementary Fig. 6d). Together, these findings suggest that bronchiolar cells have increased basal activity of the Nrf2 pathway and thus are more responsive to Nrf2-mediated transformation. Moreover, consistent with previous imaging observations36, Cx43 expression was enriched specifically in normal alveolar epithelium (Fig. 4g). Taken together, these findings suggest that the decreased expression of Cx43 (Fig. 4a) and absence of macrophage expansion (Fig. 3a) may be due to a distinct bronchiolar, rather than alveolar, cell-of-origin of KK tumors.
Fig. 4.
Keap1 loss preferentially transforms bronchiolar cells. a Expression of Cx43 in KP (n = 5) and KK (n = 7) tumor pieces, relative to KP. Mann–Whitney test **p = 0.0025. Mean ± SEM. b Expression of Connexin-43 (Cx43) in alveolar macrophages isolated from KP (n = 4) and KK (n = 5) tumor-bearing lungs, relative to Gapdh control. Unpaired student t test ****p < 0.0001. Mean ± SEM. c Quantification of alveolar (EpCAM+CD104−) compartment in uninfected (U; n = 9) and K (n = 4), KP (n = 4) and KK (n = 5) 3 months post Ad5-CMV-Cre administration. Kruskal–Wallis test/Dunn’s multiple comparisons test, U v K **p = 0.0034, U v KP **p = 0.0095. Mean ± SEM. d Quantification of bronchiolar (EpCAM+CD104+) compartment in uninfected (U; n = 9) and K (n = 3), KP (n = 4) and KK (n = 6) 3 months post Ad5-CMV-Cre administration. Kruskal–Wallis test/Dunn’s multiple comparisons test, U v KK **p = 0.0014, U v KP *p = 0.0308. Mean ± SEM. e Representative H&E stained KP and KK lungs 3 weeks post Ad5-CMV-Cre infection. Scale, 200 μm; inset, 50 μm. f Expression of Nqo1 in alveolar (A) and bronchiolar (B) cells (n = 3). ****FDR p < 0.0001. Mean ± SEM. g Expression of Cx43 mRNA in alveolar (A) and bronchiolar (B) cells (n = 3). **FDR p = 0.0055. Mean ± SEM
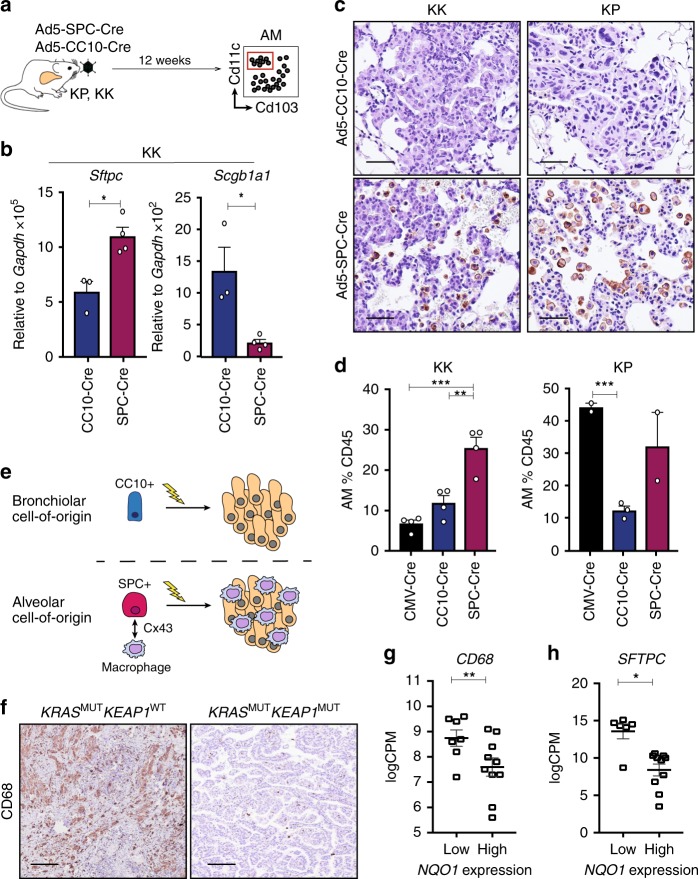
The cell-of-origin dictates the immune microenvironment
To further explore whether the phenotype of the cancer-initiating cells directly influences the immune contexture, cell-type specific Ad5-Cre viruses were used to initiate tumors in KK and KP mice specifically in AT2 (Ad5-SPC-Cre) or bronchiolar Club (Ad5-CC10-Cre) cells in the lung7,9 (Fig. 5a). Consistent with the cell restricted nature of the viruses, Sftpc (pro-SPC) expression was significantly enhanced in tumors initiated from AT2 cells, while elevated expression of Scgb1a1 (CC10) was detected in tumors following Ad5-CC10-Cre infection (Fig. 5b and Supplementary Fig. 7a). Strikingly, F4/80+ infiltrating macrophages were only observed in KP and KK tumors initiated from an AT2 cell-of-origin (Fig. 5c). This restricted expansion of the macrophage compartment was further validated by flow cytometric analysis of alveolar macrophages (Fig. 5d and Supplementary Fig. 7b). Together, these findings suggest that the cell-of-origin, rather than the genetic alteration, is the commanding determinant of alveolar macrophage expansion in KRAS-mutant LUAD (Fig. 5e).
Fig. 5.
Cell-of-origin determines the alveolar macrophage composition in LUAD. a Schematic of cell type-specific Ad5-Cre experimental design. b Expression of Sftpc and Scgb1a1 in KK lung tumor pieces 3 months following administration of Ad5-CC10-Cre (n = 3) or Ad5-SPC-Cre (n = 4). Unpaired t test, Sftpc *p = 0.0168; Scgb1a1 *p = 0.0107. Mean ± SEM. c F4/80 immunostaining on lung tissue from KK and KP mice infected with Ad5-CC10-Cre or Ad5-SPC-Cre. Scale, 50 μm. d Quantification of alveolar macrophages in CD45+ immune lung infiltrate of Ad5-CMV-Cre infected KK (n = 4) and KP (n = 4), Ad5-CC10-Cre infected KK (n = 4) and KP (n = 2) and Ad5-SPC-Cre infected KK (n = 4) and KP (n = 3) mice. KK, ordinary one-way ANOVA/Holm-Sidak’s multiple comparisons test CMV-Cre v SPC-Cre ***p = 0.0002, SPC-Cre v CC10-Cre **p = 0.0016. KP, unpaired t test CMV-Cre v CC10-Cre ***p = 0.0006. Mean ± SEM. e Schematic of cell-of-origin hypothesis and enhanced macrophage number in lung tumors arising from alveolar epithelial cells. Lightning bolt depicts genetic alterations. f Immunostaining of CD68 on KRASMUTKEAP1WT and KRASMUTKEAP1MUT LUAD. Scale, 200 μm. g Analysis of CD68 expression in NQO1low (n = 7) and NQO1high (n = 10) KRAS-mutant LUAD TCGA patient samples. **FDR p = 0.0012. Mean ± SEM. h Analysis of SFTPC expression in NQO1low (n = 7) and NQO1high (n = 10) KRAS-mutant LUAD TCGA patient samples. **FDR p = 0.0108. Mean ± SEM
To determine whether the effect of NRF2 pathway activation on the immune microenvironment is conserved in patient cohorts, we next curated an independent LUAD cohort of FFPE blocks with known KRAS and TP53 mutation status (n = 48), hereafter the St Vincent’s cohort (Supplementary Data 2). Immunostaining of NQO1 and CD68 revealed a negative correlation between macrophage infiltration and NRF2 pathway activity (Supplementary Fig. 7c, d), concordant with the GEMM findings. Furthermore, patient samples of known KEAP1 mutation status were evaluated for CD68 intensity, revealing reduced macrophage infiltration in KRASMUTKEAP1MUT patient samples (Fig. 5f). In the independent TCGA LUAD cohort, CD68 expression was significantly reduced in the KRASMUTNQO1high patient samples (Fig. 5g; FDR p = 0.0012), as was the expression of SFTPC, a specific marker of AT2 cells (Fig. 5h; FDR p = 0.0108). Thus, loss-of-function mutations in KEAP1 alter the immune microenvironment by facilitating malignant transformation from bronchiolar epithelial cells.
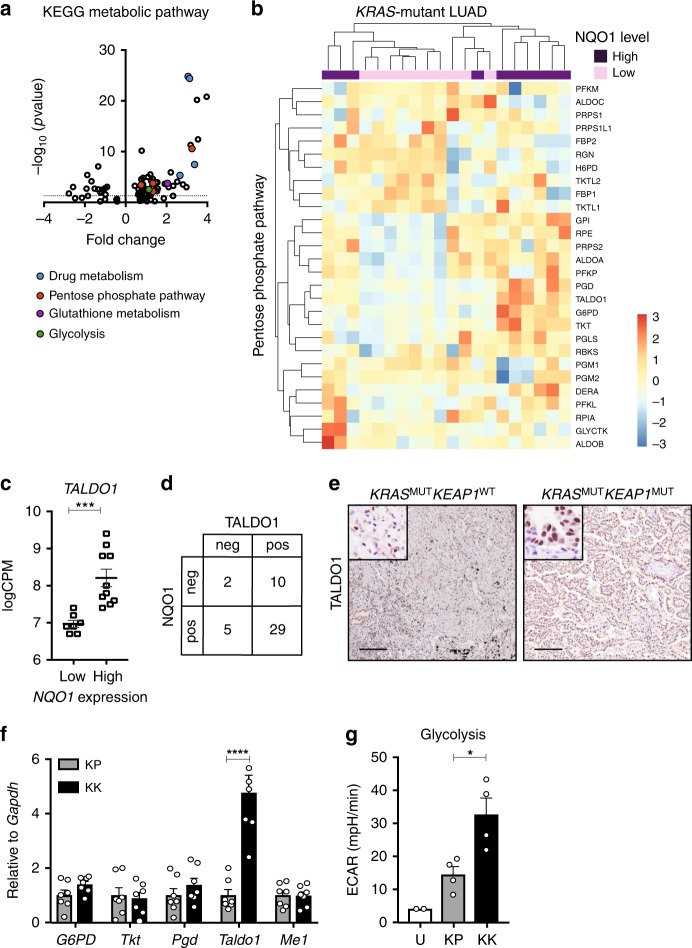
TALDO1 is upregulated in LUAD with high NRF2 activity
Having established the unique nature of the bronchiolar-induced immune microenvironment in KEAP1-mutant KRAS-driven LUAD, we sought to identify the underlying mechanisms of tumor progression in this genetic subtype. We surveyed KEGG pathways differentially expressed in the KRASMUTNQO1high versus KRASMUTNQO1low TCGA cohort, and identified upregulation of pathways including the pentose phosphate pathway (PPP), glutathione metabolism and drug metabolism (Fig. 6a), consistent with increased NRF2 pathway activity15,18,39. Both the PPP as a whole (Fig. 6b) and the specific expression of PPP enzyme TALDO1 (Fig. 6c) significantly correlated with the KRASMUTNQO1high TCGA dataset. In addition, TALDO1 protein expression significantly correlated with NQO1 expression in the independent St Vincent’s cohort (Fig. 6d and Supplementary Data 2). Importantly, KRASMUTKEAP1MUT LUADs were strongly positive for TALDO1 protein expression, while KRASMUTKEAP1WT LUADs were not (Fig. 6e). This correlation was conserved in the GEMMs, whereby Taldo1 mRNA and protein expression were substantially increased in KK tumors, in comparison to levels in KP tumors (Fig. 6f and Supplementary Fig. 8a). Functionally, we tested the glycolytic rate in tumor cells from KK and KP mice using a protocol developed specifically for freshly isolated primary cells (Supplementary Fig. 8b). We found that KK tumor cells exhibited both an increased basal acidification rate and overall glycolytic rate compared to KP tumors (Fig. 6g and Supplementary Fig. 8c, d). Together, these findings highlight that loss of Keap1 rewires cellular metabolism by processes distinct to that of p53 to potentiate KrasG12D-induced tumorigenesis
Fig. 6.
Enhanced glucose metabolism in Keap1-mutant KrasG12D LUAD. a Volcano plot of top KEGG metabolic pathways differentially expressed in NQO1low (n = 10) and NQO1high (n = 10) KRAS-mutant LUAD from the TCGA dataset. Pathways involved in drug metabolism, pentose phosphate pathway, glutathione metabolism, and glycolysis have been highlighted. Dotted line represents p = 0.05. b Heatmap of KEGG pentose phosphate pathway in NQO1low (n = 10) and NQO1high (n = 10) KRAS-mutant LUAD from the TCGA dataset. c Analysis of TALDO1 expression in NQO1low (n = 7) and NQO1high (n = 10) KRAS-mutant LUAD TCGA patient samples. ***FDR p = 0.0006. Mean ± SEM. d Correlation of TALDO1 and NQO1 immunostaining in KRAS-mutant LUAD (n = 46). e TALDO1 immunostaining on KRASMUTKEAP1WT and KRASMUTKEAP1MUT patient samples. Scale, 200 μm; inset, 50 μm. f Expression of glycolytic enzyme (G6PD), pentose phosphate pathway enzymes (Tkt, Pgd, Taldo1) and malic enzyme (Me1) in tumor pieces from KP (n = 7) and KK (n = 7) lungs. Expression relative to Gapdh housekeeper control and quantified relative to KP expression. Two-way ANOVA/Sidak’s multiple comparisons test Taldo1 KP v KK ****p < 0.0001. Mean ± SEM. g Rate of glycolysis measured by extracellular acidification rate (ECAR) of uninfected lung epithelium (U; n = 2 experiments, n = 6 mice per experiment) and KP (n = 4) as well as KK (n = 4) flow cytometry isolated tumor cells 3 months following Ad5-CMV-Cre infection. Ordinary one-way ANOVA/Holm-Sidak’s multiple comparisons test, KP v KK *p = 0.0198. Mean ± SEM
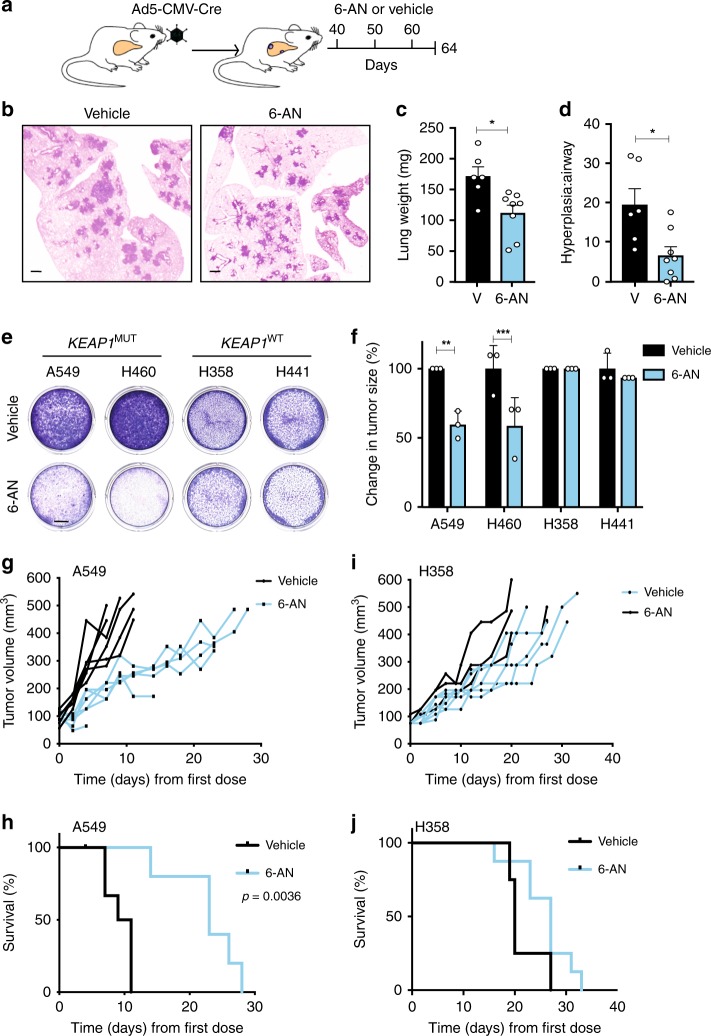
KEAP1-mutant LUAD are sensitive to 6-AN treatment
To dissect whether increased PPP activity results in a metabolic vulnerability in KEAP1-mutant tumors, we used 6-AN, an inhibitor of 6-phosphogluconate dehydrogenase (PGD)40,41, integral to both the oxidative and non-oxidative arms of the PPP (Supplementary Fig. 9a). 6-AN significantly reduced colony forming potential in Keap1-deficient primary cell lines derived from KPK and KK tumors, and had no effect on the growth of KP tumor cells (Supplementary Fig. 9b, c). To investigate the therapeutic potential of targeting PPP in Keap1 mutant tumors in a spontaneous lung tumor setting, 40 days post Ad5-CMV-Cre administration, KK and KP mice were treated with three cycles of 6-AN (Fig. 7a). While extensive adenomas formed in vehicle-treated KK mice, only hyperplasia was observed in 6-AN-treated KK mice (Fig. 7b). Consistent with histological examination, there was a significant reduction in lung weight of 6-AN treated KK mice (Fig. 7c), and an increase in unobstructed airway, quantified as a decreased hyperplasia to airway ratio (Fig. 7d). Conversely, KP mice treated with 6-AN exhibited no reduction in adenomatous lesion formation (Supplementary Fig. 9d) nor change in lung weight (Supplementary Fig. 9e) or hyperplasia parameters (Supplementary Fig. 9f, g), relative to vehicle control. Together, these findings highlight a specific vulnerability of Keap1-mutant tumors to inhibition of PPP activity in vivo.
Fig. 7.
PPP blockade abrogates the growth of KEAP1-mutant LUAD. a Schematic of spontaneous tumor treatment study. Briefly, KK or KP mice were randomized into 20 mg/kg 6-AN or vehicle treated 40 days post Ad5-CMV-Cre intranasal infection. Lungs were harvested for analysis on day 64. b Representative H&E images of KK vehicle or 6-AN-treated lungs. Scale, 1 mm. c Quantification of KK superior lobe lung weight (milligrams, mg) following vehicle (n = 6) or 6-AN (n = 8) treatment. Unpaired t test *p = 0.0106. Mean ± SEM. d Ratio of KK hyperplasia relative to large airway size in vehicle (n = 6) and 6-AN (n = 8) treated lungs. Unpaired t test *p = 0.0116. Mean ± SEM. e Colony assay 72 h following treatment with 62.5 μM 6-AN vs vehicle in KEAP1MUT and KEAP1WT NSCLC cell lines. Scale, 5 mm. f Relative change in tumor size of xenograft models (n = 3/cell line) of KEAP1MUT and KEAP1WT 48 h following treatment with 20 mg/kg 6-AN or vehicle. Change in size relative to vehicle of each cell line. Two-way ANOVA/Sidak’s multiple comparisons test: A549 **p = 0.0012; H460 ***p = 0.001. Mean ± SD. g Tumor measurements of A549 cell line xenograft following treatment with 20 mg/kg 6-AN (n = 6) or vehicle (n = 6) every 10 days. Survival log-rank (Mantel-Cox) test **p = 0.0023. h Kaplan–Meier survival curve of A549 xenograft NSG mice treated with 20 mg/kg 6-AN (n = 6) or vehicle (n = 6) every 10 days. Mantel–Cox test **p = 0.0017. i Tumor measurements of H358 xenograft following treatment with 20 mg/kg 6-AN (n = 8) or vehicle (n = 4) every 10 days. j Kaplan–Meier survival curve of H358 xenograft NSG mice treated with 20 mg/kg 6-AN (n = 8) or vehicle (n = 4) every 10 days
To explore the sensitivity of human NSCLC cell lines to 6-AN, we used KRAS-mutant A549, H460 (TP53WT;STK11MUT;KEAP1MUT), H358 and H441 (TP53MUT;STK11WT;KEAP1WT). KEAP1-mutant cell lines displayed increased NQO1 and TALDO1 expression (Supplementary Fig. 10), more aggressive behavior (Supplementary Fig. 11a) and greater ROS clearance capacity (Supplementary Fig. 11b), indicative of enhanced NRF2 pathway activity. In this setting, the activity of 6-AN was confirmed to impact the glycolytic, and not oxidative, capacity of KEAP1-mutant cell lines (Supplementary Fig. 11c), consistent with inhibition of PGD42. In line with mouse cell line and spontaneous tumor studies, KEAP1-mutant cell lines displayed increased sensitivity to PPP inhibition (IC50 KEAP1MUT 9.9 ± 6.4 μM vs. KEAP1WT 44.5 ± 7.9 μM; Supplementary Fig. 10d). Furthermore, the sensitivity was more rapid in KEAP1-mutant cell lines (Supplementary Fig. 10e) and abrogated cell growth and survival with increased expediency (Fig. 7e and Supplementary Fig. 10f). Moreover, to examine the in vivo response of the human cell lines to 6-AN, a subcutaneous xenograft transplantation of A549 and H358 was performed in immune-deficient mice. Consistent with the spontaneous GEMM treatment study, A549 recipient mice treated with 6-AN displayed reduced tumor growth (Fig. 7f, g) and increased survival (Fig. 7h), while H358 recipient mice received no survival benefit from 6-AN (Fig. 7i, j). Together, these findings suggest a specific dependency of KRASMUTKEAP1MUT tumors to the PPP, that can be abrogated in vivo using pharmacological inhibitors of the pathway.
Discussion
In this study, we directly addressed the heterogeneity of KRAS-mutant LUAD through the generation of a series of GEMMs. We demonstrate that KEAP1 is a potent tumor suppressor that promotes malignancy through a metabolic dependency on the PPP. Together with our previous studies17, our data indicate that bronchiolar epithelium are particularly sensitive to Keap1 inactivation, with tumor initiation from this cellular compartment imposing a profound effect on the immune microenvironment of KRAS-mutant LUAD. We reveal a pro-tumorigenic function for macrophages in KrasG12D lung tumors induced from alveolar cells. Together, these data highlight that KRAS-mutant cancers hijack diverse processes to evolve. Importantly, these differing mechanisms should be considered therapeutically in order to effectively impede tumor progression.
Although KRAS can activate a basal level of NRF2 activity43,44, the enrichment of KEAP1 alterations in KRAS-mutant LUADs suggest that augmented NRF2 pathway activation is favorable in driving malignant progression. Indeed, utilizing Cre-loxP recombination technology, we demonstrate that Keap1 inactivation accelerates KrasG12D-induced tumorigenesis. Interestingly, CRIPSR/Cas9 genomic editing of Keap1 failed to accelerate KrasG12D-induced tumorigenesis in an in vivo boutique screen19,20, while transduction of an independent sgKeap1 lentiviral construct led to accelerated tumorigenesis on the KP background18. These findings suggest that, while CRISPR models may mimic the heterogeneous mutation landscape of patient tumors, in the context of defining tumor suppressors, consistent bi-allelic inactivation using Cre-loxP models provide a definitive genetic tool. Interestingly, conditional activation of Keap1 (Keap1R554Q) was recently shown to delay lung tumorigenesis on the KP background21, highlighting the need to dissect differences between loss-of-function versus mutant proteins in a tissue- and cell-specific context, akin to the controversies surrounding TP5345. In this study, the absence of synergistic activity of Keap1 and p53 loss in the context of oncogenic KrasG12D activation aligns with the mutual exclusivity of these genetic alterations in KRAS-mutant LUAD14. Moreover, these findings suggest that p53 and Keap1 may be acting in similar tumor suppressive pathways, with co-mutated cells exhibiting no selective advantage. One might therefore speculate that targeting intact TP53, using small molecular inhibitors such as Nutlin, might be efficacious in this TP53WT subgroup of tumors.
While KEAP1 and STK11 are co-mutated in a subset of KRAS-mutant LUAD, KL and KLK mice exhibited similar survival rates following Ad5-CMV-Cre administration. Moreover, the tumor plasticity observed in KrasG12D models carrying Lkb1 loss was also retained following combined loss of Keap1. The apparent dominance of SqCC tumors in KLK mice is concordant with the observed increase in Nqo1 expression and accompanying reduction in ROS levels in SqCC tumors detected in KL mice46, suggesting that augmentation of KEAP1-NRF2 pathway modulates tumor cell plasticity. Recent clinical evidence highlights a crucial role of STK11 in dictating the therapeutic response to immune-based therapies47. This highlights the importance of establishing the contribution alteration of KEAP1 plays in this setting, and in establishing a pure LUAD immunocompetent murine model will aid in addressing this clinically-relevant question.
The advent of immunotherapeutic agents, with in an increasing number of mechanisms to unleash immune cells to identify and kill tumor cells, has resurrected the importance of characterizing the immune microenvironment of tumors. In fact, Sox2-driven models of squamous carcinomas are characterized by increased neutrophil recruitment8,33, just as KL adenosquamous tumors displayed increased tumor associated neutrophils, while adenocarcinoma lesions did not48. These findings suggest that the lesion type, and corresponding cell-of-origin, may play a role in the immune cells recruited to lung tumors. While there is strong evidence that KrasG12D-driven tumors arise from an alveolar cell-of-origin, the direct impact the initiating cell has on the well-characterized macrophage inflammation of these tumors is poorly understood13. We identify that restricted activation of KrasG12D concomitant with inactivation of either p53 or Keap1 in SPC-expressing AT2 cells resulted in the formation of lung tumors characterized by macrophage infiltration. Importantly, this data represents a paradigm shift, whereby the immune microenvironment of the tumor is directly influenced by the initiating cell, and not the genetic alterations themselves. Indeed, our analysis revealed that untransformed alveolar cells express high levels of the gap junction protein Cx43, a crucial component of the interaction between alveolar cells and alveolar macrophages. Moreover, macrophages infiltrating KRAS-mutant tumors are pro-tumorigenic, and could represent a therapeutic target in inflamed LUAD. Therapies targeting macrophages have been investigated for solid tumors, with a number of clinical trials on-going investigating the benefits of macrophage depletion (reviewed in Poh et al.49). These findings highlight an immune-based approach to abrogate the growth and progression of KRAS-mutant LUAD.
The observed lack of macrophage infiltration with pro-tumorigeneic characteristics in KEAP1-mutant tumors may suggest that KEAP1-deficient tumors hijack alternative tumor-promoting mechanisms to drive and sustain tumor cell growth. Indeed, there is strong evidence linking NRF2 pathway activation and cellular metabolism50, with recent preclinical data suggesting that inhibition of such dependencies may be a viable therapeutic approach. Here, we demonstrate the metabolic dependency of KEAP1-mutant tumors to the pentose phosphate pathway (PPP). The studies herein describe the dependency of KEAP1-mutant tumors on the induction of TALDO1, a key enzyme in the non-oxidative arm of the PPP. We and others have previously described the presence of biomarkers17 and genetic regulation of enzyme expression39,51 implicating the importance of PPP metabolism in KEAP1-deficient cells. Notably, the use of 6-AN may have two-fold implications on KEAP1-mutant tumors. As a PGD inhibitor, 6-AN constricts the ability of tumor cells to utilize the PPP40 and may have additional on-target effects on glutathione (GSH) synthesis, via glutamine-cysteine ligase (GCLC)52. Production of GSH is an important product of NRF2 activation, essential for redox homeostasis, and therefore may provide an additional anti-tumor mechanism in 6-AN treated cells. Importantly, these findings highlight that metabolic rewiring by the NRF2 pathway is a key effector of tumor progression. Targeting metabolic pathways, either the PPP, serine biosynthesis53,54 or glutaminase18,55, can sufficiently block the metabolic advantage of KEAP1-mutant LUAD. These studies highlight that while robustly inhibiting tumor potential, like most other therapeutics, metabolic inhibitors will need to be applied in combination to exert a profound effect.
In conclusion, we have generated series of mouse models that recapitulate the heterogeneity of KRAS-mutant LUAD. Importantly, the identification of neoplastic abnormalities co-occurring with oncogenic KRAS must be considered in the both research models and in the clinic. Indeed, this is evidenced by the resistance to anti-PD-1 checkpoint inhibitors in KRAS-mutant LUADs harboring STK11 alterations. Based on findings presented herein, it is tempting to speculate that both the genetic alterations and cell-of-origin impact the behavior and treatment response of the tumor. Concordant with this, we demonstrate that KEAP1-deficient tumors exhibit unique characteristics dictated by their cellular origin and metabolic program. Importantly, the findings within highlight the power of targeting metabolic and immune dependencies in KRAS-mutant LUAD, thus providing an exciting alternative solution to targeting the oncoprotein itself.
Methods
Ethics and human samples
We obtained all patient material according to protocols approved by the Human Research Ethics Committee of the Walter and Eliza Hall Institute of Medical Research (WEHI) and St Vincent’s Hospital Human Research Ethics Committee (#10/04 and #030/12, respectively). The KRAS-mutant LUAD dataset and samples were obtained through the Clinical Lung Cancer Genome Project (CLCGP)26 and the Victorian Thoracic Malignancies Prospective Cohort Study. Sections of KRAS-mutant LUAD patient FFPE blocks were obtained from St Vincent’s Hospital (Melbourne, Australia).
Ethics and mice
We conducted all animal experiments according to the regulatory standards approved by the Walter and Eliza Hall Institute Animal Ethics Committee (AEC 2016.024). Keap1flox mice27 were a generous gift from S. Biswal (John Hopkins Bloomberg School of Public Health). KrasG12D/+;p53flox/flox mice, Lkb1flox/flox mice and EYFPT/+ mice were previously described10,29,30 and were obtained from Jackson Laboratory. All animals were maintained on a C57BL/6 background and equal proportions of males and females were used in all experiments (genotyping primers listed in Supplementary Table 2).
Seven-to-eight-week old mice were intranasally (i.n.) infected with 20 μL of 1 × 1010 PFU/mL Ad5-CMV-Cre, Ad5-SPC-Cre or Ad5-CC10-Cre virus (University of Iowa Gene Transfer Core Facility #VVC-U of Iowa-5, VVC-Berns-1168) according to standard procedures56. At 3-weeks, 2-months or 3-months following infection, or at ethical endpoint, lungs were harvested for further analysis. Mice were injected intra-peritoneally (i.p.) 1 h prior to tissue collection with 5-Bromo-2-deoxyuridine (BrdU; 0.5 mg/10 g body weight; Sigma-Aldrich B5002).
Flow cytometry
The superior lobe of the left lung was dissected at the bifurcation of the left primary bronchus and weighed. Single cell suspensions were generated as described in detail previously56. Primary antibodies (Supplementary Table 3) were incubated for 30 min at 4 °C. Population definitions: Alveolar cells (PI−CD45−CD31−EpCAM+CD104−), Bronchiolar cells (PI−CD45−CD31−EpCAM+CD104+), T cells (PI−CD45+SSCloFSCloCD3+); CD4+ T cells (PI−CD45+SSCloFSCloCD3+CD4+); CD8+ T cells (PI−CD45+SSCloFSCloCD3+CD8+); B cells (PI−CD45+SSCloFSCloCD19+); NK cells (PI−CD45+SSCloFSCloCD3−NKp46+DX5+); Monocytes (PI−CD45+CD11b+SSCloLy6G−); Neutrophils (PI−CD45+CD11b+Ly6G+); Eosinophils (PI−CD45+CD11b+SSChiLy6G−); Alveolar Macrophages (PI−CD45+CD11c+CD103−); CD103+ Dendritic Cells (PI−CD45+CD11c+CD103+). Flow cytometry was performed on the LSR II flow cytometer (BD Biosciences) and data were analyzed using FlowJo software (FlowJo LLC). Fluorescence activated cell sorting (FACS) was performed on the ARIA flow cytometer (BD Biosciences).
Cell culture
Single cell suspensions of primary tumor cells were seeded in tumor cell medium (DMEM-F12 + GlutaMAX (Gibco), 10 % FBS (Sigma-Aldrich), 100 U/mL penicillin (Gibco), 100 μg/mL streptomycin (Gibco), 0.04 mg/mL hydrocortisone (Sigma-Aldrich), 1 X Insulin-Transferrin-Selenium-Ethanolamine (Gibco), 5 ng/mL epidermal growth factor (Sigma-Aldrich). Supernatant from the first 6 h of culture was collected for TNF (eBioscience, #5017331) and IL-6 (eBioscience, #501128696) ELISA according to the manufacturer’s instructions. The human lung cancer derived cell lines A549, H460, H441 and H358 were obtained from ATCC and cultured in RPMI-1640 + GlutaMAX medium (Gibco) supplemented with 10 % FBS (Sigma-Aldrich), 100 U/mL penicillin 100 μg/mL streptomycin (Gibco). MTS (CellTiter96 Aqueous Non-Radioactive Cell Proliferation Assay, Promega) absorbance assay was used to measure growth of 2000 cells analyzed after 120 h to determine relative growth of human cell lines.
Reactive oxygen species assay
2,7-dichlorofluorescin diacetate (DCFDA) ROS detection assay (Abcam #Ab113851) was performed according to manufacturer’s protocol in opaque-walled 96-well plates (Greiner Bio-One). Freshly sorted macrophages, or KK and KP primary tumor cell lines were seeded at 60,000 cells/well, treated with 20 μM DCFDA at 37 °C for 30 min, washed, then treated with 110 μM tert-butyl hydrogen peroxide (TBHP) at 37 °C for 2 h. Fluorescence at excitation/emission 484 nm/535 nm was measured using a Hidex Chameleon microplate reader (LabLogic).
Seahorse assay
Single cell suspensions were seeded onto 2 mg/mL type 1 collagen (Corning) coated Seahorse XF96 cell culture microplates (Agilent) at 120,000 cells/well (freshly sorted macrophages or EpCAM+ cells). Samples were centrifuged at 400 g at 4 °C for 15 min without brake, then incubated at 37 °C for 1 h. Extracellular acidification rate (ECAR) or oxygen consumption rate (OCR) were measured by XF96 Extracellular Flux Analyzer (Agilent) using serial injections. ECAR: 5 mM glucose, 1 μM oligomycin and 50 mM 2-deoxy-D-glucose (2-DG). OCR: 1 μM oligomycin, 0.7 μM FCCP (carbonyl cyanide-p-trifluoromethoxyphenylhydrazone) and 1 μM rotenone and antimycin A.
Gap19 treatment study
C57BL/6 mice were subject to intranasal inhalation of 50 μL 2 mg/mL Gap19 peptide (Tocris Bioscience #5353) or PBS vehicle, and collected at 3 and 24 h following infection. Bronchiolar lavage of PBS was passed through the lungs to clear unattached cells, and remaining tissue was prepared for flow cytometry, as above.
Clodronate liposome treatment study
KP mice were subject to intranasal inhalation of Ad5-CMV-Cre at 6–8 weeks of age, and randomized into control PBS-liposomes (FormuMax #F70101-NH) or clodronate-liposomes (FormuMax F70101C-NH) four weeks post Ad5-CMV-Cre. Liposomes were administered as 50 μL intranasal injections of 7 mg/mL twice per week for the first week, and weekly thereafter for 7 subsequent weeks. At 12 weeks post Ad5-CMV-Cre, mice were harvested, bronchiolar lavage collected, and lungs processed for histology and flow cytometry, as above.
6-AN treatment study
For in vitro single dose studies, A549, H460, H358 and H441 cell lines were treated with 62.5 μM 6-AN (Cayman Chemicals #10009315) for 72 h, and cell survival was then measured using the MTS assay (CellTiter96 Aqueous Non-Radioactive Cell Proliferation Assay, Promega) relative to DMSO vehicle treated cells. Crystal violet colony-forming assay was performed as previously described57. For in vivo studies, 6-AN was administered intra-peritoneally at 20 mg/kg body weight once every ten days. Tumor xenografts were generated by subcutaneous transplant of 500,000 cells in 50 % growth factor reduced Matrigel (BD Biosciences) into NSG immune-deficient mice, with treatment commencing once tumors reached a volume of 70–100 mm3.
Histology and immunohistochemistry
Lungs were perfused and fixed in 4% paraformaldehyde for 24 h at 4 °C and embedded in paraffin. Sections 2 μm thick were stained with haematoxylin and eosin (H&E) and sections 4 μm thick were immunostained according to standard procedures. Primary antibodies (Supplementary Table 3) were applied overnight at 4 °C in a humidifier box. Slides were imaged using Nikon Eclipse 50i microscope with Axiovision software (Zeiss). Hyperplasia and airway area were quantified using the measure tool on Image J software (Softonic).
Quantitative RT-PCR
cDNA was generated from ground lung, tumor tissue or snap-frozen cell pellets using the RNeasy RNA extraction kit (Qiagen), followed by the SuperScript III kit (Thermo Fisher). Quantitative RT-PCR was performed using SyberGreen (Bioline QT605-05) on the Viia7 Real-Time PCR System (Thermo Scientific). Relative mRNA was calculated compared to Gapdh internal control using the delta-delta-cT statistical method (primers in Supplementary Table 2).
Western blotting
Cell pellets were lysed in RIPA buffer (2% Triton X-100, 0.2% sodium dodecyl sulfate, 0.02% sodium deoxycholate, 0.3 M NaCl, 20 mM Tris hydrochloride, 0.02% sodium azide, complete mini EDTA-free protease inhibitor cocktail (Roche)), and western blotting performed by standard procedures. Primary antibodies (Supplementary Table 3) were incubated overnight at 4 °C and blots exposed using ECL Prime reagent (GE Healthcare) and imaged using Chemidoc Touch (Bio-Rad).
Analysis for TCGA LUAD KRAS-mutated samples
Gene-wise RNA-seq read counts for lung adenocarcinomas from The Cancer Genome Atlas (TCGA) project4 were retrieved using the RTCGAToolbox package58. One hundred and sixty-two samples from the 20,160,128 release were further stratified by their KRAS mutation status14 leaving 35 samples which were stratified into three groups of similar size based on either their NRF2 signature score (this gene signature was defined by taking the intersection of NRF2 gene lists from Romero et al. (Supplementary Table 3)18, DeNicola et al. (Supplementary Fig. 8)53, and Goldstein et al. (Supplementary Table S2)59, calculating the mean log2 counts per million (log-CPM) for these genes per sample and splitting the samples into low (n = 12), medium (n = 11) and high (n = 12) expression groups) or their NQO1 expression levels (low (n = 12), medium (n = 11) and high (n = 12) expression). Differential expression was assessed for the high vs low groups using limma-voom60,61 with robust fitting option after trimmed mean of M-values (TMM) normalization62 using edgeR63. Adjustment for multiple testing was performed using the FDR method64. Enrichment of KEGG metabolism pathways was tested for the high vs low comparison using EGSEA65 with 10 methods (camera, safe, gage, padog, plage, zscore, gsva, ssgsea, globaltest, and ora) and the median rank to prioritize results. The pheatmap (https://CRAN.R-project.org/package = pheatmap) R package was used to generate heatmaps of expression quantified as log counts per million (log-CPM) values for genes from selected pathways. Software package details can be found in Supplementary Table 4.
Analysis of mouse RNA-seq data
RNA-seq read count data were obtain from GEO series GSE8399138. Filtering genes with low counts (a count per million greater than one in at least three samples was required) was followed by normalization using the TMM method in the edgeR package63. Differential expression analyses used limma-voom60,61 together with TREAT66 to test relative to a fold-change cut-off of 1 and multiple testing correction using the FDR method64. The NRF2 gene signature defined above was converted from human to mouse using biomaRt67 and a limma barcode enrichment plot was generated using moderated t-statistics68. Gene set testing of MSigDB’s69 c5 (Gene Ontology) collection was performed using EGSEA65 using the 11 methods (camera, safe, gage, padog, plage, zscore, gsva, ssgsea, globaltest, fry, and ora) and the median rank to prioritize results. Differential expression testing of custom gene signatures was performed using ROAST70.
Statistics
Statistical analysis was performed using Prism software (GraphPad Software). Aggressive score was determined as an average of the numerical score attributed to stage. Pairwise comparisons were performed using an unpaired Student t test and multivariate comparisons were performed using one-way ANOVA (Kruskal–Wallis test) with Tukey’s multiple comparisons test or two-way ANOVA with Dunn’s multiple comparisons test for grouped analyses.
Reporting summary
Further information on research design is available in the Nature Research Reporting Summary linked to this article.
Supplementary information
Description of Additional Supplementary Files
Acknowledgements
We are grateful to S. Oliver, C. Alvarado, L. Scott, S. O’Connor for animal husbandry, S. Monard in the WEHI Flow Cytometry Facility and E. Tsui in the WEHI Histology Facility for expert support. We acknowledge P. Maltezos in the WEHI Graphics Department for the design and preparation of figure illustrations. We thank R.K. Thomas (Department of Translational. Genomics, University of Cologne) for sequencing data for the Melbourne cohort of the CLCGP. We are thankful to A. Berns, A. Strasser and J. Vissers for critical reading of the manuscript and J. Visvader for useful discussions. This work was supported by an Australian National Health and Medical Research Council (NHMRC) Project Grant to K.D.S. and M.E.R. (1138275), S.A.B (1159002), and Career Development Fellowship to M.E.R. (1104924). K.D.S. is supported by a Victorian Cancer Agency Mid-Career Research Fellowship (18003) and the Peter and Julie Alston Centenary Fellowship; S.D. was supported by an Alan W. Harris Scholarship. This work was made possible through Victorian Government Operational Infrastructure Support and Australian Government.
Author contributions
The experiments were conceived and designed by S.A.B. and K.D.S. Experiments were performed mainly by S.A.B. with the assistance of A.K., S.D., K.L., B.R., and J.V. Bioinformatic analysis was performed by Y.X. and X.D. under the supervision of M.E.R. Histological examination was performed by V.R. and J.-Y.S. and patient clinical and genomic data was curated by V.R. and G.M.W. The manuscript was written by S.A.B. and K.D.S.
Data availability
All data that support the findings of this study is available in the Article, Supplementary Information or available upon reasonable request from the corresponding author. Previously published datasets used in this study are available at Gene Expression Omnibus GSE83991 and through dbGAP with accession #PHS000178.v10.p8 (https://portal.gdc.cancer.gov/projects/TCGA-LUAD).
Competing interests
The authors declare no competing interests.
Footnotes
Peer review information Nature Communications thanks David Barbie and other anonymous reviewer(s) for their contribution to the peer review of this work. Peer reviewer reports are available.
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Supplementary Information accompanies this paper at 10.1038/s41467-019-12164-y.
References
- 1.Prior IA, Lewis PD, Mattos C. A comprehensive survey of Ras mutations in cancer. Cancer Res. 2012;72:2457–2467. doi: 10.1158/0008-5472.CAN-11-2612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Quinlan MP, Settleman J. Isoform-specific ras functions in development and cancer. Future Oncol. 2009;5:105–116. doi: 10.2217/14796694.5.1.105. [DOI] [PubMed] [Google Scholar]
- 3.Papke B, Der CJ. Drugging RAS: know the enemy. Science. 2017;355:1158–1163. doi: 10.1126/science.aam7622. [DOI] [PubMed] [Google Scholar]
- 4.Cancer Genome Atlas Research, N. Comprehensive molecular profiling of lung adenocarcinoma. Nature. 2014;511:543–550. doi: 10.1038/nature13385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Jackson EL, et al. Analysis of lung tumor initiation and progression using conditional expression of oncogenic K-ras. Genes Dev. 2001;15:3243–3248. doi: 10.1101/gad.943001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mainardi S, et al. Identification of cancer initiating cells in K-Ras driven lung adenocarcinoma. Proc. Natl Acad. Sci. USA. 2014;111:255–260. doi: 10.1073/pnas.1320383110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Sutherland KD, et al. Multiple cells-of-origin of mutant K-Ras-induced mouse lung adenocarcinoma. Proc. Natl Acad. Sci. USA. 2014;111:4952–4957. doi: 10.1073/pnas.1319963111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ferone G, et al. SOX2 is the determining oncogenic switch in promoting lung squamous cell carcinoma from different cells of origin. Cancer Cell. 2016;30:519–532. doi: 10.1016/j.ccell.2016.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Sutherland KD, et al. Cell of origin of small cell lung cancer: inactivation of Trp53 and Rb1 in distinct cell types of adult mouse lung. Cancer Cell. 2011;19:754–764. doi: 10.1016/j.ccr.2011.04.019. [DOI] [PubMed] [Google Scholar]
- 10.Jackson EL, et al. The differential effects of mutant p53 alleles on advanced murine lung cancer. Cancer Res. 2005;65:10280–10288. doi: 10.1158/0008-5472.CAN-05-2193. [DOI] [PubMed] [Google Scholar]
- 11.Ji H, et al. LKB1 modulates lung cancer differentiation and metastasis. Nature. 2007;448:807–810. doi: 10.1038/nature06030. [DOI] [PubMed] [Google Scholar]
- 12.Busch SE, et al. Lung cancer subtypes generate unique immune responses. J. Immunol. 2016;197:4493–4503. doi: 10.4049/jimmunol.1600576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ji H, et al. K-ras activation generates an inflammatory response in lung tumors. Oncogene. 2006;25:2105. doi: 10.1038/sj.onc.1209237. [DOI] [PubMed] [Google Scholar]
- 14.Skoulidis F, et al. Co-occurring genomic alterations define major subsets of KRAS-mutant lung adenocarcinoma with distinct biology, immune profiles, and therapeutic vulnerabilities. Cancer Discov. 2015;5:860–877. doi: 10.1158/2159-8290.CD-14-1236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Best SA, Sutherland KD. “Keaping” a lid on lung cancer: the Keap1-Nrf2 pathway. Cell Cycle. 2018;17:1696–1707. doi: 10.1080/15384101.2018.1496756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hayes JD, Dinkova-Kostova AT. The Nrf2 regulatory network provides an interface between redox and intermediary metabolism. Trends Biochem. Sci. 2014;39:199–218. doi: 10.1016/j.tibs.2014.02.002. [DOI] [PubMed] [Google Scholar]
- 17.Best SA, et al. Synergy between the KEAP1/NRF2 and PI3K pathways drives non-small-cell lung cancer with an altered immune microenvironment. Cell Metab. 2018;27:935–943. doi: 10.1016/j.cmet.2018.02.006. [DOI] [PubMed] [Google Scholar]
- 18.Romero R, et al. Keap1 loss promotes Kras-driven lung cancer and results in dependence on glutaminolysis. Nat. Med. 2017;23:1362–1368. doi: 10.1038/nm.4407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Rogers ZN, et al. A quantitative and multiplexed approach to uncover the fitness landscape of tumor suppression in vivo. Nat. Methods. 2017;14:737. doi: 10.1038/nmeth.4297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Rogers Zoë N., McFarland Christopher D., Winters Ian P., Seoane Jose A., Brady Jennifer J., Yoon Stephanie, Curtis Christina, Petrov Dmitri A., Winslow Monte M. Mapping the in vivo fitness landscape of lung adenocarcinoma tumor suppression in mice. Nature Genetics. 2018;50(4):483–486. doi: 10.1038/s41588-018-0083-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kang, Y. P. et al. Cysteine dioxygenase 1 is a metabolic liability for non-small cell lung cancer. Elife, 8, e45572 (2019). [DOI] [PMC free article] [PubMed]
- 22.Imielinski Marcin, Berger Alice H., Hammerman Peter S., Hernandez Bryan, Pugh Trevor J., Hodis Eran, Cho Jeonghee, Suh James, Capelletti Marzia, Sivachenko Andrey, Sougnez Carrie, Auclair Daniel, Lawrence Michael S., Stojanov Petar, Cibulskis Kristian, Choi Kyusam, de Waal Luc, Sharifnia Tanaz, Brooks Angela, Greulich Heidi, Banerji Shantanu, Zander Thomas, Seidel Danila, Leenders Frauke, Ansén Sascha, Ludwig Corinna, Engel-Riedel Walburga, Stoelben Erich, Wolf Jürgen, Goparju Chandra, Thompson Kristin, Winckler Wendy, Kwiatkowski David, Johnson Bruce E., Jänne Pasi A., Miller Vincent A., Pao William, Travis William D., Pass Harvey I., Gabriel Stacey B., Lander Eric S., Thomas Roman K., Garraway Levi A., Getz Gad, Meyerson Matthew. Mapping the Hallmarks of Lung Adenocarcinoma with Massively Parallel Sequencing. Cell. 2012;150(6):1107–1120. doi: 10.1016/j.cell.2012.08.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Jordan EJ, et al. Prospective comprehensive molecular characterization of lung adenocarcinomas for efficient patient matching to approved and emerging therapies. Cancer Discov. 2017;7:596–609. doi: 10.1158/2159-8290.CD-16-1337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Cerami E, et al. The cBio cancer genomics portal: an open platform for exploring multidimensional cancer genomics data. Cancer Discov. 2012;2:401–404. doi: 10.1158/2159-8290.CD-12-0095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Gao J, et al. Integrative analysis of complex cancer genomics and clinical profiles using the cBioPortal. Sci. Signal. 2013;6:pl1. doi: 10.1126/scisignal.2004088. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Clinical Lung Cancer Genome Project & Network Genomic Medicine. A genomics-based classification of human lung tumors. Sci. Transl. Med. 5, 209ra153 (2013).. [DOI] [PMC free article] [PubMed]
- 27.Blake DJ, et al. Deletion of Keap1 in the lung attenuates acute cigarette smoke-induced oxidative stress and inflammation. Am. J. Respir. Cell Mol. Biol. 2010;42:524–536. doi: 10.1165/rcmb.2009-0054OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Solis L. M., Behrens C., Dong W., Suraokar M., Ozburn N. C., Moran C. A., Corvalan A. H., Biswal S., Swisher S. G., Bekele B. N., Minna J. D., Stewart D. J., Wistuba I. I. Nrf2 and Keap1 Abnormalities in Non-Small Cell Lung Carcinoma and Association with Clinicopathologic Features. Clinical Cancer Research. 2010;16(14):3743–3753. doi: 10.1158/1078-0432.CCR-09-3352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Srinivas, S. et al. Cre reporter strains produced by targeted insertion of EYFP and ECFP into the ROSA26 locus. BMC Develop. Biol.1, 4 (2001). [DOI] [PMC free article] [PubMed]
- 30.Bardeesy N, et al. Loss of the Lkb1 tumour suppressor provokes intestinal polyposis but resistance to transformation. Nature. 2002;419:162–167. doi: 10.1038/nature01045. [DOI] [PubMed] [Google Scholar]
- 31.Kitajima S, et al. Suppression of STING associated with LKB1 loss in KRAS-driven lung cancer. Cancer Discov. 2019;9:34–45. doi: 10.1158/2159-8290.CD-18-0689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Koyama S, et al. STK11/LKB1 deficiency promotes neutrophil recruitment and proinflammatory cytokine production to suppress T-cell activity in the lung tumor microenvironment. Cancer Res. 2016;76:999–1008. doi: 10.1158/0008-5472.CAN-15-1439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Mollaoglu G, et al. The lineage-defining transcription factors SOX2 and NKX2-1 determine lung cancer cell fate and shape the tumor immune microenvironment. Immunity. 2018;49:764–779. doi: 10.1016/j.immuni.2018.09.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Snelgrove RJ, et al. A critical function for CD200 in lung immune homeostasis and the severity of influenza infection. Nat. Immunol. 2008;9:1074. doi: 10.1038/ni.1637. [DOI] [PubMed] [Google Scholar]
- 35.Jiang‐Shieh YF, et al. Distribution and expression of CD200 in the rat respiratory system under normal and endotoxin‐induced pathological conditions. J. Anat. 2010;216:407–416. doi: 10.1111/j.1469-7580.2009.01190.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Westphalen K, et al. Sessile alveolar macrophages communicate with alveolar epithelium to modulate immunity. Nature. 2014;506:503. doi: 10.1038/nature12902. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Desai TJ, Brownfield DG, Krasnow MA. Alveolar progenitor and stem cells in lung development, renewal and cancer. Nature. 2014;507:190–194. doi: 10.1038/nature12930. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Weeden CE, et al. Lung basal stem cells rapidly repair DNA damage using the error-prone nonhomologous end-joining pathway. PLoS Biol. 2017;15:e2000731. doi: 10.1371/journal.pbio.2000731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Mitsuishi Y, et al. Nrf2 redirects glucose and glutamine into anabolic pathways in metabolic reprogramming. Cancer Cell. 2012;22:66–79. doi: 10.1016/j.ccr.2012.05.016. [DOI] [PubMed] [Google Scholar]
- 40.Koutcher JA, et al. Effect of 6‐aminonicotinamide on the pentose phosphate pathway: 31P NMR and tumor growth delay studies. Magn. Reson. Med. 1996;36:887–892. doi: 10.1002/mrm.1910360611. [DOI] [PubMed] [Google Scholar]
- 41.Gupte S, Li K-X, Okada T, Sato K, Oka M. Inhibitors of pentose phosphate pathway cause vasodilation: involvement of voltage-gated potassium channels. J. Pharmacol. Exp. Ther. 2002;301:299–305. doi: 10.1124/jpet.301.1.299. [DOI] [PubMed] [Google Scholar]
- 42.Street JC, Mahmood U, Ballon D, Alfieri AA, Koutcher JA. C and P NMR investigation of effect of 6-aminonicotinamide on metabolism of RIF-1 tumor cells in vitro. J. Biol. Chem. 1996;271:4113–4119. doi: 10.1074/jbc.271.8.4113. [DOI] [PubMed] [Google Scholar]
- 43.DeNicola GM, et al. Oncogene-induced Nrf2 transcription promotes ROS detoxification and tumorigenesis. Nature. 2011;475:106–109. doi: 10.1038/nature10189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Gwinn DM, et al. Oncogenic KRAS regulates amino acid homeostasis and asparagine biosynthesis via ATF4 and alters sensitivity to L-Asparaginase. Cancer Cell. 2018;33:91–107. doi: 10.1016/j.ccell.2017.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Sabapathy K, Lane DP. Therapeutic targeting of p53: all mutants are equal, but some mutants are more equal than others. Nat. Rev. Clin. Oncol. 2018;15:13–30. doi: 10.1038/nrclinonc.2017.151. [DOI] [PubMed] [Google Scholar]
- 46.Li F, et al. LKB1 inactivation elicits a redox imbalance to modulate non-small cell lung cancer plasticity and therapeutic response. Cancer Cell. 2015;27:698–711. doi: 10.1016/j.ccell.2015.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Skoulidis F, et al. STK11/LKB1mutations and PD-1 inhibitor resistance in KRAS-mutant lung adenocarcinoma. Cancer Discov. 2018;8:822–835. doi: 10.1158/2159-8290.CD-18-0099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Nagaraj AS, et al. Cell of origin links histotype spectrum to immune microenvironment diversity in non-small-cell lung cancer driven by mutant Kras and loss of Lkb1. Cell Rep. 2017;18:673–684. doi: 10.1016/j.celrep.2016.12.059. [DOI] [PubMed] [Google Scholar]
- 49.Poh AR, Ernst M. Targeting macrophages in cancer: from bench to bedside. Front Oncol. 2018;8:49. doi: 10.3389/fonc.2018.00049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.DeNicola GM, Cantley LC. Cancer’s fuel choice: new flavors for a picky eater. Mol. Cell. 2015;60:514–523. doi: 10.1016/j.molcel.2015.10.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Singh A, et al. Transcription factor NRF2 regulates miR-1 and miR-206 to drive tumorigenesis. J. Clin. Invest. 2013;123:2921–2934. doi: 10.1172/JCI66353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Li H, et al. 6-Phosphogluconate dehydrogenase links cytosolic carbohydrate metabolism to protein secretion via modulation of glutathione levels. Cell Chem. Biol. 2019;26:1–9. doi: 10.1016/j.chembiol.2018.12.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.DeNicola GM, et al. NRF2 regulates serine biosynthesis in non-small cell lung cancer. Nat. Genet. 2015;47:1475–1481. doi: 10.1038/ng.3421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Mullarky E, et al. Identification of a small molecule inhibitor of 3-phosphoglycerate dehydrogenase to target serine biosynthesis in cancers. Proc. Natl Acad. Sci. USA. 2016;113:1778–1783. doi: 10.1073/pnas.1521548113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Sayin VI, et al. Activation of the NRF2 antioxidant program generates an imbalance in central carbon metabolism in cancer. Elife. 2017;6:e28083. doi: 10.7554/eLife.28083. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Best SA, Kersbergen A, Asselin-Labat ML, Sutherland KD. Combining cell type-restricted adenoviral targeting with immunostaining and flow cytometry to identify cells-of-origin of lung cancer. Methods Mol. Biol. 2018;1725:15–29. doi: 10.1007/978-1-4939-7568-6_2. [DOI] [PubMed] [Google Scholar]
- 57.Best SA, Nwaobasi A, Schmults C, Ramsey M. CCAR2 is required for proliferation and tumor maintenance in human squamous cell carcinoma. J. Invest. Dermatol. 2017;137:506–512. doi: 10.1016/j.jid.2016.09.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Samur MK. RTCGAToolbox: a new tool for exporting TCGA firehose data. PLoS ONE. 2014;9:e106397. doi: 10.1371/journal.pone.0106397. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Goldstein LD, et al. Recurrent loss of NFE2L2 exon 2 is a mechanism for Nrf2 ncers. Cell Rep. 2016;16:2605–2617. doi: 10.1016/j.celrep.2016.08.010. [DOI] [PubMed] [Google Scholar]
- 60.Ritchie ME, et al. limma powers differential expression analyses for RNA-sequencing and microarray studies. Nucleic Acids Res. 2015;43:e47. doi: 10.1093/nar/gkv007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Law, C. W., Chen, Y., Shi, W. & Smyth, G. K. voom: precision weights unlock linear model analysis tools for RNA-seq read counts. Genome Biol.15, R29 (2014). [DOI] [PMC free article] [PubMed]
- 62.Robinson, M. & Oshlack, A. A scaling normalization method for differential expression analysis of RNA-se1 data. Genome Biol.11, R25 (2010). [DOI] [PMC free article] [PubMed]
- 63.Robinson MD, McCarthy DJ, Smyth GK. edgeR: a Bioconductor package for differential expression analysis of digital gene expression data. Bioinformatics. 2010;26:139–140. doi: 10.1093/bioinformatics/btp616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Benjamini Y, Hockberg Y. Controlling the false discovery rate: a practical and powerful approach to multiple testing. J. R. Stat. Soc. 1995;57:289–300. [Google Scholar]
- 65.Alhamdoosh, M. et al. Combining multiple tools outperforms individual methods in gene set enrichment analyses. Bioinformatics33, 414–424 (2016). [DOI] [PMC free article] [PubMed]
- 66.McCarthy DJ, Smyth GK. Testing significance relative to a fold-change threshold is a TREAT. Bioinformatics. 2009;25:765–771. doi: 10.1093/bioinformatics/btp053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Durinck S, et al. Mapping identifiers for the integration of genomic datasets with the R/Bioconductor package biomaRt. Nat. Protoc. 2009;4:1184–1191. doi: 10.1038/nprot.2009.97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Smyth GK. Linear models and empirical bayes methods for assessing differential expression in microarray experiments. Stat. Appl. Genet. Mol. Biol. 2004;3:1–25. doi: 10.2202/1544-6115.1027. [DOI] [PubMed] [Google Scholar]
- 69.Subramanian A, et al. Gene set enrichment analysis: A knowledge-based approach for interpreting genome-wide expression profiles. Proc. Natl Acad. Sci. USA. 2005;102:15545–15550. doi: 10.1073/pnas.0506580102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Wu D, et al. ROAST: rotation gene set tests for complex microarray experiments. Bioinformatics. 2010;26:2176–2182. doi: 10.1093/bioinformatics/btq401. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Description of Additional Supplementary Files
Data Availability Statement
All data that support the findings of this study is available in the Article, Supplementary Information or available upon reasonable request from the corresponding author. Previously published datasets used in this study are available at Gene Expression Omnibus GSE83991 and through dbGAP with accession #PHS000178.v10.p8 (https://portal.gdc.cancer.gov/projects/TCGA-LUAD).