Abstract
Objective
Posterior interbody fusion is commonly performed for degenerative lumbar conditions. A minimally invasive technique of midline exposure limited only to the facets and fixation with laterally directed cortical bone trajectory (CBT) screws was introduced with the intent of decreasing surgical morbidity. The purpose of this study was to determine if posterior interbody fusion with this limited midline exposure will have less blood loss and shorter operative times (i.e., can be considered minimally invasive) compared to traditional open transforaminal interbody fusion.
Methods
A consecutive single-surgeon series of patients who underwent posterior interbody fusion with either a navigated, midline only exposure (MidLIF) or full, traditional open, exposure of the transverse processes with a posterolateral fusion (open TLIF) were identified. Demographic, peri-operative data, patient reported outcomes (PROs), and reoperation/readmission rates were collected and compared.
Results
There were 29 cases in the MidLIF and 27 in the open TLIF group. Both groups were similar with respect to surgical indications, age, BMI, gender, ASA grade and operative level. The MidLIF group had significantly lower estimated blood loss (266 vs. 446 cc, p = 0.003), shorter operative time (170 vs. 210 minutes, p = 0.003), and shorter length of hospital stay (2.9 vs. 3.7 days, p = 0.016) compared to the open TLIF group. A sub-analysis of single-level cases showed similar findings with significantly lower estimated blood loss (247 vs. 411 cc, p = 0.10), shorter operative time (159 vs. 199 min, p = 0.003), and shorter length of hospital stay (2.9 vs. 3.7 days, p = 0.023) in the MidLIF group. Patient reported outcomes at 6 weeks, 3 months, 6 months, 12 months and 24 months post-operative favored MidLIF with significantly greater ODI improvements at both 6 weeks and 12 months; and lower ODI and back pain at both 12 months and 24 months.
Conclusions
MidLIF had lower blood loss and shorter operative time compared to the traditional open TLIF technique. These differences compare well to reported values in the literature for tubular minimally-invasive TLIF. Patient reported outcomes from 6 weeks to 24 months post-operative, hospital length of stay, and reoperation/readmission rates all favored MidLIF compared to traditional open TLIF.
Keywords: Medicine, Surgery, Neurology, Transforaminal interbody fusion, Lumbar degenerative disease, Midline interbody fusion
1. Introduction
The concept of “minimally invasive surgery” (MIS) continues to attract the attention of patients and surgeons. The potential to obtain the full benefits of surgical treatment with less morbidity is a universal goal. While long-term patient reported outcomes and reoperation rates may be the ultimate measure of success, perioperative metrics such as length of surgery and blood loss can further our understanding of “invasiveness.” Additionally, shorter operative times and less blood loss can translate into cost-savings, which are of utmost importance in the current social-medical climate (see Figs. 1 and 2).
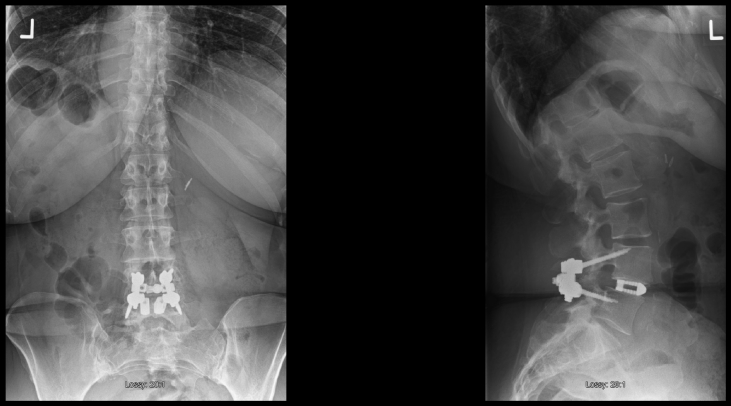
Fig. 1.
65yo with a mobile Degenerative Spondylolisthesis with Lumbar Spinal Stenosis and Neurogenic Claudication. Pre-op ODI = 38, Back pain = 7, andLeg pain = 5.
Fig. 2.
Post-operative MidLIF with ODI = 9, Back pain = 0, and Leg pain = 0. Notice the medial to lateral Cortical Bone Screw (CBT) trajectory and the avoidance of the supra-adjacent facet.
Previous studies on tubular MIS transforaminal interbody fusion (TLIF) have used estimated blood loss (EBL) as a marker of invasiveness [1]. Surgical blood loss has been associated with increased surgical risks including infection and other complications [2]. Costs associated with surgical blood loss include cell saver costs and allogenic transfusion [3, 4]. Recent meta-analyses have shown that tubular MIS TLIF is associated with lower blood loss compared to open TLIF [5, 6, 7, 8, 9].
Operative time is associated with direct costs including personnel and operating room costs. The charge for 1 h of operating room time (excluding physician time) has been reported to be $3720 or more [10, 11]. Recent meta-analyses have shown that operative time for tubular MIS TLIF is not significantly different from open TLIF [5, 7, 8, 9], with one meta-analysis showing increased operative time for MIS TLIF [6].
The purpose of the current study is to quantify the “invasiveness” of a newer technique for posterior decompression and interbody fusion with limited midline exposure. The technique relies on the cortical bone trajectory for pedicle fixation, which does not require exposure lateral to the facet and avoids the additional dissection required to expose the transverse processes. The decompression and interbody fusion can be performed via the familiar midline exposure which greatly diminishes the learning curve. The study authors believe that this technique has been a substantial advancement in their clinical practice with significant improvements in EBL, operative time, length of stay, and patient reported outcomes (PROs) compared to their previous experience with traditional open TLIF. We hypothesized that a single-surgeon consecutive series would show these significant improvements and compare well with literature controls for tubular MIS TLIF.
2. Methods
A consecutive single-surgeon series of patients who underwent posterior interbody fusion from December 2014 to December 2016, during the transition from full, traditional open exposure of the transverse processes with freehand pedicle screws (open TLIF) to a navigated, limited midline exposure (MidLIF) with cortical bone trajectory screws, were identified. Demographic, peri-operative, and patient reported outcome data were collected and compared.
2.1. MidLIF surgical technique
A standard midline incision and subperiosteal dissection is made out to the lateral portion of the facet joint. A self-retaining retractor is placed and maintained until time of closure. A navigation frame is mounted to a spinous process clamp on the cranial end of the incision. Using intra-operative computed tomography based navigation instruments, screw paths are prepared using a cortical bone trajectory (inferior to superior, medial to lateral) through the pedicle. Care is taken to avoid impingement on the supra-adjacent facet. Decompression of the spinal stenosis and interbody fusion is then preformed using standard techniques. Remaining facets joints are decorticated and bone graft is placed. The self-retaining retractor is removed and the wound closed in standard fashion, typically without drains.
2.2. Traditional open TLIF surgical technique
A standard midline incision and subperiosteal dissection is made out to the tips of the transverse processes which elevates and detaches the longissimus and multifidus from the posterolateral gutter. Retractors typically are placed, but must be moved and adjusted to allow for the lateral to medial trajectory of traditional pedicle screws using a standard, “free-hand” technique. The decompression and interbody fusion then proceeds in standard fashion. Prior to closure, decortication and bone grafting of remaining facets and the transverse processes (lateral gutters) is performed.
This study was reviewed and approved by the University of Louisville Institutional Review Board.
3. Results
The two groups had similar demographics (Table 1) and number of surgical levels (Table 2). All surgeries were primary (non-revision) fusions of the index level. Surgical indications were similar between groups and included mobile spondylolisthesis and foraminal stenosis which required facet resection and/or elevation of foraminal height for adequate decompression.
Table 1.
Summary of demographic parameters.
| MidLIF | Open TLIF | p-value | |
|---|---|---|---|
| N | 29 | 27 | |
| Males, N | 7 | 9 | 0.647 |
| Age, years, mean (SD) | 61.66 (7.81) | 58.26 (9.94) | 0.164 |
| BMI, kg/m [2], mean (SD) | 34.79 (5.94) | 34.66 (7.67) | 0.943 |
| ASA Grade, N | |||
| 2 | 3 | 5 | 0.375 |
| 3 | 26 | 21 | |
| 4 | 0 | 1 |
Table 2.
Summary of surgical parameters.
| MidLIF | Open TLIF | p-value | |
|---|---|---|---|
| N | 29 | 27 | |
| Estimated Blood Loss, cc, mean (SD) | 266.38 (129.09) | 446.11 (261.88) | 0.003 |
| Cell Saver | |||
| Patients infused | 9 | 16 | 0.060 |
| Volume infused | 42.41 (64.40) | 133.15 (152.67) | 0.007 |
| Operative Time, min, mean (SD) | 170.10 (36.51) | 209.92 (53.65) | 0.003 |
| No of Surgical Levels, N | 0.978 | ||
| 1 | 23 | 22 | |
| 2 | 5 | 5 | |
| No of Interbody Fusions, N | 0.760 | ||
| 1 | 26 | 25 | |
| 2 | 3 | 2 | |
| Length of Hospital Stay | 2.90 (1.24) | 3.70 (1.20) | 0.016 |
Estimated blood loss was significantly less in the MidLIF group (266 vs. 446 mL, p = 0.003). Consistent with lower EBL in the MidLIF group, cell saver volume infused was significantly less in the MidLIF group (42 vs. 133 mL, p = 0.007). Surgical time (170 vs. 210 minutes, p = 0.003) and length of hospital stay was significantly less in the MidLIF group (2.9 vs. 3.7 days, p = 0.016).
A sub-group analysis of single level cases (Table 3) showed similar results with less EBL (247 vs. 411 mL, p = 0.010), surgical time (159 vs. 199 minutes, p = 0.003), and hospital stay (2.9 vs. 3.6 days, p = 0.023) in the minimally invasive, MidLIF group.
Table 3.
Sub-analysis of single level cases.
| MidLIF | Open TLIF | p-value | |
|---|---|---|---|
| N | 23 | 22 | |
| Age, years, mean | 60.04 (7.59) | 58.45 (9.10) | 0.529 |
| BMI, kg/m [2], mean | 34.76 (6.11) | 35.67 (7.09) | 0.647 |
| Males | 5 | 8 | 0.279 |
| ASAGrade | 0.382 | ||
| 2 | 3 | 5 | |
| 3 | 20 | 16 | |
| 4 | 0 | 1 | |
| Estimated Blood Loss, cc, mean (SD) | 247 (127.10) | 411 (252.40) | 0.010 |
| Operative Time, min, mean (SD) | 159 (28.32) | 199 (50.74) | 0.003 |
| Length of Hospital Stay | 2.91 (1.16) | 3.64 (1.29) | 0.023 |
Patient reported outcomes (PROs) at baseline, 6 weeks, 3 months, 6 months, 12 months and 24 months are shown in Table 4. Pre-operative PROs showed a slightly lower baseline Back Pain in the MidLIF group (6.3 vs. 7.7, p = 0.003). Six week PROs showed greater ODI improvement in the MidLIF group (23 vs. 7, p = 0.008). Twelve-month PROs favored MidLIF with lower ODI (less lumbar disability) (26.7 vs. 43.1, p = 0.009), more improvement in ODI (23.1 vs. 7.3, p = 0.018) and less Back Pain (2.45 vs. 5.14, p = 0.002). Twenty-four month PROs also favored MidLIF with lower ODI (less lumbar disability) (26.9 vs. 47.1, p = 0.015) and less Back Pain (2.79 vs. 5.54, p = 0.019) compared to the open TLIF group.
Table 4.
Patient Reported Outcomes for patients with 12 month and 24 month follow-up.
| MidLIF |
Open TLIF |
p-value |
|||
| N |
29 |
27 |
|||
| N Baseline PROs | 28 | 24 | |||
| Mean |
SD |
Mean |
SD |
p-value |
|
| Baseline ODI | 48.11 | 16.28 | 54.03 | 18.86 | 0.239 |
| Baseline BP | 6.30 | 1.51 | 7.67 | 1.63 | 0.003 |
| Baseline LP | 6.14 | 2.45 | 7.21 | 2.23 | 0.106 |
| Baseline EQ5D |
0.56 |
0.21 |
0.46 |
0.25 |
0.247 |
| N 6 week PROs | 28 | 18 | |||
| Mean |
SD |
Mean |
SD |
p-value |
|
| 6 week ODI | 26.82 | 18.45 | 42.45 | 18.32 | |
| 6 week BP | 2.45 | 2.23 | 3.80 | 2.38 | 0.052 |
| 6 week LP | 1.55 | 2.01 | 2.65 | 2.25 | 0.088 |
| 6 week EQ5D | 0.76 | 0.17 | 0.66 | 0.16 | 0.132 |
| Change_6w_ODI | 22.85 | 18.20 | 6.66 | 18.98 | 0.008 |
| Change_6w_BP | 3.78 | 2.33 | 3.33 | 2.91 | 0.591 |
| Change_6w_LP | 4.71 | 2.61 | 3.94 | 3.67 | 0.446 |
| Change_6w_EQ5D |
0.24 |
0.25 |
0.28 |
0.16 |
0.612 |
| N 3 month PROs | 24 | 21 | |||
| Mean |
SD |
Mean |
SD |
p-value |
|
| 3 month ODI | 26.23 | 17.94 | 40.68 | 21.31 | |
| 3 month BP | 2.85 | 2.51 | 3.87 | 2.74 | 0.180 |
| 3 month LP | 2.33 | 2.59 | 3.17 | 3.08 | 0.307 |
| 3 month EQ5D | 0.71 | 0.22 | 0.60 | 0.25 | 0.178 |
| Change_3m_ODI | 24.63 | 22.86 | 13.23 | 20.23 | 0.083 |
| Change_3m_BP | 3.40 | 2.90 | 3.43 | 3.06 | 0.974 |
| Change_3m_LP | 3.69 | 3.75 | 3.62 | 3.44 | 0.945 |
| Change_3m_EQ5D |
0.16 |
0.28 |
0.24 |
0.23 |
0.509 |
| N 6 month PROs | 19 | 16 | |||
| Mean |
SD |
Mean |
SD |
p-value |
|
| 6 month ODI | 27.15 | 17.26 | 43.18 | 22.60 | |
| 6 month BP | 3.15 | 2.11 | 3.89 | 2.52 | 0.337 |
| 6 month LP | 2.45 | 3.27 | 3.17 | 2.64 | 0.460 |
| 6 month EQ5D | 0.72 | 0.23 | 0.57 | 0.23 | 0.143 |
| Change_6m_ODI | 22.32 | 21.00 | 9.00 | 23.46 | 0.096 |
| Change_6m_BP | 3.05 | 2.50 | 3.00 | 3.06 | 0.956 |
| Change_6m_LP | 4.11 | 3.89 | 3.25 | 2.84 | 0.458 |
| Change_6m_EQ5D |
0.13 |
0.21 |
0.15 |
0.16 |
0.898 |
| N 12 month PROs | 20 | 22 | |||
| Mean |
SD |
Mean |
SD |
p-value |
|
| 12 month ODI | 26.65 | 21.59 | 43.14 | 16.42 | 0.009 |
| 12 month BP | 2.45 | 2.50 | 5.14 | 2.61 | 0.002 |
| 12 month LP | 2.75 | 2.85 | 4.23 | 2.86 | 0.102 |
| 12 month EQ5D | 0.72 | 0.22 | 0.56 | 0.24 | 0.158 |
| Change_12m_ODI | 23.11 | 22.51 | 7.29 | 16.54 | 0.018 |
| Change_12m_BP | 3.61 | 2.81 | 2.35 | 2.54 | 0.157 |
| Change_12m_LP | 3.74 | 3.96 | 2.55 | 3.25 | 0.314 |
| Change_12m_EQ5D |
0.20 |
0.20 |
0.17 |
0.22 |
0.764 |
| N 24 month PROs | 14 | 13 | |||
| Mean |
SD |
Mean |
SD |
p-value |
|
| 24 month ODI | 26.86 | 21.21 | 47.08 | 19.06 | 0.015 |
| 24 month BP | 2.79 | 2.86 | 5.54 | 2.82 | 0.019 |
| 24 month LP | 3.23 | 3.42 | 4.62 | 2.66 | 0.261 |
| 24 month EQ5D | 0.73 | 0.24 | 0.61 | 0.24 | 0.198 |
| Change_24m_EQ5D | 0.12 | 0.24 | 0.17 | 0.24 | 0.622 |
| Change_24m_ODI | 16.50 | 21.98 | 4.82 | 12.19 | 0.107 |
| Change_24m_BP | 3.29 | 3.02 | 1.36 | 2.54 | 0.098 |
| Change_24m_LP | 2.85 | 4.10 | 1.73 | 2.05 | 0.399 |
ODI = Oswestry Disability Index (0–100), BP = Back pain (0–10), LP = Leg pain (0–10), EQ5D = EuroQol-5D (0–1).
Readmissions and reoperations are reported in Table 5. Readmission rates (<90 days) were not significantly different between groups. Late reoperations for symptomatic adjacent segment pathology (Adjacent Segment Disease) were significantly greater in the traditional open TLIF group (4/27 vs. 0/29, p = 0.048). Late reoperations for pseudoarthrosis were not significantly different between groups.
Table 5.
Re-admissions and Re-operations.
| MIDLIF N = 29 | Open TLIF N = 27 | p-value | |
|---|---|---|---|
| Readmission (<90 days) Total | 2 | 5 | 0.244 |
| Readmission (<90 days) for medical complication (chest pain) | 0 | 1 | 0.999 |
| Readmission (<90 days) with reoperation for wound complication | 1 | 2 | 0.605 |
| Readmission (<90 days) with reoperation for persistent radiculopathy | 1 | 1 | 1.000 |
| Late reoperation for Adjacent Segment Disease | 0 | 4 | 0.048 |
| Late reoperation for Pseudoarthrosis | 1 | 0 | 1.000 |
4. Discussion
The “MidLIF” using a cortical bone trajectory for pedicle screw fixation is a modification of the traditional midline exposure used in the open TLIF technique. The difference with this “minimally invasive” modification is limiting the exposure just lateral edge of the facet. Avoiding exposure lateral to the facet avoids elevating the multifidus, avoids detaching the longissimus from the transverse process, and potentially spares the neurovascular bundle to the erector spinae muscles. The concept of the cortical bone trajectory has made pedicle screw fixation possible through this limited midline exposure. Because the technique is relatively new, significant questions still remain. One of these questions is the “invasiveness” of the surgery. “Invasiveness” can be measured in various ways. The purpose of the current study was to look at three commonly measured perioperative parameters (i.e. surgical time, blood loss, and length of hospital stay) and to compare the new technique to the traditional technique. Secondarily, by looking at the existing literature, we are able to establish reference standards for open TLIF and minimally invasive TLIF.
The current study was designed as a single-surgeon series to minimize the inherent variability from surgeon to surgeon in experience and surgical technique. The study was designed as a consecutive series to minimize selection bias, as well as, present a “worse case scenario” for the learning curve of the new technique. Additionally, the transition period between the old technique and the new technique minimizes any confounding changes that may evolve over time in a surgeon's practice.
The current literature contains extensive comparisons between traditional open TLIF and minimally invasive TLIF [5, 6, 7, 8, 9, 12, 13, 14]. The term “minimally invasive TLIF” is most commonly used to refer to a paramedian approach where a tubular retractor and “percutaneous” screws are used to accomplish the surgical goals of decompression and stabilization. The tubular MIS TLIF literature has matured to the point where systematic reviews and meta-analyses are possible [5, 6, 7, 8, 9]. The majority of these recent meta-analyses have shown that there is no significant difference in surgical time between tubular MIS TLIF and Open TLIF [5, 7, 8, 9, 12, 13], with the exception of Hu [6] et al that showed increased operative time for the MIS group. All of the meta-analyses have consistently shown that EBL is lower in MIS TLIF when compared to Open TLIF. The results of the current study compare favorably to this best-available evidence regarding MIS TLIF (Table 6). Also, the results compare favorably to a recent comparative study from the same institution as the current study [15]. (Table 6).
Table 6.
Current study data for single level MidLIF cases compares favorably to literature controls for tubular “minimally invasive surgery” (MIS) TLIF.
| Comparative study or meta-analysis | EBL (cc), mean |
Difference favoring MIS (cc) | Surgical time (min), mean |
Difference favoring MIS (min) | ||
|---|---|---|---|---|---|---|
| MIS | Open | MIS | Open | |||
| Current (MidLIF) | 247 | 411 | 164 | 159 | 199 | 40 |
| Djurasovic (Comparative MIS) | 262 | 614 | 352 | 264 | 279 | NS |
| Xie (Meta-analysis MIS) | 224 | 506 | 266 | 195 | 198 | NS |
| Hu (Meta-analysis MIS) | 267 | 535 | 268 | 212 | 190 | * |
| Goldstein (Meta-analysis MIS) | NR | NR | 260 | NR | NR | NS |
| Phan (Meta-analysis MIS) | 177 | 461 | 256 | 185 | 186 | NS |
| Tian (Meta-analysis MIS) | NR | NR | 219 | NR | NR | NS |
NS = No Significant difference, NR = Not Reported, * = Favors open.
Limitations of the current study include the relatively small sample size and single surgeon series. Future studies with more patients and more surgeons are needed to determine if the same technique advantages are generalizable. Additionally, it is important to note that lack of formal posterolateral fusion (which is similar to the tubular TLIF techniques) likely requires successful interbody fusion for long-term success. Formal assessment of fusion was not possible in this series, as the majority of patients did not have postoperative computed tomography and plain radiographs are generally considered inadequate for fusion assessment. Although we did not see a significant difference in reoperation rates for pseudoarthrosis in this series, fusion success will depend on various patient specific and surgeon controlled variables that may become more apparent with additional experience and study.
The results of the study suggest that “minimally invasive” MidLIF compares favorably to open TLIF and MIS tubular TLIF with regards to EBL and surgical time. Importantly, patient reported outcomes and reoperation rates also favored MidLIF when compared to a traditional open TLIF technique. Future experience and study will ultimately determine if the procedure advantages are generalizable to a broader patient and surgeon population.
Declarations
Author contribution statement
Charles H. Crawford III: Conceived and designed the experiments; Performed the experiments; Analyzed and interpreted the data; Contributed reagents, materials, analysis tools or data; Wrote the paper.
Roger K. Owens II, Mladen Djurasovic, Jeffrey L. Gum: Performed the experiments; Contributed reagents, materials, analysis tools or data; Wrote the paper.
John R. Dimar II: Performed the experiments; Contributed reagents, materials, analysis tools or data.
Leah Y. Carreon: Conceived and designed the experiments; Analyzed and interpreted the data; Contributed reagents, materials, analysis tools or data.
Funding statement
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Competing interest statement
The authors declare the following conflict of interests: Charles H. Crawford III: is an employee of Norton Healthcare; received consulting fees from Alphatec, Medtronic and Nuvasive; received payments for speaking from Medtronic and Titan; received funds for trips and travel from SRS and NASS and is on the scientific board of Medtronic. Roger K. Owens II: is an employee of Norton Healthcare; receives consulting fees from Medtronic, Alphatec and Nuvasive; funds for trips and travel from DePuy, Sunthes. Mladen Djurasovic: is an employee of Norton Healthcare; receives consulting fees from Medtronic and Nuvasive, Jeffrey L. Gum: receives royalties from Acuity; receives consulting fees from Medtronic, DePuy, Alphatec, Stryker, Acuity, K2M, Nuvasuve, PacMed; receives honoraria from Pacira; John R. Dimar II: is an employee of Norton Healthcare; receives royalties, consulting and speaker fees from Medtronic, Member of Board of Directors of the Scoliosis Research Society Leah Y. Carreon: is an employee of Norton Healthcare; Member, Editorial Advisory Board, Spine Deformity, Spine and Spine Journal; Institutional Review Board Member, University of Louisville.
Additional information
No additional information is available for this paper.
References
- 1.Mirza S.K., Deyo R.A., Heagerty P.J., Konodi M.A., Lee L.A., Turner J.A. Development of an index to characterize the "invasiveness" of spine surgery: validation by comparison to blood loss and operative time. Spine (Phila Pa 1976) 2008 Nov 15;33(24):2651–2661. doi: 10.1097/BRS.0b013e31818dad07. [DOI] [PubMed] [Google Scholar]
- 2.Wu W.C., Smith T.S., Henderson W.G., Eaton C.B., Poses R.M., Uttley G. Operative blood loss, blood transfusion, and 30-day mortality in older patients after major noncardiac surgery. Ann. Surg. 2010 Jul;252(1):11–17. doi: 10.1097/SLA.0b013e3181e3e43f. [DOI] [PubMed] [Google Scholar]
- 3.Canan C.E., Myers J.A., Owens R.K., Crawford C.H., 3rd, Djurasovic M., Burke L.O. Blood salvage produces higher total blood product costs in single-level lumbar spinal surgery. Spine (Phila Pa 1976) 2013 Apr 15;38(8):703–708. doi: 10.1097/BRS.0b013e3182767c8c. [DOI] [PubMed] [Google Scholar]
- 4.Owens R.K., Crawford C.H., 3rd, Djurasovic M., Canan C.E., Burke L.O., Bratcher K.R. Predictive factors for the use of cell saver in lumbar spinal surgery. Spine (Phila Pa 1976) 2013 Feb 15;38(4):E217–E222. doi: 10.1097/BRS.0b013e31827f044e. [DOI] [PubMed] [Google Scholar]
- 5.Goldstein C.L., Macwan K., Sundararajan K., Rampersaud Y.R. Perioperative outcomes and adverse events of minimally invasive versus open posterior lumbar fusion: meta-analysis and systematic review. J. Neurosurg. Spine. 2016;24:416–427. doi: 10.3171/2015.2.SPINE14973. [DOI] [PubMed] [Google Scholar]
- 6.Hu W., Tang J., Wu X., Zhang L., Ke B. Minimally invasive versus open transforaminal lumbar fusion: a systematic review of complications. Int. Orthop. 2016;40:1883–1890. doi: 10.1007/s00264-016-3153-z. [DOI] [PubMed] [Google Scholar]
- 7.Phan K., Rao P.J., Kam A.C., Mobbs R.J. Minimally invasive versus open transforaminal lumbar interbody fusion for treatment of degenerative lumbar disease: systematic review and meta-analysis. Eur. Spine J. 2015;24:1017–1030. doi: 10.1007/s00586-015-3903-4. [DOI] [PubMed] [Google Scholar]
- 8.Tian N.F., Wu Y.S., Zhang X.L., Xu H.Z., Chi Y.L., Mao F.M. Minimally invasive versus open transforaminal lumbar interbody fusion: a meta-analysis based on the current evidence. Eur. Spine J. 2013;22:1741–1749. doi: 10.1007/s00586-013-2747-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Xie L., Wu W.J., Liang Y. Comparison between minimally invasive transforaminal lumbar interbody fusion and conventional open transforaminal interbody fusion: an updated meta-analysis. Chin. Med. J. 2016;129:1969–1986. doi: 10.4103/0366-6999.187847. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Raft J., Millet F., Meistelman C. Example of cost calculations for an operating room and a post-anaesthesia care unit. Anaesth. Crit. Care Pain Med. 2015 Aug;34(4):211–215. doi: 10.1016/j.accpm.2014.11.002. Epub 2015 May 27. [DOI] [PubMed] [Google Scholar]
- 11.Volpin A., Khan O., Haddad F.S. Theater cost is £16/Minute so what are you doing just standing there? J. Arthroplast. 2016 Jan;31(1):22–26. doi: 10.1016/j.arth.2015.08.008. [DOI] [PubMed] [Google Scholar]
- 12.Adogwa O., Parker S.L., Bydon A., Cheng J., McGirt M.J. Comparative effectiveness of minimally invasive versus open transforaminal lumbar interbody fusion: 2-year assessment of narcotic use, return to work, disability, and quality of life. J. Spinal Disord. Tech. 2011 Dec;24(8):479–484. doi: 10.1097/BSD.0b013e3182055cac. [DOI] [PubMed] [Google Scholar]
- 13.Price J.P., Dawson J.M., Schwender J.D., Schellhas K.P. Clinical and radiologic comparison of minimally invasive surgery with traditional open transforaminal lumbar interbody fusion: a review of 452 patients from a single center. Clin. Spine Surg. 2018 Mar;31(2):E121–E126. doi: 10.1097/BSD.0000000000000581. [DOI] [PubMed] [Google Scholar]
- 14.Singh K., Nandyala S.V., Marquez-Lara A., Fineberg S.J., Oglesby M., Pelton M.A. A perioperative cost analysis comparing single-level minimally invasive and open transforaminal lumbar interbody fusion. Spine J. 2014 Aug 1;14(8):1694–1701. doi: 10.1016/j.spinee.2013.10.053. [DOI] [PubMed] [Google Scholar]
- 15.Djurasovic M., Rouben D., Glassman S.D., Casnellie M., Carreon L.Y. Clinical Outcomes of Minimally Invasive versus Open TLIF: A Propensity-Matched Cohort Study. Am J Orthop. 2016;45(3):E77–E82. [PubMed] [Google Scholar]